Abstract
Background: Although 98% of mothers in our cohort initiated human milk (HM) provision for their very low–birthweight (VLBW) infants, fewer black infants received HM at neonatal intensive care unit (NICU) discharge than non-black infants. This study examined neighborhood structural factors associated with HM feeding at discharge to identify potential barriers.
Materials and Methods: Sociodemographic and HM data were prospectively collected for 410 VLBW infants and mothers. Geocoded addresses were linked to neighborhood structural factors. Bivariate and multivariate logistic regression analyses were conducted for the entire cohort and racial/ethnic subgroups.
Results: HM feeding at discharge was positively correlated with further distance from Women, Infants, and Children (WIC) office, less violent crime, less poverty, greater maternal education, older maternal age, greater infant gestational age, and shorter NICU hospitalization. Multivariate analysis demonstrated that only maternal race/ethnicity, WIC eligibility, and length of NICU hospitalization predicted HM feeding at discharge for the entire cohort. The interaction between access to a car and race/ethnicity significantly differed between black and white/Asian mothers, although the predicted probability of HM feeding at discharge was not significantly affected by access to a car for any racial/ethnic subgroup.
Conclusions: Neighborhood structural factors did not significantly impact HM feeding at discharge. However, lack of access to a car may be a factor for black mothers, potentially representing restricted HM delivery to the NICU or limited social support, and warrants further study.
Introduction
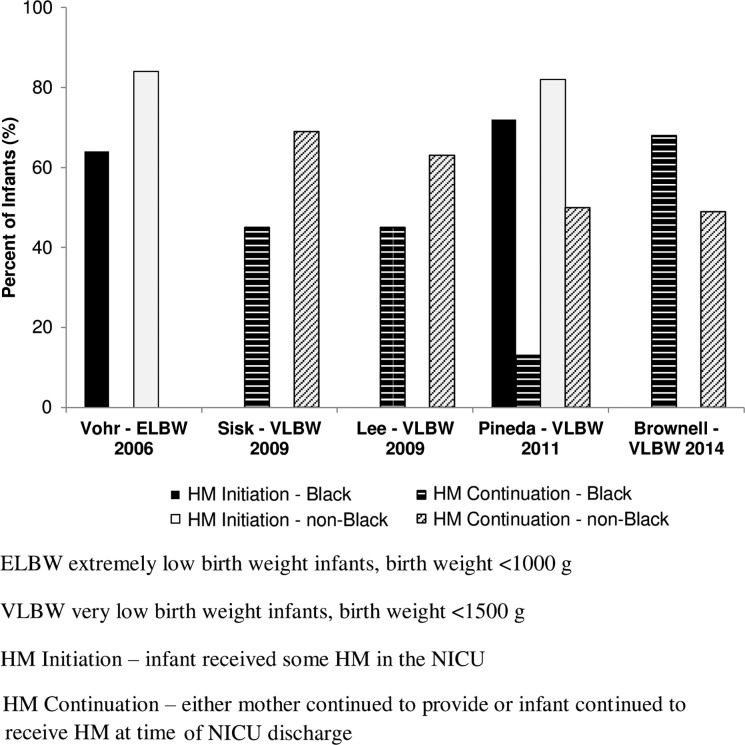
A significant body of evidence details the benefits of exclusive breastfeeding. Likewise, the American Academy of Pediatrics recommends exclusive breastfeeding for all infants for the first 6 months of life.1 Particularly for very low–birthweight (VLBW, birthweight <1500 g) infants, exclusive breastfeeding is associated with a decreased risk of developing prematurity-related morbidities and rehospitalizations, as well as a reduced risk of neurodevelopmental delays.2–4 Mothers of VLBW infants admitted to the neonatal intensive care unit (NICU) face unique barriers to exclusive breastfeeding when compared to mothers of term infants, especially the inability of the infant to feed directly at the breast and long-term breast pump dependency5,6 Beyond the barriers affecting all mothers of VLBW infants, most studies report a significant racial disparity with fewer black mothers of VLBW infants initiating and/or continuing HM feeding at NICU discharge compared to non-black mothers (Fig. 1).3,5,7–9
FIG. 1.
HM provision for premature infants in U.S. NICUs by maternal race/ethnicity. HM, human milk; NICU, neonatal intensive care unit.
In our recently completed prospective infant cohort study, 98% of the 430 VLBW infants born to racially diverse mothers (52% black, 19% white, 27% Hispanic, and 2% other) received HM, with no racial differences in lactation initiation.10 However, achievement of longer term goals for providing HM differed significantly for racial/ethnic categories as the NICU hospitalization progressed. Among black mothers, 78% indicated that their feeding goal closest to NICU discharge was to provide HM,11 but only 28% of their infants were discharged receiving any HM, a rate significantly lower than for non-black mothers (50%) (unpublished data). These findings shed new light on maternal goal setting for black mothers of VLBW infants, suggesting they wanted to continue to provide HM, but have environmental-specific barriers to achieving this goal.
Potential barriers faced by black mothers may be geospatially based, in that the neighborhood in which they reside and surrounding environs may negatively impact HM feeding at discharge through a constellation of neighborhood structural factors such as distance to the NICU or access to transportation to bring HM. Ideally, such neighborhood structural factors would apply to all racial/ethnic groups that reside in the area and may differ between communities, not by race/ethnicity but by the economic characteristics of the neighborhood. However, this conclusion does not take into consideration the long history of oppression, inequities, and institutional racism experienced by black women and their communities.12,13 Of note, the majority of black mothers in our cohort were also low income (84% Special Supplemental Nutrition Program for Women, Infants, and Children [WIC]14 eligible), and thus, neighborhood structural factors may particularly impact them more than other populations and the importance of neighborhood structural factors to child health is becoming increasingly evident.15
Previous research has revealed that reliance on public transportation and commuting long distances to the NICU negatively impact the frequency of maternal visitation to the NICU,16 and one study demonstrated a negative effect on pumping HM in mothers of VLBW infants.17 Furthermore, environments with greater poverty and high violent crime rates have been correlated with poor birth outcomes, poor maternal psychosocial well-being, harmful health behavior during pregnancy, and lower breastfeeding initiation,18,19 potentially contributing to the existing postnatal racial disparity in HM feeding at discharge by black mothers. Our objective was to identify whether neighborhood structural factors contributed to the disproportionate proportion of black VLBW infants who no longer received HM at time of discharge from the NICU.
Materials and Methods
Sample
This is a secondary analysis of an NIH-funded prospective cohort study examining health outcomes and cost of HM feedings in 430 VLBW infants born between February 2008 and December 2012 and admitted to the Level III NICU at Rush University Medical Center (RUMC) in Chicago, Illinois. Details of inclusion and exclusion criteria have been previously described.2,4,10,11 In cases of multiple births, one infant was randomly selected for study inclusion. In addition, initiation of lactation was not a criterion for study enrollment for either infant or the mother. Cases were excluded from the present analysis if the infant died before discharge (n = 7; 1.6%), the family lived out of state or more than 150 miles from RUMC (n = 5; 1.2%), or the mother was enrolled for a second VLBW birth within the 5-year study period (n = 3; 0.7%). Of the 415 eligible cases, complete data for all study variables were available for 410 (98.8%) cases that comprised the final sample.
As per standard practices in the RUMC NICU, all mothers received the same routine lactation information and services, including explanation and demonstration of breast pump use and milk collection and storage by certified breastfeeding peer counselors, who are former NICU parents and represent the racial/ethnic makeup of the patients cared for at Rush (black, white, and Hispanic).20 Nurse IBCLCs provide additional lactation support as needed in collaboration with peer counselors. All mothers initiate pumping with a hospital-grade pump and are able to rent a hospital-grade pump when discharged from the hospital with subsidized payment based on economic status and have access to a complimentary weekly taxi service to bring them to the NICU. The Rush University Institutional Review Board provided approval for this secondary analysis and signed informed consent was obtained from mothers for themselves and their infants for the original cohort study.
Measures
Data were prospectively collected for infants and their mothers. Maternal race/ethnicity (non-Hispanic white [white], non-Hispanic black [black], Hispanic, other [six Asian and one Native American]) were obtained from maternal questionnaires administered shortly after delivery and via maternal and infant medical records. Asian mothers were included in the white category for analyses for three reasons: the small number, nationally high rates of breastfeeding for Asian mothers,21 and similar socioeconomic characteristics to the white mothers in our cohort. The one Native American mother was excluded from analyses. Additional prospectively collected maternal data included age, highest educational level (less than high school, completed high school, less than 4 years of college, or 4 years of college or graduate degree), WIC eligibility (dichotomous), and home address. Prospectively collected infant characteristics included gender, birthweight (BW), gestational age (GA), length of NICU hospitalization (days), and daily intake (mL) of HM and formula from birth to NICU discharge. HM feeding at the time of infant discharge was determined by examining feedings on the last full day of hospitalization before NICU discharge and classifying infants into three mutually exclusive categories: exclusive HM (only fortified or unfortified HM, no formula); partial HM (some HM and some formula); and no HM (only formula).10
Home addresses for all participants were geocoded and linked to communities and census tracts. Neighborhood-level concentrated disadvantage22 was calculated for the census tract of residence for each participant. Concentrated disadvantage was calculated as a linear combination of four measures from the 2008–2012 American Community Survey23 (a) families below poverty, (b) renter-occupied housing, (c) unemployment, and (d) female-headed households. This measure is normed across all US census tracts as a z-score for each tract, allowing comparison relative to the average level of concentrated disadvantage in the United States. Rates (incidence per 100,000 residents) of neighborhood violent crime (murder, criminal sexual assault, robbery, and aggravated assault/battery) for the 2010 calendar year were obtained from the Chicago Police Department and Illinois State Police.24 Rates in the city of Chicago were calculated for each census tract, while suburban/rural rates were calculated for the entire community.
Geocoded addresses were used to calculate distances to the following locations: (a) RUMC; (b) the nearest WIC office as a marker of the neighborhood breastfeeding culture since during the study period, WIC offices in the greater Chicago area did not consistently have peer counselors or provide breast pumps and often provided formula,25 and (c) the nearest breastfeeding support as a marker of the neighborhood breastfeeding culture.26,27 Geocoding of addresses and calculation of distances were completed using ArcGIS version 10.2.2 (Esri, Redlands, CA). Access to the use of a car, either personal or through a friend or family member, was assessed in two ways. First, subjects who selected a monthly parking voucher as compensation for participation in the study were considered to have access to a car. Second, for subjects who selected a gift card instead of the monthly parking voucher, infant and maternal medical records and social work documentation were abstracted retrospectively to identify additional subjects who had access to a car.
Data analysis
The following neighborhood structural factors were examined in relation to HM feeding at discharge: (1) neighborhood concentrated disadvantage,18,28,29 (2) neighborhood violent crime rate,18 (3) distance to nearest WIC office,30 (4) distance to nearest breastfeeding support,28,29 (5) distance to RUMC,16,17 and (6) access to a car.16,17 Previous literature has demonstrated that these geospatial factors may influence either infant feeding decision or duration, maternal behavior prenatally and/or postnatally, as well as visitation frequency in mothers of term and preterm infants. Bivariate measures of association were evaluated using binary logistic regression. Multivariate binary hierarchical logistic regression analysis was used to regress HM at discharge on geospatial factors, controlling for maternal and infant characteristics. Predictor variables were entered in three steps. In the first step, maternal and child characteristics were entered. In the second step, geospatial factors were entered. In the third step, an interaction term between race/ethnicity and access to car was entered. Model-adjusted probabilities for the race/ethnicity by access to car interaction effect were calculated using planned estimates. Differences by access to car at each race/ethnicity were tested using planned contrasts. All analyses were conducted in SAS, version 9.3 (SAS Institute, Cary, NC). Significance set at p < 0.05 for all analyses.
Results
Characteristics of the sample
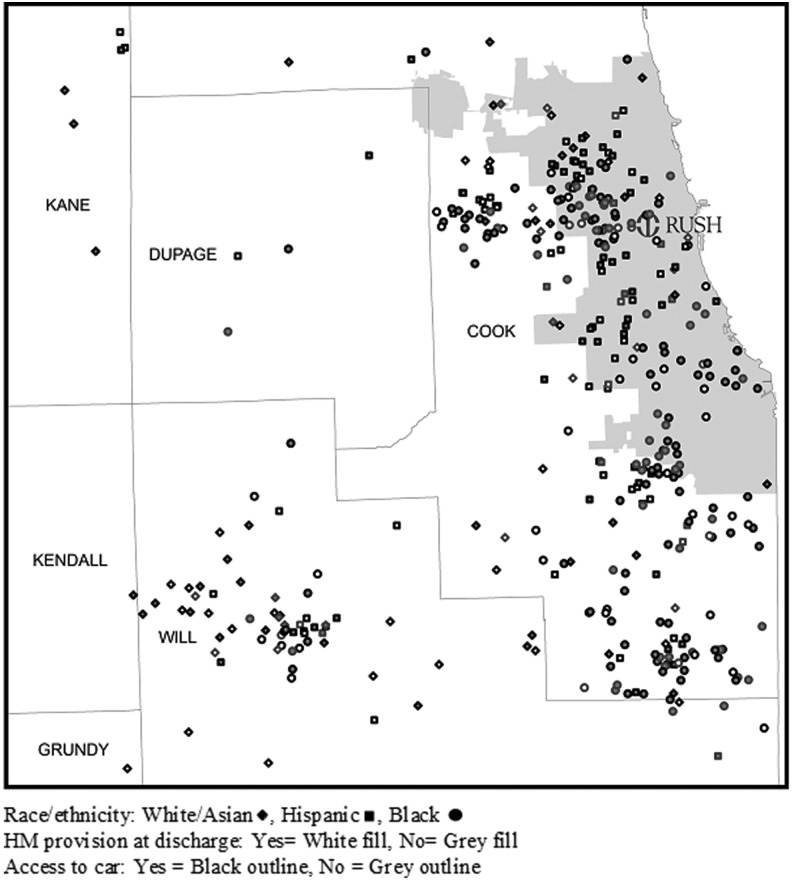
Table 1 summarizes the maternal and infant characteristics of the sample. Overall, the participants lived in areas with higher than average (0.8 standard deviations above the US means) levels of concentrated disadvantage and violent crime with 500 incidents of violent crime per 100,000 residents (compared to a national rate of 404 incidents per 100,000). Neighborhood concentrated disadvantage and crime were higher for black mothers than for white or Hispanic mothers. The average distance to the nearest WIC office was 2.1 miles, to the nearest breastfeeding support was 4.3 miles, and to RUMC was 16.4 miles. These distances were greater for whites than the other subgroups. More than two-thirds of participants had access to a car (Fig. 2).
Table 1.
Characteristics of Cohort
| Entire sample (N = 410) | White/Asian (n = 89) | Hispanic (n = 112) | Black (N = 209) | p | |
|---|---|---|---|---|---|
| Maternal characteristics | |||||
| Maternal age (years) | 27.2 ± 6.5 | 29.0 ± 5.7 | 28.0 ± 7.0 | 26.1 ± 6.3 | <0.001 |
| Maternal race/ethnicity | |||||
| White/Asian (non-Hispanic) | 89 (21.7%) | ||||
| Hispanic | 112 (27.3%) | ||||
| Black (non-Hispanic) | 209 (51.0%) | ||||
| WIC eligible | 299 (72.9%) | 33 (37.1%) | 90 (80.4%) | 176 (84.2%) | <0.001 |
| Maternal education | <0.001 | ||||
| Less than high school | 69 (16.8%) | 8 (9.0%) | 40 (35.7%) | 21 (10.0%) | |
| High school complete | 110 (26.8%) | 16 (18.0%) | 32 (28.6%) | 62 (29.7%) | |
| Some college or trade school | 153 (37.3%) | 31 (34.8%) | 26 (23.2%) | 96 (45.9%) | |
| Completed 4 years of college | 78 (19.0%) | 34 (38.2%) | 14 (12.5%) | 30 (14.4%) | |
| Infant characteristics | |||||
| Female | 190 (46.3%) | 40 (44.9%) | 53 (47.3%) | 97 (46.4%) | 0.945 |
| Gestational age (weeks) | 28.0 ± 2.4 | 27.7 ± 2.5 | 28.2 ± 2.4 | 28.0 ± 2.4 | 0.373 |
| Birthweight (g) | 1045 ± 255 | 1009 ± 242 | 1107 ± 250 | 1027 ± 258 | 0.009 |
| Length of NICU hospitalization (days) | 72.7 ± 35.4 | 77.3 ± 33.6 | 67.6 ± 30.6 | 73.4 ± 38.3 | 0.143 |
| Geospatial factors | |||||
| Neighborhood concentrated disadvantage (z-score) | 0.8 ± 1.3 | −0.3 ± 0.8 | 0.5 ± 0.7 | 1.3 ± 1.3 | <0.001 |
| Neighborhood violent crime rate (incidents per 100,000 residents) | 499 ± 522 | 205 ± 226 | 331 ± 256 | 714 ± 617 | <0.001 |
| Distance to nearest WIC office (miles) | 2.1 ± 2.1 | 4.3 ± 3.0 | 1.5 ± 1.2 | 1.6 ± 1.2 | <0.001 |
| Distance to nearest breastfeeding support (miles) | 4.3 ± 3.5 | 5.3 ± 5.3 | 4.0 ± 2.4 | 4.1 ± 2.9 | 0.008 |
| Distance to RUMC (miles) | 16.4 ± 11.5 | 24.3 ± 13.2 | 13.5 ± 10.7 | 14.6 ± 9.5 | <0.001 |
| Access to a car | 313 (76.3%) | 71 (79.8%) | 97 (86.6%) | 145 (69.4%) | 0.001 |
| Dependent variable | |||||
| HM continuation at NICU discharge | 136 (33.2%) | 38 (42.7%) | 49 (43.8%) | 49 (23.4%) | <0.001 |
Data reflect n (%) or mean ± SD. Neighborhood Concentrated Disadvantage values reflect z scores compared to the average level of concentrated disadvantage in the United States.
Bold values indicate p < 0.05.
HM, human milk; NICU, neonatal intensive care unit; RUMC, Rush University Medical Center; SD, standard deviation; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
FIG. 2.
HM provision at NICU discharge in the Greater Chicago Area.
Bivariate analyses of HM continuation
Table 2 shows bivariate correlations between HM feeding at discharge and sociodemographic and neighborhood structural factors. Factors that were significantly associated with increased HM feeding at discharge were maternal age, completing a 4-year college degree, older GA, greater BW, and greater distance to the nearest WIC office. Factors that were significantly associated with reduced likelihood of HM feeding at discharge included black race/ethnicity, WIC eligibility, longer NICU hospitalization, greater concentrated disadvantage, and more crime.
Table 2.
HM Feeding at Discharge—Bivariate and Multivariate Logistic Regression Analyses
| Bivariate analyses | Step 1 | Step 2 | Step 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Covariate | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Maternal characteristics | ||||||||
| Maternal age (years) | 1.08 (1.05–1.12) | <0.001 | 1.04 (1.00–1.08) | 0.041 | 1.04 (1.00–1.08) | 0.064 | 1.04 (1.00–1.09) | 0.042 |
| Maternal race/ethnicity | <0.001 | 0.006 | 0.020 | 0.062 | ||||
| White/Asian (Ref) | ||||||||
| Hispanic | 1.04 (0.60–1.83) | 0.881 | 1.89 (0.94–3.79) | 0.074 | 2.12 (0.95–4.70) | 0.065 | 0.99 (0.21–4.54) | 0.986 |
| Black/non-Hispanic | 0.41 (0.24–0.70) | 0.001 | 0.73 (0.39–1.38) | 0.338 | 0.88 (0.42–1.86) | 0.736 | 0.26 (0.07–1.00) | 0.051 |
| WIC eligible | 0.26 (0.16–0.41) | <0.001 | 0.39 (0.21–0.73) | 0.003 | 0.40 (0.21–0.75) | 0.005 | 0.41 (0.22–0.79) | 0.007 |
| Maternal education | <0.001 | 0.120 | 0.125 | 0.133 | ||||
| Less than high school (Ref) | ||||||||
| High school complete | 0.60 (0.30–1.18) | 0.135 | 0.71 (0.34–1.50) | 0.371 | 0.72 (0.33–1.53) | 0.387 | 0.68 (0.31–1.47) | 0.329 |
| Some college or trade school | 0.89 (0.48–1.65) | 0.710 | 0.95 (0.46–1.96) | 0.889 | 0.92 (0.44–1.92) | 0.826 | 0.87 (0.41–1.86) | 0.720 |
| Completed 4 years of college | 2.91 (1.48–5.73) | 0.002 | 1.79 (0.74–4.31) | 0.194 | 1.80 (0.74–4.36) | 0.196 | 1.67 (0.67–4.15) | 0.266 |
| Infant characteristics | ||||||||
| Female gender | 1.19 (0.79–1.80) | 0.403 | 1.08 (0.68–1.71) | 0.744 | 1.08 (0.68–1.72) | 0.754 | 1.05 (0.66–1.68) | 0.835 |
| Gestational age (weeks) | 1.09 (1.01–1.19) | 0.037 | 0.94 (0.80–1.10) | 0.465 | 0.96 (0.82–1.13) | 0.619 | 0.95 (0.81–1.12) | 0.560 |
| Birthweight (100 g) | 1.09 (1.00–1.18) | 0.049 | 0.94 (0.82–1.09) | 0.433 | 1.00 (1.00–1.00) | 0.491 | 0.94 (0.81–1.09) | 0.445 |
| Length of NICU hospitalization (days) | 0.99 (0.98–1.00) | 0.001 | 0.98 (0.97–0.99) | 0.002 | 0.98 (0.97–0.99) | 0.005 | 0.98 (0.97–0.99) | 0.003 |
| Geospatial factors | ||||||||
| Neighborhood concentrated disadvantage | 0.72 (0.60–0.86) | <0.001 | 1.00 (0.73–1.37) | 0.986 | 0.97 (0.71–1.34) | 0.877 | ||
| Neighborhood violent crime rate | 0.93 (0.89–0.98) | 0.003 | 1.00 (1.00–1.00) | 0.666 | 0.99 (0.93–1.07) | 0.891 | ||
| Distance to nearest WIC office | 1.11 (1.01–1.22) | 0.035 | 0.99 (0.83–1.18) | 0.948 | 1.01 (0.84–1.20) | 0.946 | ||
| Distance to nearest breastfeeding support | 0.96 (0.90–1.02) | 0.221 | 0.92 (0.83–1.00) | 0.060 | 0.92 (0.83–1.00) | 0.063 | ||
| Distance to RUMC | 1.01 (0.99–1.03) | 0.219 | 1.02 (0.99–1.05) | 0.165 | 1.02 (0.99–1.06) | 0.145 | ||
| Access to a car | 1.48 (0.89–2.45) | 0.129 | 1.08 (0.61–1.92) | 0.785 | 0.37 (0.11–1.21) | 0.100 | ||
| Race/ethnicity and access to a car | 0.100 | |||||||
| White/Asian (Ref) | ||||||||
| Hispanic | 2.71 (0.50–14.58) | 0.245 | ||||||
| Black | 4.84 (1.14–20.44) | 0.032 | ||||||
Bold values indicate p < 0.05.
OR, odds ratio.
Multivariate binary logistic regression analysis
In the multivariate logistic regression analysis, race/ethnicity, WIC eligibility, and length of NICU hospitalization remained statistically significant predictors of HM feeding at discharge (Table 2, steps 1–3). To further investigate the significant differences in HM feeding at discharge by race/ethnicity, we explored interactions between predictors and race/ethnicity. The interaction between access to a car and race/ethnicity was significantly different for black mothers compared to white mothers (step 3). To explore this interaction, we calculated predicted probabilities for access to a car and HM feeding at discharge (Table 3). No significant impact of access to car was detected for any of the race/ethnicity subgroups.
Table 3.
Adjusted Predicted Probability of HM Continuation by Race/Ethnicity and Access to a Car
| Race/ethnicity and car access | HM continued probability | p |
|---|---|---|
| White/Asian | 0.099 | |
| Car access = yes | 0.23 | |
| Car access = no | 0.45 | |
| Hispanic | 0.986 | |
| Car access = yes | 0.45 | |
| Car access = no | 0.44 | |
| Black | 0.155 | |
| Car access = yes | 0.27 | |
| Car access = no | 0.17 |
Discussion
To our knowledge, this is the first study to examine the impact of geospatial factors on HM feeding at discharge in a racially diverse cohort of mothers of VLBW infants admitted to the NICU. Although multiple factors, including neighborhood structural factors, were associated with HM feeding at discharge in bivariate analyses, only race/ethnicity, WIC eligibility, and length of NICU hospitalization significantly predicted HM feeding at discharge in multivariate logistic regression analysis. Our findings are similar to a large national study which reported that socioeconomic status affected breastfeeding rates in all racial/ethnic groups, but disproportionately affected black mothers to a greater degree than white or Hispanic mothers.31 Previous research supports the impact of maternal age on rates of breastfeeding and/or HM provision in mothers of term and preterm infants.8,19,32 However, in our cohort, maternal age was marginally significant suggesting that other parental and neighborhood factors may partially mediate the effect of maternal age seen in other studies. Burdette also found no effect of maternal age on breastfeeding behavior with adjustment for neighborhood context in a study of urban mothers.28
The literature addressing the relationship between the duration of NICU hospitalization and HM feeding at NICU discharge is inconclusive. Consistent with our findings, a large study of 6,790 VLBW infants demonstrated that a shorter NICU hospitalization was associated with higher rates of HM feeding at discharge.7 In contrast, a shorter NICU hospitalization did not significantly predict HM feeding at discharge in two smaller studies of VLBW infants.5,8 We theorize that longer NICU hospitalization could negatively impact HM feeding at discharge since mothers would be breast pump dependent for a longer time. In addition, longer NICU hospitalization may reflect a greater degree of infant prematurity and/or severity of illness, which could be associated with greater maternal lactation risk, including chronic illness and stress.33,34
Previous studies have reported the negative impact of neighborhood violent crime rate and neighborhood economic disadvantage on pregnancy, breastfeeding, and childhood outcomes, including allostatic load, which is the “wear and tear” on the body, potentially leading to increased cardiometabolic risk, in response to chronic actual or perceived stress.18,28,29,35 While allostatic load has not been directly linked to lactation to our knowledge, it may provide a mechanistic link between neighborhood structural factors and lactation outcomes. Burdette reported an association between neighborhood economic deprivation and lower odds of initiation but not duration of breastfeeding, even after accounting for individual socioeconomic factors in a longitudinal low-income non-NICU birth cohort.28 In contrast, Cubbin et al. reported no relationship between neighborhood factors and breastfeeding initiation after accounting for individual socioeconomic factors in a secondary analysis of CDC data.19
However, the impact of neighborhood structural factors on HM feeding at discharge for VLBW infants has not been examined until now. Our data demonstrate that black families disproportionately live in lower socioeconomic neighborhoods. However, despite these differences, we did not find an effect of neighborhood structural factors on lactation initiation or HM feeding at discharge in the entire cohort. We speculate that the intensive lactation support in our NICU may have mitigated the effect of neighborhood structural factors. Alternatively, this lack of effect may be a function of prematurity and/or infant vulnerability, because mothers of VLBW infants provide HM at rates higher than the general US population.36 In addition, the impact of neighborhood factors may have been accounted for when we adjusted for individual-level socioeconomic factors.
Neither distance to the nearest breastfeeding support nor distance to RUMC remained significant predictors of HM feeding at discharge despite other studies' findings of a positive association between information/support within one's neighborhood and rates for breastfeeding initiation and duration.28 Similarly, whereas access to peer counselors and related breastfeeding resources improves breastfeeding outcomes, in particular, for low-income women or those who are geographically and/or socially isolated,17 the mothers in our study received NICU-specific lactation support, perhaps lessening the impact of these neighborhood factors. Examining the impact of distance to the NICU on HM feeding at discharge for VLBW infants has been studied minimally. According to Sisk et al., as the distance to the NICU increased for their rural population, issues such as difficulty adhering to a pumping schedule and/or the cost of gasoline posed potential barriers to HM maintenance for mothers of VLBW infants.17 Although we had hypothesized that distance to the NICU would be a significant barrier, this was not significant in our study. This may be due to the urban location of our NICU, such that greater distance is associated with suburban and potentially more affluent neighborhoods, which may enable mothers with resources to compensate for the increased distance and travel time to the NICU (Fig. 2). Although only indirectly related to HM provision, increasing geographical distance from the NICU reduces the frequency of maternal visits to the NICU in some studies,16 while not affecting it in others.37
The interaction between race/ethnicity and access to a car was significantly different for black mothers compared to white mothers. Having access to a car was associated with a nonsignificant increase in HM feeding at discharge for black mothers, while the opposite direction of effect was noted in white mothers. However, further analyses did not reveal a significant impact of access to car on the predicted probability of HM feeding at discharge for any racial/ethnic subgroup. We were surprised at this finding as we had theorized that lack of access to a car could reflect a barrier for black mothers to visiting their infants and bringing HM to the NICU, or reliance on public transportation could compromise pumping schedule,17 or lack of access to a car could represent limited social support.38 Other research has reported a significant difference in participation in health promotion activities such as breast cancer screening with limited or no access to a car.39 Our findings may reflect the urban setting of our NICU where public transportation is more readily available than in more rural settings. Although the study NICU provides a taxi service to attend weekly meetings, this frequency may not be adequate to support the maintenance of HM provision for the prolonged NICU hospitalization.
A limitation of this study is the use of infant HM feedings at time of discharge to represent mothers continuing to provide HM. It is possible that we may have overestimated the HM provision rate by including infants who continued to receive stored frozen HM from earlier in the NICU hospitalization. However, similar studies have also used the infant's receipt of HM at discharge as the primary outcome measure for the maintenance of maternal lactation because of its objectivity versus mothers' self-report of pumping.5,7–9 In addition, there were other elements that may have influenced HM provision at NICU discharge that were not measured, such as the impact of perceived racial discrimination and the type of support system at home. This is also a single-center study with an intensive, evidence-based in-NICU lactation support program.40 However, even with these resources, black mothers did not achieve their personal HM feeding goals.
Strengths of this study included the large racially and ethnically diverse sample with extensive detailed data allowing robust statistical modeling. The study also used innovative geospatial analyses to investigate a significant clinical concern with public health implications.
Conclusion
While neighborhood structural factors were associated with HM feeding at discharge, none was a significant barrier for the entire cohort of mothers. Socioeconomic factors were identified as significant predictors for HM feeding at discharge, consistent with findings from earlier studies on this topic. There was a trend of decreased HM feeding at discharge in black mothers without access to a car. Future studies should seek to determine if access to a car, or the ease of access to the NICU and/or social support that a car may represent for mothers, is a significant barrier in other populations, especially in relation to maternal socioeconomic status, and other locations such as rural settings where distances may be greater or there may be limited alternate means of transportation.
Acknowledgments
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R03HD081412. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.Eidelman AI, Schanler RJ. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–e841 [DOI] [PubMed] [Google Scholar]
- 2.Patel AL, Johnson TJ, Engstrom JL, et al. Impact of early human milk on sepsis and health care costs in very low birthweight infants. J Perinatol 2013;33:514–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vohr BR, Poindexter BB, Dusick AM, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics 2006;118:e115–e123 [DOI] [PubMed] [Google Scholar]
- 4.Johnson TJ, Patel AL, Bigger HR, et al. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology 2015;107:271–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pineda RG. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed Med 2011;6:15–19 [DOI] [PubMed] [Google Scholar]
- 6.Meier PP, Engstrom JL, Janes JE, et al. Breast pump suction patterns that mimic the human infant during breastfeeding: Greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol 2012;32:103–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee HC, Gould JB. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J Pediatr 2009;155:657–662.e1–e2. [DOI] [PubMed] [Google Scholar]
- 8.Sisk PM, Lovelady CA, Dillard RG, et al. Maternal and infant characteristics associated with human milk feeding in very low birth weight infants. J Hum Lact 2009;25:412–419 [DOI] [PubMed] [Google Scholar]
- 9.Brownell EA, Lussier MM, Hagadorn JI, et al. Independent predictors of human milk receipt at neonatal intensive care unit discharge. Am J Perinatol 2014;31:891–898 [DOI] [PubMed] [Google Scholar]
- 10.Bigger HR, Fogg LJ, Patel A, et al. Quality indicators for human milk use in very low-birthweight infants: Are we measuring what we should be measuring? J Perinatol 2014;34:287–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoban R, Bigger H, Patel AL, et al. Goals for human milk feeding in mothers of very low birth weight infants: How do goals change and are they achieved during the NICU hospitalization? Breastfeed Med 2015;10:305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis AY. Women, Race, & Class. New York: Random House, 1981 [Google Scholar]
- 13.Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. New York: Routledge, 2008 [Google Scholar]
- 14.U.S. Department of Agriculture. WIC Income Eligibility Guidelines 2013–2014. Updated 2013. Available at http://origin.www.fns.usda.gov/wic/howtoapply/incomeguidelines.htm (accessed June30, 2014)
- 15.Jutte DP, Miller JL, Erickson DJ. Neighborhood adversity, child health, and the role for community development. Pediatrics 2015;135 Suppl 2:S48–S57 [DOI] [PubMed] [Google Scholar]
- 16.Latva R, Lehtonen L, Salmelin RK, et al. Visits by the family to the neonatal intensive care unit. Acta Paediatr 2007;96:215–220 [DOI] [PubMed] [Google Scholar]
- 17.Sisk PM, Quandt S, Parson N, et al. Breast milk expression and maintenance in mothers of very low birth weight infants: Supports and barriers. J Hum Lact 2010;26:368–375 [DOI] [PubMed] [Google Scholar]
- 18.Anthopolos R, Kaufman JS, Messer LC, et al. Racial residential segregation and preterm birth: Built environment as a mediator. Epidemiology 2014;25:397–405 [DOI] [PubMed] [Google Scholar]
- 19.Cubbin C, Marchi K, Lin M, et al. Is neighborhood deprivation independently associated with maternal and infant health? Evidence from Florida and Washington. Matern Child Health J 2008;12:61–74 [DOI] [PubMed] [Google Scholar]
- 20.Meier PP, Engstrom JL, Rossman B. Breastfeeding peer counselors as direct lactation care providers in the neonatal intensive care unit. J Hum Lact 2013;29:313–322 [DOI] [PubMed] [Google Scholar]
- 21.Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolan PH, Gorman-Smith D, Henry DB. The developmental ecology of urban males' youth violence. Dev Psychol 2003;39:274–291 [DOI] [PubMed] [Google Scholar]
- 23.United States Census Bureau. Design and Methodology: American Community Survey. Washington, DC: U.S. Government Printing Office, 2014 [Google Scholar]
- 24.United States Department of Justice. Summary Reporting System (SRS) User Manual. Clarksburg, WV: Federal Bureau of Investigation, 2013 [Google Scholar]
- 25.Illinois WIC Program Locations. Available at www.wicprograms.org/state/illinois (accessed September17, 2013)
- 26.Breastfeed Chicago website. Available at https://maps.google.com/maps/ms?msid=202719338434082760314.0004c123df27e636bfd1f&msa=0&ie=UTF8&t=m&ll=41.916585,-87.684631&spn=0.981013,1.757813&z=9&source=embed (accessed September17, 2013)
- 27.La Leche League. Available at www.llli.org/search/groups (accessed September17, 2013)
- 28.Burdette AM. Neighborhood context and breastfeeding behaviors among urban mothers. J Hum Lact 2013;29:597–604 [DOI] [PubMed] [Google Scholar]
- 29.Vinikoor-Imler LC, Messer LC, Evenson KR, et al. Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Soc Sci Med 2011;73:1302–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ware JL, Webb L, Levy M. Barriers to breastfeeding in the African American population of Shelby county, Tennessee. Breastfeed Med 2014;9:385–392 [DOI] [PubMed] [Google Scholar]
- 31.Li R, Grummer-Strawn L. Racial and ethnic disparities in breastfeeding among United States infants: Third national health and nutrition examination survey, 1988–1994. Birth 2002;29:251–257 [DOI] [PubMed] [Google Scholar]
- 32.Omarsdottir S, Adling A, Bonamy AKE, et al. Predictors of sustained maternal milk feeds in extremely preterm infants. J Perinatol 2015;35:367–372 [DOI] [PubMed] [Google Scholar]
- 33.Lau C, Hurst NM, Smith EO, et al. Ethnic/racial diversity, maternal stress, lactation and very low birthweight infants. J Perinatol 2007;27:399–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dewey KG. Maternal and fetal stress are associated with impaired lactogenesis in humans. J Nutr 2001;131:3012S–3015S [DOI] [PubMed] [Google Scholar]
- 35.Brody GH, Lei MK, Chen E, et al. Neighborhood poverty and allostatic load in African American youth. Pediatrics 2014;134:e1362–e1368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colaizy TT, Saftlas AF, Morriss FH., Jr. Maternal intention to breast-feed and breast-feeding outcomes in term and preterm infants: Pregnancy risk assessment monitoring system (PRAMS), 2000–2003. Public Health Nutr 2012;15:702–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gonya J, Nelin LD. Factors associated with maternal visitation and participation in skin-to-skin care in an all referral level IIIc NICU. Acta Paediatr 2013;102:e53–e56 [DOI] [PubMed] [Google Scholar]
- 38.Greene MM, Rossman B, Patra K, et al. Depression, anxiety, and perinatal-specific posttraumatic distress in mothers of very low birth weight infants in the neonatal intensive care unit. J Dev Behav Pediatr 2015;36:362–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jensen LF, Pedersen AF, Andersen B, et al. Distance to screening site and non-participation in screening for breast cancer: A population-based study. J Public Health 2014;36:292–299 [DOI] [PubMed] [Google Scholar]
- 40.Meier PP, Patel AL, Bigger HR, et al. Supporting breastfeeding in the neonatal intensive care unit: Rush mother's milk club as a case study of evidence-based care. Pediatr Clin North Am 2013;60:209–226 [DOI] [PubMed] [Google Scholar]