Abstract
Background
The present study aimed at determining whether 12 weeks of yoga practice in patients with chronic LBP and MRI-based degenerative changes would result in differences in: (i) self-reported pain, anxiety, and spinal flexibility; and (ii) the structure of the discs or vertebrae.
Material/Methods
Sixty-two persons with MRI-proven degenerative intervertebral discs (group mean ±S.D., 36.2±6.4 years; 30 females) were randomly assigned to yoga and control groups. However, testing was conducted on only 40 subjects, so only their data are included in this study. The assessments were: self-reported pain, state anxiety, spinal flexibility, and MRI of the lumbosacral spine, performed using a 1.5 Tesla system with a spinal surface column. The yoga group was taught light exercises, physical postures, breathing techniques, and yoga relaxation techniques for 1 hour daily for 3 months. No intervention was given to the control group except for routine medical care. A repeated-measures analysis of variance (ANOVA) with post hoc analyses (which was Bonferroni-adjusted) was used. The Ethics Committee of Patanjali Research Foundation had approved the study which had been registered in the Clinical Trials Registry of India (CTRI/2012/11/003094).
Results
The yoga group showed a significant reduction in self-reported pain and state anxiety in a before/after comparison at 12 weeks. A few patients in both groups showed changes in the discs and vertebrae at post-intervention assessment.
Conclusions
Within 12 weeks, yoga practice reduced pain and state anxiety but did not alter MRI-proven changes in the intervertebral discs and in the vertebrae.
MeSH Keywords: Anxiety, Low Back Pain, Magnetic Resonance Imaging, Yoga
Background
Low back pain (LBP) is one of the most common and significant clinical, social, economic, and public health problems affecting people all over the world [1]. Most back pain has no demonstrable cause on imaging studies and is usually attributed to muscle strain or ligament injuries in 65–70% of cases [2]. In 5–15% of cases the source of LBP is degenerative joints and intervertebral disc diseases [3]. Cases of disc herniation may undergo improvement in symptoms with spontaneous resolution of the LBP but 37–50% persist for 12 or more months [1,4].
Apart from conservative therapy, all other forms of treatment are targeted at decompression of the nerve roots. This is usually done by surgical intervention. Outcome studies of lumbar disc surgeries document a success rate of between 49–95% [5]. The same author [5] reported recurrence of pain after surgery, ranging from 4–15%, after which there is an approximately 15% chance of further recurrence of pain.
With this background of a varying outcome of surgical interventions, there is increasing interest in non-surgical methods to manage LBP. Some of the conventional methods include epidural steroid injections or nerve root sleeve block [5]. Another approach is to use physiotherapy or complementary and alternative therapies. In a survey, LBP was the most common medical condition for which people used complementary and alternative medicine [6]. Many patients with LBP have used yoga as the complementary therapy of choice [7,8].
There have been several studies assessing the effectiveness of yoga for chronic LBP. Those studies most relevant to the present trial are briefly reviewed here. A 1-year randomized controlled trial (RCT) demonstrated that the benefits obtained by yoga practice after 3 months were sustained [9]. The study randomized 313 adults with chronic or recurrent LBP to yoga or usual care. Assessments were performed at 3, 6, and 12 months. The yoga group had better back function at 3 [−2.4 (mean changes from baseline)], 6 [−1.7 (mean changes from baseline)], and 12 months [−0.7 (mean changes from baseline)] compared with the usual care group. Both groups had similar back pain and general health scores at 3, 6, and 12 months. The yoga group had higher pain self-efficacy scores, indicating better self-efficacy at 3 and 6 months. The overall conclusion was that a 12-week yoga program followed by home practice led to greater improvement in back function compared to usual care.
Twelve weeks of yoga were beneficial in 101 adults with chronic LBP [10]. Participants were randomized to 3 groups: (i) yoga, (ii) conventional exercise classes, and (iii) self-care based on a book. Participants of the yoga and exercise groups practiced 75-min classes for 12 weeks. The yoga intervention was viniyoga, which included 5–12 postures and breathing exercises, guided deep relaxation, and a question and answer session. The exercise session consisted of simple warm-ups, repetitions of a series of 7 aerobic exercises and strengthening exercises, and an educational talk. The self-care group participants were mailed a copy of a back pain self-help book. After 12 weeks, there were the following changes: the yoga group was significantly better in back-related functions compared to the self-help book and exercise groups; and at 26-week followed-up, the yoga group was more effective than the self-help group with respect to patients’ reported function [−3.6 (mean score difference)].
Another RCT described the benefits of yoga on chronic LBP where the intervention was intensive and short-term (7 days) [11,12]. One of the studies was a randomized controlled single-blind study on 80 patients assigned to yoga and physical exercise groups [12]. The yoga intervention consisted of specific postures, breathing exercises, meditation, counseling, and lectures on yoga philosophy. The physical exercise group had regular physical therapy exercises for back pain and comparable counseling and lectures as the yoga group. While both groups showed significant reduction in pain, depression, and spinal flexibility, state and trait anxiety were lower in the yoga alone group.
There have been other randomized controlled trials which have shown the benefits of yoga practice for specific ethnic groups [13] and specific yoga interventions [14].
In all the studies cited above, the outcome measures were pain or associated self-reported assessments such as self-efficacy [9] and quality of life [13]. Magnetic resonance imaging (MRI) in a single study [15] evaluated the effects of yoga on the vertebral column. This was a matched-pairs study. Eighteen yoga instructors who had over 10 years of experience were compared with 18 asymptomatic persons who were not yoga practitioners. The cervical and lumbar discs visualized with a spinal MRI were graded using a scale previously validated. The overall disc scores for cervical plus lumbar discs indicated fewer non-significant degenerative changes compared to the control group. The study compared 2 groups of normal individuals, while those with disc abnormalities were not included. The findings were interpreted as suggestive of slowing normally occurring, disc degenerative changes with yoga practice.
This is possibly the first study to evaluate MRI changes in LBP after yoga. Hence, the present study aimed at determining whether patients with chronic LBP and MRI-based degenerative changes would show: (i) changes in self-reported pain, anxiety, and spinal flexibility; and (ii) structural changes in the vertebrae and intervertebral discs after 12 weeks of yoga practice.
Material and Methods
Participants
Sixty-two persons with MRI-proven degenerative changes in the intervertebral discs based on a standard grading system [16] detailed below participated in the trial. Their ages were between 20 and 45 years (group mean ±S.D., 36.22±6.39 years; 30 females). The effect size and power are based on a study which reported changes in visual analog scales for pain following 4 weeks of Iyengar yoga for chronic low back pain [14]. Based on this, the effect size is 0.63 (large), Cohen’s d=1.64, and Power=0.669 [17]. Participants stayed close to a residential yoga center in north India. They were recruited through advertisements in local newspapers and flyers in primary care hospitals close to the center. To be included in the trial, the criteria were: (i) pathological changes in at least 1 intervertebral disc based on a standard grading system detailed below [15] and determined from the MRI report, (ii) willingness to follow the study protocol, and (iii) age between 20 and 45 years. Participants were excluded if they had any of the following: (i) previous spinal surgery, (ii) central canal stenosis, (iii) compromised cardiovascular functions, (iv) pregnancy, or (v) inability to comply with the study protocol due to mental health disorders or any other conditions. Their participation was voluntary and no incentive was given to them. After preliminary assessments, the 62 participants were randomly assigned to 2 groups; the baseline characteristics are given in Table 1. Signed informed consent of all participants was obtained after the study protocol was explained to them. The Ethics Committee of Patanjali Research Foundation had approved the study, which had been registered in the Clinical Trials Registry of India (CTRI/2012/11/003094). The trial was carried out between July and September 2011.
Table 1.
Baseline characteristics of yoga and control groups.
| Groups | Yoga (n=20) | Control (n=20) |
|---|---|---|
| Age (in years) | 36.10 (7.33)* | 37.40 (4.85)* |
| Age range (years) | 20–45 | 32–45 |
| Gender ratio (M: F) | 9: 11 | 8: 12 |
| NSAIDs or analgesic tablets per day in past two weeks | ||
| Nil | 15 (75.00%) | 11 (55.00%) |
| 1–8 | 3 (15.00%) | 5 (25.00%) |
| >8 | 2 (10.00%) | 4 (20.00%) |
| PAS (in cm); (n=20 in each group) | 6.36 (2.29)* | 6.13 (2.83)* |
| STAI-S Scores (n=20 in each group) | 48.40 (12.63)* | 48.80 (11.60)* |
| Spinal Flexibility (in cm); (n=20 in each group) | 17.06 (10.11)* | 17.50 (9.04)* |
| MRI testing (n) | 20 | 20 |
n – number of participants at pre assessment;
values are group mean (S.D.);
M – Male; F – Female; PAS – pain analogue scale; STAI-S – state anxiety.
Study design
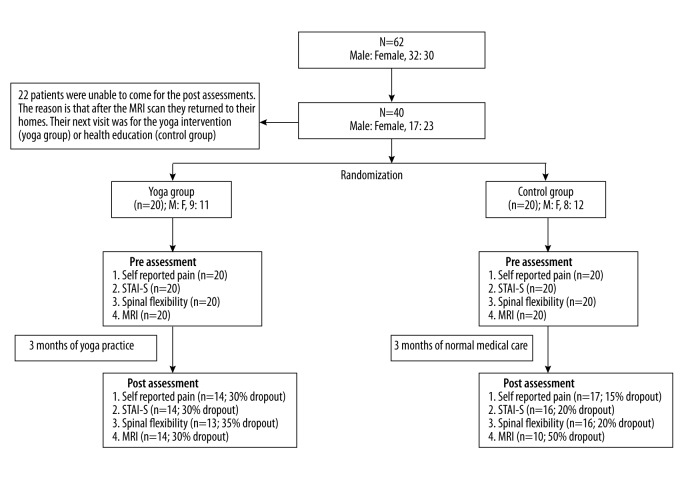
Participants were randomly assigned to yoga and waitlist control groups using a computer-generated random number sequence [18]. Randomization was carried out as follows. (i) Participants were given numbers from 1 to 62 which were not dependent on their names, the order in which they were enrolled, or any other factor. (ii) Sixty-two random numbers were generated using specific software [18]. (iii) In a separate column adjacent to the serial numbers of the participants, all the random numbers were written. (iv) Identical-sized pieces of paper were used to write the random numbers. They were folded identically and mixed. (v) The slips of paper were placed alternately in 2 boxes (labeled as Box ‘A’ and Box ‘B’) by a person who was unaware of the trial. (vi) Individuals allotted to Group ‘A’ were given the yoga intervention while individuals in group ‘B’ were assigned to the waitlist control group. In 22 of the 62 participants we were unable to collect data on (i) visual analog scales for pain, (ii) sit and reach for spinal flexibility, and (iii) STAI-S because after the MRI scan they returned to their homes. Their next visit was for the yoga intervention (yoga group) or health education (control group). Hence, the data of 40 participants randomized to yoga and control groups is presented. Accordingly, Table 2 (MRI data) presents data on these 40 patients. Figure 1 is the Trial Profile, which mentions the number of participants in yoga and control groups at different stages. Hence, both groups were allocated 20 participants each and in this way the study design is a parallel group design with an allocation ratio of 1:1. Recruitment of the participants was done in June 2011 and post-intervention assessments were completed in October 2011.
Table 2.
Details about disc degeneration (grade), and vertebral changes (nerve compression, endplate changes, and facet joint changes) for yoga and waitlist control groups.
| Group | Intervertebral disc grades | Nerve compression | Endplate changes | Facet joint changes | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Pre (n=20 in yoga; 20 in control) | Post (n=14 in yoga; 10 in control) | Pre (n=20 in yoga; 20 in control) | Post (n=14 in yoga; 10 in control) | Pre (n=20 in yoga; 20 in control) | Post (n=14 in yoga; 10 in control) | Pre (n= 20 in yoga; 20 in control) | Post (n=14 in yoga; 10 in control) | |
| Yoga | Grade 1, n=9 | Grade 1, n=6 (1 changed from Grade 2 to 1), (3 changed to Grade 2), (1 dropout, out of 9) | Present, n=13 | Present n=8, (5 dropouts, out of 13) | Present, n=13 | Present, n=9 (n=1, present to normal), (3 dropouts, out of 13) | Normal, n=20 | Normal, n=14, (6 drop-outs, out of 20) |
| Grade 2, n=9 | Grade 2, n=8 (3 changed from Grade 1 to 2), (1 changed to Grade1), (3 dropouts, out of 9) | Not present, n=7 | Not present, n=6, (1 dropout, out of 7) | Normal, n=7 | Normal, n=5, (n=1, present to normal), (3 dropouts, out of 7) | |||
| Grade 3, n=1 | Grade 3, n=0 (1 dropout, out of 1) | |||||||
| Grade 4, n=1 | Grade 4, n=0 (1 dropout, out of 1) | |||||||
|
| ||||||||
| Control | Grade 1, n=10 | Grade 1, n=5 (2 changed from Grade 2 to 1), (2 changed to Grade 2), (5 dropouts, out of 10) | Present, n=13 | Present n=9, (4 dropouts, out of 13) | Present, n=14 | Present n=9, (n=1, normal to present), (6 dropouts, out of 14) | Normal, n=20 | Normal, n=10, (10 drop-outs, out of 20) |
| Grade 2, n=8 | Grade 2, n=5, (2 changed from Grade 2 to 1), (2 changed to Grade 2), (3 dropouts, out of 8) | Not present, n=7 | Not present, n=1, (6 dropouts, out of 7) | Normal, n=6 | Normal, n=1, (n=1, normal to present), (4 dropouts, out of 6) | |||
| Grade 3, n=2 | Grade 3, n=0 (2 dropouts, out of 2) | |||||||
Figure 1.
Trial profile.
A record was kept of participant medication intake. Participants took NSAID (non-steroidal anti-inflammatory drugs) or analgesics when they felt the need. This was recorded.
Assessments
Assessments such as (i) self-rated pain, (ii) state anxiety, (iii) spinal flexibility, and (iv) MRI of the lumbosacral spine were done before and after the intervention program for all participants.
The primary outcome measure was pain. Secondary outcome measures were: (i) state anxiety, (ii) spinal flexibility, and (iii) MRI scans. MRI scans were taken on 1 day and the other 3 assessments were performed on the subsequent day in the following order: pain, state anxiety, and spinal flexibility.
Self rated pain
A 10-cm linear visual analogue scale was used to assess each participant’s rating of their level of pain [19]. The visual analogue scale is a double-anchored horizontal line where each end represents opposite ends of a continuum that extends from “not at all” (score=0) at the left end of the scale to “the worst possible” (score=10) at the right end of the line. Participants were instructed to indicate their level of pain with a mark made on the linear scale.
State-anxiety
State anxiety was measured using a sub-scale of the State-Trait Anxiety Inventory, which has 20 items to assess state anxiety or anxiety at the moment of testing [20]. Participants selected the number that best described the intensity of their feelings at the moment of testing, where “1” was “not at all”, “2” was “somewhat”, “3” was “moderately”, and “4” was “very much so”.
Spinal flexibility test
Spinal flexibility was measured using the Sit and Reach flexibility tester, (Model 01285A, Lafayette Instrument, U.S.A.). This test involved sitting on the floor with legs stretched out straight ahead. Participants’ bare feet were placed with the soles flat against the box, shoulder-width apart. Both knees were held flat against the floor by the experimenter. With hands on top of each other and palms facing down, the participant reached forward, flexing the spine, to reach a point along the measuring line as far as possible. Participants of both groups performed this test 3 times and the maximum performance, noted as the distance in cm, was recorded and used in the analysis.
MRI scanning
MRI scans were performed with a 1.5 Tesla superconducting scanner (Achieva Philips Medical Systems, Best, The Netherlands) using a spinal surface coil. Pulse sequences were as follows:
Sagittal T2-weighted turbo spin echo [4700 ms (TR=repetition time)/120 ms (TE=echo time), 15 (echo train length), 4 mm (the thickness of a section), 280×280 mm (FOV=field of view), 240×256 (matrix size), and acquisition of 1 signal].
Sagittal T1-weighted spin echo [600 ms (TR=repetition time)/14 ms (TE=echo time), 15 (echo train length), 4 mm (the thickness of a section), 280×280 mm (FOV=field of view), 240×256 (matrix size), and acquisition of 1 signal].
Axial T2-weighted turbo spin echo over levels of intervertebral discs of the lumbar spine [4500 ms (TR=repetition time)/120 ms (TE=echo time), 15 (echo train length), 4 mm (the thickness of a section), 200×200 mm (FOV=field of view), 240×256 (matrix size), and acquisition of 1 signal].
Intervention
Yoga group
The yoga group was taught the following techniques: (i) light exercises and specific physical postures (asanas), (ii) breathing techniques (pranayamas) [21], and (iii) chanting and yoga relaxation techniques, in the morning (08: 00 AM to 09: 00 AM) for 3 months. These components were modified by an orthopedic surgeon [22], particularly for patients with back pain. The yoga program is detailed in Table 3. The yoga group first attended a course consisting of 3 group classes per week for 2 weeks in order to develop a home practice, which they were asked to continue daily for the rest of the trial. Weekly yoga classes were available throughout the trial.
Table 3.
One hour yoga therapy.
| Sl. no. | Practice | Duration |
|---|---|---|
| 1 | Meditation on the Sanskrit syllable, OM | 5 minutes |
|
| ||
| 2 | Relaxation (in Shavasana) | 5 minutes |
|
| ||
| 3 | Light exercises and asanas | 25 minutes |
|
| ||
| • Hold and rotate knees in circles (both directions) | ||
| • Roll onto one side | ||
| • Raise one leg at a time | ||
| • Lift the head and shoulders | ||
| • Pelvic tilting | ||
| • Touch the face to flexed knees (with one leg) | ||
| • Supine twist (Supta Matsyendrasana) | ||
| • Cobra pose (Bhujangasana) | ||
| • Locust pose (Shalabhasana) | ||
| • Child pose (Balasana) | ||
|
| ||
| 4 | Relaxing postures | 10 minutes |
| • Shavasana/yoganidra | ||
|
| ||
| 5 | Pranayama | |
| • Slow breathing | 7 minutes | |
| • Kapalabhati (1 stroke per second, not forcefully) | 3 minutes | |
|
| ||
| 6 | Meditation and ending prayer | 5 minutes |
|
| ||
| Total duration | 60 minutes | |
Yoga was taught by trained instructors who had a 2-year post-graduate degree in yoga (their training included both theory and practice). Class attendance was monitored by another person. Yoga instructors were asked to specifically monitor any adverse event during yoga practice, but no such event was reported.
Waitlist control group
In the beginning, health education advice was offered to the waitlist control group but after 2 weeks the attendance was less than 30% so the classes were discontinued. No intervention was given to the control group except that they were asked to carry on with the routine medical care suggested by their physician, consisting of (i) analgesics and/or (ii) non-steroidal anti-inflammatory medication, which they took when they were in pain.
Data extraction
A person blinded to which group the participants belonged to performed the scoring of all the assessments.
The primary outcome measure
Self-reported pain
The level of pain of each participant was obtained using the pain analogue scale. The calculation was made from the left of the line (considered as zero) to the mark made by the participants; this distance was measured in cm. Measurements were precise up to 0.1 mm.
Accurately recorded data were available for 20 individuals each in the yoga group and the control group.
The secondary outcome measures
State-anxiety inventory
Each STAI-S item is given a weighted score of 1 to 4. A standard method was used to score the data [20]. Higher scores are positively correlated with a higher anxiety level.
Spinal flexibility test
The values in cm were directly used for analysis.
MRI (Magnetic Resonance Imaging)
The MRI with all necessary details to grade it was obtained from a trained radiologist. An established system for grading [16] was used to assess the discs from D12 to S1, as well as changes in the vertebrae: (i) nerve compression, (ii) endplate changes, and (iii) changes in facet joints. The 5 grades for structural disc changes as they appeared in the scan are: Grade I (homogeneous, bright white), Grade II (inhomogeneous with or without horizontal bands), Grade III (inhomogeneous, gray), Grade IV (inhomogeneous, gray to black), and Grade V (inhomogeneous, black).
Apart from grading the intervertebral discs, changes in the vertebrae, especially (i) nerve compression, (ii) end-plate changes, and (iii) facet-joints changes, were noted as present or not. If present, they were scored as 1 (one) and absent as 0 (zero).
The grading was scored independently by 2 researchers based on the radiology reports; they were blind to the participant’s group. Details about disc degeneration (grade), nerve compression, endplate changes, and facet joint changes for the yoga group and the waitlist control group are given in Table 2.
Statistical analysis
In both the yoga and waitlist control groups there were dropouts between baseline and post-assessments at three months. Hence an intention-to-treat analysis was performed calculating the missing values using PASW Version 18.0. A repeated measures analysis of variance (ANOVA) with Bonferroni correction for post-hoc analyses was used. The Bonferroni value was adjusted to 0.025. The ANOVA compared data of the 2 groups as a between-subjects factor and data recorded at baseline with that recorded at 3 months as a within-subjects factor. Statistical significance (α) was set at 0.05.
Results
For each assessment, group mean values ±S.D. are shown in Table 4.
Table 4.
Self rated pain, state anxiety and spinal flexibility of the two groups. Values are group mean (S.D.).
| Variables | Yoga group (n=20) | Control group (n=20) | ||||
|---|---|---|---|---|---|---|
| Baseline | 12 weeks | Cohen’s d | Baseline | 12 weeks | Cohen’s d | |
| PAS (cm) | 6.36 (2.29) | 4.68 (2.30)* | 0.734 | 6.13 (2.83) | 6.10 (2.19) | 0.012 |
| STAI-S scores | 48.40 (12.63) | 37.15 (8.68)** | 1.056 | 48.80 (11.60) | 43.80 (10.88) | 0.445 |
| Spinal flexibility (cm) | 17.06 (10.11) | 16.67 (9.44) | 0.040 | 17.50 (9.04) | 13.78 (8.03) | 0.436 |
PAS – pain analogue scale; STAI-S – state anxiety;
p<.05, post-hoc analysis with Bonferroni adjustment (Missing Value analysis);
p<.01, post-hoc analysis with Bonferroni adjustment compared with pre (Missing Value analysis).
The effect size and power were calculated based on published data of changes in the visual analog scales for pain in patients of low back pain after 4 weeks [14]. These data were used to derive the ideal sample as well as the power of the statistics used in this study. These analyses showed the present study has a small sample size and hence the power of statistical tests is medium (Table 5). This is a limitation of the present study which is mentioned in the Discussion.
Table 5.
Statistical calculations based on VAS of pain as a criterion.
| Variables | From the literature (Nambi et al., 2014) | From the present study |
|---|---|---|
| Sample size (Group 1) | 29 | 18 |
| Sample size (Group 2) | 29 | 18 |
| Total sample size | 58 | 36 |
| Power | 0.669 | 0.49 |
| Effect size | 0.63 (large) | 0.30 (medium) |
| Cohen’s d | 1.64 | 0.632 |
| Level of significance | 0.05 | 0.05 |
Pain, state anxiety, and spinal flexibility
(i) Repeated Measures Analysis of Variance (ANOVA)
Values for the factors such as Within-Subjects (States), Between-Subjects (Groups), and interaction between the 2 for the (i) pain analogue scale, (ii) STAI-S, and (iii) spinal flexibility are given in Table 6. The significant Groups X States interaction indicated interdependence.
Table 6.
ANOVA for different variables (self rated pain, state anxiety and spinal flexibility); Missing Value analysis.
| Sl. no. | Factors | Variables | F | df | Huynh-Feldt ɛ | p |
|---|---|---|---|---|---|---|
| 1 | Within subjects (States) | PAS | 2.322 | 1, 38 | 1 | 0.136 |
| STAI-S | 13.035 | 1, 38 | 1 | 0.001 | ||
| Spinal flexibility | 1.697 | 1, 38 | 1 | 0.201 | ||
| 2 | Between subjects (Groups) | PAS | 1.338 | 1, 38 | – | 0.255 |
| STAI-S | 1.743 | 1, 38 | – | 0.195 | ||
| Spinal flexibility | 0.251 | 1, 38 | – | 0.619 | ||
| 3 | States X Groups | PAS | 2.136 | 1, 38 (States) X 38 (Groups) | – | 0.152 |
| STAI-S | 1.928 | 1, 38 (States) X 38 (Groups) | – | 0.173 | ||
| Spinal flexibility | 1.113 | 1, 38 (States) X 38((Groups) | – | 0.298 |
PAS – pain analogue scale; STAI-S – state anxiety.
(ii) Post-hoc analyses
Comparisons were made with respective ‘pre’ States within a group and between groups. Significant changes occurred only in before/after comparisons.
MRI data
The MRI data were not statistically analyzed because it was evident that there was no significant change in group between values at baseline and at 3 months. The data of individual patients are reported.
Disc changes based on MRI scans
According to the grades given to disc changes, the number(s) of patients who showed signs of improvement after 3 months was 1 in the yoga group and 2 in the control group according to the intervertebral disc grades shown in Table 2. The number of patients who worsened after 3 months based on disc grades was 3 in the yoga group and 2 in the control group.
Vertebral changes (nerve compression, endplate changes, and facet joint changes)
Nerve compression
This remained the same in both groups at the post-intervention assessment.
Endplate changes
In 1 patient, endplate changes returned to normal in the yoga group at post-intervention assessment and in the control group 1 patient developed endplate changes at the post-intervention assessment.
Facet joint changes
There were no facet joint changes in either group at baseline or post-intervention assessment.
Discussion
Patients with chronic LBP who practiced yoga for 12 weeks showed a significant reduction in self-reported pain and state anxiety in a before/after comparison. Conventional care had no significant benefits.
There have been speculations about the mechanisms by which yoga practice might relieve back pain. Yoga practice places as much emphasis on mental focus as on physical movement [23]. During the practice of yoga, the breath is regulated and mental focus is directed to it, resulting in physical and psychological benefits [24]. From a physical point of view, it is considered that yoga increases flexibility and strength, tones the muscles, and reduces muscular tension [25–27]. Yoga practice also increases proprioceptive ability and hence may help in adopting the correct posture to relax muscular tension and to relieve mental stress [28]. It is possible that the perceived decrease in pain may have been due to reduced tension in para-vertebral muscles.
The absence of a change in flexibility in the present study compared to other studies [11] could be due to differences in the yoga regimen. The present yoga protocol was developed by an orthopedic surgeon and has been shown to reduce back-related dysfunction using the Roland Morris Disability Questionnaire; the yoga group score was 3.29 points lower than in the control group (0.98, 5.61; p=0.006) [29]. The yoga protocol used in the cited study [29] and the present study are the same. This protocol does not include certain lumbar stretches are considered useful to increase flexibility. These include bridge pose lumbar stretch (Sethubandhasana breathing), folded leg lumbar stretch (Supta Udarakarshanasana), and crossed leg lumbar stretch (Shavaudrakarshanasana) [30]. These particular practices were included in the studies [11,12] that reported an increase in flexibility. The protocol used in the present study was developed by an orthopedic surgeon and was more conservative.
There was a 26.4% reduction in pain after 12 weeks of yoga in the present study. In earlier studies the reduction was greater − 49.0% in the yoga group after a 7-day residential yoga program [12] and 72.8% in the yoga group at 6-month follow-up after Iyengar yoga [14]. Differences in the yoga program could explain why the reduction was less in this study. Yoga programs mentioned in earlier studies [12,14] were more intensive in terms of: (i) time (8 hours per day [12] versus 1 hour per day in the present trial) or (ii) number of yoga postures (29 postures [14] versus 10 postures in the present trial).
The MRI scans were examined for changes in: (i) the intervertebral disc, (ii) nerve compression, (iii) end-plate changes, and (iv) facet joints changes. There were some changes in the intervertebral disc grades, nerve compression, and end-plate changes in both groups at post-intervention assessment. However, the numbers were too small to indicate trends of improvement or worsening.
The changes in pain and state anxiety could not be related to differences in the severity of structural damage or nerve compression at baseline. The absence of change in the intervertebral discs, the vertebrae, and nerve compression could possibly be related to the relatively short duration (12 weeks) of the yoga intervention. However, there is no basis to suggest that a structurally altered vertebra and intervertebral disc would change with yoga. In specific cases pain is associated with changes in the skeletal muscle [31], but that was not the case here. The only study which documented MRI changes in the spine was a matched controlled study carried out on asymptomatic normal individuals who did not have LBP. Hence, after 12 weeks of yoga practice no changes were demonstrable in the spine, although patients with LBP experienced less pain and lower state anxiety.
The findings of the present study are limited by the following factors. (i) The number of patients was small and (ii) the duration of follow-up was short. Every attempt was made to contact participants of both groups at 6 months but the number of participants in both groups available for follow up assessment was less than 5%. (iii) The high dropout rate (15–50% for different assessments) compared to other studies (none [12] and 10% [14]). It is difficult to understand why the dropout rate was so high. A possible reason is that during the period of the study (July to September, 2011), heavy monsoon rains make commuting or traveling to the place of assessment and to the yoga class difficult.
Conclusions
Despite its limitations, the present study has shown that within 12 weeks, yoga practice reduces pain and state anxiety but does not alter MRI-proven changes in the intervertebral discs and vertebrae.
Acknowledgements
The authors gratefully acknowledge the help of Dr. (Col.) Harish Bhatia (Senior MRI Consultant, Doon MRI Centre, Dehradoon, India), Ankur Kumar (Yoga teacher), and all the members of Patanjali Research Foundation, Haridwar, India for their assistance in data collection.
Footnotes
Conflict of interest
None declared.
Source of support: The project was funded by Patanjali Yogpeeth, Haridwar, India
References
- 1.Freynhagen RBR, Gockel U, Tölle TR. Pain DETECT: A new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22:1911–20. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- 2.Sardar K, Das G, Mahta P, et al. Medical ozone in herniated disc: A classical review. J Pain Relief. 2014;3(3):1000148. [Google Scholar]
- 3.Kaki AM, El-Yaski AZ, Youseif E. Identifying neuropathic pain among patients with chronic low-back pain: Use of the leeds assessment of neuropathic symptoms and signs pain scale. Reg Anesth Pain Med. 2005;30:422–28. doi: 10.1016/j.rapm.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SP, Williams S, Kurihara C, et al. Nucleoplasty with or without intradiscalelectrothermal therapy (IDET) as a treatment for lumbar herniated disc. J Spinal Disord Tech. 2005;18:S119–24. doi: 10.1097/01.bsd.0000127823.54485.3f. [DOI] [PubMed] [Google Scholar]
- 5.Jain N. Slip disc with sciatica – newer non-surgical treatment. Journal of International Medical Sciences Academy. 2013;26(4):249–51. [Google Scholar]
- 6.Kanodia AK, Legedza AT, Davis RB, et al. Perceived benefit of Complementary and Alternative Medicine (CAM) for back pain: A national survey. J Am Board Fam Med. 2010;23(3):354–62. doi: 10.3122/jabfm.2010.03.080252. [DOI] [PubMed] [Google Scholar]
- 7.Wolsko PM, Eisenberg DM, Davis RB, et al. Patterns and perceptions of care for treatment of back and neck pain: results of a national survey. Spine. 2003;28(3):292–97. doi: 10.1097/01.BRS.0000042225.88095.7C. [DOI] [PubMed] [Google Scholar]
- 8.Saper RB, Eisenberg DM, Davis RB, et al. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Altern Ther Health Med. 2004;10(2):44–49. [PubMed] [Google Scholar]
- 9.Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain: A randomized trial. Ann Intern Med. 2011;155(9):569–78. doi: 10.7326/0003-4819-155-9-201111010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Sherman KJ, Cherkin DC, Erro J, et al. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143(12):849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 11.Haldavnekar RV, Tekur P, Nagarathna R, Nagendra HR. Effect of yogic colon cleansing (LaghuSankhaprakshalanaKriya) on pain, spinal flexibility, disability and state anxiety in chronic low back pain. Int J Yoga. 2014;7(2):111–19. doi: 10.4103/0973-6131.133884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tekur P, Nagarathna R, Chametcha S, et al. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: An RCT. Complement Ther Med. 2012;20(3):107–18. doi: 10.1016/j.ctim.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Saper RB, Sherman KJ, Cullum-Dugan D, et al. Yoga for chronic low back pain in a predominantly minority population: a pilot randomized controlled trial. Altern Ther Health Med. 2009;15(6):18–27. [PMC free article] [PubMed] [Google Scholar]
- 14.Nambi GS, Inbasekaran D, Khuman R, et al. Changes in pain intensity and health related quality of life with Iyengar yoga in nonspecific chronic low back pain: A randomized controlled study. Int J Yoga. 2014;7(1):48–53. doi: 10.4103/0973-6131.123481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeng CM, Cheng TC, Kung CH, Hsu HC. Yoga and disc degenerative disease in cervical and lumbar spine: an MR imaging-based case control study. Eur Spine J. 2011;20(3):408–13. doi: 10.1007/s00586-010-1547-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26(17):1873–78. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behav Res Methods Instrum Comput. 1996;28:1–11. [Google Scholar]
- 18.Random Number Generator. http://www.random.org/sequences.
- 19.Cacioppo JT, Tassinary LG. Principles of psychophysiology: Physical, social, and inferential elements. New York: Cambridge University Press; 1990. [Google Scholar]
- 20.Gaudry E, Spielberger CD. Anxiety and intelligence in paired-associate learning. J Educ Psychol. 1970;61:386–91. doi: 10.1037/h0029796. [DOI] [PubMed] [Google Scholar]
- 21.Telles S, Singh N, Balkrishna A. Metabolic and ventilatory changes during and after high-frequency yoga breathing. Med Sci Monit Basic Res. 2015;21:161–71. doi: 10.12659/MSMBR.894945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dongaonkar D. Yoga application for low back pain. New Delhi, London, Philadelphia, Panama: Jaypee Brothers Medical Publishers (P); 2013. [Google Scholar]
- 23.Yoga. The ultimate mind-body workout. Harv Health Lett. 1998;24:4–5. [PubMed] [Google Scholar]
- 24.Sovik R. The science of breathing – the yogic view. Prog Brain Res. 2000;122:491–505. doi: 10.1016/s0079-6123(08)62159-7. [DOI] [PubMed] [Google Scholar]
- 25.Discovering yoga. Nursing. 2001;31:20. doi: 10.1097/00152193-200131020-00007. [DOI] [PubMed] [Google Scholar]
- 26.Spilner M. Flex away back pain. Prevention. 1999:53. [Google Scholar]
- 27.Globus S. What yoga can do for you. Current Health. 2000:30. [Google Scholar]
- 28.Krishnamurthy M, Telles S. Effect of yoga and an ayurveda preparation on gait, and mobility in older persons. Med Sci Monit. 2007;13(12):LE19–20. [PubMed] [Google Scholar]
- 29.Monro R, Bhardwaj AK, Gupta RK, et al. Disc extrusions and bulges in nonspecific low back pain and sciatica: Exploratory randomized controlled trial comparing yoga therapy and normal medical treatment. J Back Musculoskelet Rehabil. 2015;28(2):383–92. doi: 10.3233/BMR-140531. [DOI] [PubMed] [Google Scholar]
- 30.Nagarathna R, Nagendra HR. Yoga for back pain. Bengaluru: Swami Vivekananda Yoga Prakashana; 2011. [Google Scholar]
- 31.Abdallah A, Gokcedag A, Ofluoglu AE, Emel E. Non-traumatic myositis ossificans in the lumbar spine. Am J Case Rep. 2014;15:421–25. doi: 10.12659/AJCR.891151. [DOI] [PMC free article] [PubMed] [Google Scholar]