Abstract
Background
Errors directly causing serious harm are rare during pediatric trauma resuscitation, limiting the use of adverse outcome analysis for performance improvement in this setting. Errors not causing harm due to mitigation or chance may have similar causation and are more frequent than those causing adverse outcomes. Analyzing these error types is an alternative to adverse outcome analysis. The purpose of this study was to identify errors of any type during pediatric trauma resuscitation and evaluate team responses to their occurrence.
Methods
Errors identified using video analysis were classified as errors of omission or commission, and selection errors using input from trauma experts. The responses to error types and error frequency based on patient and event features were compared.
Results
Thirty-nine resuscitations were reviewed, identifying 337 errors (range 2–26 per resuscitation). The most common errors were related to cervical spine stabilization (n=93, 27.6%). Errors of omission (n=135) and commission (n=106) were more common than errors of selection (n=96). Although 35.9% of all errors were acknowledged and compensation occurred after 43.6%, no response (acknowledgement or compensation) was observed after 51.3% of errors. Errors of omission and commission were more often acknowledged (40.7% and 39.6% vs. 25.0%, p=0.03 and p=0.04, respectively) and compensated for (50.4% and 47.2% vs. 29.2%, p=0.004 and p=0.01, respectively) than selection errors. Response differences between errors of omission and commission were not observed. The number of errors and the number of high-risk errors that occurred did not differ based on patient or event features.
Conclusions
Errors are common during pediatric trauma resuscitation. Teams did not respond to most errors, although differences in team response were observed between error types. Determining causation of errors may be an approach for identifying latent safety threats contributing to adverse outcomes during pediatric trauma resuscitation.
LEVEL OF EVIDENCE
VI
STUDY TYPE
prognostic
Keywords: errors, medical, team performance, trauma, healthcare quality assessment, clinical practice patterns
BACKGROUND
Despite significant efforts to improve patient safety over the past two decades, medical errors remain an important cause of morbidity and mortality among patients treated in acute care settings.(1, 2) Identifying risk conditions for errors and understanding steps taken to mitigate the effect of errors are essential components of any performance improvement process. Traditional error analysis relies on root cause analysis or its variations, in which errors leading to an adverse event are determined and processes or structural changes needed to prevent future errors are identified.(3) Although root cause analysis has a key role in performance improvement, it is limited by its reliance on retrospective analysis of the small subset of errors that lead to patient harm and by its vulnerability to hindsight bias.(1, 4) Near misses, or errors not causing patient harm due to mitigation or chance, are more frequent than errors leading to adverse outcomes.(5) Because near misses may have similar causation as errors leading to adverse outcomes, analyzing near misses has been proposed as a more effective and feasible approach for performance improvement than traditional root cause analysis.(6)
Critically injured patients have up to a four-fold higher risk of death from errors than general hospital patients(7), with nearly half of these preventable deaths related to errors that occur during the initial resuscitation phase of treatment.(8, 9) Although errors in the initial evaluation and treatment of injured patients are frequent, previous studies have shown that most of these errors do not lead to adverse outcomes in the trauma setting.(3, 10) Because the acuity of injured children is often lower than that of adults treated in most trauma centers, relying on adverse event analysis to improve the process of care for injured children is even more challenging. Analyzing the events that lead to and surround near misses, as well as compensation for near misses, may guide the prevention or mitigation of future errors and corresponding adverse events among injured children.
The purpose of this study was to: 1. identify and classify errors occurring during pediatric trauma resuscitation, 2. determine the trauma team’s response to these errors and 3. assess patient and trauma resuscitation features associated with the occurrence or errors. Our focus was on detecting all types of errors not just errors directly leading to harm.
METHODS
Study Setting
Children’s National Medical Center (CNMC) is a level 1 pediatric trauma center verified by the American College of Surgeons, State of Maryland and the District of Columbia serving the greater Washington, DC region. About 600 injured children each year are evaluated in the emergency department by the trauma team based on pre-hospital triage criteria. The trauma bays are equipped with a video recording system that records each evaluation. Patients are triaged to one of three activation levels based on pre-hospital reports of mechanism of injury and physiological status. Lower acuity patients coming from the scene of injury are triaged as “stat” trauma activations. Stable patients initially treated at an outside hospital are triaged as “transfer” activations. Patients high-acuity injuries are triaged as “stat attending” activations. The use of video recordings has been approved for use for research purposes by the Institutional Review Board at Children’s National Medical Center.
Data Source
To capture all potential errors, we evaluated video recordings of resuscitations for the occurrence of non-routine events (NREs), a broad class of events defined as any event that is unusual or atypical in the resuscitation process.(11) Videos were reviewed jointly by a surgeon with Advanced Trauma Life Support (ATLS) certification and a trauma clinical nurse specialist to identify NREs. NREs within the control of the team and with any potential for patient harm were coded as errors, while NREs that did not have a potential for harm or that were caused by circumstances beyond the control of the team were coded as non-errors or “non-process deviations.” We further classified errors as low- or high-risk based on the level of potential harm to the patient if unnoticed or unaddressed. Error risk was determined based on the type of error as well as patient and situation features. For example, listening to breath sounds over clothing as part of routine analysis of a stable child was categorized as a low risk error, while tachycardia that was not acknowledged or acted on for 30 seconds or more was categorized as a high-risk error. The team’s response to each NRE was also determined by video review and was defined as either verbal acknowledgement by any team member that the error occurred or a team member taking action to compensate for the error. Team responses to errors included acknowledgement, compensation or both. In a separate phase of analysis, two trauma surgeons and one pediatric emergency medicine physician independently classified the identified errors as errors of omission, commission, or selection and further classified the errors into subtypes using a previously described classification scheme (Appendix).(10) Non-process deviations were classified using a modification of a previously used approach (Appendix).(12) The three physicians resolved differences in classification by group consensus.
An increased number of significant physiologic disturbances has previously been reported to be associated with more frequent NREs during anesthesia induction in the operating room.(13) We defined significant physiologic disturbances as vital sign values greater than two standard deviations from the mean for age based on published standards and desaturation defined as oxygen saturation <90%.(14–16) We identified significant physiologic disturbances by reviewing recordings of the patient monitor and team responses to significant physiologic disturbances by video review.
We obtained additional data from our trauma database or from medical chart review, including patient age, gender, triage level, mechanism of injury, date and time of patient arrival, Injury Severity Score (ISS), and training background of team leaders. The number of NREs per resuscitation was compared between different patient and event features. Comparison groups included gender, triage level, team pre-notification, mechanism of injury (blunt versus penetrating), daytime versus nighttime events, weekend versus weekday events, ISS level (≤10 versus >10), surgical coordinator’s training level (senior resident versus surgical fellow), and examining provider’s background (junior resident versus other role as examiner [trauma nurse practitioner, emergency medicine fellow or surgical fellow]). A chart review of each patient’s hospitalization was performed to identify any adverse outcomes related to treatment during the initial trauma resuscitation.
During a five-month period (August –December 2014), 205 children presented as trauma activations. Video from 99 resuscitations were available for analysis after excluding 67 events because of poor video quality or unintended erasure and 35 events because of inability to obtain consent. In a similar analysis of trauma resuscitation, a 25% difference in the proportion of errors of omission and other major error types (errors of commission and selection errors) was observed.(10) Power analysis showed that 38 resuscitations was sufficient to show a similar effect size with a power of 0.80 and an alpha of 0.025. A convenient sample of 39 events from the study period was selected to coincide with a separate and on-going analysis of trauma resuscitation workflow. Patient and resuscitation features and any known errors or adverse events were not known or used in selecting events for analysis. Patient and resuscitation features were compared between sampled and non-sampled events to assess whether this sampling process may have lead to a biased sample.
Data Analysis
Differences between the coded and non-coded resuscitations were assessed using Pearson’s χ2 test, Wilcoxon rank sum test, or Fisher’s exact text where appropriate. Differences in number of errors between patient and event feature cohorts were compared using the Wilcoxon rank sum test. Differences in response to error and significant physiologic disturbances between classification and risk groups were calculated using Pearson’s χ2 test and multivariate logistic regression using random effects modeling that considered clustering of errors within patients. We assessed the correlation between the number of errors and number of non-error NREs per resuscitation and between the number of errors and the duration and number of significant physiologic disturbances using Spearman’s correlation coefficient. We defined statistical significance at p<0.05 for all tests.
RESULTS
Overview of Patient and Resuscitation Features
Patients were mostly male (82.1%), and varied in age from 2 weeks old to 16 years old (mean 8.2 ± 5.2 years, Table 1). Most were triaged as a “stat” activation (56.4%) and arrived after notification of the trauma team (87.2%). Most resuscitations occurred on weekdays and in the evening. Most patients were injured by a blunt injury mechanism (92.3%). The median ISS was 4, with 12.8% of patients having an ISS greater than 10 (Table 1). A review of performance improvement data showed that no identified resuscitation error led directly to an adverse patient outcome. We observed no significant differences in patient or events features between coded and non-coded resuscitations (Table 1).
Table 1.
Summary Statistics
| Resuscitation Features | Coded Resuscitations (n=39) | Other Resuscitations (n=64) | p-value |
|---|---|---|---|
| Male (%) | 82.1% | 93.8% | 0.06 |
| Age, years (mean±SD) | 8.2 ± 5.2 | 7.3± 5.1 | 0.49 |
| Penetrating mechanism (%)* | 5.1% | 9.4% | 0.71 |
| ISS | |||
| ISS > 10 | 12.8% | 25.0% | 0.14 |
| Median ISS (interquartile range) | 4 (1–9) | 4 (1–17) | 0.90 |
| Activation level | |||
| Stat | 56.4% | 67.2% | |
| Transfer | 43.6% | 26.6% | 0.09 |
| Attending Stat | 0.0% | 6.3% | |
| Surgical fellow present | 41.0% | 40.6% | 0.97 |
| Junior resident as examiner* | 89.7% | 81.3% | 0.28 |
| No pre-notification | 12.8% | 21.9% | 0.25 |
| Weekend event | 46.2% | 32.8% | 0.18 |
| Daytime event (7 AM–7 PM) | 43.6% | 59.4% | 0.12 |
SD, standard deviation; ISS, injury severity score;
Fisher’s exact test used because of the small number of penetrating injuries and other types of examiners
Analysis of Errors, Non-error Process Deviations and Significant Physiological Disturbances
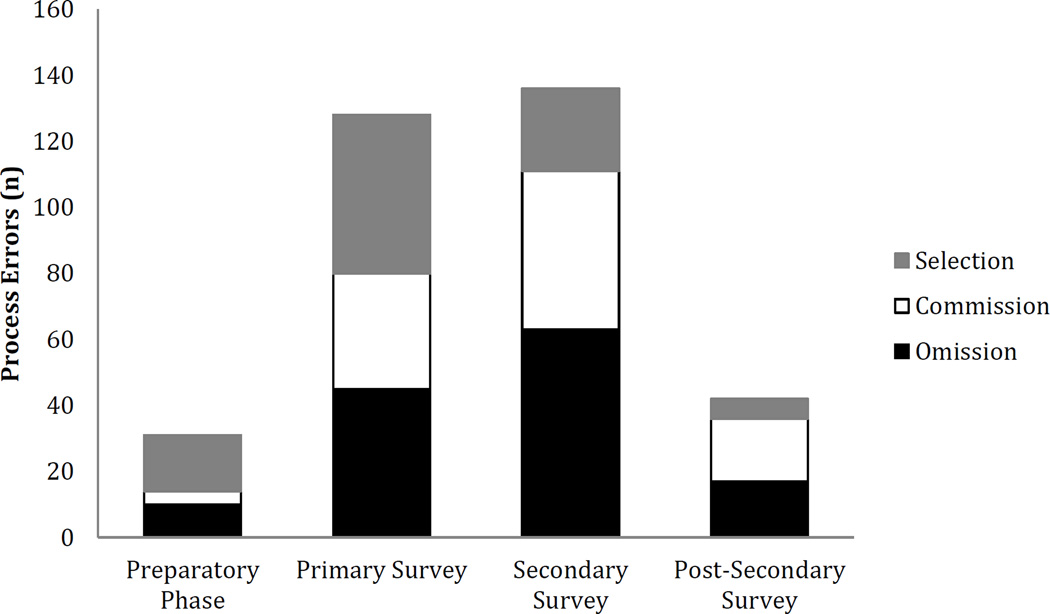
Among the 39 resuscitations, 337 errors were identified, with a median of eight errors per resuscitation (range 2 to 26 per resuscitation, Table 2). The most common errors were related to cervical spine stabilization (n=93, 27.6%), including lapses in in-line stabilization (n=55, 16.3%) and incorrect placement of a cervical collar (n=14, 4.1%). Errors of omission (n=135, 40.1%) and commission (n=106, 31.5%) were more frequent than errors of selection (n=96, 28.5%). Errors of omission classified as “partial” (n=75, 22.3%) were the most frequent errors in this category. Errors of commission classified as “prohibited” (n=78, 23.2%) and errors of selection classified as “precondition” (n=41, 12.2%) were the most common subclasses within their respective categories (Table 2). The mean time from patient arrival to occurrence of the first error was 5 min 36 sec (range 9 min 43 sec before patient arrival to 34 min 7 sec after patient arrival). Errors of all classes occurred more frequently during the primary and secondary survey than during preparatory and post-resuscitative phases (Figure 1).
Table 2.
Classification of and Team Recovery from Errors
| Error type | No. of Events (% of total) |
Median per resuscitation (IQR) |
Error acknowledged (% of class) |
Compensation (% of class) |
Any Response (% of class) |
|---|---|---|---|---|---|
| Overall | 337 | 8 (6–11) | 121 (35.9) | 146 (43.3) | 164 (48.7) |
| Omission | 135 (40.1) | 3 (1–5) | 55 (40.7) | 68 (50.4) | 75 (55.6) |
| Partial | 75 (22.3) | 2 (1–3) | 33 (44.0) | 45 (60.0) | 47 (62.7) |
| Total | 60 (17.8) | 1 (0–2) | 22 (36.7) | 23 (38.3) | 28 (46.7) |
| Commission | 106 (31.5) | 2 (0–5) | 42 (39.6) | 50 (47.2) | 54 (50.9) |
| Irrelevant | 5 (1.5) | 0 (0–0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Prohibited | 78 (23.2) | 2 (0–3) | 29 (37.2) | 37 (47.4) | 40 (51.3) |
| Redundant | 21 (6.2) | 0 (0–1) | 13 (61.9) | 12 (57.1) | 13 (61.9) |
| Unmotivated | 2 (0.6) | 0 (0–0) | 0 (0.0) | 1 (50.0) | 1 (50.0) |
| Selection | 96 (28.3) | 2 (1–4) | 24 (25.0) | 28 (29.2) | 35 (36.5) |
| Contraindicated | 2 (0.6) | 0 (0–0) | 1 (50.0) | 0 (0.0) | 1 (50.0) |
| Dependency | 1 (0.3) | 0 (0–0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Precedence | 11 (3.3) | 0 (0–0) | 8 (72.7) | 9 (81.8) | 9 (81.8) |
| Preconditions | 41 (12.2) | 1 (0–2) | 7 (17.1) | 12 (31.7) | 15 (36.6) |
| Preference | 15 (4.5) | 0 (0–1) | 1 (6.7) | 1 (6.7) | 1 (6.7) |
| Priority | 23 (6.8) | 0 (0–1) | 5 (21.7) | 5 (21.7) | 7 (30.4) |
| Urgency | 3 (0.9) | 0 (0–0) | 2 (66.7) | 1 (33.3) | 2 (66.7) |
| High-risk | 166 (49.3) | 3 (2–5) | 60 (36.1) | 82 (49.4) | 91 (54.8) |
| Low-risk | 171 (50.7) | 4 (2–6) | 61 (35.7) | 64 (37.4) | 73 (42.7) |
IQR= interquartile range
Figure 1.
Number of errors by resuscitation phase and error class
Teams responded to 48.7% of errors, 35.9% by acknowledgement and 43.3% by compensation (Table 2). Errors of omission had the greatest frequency of acknowledgment and compensation (40.7% and 50.4%, respectively, Table 2) and were more likely to be acknowledged and compensated for than errors of selection (p=0.01, and p=0.002, respectively). Errors of commission were also more likely to be acknowledged and compensated for than errors of selection (p=0.03 and p=0.01, respectively). We observed no difference, however, in acknowledgement or compensation between errors of omission and commission (p=0.86 and p=0.62, respectively). Teams responded to errors of commission and omission more often than to errors of selection (p=0.04 and p=0.004, respectively). We observed no difference in response between errors of commission and omission (p=0.48).
Errors rated as low-risk occurred at a similar percentage as those classified as high-risk. Errors of selection were less frequently classified as high-risk (34.4%) than were errors of commission and omission (62.3% p<0.001 and 49.6% p=0.02). No significant difference in the level of risk between errors of commission and omission was observed. Although no significant difference was observed between team acknowledgement of high and low-risk errors, teams compensated for and responded to high-risk errors more frequently than low-risk errors (p=0.04 and p=0.03).
One hundred seventy-eight non-error process deviations were observed, with a median of three events per resuscitation (range 0 to16 per resuscitation). Equipment malfunction was the most common among this class of deviations (n=33, 18.5%), followed by aberrant personnel (n=32, 18.0%) and patient factors (n=30, 16.9%, Table 3). The average time to non-error process deviations was 4 min 59 sec after patient arrival (range 9 min 57 sec before patient arrival to 29 min 52 sec after patient arrival). Non-error process deviations occurred mostly during the primary (33.2%) and secondary survey (31.5%). Teams responded to most non-error process deviations (78.1%, Table 3). Among non-error process deviations, teams responded to external events least frequently (58.6%, Table 3).
Table 3.
Classification of and Team Recovery from Non-Error Events
| Non-error Event type | No. of Events (% of total) |
Median per resuscitation (IQR) |
Acknowledged (% of Class) |
Compensation (% of class) |
Any Response (% of class) |
|---|---|---|---|---|---|
| Non-error Process Deviations | 178 | 3 (1–7) | 128 (71.9) | 123 (69.1) | 139 (78.1) |
| Equipment Malfunction | 33 (18.5) | 0 (0–1) | 27 (81.8) | 24 (72.7) | 27 (81.8) |
| Aberrant Personnel | 32 (18.0) | 0 (0–1) | 23 (71.9) | 28 (87.5) | 30 (93.8) |
| Patient Factors | 30 (16.9) | 0 (0–1) | 26 (86.7) | 23 (76.7) | 26 (86.7) |
| Interruption | 26 (14.6) | 0 (0–1) | 18 (69.2) | 12 (46.2) | 18 (69.2) |
| Patient Action | 23 (12.9) | 0 (0–0) | 17 (73.9) | 18 (78.3) | 18 (78.3) |
| External | 29 (16.3) | 0 (0–1) | 14 (48.3) | 15 (51.7) | 17 (58.6) |
| Family Action | 5 (2.8) | 0 (0–0) | 3 (60.0) | 3 (60.0) | 3 (60.0) |
| Significant Physiologic Disturbance |
243 | 6 (4–8) | 30 (12.3) | 27 (11.1) | 40 (16.5) |
| Tachypnea | 73 (30.0) | 1 (0–4) | 1 (1.4) | 0 | 1 (1.4) |
| Tachycardia | 72 (29.6) | 1 (0–4) | 15 (20.8) | 19 (26.4) | 23 (31.9) |
| Hypertension | 50 (20.6) | 1 (1–2) | 6 (12.0) | 3 (6.0) | 7 (14.0) |
| Respiratory depression | 37 (15.2) | 0 (0–1) | 4 (10.8) | 3 (8.1) | 4 (10.8) |
| Desaturation | 7 (2.9) | 0 (0–0) | 4 (57.1) | 1 (14.3) | 4 (57.1) |
| Bradycardia | 2 (0.8) | 0 (0–0) | 0 | 0 | 0 |
| Hypotension | 2 (0.8) | 0 (0–0) | 0 | 1 (50.0) | 1 (50.0) |
IQR= interquartile range
Two hundred forty-three significant physiologic disturbances were observed with a mean of six significant physiologic disturbances per resuscitation (range 1 to 14 per resuscitation). Tachypnea (n=73, 30.0%) and tachycardia (n=72, 29.6%) were the most frequently observed significant physiological disturbances. Teams responded to only 16.5% of significant physiologic disturbances (Table 3). Among all the frequently occurring significant physiologic disturbances, team acknowledgement and compensation occurred more frequently for tachycardia (n=15, 20.8% and n=19, 26.4%, Table 3). The average duration of a significant physiologic disturbance was 2 min 57 sec, ranging from was 30 sec to 33 min 52 sec.
The number of errors and the number of high-risk errors per resuscitation increased with the number of non-error process deviations per resuscitation (correlation coefficient=0.42 p=0.01 and correlation coefficient=0.62 p<0.001, respectively). Neither the number of errors or the number of high-risk errors per resuscitation, however, correlated with the number of significant physiologic disturbances per resuscitation (correlation coefficient=0.07 p=0.69 and correlation coefficient=0.17 p=0.30, respectively) or the total duration of significant physiologic disturbances per resuscitation (correlation coefficient=0.20 p=0.22). Daytime events had more errors than nighttime events (p=0.03, Table 4). Events during which a role other than a junior surgical resident performed the examination had more errors and more high-risk errors (p=0.03 and p=0.04, respectively [Table 4]). No significant difference or correlation between any other patient or resuscitation feature and error or high-risk error frequency was observed (Table 4). The effects of time of day and bedside provider role on number of errors and high-risk errors, however, were not significant in multivariate analysis controlling for injury severity (ISS), initial triage level and team pre-notification.
Table 4.
Association of Patient and Resuscitation Features with Number of Errors and High-Risk Errors
| Resuscitation Features | Median Number of Errors (IQR) |
Correlation Coefficient for all Errors |
p- value |
Median Number of High- risk Errors (IQR) |
Correlation Coefficient for High- risk Errors |
p- value |
|---|---|---|---|---|---|---|
| Age | 0.07 | 0.65 | 0.15 | 0.37 | ||
| Gender | ||||||
| Male | 7.5 (6–10.5) | 0.50 | 3 (2–5) | 0.70 | ||
| Female | 9 (5–15) | 4 (2–10) | ||||
| Mechanism of injury | ||||||
| Blunt (reference) | 8 (6–11) | 3.5 (2–5) | ||||
| Penetrating | 9.5 (3–16) | 0.95 | 2.5 (2–3) | 0.37 | ||
| Burn | 3 (3–3) | 0.13 | 3 (3–3) | 0.78 | ||
| ISS | ||||||
| All values | 0.09 | 0.58 | 0.15 | 0.36 | ||
| ISS ≤ 10 | 8 (6–11) | 0.93 | 3 (2–5) | 0.35 | ||
| ISS > 10 | 6 (5–15) | 3 (2–4) | ||||
| Activation level | ||||||
| Stat | 8 (6–12) | 0.48 | 2.5 (2–5) | 0.14 | ||
| Transfer | 7 (6–10) | 4 (3–5) | ||||
| Surgical team | ||||||
| Fellow not present | 8 (5–11) | 0.77 | 3 (2–5) | 0.83 | ||
| Fellow present | 8 (6–11.5) | 3 (2–5) | ||||
| Junior resident as examiner | 7 (5–10) | 0.03 | 3 (2–4) | 0.04 | ||
| Other role as examiner | 11.5 (11–13.5) | 7.5 (4–12.5) | ||||
| Team pre-notification | ||||||
| Pre-notification | 7 (5–10) | 0.13 | 3 (2–5) | 0.39 | ||
| No pre-notification | 11 (8–12) | 4 (3–6) | ||||
| Time of resuscitation | ||||||
| Weekday event | 8 (6–12) | 0.51 | 3 (2–4) | 0.60 | ||
| Weekend event | 7.5 (6–10) | 4 (2–6) | ||||
| Daytime event (7 AM–7 PM) | 10 (8–12) | 0.03 | 3 (2–4) | 0.90 | ||
| Nighttime event (7 PM–7 AM) | 6 (4–10) | 3 (2–6) | ||||
ISS, injury severity score
In multivariate models that controlled for patient and event features, selection errors were less commonly associated with all categories of response (acknowledgement p=0.03, compensation p=0.004, response p=0.01) than errors of omission. Selection errors were also less commonly associated with acknowledgement and compensation (p=0.04 and p=0.01, respectively) than errors of commission (Table 5). No significant difference in the association of errors of omission and commission with response was observed (p=0.64). No significant difference in response of any kind was seen between high and low-risk errors (acknowledgement p=0.86, compensation p=0.06, response p=0.10). Errors occurring after the secondary survey were less frequently compensated for than errors committed during all other phases (preparatory p=0.03, primary survey p<0.001, secondary survey p=0.003) and less frequently responded to than errors during the primary and secondary surveys (p=0.02 and p=0.05, respectively [Table 5]). Errors occurring in the evaluation and management of patients injured by a penetrating mechanism were more frequently acknowledged, compensated for, and responded to than those injured by a blunt mechanism (p=0.01, p=0.04, and p=0.04, respectively [Table 5]). Errors occurring during a resuscitation in which a role other than a junior surgical resident performed the bedside evaluation were more frequently acknowledged (p=0.03 [Table 5]).
Table 5.
Multivariate Analysis of Patient, Event and Error Features and Team Response to Errors
| Features | Error Acknowledgement Odds Ratio (CI) |
Error Compensation Odds Ratio (CI) |
Overall Team Response Odds Ratio (CI) |
|---|---|---|---|
| Male (reference = female) | 1.05 (0.51, 2.15) | 0.57 (0.24, 1.35) | 0.64 (0.28, 1.46) |
| Age | 0.99 (0.51, 1.04) | 0.99 (0.92, 1.06) | 0.99 (0.93, 1.06) |
| Transfer triage (reference = triage as ‘stat’) | 0.81 (0.42, 1.55) | 0.90 (0.40, 2.01) | 1.01 (0.47, 2.18) |
| Mechanism of injury (reference = blunt) | |||
| Penetrating | 5.91 (1.42, 24.52) | 7.12 (1.13, 44.67) | 6.53 (1.10, 38.60) |
| Burn | na* | 3.16 (0.19, 53.69) | 2.37 (0.15, 37.67) |
| ISS > 10 (reference = ISS ≤ 10) | 1.31 (0.50, 3.39) | 0.88 (0.28, 2.74) | 1.10 (0.37, 3.27) |
| No pre-notification (reference = team notified in advance) | 0.66 (0.30, 1.46) | 1.15 (0.45, 3.97) | 0.98 (0.40, 2.45) |
| Weekend (reference = weekday) | 1.01 (0.57, 1.80) | 0.97 (0.49, 1.93) | 1.16 (0.60, 2.23) |
| Daytime (reference = nighttime) | 0.52 (0.23, 1.16) | 0.65 (0.26, 1.65) | 0.54 (0.22, 1.33) |
| Surgical fellow present | 1.13 (0.61, 2.10) | 0.77 (0.36, 1.64) | 0.99 (0.49, 2.02) |
| Junior resident present | 0.36 (0.14, 0.92) | 0.58 (0.18, 1.89) | 0.39 (0.13, 1.18) |
| High risk | 0.95 (0.56, 1.62) | 1.72 (0.98, 3.00) | 1.58 (0.92, 2.73) |
| Error class (reference = selection) | |||
| Omission | 2.07 (1.09, 3.93) | 2.58 (1.35, 4.95) | 2.25 (1.20, 4.21) |
| Commission | 2.10 (1.05, 4.21) | 2.53 (1.24, 5.14) | 1.95 (0.98, 3.88) |
| Commission (reference = omission) | 1.02 (0.56, 1.62) | 0.98 (0.54, 1.79) | 0.87 (0.48, 1.57) |
| Phase (reference = post-secondary survey) | |||
| Preparatory phase | 1.89 (0.64, 5.61) | 3.78 (1.17, 12.16) | 1.88 (0.63, 5.63) |
| Primary survey | 1.59 (0.69, 3.68) | 5.65 (2.24, 14.23) | 2.73 (1.18, 6.36) |
| Secondary survey | 1.77 (0.80, 3.91) | 3.76 (1.56, 9.04) | 2.23 (1.00, 4.98) |
ISS, injury severity score; na, not applicable;
no errors were acknowledge during the resuscitation of the burn patient
DISCUSSION
Medical errors leading to patient harm remain a significant health burden.(17) Identifying factors associated with these errors, as well as responses to them, is a critical step in reducing their occurrence and mitigating their effect. In this preliminary report, we performed an analysis of errors in pediatric trauma resuscitation at our institution to identify patterns of behavior associated with their occurrence. Many errors that can lead to patient harm cannot be anticipated. For this reason, error analysis that accounts for near misses in addition to those leading to adverse events has been proposed as a strategy for understanding error causation and response.(6, 10, 18–20) The hypothesis underlying this approach is that the causation of errors that lead to harm is similar to that of errors that do not reach the patient because of mitigation, patient status or chance. By identifying errors and associated patterns, regardless of actual patient harm, strategies may be developed to reduce errors or mitigate their effects.
Although identification of specific errors is useful, classification of errors into broader groups further facilitates error analysis. A reproducible classification in the context of pediatric trauma resuscitation may allow differentiating errors that are observed from factors that lead to them.(21) Errors have been studied in diverse medical disciplines and error types, team response, and potential error impact differ among disciplines, and even among studies addressing trauma resuscitation.(10, 22–24) These differences may be attributable to variations in practices between disciplines and differences in patient profiles. Because of these variations, development of a generalizable classification scheme will be useful for clarifying the impact of errors in different clinical settings.
Previous work has shown an increased incidence of NREs among patients experiencing significant physiologic disturbances in the operating room.(13) Assessment of factors surrounding or associated with errors, such as non-error process deviations and significant physiologic disturbances, may help identify conditions that should lead teams to have increased vigilance for errors. In this initial study, we were unable to show an association between error frequency and the frequency of significant physiologic disturbances. We were, however, able to show a positive correlation between the frequency of errors that occurred and the frequency of non-error process deviations. This finding suggests the occurrence of non-preventable non-routine events creates an environment in which teams may be more likely to commit preventable errors. The correlation between non-error events and errors within trauma resuscitation is similar to findings in a study of errors occurring during cardiac surgery.(25)
We observed that errors of all types were most common during the primary and secondary survey. Previous studies evaluating errors during trauma resuscitation have also found high error occurrence during the initial assessment phases.(3, 8, 9, 26) This finding may be related to a higher frequency of tasks during these phases, increasing the opportunity for error and increasing the vulnerability to error occurrence because of workload. In contrast to previous studies of trauma resuscitation, we did not observe an association between the number of errors and either injury severity or team leader experience.(27, 28) Because we also observed no association between injury severity or leader experience and the number of high-risk errors per resuscitation, this finding was not related to our use of a broader definition for errors that also included those at low-risk for patient harm.
In our study, near-miss errors were commonly observed, with more than half not recognized or acknowledged by the trauma teams. The reasons that near-misses that had no apparent team response did not cause harm may have been related to several factors, including patient ‘robustness’ (resilience to the impact of a given error) (19), the absence of an injury that the error would have impacted, the occurrence of errors at low risk for potential harm (errors with a low probability of causing harm even among vulnerable patients) and ‘luck’ (unidentified circumstances preventing error propagation to the patient) (19). We also observed that the teams’ response to errors differed by error type and risk as well as phase of the resuscitation and mechanism of injury. We did not observe differences in response to errors related to either injury severity or type of team leader. These findings highlight the importance of assessing not only error occurrence but also response to errors when implementing performance improvement interventions in this setting.
This study has several limitations. First, because this study was performed at a single institution, the results may not be generalizable to other trauma centers. Second, this study was based on a sample of trauma resuscitations with few severely injured children. Confirmation of results in a large population and assessment of error patterns in severely injured children is critical for a complete description of deviations during trauma resuscitations. Third, error coding was based on subjective evaluation by experienced reviewers and could be subject to bias. We attempted to minimize this bias by using a two phased coding and classification approach and including several evaluators at each phase. Finally, our approach was based on the hypothesis that errors that do not lead to harm have a similar causation as those that do result in harm. Although we have classified the risk of harm, validation of this risk will require a large-scale study in which each error type is linked with an observed adverse event.
Approaches for preventing and mitigating errors may depend on the nature of and frequency of each error type. For frequently occurring errors, education or changes in the processes used for trauma resuscitation may help prevent their occurrence. For rare or unpredictable errors, strategies that are focused on early recognition and mitigation may be more appropriate. Analysis of near-misses has many advantages over adverse event analysis for identifying strategies for improving performance, including a greater frequency allowing quantitative analysis of error causation and response. Our study highlighted the advantages of quantitative error analysis, providing several new insights based on analyses of the type of and responses to errors and their association with patient and resuscitation features. Although these errors did not cause harm, our findings show the potential for using observation of everyday clinical work and the errors that occur within it as a method for performance improvement when adverse outcomes are rare. Identification of patterns of errors that do not lead to patient harm can aid in identifying risk factors for adverse outcomes and prevention of error-related patient injury.
Supplementary Material
Acknowledgments
Disclosures: Research reported in this paper was supported by the National Library of Medicine of the National Institutes of Health under award number R01LM011834.
Footnotes
Meeting Presentations: Pediatric Trauma Society Podium Presentation, November 6, 2015
Author Contribution:
Rachel Webman: study design, literature search, data collection, data analysis and interpretation, writing
Jennifer Fritzeen: study design, data collection, data interpretation, critical revision
JaeWon Yang: data collection, data analysis
Grace Ye: data collection
Paul Mullan: data collection, data analysis, critical revision
Faisal Qureshi: data collection, data analysis
Sarah Parker: study design, literature search, critical revision
Aleksandra Sarcevic: study design, critical revision
Ivan Marsic: study design, critical revision
Randall Burd: study design, literature search, data analysis, data interpretation, writing, critical revision
Contributor Information
Rachel Webman, Email: rwebman@childrensnational.org.
Jennifer Fritzeen, Email: jfritzee@childrensnational.org.
JaeWon Yang, Email: jayang@childrensnational.org.
Grace F. Ye, Email: grace_ye@gwmail.gwu.edu.
Paul C. Mullan, Email: mullan20@gmail.com.
Faisal G. Qureshi, Email: Faisal.Qureshi@UTSouthwestern.edu.
Sarah H. Parker, Email: sarah.henrickson.parker@gmail.com.
Aleksandra Sarcevic, Email: as3653@drexel.edu.
Ivan Marsic, Email: imarsic@gmail.com.
Randall S. Burd, Email: rburd@childrensnational.org.
REFERENCES
- 1.Pucher PH, Aggarwal R, Twaij A, Batrick N, Jenkins M, Darzi A. Identifying and addressing preventable process errors in trauma care. World journal of surgery. 2013;37(4):752–758. doi: 10.1007/s00268-013-1917-9. [DOI] [PubMed] [Google Scholar]
- 2.Georgiou A, Lockey DJ. The performance and assessment of hospital trauma teams. Scandinavian journal of trauma, resuscitation and emergency medicine. 2010;18:66. doi: 10.1186/1757-7241-18-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzgerald M, Gocentas R, Dziukas L, Cameron P, Mackenzie C, Farrow N. Using video audit to improve trauma resuscitation--time for a new approach. Canadian journal of surgery Journal canadien de chirurgie. 2006;49(3):208–211. [PMC free article] [PubMed] [Google Scholar]
- 4.Vincent CA. Analysis of clinical incidents: a window on the system not a search for root causes. Quality & safety in health care. 2004;13(4):242–243. doi: 10.1136/qshc.2004.010454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinger MB, Slagle J, Jain S, Ordonez N. Retrospective data collection and analytical techniques for patient safety studies. Journal of biomedical informatics. 2003;36(1–2):106–119. doi: 10.1016/j.jbi.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Corcorn WR. Defining and Analyzing Precursors. In: Phimister JR, Bier VM, Kunreuther HC, editors. Accident Precursor Analysis and Management: Reducing Technological Risk Through Diligence. Washington DC: National Academy of Engineering; 2004. pp. 79–88. [Google Scholar]
- 7.Stahl KD, Brien SE. Reducing Patient Errors in Trauma Care. In: Cohn SM, editor. Acute Care Surgery and Trauma: Evidence Based Practice. London United Kingdom: Informa Healthcare; 2009. pp. 268–277. [Google Scholar]
- 8.Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, et al. Trauma deaths in a mature urban trauma system: is "trimodal" distribution a valid concept? Journal of the American College of Surgeons. 2005;201(3):343–348. doi: 10.1016/j.jamcollsurg.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Annals of surgery. 2006;244(3):371–380. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarke JR, Spejewski B, Gertner AS, Webber BL, Hayward CZ, Santora TA, et al. An objective analysis of process errors in trauma resuscitations. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2000;7(11):1303–1310. doi: 10.1111/j.1553-2712.2000.tb00480.x. [DOI] [PubMed] [Google Scholar]
- 11.Weinger MB, Slagle J. Human factors research in anesthesia patient safety. Proceedings / AMIA Annual Symposium AMIA Symposium. 2001:756–760. [PMC free article] [PubMed] [Google Scholar]
- 12.Schraagen JM, Schouten T, Smit M, Haas F, van der Beek D, van de Ven J, et al. A prospective study of paediatric cardiac surgical microsystems: assessing the relationships between non-routine events, teamwork and patient outcomes. BMJ quality & safety. 2011;20(7):599–603. doi: 10.1136/bmjqs.2010.048983. [DOI] [PubMed] [Google Scholar]
- 13.Slagle JM, Anders S, Porterfield E, Arnold A, Calderwood C, Weinger MB. Significant Physiological Disturbances Associated With Non-Routine Event Containing and Routine Anesthesia Cases. Journal of patient safety. 2014 doi: 10.1097/PTS.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 14.Bonafide CP, Brady PW, Keren R, Conway PH, Marsolo K, Daymont C. Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics. 2013;131(4):e1150–e1157. doi: 10.1542/peds.2012-2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Swiet M, Fayers P, Shinebourne EA. Systolic blood pressure in a population of infants in the first year of life: the Brompton study. Pediatrics. 1980;65(5):1028–1035. [PubMed] [Google Scholar]
- 16.Rabbia F, Grosso T, Cat Genova G, Conterno A, De Vito B, Mulatero P, et al. Assessing resting heart rate in adolescents: determinants and correlates. Journal of human hypertension. 2002;16(5):327–332. doi: 10.1038/sj.jhh.1001398. [DOI] [PubMed] [Google Scholar]
- 17.Regenbogen SE, Greenberg CC, Studdert DM, Lipsitz SR, Zinner MJ, Gawande AA. Patterns of technical error among surgical malpractice claims: an analysis of strategies to prevent injury to surgical patients. Annals of surgery. 2007;246(5):705–711. doi: 10.1097/SLA.0b013e31815865f8. [DOI] [PubMed] [Google Scholar]
- 18.Bonrath EM, Gordon LE, Grantcharov TP. Characterising 'near miss' events in complex laparoscopic surgery through video analysis. BMJ quality & safety. 2015;24(8):516–521. doi: 10.1136/bmjqs-2014-003816. [DOI] [PubMed] [Google Scholar]
- 19.Kessels-Habraken M, Van der Schaaf T, De Jonge J, Rutte C. Defining near misses: towards a sharpened definition based on empirical data about error handling processes. Social science & medicine (1982) 2010;70(9):1301–1308. doi: 10.1016/j.socscimed.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Yamada NK, Yaeger KA, Halamek LP. Analysis and classification of errors made by teams during neonatal resuscitation. Resuscitation. 2015;96:109–113. doi: 10.1016/j.resuscitation.2015.07.048. [DOI] [PubMed] [Google Scholar]
- 21.Wears RL, Erik H, editors. E H. Looking for patterns in everyday clinical work. Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work 2. Surrey England: Ashgate Publishing Limited; 2015. [Google Scholar]
- 22.Ivatury RR, Guilford K, Malhotra AK, Duane T, Aboutanos M, Martin N. Patient safety in trauma: maximal impact management errors at a level I trauma center. The Journal of trauma. 2008;64(2):265–270. doi: 10.1097/TA.0b013e318163359d. discussion 70–2. [DOI] [PubMed] [Google Scholar]
- 23.Fabri PJ, Zayas-Castro JL. Human error, not communication and systems, underlies surgical complications. Surgery. 2008;144(4):557–563. doi: 10.1016/j.surg.2008.06.011. discussion 63–5. [DOI] [PubMed] [Google Scholar]
- 24.Barach P, Johnson JK, Ahmad A, Galvan C, Bognar A, Duncan R, et al. A prospective observational study of human factors, adverse events, and patient outcomes in surgery for pediatric cardiac disease. The Journal of thoracic and cardiovascular surgery. 2008;136(6):1422–1428. doi: 10.1016/j.jtcvs.2008.03.071. [DOI] [PubMed] [Google Scholar]
- 25.Solis-Trapala IL, Carthey J, Farewell VT, de Leval MR. Dynamic modelling in a study of surgical error management. Statistics in medicine. 2007;26(28):5189–5202. doi: 10.1002/sim.2886. [DOI] [PubMed] [Google Scholar]
- 26.Houshian S, Larsen MS, Holm C. Missed injuries in a level I trauma center. The Journal of trauma. 2002;52(4):715–719. doi: 10.1097/00005373-200204000-00018. [DOI] [PubMed] [Google Scholar]
- 27.Tsang B, McKee J, Engels PT, Paton-Gay D, Widder SL. Compliance to advanced trauma life support protocols in adult trauma patients in the acute setting. World journal of emergency surgery : WJES. 2013;8(1):39. doi: 10.1186/1749-7922-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oakley E, Stocker S, Staubli G, Young S. Using video recording to identify management errors in pediatric trauma resuscitation. Pediatrics. 2006;117(3):658–664. doi: 10.1542/peds.2004-1803. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.