Abstract
Background
Grey matter (GM) abnormalities are robust features of schizophrenia and of people at ultra high-risk for psychosis. However the extent to which neuroanatomical alterations are evident in non-clinical subjects with isolated psychotic experiences is less clear.
Methods
Individuals (mean age 20 years) with (n = 123) or without (n = 125) psychotic experiences (PEs) were identified from a population-based cohort. All underwent T1-weighted structural, diffusion and quantitative T1 relaxometry MRI, to characterise GM macrostructure, microstructure and myelination respectively. Differences in quantitative GM structure were assessed using voxel-based morphometry (VBM). Binary and ordinal models of PEs were tested. Correlations between socioeconomic and other risk factors for psychosis with cortical GM measures were also computed.
Results
GM volume in the left supra-marginal gyrus was reduced in individuals with PEs relative to those with no PEs. The greater the severity of PEs, the greater the reduction in T1 relaxation rate (R1) across left temporoparietal and right pre-frontal cortices. In these regions, R1 was positively correlated with maternal education and inversely correlated with general psychopathology.
Conclusions
PEs in non-clinical subjects were associated with regional reductions in grey-matter volume reduction and T1 relaxation rate. The alterations in T1 relaxation rate were also linked to the level of general psychopathology. Follow up of these subjects should clarify whether these alterations predict the later development of an ultra high-risk state or a psychotic disorder.
Keywords: Psychosis, Grey matter, VBM, DTI, MR relaxometry, ALSPAC, Neurodevelopment
Highlights
-
•
Differences in cortical R1 in young adults with psychotic experiences were found.
-
•
Implicates developmental processes related to myelination in psychotic illness.
-
•
The study utilises a large and well-controlled epidemiological cohort.
-
•
A novel approach to mapping microstructural parameters in cortex was employed.
1. Introduction
Grey matter (GM) abnormalities have been identified in several structures in schizophrenia patients (Ellison-Wright et al., 2008, Haijma et al., 2013, Honea et al., 2005, Velakoulis et al., 2006, Vita et al., 2006, Wright et al., 2000). The most heavily implicated are the prefrontal, parietal, temporal, anterior cingulate cortices, and hippocampus (Kanaan et al., 2005). GM volume is reduced in chronic versus first episode schizophrenia patients (Meisenzahl et al., 2008) and falls progressively with age(Vita et al., 2012).
In order to delineate structural brain differences that might predispose to psychosis, it is important to examine them without confounding effects of medication or chronic illness. Studies that examine first-episode or drug naive patients overcome such issues to some extent. A number of studies have also focused on high-risk groups: individuals presenting with the At-Risk Mental State (ARMS) or those deemed to be at ultra-high-risk (UHR) for psychosis (Fusar-Poli et al., 2013, Simon et al., 2011). Studies of GM alterations in this group have found macroscopic changes in the cerebral cortex (Borgwardt et al., 2007, Mechelli et al., 2011). A meta-analysis of VBM studies (Fusar-Poli et al., 2011) showed that at-risk groups tend to show reductions in GM volume in many of the regions implicated in schizophrenia, although the changes are generally less severe (Ziermans et al., 2009, Ziermans et al., 2012). Other meta-analyses (Borgwardt et al., 2011, Fusar-Poli et al., 2011) also found that reduced GM volume in prefrontal, cingulate, temporo-parietal, insular and cerebellar regions were significant predictors of transition to full-blown psychosis. More recent, larger and better controlled studies show defined GM structural changes associated with both risk of (Cropley et al., 2016) and transition to psychosis (Cannon et al., 2014, Mechelli et al., 2011, Pantelis et al., 2003, Ziermans et al., 2009). Of particular interest is the North American Prodrome Longitudinal Study which showed that young adults who later transition to psychosis have reduced frontal grey matter compared to those who do not transition (Cannon et al., 2015). Another large cohort, The Philadelphia Neurodevelopmental Cohort, of young adults with psychotic experiences showed reduced grey matter volume in medial temporal regions (Satterthwaite et al., 2016).
While numerous studies have examined GM morphometry in schizophrenia and at-risk groups, other imaging modalities that can provide insights into cortical microstructure have seldom been explored. MRI methods commonly used to quantify myelination and microstructure in white-matter may be used as putative measure of cyto- and myeloarchitecture in cortex (Weiskopf et al., 2015). For example, T1 relaxometry (Homer and Beevers, 1985) is sensitive to myelin content in health and disease and can be used to derive high-resolution cortical myelin maps in vivo (Dinse et al., 2015, Lutti et al., 2013). To our knowledge, no studies have investigated in vivo cortical myelination using MRI in schizophrenia or in at risk-groups. Diffusion tensor imaging (DTI) (Basser et al., 1994), has been applied to investigate changes in cortical microstructure in a number of clinical groups (Kang et al., 2012, Muñoz Maniega et al., 2004, Oreja-Guevara et al., 2005, Rovaris et al., 2006, Vite et al., 2008), Most commonly, mean diffusivity (MD) is used as an inverse measure of cellular density. One recent study (Park et al., 2014) examined diffusivity of frontal and temporal cortices and found it to be higher in schizophrenia patients. To our knowledge, there are no published MRI studies of cortical diffusivity in non-familial at-risk groups.
There are several risk-factors associated with the development of psychosis. These include obstetric factors (Abel et al., 2010, Dalman et al., 2001, Foerster et al., 1991, Lewis, 2002, Rifkin et al., 1994) socioeconomic disadvantage (Byrne et al., 2004, Gallagher et al., 2013, O'Donoghue et al., 2015, Werner et al., 2007), premorbid IQ (David et al., 1997, Woodberry et al., 2008, Zammit et al., 2004), childhood trauma and life stress (Gallagher et al., 2013, Kraan et al., 2015, Morgan and Fisher, 2007, Norman and Malla, 1993) and substance abuse (Kelly, 2000, Koskinen et al., 2009, Moore et al., 2007). The pathogenic processes underlying these factors are unknown and multiple mechanisms are possible. Some may operate through the cyto- and myeloarchitecture of the cerebral cortex.
This study utilises a large epidemiological birth cohort, the Avon Longitudinal Study of Parents and Children (ALSPAC) (Boyd et al., 2013, Golding et al., 2001) cohort, which has rich biological, clinical and psychosocial data to examine the association between GM structure and PEs. Neuroimaging of this cohort has previously shown significant alterations white matter circuitry (Drakesmith et al., 2015, Drakesmith et al., 2016). We tested the hypothesis that abnormalities in GM volume and myeloarchitecture are associated with PEs even in the absence of a clinically identified disorder. This approach has a number of advantages. In particular, it allows the examination of PEs without selection biases and confounding factors such as secondary effects of illness including pharmacological treatment. Furthermore, the cohort has accrued unbiased longitudinal data on a number of developmental and socio-economic variables that can constitute risk factors for psychosis, affording us an opportunity to identify any relationships between them and GM abnormalities that may also be linked to PEs.
2. Methods and materials
2.1. Subjects
Subjects were recruited from the Avon Longitudinal Study of Parents and Children (ALSPAC) (Boyd et al., 2013, Golding et al., 2001) cohort. The original sample consisted of pregnant women whose expected delivery dates were between April 1991 and December 1992 resulting in the birth of 15,458 foetuses (see Supplementary material, Section 1 for full description of cohort). 4320 subjects from the cohort were assessed for psychotic experiences (PEs) using the Psychotic-like Symptoms (PLIKS) semi-structured interview (Horwood et al., 2008, Zammit et al., 2008), conducted at 17/18 years of age by trained psychologists. Those who were found to have one or more psychotic experience were invited to undergo scanning. The presence of PEs was judged according to clinical criteria of the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) (Wing et al., 1990) and excluded experiences occurring due to waking, falling asleep, fever or drug consumption. PEs were further categorised as ‘suspected’ (n = 44), ‘definite’, (n = 47) and ‘clinical disorder’ (PEs plus functional deterioration and/or help-seeking; n = 32) (Zammit et al., 2013). 126 subjects with PEs were recruited and an equal number of randomly-selected controls, who had completed the same assessments but who were rated as not having had PEs experiences were also scanned. At the time of scanning all subjects were approximately 20 years old (see Table 1 for details).
Table 1.
Descriptive and inferential statistics for the candidate covariates. Descriptive statistics for continuous variables report mean ± standard error for each group. Descriptive statistics for ordinal and categorical variables are reported as tabulated frequencies. Inferential statistics for the 2-group binary classification uses the student t-test for continuous, the χ2-test for categorical and the Cochrane-Armitage χ2-test (denoted χ2CM) for ordinal variables. Inferential statistics for the 4-group ordinal classification uses Spearman's ρ correlation for continuous and ordinal variables and χ2CM test for categorical variables.
| Variable | Descriptive statistics |
Inferential statistics |
Proportion imputed | |||||
|---|---|---|---|---|---|---|---|---|
| No PEs | With PEs |
2-Group binary classification | 4-Group ordinal classification | |||||
| Suspect | Definite | Clinical | Total | |||||
| 1. Premorbid IQ | 111.44 ± 0.12 | 104.65 ± 0.31 | 106.79 ± 0.32 | 103.13 ± 0.42 | 105.07 ± 0.12 |
t = 3.456 p = 0.001⁎⁎ |
ρ = − 0.188 p = 0.003⁎⁎ |
0.137 |
| 2. CIS-R score | 6.30 ± 0.05 | 9.16 ± 0.17 | 12.26 ± 0.18 | 16.78 ± 0.34 | 12.33 ± 0.08 |
t = − 5.903 p = 1.2 × 10− 8⁎⁎ |
ρ = 0.408 p = 2.3 × 10− 11⁎⁎ |
0.065 |
| 3. Parental social class | 0.173 | |||||||
| I | 10 | 4 | 5 | 0 | 9 | χ2CM = 9.229, p = 0.002⁎⁎ | ρ = 0.204, p = 0.001⁎⁎ | |
| II | 54 | 10 | 16 | 5 | 31 | |||
| III (non-manual) | 52 | 24 | 23 | 20 | 67 | |||
| III (manual) | 6 | 0 | 0 | 2 | 2 | |||
| IV | 3 | 5 | 2 | 3 | 10 | |||
| V | 0 | 1 | 1 | 2 | 4 | |||
| 4. Highest maternal education | 0.065 | |||||||
| None | 11 | 8 | 5 | 5 | 18 | χ2CM = 9.022, p = 0.003⁎⁎ | ρ = − 0.197, p = 0.002⁎⁎ | |
| Vocational | 6 | 5 | 3 | 1 | 9 | |||
| Ordinary Level | 39 | 16 | 21 | 19 | 56 | |||
| Advanced Level | 34 | 7 | 7 | 4 | 18 | |||
| Degree | 35 | 8 | 11 | 3 | 22 | |||
| 5. Birth weight (g) | 3466.2 ± 4.0 | 3323.4 ± 12.6 | 3401.7 ± 9.7 | 3165.3 ± 18.5 | 3312.2 ± 4.3 | t = 2.335, p = 0.020⁎ | ρ = − 0.155, p = 0.015⁎ | 0.060 |
| 6. Resuscitated at birth | 0.387 | |||||||
| No | 106 | 33 | 38 | 27 | 98 | χ2 = 1.538, p = 0.463 | χ2CM = 0.141, p = 0.707 | |
| Yes | 19 | 11 | 9 | 5 | 25 | |||
| 7. Stressful life events | 0.173 | |||||||
| No | 111 | 36 | 40 | 23 | 99 | χ2 = 3.301, p = 0.069 | χ2CM = 4.451, p = 0.035⁎ | |
| Yes | 14 | 8 | 7 | 9 | 24 | |||
| 8. Handedness | 0.411 | |||||||
| Right | 92 | 36 | 34 | 22 | 92 | χ2CM = 0.001, p = 0.971 | ρ = 0.022, p = 0.737 | |
| No dominance | 25 | 6 | 9 | 7 | 22 | |||
| Left | 8 | 2 | 4 | 3 | 9 | |||
| 9. aTobacco consumption (cigarettes per day) | 0.59 ± 0.02 | 1.27 ± 0.08 | 0.44 ± 0.04 | 2.23 ± 0.14 | 1.20 ± 0.03 | t = − 1.717, p = 0.087 | ρ = 0.021, p = 0.737 | 0.472 |
| 10. bCannabis consumption | 0.411 | |||||||
| Never | 87 | 28 | 32 | 19 | 79 | χ2CM = 1.588, p = 0.208 | ρ = 0.077, p = 0.226 | |
| Once or twice | 11 | 6 | 4 | 1 | 11 | |||
| Less than monthly | 25 | 6 | 8 | 10 | 24 | |||
| Monthly or more | 2 | 4 | 3 | 2 | 9 | |||
| 11. cAlcohol consumption | 0.020 | |||||||
| Never | 16 | 6 | 2 | 0 | 8 | χ2CM = 1.045, p = 0.307 | ρ = 0.053, p = 0.408 | |
| Once or twice | 23 | 5 | 9 | 6 | 20 | |||
| Less than monthly | 12 | 5 | 9 | 6 | 20 | |||
| Monthly | 52 | 21 | 19 | 14 | 54 | |||
| Weekly or more | 22 | 7 | 8 | 6 | 21 | |||
| 12. dMonth of birth | 2.30 ± 7.52 | 1.72 ± 7.33 | 1.31 ± 7.50 | 2.18 ± 7.51 | 1.71 ± 7.44 | F = 1.565, p = 0.212 | ρ = 0.088, p = 0.384 | 0 |
| Standard covariates (included in all analyses) | ||||||||
| Age (years) | 20.11 ± 0.004 | 20.14 ± 0.013 | 19.88 ± 0.011 | 20.04 ± 0.015 | 20.01 ± 0.004 | t = 1.488, ρ = 0.138 | ρ = − 0.147, p = 0.020⁎ | 0 |
| Gender | 0 | |||||||
| Male | 49 | 14 | 16 | 7 | 37 | χ2 = 2.2757, p = 0.131 | χ2CM = 2.952, ρ = 0.085 | |
| Female | 76 | 30 | 31 | 25 | 86 | |||
The number of cigarettes participant smokes every day on average in the last 30 days.
From a multiple-choice question asking how many times the participant used cannabis in the past 12 months (all substance use data gathered at age 17/18).
6 or more units of alcohol in the past year.
As a scale from 0 (1st January) to 12 (31st December). A Watson-Williams 2-sample F-test and a circular-linear. ρ-correlation using the circular statistics toolbox (Berens and Baclawski, 2009).
p < 0.05.
p < 0.01.
Informed consent was obtained prior to scanning. Ethical approval was granted by the Cardiff University School of Psychology Ethics Committee and the ALSPAC Ethics and Law Committee. Of the subjects initially scanned, 3 PE subjects and 1 control were unable to complete the full MRI acquisition. While all participants completed the T1-weighted structural scan, the sample sizes for the relaxometry and diffusion MRI scans of the two groups were n = 123 and n = 125, respectively.
2.2. Risk factors
A number of candidate variables hypothesized to contribute to psychosis risk were obtained from the ALSPAC variable catalogue (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/). These included age and gender plus 12 other risk-factors: (1) IQ at age 8 estimated from the WISC (Wechsler Intelligence Scale for Children (WISC-IIIUK)) (Golombok and Rust, 1992); (2) current general psychopathology at age 17/18 measured using the computerised Clinical Interview Schedule (revised: CIS-R) (Lewis et al., 1992); (3) parental social class (OPCS, 1991); (4) maternal education; (5) birth weight; (6) resuscitation at birth; (7) stressful life events at age 15/16 measured on the Development and Wellbeing Assessment (DAWBA) questionnaire (Goodman et al., 2000); (8) handedness; (9) tobacco use; (10) alcohol consumed; (11) cannabis consumption (all substance use data gathered at age 17/18); (12) month of birth.
Any missing data points for each subject were estimated using regression imputation (S. F. Buck, 1960) across the entire cohort. Descriptive and inferential statistics of all selected risk factors are detailed in Table 1.
3. Imaging
3.1. Structural MRI acquisition
All MRI data were acquired at Cardiff University Brain Imaging Research Centre, UK on a 3 T General Electric HDx MRI system (GE Medical Systems, Milwaukee, WI) using an eight-channel receive-only head RF coil. T1-weighted structural images were acquired with a 3D fast spoiled gradient echo (FSPGR) sequence (TR = 7.8 ms, TE = 3.0 ms, flip angle 20°, voxel size = 1 mm3 isomorphic).
3.2. Relaxometry MRI acquisition and pre-processing
Relaxometry images were acquired using driven equilibrium single pulse observation of T1 with high-speed incorporation of RF field inhomogeneities (DESPOT1-HIFI) (Deoni, 2007). A series of spoiled gradient echo (SPGR) images was acquired with 8 flip angles plus an additional inversion-recovery (IR) SPGR image. All images had TE = 2.11 ms and TR = 4.7 ms, voxel resolution: 1.70 × 1.72 × 1.72 mm. SPGR images were acquired with flip angles of 3°, 4°, 5°, 6°, 7°, 9°, 13° and 18°. For the IR-SPGR acquisition, Inversion time = 450 ms and flip angle = 5°. The DESPOT1 protocol constitutes part of the mCDESPOT protocol (Deoni et al., 2008) which was also collected from this cohort. This method and associated findings are reported in Supplementary material, section 2.
Relaxometry data were pre-processed using FSL v5.0 (Jenkinson et al., 2012). All SPGR/IR-SPGR images were coregistered to each other using a rigid affine transform and skull-stripped (Smith, 2002). Relaxation rate (R1 = 1/T1) maps were derived using the (DESPOT1-HIFI) model (Deoni, 2007), which incorporates correction for B1 field inhomogeneities with in-house code. A synthetic T1-weigted image was computed from the quantitative T1 map with contrast matching that of the FSPGR image. This was used to compute a non-rigid affine transform using a mutual information cost function from the DESPOT space to the FSPGR space. This transform was then applied to the R1 maps so that they are now in the same space as the FSPGR T1-weighted images. Mislocalisation error between the two spaces was quantified to assess any potential impact these might have on subsequent statistical analysis (see Supplementary material, Section 4).
3.3. Diffusion acquisition and pre-processing
Diffusion MRI comprising a cardiac-gated diffusion-weighted spin-echo echo-planar imaging sequence was used to acquire high angular resolution diffusion weighted images (HARDI) (Jones et al., 1999). 60 gradient orientations and 6 unweighted (b = 0 s/mm2) images were acquired with the following parameters: TE = 87 ms, b = 1200 s/mm2, 60 slices, slice thickness = 2.4 mm, FoV = 230 × 230 mm, acquisition matrix = 96 × 96, resulting in data acquired with a 2.4 × 2.4 × 2.4 mm isotropic resolution following zero-filling to a 128 × 128 in-plane matrix for the fast Fourier transform. The final image resolution was therefore 1.8 × 1.8 × 2.4 mm.
HARDI data were pre-processed in ExploreDTI v4.8.3 (Leemans et al., 2009). Data were corrected for motion and eddy currents prior to tractography. Motion artefacts and eddy current distortions were corrected with B-matrix rotation (Leemans and Jones, 2009); field inhomogeneities were also corrected using standard approaches(Wu et al., 2008). Diffusion weighted images (DWIs) were non-linearly warped to a synthetic T1-weigted image computed from the quantitative T1 map from the DESPOT processing pipeline (see above) and using the fractional anisotropy map computed from the DWIs as a reference. Warps were computed using ‘Elastix’ (Klein et al., 2010) using normalised mutual information as the cost function and constraining deformations to the phase-encoding direction. The corrected DWIs are therefore in the same (undistorted) space as the mcDESPOT images.
The corrected HARDI data were fitted to the diffusion tensor (DT) and corrected for CSF-partial volume effects (Pasternak et al., 2009) was applied to the DTs. The mean diffusivity (MD) was then computed from the DT. Intra-scan head motion was quantified and assessed for potential impact on subsequent statistics (see Supplementary material, Section 4).
3.4. Voxel Based Morphometry (VBM).
Differences in GM were analysed using Voxel Based Morphometry (VBM) (Ashburner and Friston, 2000, Good et al., 2001) using an optimised VBM protocol in FSL (Douaud et al., 2007). T1-weighted structural images were skull stripped (Smith, 2002) and GM segmented (Zhang et al., 2001). The GM images were then non-linearly registered to the MNI152 brain template and a study-specific template was created from the average of the transformed GM images. All native GM images were non-linearly registered to this study-specific template and “modulated” to correct for local expansion and contraction due to non-linear components of the spatial transformation. The modulated GM images were then smoothed with an isotropic Gaussian kernel with a FWHM of 4mm3.
MD and R1 maps were also analysed with VBM. The MD and R1 data were registered to the original FSPGR T1-wieghted space using a non-rigid affine transform with the synthetic T1-wighted image as a reference. The grey matter segmentation from the FSPGR was then used to mask the grey matter in each image. The images were then registered to the VBM template using the same warp fields originally used to register the GM images. R1 and MD images were then smoothed with Gaussian kernels of 4mm3 and 8mm3, respectively, to accommodate differences in voxel size. Unlike the GM volume images, modulation was not performed for these images as these variables are not quantifying spatial properties, unlike GM volume. Modulation is therefore not appropriate for these images.
3.5. Statistical analysis
Statistical analyses were performed using a voxel-wise general linear model on the template-space images. Multiple comparisons across voxels were corrected using permutation-based non-parametric testing (Nichols and Holmes, 2002), with threshold-free cluster enhancement (Smith and Nichols, 2009) across 5000 permutations.
Two designs were tested. The first treats PE status as a binary classification (with PEs vs. without PEs). The second model treats the PE status as a 4-point ordinal scale (no PEs > suspected > definite > ‘clinical disorder’). In both cases, age and gender were treated as covariates. Maps of permutation corrected p-values (pcorr) were computed for each image metric (MD and R1) and each design (i.e. binary or 4-point ordinal classification). Effects are treated as significant at pcorr < 0.05. In the cases where was a significant correlation between a risk-factor and PEs, the analysis was also performed with the inclusion of the relevant risk factor as a covariate. In addition, correlations between GM measurements and the other risk factors were tested for, with age and gender treated as covariates.
4. Results
4.1. Demographics
Group effects on each of the candidate risk factors are reported in Table 1. Premorbid IQ, CIS-R scores, parental social class and maternal education all show strong effects in both the binary and the ordinal classifications (p < 0.01). A smaller, but still significant, group effect was also observed for birth weight (p < 0.05). All other risk factors showed no significant group effects.
4.2. Binary classification
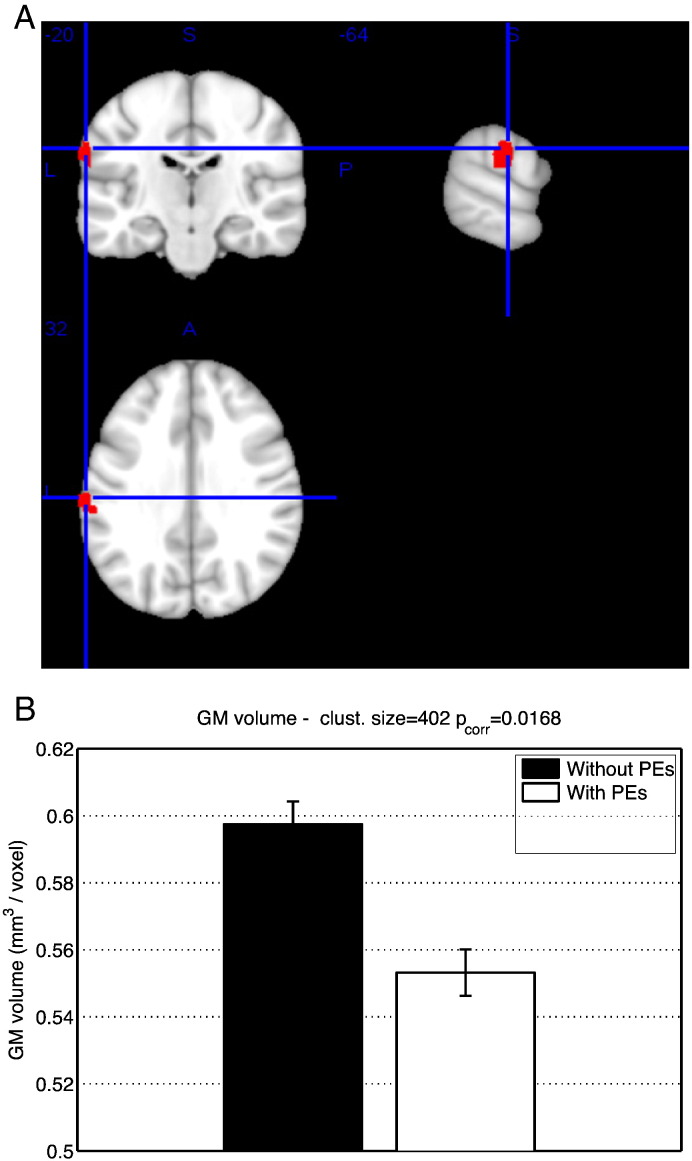
GM volume in a region of the left supramarginal gyrus (Fig. 1, Table 2) was decreased in subjects with PEs compared to subjects with no PEs. There were no group effects on MD or R1.
Fig. 1.
(A) Significant negative effects of PEs on GM volume using the binary classification of PEs. ROI volume 1976 mm3. MNI coordinates [− 64 − 20 32]. (B). mean and standard error of GM volume in significant ROI, with binary classification of PEs.
Table 2.
Regions of AAL atlas overlapping with regions of significant effect on GM volume, using the binary classification of PEs.
| Region | Overlap with ROI (# voxels) |
min pcrr | MNI coordinates |
|---|---|---|---|
| Supramarginal gyrus (left) | 164 | 0.027 | − 64 -20 32 |
| Postcentral (left) | 26 | 0.031 | − 62 -18–30 |
| Superior temporal (left) | 20 | 0.031 | − 56 -24–18 |
4.3. Ordinal model
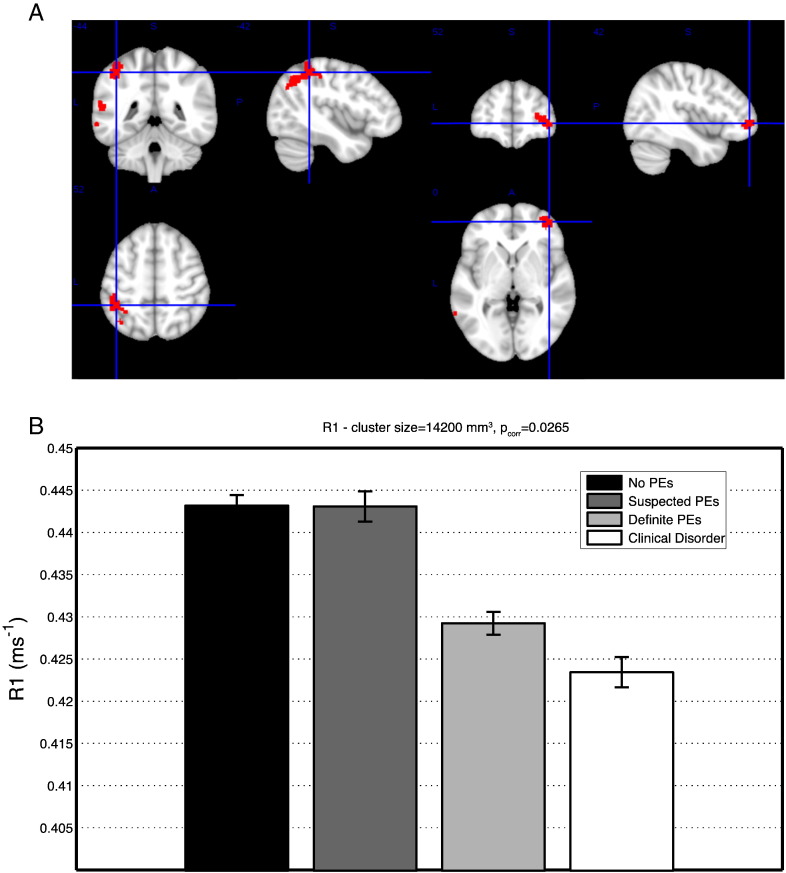
There was a significant negative effect in R1 in left temporoparietal and right pre-frontal regions (Fig. 2, Table 3), with R1 lowest for the suspected and definite PE groups. No significant effects were identified with GM volume or MD.
Fig. 2.
(A) Regions of significant effects of PEs on R1 inferred using the ordinal classification of PEs in left parietal and right frontal cortices. Parietal ROI: volume 11,088 mm3, MNI coordinates [− 42 − 44 52], Frontal ROI: volume 2696mm3 MNI coordinates [42 52 0]. (B) Mean and standard error of R1 value in the significant ROI, with ordinal classification of PEs.
Table 3.
Regions of the AAL atlas where R1 significantly correlates with PEs.
| Region | Overlap with ROI (# voxels) |
min pcorr | MNI coordinates |
|---|---|---|---|
| Parietal/temporal | |||
| Inferior parietal (left) | 399 | 0.026 | − 42 ·-44 52 |
| Middle temporal (left) | 392 | 0.028 | − 62 -50 − 10 |
| Angular gyrus (left) | 257 | 0.031 | − 52 -52 − 28 |
| Superior temporal (left) | 133 | 0.028 | − 58 -48 − 16 |
| Superior parietal (left) | 51 | 0.032 | − 38 -44 − 62 |
| Middle occipital (left) | 48 | 0.038 | − 36 -70 − 36 |
| Supramarginal gyrus (left) | 46 | 0.031 | − 54 -50 − 26 |
| Postcentral gyrus (left) | 45 | 0.032 | − 42 -38 − 58 |
| Frontal | |||
| Middle frontal (right) | 187 | 0.032 | 40 52 − 2 |
| Medial orbitofrontal (right) | 64 | 0.032 | 42 52 0 |
| Superior frontal (right) | 61 | 0.042 | 32 -52 − 10 |
| Inferior frontal operculum (left) | 38 | 0.044 | − 46 14 − 18 |
| Inferior orbitofrontal (right) | 22 | 0.034 | 40 48 0 |
(See Supplementary material, Section 3).
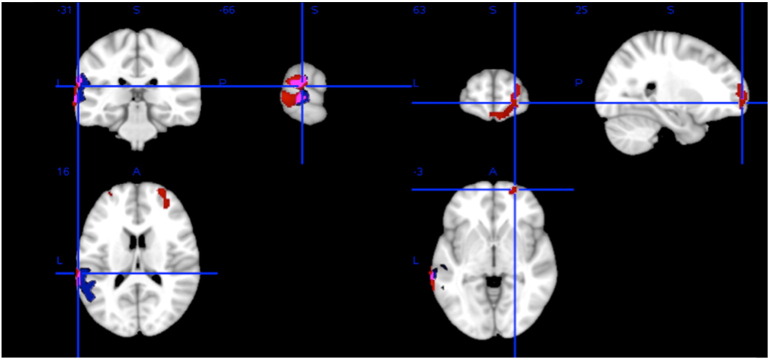
4.4. Correlation with risk factors
There were significant negative correlations between R1 and CIS-R and significant positive correlations between R1 and maternal education. Both these correlations overlap spatially with the correlations with PE status, although in the case of maternal education, the effect is limited to the left temporoparietal region (Fig. 3 and Table 4).
Fig. 3.
Regions of significant negative correlation between R1 and CIS-R score (red) and significant positive correlation between R1 and maternal education (blue). Overlap between the two Is violet. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Table 4.
Regions of the AAL atlas where R1 significantly correlates with CIS-R and maternal education.
| Region | Negative correlation with CIS-R score |
Positive correlation with maternal education |
||||
|---|---|---|---|---|---|---|
| Overlap with ROI (# voxels) |
min pcorr | MNI coordinates | Overlap with ROI (# voxels) |
min pcorr | MNI coordinates | |
| Frontal | ||||||
| Superior frontal (right) | 262 | 0.024 | 24 64 − 2 | 0 | – | – |
| Superior orbitofrontal (right) | 170 | 0.026 | 24 64 0 | 0 | – | – |
| Middle frontal (left) | 30 | 0.046 | − 28 56 − 14 | 0 | – | – |
| Middle frontal (right) | 216 | 0.024 | 32 58 − 20 | 0 | – | – |
| Middle orbitofrontal (right) | 84 | 0.032 | 10 64 14 | 0 | – | – |
| Inferior orbitofrontal (right) | 11 | 0.048 | 48 50 10 | 0 | – | – |
| Medial orbitofrontal (right) | 34 | 0.030 | 10 64 14 | 0 | – | – |
| Gyrus rectus (left) | 26 | 0.030 | 2 64 16 | 0 | – | – |
| Gyrus rectus (right) | 30 | 0.028 | 4 66 16 | 0 | – | – |
| Parietal/temporal | ||||||
| Supramarginal gyrus (left) | 77 | 0.020 | -64 -34 − 24 | 216 | 0.022 | − 54 -38 − 28 |
| Superior temporal (left) | 105 | 0.018 | − 64 -40 − 20 | 204 | 0.026 | − 60 -36 − 18 |
| Middle temporal (left) | 352 | 0.016 | − 68 -38 − 4 | 176 | 0.034 | − 52 -56 − 20 |
In addition, there were widespread positive correlations between MD and birth-weight, mostly in posterior cingulate, parietal and occipital cortices [data not shown] which did not overlap with the R1 changes nor were they associated with PEs. No other significant correlations were identified.
5. Discussion
This study used structural MRI, T1 relaxometry and diffusion tensor imaging (DTI) in conjunction with voxel-based morphometry (VBM) to characterise GM macrostructure and microstructure associated with psychotic experiences (PEs) in a large population-based sample of young adults.
Reduction in GM volume in this otherwise healthy group with PEs, centred on a single region: the left supramarginal gyrus, a key component of the ‘heteromodal association cortex’ regarded by some as being selectively affected in the pathological anatomy of schizophrenia (Buchanan et al., 2004). GM Abnormalities in those at increased genetic risk (Bhojraj et al., 2011), have also been detected in this region. However, when we compared our simple binary- with an ordinal-based model closer to the idea of a continuum of psychopathology, the binary model of PEs was associated with reduced volume whereas the ordinal model was not.
Alternately, it was the ordinal model that showed a reduction in cortical R1 in non-overlapping left temporoparietal and right prefrontal regions also noted to show changes in those at high risk of psychosis using conventional volumetric MRI. Such a broad topography of cortical regions has the potential to impinge on many important linguistic and executive functions. The discrepancy between our two main findings might be interpreted as different neuroanatomical substrates for general psychopathology, and more specific pathology relating to psychosis. However, there were no significant relationships with GM volume and CIS-R, or any other risk factors.
The regions where R1 is reduced with PEs are consistent with some of those previously found to show cortical pathology in psychosis risk-groups (Fusar-Poli et al., 2011, Smieskova et al., 2010), particularly pre-frontal and superior temporal regions. It is possible that GM volume reduction becomes more apparent at later stages of development. A meta-analysis (Fusar-Poli et al., 2011) found that GM volume was significantly reduced in older at-risk groups (25 + years) compared to younger at-risk groups.
The interpretation that reduced R1 is reflective of reductions in cortical myelination (Lutti et al., 2014) is consistent with previous histological and post-mortem studies (see (Bakhshi and Chance, 2015, Esiri and Crow, 2008, Harrison and Harrison, 1999) for reviews). Of relevance are studies that have shown evidence of reduced oligodendrocyte number (Hof et al., 2002, Hof et al., 2003, Uranova et al., 2004), notably in frontal cortex particularly affecting layer VI, but not in the adjacent white-matter (Uranova et al., 2004). This could be a pathological corollary of the R1 relaxometry findings. More evidence exists of reductions in myelin basic protein (MBP) staining in schizophrenia (Chambers and Perrone-Bizzozero, 2004, Honer et al., 1999) and altered expression of myelin-related genes (Hakak et al., 2001, Katsel et al., 2005, Roussos and Haroutunian, 2014).
In addition, there is evidence that the developmental trajectory of myelination predicts the trajectory of grey matter volume (Gilmore et al., 2012, Sowell et al., 2003), although this relationship is complex (Deoni et al., 2015). It is possible that changes seen in cortical myelination will manifest as changes in cortical volume later in life and there is some evidence supporting this in our data (see Supplementary material, Section 5). Changes in cortical myelination may be related to synaptic pruning in late adolescence (Huttenlocher and Dabholkar, 1997, Paus et al., 2008), which leads to later reductions in cortical volume. The effects observed in the present study may reflect either a delay or a reduction of this process. Further imaging of the cohort will help verify this. It is also interesting to note that the temporoparietal region where the effect of R1 is seen, has been identified as having the most protracted rate of cortical development (Sowell et al., 2003) which might render it vulnerable to a range of insults over time. Furthermore the absence of correlations between RI measures and early neurodevelopmental factors (birthweight and premorbid IQ at age 8) indicate that such factors are not implicated in the proposed myelin-related pathogenesis of psychosis which occurs at developmental stages closer to the age of the cohort. It is important to note that that T1 relaxation is also sensitive to other factors such as macromolecular composition (proteins and lipids) (Bottomley et al., 1984, Rooney et al., 2007) and iron content (Gelman et al., 2001), so the interpretation of reduced R1 reflecting reduced cortical myelination should be made with caution.
The correlation analysis revealed significant associations between CIS-R score and maternal education, a proxy for socio-economic status, on R1, in regions overlapping with those where the main effect with PEs was observed. It is therefore possible that myelination, and possibly the neurodevelopmental processes described above, are delayed or diminished by poor socioeconomic environment, perhaps via physiological stress mechanisms, e.g., infection and inflammation (Najjar and Pearlman, 2014). The correlations with these factors and the absence of any cortical R1 effects when covarying for these factors suggest myelination, macromolecular composition or iron content is related to more general psychopathology and socioeconomic influences rather than specifically psychosis. The absence of any apparent effect in cortical diffusivity, suggests that change in cell density is not necessarily associated with PEs when seen in a non-clinical context. As with GM volume change, this may be something that does not manifest until later stages of illness. Again longitudinal studies will help clarify this.
There were negative correlations between cortical diffusivity and birth weight, indicating a possible early neurodevelopment influence on the cytoarchitecture of mature cortex, but we found no relationship with psychopathology, despite such an association being documented (Abel et al., 2010, Rifkin et al., 1994). Furthermore, this effect appeared to be independent of any other measured properties in cortex.
The study has a number of strengths, namely the size and population base of the sample uncontaminated by for example medication exposure. Psychopathology was verified using a structured clinical interview and there was extensive socio-demographic and clinical data available on the sample. The imaging methodology was state-of-the-art and included novel application of measures to at-risk groups for psychosis. Weaknesses include the cross sectional nature of the imaging data and the narrow age-range of the participants limiting the developmental inferences that can be drawn. A further limitation is the lack of follow-up information on the cohort, pertaining to progression or remission of PEs. As a result the clinical significance of PEs is unclear. In particular, the risk of a later UHR state, or psychotic disorder is unknown.
In conclusion, there is evidence of a link between cortical volume and R1 in cortex and verified psychotic experiences in young adults drawn from the general population. The alterations in R1 may be reflective of decreased cortical myelination, although macromolecular composition may also be responsible. The effect is consistent with an altered neurodevelopmental trajectory, prior to measureable changes in cortical volume as typically seen in schizophrenia patients and ultra high risk groups. There is also evidence that this marker of neurodevelopment is affected by socioeconomic environment.
Financial declarations
All authors report no biomedical financial interests or potential conflicts of interest.
Acknowledgements
This research project was funded by a grant from the UK Medical Research Council (grant number: G0901885).
The UK Medical Research Council and the Wellcome Trust (Grant number: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC.
Research was also supported by a Wellcome Trust New Investigator Award, awarded to DKJ. ASD, AD and AR were supported by the National Institutes of Health Research Biomedical Research Centre at the South London & Maudsley Hospital Foundation NHS Trust and the Institute of Psychiatry, Kings College London.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.nicl.2016.09.002.
Appendix A. Supplementary data
Supplementary material.
References
- Abel K.M., Wicks S., Susser E.S., Dalman C., Pedersen M.G., Mortensen P.B., Webb R.T. Birth weight, schizophrenia, and adult mental disorder: is risk confined to the smallest babies? Arch. Gen. Psychiatry. 2010;67:923–930. doi: 10.1001/archgenpsychiatry.2010.100. [DOI] [PubMed] [Google Scholar]
- Ashburner J., Friston K.J. Voxel-based morphometry—the methods. NeuroImage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- Bakhshi K., Chance S.A. The neuropathology of schizophrenia: a selective review of past studies and emerging themes in brain structure and cytoarchitecture. Neuroscience. 2015;303:82–102. doi: 10.1016/j.neuroscience.2015.06.028. [DOI] [PubMed] [Google Scholar]
- Basser P.J., Mattiello J., LeBihan D. MR diffusion tensor spectroscopy and imaging. Biophys. J. 1994;66:259–267. doi: 10.1016/S0006-3495(94)80775-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berens P., Baclawski K. CircStat: a MATLAB toolbox for circular statistics. J. Stat. Softw. 2009;30:1–3. [Google Scholar]
- Bhojraj T.S., Sweeney J.A., Prasad K.M., Eack S., Rajarethinam R., Francis A.N., Montrose D.M., Keshavan M.S. Progressive alterations of the auditory association areas in young non-psychotic offspring of schizophrenia patients. J. Psychiatr. Res. 2011;45:205–212. doi: 10.1016/j.jpsychires.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgwardt S.J., McGuire P.K., Aston J., Berger G., Dazzan P., Gschwandtner U., Pflüger M., D'Souza M., Radue E.-W., Riecher-Rössler A. Structural brain abnormalities in individuals with an at-risk mental state who later develop psychosis. Br. J. Psychiatry Suppl. 2007;51:s69–s75. doi: 10.1192/bjp.191.51.s69. [DOI] [PubMed] [Google Scholar]
- Borgwardt S., McGuire P., Fusar-Poli P. Gray matters!—mapping the transition to psychosis. Schizophr. Res. 2011;133:63–67. doi: 10.1016/j.schres.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Bottomley P.A., Foster T.H., Argersinger R.E., Pfeifer L.M. A review of normal tissue hydrogen NMR relaxation times and relaxation mechanisms from 1–100 MHz: dependence on tissue type, NMR frequency, temperature, species, excision, and age. Med. Phys. 1984;11:425–448. doi: 10.1118/1.595535. [DOI] [PubMed] [Google Scholar]
- Boyd A., Golding J., Macleod J., Lawlor D.a., Fraser A., Henderson J., Molloy L., Ness A., Ring S., Smith G.D. Cohort profile: the “children of the 90s”-the index offspring of the Avon longitudinal study of parents and children. Int. J. Epidemiol. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan R.W., Francis A., Arango C., Miller K., Lefkowitz D.M., McMahon R.P., Barta P.E., Pearlson G.D. Morphometric assessment of the heteromodal association cortex in schizophrenia. Am. J. Psychiatry. 2004;161:322–331. doi: 10.1176/appi.ajp.161.2.322. [DOI] [PubMed] [Google Scholar]
- Buck S.F. A method of estimation of missing values in multivariate data suitable for use with an electronic computer. J. R. Stat. Soc. Ser. B. 1960;22:302–306. [Google Scholar]
- Byrne M., Agerbo E., Eaton W.W., Mortensen P.B. Parental socio-economic status and risk of first admission with schizophrenia - a Danish national register based study. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39:87–96. doi: 10.1007/s00127-004-0715-y. [DOI] [PubMed] [Google Scholar]
- Cannon T.D., Chung Y., He G., Sun D., Jacobson A., van Erp T.G.M., McEwen S., Addington J., Bearden C.E., Cadenhead K., Cornblatt B., Mathalon D.H., McGlashan T., Perkins D., Jeffries C., Seidman L.J., Tsuang M., Walker E., Woods S.W., Heinssen R. Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biol. Psychiatry. 2014;77:147–157. doi: 10.1016/j.biopsych.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon T.D., Chung Y., He G., Sun D., Jacobson A., Van Erp T.G.M., McEwen S., Addington J., Bearden C.E., Cadenhead K., Cornblatt B., Mathalon D.H., McGlashan T., Perkins D., Jeffries C., Seidman L.J., Tsuang M., Walker E., Woods S.W., Heinssen R. Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biol. Psychiatry. 2015;77:147–157. doi: 10.1016/j.biopsych.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers J.S., Perrone-Bizzozero N.I. Altered myelination of the hippocampal formation in subjects with schizophrenia and bipolar disorder. Neurochem. Res. 2004;29:2293–2302. doi: 10.1007/s11064-004-7039-x. [DOI] [PubMed] [Google Scholar]
- Cropley V.L., Lin A., Nelson B., Reniers R.L.E.P., Yung A.R., Bartholomeusz C.F., Klauser P., Velakoulis D., McGorry P., Wood S.J., Pantelis C. Baseline grey matter volume of non-transitioned “ultra high risk” for psychosis individuals with and without attenuated psychotic symptoms at long-term follow-up. Schizophr. Res. 2016;173:152–158. doi: 10.1016/j.schres.2015.05.014. [DOI] [PubMed] [Google Scholar]
- Dalman C., Thomas H.V., David A.S., Gentz J., Lewis G., Allebeck P. Signs of asphyxia at birth and risk of schizophrenia. Population-based case-control study. Br. J. Psychiatry. 2001;179:403–408. doi: 10.1192/bjp.179.5.403. [DOI] [PubMed] [Google Scholar]
- David A.S., Malmberg A., Brandt L., Alleback P., Lewis G. IQ and risk for schizophrenia: a population-based cohort study. Psychol. Med. 1997;27:1311–1323. doi: 10.1017/s0033291797005680. [DOI] [PubMed] [Google Scholar]
- Deoni S.C.L. High-resolution T1 mapping of the brain at 3T with driven equilibrium single pulse observation of T1 with high-speed incorporation of RF field inhomogeneities (DESPOT1-HIFI) J. Magn. Reson. Imaging. 2007;26:1106–1111. doi: 10.1002/jmri.21130. [DOI] [PubMed] [Google Scholar]
- Deoni S.C.L., Rutt B.K., Arun T., Pierpaoli C., Jones D.K. Gleaning multicomponent T1 and T2 information from steady-state imaging data. Magn. Reson. Med. 2008;60:1372–1387. doi: 10.1002/mrm.21704. [DOI] [PubMed] [Google Scholar]
- Deoni S.C.L., Dean D.C., Remer J., Dirks H., O'Muircheartaigh J. Cortical maturation and myelination in healthy toddlers and young children. NeuroImage. 2015;115:47–161. doi: 10.1016/j.neuroimage.2015.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinse J., Härtwich N., Waehnert M.D., Tardif C.L., Schäfer A., Geyer S., Preim B., Turner R., Bazin P.-L. A cytoarchitecture-driven myelin model reveals area-specific signatures in human primary and secondary areas using ultra-high resolution in-vivo brain MRI. NeuroImage. 2015;114:71–87. doi: 10.1016/j.neuroimage.2015.04.023. [DOI] [PubMed] [Google Scholar]
- Douaud G., Smith S., Jenkinson M., Behrens T., Johansen-Berg H., Vickers J., James S., Voets N., Watkins K., Matthews P.M., James A. Anatomically related grey and white matter abnormalities in adolescent-onset schizophrenia. Brain. 2007;130:2375–2386. doi: 10.1093/brain/awm184. [DOI] [PubMed] [Google Scholar]
- Drakesmith M., Caeyenberghs K., Dutt A., Zammit S., Evans C.J., Reichenberg A., Lewis G., David A.S., Jones D.K. Schizophrenia-like topological changes in the structural connectome of individuals with subclinical psychotic experiences. Hum. Brain Mapp. 2015;36:2629–2643. doi: 10.1002/hbm.22796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drakesmith M., Dutt A., Fonville L., Zammit S., Reichenberg A., Evans C.J., Lewis G., Jones D.K., David A.S. Mediation of developmental risk factors for psychosis by white matter microstructure in young adults with psychotic experiences. JAMA Psychiatry. 2016;73:1–11. doi: 10.1001/jamapsychiatry.2015.3375. [DOI] [PubMed] [Google Scholar]
- Ellison-Wright I., Glahn D.C., Laird A.R., Thelen S.M., Bullmore E. The anatomy of first-episode and chronic schizophrenia: an anatomical likelihood estimation meta-analysis. Am. J. Psychiatry. 2008;165:1015–1023. doi: 10.1176/appi.ajp.2008.07101562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esiri M., Crow T. Psychiatric disease. In: Love S., Louis D., Ellison D.W., editors. vol. 1. Hodder Arnold; 2008. pp. 1153–1196. (Greenfield's Neuropathology). [Google Scholar]
- Foerster A., Lewis S.W., Owen M.J., Murray R.M. Low birth weight and a family history of schizophrenia predict poor premorbid functioning in psychosis. Schizophr. Res. 1991;5:13–20. doi: 10.1016/0920-9964(91)90049-w. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Borgwardt S., Crescini A., Deste G., Kempton M.J., Lawrie S., McGuire P., Sacchetti E. Neuroanatomy of vulnerability to psychosis: a voxel-based meta-analysis. Neurosci. Biobehav. Rev. 2011;35:1175–1185. doi: 10.1016/j.neubiorev.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Borgwardt S., Bechdolf A., Addington J., Riecher-Rössler A., Schultze-Lutter F., Keshavan M., Wood S., Ruhrmann S., Seidman L.J., Valmaggia L., Cannon T., Velthorst E., De Haan L., Cornblatt B., Bonoldi I., Birchwood M., McGlashan T., Carpenter W., McGorry P., Klosterkötter J., McGuire P., Yung A. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA psychiatry. 2013;70:107–120. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher B.J., Jones B.J., Pardes M. Stressful life events, social class and symptoms of schizophrenia. Clin. Schizophr. Relat. Psychoses. 2013:1–25. [PubMed] [Google Scholar]
- Gelman N., Ewing J.R., Gorell J.M., Spickler E.M., Solomon E.G. Interregional variation of longitudinal relaxation rates in human brain at 3.0 T: relation to estimated iron and water contents. Magn. Reson. Med. 2001;45:71–79. doi: 10.1002/1522-2594(200101)45:1<71::aid-mrm1011>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Gilmore J.H., Shi F., Woolson S.L., Knickmeyer R.C., Short S.J., Lin W., Zhu H., Hamer R.M., Styner M., Shen D. Longitudinal development of cortical and subcortical gray matter from birth to 2 years. Cereb. Cortex. 2012;22:2478–2485. doi: 10.1093/cercor/bhr327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding J., Pembrey M., Jonesa R., The ALSPAC Study Team ALSPAC-the Avon longitudinal study of parents and children. Paediatr. Perinat. Epidemiol. 2001;15:74–87. doi: 10.1046/j.1365-3016.2001.00325.x. [DOI] [PubMed] [Google Scholar]
- Golombok S., Rust J. The UK revision. In: Wechsler D., editor. The Manual of the Wechsler Intelligence Scale for Children - 3rd Revision. The Psychological Corporation; London: 1992. [Google Scholar]
- Good C.D., Johnsrude I.S., Ashburner J., Henson R.N., Friston K.J., Frackowiak R.S. A voxel-based morphometric study of ageing in 465 normal adult human brains. NeuroImage. 2001;14:21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- Goodman R., Ford T., Richards H., Gatward R., Meltzer H. The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J. Child Psychol. Psychiatry. 2000;41:645–655. [PubMed] [Google Scholar]
- Hakak Y., Walker J.R., Li C., Wong W.H., Davis K.L., Buxbaum J.D., Haroutunian V., Fienberg A.A. Genome-wide expression analysis reveals dysregulation of myelination-related genes in chronic schizophrenia. Proc. Natl. Acad. Sci. 2001;98:4746–4751. doi: 10.1073/pnas.081071198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison P.J., Harrison P.J. The neuropathology of schizophrenia: a critical review of the data and their interpretation. Brain. 1999;122:593–624. doi: 10.1093/brain/122.4.593. [DOI] [PubMed] [Google Scholar]
- Hof P.R., Haroutunian V., Copland C., Davis K.L., Buxbaum J.D. Molecular and cellular evidence for an oligodendrocyte abnormality in schizophrenia. Neurochem. Res. 2002;27:1193–1200. doi: 10.1023/a:1020981510759. [DOI] [PubMed] [Google Scholar]
- Hof P.R., Haroutunian V., Friedrich V.L., Byne W., Buitron C., Perl D.P., Davis K.L. Loss and altered spatial distribution of oligodendrocytes in the superior frontal gyrus in schizophrenia. Biol. Psychiatry. 2003;53:1075–1085. doi: 10.1016/s0006-3223(03)00237-3. [DOI] [PubMed] [Google Scholar]
- Homer J., Beevers M.S. Driven-equilibrium single-pulse observation of T1 relaxation. A reevaluation of a rapid “new” method for determining NMR spin-lattice relaxation times. J. Magn. Reson. 1985;63:287–297. [Google Scholar]
- Honea R., Crow T.J., Passingham D., Mackay C.E. Regional deficits in brain volume in schizophrenia: a meta-analysis of voxel-based morphometry studies. Am. J. Psychiatry. 2005;162:2233–2245. doi: 10.1176/appi.ajp.162.12.2233. [DOI] [PubMed] [Google Scholar]
- Honer W.G., Falkai P., Chen C., Arango V., Mann J.J., Dwork A.J. Synaptic and plasticity-associated proteins in anterior frontal cortex in severe mental illness. Neuroscience. 1999;91:1247–1255. doi: 10.1016/s0306-4522(98)00679-4. [DOI] [PubMed] [Google Scholar]
- Horwood J., Salvi G., Thomas K., Duffy L., Gunnell D., Hollis C., Lewis G., Menezes P., Thompson A., Wolke D., Zammit S., Harrison G. IQ and non-clinical psychotic symptoms in 12-year-olds: results from the ALSPAC birth cohort. Br. J. Psychiatry. 2008;193:185–191. doi: 10.1192/bjp.bp.108.051904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttenlocher P.R., Dabholkar A.S. Regional differences in synaptogenesis in human cerebral cortex. J. Comp. Neurol. 1997;387:167–178. doi: 10.1002/(sici)1096-9861(19971020)387:2<167::aid-cne1>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Jenkinson M., Beckmann C.F., Behrens T.E.J., Woolrich M.W., Smith S.M. FSL. NeuroImage. 2012;62:782–790. doi: 10.1016/j.neuroimage.2011.09.015. [DOI] [PubMed] [Google Scholar]
- Jones D.K., Simmons A., Williams S.C.R., Horsfield M.A. Non-invasive assessment of axonal fiber connectivity in the human brain via diffusion tensor MRI. Magn. Reson. Med. 1999;42:37–41. doi: 10.1002/(sici)1522-2594(199907)42:1<37::aid-mrm7>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Kanaan R.A.A., Kim J.-S., Kaufmann W.E., Pearlson G.D., Barker G.J., McGuire P.K. Diffusion tensor imaging in schizophrenia. Biol. Psychiatry. 2005;58:921–929. doi: 10.1016/j.biopsych.2005.05.015. [DOI] [PubMed] [Google Scholar]
- Kang X., Herron T.J., Turken A.U., Woods D.L. Diffusion properties of cortical and pericortical tissue: regional variations, reliability and methodological issues. Magn. Reson. Imaging. 2012;30:1111–1122. doi: 10.1016/j.mri.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Katsel P., Davis K.L., Haroutunian V. Variations in myelin and oligodendrocyte-related gene expression across multiple brain regions in schizophrenia: a gene ontology study. Schizophr. Res. 2005;79:157–173. doi: 10.1016/j.schres.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Kelly C. Cigarette smoking and schizophrenia. Adv. Psychiatr. Treat. 2000;6:327–331. [Google Scholar]
- Klein S., Staring M., Murphy K., Viergever M.A., Pluim J.P.W. Elastix: a toolbox for intensity-based medical image registration. IEEE Trans. Med. Imaging. 2010;29:196–205. doi: 10.1109/TMI.2009.2035616. [DOI] [PubMed] [Google Scholar]
- Koskinen J., Löhönen J., Koponen H., Isohanni M., Miettunen J. Prevalence of alcohol use disorders in schizophrenia—a systematic review and meta-analysis. Acta Psychiatr. Scand. 2009;120:85–96. doi: 10.1111/j.1600-0447.2009.01385.x. [DOI] [PubMed] [Google Scholar]
- Kraan T., Velthorst E., Smit F., de Haan L., van der Gaag M. Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophr. Res. 2015;161:143–149. doi: 10.1016/j.schres.2014.11.026. [DOI] [PubMed] [Google Scholar]
- Leemans A., Jones D.K. The B-matrix must be rotated when correcting for subject motion in DTI data. Magn. Reson. Med. 2009;61:1336–1349. doi: 10.1002/mrm.21890. [DOI] [PubMed] [Google Scholar]
- Leemans A., Jeurissen B., Sijbers J., Jones D.K. ExploreDTI: a graphical toolbox for processing, analyzing, and visualizing diffusion MR data; Proceedings of the International Society for Magnetic Resonance in Medicine. Honolulu, Hawai'i, USA; 2009. p. 3537. [Google Scholar]
- Lewis G. Asphyxia at birth and schizophrenia. Br. J. Psychiatry. 2002;180:465. doi: 10.1192/bjp.180.5.465. [DOI] [PubMed] [Google Scholar]
- Lewis G., Pelosi A.J., Araya R., Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol. Med. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- Lutti A., Dick F., Sereno M.I., Weiskopf N. Using high-resolution quantitative mapping of R1 as an index of cortical myelination. NeuroImage. 2013;93:176–188. doi: 10.1016/j.neuroimage.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Lutti A., Dick F., Sereno M.I., Weiskopf N. Using high-resolution quantitative mapping of R1 as an index of cortical myelination. NeuroImage. 2014;93(Pt 2):176–188. doi: 10.1016/j.neuroimage.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Mechelli A., Riecher-Rössler A., Meisenzahl E.M., Tognin S., Wood S.J., Borgwardt S.J., Koutsouleris N., Yung A.R., Stone J.M., Phillips L.J., McGorry P.D., Valli I., Velakoulis D., Woolley J., Pantelis C., McGuire P. Neuroanatomical abnormalities that predate the onset of psychosis: a multicenter study. Arch. Gen. Psychiatry. 2011;68:489–495. doi: 10.1001/archgenpsychiatry.2011.42. [DOI] [PubMed] [Google Scholar]
- Meisenzahl E.M., Koutsouleris N., Bottlender R., Scheuerecker J., Jäger M., Teipel S.J., Holzinger S., Frodl T., Preuss U., Schmitt G., Burgermeister B., Reiser M., Born C., Möller H.-J. Structural brain alterations at different stages of schizophrenia: a voxel-based morphometric study. Schizophr. Res. 2008;104:44–60. doi: 10.1016/j.schres.2008.06.023. [DOI] [PubMed] [Google Scholar]
- Moore T.H.M., Zammit S., Lingford-Hughes A., Barnes T.R.E., Jones P.B., Burke M., Lewis G. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Morgan C., Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr. Bull. 2007;33:3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz Maniega S., Bastin M.E., Armitage P.A., Farrall A.J., Carpenter T.K., Hand P.J., Cvoro V., Rivers C.S., Wardlaw J.M. Temporal evolution of water diffusion parameters is different in grey and white matter in human ischaemic stroke. J. Neurol. Neurosurg. Psychiatry. 2004;75:1714–1718. doi: 10.1136/jnnp.2003.033852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najjar S., Pearlman D.M. Neuroinflammation and white matter pathology in schizophrenia: systematic review. Schizophr. Res. 2014;161:102–112. doi: 10.1016/j.schres.2014.04.041. [DOI] [PubMed] [Google Scholar]
- Nichols T.E., Holmes A.P. Nonparametric permutation tests for functional neuroimaging: a primer with examples. Hum. Brain Mapp. 2002;15:1–25. doi: 10.1002/hbm.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman R.M., Malla A.K. Stressful life events and schizophrenia. I: A review of the research. Br. J. Psychiatry. 1993;162:161–166. doi: 10.1192/bjp.162.2.161. [DOI] [PubMed] [Google Scholar]
- O'Donoghue B., Fanning F., Lyne J., Renwick L., Madigan K., Kinsella A., Lane A., Turner N., O'Callaghan E., Clarke M. Int. J. Soc; Psychiatry: 2015. Social Class at Birth and Risk of Psychosis. [DOI] [PubMed] [Google Scholar]
- Office of Population Censuses and Surveys . OPCS Omnibus Survey, September 1991. 1991. Social Survey Division. (1996). UK Data Service. SN: 3080. [Google Scholar]
- Oreja-Guevara C., Rovaris M., Iannucci G., Valsasina P., Caputo D., Cavarretta R., Sormani M.P., Ferrante P., Comi G., Filippi M. Progressive gray matter damage in patients with relapsing–remitting multiple sclerosis: a longitudinal diffusion tensor magnetic resonance imaging study. Arch. Neurol. 2005;62:578–584. doi: 10.1001/archneur.62.4.578. [DOI] [PubMed] [Google Scholar]
- Pantelis C., Velakoulis D., McGorry P.D., Wood S.J., Suckling J., Phillips L.J., Yung A.R., Bullmore E.T., Brewer W., Soulsby B., Desmond P., McGuire P.K. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet (London, England) 2003;361:281–288. doi: 10.1016/S0140-6736(03)12323-9. [DOI] [PubMed] [Google Scholar]
- Park J.Y., Park H.-J., Kim D.-J., Kim J.-J. Positive symptoms and water diffusivity of the prefrontal and temporal cortices in schizophrenia patients: a pilot study. Psychiatry Res. Neuroimaging. 2014;224:49–57. doi: 10.1016/j.pscychresns.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Pasternak O., Sochen N., Gur Y., Intrator N., Assaf Y. Free water elimination and mapping from diffusion MRI. Magn. Reson. Med. 2009;62:717–730. doi: 10.1002/mrm.22055. [DOI] [PubMed] [Google Scholar]
- Paus T., Keshavan M., Giedd J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008;9:947–957. doi: 10.1038/nrn2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifkin L., Lewis S., Jones P., Toone B., Murray R. Low birth weight and schizophrenia. Br. J. Psychiatry. 1994;165:357–362. doi: 10.1192/bjp.165.3.357. [DOI] [PubMed] [Google Scholar]
- Rooney W.D., Johnson G., Li X., Cohen E.R., Kim S.-G., Ugurbil K., Springer C.S. Magnetic field and tissue dependencies of human brain longitudinal1H2O relaxation in vivo. Magn. Reson. Med. 2007;57:308–318. doi: 10.1002/mrm.21122. [DOI] [PubMed] [Google Scholar]
- Roussos P., Haroutunian V. Schizophrenia: susceptibility genes and oligodendroglial and myelin related abnormalities. Front. Cell. Neurosci. 2014;8:5. doi: 10.3389/fncel.2014.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovaris M., Judica E., Gallo A., Benedetti B., Sormani M.P., Caputo D., Ghezzi A., Montanari E., Bertolotto A., Mancardi G., Bergamaschi R., Martinelli V., Comi G., Filippi M. Grey matter damage predicts the evolution of primary progressive multiple sclerosis at 5 years. Brain. 2006;129:2628–2634. doi: 10.1093/brain/awl222. [DOI] [PubMed] [Google Scholar]
- Satterthwaite T.D., Wolf D.H., Calkins M.E., Vandekar S.N., Erus G., Ruparel K., Roalf D.R., Linn K.A., Elliott M.A., Moore T.M., Hakonarson H., Shinohara R.T., Davatzikos C., Gur R.C., Gur R.E. Structural brain abnormalities in youth with psychosis spectrum symptoms. JAMA Psychiatry. 2016;73:515–524. doi: 10.1001/jamapsychiatry.2015.3463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon A.E., Velthorst E., Nieman D.H., Linszen D., Umbricht D., de Haan L. Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophr. Res. 2011;132:8–17. doi: 10.1016/j.schres.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Smieskova R., Fusar-Poli P., Allen P., Bendfeldt K., Stieglitz R.D., Drewe J., Radue E.W., McGuire P.K., Riecher-Rössler A., Borgwardt S.J. Neuroimaging predictors of transition to psychosis—a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2010;34:1207–1222. doi: 10.1016/j.neubiorev.2010.01.016. [DOI] [PubMed] [Google Scholar]
- Smith S.M. Fast robust automated brain extraction. Hum. Brain Mapp. 2002;17:143–155. doi: 10.1002/hbm.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.M., Nichols T.E. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage. 2009;44:83–98. doi: 10.1016/j.neuroimage.2008.03.061. [DOI] [PubMed] [Google Scholar]
- Sowell E.R., Peterson B.S., Thompson P.M., Welcome S.E., Henkenius A.L., Toga A.W. Mapping cortical change across the human life span. Nat. Neurosci. 2003;6:309–315. doi: 10.1038/nn1008. [DOI] [PubMed] [Google Scholar]
- Uranova N.a., Vostrikov V.M., Orlovskaya D.D., Rachmanova V.I. Oligodendroglial density in the prefrontal cortex in schizophrenia and mood disorders: a study from the Stanley neuropathology consortium. Schizophr. Res. 2004;67:269–275. doi: 10.1016/S0920-9964(03)00181-6. [DOI] [PubMed] [Google Scholar]
- Haijma S.V., Van Haren N., Cahn W., Koolschijn P.C.M.P., Hulshoff Pol H.E., Kahn R.S. Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr. Bull. 2013;39:1129–1138. doi: 10.1093/schbul/sbs118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velakoulis D., Wood S.J., Wong M.T.H., McGorry P.D., Yung A., Phillips L., Smith D., Brewer W., Proffitt T., Desmond P., Pantelis C. Hippocampal and amygdala volumes according to psychosis stage and diagnosis. Arch. Gen. Psychiatry. 2006;63:139. doi: 10.1001/archpsyc.63.2.139. [DOI] [PubMed] [Google Scholar]
- Vita A., De Peri L., Silenzi C., Dieci M. Brain morphology in first-episode schizophrenia: a meta-analysis of quantitative magnetic resonance imaging studies. Schizophr. Res. 2006;82:75–88. doi: 10.1016/j.schres.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Vita A., De Peri L., Deste G., Sacchetti E. Progressive loss of cortical gray matter in schizophrenia: a meta-analysis and meta-regression of longitudinal MRI studies. Transl. Psychiatry. 2012;2 doi: 10.1038/tp.2012.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vite C.H., Magnitsky S., Aleman D., O'Donnell P., Cullen K., Ding W., Pickup S., Wolfe J.H., Poptani H. Apparent diffusion coefficient reveals gray and white matter disease, and T2 mapping detects white matter disease in the brain in feline alpha-mannosidosis. AJNR Am. J. Neuroradiol. 2008;29:308–313. doi: 10.3174/ajnr.A0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiskopf N., Mohammadi S., Lutti A., Callaghan M.F. Advances in MRI-based computational neuroanatomy. Curr. Opin. Neurol. 2015;28:313–322. doi: 10.1097/WCO.0000000000000222. [DOI] [PubMed] [Google Scholar]
- Werner S., Malaspina D., Rabinowitz J. Socioeconomic status at birth is associated with risk of schizophrenia: population-based multilevel study. Schizophr. Bull. 2007;33:1373–1378. doi: 10.1093/schbul/sbm032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing J.K., Babor T., Brugha T., Burke J., Cooper J.E., Giel R., Jablenski A., Regier D., Sartorius N. SCAN. Schedules for clinical assessment in neuropsychiatry. Arch. Gen. Psychiatry. 1990;47:589–593. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
- Woodberry K.A., Giuliano A.J., Seidman L.J. Premorbid IQ in schizophrenia: a meta-analytic review. Am. J. Psychiatry. 2008;165:579–587. doi: 10.1176/appi.ajp.2008.07081242. [DOI] [PubMed] [Google Scholar]
- Wright I.C., Rabe-Hesketh S., Woodruff P.W., David A.S., Murray R.M., Bullmore E.T. Meta-analysis of regional brain volumes in schizophrenia. Am. J. Psychiatry. 2000;157:16–25. doi: 10.1176/ajp.157.1.16. [DOI] [PubMed] [Google Scholar]
- Wu M., Chang L.C., Walker L., Lemaitre H., Barnett A.S., Marenco S., Pierpaoli C. Comparison of EPI distortion correction methods in diffusion tensor MRI using a novel framework. Med. Image Comput. Comput. Interv. 2008;2008(11):321–329. doi: 10.1007/978-3-540-85990-1_39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit S., Allebeck P., David A.S., Dalman C., Hemmingsson T., Lundberg I., Lewis G. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch. Gen. Psychiatry. 2004;61:354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- Zammit S., Horwood J., Thompson A., Thomas K., Menezes P., Gunnell D., Hollis C., Wolke D., Lewis G., Harrison G. Investigating if psychosis-like symptoms (PLIKS) are associated with family history of schizophrenia or paternal age in the ALSPAC birth cohort. Schizophr. Res. 2008;104:279–286. doi: 10.1016/j.schres.2008.04.036. [DOI] [PubMed] [Google Scholar]
- Zammit S., Kounali D., Cannon M., David A.S., Gunnell D., Heron J., Jones P.B., Lewis S., Sullivan S., Wolke D., Lewis G. Psychotic experiences and psychotic disorders at age 18 in relation to psychotic experiences at age 12 in a longitudinal population-based cohort study. Am. J. Psychiatry. 2013;170:742–750. doi: 10.1176/appi.ajp.2013.12060768. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Brady M., Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans. Med. Imaging. 2001;20:45–57. doi: 10.1109/42.906424. [DOI] [PubMed] [Google Scholar]
- Ziermans T.B., Durston S., Sprong M., Nederveen H., van Haren N.E.M., Schnack H.G., Lahuis B.E., Schothorst P.F., van Engeland H. No evidence for structural brain changes in young adolescents at ultra high risk for psychosis. Schizophr. Res. 2009;112:1–6. doi: 10.1016/j.schres.2009.04.013. [DOI] [PubMed] [Google Scholar]
- Ziermans T.B., Schothorst P.F., Schnack H.G., Koolschijn P.C.M.P., Kahn R.S., Van Engeland H., Durston S. Progressive structural brain changes during development of psychosis. Schizophr. Bull. 2012;38:519–530. doi: 10.1093/schbul/sbq113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.