Abstract
Context
Skin cancer is a preventable and commonly diagnosed cancer in the U.S. Excessive ultraviolet radiation exposure is a known cause of skin cancer. This article presents updated results of two types of interventions evaluated in a previously published Community Guide systematic review: multicomponent community-wide (MCCW) interventions and mass media (MM) interventions when used alone.
Evidence acquisition
Studies assessing MCCW and MM interventions to prevent skin cancer by reducing ultraviolet radiation exposure were evaluated using Community Guide systematic review methods. Relevant studies published between 1966 and 2013 were included and analyzed for this review.
Evidence synthesis
Seven studies evaluating the effectiveness of MCCW interventions showed a median increase in sunscreen use of 10.8 percentage points (interquartile interval=7.3, 23.2); a small decrease in ultraviolet radiation exposure; a decrease in indoor tanning device use of 4.0 percentage points (95% CI=2.5, 5.5); and mixed results for other protective behaviors. Four studies evaluating the effectiveness of MM interventions found that they generally led to improved ultraviolet protection behaviors among children and adults.
Conclusions
The available evidence showed that MCCW interventions are effective in reducing ultraviolet radiation exposure by increasing sunscreen use. There was, however, insufficient evidence to determine the effectiveness of MM interventions alone in reducing ultraviolet radiation exposure, indicating a continuing need for more research in this field to improve assessment of effectiveness.
Context
In the Call to Action to Prevent Skin Cancer, the U.S. Surgeon General identified skin cancer as a serious public health concern.1 Each year, nearly 5 million U.S. adults are treated for skin cancer at an annual cost of $8.1 billion.2 The three most common types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma.3 Melanoma accounts for most skin cancer deaths and is the fifth and sixth most common cancer in white men and white women, respectively.4 Of the estimated $8.1 billion associated with skin cancer treatment in the U.S., $4.8 billion is attributable to the treatment of BCC and SCC, with $3.3 billion for melanoma.5 Although skin cancer incidence rates have continued to rise among Americans in recent years, most cases are preventable.6–9
Ultraviolet radiation (UVR) exposure from the sun and/or from indoor tanning devices is considered a major contributing factor and the most preventable risk factor for developing skin cancer. Genetic risk factors for skin cancer include having fair skin; blue or green eyes; blond or red hair10–12; a high prevalence of benign pigmented nevi (moles)13,14; and a personal or family history of skin cancer.15 Excessive exposure of skin to UVR often results in suntan or sunburn, with changes in skin coloration proportional to the intensity of sun exposure and severity of damage to skin cells.16 Environmental factors affecting the intensity of UVR that an individual receives include latitude, time of day, season, altitude, and temperature.17,18
To minimize the harmful effects of UVR exposure, agencies including CDC and the International Agency for Research on Cancer promote effective UVR protection, including seeking shade, especially during midday hours; wearing a hat with a wide brim to shade the face, head, ears, and neck; wearing clothing to protect exposed skin; wearing protective sunglasses; using sunscreen with sun protective factor (SPF) 15 or higher and both UVA and UVB (broad spectrum) protection; and avoiding indoor tanning.19–21 National surveillance data indicate that use of UVR protection remains low in the U.S., and sunburn and indoor tanning remain common among certain groups.22–25
In 2000, the Community Guide conducted several systematic reviews on the effectiveness of community-based interventions to prevent skin cancer.22 To reflect the most recent evidence, this article reports on updates of two interventions included in those systematic reviews: multicomponent community-wide interventions (MCCW) and mass media interventions (MM) when used alone.
Evidence Acquisition
The Community Guide systematic review process has been described in detail elsewhere.26,27 In brief, the process includes forming a coordination team (the team) of systematic review scientists and research fellows from CDC’s Community Guide Branch, who collaborate with subject matter experts and consultants on skin cancer prevention from CDC and other agencies, organizations, and academic institutions, with oversight from the Community Preventive Services Task Force (Task Force).
Definitions
Mass media (MM) interventions to prevent skin cancer by reducing exposure to UVR use communication channels such as print media (e.g., newspapers, magazines), broadcast media (e.g., radio, TV), billboards, or the Internet to disseminate information, behavioral guidance, or a combination of these. Messages may target specific audiences, although, typically, interventions rely on broad distribution channels. Some interventions provide up-to-date information about the intensity of the sun’s rays (UV index), with the goal of raising awareness and prompting UVR protection measures. Others use techniques that provide information on the dangers of UVR exposure to promote change in knowledge, attitudes, beliefs, intentions, and UVR protective behaviors.
Included interventions could also incorporate small media (e.g., brochures, fliers, newsletters) or promotional products to increase awareness of campaign messages in addition to mass media.
Since 2000, when the original Community Guide reviews were conducted, technological advances have spawned new approaches to disseminating information to the public through media, particularly the Internet and social media. Therefore, for this update, studies using new media (i.e., Internet and social media) were also included, as long as the messages were distributed to a large audience and were received passively.
Multicomponent community-wide (MCCW) interventions to prevent skin cancer combine individually directed strategies (e.g., educational), MM campaigns (see definition above), and environmental and policy changes (e.g., creating shade areas, distributing sunscreen, using school-based policies to restrict outdoor activities during peak UVR hours) in multiple settings within a defined geographic area (i.e., city, state, province, or country) in an integrated effort to influence UVR protective behaviors. They are usually delivered with a defined theme, name, logo, and set of messages. Programs vary substantially, however, in duration (e.g., months to years) and number of components/strategies used.
Conceptual Approach and Analytic Framework
The team developed analytic frameworks to describe the overall conceptual approach to preventing skin cancer by reducing UVR exposure. Figure 1 shows the relationship of MCCW and MM interventions to the relevant intermediate outcomes (e.g., knowledge, attitudes, and intentions), key UVR protective behaviors to decrease excessive UVR exposure (e.g., increased use of sunscreen, protective clothing, hats, sunglasses, seeking shade; avoidance of indoor tanning), selected health outcomes (e.g., sunburn), and, ultimately, skin cancer prevention.
Figure 1.
Analytic framework for mass media and multicomponent community-wide interventions.
UVR, ultraviolet radiation
MCCW interventions may include different combinations of the individually directed, environmental and policy, and MM components, whereas MM interventions used only mass media channels. All of these components may influence UVR protection and exposure by changing knowledge, attitudes, and social norms. In addition, environmental or policy components can lead more directly to changes in UVR protection. The analytic framework also addresses the possibility of harms such as vitamin D deficiency and a decrease in physical activity because of decreased outdoor activity.
Inclusion and Exclusion Criteria
The inclusion criteria for this review were adapted from the prior review, with minor revisions. In the prior review, although factors like sunscreen use (by itself) and exposure to indoor UVR (e.g., indoor tanning) were assumed to be associated with preventing skin cancer, they were not considered proxies for health outcomes. However, increased sunscreen use was considered part of the composite UVR protective behaviors in many included programs. Recent evidence has supported the association of sunscreen use and avoidance of indoor tanning devices with reduced development of skin cancer.19,28,29 Therefore, based on the recent evidence, these UVR protective behaviors—sunscreen use and avoidance of indoor tanning devices—were added to the outcomes of interest for these updated reviews.
To qualify for inclusion in these reviews, a study had to:
evaluate an intervention meeting the definition of either MCCW or MM alone interventions;
be primary research and published in an English-language journal, or available as a dissertation or technical or government report;
include a concurrent comparison group or have an interrupted time-series design with at least two measurements before and after the intervention or uncontrolled before-and-after study design with measurements before and after the intervention implementation;
be conducted in a country with a high-income economy30; and
evaluate the effectiveness of MCCW or MM interventions on at least one of the primary outcomes of interest (i.e., the health outcomes or behavioral proxies listed below).
In addition, to be included in the MCCW review, a study had to include an intervention that:
was multicomponent, that is, included a combination of at least two distinct components (e.g., educational, environmental, policy, or MM); and
was implemented in two or more different settings (e.g., schools, outdoor recreation areas, daycare centers) or was delivered to an entire community in a defined geographic area, such as a city, county, or school district.
Exclusion criteria
Studies that evaluated only the intermediate outcomes described in Figure 1 (e.g., changes in knowledge, attitudes, and social norms) were excluded.
Search for Evidence
For conducting these updated reviews, the evidence from the original review22 (search period 1966–2000) was combined with the new evidence published between June 2000 and April 2013. Potentially relevant studies were identified primarily through searches of three databases (Medline, CINAHL, and PsycINFO). Details of the search strategy are available at www.thecommunityguide.org/cancer/skin/supportingmaterials/SS-skincancer-2013.html. A broad search for skin cancer prevention studies identified a total of 11,106 citations; as indicated in Figure 2, four studies were included in the MM review and seven in the MCCW review.
Figure 2.
Search yield for evidence included in MM and MCCW interventions.
Note: As per update methods, the original 1966–2000 search for evidence was not repeated. MCCW, multicomponent community-wide; MM, mass media.
Assessing and Summarizing the Evidence
Abstraction and evaluation of studies
Each study that met the inclusion criteria was abstracted by two independent reviewers using the standard Community Guide abstraction process.27 Disagreements between reviewers were resolved by consensus. Community Guide methods were used to assess each study for internal and external validity (for details see Appendix A, available online).26 Information about suitability of study design, quality of execution, sampling, comparison groups, effect modifiers, and outcomes was assessed according to the standard methodology of The Community Guide (www.thecommunityguide.org/methods/abstractionform.pdf).
Primary outcomes of interest
Several categories of outcome measures were abstracted and summarized for this review, including adoption of UVR protective behaviors, UVR exposure, and health outcomes (i.e., incidence of sunburn and skin cancer).
-
UVR protective behaviors: Typically measured by self-reported or observed use of sunscreen, hat, protective clothing, sunglasses, shade, and by limiting time spent in the sun during peak UVR hours (10 AM to 4 PM daylight savings or 9 AM to 3 PM standard time). Other UVR protective behaviors include decrease in use of indoor tanning devices which is typically measured by proportion of individuals using tanning devices (e.g., tanning beds, lamps) or total number of tanning sessions.
A combined sun protective score is commonly measured by combining effect estimates for multiple UVR protective behaviors.
UVR exposure: UVR exposure can be assessed by change in levels of skin coloration (e.g., measured with a colorimeter or spectrophotometer) associated with UVR from sun rays or tanning devices.
Sunburn incidence: Sunburn is a marker for both sun sensitivity and intermittent sun exposure.20–22 The definition of sunburn varies across studies, ranging from the presence of any sunburn to sunburns that are painful and/or blistering. Incidence of sunburn is generally measured as number of sunburns in a specified time period.
Incidence of skin cancer: Measured by the number of new skin cancer cases.
In addition, the reviews examined which factors contributed to intervention effectiveness: (1) type of setting (e.g., schools, recreation areas); (2) population characteristics (e.g., gender, age, skin type); (3) intervention characteristics, such as scope (e.g., national, state, or local) or intensity (e.g., reach, duration, number of components); or (4) different combinations of these factors.
Summarizing Evidence
To evaluate the effectiveness of these interventions, the effect estimates were expressed as absolute percentage point change and difference-in-differences of the mean change of combined evidence when possible. (Formulas used to calculate effect sizes are provided in Appendix B, available online.)
Evidence Synthesis
Multicomponent Community-wide Interventions
Intervention effectiveness
For the updated review, three studies31–33 from the new literature search period (June 2000–April 2013) and four studies34–37 from the original review (search period 1966–2000) qualified for inclusion in the analysis. Thus, evidence is based on seven studies31–37 that evaluated intervention effects on multiple UVR protective behaviors (Figure 2). All included studies in the updated review had fair quality of execution; two studies were RCTs32,34 and five were before-and-after studies.31,33,35–37
Most interventions31,32,34–37 in this review were conducted in the 1980s and 1990s, mostly in communities with a balanced mix of settings and directed at a variety of populations (e.g., children, youth, general population). All but one of the interventions (assessed in two included studies) used a mass media component as a part of the multicomponent program32,34; most also included components implemented in specific community settings, most commonly schools, outdoor recreation areas, and child care centers. The evidence came primarily from outside the U.S., one study from United Kingdom33 and three studies from Australia31,36,37 (Appendix C Table 1, available online).
All included studies reported evidence31–37 on protective behavior changes and two31,35 assessed changes in sunburn incidence. None assessed effectiveness of the intervention for decrease in skin coloration and skin cancer incidence.
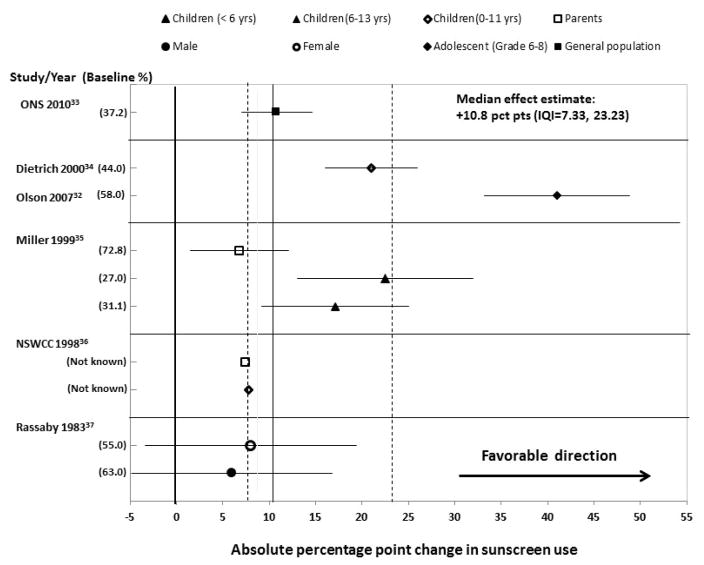
All seven studies indicated an increase in sunscreen use associated with the intervention. Six studies with results that could be expressed in the same metric showed a median increase of 10.8 percentage points (pct pts) (interquartile interval=7.3, 23.2) in sunscreen use after the intervention implementation (Figure 3).32–37 The seventh study31 demonstrated long-term improvements in the three sun protective behaviors assessed (i.e., use of hat and sunscreen, wearing of long-sleeved clothing) after implementation of the SunSmart program in Victoria, Australia.
Figure 3.
Changes in sunscreen use attributable to MCCW interventions.
IQI, interquartile interval; MCCW, multicomponent community-wide; MM, mass media.
For other protective behaviors assessed—seeking shade, wearing hats, and use of protective clothing—results were mixed, with several small or negative effect estimates (Appendix C Figure 1, available online). Three studies31,33,35 showed a small decrease in efforts to limit UVR exposure; two studies33,35 found a decrease in the proportion of individuals either sunbathing or spending time in the sun during peak hours (2.1 and 2.8 pct pts, respectively) ; and one study33 reported a 4.0 pct pt (95% CI=2.5, 5.5) decrease in tanning bed use. Similarly, two studies31,35 indicated a decrease in sunburns (Appendix C Figure 2, available online): One study35 showed decreases in sunburn incidence of 15.4 pct pts (95% CI= −21.2, −9.6) among children aged <6 years and 6.8 pct pts (95% CI= −14.8, −1.2) among 6–13-year-olds. The other found a reduction of 5 pct pts over a 14-year period.31
Applicability of findings
Although most evidence for the review came from outside the U.S., the findings are likely applicable to the U.S. context because results were similar across countries. All interventions were relatively intensive campaigns designed to reach a substantial proportion of the target population, for an extended period, in multiple contexts. All programs lasted at least 1 year, and one has been ongoing for decades.31 It is unclear whether less extensive interventions would achieve similar results.
Although favorable effects were observed across all age groups, children showed relatively larger increases in sunscreen use. Limited information was available about effectiveness among different demographic groups. Among different racial and ethnic groups, and among people of different skin sensitivities, there may be important differences in the effectiveness of such interventions for changing UVR protective behavior, and in the effects of such behavior changes on skin cancer risk.
Conclusions for MCCW Interventions
According to Community Guide rules,26 this updated review found sufficient evidence that MCCW interventions are effective in increasing sunscreen use. Available evidence indicates mixed results for other protective behaviors, such as wearing protective clothing and hats, seeking shade, and limiting outdoor activities during peak UVR hours. Some evidence also indicated benefits in reducing sunburns.
Mass Media (MM) Interventions Alone
Intervention effectiveness
The effectiveness of the intervention is based on the combined evidence published between 1966 and April 2013. A total of four studies24,31,38,39 was included in this review.
Of these studies, one31 used a time series study design and the remainder used a before-and-after study design24,38,39; one study31 had good quality of execution and three studies24,38,39 had fair quality. Two studies24,31 were conducted in Australia, one38 in the U.S., and one39 in Denmark (Appendix C Table 2, available online).
All included studies24,31,38,39 reported evidence on behavior change among adults; none assessed sunburn or skin cancer outcomes. Results from two studies24,38 using similar effect metrics showed mixed findings for UVR protective behaviors among children and adults (e.g., sunscreen use; Figure 4) and other protective behaviors including clothing, hats, and shade (Appendix C Figures 3 and 4, available online).
Figure 4.

Changes in sunscreen use attributable to MM interventions.
MM, mass media.
The third study31 found that the degree of audience exposure to televised UVR protection messages over a 14-year period (1987–2002) was associated with a significant increase in use of hats (OR=1.24; 95% CI=1.15, 1.33) and sunscreen (OR=1.16; 95% CI=1.07, 1.25) and a significant reduction in average amount of body exposure (OR= −0.02; 95% CI= −0.02, −0.01; Appendix C Table 3, available online). The fourth study39 that used both traditional MM and social media to reduce tanning bed use led to a decrease in overall incidence of use (OR=0.61; 95% CI=0.54, 0.69) as well as a decrease in the proportion of teens who started using tanning beds in early adolescence (aged <13 years: 13% to 8%, p<0.001; aged 13–15 years: 75% to 65%, p<0.001). Some of these observed effects may be attributable to a successful lobbying and public relations campaign that resulted in increased publicity around the intervention and caused some local governments to remove sunbeds from public facilities.
Applicability of findings
Half of the included evidence was derived from Australia, where the climate and population demographics contribute to high skin cancer rates. In response to the public health burden of skin cancer, Australia has engaged in a longstanding, intensive, and multi-pronged health promotion campaign to improve UVR protective behaviors. The Australian studies included in this review evaluated effectiveness of MM interventions that were part of this comprehensive campaign and implemented in a context where extensive educational or policy interventions to reduce UVR exposure were already being conducted. Although results of the Australian studies can be useful in informing U.S. policymakers, their direct applicability is uncertain.
Conclusion on MM Interventions Alone
According to Community Guide rules,26 evidence was insufficient to determine the effectiveness of MM interventions alone. Although available evidence generally indicates that MM interventions are associated with improvements in protective and preventive behaviors, the evidence is based on a small number of studies, mostly conducted outside the U.S. This makes it difficult to draw any conclusions on the effectiveness of these interventions in the U.S. context.
Economic Evaluation
Economic evidence acquisition
A systematic review of economic evaluation studies was conducted by the economics team, comprising economists and subject matter experts on skin cancer prevention from various agencies, organizations, and academic institutions together with qualified systematic reviewers from The Community Guide Branch at CDC. Methods used in conducting systematic reviews of economic evaluations are described elsewhere (www.thecommunityguide.org/about/economics.html). In the original review,22 economic evaluations were not performed because effectiveness of the intervention was not established. Therefore, the economics team considered all available evidence on skin cancer prevention through April 2013 that included economic-specific keywords such as cost, cost–benefit, cost-effectiveness, and cost-utility. All monetary values were adjusted to 2013 U.S. dollars.
The search for evidence yielded two studies40,41 that evaluated costs and associated economic benefits for MCCW interventions; no economic studies met the inclusion criteria to evaluate the economic effectiveness of MM interventions.
Intervention costs
Both studies40,41 referenced cost data from the MCCW SunSmart campaign in Australia, which implements a combination of interventions including mass media, educational resources, and environmental and legislative changes at community level. The data were cited from the Anti-Cancer Council of Victoria, which estimated the average cost of the intervention at $0.26 per person (assuming a population of 18 million).
Economic summary measure
Two studies40,41 evaluated the cost of the SunSmart campaign in comparison to the savings from reduced healthcare expenditures for treatment of skin cancer. One study41 evaluated the costs and associated savings (reduced healthcare expenditures) of a prior SunSmart campaign which ran from 1988 to 2003, and estimated the benefit–cost ratio at 3.6:1. Both studies estimated the costs and savings of running a future national campaign based on SunSmart for the next 20 years. One study41 estimated the intervention would yield a return on investment of 2.3:1, and the second study40 estimated net savings to the Australian government ranging from $10.4 million to $98.9 million. The latter range is attributable to the perspective taken in the study. The larger value—$98.9 million—is estimated if the comparator is “do nothing”; the other value—$10.4 million—takes into account the current skin cancer prevention initiatives put in place by state/territorial governments and advocacy groups.
Both studies also expanded the perspective to include costs to individuals for complying with the SunSmart recommendation (i.e., cost of sunscreen and hat). Taking into account the cost to the individual, the intervention was no longer cost saving. However, the intervention was cost effective, with an estimate of $20,275 per life year saved and $13,142 per disability-adjusted life year.
Other Potential Benefits and Harms
No other benefits or harms related to MCCW and MM interventions were identified by the review team. In the existing literature, some concerns had been postulated about the association of increased UVR protection with vitamin D deficiency and decreased physical activity. According to the WHO, however, optimal concentrations of vitamin D can be attained in most individuals by 5–15 minutes of casual sun exposure on face, arms, and hands two to three times a week,42 although individuals with dark skin may need three to six times more sun exposure than those with fair skin.43 Further, adequate levels of vitamin D can be established with a healthy diet and oral supplements,44 avoiding the harmful effects of overexposure to UVR. Evidence also has shown that promotion of sun safety messages is not likely to be associated with reduced physical activity.45
Discussion
Summary of Findings
The available evidence showed that MCCW interventions (seven studies)31–37 are effective in reducing UVR exposure by increasing sunscreen use at the community level. This suggests that using these strategies can be effective in promoting UVR protection at the community level.
However, there was insufficient evidence to determine the effectiveness of MM alone (four studies)24,31,38,39 in reducing UVR exposure, indicating a continuing need for more research in this field to better assess effectiveness of these interventions.
Limitations
As with the original review, certain limitations were common across the entire body of evidence in these update reviews. These concerns relate to study design and analysis, description of the target population and intervention, and outcome measures. Of ten included studies24,31–39 in these analyses, most evidence was derived from before-and-after (eight studies)24,31,33,35–39 and time series (one study)31 studies (the Dobbinson study31 evaluated the effectiveness of a before-and-after study design for MM interventions and time series study designs for MCCW interventions, so it is counted twice in the total body of evidence). Only two studies32,34 were RCTs. Time series and before-and-after study designs have strengths over tightly controlled trials, such as fewer problems related to external validity. But both time series and uncontrolled pre- and post-assessments contain potential sources of bias.
Furthermore, many of the interventions were developed in ways that made it difficult to distinguish intervention effects clearly from changes in behavior related to other factors. For example, many interventions were implemented over time on a national level, offering little opportunity to identify unexposed populations.
Evidence Gaps
Existing evidence showed that more research is needed to identify the key components that play critical roles in the success of these interventions. For example, most MCCW programs included in this review were relatively intensive campaigns with combinations of multiple intervention components designed to reach broad populations; it is unclear whether less extensive interventions would show similar results.
Limitations arising from the before-and-after study design, discussed above, also suggest other considerations for future research. Additional studies with stronger research designs would be valuable to clarify effectiveness of MM and MCCW interventions to reduce UVR exposure. Limited evidence was available to determine variability in effectiveness of interventions based on type of population demographics (e.g., age, race/ethnicity, type of skin) and setting and population characteristics (e.g., general population, children and their caregivers, race/ethnicity, type of skin), as well as intervention characteristics such as scope (e.g., national versus local level). Better descriptions of these areas in published papers would help in assessing the applicability of findings and/or in explaining variability in effects.
Finally, included studies provided no evidence on change in the incidence of skin cancer attributable to these interventions. Although the link between development of skin cancer and exposure to UVR is well established, more long-term studies about how UVR protective behaviors relate to development of skin cancer are needed.
Supplementary Material
Acknowledgments
This review would not have been possible without the subject matter expertise and contributions of our coordination team from areas of CDC other than the Community Guide Branch as well as outside organizations. We also recognize Kate W. Harris, Kristen Folsom, and Onnalee Gomez for their assistance throughout the review process.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
References
- 1.DHHS. [Accessed August 19, 2015];The Surgeon General’s call to action to prevent skin cancer. 2014 www.surgeongeneral.gov/library/calls/prevent-skin-cancer/call-to-action-prevent-skin-cancer.pdf. [PubMed]
- 2.Guy GP, Jr, Machlin SR, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. Am J Prev Med. 2015;48(2):183–187. doi: 10.1016/j.amepre.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karagas MR, Weinstock MA, Nelson HH. Keratinocyte carcinomas (basal and squamous cell carcinomas of the skin) In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. New York: Oxford University Press; 2006. pp. 1230–1251. [Google Scholar]
- 4.U.S. Cancer Statistics Working Group. [Accessed August 19, 2015];United States cancer statistics: 1999–2011 incidence and mortality web-based report. 2014 www.cdc.gov/uscs.
- 5.Agency for Healthcare Research and Quality. [Accessed September 8, 2015];Medical Expenditure Panel survey. meps.ahrq.gov/mepsweb/
- 6.Machlin S, Carper K, Kashihara D. Health care expenditures for non-melanoma skin cancer among adults, 2005–2008 (average annual) Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 7.Jemal A, Saraiya M, Patel P, et al. Recent trends in cutaneous melanoma incidence and death rates in the United States, 1992–2006. J Am Acad Dermatol. 2011;65(5 Suppl 1):S17–25. e11–13. doi: 10.1016/j.jaad.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 8.Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279–282. doi: 10.1001/archdermatol.2010.4. [DOI] [PubMed] [Google Scholar]
- 9.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166(5):1069–1080. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Cancer Statistics Working Group. [Accessed August 19, 2015];Skin cancer statistics. 2013 www.cdc.gov/cancer/skin/statistics/index.htm.
- 11.American Cancer Society. [Accessed August 19, 2015];Cancer facts and figures. 2013 www.cancer.org/cancer/skincancer-melanoma/detailedguide/melanoma-skin-cancer-key-statistics.
- 12.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41(14):2040–2059. doi: 10.1016/j.ejca.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 13.Augustsson A, Stierner U, Rosdahl I, Suurkula M. Common and dysplastic naevi as risk factors for cutaneous malignant melanoma in a Swedish population. Acta Derm Venereol. 1991;71(6):518–524. [PubMed] [Google Scholar]
- 14.Green A, MacLennan R, Siskind V. Common acquired naevi and the risk of malignant melanoma. Int J Cancer. 1985;35(3):297–300. doi: 10.1002/ijc.2910350303. [DOI] [PubMed] [Google Scholar]
- 15.Greene MH, Clark WH, Jr, Tucker MA, Kraemer KH, Elder DE, Fraser MC. High risk of malignant melanoma in melanoma-prone families with dysplastic nevi. Ann Intern Med. 1985;102(4):458–465. doi: 10.7326/0003-4819-102-4-458. [DOI] [PubMed] [Google Scholar]
- 16.Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18(8):614–627. doi: 10.1016/j.annepidem.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vainio H, Miller AB, Bianchini F. An international evaluation of the cancer-preventive potential of sunscreens. Int J Cancer. 2000;88(5):838–842. doi: 10.1002/1097-0215(20001201)88:5<838::aid-ijc25>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Environmental Protection Agency (EPA) [Accessed August 20, 2015];UV radiation. 2010 www.epa.gov/sunwise/doc/uvradiation.html.
- 19.Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757. doi: 10.1136/bmj.e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin JS, Eder M, Weinmann S, et al. Behavioral counseling to prevent skin cancer: systematic evidence review to update the 2003 U.S. Preventive Services Task Force recommendation. Rockville MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 21.CDC. [Accessed August 19, 2015];What can I do to reduce my risk of skin cancer? 2013 www.cdc.gov/cancer/skin/basic_info/prevention.htm.
- 22.Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med. 2004;27(5):422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Parkin DM, Mesher D, Sasieni P. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br J Cancer. 2011;105(Suppl 2):S66–S69. doi: 10.1038/bjc.2011.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith BJ, Ferguson C, McKenzie J, et al. Impacts from repeated mass media campaigns to promote sun protection in Australia. Health Promot Int. 2002;17(1):51–60. doi: 10.1093/heapro/17.1.51. [DOI] [PubMed] [Google Scholar]
- 25.Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance--United States, 2013. MMWR Surveill Summ. 2014;63(Suppl 4):1–168. [PubMed] [Google Scholar]
- 26.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. Am J Prev Med. 2000;18(1 Suppl):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 27.Zaza S, Wright-De Aguero LK, Briss PA, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(1 Suppl):44–74. doi: 10.1016/s0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 28.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29(3):257–263. doi: 10.1200/jco.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- 29.Dore JF, Chignol MC. Tanning salons and skin cancer. Photochem Photobiol Sci. 2012;11(1):30–37. doi: 10.1039/c1pp05186e. [DOI] [PubMed] [Google Scholar]
- 30.World Bank. [Accessed August 19, 2015];Country and lending groups. data.worldbank.org/about/country-and-lending-groups.
- 31.Dobbinson SJ, Wakefield MA, Jamsen KM, et al. Weekend sun protection and sunburn in Australia trends (1987–2002) and association with SunSmart television advertising. Am J Prev Med. 2008;34(2):94–101. doi: 10.1016/j.amepre.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 32.Olson AL, Gaffney C, Starr P, Gibson JJ, Cole BF, Dietrich AJ. SunSafe in the middle school years: a community-wide intervention to change early-adolescent sun protection. Pediatrics. 2007;119(1):e247–256. doi: 10.1542/peds.2006-1579. [DOI] [PubMed] [Google Scholar]
- 33.Office of National Statistics (UK) SunSmart Survey 2003–10 - Trends Analysis. Cancer Research UK Commissions; 2010. [Google Scholar]
- 34.Dietrich AJ, Olson AL, Sox CH, Tosteson TD, Grant-Petersson J. Persistent increase in children’s sun protection in a randomized controlled community trial. Prev Med. 2000;31(5):569–574. doi: 10.1006/pmed.2000.0746. [DOI] [PubMed] [Google Scholar]
- 35.Miller DR, Geller AC, Wood MC, Lew RA, Koh HK. The Falmouth Safe Skin Project: evaluation of a community program to promote sun protection in youth. Health Educ Behav. 1999;26(3):369–384. doi: 10.1177/109019819902600307. [DOI] [PubMed] [Google Scholar]
- 36.New South Wales Cancer Council. Report on the Seymour Snowman Sun Protection Campaign (1997–1998) North Sydney, New South Wales, Australia: New South Wales Cancer Council; 1998. [Google Scholar]
- 37.Rassaby J. Slip Slop Slap: health education about skin cancer. Cancer Forum. 1983;7:63–69. [Google Scholar]
- 38.Broadwater C, Heins J, Hoelscher C, Mangone A, Rozanas C. Skin and colon cancer media campaigns in Utah. Prev Chronic Dis. 2004;1(4):A18. [PMC free article] [PubMed] [Google Scholar]
- 39.Koster B, Thorgaard C, Philip A, Clemmensen I. Sunbed use and campaign initiatives in the Danish population, 2007–2009: a cross-sectional study. J Eur Acad Dermatol Venereol. 2011;25(11):1351–1355. doi: 10.1111/j.1468-3083.2010.03960.x. [DOI] [PubMed] [Google Scholar]
- 40.Carter R, Robin M, David H. Could a national skin cancer primary prevention campaign in Australia be worthwhile? An economic perspective. Health Promot Int. 1999;14(1):73–82. doi: 10.1093/heapro/14.1.73. [DOI] [Google Scholar]
- 41.Shih ST, Carter R, Sinclair C, Mihalopoulos C, Vos T. Economic evaluation of skin cancer prevention in Australia. Prev Med. 2009;49(5):449–453. doi: 10.1016/j.ypmed.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization. [Accessed March 4, 2016];Ultraviolet radiation and the INTERSUN Programme: The known health effects of UV. 2013 http://www.who.int/uv/faq/uvhealtfac/en/index1.html.
- 43.Cancer Council Victoria. [Accessed August 20, 2015];Getting the balance right - vitamin D and sun protection. 2013 www.cancer.org.au/content/pdf/PreventingCancer/BeSunsmart/How_much_sun_is_enough_FINAL2012.pdf.
- 44.American Academy of Dermatology. [Accessed August 20, 2015];Position statement on vitaminD. 2009 www.aad.org/forms/policies/uploads/ps/ps-vitamin%20d.pdf.
- 45.Tran AD, Aalborg J, Asdigian NL, et al. Parents’ perceptions of skin cancer threat and children’s physical activity. Prev Chronic Dis. 2012;9:E143. doi: 10.5888/pcd9.110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.