Abstract
Objective
To describe a single-institution pilot study regarding prevalence and risk factors for delirium in critically ill children.
Design
A prospective observational study, with secondary analysis of data collected during the validation of a pediatric delirium screening tool, the Cornell Assessment of Pediatric Delirium (CAPD).
Setting
This study took place in the pediatric intensive care unit (PICU) at an urban academic medical center.
Patients
99 consecutive patients, ages newborn to 21 years.
Intervention
Subjects underwent a psychiatric evaluation for delirium based on the DSM-IV criteria.
Measurements and Main Results
Prevalence of delirium in this sample was 21%. In multivariate analysis, risk factors associated with the diagnosis of delirium were presence of developmental delay, need for mechanical ventilation, and age 2-5 years.
Conclusions
In our institution, pediatric delirium is a prevalent problem, with identifiable risk factors. Further large-scale prospective studies are required to explore multi-institutional prevalence, modifiable risk factors, therapeutic interventions, and effect on long-term outcomes.
Keywords: delirium, pediatrics, critical care, pediatric critical care, prevalence, risk factor
Introduction
Delirium is the behavioral manifestation of acute cerebral dysfunction associated with serious underlying medical illness. It presents as an acute and fluctuating change in mental status, with disordered attention and cognition.(1) It is a well-known and prevalent problem in adult intensive care, linked to short- and long-term morbidity (2), increased mortality,(3) and astronomical healthcare costs.(4)
The pathophysiology of ICU delirium is complex and multifactorial. It is the end-result of diffuse cerebral metabolic abnormality. Broadly, alterations in neurotransmission, cerebral blood flow, energy metabolism, and disordered cellular homeostasis all play a role.(5)(6)(7) Although it can occasionally be traced to a single etiology (for example: alcohol toxicity or delirium tremens), in the intensive care unit it is frequently a result of 3 synergistic events: the underlying disease process, side-effects of treatment, and the highly abnormal critical care unit environment.(8)(9)
As an example, let us consider the patient admitted to the ICU with pneumonia and associated acute hypoxemic respiratory failure. The inflammatory process associated with the infection and hypoxia predisposes the patient to delirium. The benzodiazepine prescribed to facilitate patient-ventilator synchrony is itself deliriogenic. The prolonged period of immobilization in the ICU bed, the presence of invasive lines and monitors, and the disruption of the patient’s sleep-wake cycle all contribute to the evolving delirium.(10)(9)
It is important to recognize that delirium is a medical diagnosis and not simply a constellation of symptoms. Delirium is not untreated pain, over-sedation, sleep deprivation, or withdrawal (although any of these may contribute to the development of delirium).(11)(12) Delirium is a syndrome that is the final common pathway of many factors. It represents acute non-traumatic brain injury, and must be recognized as such to allow for proper treatment and prevention.(13-16)
Epidemiology and risk factors for pediatric delirium are not yet well-described, due in part to the absence of widespread screening, under-recognition, and lack of evidence-based data.(17-19) The recent development of validated screening tools for use in critically ill children is a promising step.(20-23) With heightened awareness and detection of pediatric delirium, we can identify and address modifiable risk factors, investigate treatments, and assess the effects of delirium on long term health and quality of life of PICU survivors.
The objective of this pilot study is to describe the prevalence and risk factors for delirium in critically ill children in our intensive care unit over a 10 week time period. In this brief report, we present a secondary analysis of data prospectively collected during the validation of the Cornell Assessment of Pediatric Delirium (CAPD), a rapid observational tool used by the bedside nurse to screen for delirium in PICU patients of all ages.(21)
Methods
This is a prospective observational study, conducted over 10 weeks in an urban academic tertiary care PICU. All patients were eligible for inclusion, regardless of age or diagnosis. Parent or guardian was approached by study investigators for consent, and if consent was granted, the child was enrolled. When appropriate, assent was obtained from the child as well. Consent rate was 88.5%.
Subjects were assessed for delirium by a child psychiatrist at approximately noon each day. Sedation was not interrupted for the assessment, as our unit standard-of-care is to keep all patients as lightly sedated as possible given their underlying medical condition. Subjects’ level of consciousness ranged from moderately sedated (arousable to verbal stimulation), to awake, and agitated. Patients who were deeply sedated – defined here as unarousable to verbal stimulation – were excluded as they could not be assessed for delirium. In our institution, we assess sedation status using the widely-accepted (although not yet validated in pediatrics) Richmond Agitation Sedation Scale (RASS) every 4 hours.(24) All subjects with scores of -3 (movement or eye opening to voice) or higher were included. All children diagnosed with delirium were reported to the medical team so that appropriate treatment could be initiated.
Enrolled subjects were assessed for delirium daily, taking into consideration the past 24 hour period. The child psychiatrist completed a detailed interview and examination, utilizing the gold-standard DSM-IV diagnostic criteria.(1) Six child psychiatrists participated in these 252 assessments, and 4 training sessions took place to establish group consistency in concepts and vocabulary. Using a developmental framework, the child psychiatrists were able to reliably diagnose delirium even in the youngest of children. (25)
Children with developmental delay (defined as severe impairment in ability to communicate in age-appropriate way with caregiver at prehospital baseline) were assessed for delirium by these seasoned clinicians, who took into account the child’s baseline and assessed for a fluctuating change in consciousness and cognition consistent with delirium (acute brain dysfunction, due to the underlying medical illness). With careful attention to baseline, the psychiatrist was able to make a determination as to presence or absence of delirium in these subjects.
Demographic and clinical data were collected upon enrollment, including age, gender, diagnosis, severity of illness score using Pediatric Index of Mortality II (PIM2), and history of prematurity. Severe impairment in the child’s ability to communicate with caregiver at baseline was used as a proxy for severe developmental delay. Clinical data was collected daily, including need for oxygen and mechanical ventilation. Hospital length of stay was calculated from day of hospital admission to day of hospital discharge. This study was approved by the Institutional Review Board at Weill Cornell Medical College.
Enrollment goal was 100 individual subjects and 250 encounters (each subject could be assessed up to a predetermined maximum of 5 times to avoid biasing the results). Sample size was determined by a conservative assumption of 15% delirium prevalence overall, and to allow for exploratory subgroup analysis of delirium by age and presence or absence of significant developmental delay.
Statistical Methods
Normality tests were first performed to assess whether continuous covariates were normally distributed. If covariates were normally distributed, t-tests were used. For covariates not normally distributed, the non-parametric Wilcoxon rank-sum test was used to compare the median differences of covariates by delirium status (yes or no). For discrete covariates, the chi-square test and Fisher's exact test were used to compare the frequencies/proportion of covariates by delirium status. Multivariable logistic regression was performed to evaluate the independent associations between potential confounding factors and risk factors with delirium status. Any bivariate association that achieved a p-value of <0.2 was entered into the multivariate model. The odds ratios, 95% confidence intervals, and p values of the covariates were reported. In order to correct for more than one delirium diagnosis within some individuals, generalized estimating equation (GEE) analysis was performed to determine if results obtained using the standard logistic regression analysis materially changed. All statistical tests were two-sided and p<0.05 was considered statistically significant. All analyses were performed in SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina) and figures generated in STATA 13 (StataCorp LP, College Station, Texas).
Results
Characteristics of study population and observation of delirium
111 subjects were enrolled. 99 subjects completed at least one psychiatric diagnostic interview and exam and are included in data analysis. (12 subjects were unavailable for assessment. 9 were either off the unit (in surgical or radiologic suites) or involved in clinical care that could not be interrupted at the time the psychiatrist was available; 3 subjects were transferred out of the PICU prior to the psychiatrist’s availability) (Figure 1). These 12 subjects did not differ from the included patients with respect to demographics, diagnoses, or severity-of-illness categories.
Figure 1.

Subject recruitment flow
A total of 252 psychiatric diagnostic interviews and exams were completed as part of this study. Each subject was assessed between 1-5 times. Table 1 shows the demographics by subject (n=99), and Table 2 shows the clinical characteristics by encounter (n=252). Sixty percent of the subjects were male, 54% were under 5 years old, and 18% were characterized as developmentally delayed (Table 1). Developmental delay was defined as severe impairment in ability to communicate in age appropriate way with caregiver at pre-hospital baseline. Eighteen subjects had developmental delay: 7 had an underlying genetic disorder, 7 had complications of prematurity, 2 had hypoxic-ischemic encephalopathy, 1 had a history of stroke, and 1 had autism. These were diagnoses made pre-hospitalization, and not by the study investigators. These subjects did not differ from the overall population with respect to demographics or severity-of-illness categories.
Table 1.
Subject demographics and delirium status (n=99)
| Characteristic | Number of Subjects |
Average number of assessments per subject |
Delirium diagnosis during study |
No delirium diagnosis during study |
|---|---|---|---|---|
| N | 99 | 2.5 | 21 (21.2%) | 78 (78.8%) |
| Gender | ||||
| Male | 59 (59.6%) | 2.6 | 12 (57.1%) | 47 (60.3%) |
| Female | 40 (40.4%) | 2.4 | 9 (42.9%) | 31 (39.7%) |
| Age (yr) | ||||
| 0-2 | 34 (34.3%) | 2.3 | 8 (38.1%) | 26 (33.3%) |
| 2-5 | 19 (19.2%) | 2.6 | 6 (28.5%) | 13 (16.7%) |
| 5-13 | 21 (21.2%) | 3.2 | 6 (28.5%) | 15 (19.2%) |
| >13 | 25 (25.3%) | 2.2 | 1 (4.8%) | 24 (30.8%) |
| Developmental delay | ||||
| No delay | 81 (81.8%) | 2.3 | 13 (61.9%) | 68 (87.2%) |
| Delay | 18 (18.2%) | 3.6 | 8 (38.1%) | 41 (20.6%) |
Table 2.
Clinical characteristics by encounter and delirium status (n=252)
| Characteristic | Number of Observations |
Delirium | No Delirium | p-value |
|---|---|---|---|---|
|
| ||||
| N | 252 | 53 | 199 | |
|
| ||||
| Age (years) | ||||
| 0-2 | 77 (30.6%) | 16 (30.2%) | 61 (30.7%) | <.0001 |
| 2-5 | 50 (19.8%) | 20 (37.8%) | 30 (15.1%) | |
| 5-13 | 69 (27.4%) | 15 (28.3%) | 54 (27.1%) | |
| >13 | 56 (22.2%) | 2 (3.8%) | 54 (27.1%) | |
|
| ||||
| Developmental Delay | ||||
| No Delay | 184 (73.0%) | 26 (49.0%) | 158 (79.4%) | <.0001 |
| Delay | 68 (27.0%) | 27 (51.1%) | 41 (20.6%) | |
|
| ||||
| Oxygen | ||||
| No | 117 (46.4%) | 7 (13.2%) | 110 (55.3%) | <.0001 |
| Yes | 135 (53.6%) | 46 (86.8%) | 89 (44.7%) | |
|
| ||||
| Mechanical Ventilation | ||||
| No | 190 (75.4%) | 24 (45.3%) | 166 (83.4%) | <.0001 |
| Yes | 62 (24.6%) | 29 (54.7%) | 33 (16.6%) | |
|
| ||||
| RASS* (N=249) | ||||
| 0,1,2,3 | 187 (75.1%) | 23 (44.2%) | 164 (83.2%) | <.0001 |
| −1 | 27 (10.8%) | 7 (13.4%) | 20 (10.2%) | |
| −2 | 20 (8.0%) | 11 (21.2%) | 9 (4.6%) | |
| −3 | 15 (6.0%) | 11 (21.2%) | 4 (2.0 %) | |
|
| ||||
| PIM2 (median) | 2.8 | 1.1 | 0.01 | |
RASS=Richmond Agitation Sedation Scale. See text for description of levels.
During daily assessments, 54% were on supplemental oxygen, and 25% were mechanically ventilated. Six percent were moderately sedated (arousable to voice; RASS level -3), 8% were lightly sedated (briefly awaken to voice; RASS level -2), and 11% were drowsy (RASS level -1). (Table 2).
The prevalence of delirium was 21%. Ninety percent of subjects diagnosed with delirium had a fluctuating course; 10.5% of subjects diagnosed with delirium remained delirious throughout the course of the study. The average number of delirium diagnoses per patient was 2.52. There was a significant association with observations of pediatric delirium and developmental delay (p<0.0001), need for oxygen (p<0.0001), use of mechanical ventilation (p<0.0001), and deeper sedation level (p<0.0001) (Figure 2). Median severity of illness score (PIM2) was significantly higher in the group with pediatric delirium (2.8 vs. 1.1, p=0.01).
Figure 2.

Risk factors associated with diagnosis of delirium (Data reported as percentage of entire sample, total n=252 encounters)
Factors predicting Pediatric Delirium
Multivariable logistic regression analysis predicting pediatric delirium (Table 3) indicated that when adjusting for prognostic parameters, preschool age (2-5 years old) was found to be statistically significant in predicting pediatric delirium when compared with adolescents (>13 years old, OR=8.80 (1.82, 42.53); p =0.007) and when compared with infants (0-2 years old, OR = 2.57 (1.11, 5.93); p =0.027). Compared to children with typical development, children with developmental delay had a 3.45 greater likelihood of having a diagnosis of delirium (OR=3.45 (1.54, 7.76), p = 0.003). Requirement for mechanical ventilation was also found to be statistically significant in predicting pediatric delirium (OR=3.86 (1.81, 8.24), p = 0.0005). Mechanical ventilation was highly associated with both need for oxygen (p<0.0001) and depth of sedation (p<0.0001); therefore we did not enter these as independent variables in the multivariate model. Severity of illness (as determined by PIM2 score) and gender were not independent predictors of pediatric delirium.
Table 3.
Multivariable Logistic Regression Analyses predicting delirium (n=252)
| Predictor Variable | Adjusted Odds Ratio (95% CI)* | p-value |
|---|---|---|
| Age category (years) | ||
| 0-2 | Reference | -- |
| 2-5 | 2.57 (1.11, 5.93) | 0.027 |
| 5-13 | 0.87 (0.33, 2.33) | 0.79 |
| >13 | 0.29 (0.06, 1.43) | 0.13 |
| 0-2 | 3.43 (0.70, 16.78) | 0.13 |
| 2-5 | 8.80 (1.82, 42.53) | 0.007 |
| 5-13 | 2.99 (0.58, 15.41) | 0.19 |
| >13 | Reference | -- |
| Developmental delay | ||
| Yes | 3.45 (1.54, 7.76) | 0.003 |
| No | Reference | -- |
| Mechanical Ventilation | ||
| Yes | 3.86 (1.81, 8.24) | 0.0005 |
| No | Reference |
CI = confidence interval
Analysis controlled for potential confounders including severity of illness and gender.
GEE was performed in order to adjust for individuals who had more than one diagnosis of delirium. The statistical significance of the primary predictors in the model (Table 3) did not materially change. For example, the p value for developmental delay went from 0.003 to 0.021 and mechanical ventilation went from 0.0005 to 0.004.
Possible association between diagnosis of delirium and hospital length of stay
Hospital length of stay (LOS) for children diagnosed with delirium during this study was significantly higher than LOS for children who were not diagnosed with delirium (median = 3 days vs. 18 days; p<0.0001) (Figure 3). This association remained highly significant even when controlling for severity of illness.
Figure 3.
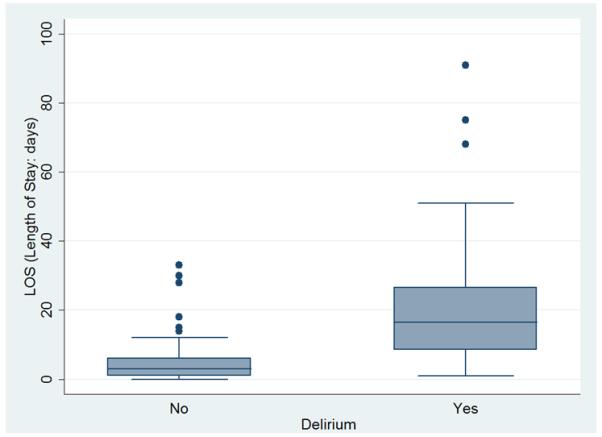
Association between subjects diagnosed with delirium during this study and hospital LOS (*one outlier (LOS = 267 days) was included in analysis, but removed from this figure).
Discussion
Delirium is prevalent in the pediatric intensive care unit. Children with significant developmental delay are at highest risk for developing delirium during their ICU stay. An atypical brain at baseline may be more vulnerable to the toxic/metabolic effects of critical illness through any number of proposed pathways associated with delirium. In this respect, children with developmental delay may be most analogous to adults with dementia, a well-described high-risk group in adult critical care.(4)
This highlights a current area of debate in pediatric delirium research. Children with developmental delay are notoriously hard to assess in the acute care setting.(24) As the diagnosis of delirium requires alteration from baseline, what is often required is a comprehensive and time-consuming history to establish the particular child’s baseline prior to definitively diagnosing delirium. It would be more efficient to exclude these difficult-to-assess children from ongoing delirium research, but that would exclude an important high-risk population.
Consistent with adult delirium research (5), we have demonstrated a higher risk for delirium in subjects who required supplemental oxygen, and the highest risk with need for invasive mechanical ventilation. We did not capture data regarding duration or severity of hypoxia (as measured by pO2). This is an interesting area for further research; a study investigating the association between brain tissue oxygen tension, as measured by non-invasive oximetry, and development of delirium may be warranted.
Not surprisingly, we found that deeper levels of sedation were highly correlated with mechanical ventilation (p<0.0001). An emerging literature in adult delirium research has identified a subset of delirium, sedation-induced delirium, which resolves shortly after sedative interruption. This delirium subtype does not seem to have the same poor prognosis when compared to persistent delirium in adults.(26) If the increased prevalence of delirium noted in mechanically ventilated children is at least partially due to sedation, this may have a better long-term prognosis than delirium of other etiologies. Further research is needed.
When assessed by age subgroups, in multivariate analyses that control for severity of illness, pre-school age children (2-5 years old) seem to be at highest risk for developing delirium in this cohort. The etiology of this increased risk has not been determined and needs to be reproduced in larger studies.
A possible contributing factor is the reliance of the 2-5 year old child on constant stimulation from the environment.(27) The developmentally-inappropriate immobility in the PICU may be extremely disruptive to this particular age-group. Interventions designed at increasing mobilization may be therapeutic, or even prophylactic, as found in the adult population.(28) Prospective studies are required to assess this possibility.
Another factor may be that these pre-school age children are exquisitely sensitive to disruption of their sleep-wake cycles.(29, 30) School-age children and adolescents are, in general, less sensitive to sleep disruption. Infants may be somewhat protected as their circadian rhythm is incompletely established, while preschool-age children have newly acquired consolidation of sleep at this developmental stage.(31) This potential mechanism requires further study.
Importantly, these data show a possible association between the diagnosis of delirium and increased hospital length of stay, even when controlling for severity of illness. This is consistent with previous pediatric delirium research (32), and suggests that pediatric delirium is associated with substantial increase in medical costs. Effectively managing delirium in children presents a significant opportunity for health care savings.(33)
Limitations of this study involve its pilot nature, as it was a secondary aim of a validation study for a delirium screening tool. As such, it presents only a cross section of pediatric delirium over a finite period in a single PICU. The data reported here are novel, and represent an important contribution to pediatric delirium research. However, it is important not to over-conclude based on these findings.(34)
In this pilot study, although we captured level of sedation, we did not collect data regarding particular sedation agents used, or doses. This is a limitation as the effects of particular sedatives, (particularly benzodiazepines), and their doses, may be important. A large scale, prospective observational longitudinal study is necessary to determine the association between delirium and modifiable risk factors, such as medications (particularly anticholinergics, sedatives, and steroids) and targeted interventions (both behavioral and pharmacologic). Preparation for such a study is underway.
Conclusion
Critically ill children are at risk for developing delirium during the course of their stay in the intensive care unit. Our preliminary data suggest that there are clearly identifiable sub-groups at higher risk. With heightened awareness to this prevalent problem, many PICUs are implementing delirium screening as standard of care. This will allow for a multi-institutional collaborative approach to furthering pediatric delirium research, and improving the care we provide to these vulnerable children.
Acknowledgments
Financial support: Statistical support from the Clinical Translational Science Center (CTSC), National Center for Advancing Translational Sciences (NCATS) grant #UL1-TR000457-06 is gratefully acknowledged.
Footnotes
Name of Institution where work performed: Weill Cornell Medical College/NY Presbyterian Hospital
Address for reprints: Reprints will not be ordered.
Pediatric Intensive Care Unit, Weill Cornell Medical College/NY Presbyterian Hospital, 525 East 68th St. M-508, New York, NY 10065
Contributor Information
Gabrielle Silver, Weill Cornell Medical College.
Chani Traube, Weill Cornell Medical College.
Linda M. Gerber, Weill Cornell Medical College.
Xuming Sun, Weill Cornell Medical College.
Julia Kearney, Memorial Sloan-Kettering Cancer Center.
Anita Patel, NY Presbyterian Hospital.
Bruce Greenwald, Weill Cornell Medical College.
REFERENCES
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. American Psychiatric Association; Washington, DC: 2000. p. 943. American Psychiatric Association. [Google Scholar]
- 2.Van den Boogaard M, Schoonhoven L, Evers AWM, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012 Jan;40(1):112–8. doi: 10.1097/CCM.0b013e31822e9fc9. [DOI] [PubMed] [Google Scholar]
- 3.Pisani MA, Kong SYJ, Kasl SV, Murphy TE, Araujo KLB, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009 Dec 1;180(11):1092–7. doi: 10.1164/rccm.200904-0537OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 5.Williams ST. Pathophysiology of Encephalopathy and Delirium. J Clin Neurophysiol. 2013;30(5):435–7. doi: 10.1097/WNP.0b013e3182a73e04. [DOI] [PubMed] [Google Scholar]
- 6.Sanders RD. Hypothesis for the pathophysiology of delirium: Role of baseline brain network connectivity and changes in inhibitory tone. Med Hypotheses. 2011 Jul;77(1):140–3. doi: 10.1016/j.mehy.2011.03.048. [DOI] [PubMed] [Google Scholar]
- 7.Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789–856. ix. doi: 10.1016/j.ccc.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Smith HAB, Brink E, Fuchs DC, Ely EW, Pandharipande PP. Pediatric Delirium. Pediatr Clin North Am. 2013 Jun;60(3):741–60. doi: 10.1016/j.pcl.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Reade MC, Finfer S. Sedation and Delirium in the Intensive Care Unit. N Engl J Med. 2014 Jan 30;370(5):444–54. doi: 10.1056/NEJMra1208705. [DOI] [PubMed] [Google Scholar]
- 10.Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care. 2008;12(Suppl 3):S3. doi: 10.1186/cc6149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Traube C, Augenstein J, Greenwald B, LaQuaglia M, Silver G. Neuroblastoma and pediatric delirium: A case series: Neuroblastoma and Delirium. Pediatr Blood Cancer. 2014 Jun;61(6):1121–3. doi: 10.1002/pbc.24917. [DOI] [PubMed] [Google Scholar]
- 12.Traube C, Witcher R, Mendez-Rico E, Silver G. Quetiapine as treatment for delirium in critically ill children: A case series. J Pediatr Intensive Care. 2013;2(3):121–6. doi: 10.3233/PIC-13060. [DOI] [PMC free article] [PubMed] [Google Scholar]; 11 MacLullich AMJ, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009 Feb;21(1):30–42. doi: 10.1080/09540260802675031. [DOI] [PubMed] [Google Scholar]
- 13.Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010 Jul;38(7):1513–20. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jackson JC, Gordon SM, Hart RP, Hopkins RO, Ely EW. The association between delirium and cognitive decline: a review of the empirical literature. Neuropsychol Rev. 2004 Jun;14(2):87–98. doi: 10.1023/b:nerv.0000028080.39602.17. [DOI] [PubMed] [Google Scholar]
- 15.MacLullich AMJ, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009 Feb;21(1):30–42. doi: 10.1080/09540260802675031. [DOI] [PubMed] [Google Scholar]
- 16.Schieveld JNM, van Tuijl S, Pikhard T. On Nontraumatic Brain Injury in Pediatric Critical Illness, Neuropsychologic Short-Term Outcome, Delirium, and Resilience*. Crit Care Med. 2013 Apr;41(4):1160–1. doi: 10.1097/CCM.0b013e31827bf658. [DOI] [PubMed] [Google Scholar]
- 17.Silver G, Traube C, Kearney J, Kelly D, Yoon MJ, Nash Moyal W, et al. Detecting pediatric delirium: development of a rapid observational assessment tool. Intensive Care Med. 2012;38(6):1025–31. doi: 10.1007/s00134-012-2518-z. [DOI] [PubMed] [Google Scholar]
- 18.Silver GH, Kearney JA, Kutko MC, Bartell AS. Infant delirium in pediatric critical care settings. Am J Psychiatry. 2010;167(10):1172–7. doi: 10.1176/appi.ajp.2010.09111606. [DOI] [PubMed] [Google Scholar]
- 19.Hatherill S, Flisher AJ. Delirium in children and adolescents: A systematic review of the literature. J Psychosom Res. 2010 Apr;68(4):337–44. doi: 10.1016/j.jpsychores.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Smith HAB, Boyd J, Fuchs DC, Melvin K, Berry P, Shintani A, et al. Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit*. Crit Care Med. 2011 Jan;39(1):150–7. doi: 10.1097/CCM.0b013e3181feb489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Traube C, Silver G, Kearney J, Patel A, Atkinson TM, Yoon MJ, et al. Cornell Assessment of Pediatric Delirium: A Valid, Rapid, Observational Tool for Screening Delirium in the PICU*. Crit Care Med. 2014 Mar;42(3):656–63. doi: 10.1097/CCM.0b013e3182a66b76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silver G, Kearney J, Traube C, Hertzig M. Delirium screening anchored in child development: The Cornell Assessment for Pediatric Delirium. Palliative and Supportive Care. 2014 Aug 15;:1–7. doi: 10.1017/S1478951514000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schieveld JNM, Janssen NJJF, van Cauteren YJM. On the Cornell Assessment for Pediatric Delirium and Both the Diagnostic and Statistical Manual, 5th Edition, and International Classification of Diseases, 11th Revision: Quo Vadis?*. Crit Care Med. 2014 Mar;42(3):751–2. doi: 10.1097/01.ccm.0000435686.08339.b6. [DOI] [PubMed] [Google Scholar]
- 24.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 25.Silver G, Kearney J, Traube C, Atkinson TM, Wyka KE, Walkup J. Pediatric delirium: Evaluating the gold standard. Palliat Support Care. 2014 Apr 24;:1–4. doi: 10.1017/S1478951514000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel SB, Poston JT, Pohlman A, Hall JB, Kress JP. Rapidly Reversible, Sedation-related Delirium versus Persistent Delirium in the Intensive Care Unit. American Journal of Respiratory and Critical Care Medicine. 2014 Mar 15;189(6):658–65. doi: 10.1164/rccm.201310-1815OC. [DOI] [PubMed] [Google Scholar]
- 27.Ball R. The Gesell developmental schedules. J Abnorm Child Psychol. 1977;5(3):233–9. doi: 10.1007/BF00913694. [DOI] [PubMed] [Google Scholar]
- 28.Peitz GJ, Balas MC, Olsen KM, Pun BT, Ely EW. Top 10 Myths Regarding Sedation and Delirium in the ICU. Crit Care Med. 2013 Sep;41:S46–S56. doi: 10.1097/CCM.0b013e3182a168f5. [DOI] [PubMed] [Google Scholar]
- 29.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep Duration From Infancy to Adolescence: Reference Values and Generational Trends. PEDIATRICS. 2003 Feb 1;111(2):302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 30.Magee CA, Gordon R, Caputi P. Distinct developmental trends in sleep duration during early childhood. Pediatrics. 2014 Jun;133(6):e1561–1567. doi: 10.1542/peds.2013-3806. [DOI] [PubMed] [Google Scholar]
- 31.Mirmiran M, Maas YG, Ariagno RL. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med Rev. 2003 Aug;7(4):321–34. doi: 10.1053/smrv.2002.0243. [DOI] [PubMed] [Google Scholar]
- 32.Smeets IAP, Tan EYL, Vossen HGM, Leroy PLJM, Lousberg RHB, Os J, et al. Prolonged stay at the paediatric intensive care unit associated with paediatric delirium. Eur Child Adolesc Psychiatry. 2009 Sep 27;19(4):389–93. doi: 10.1007/s00787-009-0063-2. [DOI] [PubMed] [Google Scholar]
- 33.Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, et al. Costs associated with delirium in mechanically ventilated patients*. Crit Care Med. 2004 Apr;32(4):955–62. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 34.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011 May;45(5):626–9. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


