Introduction
HIV Testing in the United States
In 2013, the US Preventive Services Task Force (USPSTF) updated its HIV screening recommendations, advising that “clinicians screen for HIV infection in adolescents and adults ages 15–65 years.”1 These updated recommendations were based on findings by the USPSTF, which found that identifying asymptomatic individuals and initiating HIV therapy reduces the risk of AIDS and death and that the use of HIV therapy decreases transmission of HIV to sexual partners, thus benefiting the community.1 The benefits of therapy cannot be realized if HIV testing is not routine. According to a report of US Centers for Disease Control and Prevention (CDC), over half of the Americans still have not been tested for HIV.2 Even worse, among the more than 1 million Americans currently infected with HIV, 14% are unaware they are infected because they have not been diagnosed.3 Furthermore, the problem of under- or late HIV testing is especially significant for racial and ethnic minority communities. According to the CDC, 35% of African Americans have never been tested for HIV2 even though they are disproportionately impacted by the disease.3
Physicians are Not Testing Their Patients for HIV
Despite the 2006 CDC recommendations4 and subsequent USPSTF recommendations in 2013,1 physicians are still not routinely testing their patients for HIV. In a national survey, 72% of people reported that their physician had never suggested HIV testing.5 In a study conducted in an HIV clinic with predominantly African American patients, 71% of these HIV-positive patients had at least 1 health-care encounter during the year prior to their HIV diagnosis during which their physician failed to test them for HIV.6 In a survey of physicians caring for predominantly African American patient populations, physicians reported testing only 34% of their patients for HIV in the past year.7 These physicians also admitted that when HIV testing was ordered for patients, it was more often done because of potential risks rather than for routine testing per national recommendations.7 Additionally, a study by Arya et al reported that only 68% of physicians in a large publicly funded healthcare system in a high HIV-prevalenee area routinely tested their patients for HIV.8
Physician Recommendations Will Encourage Patients to Be Tested
Studies have shown that a health-care provider recommending HIV testing could influence patients to get tested. A national survey found that 37% of respondents had been tested because their health-care provider suggested the HIV test.5 Conversely, among those not tested for HIV, 33% reported not being tested because their doctor never recommended the test.9 In a study of African American men, 96% of patients who had a physician recommend HIV testing got tested.10 Moreover, a recent study found that over 40% of patients actually wanted their healthcare provider to recommend the HIV test, and nearly 25% of patients expected that their health-care provider would test them for HIV.11 These findings highlight the importance of health-care provider recommendations for improving HIV testing in health-care settings.
Study Objectives
Recognizing both the need to increase HIV testing and the significant role of the health-care provider in testing, this study sought to determine physician preferences for a physician-targeted campaign to increase HIV testing.
Methods
Study Location
This study took place in Houston, Texas, the fourth most populous city in the United States.12 Houston is an area with high HIV prevalence13 and ranks fifth highest for HIV prevalence rate among the top 10 most populous US cities.12,14 This study took place from January to March 2013 and surveyed physicians in 19 publicly funded community health centers in Harris County, Houston. Approximately 91% of the HIV-infected cases in the Houston area are in Hams County.15 The health centers in which the study took place have over 1 million patient visits per year and serve predominantly Hispanic (60%) and African American (25%) patient populations.16
Study Design
An anonymous Web-based survey was constructed and e-mailed to primary care physicians in Harris County health centers. The survey provided multiple-choice options for HIV testing campaign elements targeting physicians.
Study Participants
The survey was e-mailed to 561 primary care physicians. These physicians were faculty and trainees from local academic medical centers. A previous study of this population focused on interpersonal and intrapersonal barriers to HIV testing.8 This study reported that 68% of this physician population routinely tested their patients for HIV.8 For completing the survey, physicians were offered a US$10 gift card and entry into a US$100 raffle. This study was approved by the Baylor College of Medicine institutional review board.
Data Analysis
The study results were assessed using descriptive statistics; response frequencies were calculated for each campaign element listed as a survey option to assess physicians’ relative campaign preferences. Chi-square tests were subsequently performed to investigate differences in faculty versus trainee responses.
Results
One hundred seventy-five physicians participated in this study—a response rate of 31%. The majority of participants were female (66%), 45% were white, 36.25% were Asian, and 13.75% were black/African American. The mean age was 34 years, and it had been an average of 8 years since participants graduated from the medical school. Most participants were either trainees (45%) or medical school faculty (40%). Medical specialties among this population were internal medicine (39%), family practice (29%), obstetrics and gynecology (20%), internal medicine/pediatrics (12%), and pediatrics and other at 0.6% each.
Physician HIV Testing Campaign Element: HIV Testing Information
Over 50% of the physicians believed that a physician-targeted HIV testing campaign that provided a copy or summary of the latest HIV testing recommendations would help them offer HIV tests to their patients. Nearly half (49%) indicated that data showing their patient population is at risk for HIV infection would help them to offer the test to their patients; this was selected more among trainees than among faculty members (P = .04). One-third indicated that they wanted educational materials or training on HIV testing procedures, HIV testing recommendations, and/or how to provide HIV test results (see Table 1). There was no significant difference between faculty versus trainee responses for the remaining “HIV Testing Information” campaign elements (P ≥ .1).
Table I.
What HIV Testing Campaigns Do Physicians Want? Physician Responses Sorted from Highest to Lowest Frequency.
| Physician HIV Testing Campaign Elements | n | % |
|---|---|---|
| HIV testing information | ||
| Copy of latest HIV testing recommendations | 109 | 62·29 |
| Summary of updated HIV testing guidelines/ recommendations |
90 | 51·43 |
| Data showing my patient population at risk for HIV infection |
86 | 49·14 |
| Educational materials or training on HIV testing procedures and recommendations |
59 | 33·71 |
| Educational materials or training on providing HIV test results |
59 | 33·71 |
| Communication tools | ||
| Patient asking for the HIV testa | 124 | 70·86 |
| Data showing that patients are receptive to HIV testinga |
60 | 34·29 |
| Example script with sample wording on how to initiate the HIV testing discussion with my patient |
38 | 21·71 |
| Promotion strategies | ||
| An EPICa,b alert for HIV testing | 108 | 61·71 |
| Posters promoting HIV testing in my exam room | 90 | 51·43 |
| If Harris Health, Baylor College of Medicine, and/or the University of Texas Health leadership promoted HIV testing |
44 | 25·14 |
| If the professional medical society I belong to promoted HIV testing |
9 | 5·14 |
These data were reported in a previous study.8
EPIC is the electronic medical record system used in the Harris Health System.
Physician HIV Testing Campaign Element: Communication Tools
Nearly three-quarters of physicians reported that patients asking for the HIV test would help them offer it to their patients. In addition, one-third of the physicians answered that data showing patients are receptive to HIV testing may be helpful (As noted in Table 1, these data have been published previously.8). Additionally, approximately 1 in 5 physicians requested a script for initiating HIV testing discussions with patients (see Table 1). There was no significant difference between faculty and trainee responses for “communication tools” campaign elements (P ≥ .1).
Physician HIV Testing Campaign Element: Promotion Strategies
Almost two-thirds of physicians indicated that an electronic medical record (EMR) alert for HIV testing would help them offer HIV tests to patients. Half of the respondents believed an effective campaign might provide posters promoting HIV testing in examination rooms. One-quarter of the physicians reported that they would be encouraged to offer patients HIV tests if local leadership promoted HIV testing (see Table 1). There was no significant difference between faculty and trainee responses for “promotion strategies” campaign elements (P ≥ .3).
Discussion
Physicians Want HIV Testing Information
Several studies—including 2 previously published studies on this target population—have shown that physicians do not routinely test their adult patients for HIV.5–8,17 This study highlighted several physician-targeted solutions to improve physician HIV testing behavior. According to the survey results, 1 step to achieving this would be providing physicians with updated copies of HIV testing recommendations. This is not surprising, given that a 2014 review article on physician HIV testing barriers found that many physicians remain unaware of the current recommendations.18 An effective physician-targeted HIV testing campaign should address gaps in physician knowledge about HIV testing. This could be an effective physician campaign strategy, as a separate review of physician campaigns concluded that information-based campaigns are effective when physicians indicate a desire for that information,17 such as in this study population.
Physicians Want to Be Prompted to Offer HIV Tests
Based on this study, more than half of the physicians would be most encouraged to offer HIV tests to their patients if they received EMR reminders or if their patients asked for the test. Several reasons physicians want external prompts to offer HIV tests may include the aforementioned lack of knowledge in addition to competing priorities and concern about patient receptiveness.8 According to the health belief model, “cues to action”19—such as EMR-based and patient reminder systems—could help activate behavior change in physicians. However, recent studies of EMR alerts for HIV testing in the primary care setting have shown mixed results. Avery et al found an increase from 4% to 17% of patients being HIV tested after implementation of HIV testing reminders into the EMR health maintenance list.20 Goetz et al found an increase from 4.8% to 10.8% in 1 intervention site and 5.5% to 12.8% in another after incorporating an EMR HIV testing alert along with other multifaceted campaign elements to improve HIV testing.21 However, a study by Sundaram et al in a Department of Veterans Affairs health-care system found that an EMR reminder alert for HIV testing did not work, as testing rates did not increase significantly due to intervention.22 Sundaram et al22 noted that their intervention was of “modest intensity” and contrasted their findings with the intervention employed by Goetz et al. The Goetz et al study utilized a “multimodal” intervention, leading Sundaram et al to conclude that computer-based reminders alone may not be enough to alter physician HIV testing behavior21,22 and that more rigorous interventions are needed.
As noted, our study found that physicians also want patients to act as prompts, cuing them to offer the HIV test. While EMR cues may be only moderately effective, patients asking directly for the test may have a greater impact. In fact, a recent qualitative study published by White et al found that physicians find it advantageous for patients to ask for the HIV test.23 Such patient-initiated discussions could help overcome some of physicians’ interpersonal barriers that hinder HIV testing discussions.17 Furthermore, patients who are more involved and actively participate in their physicians’ appointments are met with more patient-centered communication from and are more favorably perceived by their physicians.24 A physician-targeted campaign with a component that encourages patients to engage with their physicians may improve communication and make room for conversations about HIV testing.
Physicians Want to Know That Their Patients Want to Be Tested
In conjunction with being prompted by their patients to offer the HIV test, physicians want to know that their patients are open to being tested. In this study, over one-third of physicians reported wanting data on patient receptiveness to HIV testing. Notably, patients are more receptive to being tested than physicians appear to believe. A study by McAfee et al surveyed patients in an emergency department and found that patients expect routine HIV testing and want HIV testing in this setting.11 In a 2010 study, patients in a primary care clinic were surveyed after being offered the HIV test, and most patients thought it was a good idea for the test to be offered.25 Based on these findings, a key campaign message may be to highlight the willingness of patients to be tested for HIV. This may be an effective strategy to increase the number of physicians who offer HIV tests to their patients, especially among those physicians who perceive that patients might be likely to refuse testing.
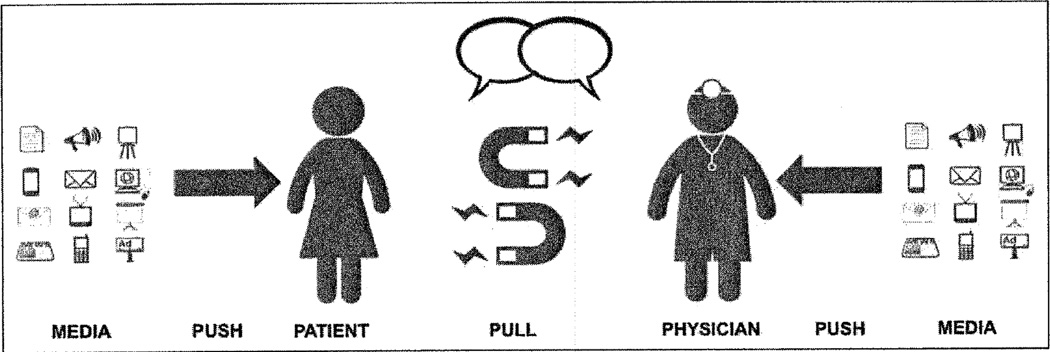
A 2-Sided HIV Testing Model
In order to maximize a campaign’s potential to increase HIV testing, both physicians and patients should ultimately be pushed to pull each other into HIV testing conversations. The push-pull capacity model is an innovative public health tool that delineates “pushing” as communicating health information to an audience and “pulling” as creating a demand for health services.26 Each of these proposed physician-targeted HIV campaign elements could “push” physicians to “pull” their patients into conversations about HIV testing. To have the greatest impact on improving HIV testing rates, a push could also be applied to patients to pull physicians into HIV testing conversations (see Figure 1). The “push-pull” model has been suggested for a patient-targeted campaign in which patients are prompted to ask their physicians for the HIV test.27 For example, a patient-centered campaign element could include directly sending patients text messages reminding them to talk to their physicians about the HIV test.27 Notably, this kind of campaign would coincide with physicians’ desire for patients to ask for the HIV test or to know their patients are receptive to the test. Such a 2-sided method could significantly increase HIV testing.
Figure I.
The 4-P Model for Health Campaigns: Media as a catalyst for pushing and pulling patients and physicians to improve communication. Adapted from “A Health Campaign Push–Pull Model” by Arya et al.27
Physicians Want HIV Testing to Be Promoted in Their Examination Rooms
In our study, over 50% of physicians recommend HIV testing posters in their examination rooms as an effective way to encourage physicians to offer HIV tests. This may further reflect physicians’ desire for a “cue to action” for both themselves and their patients, as HIV testing campaign posters in the same room as the desired HIV testing discussion could prompt both patients and physicians to initiate such a conversation. Alternatively, this finding may reflect physicians’ desire to promote HIV testing as a norm. Notably, a 2014 study reported that physicians believe public HIV testing campaigns can “legitimize” testing and decrease stigma.23 Physicians appear to be open to methods of promoting HIV testing that do not ostracize or profile patients but that indicate HIV as an acceptable topic of discussion for all patients.
Physicians Want Skills to Discuss HIV Testing
As part of a physician-targeted campaign, tools that provide physicians with resources to better communicate with their patients once in an HIV testing conversation may be an effective way to encourage physicians to offer the HIV test to their patients. Nearly 22% of physicians in our study indicated that a script for how to talk to their patients about HIV testing would encourage them to offer the test. This finding may not be surprising, given an older study by Epstein et al found that physicians realize that many of their HIV testing discussions with their patients can be “awkward.”28 An HIV testing campaign that guides physicians through these discussions might encourage physicians to offer the HIV test. This could include providing physicians with scripts to reference before initiating HIV testing discussions, conducting workshops or webinars for physicians on discussing HIV testing with their patients, or showing footage of fictional successful HIV testing discussions between physicians and patients.
Physicians Want Local Leadership to Promote HIV Testing
In addition to tangible information, cues, and communication tools, our data show that physicians would be more likely to offer HIV tests to patients if HIV testing was promoted by local leadership within their health-care system. The commitment of hospital and clinic leadership to a campaign has previously been seen as an effective way to encourage physician participation. A multifaceted campaign launched in 2007 found that the involvement of upper-level hospital officials, such as the CEO, chief medical officer, and department heads, in promoting hand hygiene was effective in “[generating] a ‘buzz’ and a positive feeling about [hand hygiene] despite the fact that [it] had been well promoted in traditional medical language prior to21 campaign.”29 By serving as an example, hospital and clinic leaders can help generate an atmosphere conducive to responding to the campaign being implemented. Alternatively, local leadership could promote HIV testing by being featured in local HIV testing campaigns (eg, photos of local leadership on HIV testing posters, quotes from local leadership in HIV testing brochures). Interestingly, physicians in our study reported HIV testing campaign promotion from their professional medical society as being least likely to encourage them to test their patients for HIV. Perhaps such specialized support is not sufficient, but a push from the physicians’ local healthcare system as a whole might be perceived as more convincing. Furthermore, medical societies may be less familiar with the patient population than the local leadership, making the latter group’s recommendations more influential.
Limitations
There are several limitations to this study. First, the physicians were all from a single health-care system, thus resulting in selection bias, which may limit the generalizability of the results to other health-care settings. Second, physician campaign preferences in this health-care system may not generalize to other health-care systems in the United States with lower HIV prevalence. Third, this study was conducted in a publicly funded health-care system; physicians in private practice settings may have different campaign preferences. Fourth, survey questions were presented in a multiple-choice format, which may have resulted in response bias in which physicians’ answers were influenced by reading the available choices. Finally, as this was an opt-in study, participation bias may have occurred reflecting only opinions of physicians who have very strong feelings for or against HIV testing campaigns. Notably, the incentive of US$10 and entry into a US$100 prize raffle is nominal for this target population, so it is unlikely that physicians were unduly influenced to participate.
Conclusion
To our knowledge, this is the first campaign design–focused study in a large publicly funded health-care system in a high HIV prevalence area to solicit primary care physicians’ suggestions for HIV testing campaigns targeting physicians on a large scale. Based on our study, it appears that an effective physician HIV testing campaign should include information about HIV testing recommendations, proof of patient receptiveness to HIV testing, cues to action, tools to improve physician–patient communication, and promotion by the leadership within the healthcare system. Ultimately, addressing the limited uptake of the 2006 CDC HIV testing recommendations and the more updated 2013 USPSTF routine HIV testing recommendations merits a need for urgent, innovative, 2-sided strategies to improve HIV testing. Both physicians and patients need to be activated to increase HIV testing discussions and increase HIV testing rates. Such a movement would help fulfill the Healthy People 2020 and National HIV/AIDS Strategy objectives to improve HIV testing.30,31 By encouraging physicians to adhere to the CDC and USPSTF guidelines, physicians can fulfill their crucial role in mitigating the ongoing HIV epidemic in the United States.
Acknowledgments
The authors wish to acknowledge Michael Kallen for his assistance in developing the survey instrument and Amber Amspoker for her assistance with data analysis. The images in Figure 1 were acquired using free clip art from Google images.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a Baylor-UT Houston Center for AIDS Research (CFAR) grant (AI036211, PI: Arya), an NIH-funded program and the National Institute of Mental Health of the National Institutes of Health under Award Number R23MH094235 (PI: Arya). This work was also supported in part by the Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413) in Houston, TX.
Footnotes
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the National Institutes of Health or the Department of Veterans Affairs.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
We have no conflict of interests to disclose.
References
- 1.Moyer VA. Screening for HIV: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(1):51–60. doi: 10.7326/0003-4819-159-1-201307020-00645. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV testing in the United States. [Accessed January 15, 2016];CDC Fact Sheet. 2015 Web site. http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-testing-us-508.pdf.
- 3.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent area—2011. [Accessed January 15, 2016];HIV Surveillance Supplemental Report. 2013 18(5) Web site. http://www.cdc.gov/hiv/pdf/2011_monitoring_hiv_indicators_hssr_final.pdf. [Google Scholar]
- 4.Branson BM, Handsfield HH, Lampe MA, et al. Centers for Disease Control and Prevention (CDC) Revised recommendations for HIV Testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(rr-14):1–17. quiz ce1-4. [PubMed] [Google Scholar]
- 5.Kaiser Family Foundation. Summary and Chartpack. 2012 Survey of Americans on HIV/AIDS 2012. [Accessed January 15, 2016]; Web site. https://kaiserfamily-foundation.files.wordpress.com/2013/01/8334-f.pdf. [Google Scholar]
- 6.Chin T, Hicks C, Samsa G, McKellar M. Diagnosing HIV infection in primary care settings: missed opportunities. AIDS Patient Care STDS. 2013;27(7):392–397. doi: 10.1089/apc.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong EY, Jordan WC, Malebranche DJ, et al. HIV testing practices among black primary care physicians in the United States. BMC Public Health. 2013;13:96. doi: 10.1186/1471-2458-13-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arya M, Patel S, Kumar D, et al. Why Physicians Don’t Ask Interpersonal and Intrapersonal Barriers to HIV Testing—Making a Case for a Patient-Initiated Campaign [published online November 23, 2014] J Int Assoc Provid AIDS Care. 2014 doi: 10.1177/2325957414557268. pii: 2325957414557268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaiser Family Foundation. Toplines. 2012 Survey of Americans on HIV/AIDS 2012. [Accessed January 15, 2016]; Web site. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8334-t.pdf. [Google Scholar]
- 10.Petroll AE, DiFranceisco W, McAuliffe TL, Seal DW, Kelly JA, Pinkerton SD. HIV testing rates, testing locations, and healthcare utilization among urban African-American men. J Urban Health. 2009;86(1):119–131. doi: 10.1007/s11524-008-9339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAfee L, Tung C, Espinosa-Silva Y, et al. A survey of a small sample of emergency department and admitted patients asking whether they expect to be tested for HIV routinely. J Int Assoc Provid AIDS Care. 2013;12(4):247–252. doi: 10.1177/2325957413488197. [DOI] [PubMed] [Google Scholar]
- 12.United States Census Bureau Population Division. Annual Estimates of the Resident Population for Incorporated Places of 50,000 or More, Ranked by July 1, 2013 Population: April 1, 2010 to July 1, 2013. [Accessed January 15, 2016];2014 Web site. http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 13.Centers for Disease Control and Prevention. Enhanced Comprehensive HIV Prevention Planning and Implementation for Metropolitan Statistical Areas Most Affected by HIV/AIDS. [Accessed January 15, 2016];2013 Web site. http://www.cdc.gov/hiv/prevention/demonstration/echpp/
- 14.Centers for Disease Control and Prevention. HIV Surveillance Report; 2011:23. [Accessed January 15, 2016];2013 Web site. http://www.cdc.gov/hiv/pdf/statistics_2011_HIV_Surveillance_Report_vol_23.pdf.
- 15.HIV/STD Prevention and Care Branch. 2013 Texas STD and HIV Epidemiologic Profile. [Accessed January 15, 2016];2014 Web site. https://www.dshs.state.tx.us/hivstd/reports/ [Google Scholar]
- 16.Harris Health System. Facts and Figures. [Accessed January 15, 2016]; Web site. https://www.harrishealth.org/en/about-us/who-we-are/pages/statistics.aspx.
- 17.Rubio-Valera M, Pons-Vigués M, Martínez-Andrés M, Moreno-Peral P, Berenguera A, Fernández A. Barriers and facilitators for the implementation of primary prevention and health promotion activities in primary care: a synthesis through meta-ethnography. PloS One. 2014;9(2):e89554. doi: 10.1371/journal.pone.0089554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng MY, Suneja A, Chou AL, Arya M. Physician barriers to successful implementation of US Preventive Services Task Force routine HIV testing recommendations. J Int Assoc Provid AIDS Care. 2014;13(3):200–205. doi: 10.1177/2325957413514276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Theory at a glance: a guide for health promotion practice. [Accessed January 15, 2016];2005 Web site. http://www.sneb.org/2014/Theory%20at%20a%20Glance.pdf. [Google Scholar]
- 20.Avery AK, Toro MD, Einstadter D. Decreasing missed opportunities for HIV testing in primary care through enhanced utilization of the electronic medical record. J AIDS Clin Res. 2012;(suppl 4) doi: 10.4172/2155-6113.S4-006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goetz MB, Hoang T, Bowman C, et al. QUERI-HIV/Hepatitis Program Group. A system-wide intervention to improve HIV testing in the Veterans Health Administration. J Gen Intern Med. 2008;23(8):1200–1207. doi: 10.1007/s11606-008-0637-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sundaram V, Lazzeroni LC, Douglass LR, Sanders GD, Tempio P, Owens DK. A randomized trial of computer-based reminders and audit and feedback to improve HIV screening in a primary care setting. Int J STD AIDS. 2009;20(8):527–533. doi: 10.1258/ijsa.2008.008423. [DOI] [PubMed] [Google Scholar]
- 23.White BL, Walsh J, Rayasam S, Pathman DE, Adimora AA, Golin CE. What makes me screen for HIV? Perceived barriers and facilitators to conducting recommended routine HIV testing among primary care physicians in the southeastern United States. J Int Assoc Provid AIDS Care. 2015;14(2):127–135. doi: 10.1177/2325957414524025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Street RL, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65(3):586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bryce G, Wilkinson P, Nicolson S, et al. A study to assess the acceptability, feasibility and cost-effectiveness of universal HIV testing with newly registering patients (aged 16–59) in primary care. Paper presented at: 17th Annual Conference of the British HIV Association (BHIVA); April 6–8, 2011; Bournemouth, UK. [Accessed January 15, 2016]. Web site. http://www.bhiva.org/documents/Conferences/Time-ToTest2010/Presentations/Posters/P4Bryce.pdf. [Google Scholar]
- 26.Orleans CT. Increasing the demand for and use of effective smoking-cessation treatments: reaping the full health benefits of tobacco-control science and policy gains—in our lifetime. Am J Prev Med. 2007;33(6):s340–s348. doi: 10.1016/j.amepre.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Arya M, Kumar D, Patel S, Street RL, Jr, Giordano TP, Viswanath K. Mitigating HIV health disparities: the promise of mobile health for a patient-initiated solution. Am J Public Health. 2014;104(12):2251–2255. doi: 10.2105/AJPH.2014.302120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Epstein RM, Morse DS, Frarey L, Anderson K, Beckman HB. Awkward moments in patient-physician communication about HIV risk. Ann Intern Med. 1998;128(6):435–442. doi: 10.7326/0003-4819-128-6-199803150-00003. [DOI] [PubMed] [Google Scholar]
- 29.Doron SI, Kifuji K, Hynes BT, et al. Infection prevention and control a multifaceted approach to education, observation, and feedback in a successful hand hygiene campaign. Jt Comm J Qual Patient Saf. 2011;37(1):3–3ap. doi: 10.1016/s1553-7250(11)37001-8. [DOI] [PubMed] [Google Scholar]
- 30.Healthy People 2020. HIV. [Accessed January 15, 2016];2020 Topics & Objectives. 2015 Web site. http://www.healthypeople.gov/2020/topics-objectives/topic/hiv/objectives.
- 31.White House Office of National AIDS Policy. [Accessed January 15, 2016];National HIV/AIDS Strategy for the United States. 2015 Web site. https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf.