Abstract
AIM
To provide an updated of recent findings about efficacy of cognitive-behavior therapy (CBT) in reduction of command hallucinations.
METHODS
PubMed/MEDLINE, Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature, PsycINFO, ClinicalTrial.gov searches were performed using the keywords “hallucinations”, “behavioural therapy” and “ cognitive therapy” in order to identify relevant articles published during the years of 2011 to 2016. No language limits were used. Studies conducted within control group, reviews, editorials, were excluded. Data on efficacy, acceptability and tolerability were extracted by three authors independently. Disagreements were resolved in a consensus meeting or by another reviewer.
RESULTS
A total of eight articles were eligible for inclusion. Two are randomized clinical trials (RCTs) and six are observational studies. The two RCTs included showed a greater efficacy of CBT compared to standard care on auditory hallucinations (AHs). Nevertheless, they considered different CBT models, particularly Treatment of Resistant Command Hallucinations and Cognitive Therapy for Command Hallucinations. As regards non RCT-studies, all papers included showed reduction on frequency and severity of AHs and distress related to them. However, the lack of content details within non-RCTs studies decreased their comparability. In terms of predictive variables, our findings show that negative symptoms at baseline appeared to be the strongest predictor of the treatment efficacy. Indeed, negative symptoms showed a significant negative correlation on outcome.
CONCLUSION
Although more conclusive studies are still needed, we found some preliminary evidence for the efficacy of CBT in the treatment of command hallucinations.
Keywords: Auditory hallucinations, Cognitive-behavior therapy, Schizophrenia, Psychotic disorder, Treatment, Distress, Functional impairment
Core tip: Auditory hallucinations (AHs), especially command hallucinations, represent a special problem for the clinical management of schizophrenia and contribute significantly to distress and disability related to this disorder. The aim of this article is to review the current knowledge and evidence on the efficacy of cognitive-behavior therapy interventions in AHs.
INTRODUCTION
Hallucinations can be defined as sensory experiences in any sensory modality, occurring in the absence of a corresponding external stimulation whilst in a fully conscious state, and resembling veridical perceptions[1-3]. In schizophrenia, hallucinations occur with a high frequency of up to 50%-80%[4]. Among hallucinations, auditory hallucinations (AHs) are considered the highest, with prevalence estimates in schizophrenia ranging between 40% and 80%[5-7].
AHs, especially command hallucinations, are also associated with an increased risk of harmful or dangerous actions[8-13]. Shawyer et al[8] reported a median 53% prevalence of command hallucinations in adult participants with psychiatric disorders, 48% of these participants said the commands stipulated harmful or dangerous actions, rising to 69% for participants in medium secure unit. However, the link between the presence of command hallucinations and harm to self or others is not straightforward. In the MaCarthur study[14], no association was reported between the presence of delusions or command hallucinations and violence. Thoughts about violence, however, were a strong predictor of violence 6 mo later[14].
Besides the high prevalence, AHs experienced in psychotic illness contribute significantly to distress and disability[8]. Indeed, several clinical studies show that AHs appraised as malevolent are significantly and positively associated with distress[9-11]. These findings were confirmed in a recent systematic review by Mawson et al[12].
Antipsychotic agents are considered to be the first choice for the treatment of psychotic symptoms[15], but at least one third of patients exhibit persistent psychotic symptoms, despite drug treatment[16]. Treatment of drug-resistant patients can be complicated by adverse effects, due to the use of second-line drugs such as Clozapine[17] or combination therapy with multiple antipsychotic agents[18]. Moreover, there are many concerns regarding patients’ refusal to adhere with drug regimes[19] and long-term compliance to therapy[20]. Consequently, there is a growing interest on psychological interventions, which are now recognized as important components of a comprehensive therapeutic approach in the treatment of schizophrenia. AHs are some of the most prominent and distressing of the treatment-resistant symptoms, and command hallucinations are the most high risk of these[21]. Command hallucinations represent a special problem for the clinical management of psychosis. Previous research suggests cognitive-behavior therapy (CBT) to be a useful treatment for reducing compliance with harmful command hallucinations[8,22].
Specifically, CBT applied to the treatment of command hallucinations does not focus on reducing the experience of voices, but on reducing the perceived power of voices to harm the individual and to motivate compliance[8,22]. Indeed, the main rationale is that by challenging key beliefs about the power of commanding voices, the patients would show a lower level of compliance and appeasement behavior and an increase in resistance to the same voices. In a recent meta-analysis, van der Gaag et al[23] showed that CBT is effective in the treatment of AHs and delusions. Specifically, individually tailored case formulation CBT showed larger effect-size than broad CBT including standard training programs. However, in this study va der Gaag et al[23] have considered both the AHs that delusions.
The aim of our review is to provide an updated overview on the efficacy of CBT interventions in AHs. Specifically, we focus on the efficacy of CBT in reducing command hallucinations.
MATERIALS AND METHODS
This is a review of the literature published between 2011 and 2016 on trials using CBT targeted on AHs in schizophrenia and related psychotic disorders.
A comprehensive literature search of the PubMed/MEDLINE, Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature (CINHAL), PsycINFO, ClinicalTrial.gov databases were conducted. A search algorithm based on a combination of the terms: (hallucinations) AND (behavioral therapy OR cognitive therapy) was used. Moreover the bibliographies of the most relevant published articles in the field were screened. The last update of the search was on March 2016. Data on efficacy, acceptability and tolerability were extracted by three authors independently (Franco De Crescenzo, Maria Laura Pucciarini, Maria Pontillo). Disagreements were resolved in a consensus meeting or by another reviewer (Marco Armando). No language limits were used.
The search algorithm resulted in 212 articles, of which 38 referred to potentially eligible studies. Of these, 30 articles were non-empirical studies, reviews and commentaries. We found a total pool of eight studies on CBT for the treatment of AHs.
Two randomized clinical trials (RCTs)[21,24] and six observational studies[25-30] fulfilled the inclusion criteria. In terms of evidence-based medicine, the quality of these studies was moderate.
We decided to focus on the past five years (2011-2016) because this is the period in which CBT models specifically targeted on AHs were developed. In fact, for the previous period, van der Gaag et al[23] (2014) had already published a meta-analysis. However, this meta-analysis does not focus specifically on AHs.
In Figure 1 are represented the search strategy with inclusion/exclusion criteria for the papers.
Figure 1.
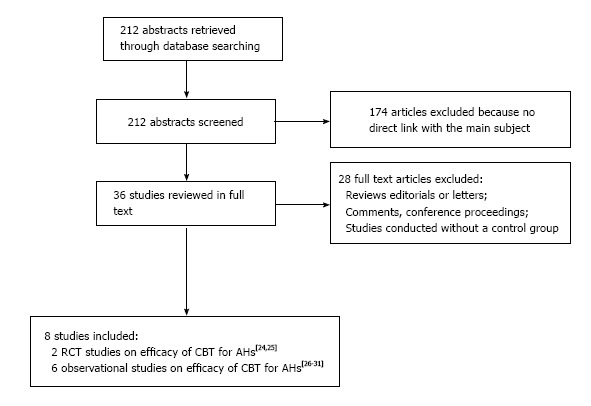
Flow chart of literature review. AHs: Auditory hallucinations; CBT: Cognitive-behavior therapy; RCT: Randomized clinical trial.
RESULTS
RCTs
During the last four years two RCTs have been conducted, proving the efficacy of CBT for the treatment of AHs, both were specifically on Command Hallucinations. Details on the methodologies and results of the studies are shown in Table 1.
Table 1.
Randomized clinical trials of cognitive behavioral therapy for auditory hallucinations
| Ref. | Sample | Methods | Criteria for diagnosis | Criteria for outcome | Focused treatment | Results | Follow-up |
| Shawyer et al[14] | n = 44 Mean age: 39 | RCT | (1) diagnosis of schizophrenia or related condition based on DSM-IV criteria (2) command hallucinations within the previous 6 mo that caused distress or dysfunction despite treatment with antipsychotic medication at therapeutic doses | Assessor-rated degree of compliance with harmful command hallucinations on a scale of 0-7 Self-rated confidence to resist obeying harmful commands and confidence in coping with general commands on a scale of 0-100 PANSS Modified GAF PSYRATS Quality of Life Enjoyment and Satisfaction Questionnaire Client Satisfaction Questionnaire VAAS BAVQ-R 8-item self-report Insight Scale RSQ | Randomized to 15 sessions of the intervention “TORCH” or the control, Befriending. A sub-sample of 17 participants was randomized to a waitlist control before being allocated to TORCH or Befriending Pharmacological treatment: Chlorpromazine equivalent dose (mg) Mean = 742.9 SD = 388.7 | Confidence to resist harmful CHs (P = n.s.) Confidence in coping with CHs (P < 0.01) PANSS total (P < 0.05) Modified GAF (P = n.s.) Distress PSYRATS (P < 0.01) Disruption PSYRATS (P < 0.01) Quality of Life ( P < 0.05) VAAS (P = n.s.) BAVQ-R (P = n.s.) | 6-mo |
| Birchwood et al[15] | n = 197 Mean age: 37.4 | RCT | (1) ICD-10 schizophrenia, schizoaffective, or mood disorders, under care of a clinical team (2) history of harmful command hallucinations of at least 6 mo duration with recent (< 9 mo) history of harm to self, others or major social transgressions as a result of the commands (full or partial compliance); or harmful command hallucinations where the individual is distressed and appeasing the powerful voice | VCS VPD Personal knowledge questionnaire/omniscience scale BAVQ-R PSYRATS Calgary Depression Rating Scale for Schizophrenia Beck Hopeleness Scale Beck Scale for Suicidal Ideation PANSS | Randomized to cognitive Therapy for command Hallucinations + treatment as usual or treatment as usual alone Adherence to cognitive therapy was excellent: only 12 (12%) of 98 participants not attending any sessions, and 79 (81%) completing the therapy (all manualised elements) Pharmacological treatment: Olanzapine equivalents dose (mg) 25.79 (SD: 21.73). | RSQ (P = n.s.) VCS experimental group: 41; control group: 49 VPD total, experimental group: 21.31; control group: 23.98 Personal knowledge questionnaire (P = 0.09) BAVQ-R (P = n.s.) PSYRATS total (P = n.s.) Calgary Depression Rating Scale for Schizophrenia (P = n.s.) Beck Scale for Suicidal Ideation (P = n.s.) PANSS total (P = n.s.) | 18-mo |
AHs: Auditory hallucinations; BAVQ-R: Beliefs about the voices questionnaire-revised; CHs: Command hallucinations; GAF: Global assessment of functioning scale; n.s.: Not significant; PANSS: Positive and negative syndrome scale; RCT: Randomized clinical trial; PSYRATS: Psychotic symptom rating scale; RSQ: Recovery style questionnaire; VAAS: Voices acceptance and action scale; VCS: Voice compliance scale; VPD: Voice power differential scale.
Shawyer et al[24] evaluated the efficacy of a cognitive behavioural intervention model called Treatment of Resistant Command Hallucinations (TORCH) compared with befriending, which is a fully manualised control intervention[31] that provides the patients with the same amount of therapist engagement and expectancy as CBT. The treatment program was conducted for 15 weekly sessions lasting approximately 50 min and with a follow up at six months. Despite TORCH participants subjectively reporting greater improvement in command hallucinations compared to Befriending participants, the study found no significant group differences in the primary outcome (e.g., degree of compliance with harmful command hallucinations), nor in the secondary outcomes (e.g., severity illness, global functioning, level of distress related to command hallucinations, quality of life), based on blinded assessment data.
Birchwood et al[21] performed a multi-centre RCT of Cognitive Therapy for Command Hallucinations (CTCH)[32] which is a subtype of CBT specifically targeted on AHs, compared to usual treatment, on 197 participants with command hallucinations, to prevent harmful compliance. This RCT was programmed to follow the patients for 19 sessions, delivered steadily over the 9 mo post-randomisation. The results showed a better efficacy of CTCH respect to treatment as usual.
Both the studies[21,24] were powered on the compliance behavior to voices. In Shawyer et al[24] the Voices Acceptance and Action Scale (VAAS)[33] was used, while in Birchwood et al[21] the Voice Compliance Scale (VCS)[34] was preferred.
The two RCTs differed in many ways. First of all, Shawyer et al[24] did not find any statistical difference between the treatments considered (TORCH vs befriending). Birchwood et al[21] is a much larger trial which found a significant difference between the treatments considered (CBT vs treatment as usual) and which was based and powered on a previous pilot study[22]. The comparisons used for the two RCTs were different as well. In Shawyer et al[24] the intervention “befriending” was used. It has a similar amount of therapist engagement and expectancy as CBT, with similar drop-out rates[35]. Befriending involves a series of conversations that resemble conversations with a friendly social acquaintance. In Birchwood et al[21] the treatment as usual[15] was used as comparison.
On the one hand, in Shawyer et al[24] no differences were found between or within the TORCH and befriending groups on confidence to resist harmful commands at endpoint or follow up. On the other hand in Birchwood et al[21] the CTCH intervention showed to be significantly superior to the usual treatment and the efficacy interpreted as the effect that is common to the 9 and 18 mo follow-up points, was calculated as an odds ratio of 0.574 (95%CI: 0.33-0.98, P = 0.042). Both the trials had high quality and a low risk of bias (Table 1).
Non-RCT clinical studies
We found six non-RCT studies examining the efficacy of CBT for AHs in patients with psychosis. Details on the methodologies and results of the studies are shown in Table 2.
Table 2.
Non randomized clinical trials of cognitive behavioral therapy for auditory hallucinations
| Ref. | Sample | Methods | Criteria for diagnosis | Criteria for outcome | Focused treatment | Results | Follow-up |
| Zanello et al[21] | n = 41 age-range: 18-65 | Naturalistic Study | (1) Diagnosis of a schizophrenia or schizoaffective disorder (2) Current AHs in the form of voices, occurring at least once per week | Reduction of AHs: BPRS Total symptom severity without AHs: BPRS | 7 sessions of CBT based upon the program “Voice Group” of Wikes et al 1999 Pharmacological treatment: New antipsychotic Combined antipsychotic Anxiolytic, mood stabilizer, hypnotic or antidepressant medication Dosage: Changed when clinically required | Decrease in the hallucinations item score of Bprs (P < 0.05) Decrease in the total symptoms severity score of BPRS (P < 0.01) | 6-mo |
| Thomas et al[16] | n = 33 Mean age: 36.4 | Non-RCT Open trial | 1) Diagnosis of a schizophrenia or schizoaffective disorder (2) Current AHs in the form of voices, occurring at least once per week (3) Voices associated with significant subjective distress (4) History of voices for at least one year; and (5) currently prescribed antipsychotic medication | Correlation between PSYRATS, PANSS, SAI and Outcome Main Outcome measure: Improvement of five points of more on the PSYSTRATS | 24 sessions of CBT based upon the manual of Fowler et al (1995) Pharmacological treatment: Chlorpromazine-equivalent pre-treatment: M = 793.1 mg, SD = 468.6 mg; post–treatment: M = 768.1 mg, SD = 473.8 mg | Only negative symptoms showed a statistically correlation with outcome (rpb = -0.60; P ≤ 0.001) | None |
| Mortan et al[17] | n = 12 age range: 18-55 | Pilot study | (1) Criteria for schizophrenia or schizoaffective based on DSM-IV-R (SCID I) (2) At least 1 psychotic attack with hospitalization (3) Ongoing AHs (4) Use of oral and injectable antipsychotic | Presence of Positive Symptoms: SAPS Presence of Negative Symptoms: SANS Comorbid symptoms: BDI HDI | 9-10 sessions of CBT upon the manual of Morrison, 2002, Goldberg, 2007) Pharmacological treatment: Oral and injectable antipsychotic medication | Difference between pre-treatment and post-treatment Treatment goup: SAPS hallucination subscale score (P = 0.027) SAPS delusion sub-scale score (P = 0.028) SANS total scored (P = 0.046) KSQ (P = n.s.) BDI (P = n.s.) Control group: SAPS hallucination subscale score (P = n.s.) SAPS delusion sub-scale score (P = n.s.) SANS total scored (P = n.s.) BDI (P = 0.043) HDI (P = n.s.) | 1-yr post-treatment follow-up |
| Hutton et al[18] | Single case, An 18-year-old man | Case report | Criteria for schizophrenia spectrum disorder based on DSM-IV Symptoms and psychosocial functioning: GAF; BPRS; Clinical questionnaire | Positive Symptoms: PSYRATS/CAARMS Beliefs about control of AHs: IVI | Brief CBT upon the mindfulness approach Pharmacological treatment: None | Pre-treatment: IVI score: 62 Post treatment: IVI score 2 The frequency and duration of AHs had reduced to zero | 1, 3, 4, 9 mo post therapy |
| Dannahy et al[19] | n = 62 divided in nine groups Mean age: 41.1 SD: 9.2 | Pilot study | The individual had been experiencing treatment-resistant and subjectively distressing voices for at least the preceding 2 yr, with the voice-distress rated at 3 or greater on at least one of the two PSYRATS voice-distress items | Primary outcome measure: Improve general psychosocial well-being (CORE-OM); Secondary measures: Reduce distress and perceived voice-control; Evaluate the relationship with voice (VAY) | Group person-based cognitive Therapy (PBCT) conducted over 8-12 sessions based upon the manual of Chadwick et al (2006) Pharmacological treatment: Standard psychiatric care Group person-based cognitive Therapy (PBCT) conducted over 8-12 sessions based upon the manual of Chadwick et al (2006) Pharmacological treatment: Standard psychiatric care | CORE-OM Total score: Post-group: 1.90b (0.70) VOICE-DISTRESS Total score: Post-group: 3.57b (0.83) VOICE-CONTROL total score: Post-group: 53.47b (23.59) VAY Voice Dependence total score: Post group: 6.76 (5.69) VAY Voice Intrusiveness total score: Post group: 9.03 (4.32) VAY Voice Dominance total score: - Post group: 14.46 (6.37) VAY Hearer distance total score: Post group: 12.93 (5.93) | 1 mo |
| Gottlieb et al[20] | n = 17 Mean age: 40.10 SD: 13.63 | Pilot study | (1) Criteria for schizophrenia, schizoaffective disorder, or psychosis, NOS based on DSM-IV (2) At least “moderate” level of AHs severity over the past week (BPRS Hallucinations item 4 or higher); (3) Between the ages of 18-65; (4) No exposure to CBTp within the past 3 yr (5) No current suicidal ideation or hospitalization within the past month (6) Taking a stable dose of an antipsychotic medication for at least one month; (7) No active substance abuse/dependence (8) MMSE score ≥ 24) | Primary outcomes: Reduce the frequency, intensity, loudness, associated distress, perceived degree of controllability of, and interference from AHs (PSYRATS) Secondary outcomes: Evaluate beliefs about AHs (BAVQ-R); Evaluate overall psychopathology (BPRS), and depression (BDI-II) | Web-based cognitive-behavioral therapy for AHs: - 10 session: - psychoeducational video tutorials - games - interactive exercises - social network to examine the coping strategies of other users. Pharmacological treatment: stable dose of antipsychotic medication for at least one month | Significant reductions from baseline to post-treatment in several measures of AHs and in overall psychopathology on the BPRS: PSYRATS AHs subscale total: P = 0.007 PSYRATS AHs Subscale: Voices location: P = 0.029 Voices intensity of negative statements: P = 0.049 PSYRATS delusions subscale total: P = 0.101 BPRS total score: P = 0.001 BPRS Subscale: BPRS Psychosis: P = 0.002 - BPRS Depression: P = 0.004 BPRS Activation: P = 0.001 BAVQ-R total score: P = 0.902 (n.s.) BDI-II-total score: P = 0.085 (n.s.) | None |
P < 0.001. BPRS: Brief psychiatric rating scale; PSYRATS: Psychotic symptom rating scale; PANSS: The positive and negative syndrome scale for schizophrenia; SAI: The Schedule for the Assessment of Insight; SCID-I: Structured Clinical Interview for DSM; SAPS: Scale for the assessment of positive symptoms; SANS: Scale for the assessment of negative symptoms; BDI-II: The Back Depression Inventory II; HDI: Hamilton depression inventory; CAARMS: Comprehensive Assessment of At-Risk Mental States; GAF: Global Assessment of functioning; IVI: Interpretation Voices of Inventory; CORE-OM: Clinical outcomes in routine evaluation-outcome measure; VAY: Voice and You; BAVQ-R: The Belief about Voices Questionnaire-Revised; MMSE: Mini Mental State Examination; AHs: Auditory hallucinations.
In the latest study, Zanello et al[30] investigated the effectiveness of a group cognitive behavioural therapy for AHs, the Voices Group, in 41 patients with schizophrenia or schizoaffective disorders. The program Voices Group was conducted for seven specific sessions. The results showed a significant reduction in the severity of AHs (P < 0.005) and in total symptoms severity score of BPRS 4.0 [Brief Psychiatric Rating Scale[36]; without hallucination (P < 0.01)]. This result remained stable after the 6-mo follow-up.
Thomas et al[25] conducted an open label trial on the efficacy of CBT in reducing AHs in 33 subjects with schizophrenia. They also investigated the role of insight, beliefs about the origin of hallucinations, negative symptoms and cognitive disorganization as predictors of the outcome. The study observed post-treatment improvements in hallucination severity when AHs were considered a specific target of psychological treatment. Only overall negative symptoms showed a significant negative correlation on (rpb = -0.60, P = 0.001) with outcome. This effect appeared to be independent of length of illness, drop-out and number of sessions.
Mortan et al[26] evaluated the effectiveness of a group-based CBT program for AHs on 7 inpatients with schizophrenia and other psychotic disorders compared to 5 in patients treated with treatment as usual. The CBT treatment program was conducted for 9-10 sessions twice/wk. The results showed a significant reduction (P < 0.005) in the severity and frequency of hallucinations, delusions, negative symptoms, distress and anxiety after group-based CBT.
A case study by Hutton and Morrison[27] described the effectiveness of brief CBT (12 wk) in an 18-year-old male with psychotic disorder and AHs who refused antipsychotic medication. By week 12, the frequency and duration of AHs had reduced to zero.
Dannahy et al[28] examined the impact of group person-based cognitive therapy (PBCT) for distressing voices in a sample of 62 participants with treatment-resistance and subjectively distressing voices. Participants were divided in nine groups and PBCT was conducted over 8-12 sessions. Results demonstrated significant improvements in the outcomes measure of general well-being (P < 0.001), voice-distress (P < 0.001), control (P < 0.01) and dependence upon voice (P < 0.05).
Gottlieb et al[29] tested the feasibility and effects of a 10 session web-based CBT for AHs in a sample of 17 individuals with schizophrenia spectrum disorder. Results showed a significant reduction of AHs, including the perception of voices as an outside entity and intensity of negative commentary. Interestingly, participants improved in depression and delusion severity, although these symptoms were not directly targeted in the program.
DISCUSSION
The present review describes the efficacy of CBT in patients with AHs. In summary, the two RCTs included showed a greater efficacy of CBT compared to standard care on AHs. However, in Shawyer et al[24], TORCH participants subjectively reporting greater improvement in command hallucinations compared to Befriending but no significant group differences on primary outcome measure that was level of compliance with harmful command hallucination. In Birchwood et al[21] instead, CTCH participants showed an improvement in this measure.
One possible explanation of the discrepancy between the two RCTs in term of efficacy on reducing level of compliance with harmful command hallucinations is that, within the general framework of CBT, different theoretical approach can play a different role on the efficacy of the intervention. Indeed, the two RCTs were built on different theoretical frameworks. The TORCH framework is based on the “acceptance” of voices by “cultivating the capacity to just notice voices and associated thoughts rather than believing and acting on them”. The CTCH focuses on targeting individuals’ appraisals, behavior and affect, and not necessarily symptoms. It is based on the nature of the relationship with the personified voice. Therefore, if the voice hearer believes the voice to have malevolent intent, and crucially to have the power to deliver the threat, this can motivate compliance or appeasement behavior. In addition, in Shawyer et al[24] the intervention “befriending” was used as the control condition and it has a similar amount of therapist engagement and expectancy as CBT. This is likely to have resulted in smaller between-group effect sizes respect to Birchwood et al[21].
As regards non RCT-studies, all papers included showed reduction on frequency and severity of AHs and distress related to them. However, the lack of content details and on rationales within non-RCTs studies decreases their comparability and therefore the chance to draw final conclusions.
In terms of predictive variables, negative symptoms appeared to be the strongest predictor of the treatment efficacy. It may be that negative symptoms are a barrier to treatment specific to hallucinations, although it would be important to verify this association in other studies. However, based on this finding, it is possible to propose that negative symptoms interfere with engagement in therapy, in rapport with the therapist, and completion to homework. This might lead to modifications of CBT to treatment for the presence of negative symptoms, such as the use of more behavioral methods.
Some limitations and strenghts should be considered in our review. Firstly, the role and the possible interference of antipsychotic medications with psychotherapy should be further assessed in the primary studies. Secondly, there is a discrepancy of study design and outcome measures between studies, which did not allow a quantitative analysis of the results. Thirdly, most studies are only preliminary and underpowered. Among strenghts, we have two RCTs with 241 individuals randomized in total and both of them conclude that CBT may be an alternative for individuals with schizophrenia who experience AHs despite antipsychotic treatment.
Overall, several CBT models were tested in the studies included. Apart TORCH and CTCH, Mindfulness approach, PBCT or web-based CBT were used.
We propose that further RCTs are needed. In particular, based on our findings, future studies should be drawn with reference to validated theoretical framework that predicts individuals’ compliance with voices and the associated distress, rather than the presence of psychotic symptoms per se. This validated theoretical framework should also consider the role of negative symptoms in predicting the effectiveness of the intervention on Ahs.
Finally, due to the efficacy and high tolerability and acceptability of RCT-studies, we believe that the treatment with CBT should be integrated into standard care for AHs, taking into account that individuals with AHs and command hallucinations especially, and more in general with psychotic disorders, show often a poor compliance to pharmacological treatments.
COMMENTS
Backgrounds
In schizophrenia, auditory hallucinations (AHs) occur with a high frequency ranging between 40% and 80%. AHs, especially command hallucinations, are also associated with an increased risk of harmful or dangerous actions and are some of the most prominent of the pharmacological treatment-resistant symptoms. Consequently, there is a growing interest on psychological interventions. The aim of this review is to provide an updated of recent findings about efficacy of cognitive-behavior therapy (CBT) in reduction of command hallucinations.
Research frontiers
Previous research suggests CBT to be a useful treatment for reducing compliance with harmful command hallucinations. Specifically, CBT applied to the treatment of command hallucinations does not focus on reducing the experience of voices, but on reducing the perceived power of voices to harm the individual and to motivate compliance. Indeed, the main rationale is that by challenging key beliefs about the power of commanding voices, the patients would show a lower level of compliance and appeasement behavior and an increase in resistance to the same voices.
Innovations and breakthroughs
In literature evidence on efficacy of CBT in reduction of command hallucinations are still few. Only in recent years CBT models specifically targeted on AHs were developed. Studies published in the last five years were critically reviewed by the authors who make a comparison between the current existing CBT models for AHs and data to support each.
Applications
This review suggests that the treatment with CBT should be integrated into standard care for AHs, taking into account that individuals with AHs and command hallucinations especially show often a poor compliance to pharmacological treatments.
Terminology
AHs can be defined as sensory experiences in auditory modality, occurring in the absence of a corresponding external stimulation whilst in a fully conscious state, and resembling veridical perceptions. CBT is a psychosocial intervention that is the most widely used evidence-based practice for treating mental disorders. CBT focuses on the development of personal coping strategies that target solving current symptoms and changing unhelpful patterns in cognitions (e.g., thoughts, beliefs, and attitudes), behaviors, and emotional regulation.
Peer-review
The topic is interesting, informative and useful for a clinician. The paper is clearly written.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interests for this article. No financial support.
Data sharing statement: Please, note that our article is a secondary study and all the primary data are available to the public in the primary studies cited in the references.
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: April 28, 2016
First decision: June 16, 2016
Article in press: August 9, 2016
P- Reviewer: Flyckt L, Kravos M, Mauri MC S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Beck AT, Rector NA. Cognitive approaches to schizophrenia: theory and therapy. Annu Rev Clin Psychol. 2005;1:577–606. doi: 10.1146/annurev.clinpsy.1.102803.144205. [DOI] [PubMed] [Google Scholar]
- 2.Waters F, Allen P, Aleman A, Fernyhough C, Woodward TS, Badcock JC, Barkus E, Johns L, Varese F, Menon M, et al. Auditory hallucinations in schizophrenia and nonschizophrenia populations: a review and integrated model of cognitive mechanisms. Schizophr Bull. 2012;38:683–693. doi: 10.1093/schbul/sbs045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larøi F, Sommer IE, Blom JD, Fernyhough C, Ffytche DH, Hugdahl K, Johns LC, McCarthy-Jones S, Preti A, Raballo A, et al. The characteristic features of auditory verbal hallucinations in clinical and nonclinical groups: state-of-the-art overview and future directions. Schizophr Bull. 2012;38:724–733. doi: 10.1093/schbul/sbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andreasen NC, Flaum M. Schizophrenia: the characteristic symptoms. Schizophr Bull. 1991;17:27–49. doi: 10.1093/schbul/17.1.27. [DOI] [PubMed] [Google Scholar]
- 5.Landmark J, Merskey H, Cernovsky Z, Helmes E. The positive triad of schizophrenic symptoms. Its statistical properties and its relationship to 13 traditional diagnostic systems. Br J Psychiatry. 1990;156:388–394. doi: 10.1192/bjp.156.3.388. [DOI] [PubMed] [Google Scholar]
- 6.Aleman A, Larøi F. Washington, DC: American Psychological Association; 2008. Hallucinations: The Science of Idiosyncratic Perception. [Google Scholar]
- 7.Sommer IE, Slotema CW, Daskalakis ZJ, Derks EM, Blom JD, van der Gaag M. The treatment of hallucinations in schizophrenia spectrum disorders. Schizophr Bull. 2012;38:704–714. doi: 10.1093/schbul/sbs034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shawyer F, Mackinnon A, Farhall J. Command hallucinations and violence: implications for detention and treatment. Psychiatry, Psychol Law. 2003;10:97–107. [Google Scholar]
- 9.Birchwood M, Chadwick P. The omnipotence of voices: testing the validity of a cognitive model. Psychol Med. 1997;27:1345–1353. doi: 10.1017/s0033291797005552. [DOI] [PubMed] [Google Scholar]
- 10.Morrison AP, Nothard S, Bowe SE, Wells A. Interpretations of voices in patients with hallucinations and non-patient controls: a comparison and predictors of distress in patients. Behav Res Ther. 2004;42:1315–1323. doi: 10.1016/j.brat.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Smith B, Fowler DG, Freeman D, Bebbington P, Bashforth H, Garety P, Dunn G, Kuipers E. Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr Res. 2006;86:181–188. doi: 10.1016/j.schres.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Mawson A, Cohen K, Berry K. Reviewing evidence for the cognitive model of auditory hallucinations: The relationship between cognitive voice appraisals and distress during psychosis. Clin Psychol Rev. 2010;30:248–258. doi: 10.1016/j.cpr.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Barrowcliff AL, Haddock G. The relationship between command hallucinations and factors of compliance: a critical review of the literature. The Journal of Forensic Psychiatry and Psychology. 2006;17:266–298. [Google Scholar]
- 14.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157:566–572. doi: 10.1176/appi.ajp.157.4.566. [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Clinical Excellence. London: Clinical Guideline; 2014. Psychosis and schizophrenia in adults: treatment and management; p. 155. [Google Scholar]
- 16.Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Thibaut F, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13:318–378. doi: 10.3109/15622975.2012.696143. [DOI] [PubMed] [Google Scholar]
- 17.Samara MT, Dold M, Gianatsi M, Nikolakopoulou A, Helfer B, Salanti G, Leucht S. Efficacy, Acceptability, and Tolerability of Antipsychotics in Treatment-Resistant Schizophrenia: A Network Meta-analysis. JAMA Psychiatry. 2016;73:199–210. doi: 10.1001/jamapsychiatry.2015.2955. [DOI] [PubMed] [Google Scholar]
- 18.Galling B, Roldán A, Rietschel L, Hagi K, Walyzada F, Zheng W, Cao XL, Xiang YT, Kane JM, Correll CU. Safety and tolerability of antipsychotic co-treatment in patients with schizophrenia: results from a systematic review and meta-analysis of randomized controlled trials. Expert Opin Drug Saf. 2016;15:591–612. doi: 10.1517/14740338.2016.1165668. [DOI] [PubMed] [Google Scholar]
- 19.Nosé M, Barbui C, Tansella M. How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychol Med. 2003;33:1149–1160. doi: 10.1017/s0033291703008328. [DOI] [PubMed] [Google Scholar]
- 20.Phan SV. Medication adherence in patients with schizophrenia. Int J Psychiatry Med. 2016;51:211–219. doi: 10.1177/0091217416636601. [DOI] [PubMed] [Google Scholar]
- 21.Birchwood M, Michail M, Meaden A, Tarrier N, Lewis S, Wykes T, Davies L, Dunn G, Peters E. Cognitive behaviour therapy to prevent harmful compliance with command hallucinations (COMMAND): a randomised controlled trial. Lancet Psychiatry. 2014;1:23–33. doi: 10.1016/S2215-0366(14)70247-0. [DOI] [PubMed] [Google Scholar]
- 22.Trower P, Birchwood M, Meaden A, Byrne S, Nelson A, Ross K. Cognitive therapy for command hallucinations: randomised controlled trial. Br J Psychiatry. 2004;184:312–320. doi: 10.1192/bjp.184.4.312. [DOI] [PubMed] [Google Scholar]
- 23.van der Gaag M, Valmaggia LR, Smit F. The effects of individually tailored formulation-based cognitive behavioural therapy in auditory hallucinations and delusions: a meta-analysis. Schizophr Res. 2014;156:30–37. doi: 10.1016/j.schres.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 24.Shawyer F, Farhall J, Mackinnon A, Trauer T, Sims E, Ratcliff K, Larner C, Thomas N, Castle D, Mullen P, et al. A randomised controlled trial of acceptance-based cognitive behavioural therapy for command hallucinations in psychotic disorders. Behav Res Ther. 2012;50:110–121. doi: 10.1016/j.brat.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Thomas N, Rossell S, Farhall J, Shawyer F, Castle D. Cognitive behavioural therapy for auditory hallucinations: effectiveness and predictors of outcome in a specialist clinic. Behav Cogn Psychother. 2011;39:129–138. doi: 10.1017/S1352465810000548. [DOI] [PubMed] [Google Scholar]
- 26.Mortan O, Tekinsav Sütcü S, German Köse G. [A pilot study on the effectiveness of a group-based cognitive-behavioral therapy program for coping with auditory hallucinations] Turk Psikiyatri Derg. 2011;22:26–34. [PubMed] [Google Scholar]
- 27.Hutton P, Morrison AP, Taylor H. Brief cognitive behavioural therapy for hallucinations: can it help people who decide not to take antipsychotic medication? A case report. Behav Cogn Psychother. 2012;40:111–116. doi: 10.1017/S135246581100035X. [DOI] [PubMed] [Google Scholar]
- 28.Dannahy L, Hayward M, Strauss C, Turton W, Harding E, Chadwick P. Group person-based cognitive therapy for distressing voices: Pilot data from nine groups. J Behav Ther Exp Psychiatry. 2011;42:111–116. doi: 10.1016/j.jbtep.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Gottlieb JD, Romeo KH, Penn DL, Mueser KT, Chiko BP. Web-based cognitive-behavioral therapy for auditory hallucinations in persons with psychosis: a pilot study. Schizophr Res. 2013;145:82–87. doi: 10.1016/j.schres.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Zanello A, Mohr S, Merlo MC, Huguelet P, Rey-Bellet P. Effectiveness of a brief group cognitive behavioral therapy for auditory verbal hallucinations: a 6-month follow-up study. J Nerv Ment Dis. 2014;202:144–153. doi: 10.1097/NMD.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 31.Bendall S, Killackey E, Jackson H, Gleeson J. Melbourne: ORYGEN Research Centre and Department of Psychology, University of Melbourne; 2003. Befriending Manual. [Google Scholar]
- 32.Byrne S, Birchwood M, Trower P, Meaden A. London & New York: Routledge; 2006. A Casebook of cognitive behaviour therapy for command hallucinations. A social rank theory approach. [Google Scholar]
- 33.Shawyer F, Ratcliff K, Mackinnon A, Farhall J, Hayes SC, Copolov D. The voices acceptance and action scale (VAAS): Pilot data. J Clin Psychol. 2007;63:593–606. doi: 10.1002/jclp.20366. [DOI] [PubMed] [Google Scholar]
- 34.Beck-Sander A, Birchwood M, Chadwick P. Acting on command hallucinations: a cognitive approach. Br J Clin Psychol. 1997;36(Pt 1):139–148. doi: 10.1111/j.2044-8260.1997.tb01237.x. [DOI] [PubMed] [Google Scholar]
- 35.Bendall S, Jackson HJ, Killackey E, Allot K, Johnson T, Harrigan S. The credibility and acceptability of Befriending as a control therapy in a randomized controlled trial of Cognitive Behaviour Therapy for acute first episode psychosis. Behav Cogn Psychoth. 2006;34:277–291. [Google Scholar]
- 36.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: The drift busters. Int J Methods Psychiatr Res. 1993;3:221–244. [Google Scholar]


