Abstract
There exists a general consensus that prolonged grief disorder (PGD), or some variant of PGD, represents a distinct mental disorder worthy of diagnosis and treatment. Nevertheless, confusion remains over whether different names and proposed symptom criteria for this disorder identify the same or different diagnostic entities. This study aimed to determine whether PGD, complicated grief (CG), and persistent complex bereavement disorder (PCBD) as described by the DSM‐5 are substantively or merely semantically different diagnostic entities. Data were derived from the Yale Bereavement Study, a longitudinal community‐based study of bereaved individuals funded by the US National Institute of Mental Health, designed explicitly to evaluate diagnostic criteria for disordered grief. The results suggested that the difference between PGD and PCBD is only semantic. The level of agreement between the original PGD test, a new version of the PGD test proposed for ICD‐11 and the PCBD test was high (pairwise kappa coefficients = 0.80‐0.84). Their estimates of rate of disorder in this community sample were similarly low (∼10%). Their levels of diagnostic specificity were comparably high (95.0‐98.3%). Their predictive validity was comparable. In contrast, the test for CG had only moderate agreement with those for PGD and PCBD; its estimate of rate of disorder was three‐fold higher (∼30%); its diagnostic specificity was poorer, and it had no predictive validity. We conclude that PGD, PCBD and proposed ICD‐11, but not CG, symptom‐diagnostic tests identify a single diagnostic entity. Ultimately, brief symptom‐diagnostic tests, such as the one proposed here for ICD‐11, may have the greatest clinical utility.
Keywords: Prolonged grief disorder, complicated grief, persistent complex bereavement disorder, DSM‐5, ICD‐11, diagnostic specificity, predictive validity
Over the past two decades, there has been increasing awareness and conclusive research demonstrating that prolonged grief disorder (PGD)1 – intense, prolonged symptoms of grief, coupled with some form of functional impairment beyond 6 months post‐loss – constitutes a distinct mental disorder. Numerous studies have demonstrated that symptoms of grief are distinct from symptoms of depression and anxiety2, 3, 4, 5, 6, 7; that PGD is distinct from other mental disorders, including major depressive disorder, generalized anxiety disorder and post‐traumatic stress disorder1, 8, 9; and that PGD, independent of other mental disorders, is associated with significant suffering and enduring functional impairments1, 3, 9, 10, 11.
In light of extensive, convincing evidence in support of PGD as a new diagnostic category, the World Health Organization (WHO) has moved to introduce PGD, and the American Psychiatric Association has moved to introduce what appears to be a version of PGD, into their respective diagnostic classification systems (ICD‐11 and DSM‐5). However, despite these advances, and perhaps due to lack of unanimity in terminology and conceptualization of the disorder, there continues to be confusion about PGD and its relationships to normative grief and to other mental disorders.
In recent years, competing characterizations and symptom‐diagnostic tests have been proposed for what would appear to be a single disorder of grief. The primary opposition has been between the notion of “prolonged grief disorder”, introduced by Prigerson et al1 and proposed for adoption in a shortened version by the ICD‐1112, 13, and the notion of “complicated grief” (CG), which has historical roots in the concept of depression as a bereavement‐related “complication”14 and has been reproposed by Shear et al15. Presented with these two main alternatives, the DSM‐516 introduced yet a third diagnostic concept, i.e. “persistent complex bereavement disorder” (PCBD), that appears a compromise between “prolonged” and “complicated” grief. It is unclear whether DSM‐5's PCBD is essentially PGD, CG or another diagnostic entity altogether.
Semantic differences between PGD, CG and PCBD hinge on the response to the central question: “is all grief normal?”.
For proponents of PGD, the answer to this question is: “no, not all grief is normal; in particular, prolonged, unresolved, intense grief is not normal”. From the PGD perspective, grief symptoms in themselves are neither atypical nor pathological. PGD is characterized by normal symptoms of grief that remain too intense for too long. That is, all symptoms of grief are normal, but some combination of their severity and their duration is not. For PGD, the pathology is in the time course of the symptoms, not in the symptoms per se.
For proponents of CG, the answer to the question is: “yes, all grief is normal; but, there are complications (mental disorders) in bereavement aside from grief that merit clinical attention”. From this perspective, neither symptoms nor processes of grief are ever intrinsically pathological17. For CG, the pathology is attributed to factors other than grief, e.g. bereavement‐related depression or trauma, that interfere with otherwise normal grief processes.
The DSM‐5 designation “persistent complex bereavement disorder” omits the term “grief” altogether, which avoids pathologizing any form of grief and thereby leaves safe the assumption that all grief is normal. The assertion that the course of grief, in itself, can be pathological in some instances, i.e., that some grieving processes are inherently abnormal, separates PGD from both CG and PCBD.
Despite semantic differences, the proposed symptom‐diagnostic tests for PGD, CG and PCBD may point to a single underlying diagnostic entity. The items included in these tests are almost entirely derived from a common set of instruments, i.e., the Inventory of Complicated Grief (ICG)18 and its revisions. There is considerable evidence that items in these instruments represent a unidimensional underlying construct1, 18, 19. Nevertheless, the items in each diagnostic formulation constitute unique criteria sets. There may be substantive differences between symptom‐diagnostic tests for PGD, CG and PCBD that pose the risk of diluting the assessment of what is, at its core, a pure grief construct.
To date, only the original symptom‐diagnostic test for PGD has been validated empirically. In a US National Institute of Mental Health (NIMH)‐funded study designed explicitly to evaluate diagnostic criteria for disordered grief, with data collected in a community‐based sample (which is essential for distinguishing between normal and pathological grief reactions), Prigerson et al1 established the construct validity, diagnostic sensitivity and specificity, and predictive validity of diagnostic criteria for PGD.
In contrast, Shear et al introduced the proposed test for CG in a review article15, without an empirical evaluation or validation. The proposed test for CG, which includes multiple items not included in the ICG, was informed by a post‐hoc analysis of ICG data20 collected in highly comorbid, treatment‐seeking, patient samples, ill‐suited for drawing distinctions between normal and pathological grief, recruited for studies that were not designed for the purpose of evaluating diagnostic criteria for CG.
The symptom‐diagnostic test for PCBD is proposed in an appendix to DSM‐516. The proposed ICD‐11 characterization of PGD presents its core diagnostic features13, but the symptoms included in this narrative proposal have yet to be reduced explicitly to a symptom‐diagnostic test, i.e., there is no specification of how many of these symptoms need to be present to satisfy the symptom criterion.
In the present investigation, we aimed to compare proposed symptom‐diagnostic tests for PGD (both the original version1 and a new one consistent with the core diagnostic features of PGD as proposed for ICD‐1113), for CG15 and for PCBD16. We restricted our focus to an examination of tests for meeting the symptom criterion for grief disorder, as opposed to the time from loss and impairment criteria, because of the central role that the symptom criterion plays in the conceptualization, definition and recognition of the disorder.
Given legitimate concerns about pathologizing normal grief reactions, we prioritized diagnostic specificity above diagnostic sensitivity, favoring tests that minimize “false positives” (i.e., normal grief reactions diagnosed as mental illness) and thereby reduce the likelihood of over‐diagnosis and over‐treatment. Furthermore, since short tests and simple algorithms are preferred in clinical practice21, 22 and lead to higher reliabilities in routine care23, we considered the brevity and simplicity of each symptom‐diagnostic test for grief disorder to be indicative of its potential ease of use and clinical utility.
METHODS
Study sample
Data were obtained from the Yale Bereavement Study (YBS), a NIMH‐funded investigation designed to evaluate consensus criteria24 for disordered grief. The YBS was a longitudinal, interview‐based study of community‐dwelling bereaved individuals. It was approved by the institutional review boards of all participating sites. Written informed consent was obtained from all study participants. Interviews were conducted by master's degree‐level interviewers trained by YBS investigators. Interviewers were required to demonstrate nearly perfect agreement (kappa ≥0.90) with the YBS investigators for diagnoses of psychiatric disorders and PGD in five pilot interviews before being permitted to interview for the study. The YBS study is described in greater detail elsewhere1.
YBS participants (N=317) completed an initial baseline interview at an average of 6.3 ± 7.0 months post‐loss; first follow‐up interviews (N=296, 93.4% of participants) at an average of 10.9 ± 6.1 months post‐loss; and second follow‐up interviews (N=263, 83.0% of participants) at an average of 19.7 ± 5.8 months post‐loss. For analysis, data were restructured into more uniform time periods (0‐6 months, 6‐12 months, and 12‐24 months post‐loss).
The average age of participants was 61.8 ± 18.7 years. The majority of participants were female (73.7%), white (95.3%), educated beyond high school (60.4%), and spouses of the deceased (83.9%).
The present study sample (N=268; 84.5% of YBS participants) included participants interviewed at least once within 6‐12 months post‐loss and who provided sufficient information to evaluate PGD, CG, PCBD and proposed ICD‐11 tests for grief or bereavement disorder.
Grief symptoms (items)
Grief and bereavement‐related symptoms (items) were assessed with the rater‐version of the Inventory of Complicated Grief ‐ Revised (ICG‐R)25, a structured interview designed to assess a wide variety of potential grief and bereavement‐related symptoms, using five‐point scales to represent increasing levels of symptom severity.
The ICG‐R is a modification of the ICG18 that includes all the symptoms proposed by the consensus panel24 and additional symptoms enabling the testing of alternative diagnostic algorithms26.
The ICG‐R and the original ICG have proven to be reliable and valid18, 25. Based on prior work24, 25, a symptom was considered present if rated “4” or “5”, and absent if rated “1”, “2” or “3” on its five‐point scale.
Symptom‐diagnostic tests
The focus of the present investigation is restricted to symptom‐diagnostic tests for grief disorder (and not other tests or criteria for disorder, e.g. timing or impairment criteria).
Each of the tests under examination has two components, one including items that capture the essence of the syndrome (hereafter, referred to as “category A” items) and another including items that collectively capture the severity of the syndrome (hereafter, referred to as “category B” items).
Each of the tests described below was assessed at 6‐12 months post‐loss.
Prolonged grief disorder (PGD) test
The PGD symptom‐diagnostic test examined here is identical to the one introduced by Prigerson et al1. It includes eleven items represented directly in the ICG‐R. A positive test indicates endorsement of at least one of two category A items and at least five of nine category B items.
Complicated grief (CG) test
Formally, the proposed CG symptom‐diagnostic test15 consists of twelve (four category A and eight category B) items. However, several of these items contain multiple elements and therefore could be met in multiple ways. For example, the item “experiencing intense emotional or physiological reactivity to memories of the person who died or to reminders of the loss” could be met four ways, yet it is presented as a single item.
Nine of the twelve CG test items can be, and were, represented directly by one or more ICG‐R items. Two CG test items, i.e. “troubling rumination” and “emotional or physiological reactivity”, can be, and were, approximated by ICG‐R items. The CG test “troubling rumination” item (i.e., “frequent troubling rumination about circumstances or consequences of the death, such as concerns about how or why the person died or about not being able to manage without their loved one, thoughts of having let the deceased person down, and others”) was approximated by the ICG‐R “preoccupation” item (i.e., “do you ever have trouble doing the things you normally do because you are thinking about [the person who died] so much?”). The CG test “emotional or physiological reactivity” item (i.e., “experiencing intense emotional or physiological reactivity to memories of the person who died or to reminders of the loss”) was approximated by the ICG‐R “memories upset you” item (i.e., “do memories of [the person who died] ever upset you?”). One CG test item contained an element of survivor guilt, which can be, and was, represented directly by the ICG‐R “survivor guilt” item, and an element of suicidal ideation, which was represented by a positive screen for suicidal ideation using the Yale Evaluation of Suicidality27.
Because we decided to use the ICG‐R “preoccupation” item to represent the CG test “troubling rumination” item, and to avoid a double counting of this symptom, we chose to count this item only once as “troubling rumination” and not also doubly as “preoccupation”. Whether this item was counted as “preoccupation” (in category A) or “troubling rumination” (in category B) had no impact on results of the CG test in the present sample. Therefore, in the present investigation, a positive CG test indicates endorsement of at least one of three category A items (i.e., excluding the fourth, operationally redundant, “preoccupation” item) and at least two of eight category B items.
DSM‐5 persistent complex bereavement disorder (PCBD) test
The proposed PCBD symptom‐diagnostic test16 consists of sixteen (four category A and twelve category B) items.
Thirteen of the sixteen PCBD test items can be, and were, represented directly by one or more ICG‐R items. Two PCBD test items can be, and were, approximated by ICG‐R items. The PCBD test “difficulty in positive reminiscing about the deceased” item was approximated by the ICG‐R “do memories of [the person who died] ever upset you?” item. The PCBD test “maladaptive appraisals about oneself in relation to the deceased or the death (e.g., self‐blame)” item was approximated by the ICG‐R “do you feel at all guilty for surviving, or that it is unfair that you should live when [the person who died] died?” item. One PCBD test item reflects suicidal ideation and was represented by a positive screen for suicidal ideation using the Yale Evaluation of Suicidality.
In the present study, and consistent with the DSM‐5 proposal16, a positive PCBD test indicates endorsement of at least one of four category A items and at least six of twelve category B items.
ICD‐11 prolonged grief disorder (ICD‐11) test
An “ICD‐11 version” of the PGD symptom‐diagnostic test was constructed based on a narrative proposal for the diagnostic assessment of PGD for ICD‐1113. This narrative proposal includes seven (two category A and five category B) items that are represented directly in the ICG‐R and that have been found to be informative and unbiased in the empirical evaluation of items presented in Prigerson et al1.
The proposal did not include specification of a symptom threshold, i.e. a minimum number of items (symptoms) required to satisfy the symptom criterion. Therefore, we conducted a receiver operating characteristic (ROC) analysis28 to determine an optimum symptom threshold.
Based on the results of this analysis, in the present study, a positive “ICD‐11” test indicates endorsement of at least one of two category A items and at least three of five category B items. Presenting with at least three of five category B items was associated with a sensitivity of 83.3% and a specificity of 96.2%. Presenting with at least two of five items yielded lower specificity (sensitivity = 100%, specificity = 87.0%), while presenting with at least four of five items yielded much lower sensitivity (sensitivity = 60.0%, specificity = 99.6%).
Criterion standard to evaluate diagnostic properties of tests
The criterion standard used to establish absence or presence of grief disorder in the present sample is the one developed, employed and described in detail in Prigerson et al1.
Construction of this criterion standard combined elements of clinical judgment, reflected in raters’ diagnoses of disordered grief, with sophisticated measurement techniques. Employing methods from item response theory29, scores from a two‐parameter logistic (2‐PL) item response model (IRM) for grief intensity – based on twelve informative unbiased ICG‐R items (symptoms) – were used to order individuals based on the severity of their grief symptoms. An optimum minimum symptom severity threshold “cutoff” score, representing a metric boundary between cases and non‐cases of disordered grief, was then determined by varying this “cutoff” score to find a point of maximum agreement between rater diagnoses of disordered grief and cases identified by means of grief intensity scores.
Outcomes employed to evaluate predictive validity of positive tests
Potential adverse outcomes following from disordered grief, i.e. subsequent other mental disorders, suicidal ideation, functional impairment, and low quality of life, were each assessed at 12‐24 months post‐loss.
Mental disorders were assessed using the Structured Clinical Interview for DSM‐IV (SCID) Non‐Patient Version30. They included generalized anxiety disorder, post‐traumatic stress disorder and major depressive disorder. Research has supported the reliability and validity of SCID diagnoses31.
Positive responses to one or more of the four Yale Evaluation of Suicidality screening questions were categorized as having suicidal ideation.
The Established Populations for Epidemiological Studies of the Elderly32 measured performance of activities of daily living33 and physical functioning34. Individuals with at least ‘‘some difficulty’’ with at least one of the fourteen tasks (e.g., bathing) were considered functionally impaired in order to make the measure sensitive to impairment in a highly functioning sample.
Scores less than 5 (below the lowest quartile) on the Medical Outcomes Short‐Form35 indicated inferior quality of life.
Statistical analysis
Pairwise agreement between tests was assessed and evaluated using kappa statistics36, 37. The diagnostic sensitivity and specificity of each test was evaluated in relation to the criterion standard. The predictive validity of each symptom‐diagnostic test (evaluated between 6 to 12 months post‐loss) was examined using logistic regression models for the examined outcomes (evaluated between 12 to 24 months post‐loss) within strata defined by the absence/presence of other mental disorders at the time of the test. Suicidal ideation was not considered to be a potential outcome for either the CG or PCBD tests, because each of these tests included suicidal ideation as an item.
RESULTS
Table 1 presents the items employed in each test. Of the combined total of twenty items, the PGD test uses eleven, the CG test eighteen, the PCBD test fifteen, and the ICD‐11 test seven.
Table 1.
Items included in symptom‐diagnostic tests
| PGD | CG | PCBD | ICD‐11 | |||||
|---|---|---|---|---|---|---|---|---|
| Symptom (Item) | Category | Item | Category | Item | Category | Item | Category | Item |
| Yearning | A | 1 | A | 1 | A | 1, 2 | A | 1 |
| Preoccupation | A | 2 | B | 1 | A | 3, 4 | A | 2 |
| Part of yourself died | B | 1 | B | 11 | B | 2 | ||
| Disbelief; Trouble accepting death | B | 2 | B | 2 | B | 1 | B | 1 |
| Avoidance of reminders | B | 3 | B | 8 | B | 6 | ||
| Hard to trust others | B | 4 | B | 5 | B | 8 | ||
| Anger; Bitterness | B | 5 | B | 4 | B | 4 | B | 3 |
| Difficulty moving on | B | 6 | B | 12 | B | 5 | ||
| Numbness | B | 7 | B | 3 | B | 2 | ||
| Life empty, meaningless, unfulfilling | B | 8 | A | 2 | B | 10 | ||
| Stunned | B | 9 | B | 3 | B | 2 | ||
| Loneliness | A | 2 | B | 9 | ||||
| Survivor guilt | A | 3 | B | 5 | B | 4 | ||
| Suicidal ideation | A | 3 | B | 7 | ||||
| Inability to care | B | 5 | ||||||
| Envious of others without loss | B | 5 | ||||||
| Symptoms of deceased | B | 6 | ||||||
| Hear or see deceased | B | 6 | ||||||
| Memories upset you | B | 7 | B | 3 | ||||
| Drawn to places | B | 8 | ||||||
PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
CG employs two items previously reported to be biased1: loneliness (reported to be biased with respect to gender, relationship to diseased, and time from loss) and inability to care (reported to be biased with respect to relationship to diseased). It also uses three items (envy, upsetting memories, and drawn to places) previously reported to be uninformative1, and one item (suicidal ideation) that might be characterized as a correlate or consequence of prolonged, intense grief rather than a symptom of grief.
PCBD employs one reportedly biased item (loneliness)1, one reportedly uninformative item (upsetting memories)1, and one item (suicidal ideation) better characterized as a correlate or consequence of prolonged, intense grief1.
Neither PGD nor ICD‐11 employs reportedly biased or uninformative items, and neither employs correlates or consequences of prolonged, intense grief as items.
Figure 1 displays the point prevalence rate of disorder at 6‐12 months post‐loss for each test. The prevalence rates for PGD, CG, PCBD and ICD‐11 were, respectively, 11.9% (95% CI: 8.1%‐15.8%), 30.2% (95% CI: 24.7%‐35.7%), 14.2% (95% CI: 10.0%‐18.4%), and 12.7% (95% CI: 8.7%‐16.7%). There were no statistically significant pairwise differences in prevalence rates between PGD, PCBD and ICD‐11 diagnoses (all pairwise p values >0.05), while the prevalence rate for CG diagnosis was significantly higher than those for PGD, PCBD and ICD‐11 diagnoses (all pairwise p values <0.001).
Figure 1.
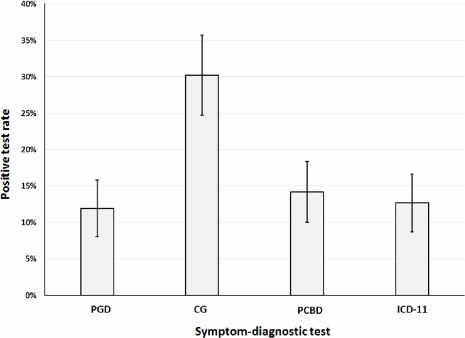
Positive symptom‐diagnostic test rates (N=268). PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Table 2 presents pairwise agreement between the four tests. The PGD, PCBD and ICD‐11 tests were in almost perfect agreement with each other (with pairwise kappa ranging from 0.80 to 0.84). The CG test was in moderate agreement with each of the other tests (with pairwise kappa ranging from 0.48 to 0.55).
Table 2.
Pairwise agreement (kappa) between symptom‐diagnostic tests (N=268)
| Test | PGD | CG | PCBD | ICD‐11 |
|---|---|---|---|---|
| PGD | 1.00 | |||
| CG | 0.48 | 1.00 | ||
| PCBD | 0.80 | 0.55 | 1.00 | |
| ICD‐11 | 0.83 | 0.50 | 0.84 | 1.00 |
PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Kappa values indicating almost perfect agreement are highlighted in bold prints
Table 3 displays properties of each test, and in particular each test's diagnostic specificity, in relation to the criterion standard. The PGD, PCBD and ICD‐11 tests had high and comparable diagnostic specificity, with values of 98.3%, 95.0%, and 96.2%, respectively. The CG test had 78.6% diagnostic specificity. The positive predictive value of the CG test was 37.0%, considerably lower than those for the PGD (87.5%), PCBD (68.4%), and ICD‐11 (73.5%) tests. Figure 2 highlights the tradeoff between diagnostic sensitivity and diagnostic specificity for each of the four tests.
Table 3.
Diagnostic sensitivity and specificity of the tests in relation to the criterion standard (N=268)
| Test | True positive | False positive | True negative | False negative | Positive predictive value | Negative predictive value | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|---|
| PGD | 28 | 4 | 234 | 2 | 87.5% | 99.2% | 93.3% | 98.3% |
| CG | 30 | 51 | 187 | 0 | 37.0% | 100.0% | 100.0% | 78.6% |
| PCBD | 26 | 12 | 226 | 4 | 68.4% | 98.3% | 86.7% | 95.0% |
| ICD‐11 | 25 | 9 | 229 | 5 | 73.5% | 97.9% | 83.3% | 96.2% |
PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Figure 2.
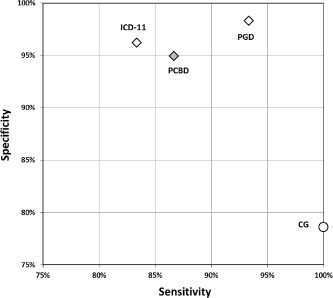
Symptom‐diagnostic test specificity versus sensitivity (N=268). PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Tables 4 and 5 present an examination of the predictive validity of each of the four tests in terms of four subsequent (12‐24 months post‐loss) adverse outcomes, i.e., other mental disorders (major depressive disorder, post‐traumatic stress disorder or generalized anxiety disorder), suicidal ideation, functional impairment, and low quality of life, stratified by absence/presence of concurrent (6‐12 month post‐loss) mental disorders.
Table 4.
Predictive validity of symptom‐diagnostic tests in the absence of other mental disorders (N=213)
| Outcome (12‐24 months post‐loss) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Test | Other mental disorders | Suicidal ideation | Functional impairment | Low quality of life | ||||
| (6‐12 months post‐loss) | RR | p | RR | p | RR | p | RR | p |
| PGD | 4.40 | 0.048 | 3.06 | 0.017 | 2.08 | 0.001 | 3.40 | 0.001 |
| CG | 2.90 | 0.101 | – | – | 0.98 | 0.926 | 1.08 | 0.834 |
| PCBD | 3.52 | 0.097 | – | – | 1.61 | 0.058 | 2.68 | 0.006 |
| ICD‐11 | 3.52 | 0.097 | 5.04 | 0.001 | 2.07 | 0.001 | 3.23 | 0.001 |
PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Other mental disorders considered were major depressive disorder, post‐traumatic stress disorder and generalized anxiety disorder
Suicide ideation is not considered as a potential outcome for CG and PCBD, because they include suicidal ideation as an item
Statistically significant values are highlighted in bold prints
Table 5.
Predictive validity of symptom‐diagnostic tests in the presence of other mental disorders (N=27)
| Outcome (12‐24 months post‐loss) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Test | Other mental disorders | Suicidal ideation | Functional impairment | Low quality of life | ||||
| (6‐12 months post‐loss) | RR | p | RR | p | RR | p | RR | p |
| PGD | 4.00 | 0.039 | 2.00 | 0.121 | 0.80 | 0.480 | 1.03 | 0.930 |
| CG | 3.14 | 0.221 | – | – | 0.86 | 0.655 | 0.86 | 0.655 |
| PCBD | 3.44 | 0.065 | – | – | 0.69 | 0.228 | 0.88 | 0.697 |
| ICD‐11 | 4.64 | 0.022 | 1.67 | 0.203 | 0.93 | 0.816 | 1.19 | 0.586 |
PGD – prolonged grief disorder test (original version), CG – complicated grief test, PCBD – persistent complex bereavement disorder test, ICD‐11 – prolonged grief disorder test (ICD‐11 proposed version)
Other mental disorders considered were major depressive disorder, post‐traumatic stress disorder and generalized anxiety disorder
Suicide ideation is not considered as a potential outcome for CG and PCBD, because they include suicidal ideation as an item
Statistically significant values are highlighted in bold prints
Among individuals without other mental disorders at 6‐12 months post‐loss (Table 4), positive PGD tests were significantly associated with other mental disorders (RR=4.40, p=0.048), suicidal ideation (RR=3.06, p=0.017), functional impairment (RR=2.08, p<0.001), and low quality of life (RR=3.40, p<0.001) at 12‐24 months post‐loss. Positive PCBD tests were associated with low quality of life (RR=2.68, p=0.006) at 12‐24 months post‐loss; and positive ICD‐11 tests were associated with suicidal ideation (RR=5.04, p<0.001), functional impairment (RR=2.07, p<0.001), and low quality of life (RR=3.23, p<0.001) at 12‐24 months post‐loss.
Among individuals with other mental disorders at 6‐12 months post‐loss (Table 5), positive PGD and ICD‐11 tests were each significantly related to other mental disorders (PGD: RR=4.00, p=0.0.039; ICD‐11: RR=4.64, p=0.022) at 12‐24 months post‐loss.
Positive CG tests were not significantly associated with other mental disorders, functional impairment and low quality of life at 12‐24 months post‐loss, either in the absence (Table 4) or in the presence (Table 5) of concurrent (6‐12 months post‐loss) mental disorders.
DISCUSSION
This study aimed to determine whether the differences between PGD, CG and PCBD are substantive or merely semantic. Our results indicate that there is no substantive difference between PGD and PCBD. The high level of agreement between the PGD, PCBD and proposed ICD‐11 tests; their similarly low estimates of rate of disorder (∼10%) in this community population; their comparably high levels of diagnostic specificity, and their comparable predictive validity, all suggest that PGD and PCBD identify the same diagnostic entity. Therefore, the difference between PGD and PCBD is mainly semantic. In contrast, the CG test had only moderate agreement with the PGD, PCBD and proposed ICD‐11 tests, a three‐fold higher estimate of rate of disorder (∼30%) in this community sample, much poorer diagnostic specificity, and no predictive validity. Therefore, the difference between PGD and PCBD on the one hand, and CG on the other, is substantive.
Given that PGD and PCBD tests identify the same diagnostic entity, the main difference between PGD (proposed for adoption in ICD‐11) and PCBD (introduced in DSM‐5) is in the meaning of terms used to describe this same entity. The primary opposition is between use of the term “grief” and use of the term “bereavement” in the name of the disorder. Grief is deep mental anguish, a process of the psyche. Bereavement is an event, the loss of a valued loved‐one due to death. Grief is a mental entity; bereavement is not. At face value, there is no mental entity identified in the name PCBD. How can the name of a mental disorder not identify a mental entity?
The use of the term “complex” in the name PCBD is also somewhat obfuscating. The PGD construct is fairly simple to understand: individuals who are “stuck” in a state of intense grief for a long time have PGD. If the underlying disorder is not difficult to understand, then what is “complex” about PCBD? The name PCBD has no clear meaning and should be abandoned by the DSM in favor of PGD. Even if the DSM retains this name, researchers, clinicians and the general public should understand that there is no substantive difference between what the DSM calls PCBD and what the ICD calls PGD.
Disagreement between the CG test on the one hand, and the PGD and PCBD tests on the other, combined with the CG test's limited specificity (78.6%), poor positive predictive value (only 37.0%), and lack of predictive validity, suggest that the CG test is not a valid indicator of a grief‐specific disorder. Indeed, in the current study sample, a majority of individuals with positive CG tests had negative PGD (original version), PCBD, and PGD (version proposed for ICD‐11) tests. For this reason, treatment studies based on samples defined in terms of the CG may be of questionable value for a grief‐specific disorder devoid of the CG “contaminants”.
The fact that one test includes a different set of items than another test does not necessarily imply that the two tests are grounded in different constructs or identify different disorders. Tests for PGD (both the original version and the one proposed for ICD‐11) and PCBD are different but essentially equivalent measures of a single, underlying attribute, i.e. intense grief, and should be viewed as such. The notion that symptoms of grief are normal but that a combination of their high intensity and long duration is abnormal reconciles the belief that all grief symptoms are normal, but not all grieving processes are normal. This view, rooted in the uni‐dimensionality of the underlying grief construct, is in opposition to the notion that some symptoms are normal and others are atypical and abnormal, i.e., that pathology is expressed in the form of atypical symptoms. Current and future alternative symptom‐diagnostic tests should be evaluated in terms of specificity, accuracy, parsimony, and perhaps in reference to external validity; not in terms of whether or not individual items on the test define the pathology.
Inclusion of biased items and external correlates of PGD (e.g., suicidal thoughts) in a criteria set for grief disorder is questionable on psychometric and conceptual grounds. The tests for CG and PCBD contain items that were previously identified to be biased1. In particular, the loneliness item included in both of these tests has been reported to be biased not only with respect to the bereaved individual's gender and relationship to the deceased, but also with respect to time from loss. Although inclusion of one or even a few biased items in a multi‐item test does not necessarily mean that the test as a whole is biased, inclusion of biased items opens the possibility that some groups of individuals may be misdiagnosed by the test due to misinterpretation of the severity of their symptoms. For example, for bereaved spouses, loneliness is a moderate symptom, whereas for bereaved non‐spouses, loneliness is a significantly more severe symptom of grief. Inclusion of the loneliness item in a diagnostic test for a disorder of grief makes it more likely that a bereaved spouse would be mistakenly diagnosed with that disorder due to a misinterpretation of the severity of his/her loneliness symptom. The tests for CG and PCBD also include an external correlate or consequence of PGD, i.e. suicidal thoughts, as an item. Suicidality may be related to grief disorder, but to include it as a symptom that represents grief is to misunderstand what grief is, and to confound the essence of the syndrome with its consequences.
In order to include an “ICD‐11 version” of a symptom‐diagnostic test for PGD in the present analysis, we needed to specify a symptom threshold. The current narrative proposal13 for an ICD‐11 version of PGD does not make this specification. In an effort to develop diagnostic guidelines that accommodate flexible exercise of clinical judgment, the WHO discourages methods of diagnostic assessment that employ arbitrary thresholds and “pick lists” of items, but supports the use of symptom thresholds that have been established empirically38. Based on results of the ROC analysis in this study, presenting with at least three of the proposed five accessory symptoms represents an optimum balance of diagnostic sensitivity and specificity in relation to our criterion standard. For this reason we recommend that future ICD‐11 research diagnostic criteria include this “at least three of five” accessory symptom rule for diagnosing cases of PGD. The brief, five‐item “ICD‐11 version” of the PGD test also has the advantage that short tests have over longer ones for ease of use and clinical utility21, 22, 23.
The present study evaluates the performance of symptom‐diagnostic tests for grief disorder applied within a period of 6 to 12 months post‐loss. This is consistent with empirical evidence that presence of enduring, intense grief beyond 6 months post‐loss is predictive of subsequent mental disorders, suicidal ideation, functional impairment, and worse quality of life1, and with proposed diagnostic criteria for PGD1, 13 and CG15. However, it is inconsistent with the DSM‐5 specification that PCBD ought not to be diagnosed within 12 months post‐loss. In our view, this DSM‐5 “time from loss” criterion is not only arbitrary but also contrary to published empirical research findings. In the present study, the PCBD test applied within 6 to 12 months post‐loss had near perfect agreement with PGD tests, had high specificity and sensitivity with respect to our criterion standard, and was predictive of subsequent (i.e., 12 to 24 month) worse quality of life. Based on these findings, the PCBD symptom‐diagnostic test applied within 6 to 12 months post‐loss is an empirically valid test for disorder notwithstanding the DSM‐5's arbitrary “at least 12 months’ time from loss” criterion for PCBD.
The present investigation has a few limitations that warrant some consideration. One limitation is that some ICG‐R items employed in the present analysis may not have mapped exactly onto some items in the proposed CG and PCBD tests. More formal instruments to assess CG and PCBD have been introduced only recently39, 40. These have yet to be established and validated in general community settings. The fact that our proxy PCBD symptom‐diagnostic test had high diagnostic specificity and sensitivity, as well as some predictive validity, suggests that some imprecision in our representation of some PCBD items did not undermine the validity of the overall PCBD test appreciably. Given the properties of the PGD and PCBD tests, future refinements in conceptualization and wording of items might be expected to make marginal improvements in what are already highly reliable and valid tests.
Another limitation of the present study is that the YBS sample represents mainly elderly, white widows living in a relatively small region of the US, whose spouses died primarily from natural causes. Future studies ought to examine whether and the extent to which properties of PGD and PGBD tests and items differ with respect to the bereaved individual's age, gender, race, ethnicity, relationship to the deceased, and geographic or cultural setting, as well as with respect to circumstances of the lost loved‐one's death.
The present study has a number of strengths. Most importantly, the YBS was designed explicitly to evaluate diagnostic criteria for disordered grief. YBS instrumentation included an extensive battery of grief items sufficient to compare the four symptom‐diagnostic tests included in the present analysis. YBS data were collected in a community sample, allowing us to evaluate methods of diagnostic assessment that are intended to discriminate between normal and disordered grief. Finally, the YBS's longitudinal design allowed us to examine the predictive validity of positive symptom‐diagnostic tests for disordered grief.
In conclusion, the PGD, PCBD and proposed ICD‐11 PGD symptom‐diagnostic tests identify a single, common diagnostic entity. Therefore, the main differences between PGD and PCBD are semantic, not substantive. The test for CG is incongruous with those for PGD and PCBD, has a poorer diagnostic specificity and no predictive validity. Clinical and scientific communities ought to recognize that PGD and PCDB are substantively the same disorder, and ought to work toward a common understanding of that disorder and adopt useful ways to recognize it clinically. The term “prolonged grief disorder” captures the essence of the disorder, facilitates understanding it, and thereby supports clinical judgment in its diagnostic assessment.
ACKNOWLEDGEMENTS
P.K. Maciejewski and H.G. Prigerson were supported by research grants MD007652 from the National Institute of Minority Health and Health Disparities, MH56529 from the National Institute of Mental Health, and CA106370 and CA197730 from the National Cancer Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. A. Maercker is chair of the ICD‐11 Working Group on Disorders Specifically Associated with Stress that developed the PGD proposal for the WHO. Unless specifically stated, the views expressed in this paper are those of this author and do not represent the official policies or positions of the WHO.
REFERENCES
- 1. Prigerson HG, Horowitz MJ, Jacobs SC et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM‐V and ICD‐11. PLoS Med 2009;6:e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Prigerson HG, Frank E, Kasl SV et al. Complicated grief and bereavement‐related depression as distinct disorders: preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry 1995;152:22‐30. [DOI] [PubMed] [Google Scholar]
- 3. Prigerson HG, Bierhals AJ, Kasl SV et al. Complicated grief as a disorder distinct from bereavement‐related depression and anxiety: a replication study. Am J Psychiatry 1996;153:1484‐6. [DOI] [PubMed] [Google Scholar]
- 4. Boelen PA, van den Bout J, de Keijser J. Traumatic Grief as a disorder distinct from bereavement‐related depression and anxiety: a replication study with bereaved mental health care patients. Am J Psychiatry 2003;160:1339‐41. [DOI] [PubMed] [Google Scholar]
- 5. Boelen PA, van den Bout J. Complicated grief, depression, and anxiety as distinct postloss syndromes: a confirmatory factor analysis study. Am J Psychiatry 2005;162:2175‐7. [DOI] [PubMed] [Google Scholar]
- 6. Golden AM, Dalgleish T. Is prolonged grief distinct from bereavement‐related posttraumatic stress? Psychiatry Res 2010;178:336‐41. [DOI] [PubMed] [Google Scholar]
- 7. Spuij M, Reitz E, Prinzie P et al. Distinctiveness of symptoms of prolonged grief, depression, and post‐traumatic stress in bereaved children and adolescents. Eur Child Adolesc Psychiatry 2012;21:673‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Horowitz MJ, Siegel B, Holen A et al. Diagnostic criteria for complicated grief disorder. Am J Psychiatry 1997;154:904‐10. [DOI] [PubMed] [Google Scholar]
- 9. Silverman GK, Jacobs SC, Kasl SV et al. Quality of life impairments associated with diagnostic criteria for traumatic grief. Psychol Med 2000;30:857‐62. [DOI] [PubMed] [Google Scholar]
- 10. Prigerson HG, Bierhals AJ, Kasl SV et al. Traumatic grief as a risk factor for mental and physical morbidity. Am J Psychiatry 1997;154:616‐23. [DOI] [PubMed] [Google Scholar]
- 11. Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults. Eur Arch Psychiatry Clin Neurosci 2007;257:444‐52. [DOI] [PubMed] [Google Scholar]
- 12. Maercker A, Brewin CR, Bryant RA et al. Proposals for mental disorders specifically associated with stress in the International Classification of Diseases‐11. Lancet 2013;381:1683‐5. [DOI] [PubMed] [Google Scholar]
- 13. Maercker A, Brewin CR, Bryant RA et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD‐11. World Psychiatry 2013;12:198‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zisook S, Shuchter SRX. Uncomplicated bereavement. J Clin Psychiatry 1993;54:365‐72. [PubMed] [Google Scholar]
- 15. Shear MK, Simon N, Wall M et al. Complicated grief and related bereavement issues for DSM‐5. Depress Anxiety 2011;28:103‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 5th ed Arlington: American Psychiatric Publishing, 2015. [Google Scholar]
- 17. Zisook S, Pies R, Corruble E. When is grief a disease? Lancet 2012;379:1590. [DOI] [PubMed] [Google Scholar]
- 18. Prigerson HG, Maciejewski PK, Reynolds CF et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res 1995;59:65‐79. [DOI] [PubMed] [Google Scholar]
- 19. Boelen PA, van den Bout J, de Keijser J et al. Reliability and validity of the Dutch version of the Inventory of Traumatic Grief. Death Stud 2003;27:227‐47. [DOI] [PubMed] [Google Scholar]
- 20. Simon NM, Wall MM, Keshaviah A et al. Informing the symptom profile of complicated grief. Depress Anxiety 2011;28:118‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Evans SC, Reed GM, Roberts MC et al. Psychologists' perspectives on the diagnostic classification of mental disorders: results from the WHO‐IUPsyS Global Survey. Int J Psychol 2013;48:177‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reed GM, Correia JM, Esparza P et al. The WPA‐WHO Global Survey of Psychiatrists’ Attitudes Towards Mental Disorders Classification. World Psychiatry 2011;10:118‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. First MB, Pincus HA, Levine JB et al. Clinical utility as a criterion for revising psychiatric diagnoses. Am J Psychiatry 2004;161:946‐54. [DOI] [PubMed] [Google Scholar]
- 24. Prigerson HG, Shear MK, Jacobs SC et al. Consensus criteria for traumatic grief. A preliminary empirical test. Br J Psychiatry 1999;174:67‐73. [DOI] [PubMed] [Google Scholar]
- 25. Prigerson HG, Jacobs S. Traumatic grief as a distinct disorder: a rationale, consensus criteria, and a preliminary empirical test In: Stroebe MS, Hansson RO, Stroebe W. et al (eds). Handbook of bereavement research: consequences, coping, and care. Washington: American Psychological Association, 2001:613‐45. [Google Scholar]
- 26. Horowitz MJ, Siegel B, Holen A et al. Diagnostic criteria for complicated grief disorder. Am J Psychiatry 1997;154:904‐10. [DOI] [PubMed] [Google Scholar]
- 27. Latham AE, Prigerson HG. Suicidality and bereavement: complicated grief as psychiatric disorder presenting greatest risk for suicidality. Suicide Life Threat Behav 2004;34:350‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Metz CE. Basic principles of ROC analysis. Semin Nucl Med 1978;8:283‐98. [DOI] [PubMed] [Google Scholar]
- 29. Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of items response theory. Newbury Park: Sage, 1991. [Google Scholar]
- 30. First MB, Spitzer RL, Gibbon M et al Structured Clinical Interview for DSM‐IV Axis I Disorders, Non‐Patient Version (SCID‐I/NP). New York: Biometrics Research Department, New York State Psychiatric Institute, 1995. [Google Scholar]
- 31. Williams JBW, Gibbon M, First MB et al. The Structured Clinical Interview for DSM‐III‐R (SCID): II. Multisite test‐retest reliability. Arch Gen Psychiatry 1992;49:630‐6. [DOI] [PubMed] [Google Scholar]
- 32. Cornoni‐Huntley J, Ostfeld AM, Taylor JO et al. Established populations for epidemiologic studies of the elderly: study design and methodology. Aging Clin Exp Res 1993;5:27‐37. [DOI] [PubMed] [Google Scholar]
- 33. Katz S, Downs TD, Cash HR et al. Progress in the development of an index of ADL. Gerontologist 1970;10:20‐30. [DOI] [PubMed] [Google Scholar]
- 34. Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q 1976;54:439‐67. [PubMed] [Google Scholar]
- 35. Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36): I. Conceptual framework and item selection. Med Care 1992;30:473‐82. [PubMed] [Google Scholar]
- 36. Cohen J. A coefficient of agreement for nominal scales. Ed Psychol Meas 1960;20:37‐46. [Google Scholar]
- 37. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159‐74. [PubMed] [Google Scholar]
- 38. First MB, Reed GM, Hyman SE et al. The development of the ICD‐11 Clinical Descriptions and Diagnostic Guidelines for Mental and Behavioural Disorders. World Psychiatry 2015;14:82‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bui E, Mauro C, Robinaugh DJ et al. The Structured Clinical Interview for Complicated Grief: reliability, validity, and exploratory factor analysis. Depress Anxiety 2015;32:485‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lee SA. The Persistent Complex Bereavement Inventory: a measure based on the DSM‐5. Death Stud 2015;39:399‐410. [DOI] [PubMed] [Google Scholar]


