Abstract
Rates of suicide are alarmingly high in military and veteran samples. Suicide rates are particularly elevated among those with post-traumatic stress disorder (PTSD) and depression, which share overlapping symptoms and frequently co-occur. Identifying and confirming factors that reduce suicide risk among veterans with PTSD and depression is imperative. The proposed study evaluated whether post-deployment social support moderated the influence of PTSD-depression symptoms on suicidal ideation among veterans returning from Iraq and Afghanistan using state of the art clinical diagnostic interviews and self-report measures. Operations Enduring and Iraqi Freedom (OEF/OIF) veterans (n=145) were invited to participate in a study evaluation returning veterans’ experiences. As predicted, PTSD-depression symptoms had almost no effect on suicidal ideation (SI) when post-deployment social support was high; however, when post-deployment social support was low, PTSD-depression symptoms were positively associated with SI. Thus, social support may be an important factor for clinicians to assess in the context of PTSD and depressive symptoms. Future research is needed to prospectively examine the interrelationship between PTSD/depression and social support on suicidal risk, as well as whether interventions to improve social support result in decreased suicidality.
1.) Introduction
A substantial proportion of Veterans returning from service in Operations Enduring and Iraqi Freedom (OEF/OIF) experience psychological symptoms associated with increased risk for suicidal behavior (Jakupcak et al., 2010; Pietrzak et al., 2010). Rates of completed suicide in OEF/OIF military service members and Veteran populations are alarmingly high (Kang and Bullman, 2008; Blow et al., 2012; McCarthy et al., 2012). Recent statistics from 2012 data indicate that 22 Veterans commit suicide per day (U.S. Department of Veterans Affairs, 2013). Additionally, while Veterans represent 1% of the population, they comprise 22% of all completed suicides in the United States (U.S. Department of Veterans Affairs, 2012). These statistics are concerning and further research is necessary to identify risk factors for suicide in this population. Although some suicides are completed impulsively, prior research demonstrates that expressed suicidal ideation (SI) predicts completed suicide attempts (Schneider et al., 2001; Angst et al., 2002). Thus, identification and confirmation of key risk factors for SI is crucial in pinpointing targets for prevention and intervention.
Multiple risk factors are associated with increased SI among OEF/OIF Veterans including: posttraumatic stress disorder (PTSD), major depressive disorder (MDD), traumatic brain injury, problematic alcohol use, psychosocial problems, history of physical or sexual abuse, stigma, barriers to care, lower resilience, lower social support, and current psychotic disorder (Jakupcak et al., 2009; Pietrzak et al., 2010; Brenner et al., 2011; Lamaire and Graham, 2011). Two of these risk factors, PTSD and MDD, are highly prevalent, share several overlapping symptoms, and frequently co-occur among OEF/OIF Veterans (Seal et al., 2007; Koenen et al., 2008). Notably, Veterans with PTSD or MDD have significantly elevated risk of SI (Jakupcak, et al., 2009; Bryan and Corso, 2011; Pukay-Martin et al., 2012; Rudd et al., 2011), although the data are mixed as to whether their co-occurrence does (Oquendo et al., 2003; Pukay-Martin et al., 2012) or does not (Jakupcak et al., 2009; Guerra and Calhoun, 2011; Lemaire and Graham, 2011) synergistically escalate risk for SI. Recent evidence suggests that, among trauma-exposed samples, these two disorders may actually be better represented by a single dimension, rather than as two separate disorders (Miller et al., 2008; Elhai et al., 2011). Specifically, in a sample of combat Veterans, a series of confirmatory factor analyses across all DSM-III diagnoses revealed that a 3-factor model best fit the data, an anxious-misery factor made up of PTSD and MDD symptoms, a fear factor, comprised of other anxiety disorders such as panic disorder and obsessive compulsive disorder, and an externalizing factor, consisting of antisocial personality disorder and substance use disorders (Elhai et al., 2008). Additionally, among Veterans diagnosed with either PTSD or MDD, scores on self-reported PTSD symptom scales were similar, suggesting that there are fewer differences than the diagnostic categories suggest (Gros et al., 2012). Thus, both PTSD and MDD loaded onto one factor, suggesting that they may be better represented via a single dimension in trauma-exposed samples.
Several factors mitigate against suicide risk, including increased social support, being married, and having a sense of purpose and control (Jakupcak et al., 2010; Lemaire and Graham, 2011; Pietrzak et al., 2011). Perceived social support (i.e., perceptions of available social support, as opposed to the number of people with whom a person is in contact) is consistently linked to reduced SI. Perceived social support in the post-deployment phase appears to be a critical factor that buffers against risk for suicide and contributes to recovery from PTSD and depression in OEF/OIF Veterans (Jakupcak et al., 2010; Pietrzak et al., 2010, Pietrzak et al., 2011).
Veterans who screened positive for PTSD experience lower rates of partner satisfaction, family cohesion, and social functioning (Tsai et al., 2012). Among OIF/OEF Veterans, social support buffers against SI, though this protective effect is reduced among those with a diagnosis of PTSD or depression (Jakupcak et al., 2010; Pietrzak et al., 2011). Thus, examining interactions among mental health symptoms and social support is imperative to inform prevention and intervention efforts aimed at decreasing Veterans’ risk for suicide.
1.1 Objective and Hypothesis
The current study examined whether perceived post-deployment social support (a modifiable risk factor) moderates the relationship between a PTSD-depression factor and SI among OEF/OIF Veterans. This study improves upon prior work in this area by utilizing clinical interviews and self-report measures that have strong psychometric properties. It was hypothesized that the effect of PTSD-depression symptoms on SI would be strongest among Veterans with low social support and weakest among Veterans with high social support.
2.) Methods
2.1 Participants
Within the Central Texas Veterans Health Care System (CTVHCS), OEF/OIF Veterans (N = 145) were recruited to participate in a study that assessed warzone experiences and post–deployment adjustment. Participants were recruited through advertisements at recruitment sites and Veterans’ service organizations, in-service presentations to VA staff (e.g., primary care, mental health, and OEF/OIF program), and mailings to OEF/OIF Veterans enrolled in the CTVHCS system. Participants were eligible if they were: (a) an OEF/OIF Veteran; (b) able to provide informed consent; and (c) able to complete the full assessment battery. Participants were excluded if they met the following criteria: (a) a diagnosis of bipolar or psychotic disorder; (b) recently began (i.e., had not reached stabilization) psychiatric medications or psychotherapy; or (c) suicidal or homicidal ideation, intent or plan warranting crisis intervention. Initial eligibility was determined via a phone screen, which assessed for OEF/OIF Veteran status, suicidal or homicidal ideation warranting crisis intervention, and status of psychiatric treatment. While severe suicidal or homicidal ideation was listed in the exclusion criteria because the study investigators felt that crisis intervention was more important than participating in the study at such time, no participants were excluded based on this criterion. Screening for bipolar disorder and schizophrenia via the MINI (Mini International Neuropsychiatric Interview; Sheehan et al., 1998) was conducted at the beginning of the clinical interview to determine final eligibility. Based on these inclusion/exclusion criteria, 15 participants were deemed ineligible resulting in a final sample of 130 eligible participants.
The mean age of the final sample was 38.0 years (SD = 10.76). Participants were primarily male (84.6%). Within the sample, 26.0% identified as Hispanic, 63.4% as Caucasian, 17.9% as African-American, 0.8% as Hawaiian/Pacific Islander, and 8.9% as “Other” (categories were not mutually exclusive). The mean education level of the sample was 14.1 years (SD = 2.5 years). The majority of participants served in the Army (82.3%). In addition, 4.7% served in the Air Force, 8.6% in the Marine Corps and 6.3% in the Navy (categories were not mutually exclusive). Further, most Veterans served in active duty (95.3%), while 46.1% served in the reserves and 16.4% served in the National Guard (categories were not mutually exclusive). Participants identified their rank at discharge as: 32.0% E1–E4, 38.4% E5–E6, 16.8% E7–E9, 4.8% O1–O3, 6.4% O4–O9, 1.6% WO1–WO5.
2.2 Procedures
Study procedures were approved by the local Institutional Review Board. Veterans were screened for initial eligibility via telephone after providing informed verbal consent. Veterans were then scheduled for a face-to-face assessment, during which written informed consent was obtained and final eligibility confirmed. Veterans completed a clinical interview to diagnose PTSD and depression, and screen for psychosis and bipolar disorder (exclusion criteria). They also completed several self-report measures to ascertain basic demographic information, history of military service, and symptoms of PTSD, depression, and SI.
2.3 Measures
2.3.1 Inclusion/Exclusion Criteria
The Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) is a clinician-administered diagnostic assessment for Axis I disorders. Sections of the MINI were employed to screen for bipolar disorder and psychotic disorders.
2.3.2 Demographic Information
A demographic questionnaire was created for the current study to assess participant characteristics including age, gender, race and ethnicity, relationship status, cohabitation status, education, employment, income and military service characteristics.
2.3.3 PTSD symptoms
The Clinician Administered PTSD Scale (CAPS; Blake et al., 1995) is a semi-structured diagnostic interview. The CAPS assesses the intensity and frequency of the 17 symptoms of PTSD as defined by DSM-IV. In the current study, the CAPS focused on traumatic events related to an OEF/OIF deployment. If the participant was unable to identify a potentially traumatic event during their service in OEF/OIF that met full Criterion A, the CAPS was conducted on the event that met Criterion A1 (i.e., an event involving actual or threatened death or serious injury, or a threat to the physical integrity of self or others) identified by the participant as being the worse event. In the rare instances in which no such event was identified, the CAPS was administered based on general deployment-related stress. In this manner, a continuous PTSD symptom score could be derived for all participants. Participants were queried regarding their symptoms during the past 30 days as well as a past month when participants identified symptoms as being most severe. The CAPS yields both a categorical PTSD diagnosis and a continuous symptom severity score. Of the total sample, 116 participants (89.2%) met criterion A. Internal consistency in the current study was 0.98.
The PTSD Checklist-Military Version (PCL-M; Forbes et al., 2001) is a 17-item self-report measure that assesses military-related PTSD symptoms during the past month according to the DSM–IV–TR (American Psychological Association, 2000). The PCL-M has outstanding validity and internal consistency (Blanchard et al., 1996). Prior research supports the utility of using both clinician-administered and self-report measures of PTSD with war Veterans (Kulka et al., 1991). A prior report from the current study indicated that PCL-M scores are more strongly associated with recent, non-traumatic life stressors than CAPS scores (Meyer et al., 2013). This suggests that self-reported PCL-M scores tap cumulative responses to traumatic stress as well as to non-traumatic stressors among returning war Veterans, which is likely relevant for understanding risk for suicide. Internal consistency for the PCL-M in the current study was 0.96.
2.3.4 MDD Symptoms
The Anxiety Disorders Interview-IV (ADIS-IV; Di Nardo et al., 1994) is a semi-structured clinician administered interview that was used to assess DSM-IV MDD symptoms. The ADIS-IV has demonstrated good reliability and good inter-rater reliability (Brown et al., 2001)
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996) is a frequently-used 21-item measure of depressive symptoms. Participants rate current depressive symptoms on a Likert scale of 0 (no depressive symptoms) to 3 (severe depressive symptoms). A score of 0–9 indicates minimal depression, 10–18 represents mild depression, 19–29 is indicative of moderate depression, and scores above 30 are considered severe depression (Beck et al., 1988). The BDI-II has demonstrated high internal consistency (Beck et al., 1996) and good test-retest reliability (Beck et al., 1996). In the current data analyses, the BDI-II item assessing SI and intent was removed in order to eliminate overlap between the predictor (depressive symptoms) and outcome variable (SI). Internal consistency for the scale in the current study was 0.96.
2.3.5 Suicidal Ideation
The Beck Scale for Suicide Ideation (BSS) is a 19-item self-report instrument that assesses thoughts, behaviors and plans to commit suicide during the past week (Beck et al., 1988; Beck and Steer, 1991; Steer, Kumar and Beck, 1993). Participants rate items on a 3-point Likert scale ranging from 0 (least severe or low suicidal intensity) to 2 (most severe or high suicidal intensity). The internal reliability, test retest stability and concurrent validity of this measure have been established (Beck and Steer, 1991; Steer et al., 1993; Beck et al., 1998). Internal consistency for the scale in the current study was 0.91.
2.3.6 Social Support
The post-deployment social support scale (PDSS) is a 15-item self-report measure from the Deployment Risk and Resilience Inventory, a set of scales that assess risk and resilience factors related to deployment in military personnel and Veterans and are designed to be used as stand-alone measures (DRRI; King et al., 2006; Vogt et al., 2008). The DRRI scales are validated for use with OEF/OIF Veterans (Vogt et al., 2008). The PDSS assesses perceived emotional and instrumental (i.e., tangible social support, such as providing resources) forms of social support from family, friends, employers and the community following deployment. There is also a 9-item version of the measure. Thirty-one participants completed the 9-item version, as the 15-item was not yet available when the study started, and scores were combined across versions. The 9-item and 15-item scales correlated highly, r = 0.96, p < 0.001. Internal consistency for the 15-item version of PDSS was 0.83, and internal consistency for the 9-item scale was 0.71.
3.) Results
Approximately 42% (n = 54) of the sample met full diagnostic criteria for current military-related PTSD at the time of the assessment, and 30% (n = 39) met full diagnostic criteria for current MDD. Consistent with prior research demonstrating high rates of comorbidity between PTSD and depression (e.g., Gros et al., 2012), 57% (31/54) of participants with PTSD also met criteria for MDD, whereas 80% (31/39) of participants with MDD also met criteria for PTSD. Thus, PTSD, MDD, and co-occurring PTSD-MDD were well represented in the sample. There was a high correlation between CAPS and BDI scores, r = 0.76, p < 0.001 as well as PCL-M and BDI scores, r = 0.80, p < 0.001. The correlation between the CAPS and PCL-M was r = 0.79, p < 0.001.
In the total sample, 18.5% endorsed suicidal ideation on the BSS. The mean score was 1.16 (SD = 3.57), and scores ranged from 0 to 21. Among the subset of participants (n = 62) with PTSD and/or MDD, 24.1%, (n = 15) endorsed suicidal ideation (mean = 2.15, SD = 4.74). BSS data were positively skewed and kurtotic. Thus, BSS scores were log transformed, which reduced both skewness and kurtosis. A small amount (2.9%) of the item-level BSS data were missing, which was addressed by substituting the mean item score.
3.1 Factor Analysis
Given high rates of co-occurrence of PTSD and MDD in both the current sample and prior research (e.g., Miller et al., 2008; Elhai et al., 2011; Gros et al., 2012), as well as evidence for a higher-order PTSD-depression factor from factor analytic studies (e.g., Miller et al., 2008), principal component analysis (PCA) was used to create a composite PTSD-depression factor from the CAPS total symptom severity score, PCL-M, and BDI-II. A single factor accounting for 85% of the variance in these measures was extracted. All three measures loaded highly onto the PTSD-depression composite factor (CAPS = .92, PCL-M = .93, BDI-II = .92), providing strong evidence for a single, underlying factor. Accordingly, the PTSD-depression composite score obtained from the PCA was used in the subsequent regression analysis to minimize issues related to multicollinearity and Type I error.
3.2 Moderated Regression Analysis
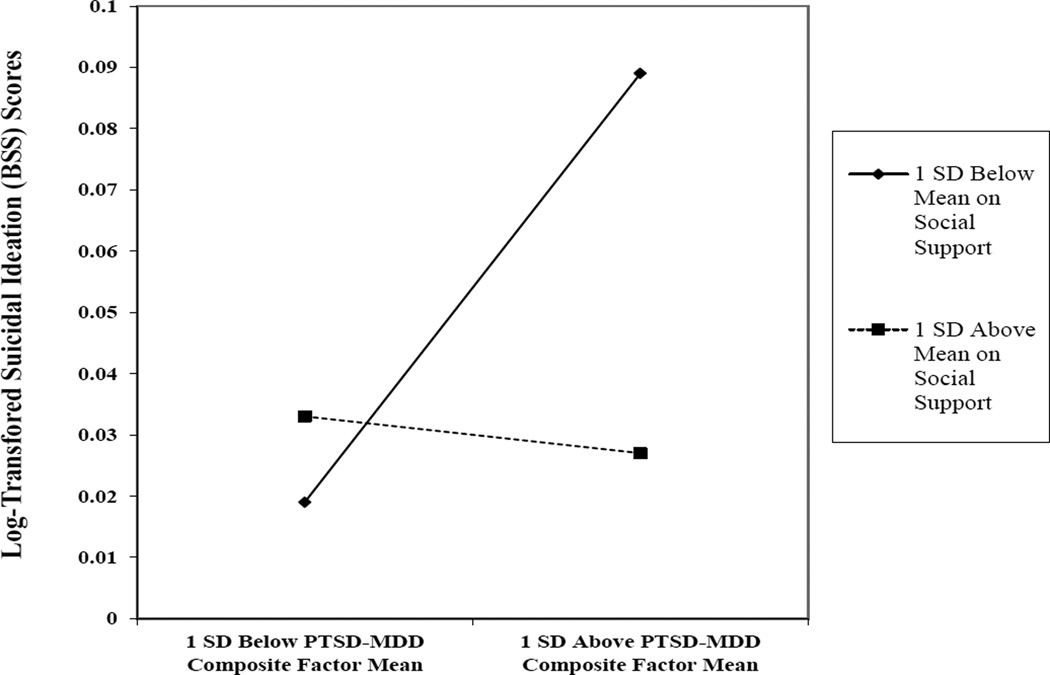
Moderated hierarchical linear regression was used to test the main hypothesis that social support moderates the effect of PTSD-depression symptoms on SI. The dependent variable was the log-transformed BSS score. Gender, age, education level, and race (dichotomized as Non-White = 0; White = 1) were entered into the first step of the regression to control for possible differences in these characteristics across diagnoses and level of SI. Composite PTSD-depression scores (which were standardized as a result of the PCA) and centered social support scores were entered in step 2. A social support × PTSD-depression interaction term was entered in step 3. As can be seen in Table 1, none of the demographic variables significantly predicted SI in step 1. Social support, β = −0.24, p = 0.05 (small effect) had a significant effect in step 2. The effect of PTSD-depression symptoms, β = 0.21, p = 0.05 (small effect), in step 2 was nearly statistically significant. In support of the main hypothesis, the social support × PTSD-depression symptoms interaction term significantly predicted SI in step 3, ΔR2 = 0.07; β = −0.27, p < 0.01, f2 = 0.09 (small effect). The interaction accounted for 7% of unique variance in SI over and above the main effects of PTSD-depression and social support. As predicted, PTSD-depression symptoms had almost no effect on SI when social support was high; however, when social support was low, PTSD-depression symptoms were positively associated with SI, such that Veterans with high levels of PTSD-depression symptoms and low levels of social support exhibited the highest overall levels of SI (Figure 1).
Table 1.
Summary of the Continuous Regression Models Predicting Suicidal Ideation
|
Full Sample (n = 130) |
PTSD or MDD Dx (n = 62) |
|||
|---|---|---|---|---|
| BSS Scores | BSS Scores | |||
| ΔR2 | β | ΔR2 | β | |
| Step 1 | 0.05 | 0.06 | ||
| Gender | −0.04 | 0.01 | ||
| Age | −0.09 | −0.10 | ||
| Education Level | −0.16 | −0.12 | ||
| Race | 0.08 | 0.19 | ||
| Step 2 | 0.14 | 0.19 | ||
| Social Support | −0.24* | −0.29* | ||
| PTSD-Depression Symptoms | 0.21a | 0.26a | ||
| Step 3 | 0.07 | 0.16 | ||
| Social Support × PTSD-Depression | −0.27** | −0.97** | ||
| Total R2 | 0.26 | 0.40 | ||
Note:
p < 0.05;
p < 0.01;
≤ 0.061.
PTSD = post-traumatic stress disorder; MDD = major depressive disorder; BSS = Beck Suicide Scale.
Figure 1.
Plot of Social Support × PTSD-Depression Symptoms Interaction Predicting Suicidal Ideation Among OEF/OIF Veterans (N = 130).
Note: PTSD = posttraumatic stress disorder; MDD = major depressive disorder; BSS = Beck Suicide Scale.
To explore how PTSD and MDD diagnoses might influence the observed interaction, post-hoc analyses were conducted in which the analyses described above were repeated with the sub-sample of Veterans who currently met full criteria for either PTSD or MDD (n = 62). As can be seen in Table 1, the results from this subgroup analysis were highly similar to those found in the overall sample. The magnitude of the interaction observed in this subsample was larger, ΔR2 = 0.16; β = −0.97, p < 0.01, f2 = 0.25 (medium effect), than that observed in the total sample, providing strong evidence that the findings from the general sample were not an artifact of including participants in the analysis who did not meet full criteria for PTSD and/or MDD.1
4.) Conclusion
The current study expands upon the existing literature by using a more comprehensive assessment (i.e., clinical diagnostic interview and well-validated self-report measures of PTSD, depression, social support and SI) in comparison to earlier reports that relied upon single item measures or items pulled from different scales. As predicted, the interaction between social support and PTSD-depressive symptoms predicted unique variance in current SI over and above demographic variables and main effects. These effects became even stronger when limiting the sample to those diagnosed with PTSD or MDD. Consistent with prior research (Jakupcak et al., 2010; Pietrzak et al., 2010; Pietrzak et al., 2011), individuals who report elevated PTSD-depressive symptoms and low perceived post-deployment social support may be at increased risk for SI compared to those reporting high levels of either risk factor alone.
Findings from the current study have direct clinical implications for assessing risk for suicide within Veteran populations, as well as informing treatment planning. In addition to established suicide risk assessment practices, our findings suggest that clinicians should assess perceptions of social support among Veterans with PTSD and depression. Individuals who experience severe symptoms of depression and/or PTSD in combination with low social support appear to be at higher risk for SI than individuals who experience the same symptom profile yet have high social support. Likewise, functional analysis of social support systems, evaluation of the accuracy of perceptions about social support, and strategies to increase social support resources may be important factors to incorporate during interventions aimed at reducing risk for suicide. Of relevance, there has been one promising trial of interpersonal-psychodynamic therapy in individuals who attempted suicide (Guthrie et al., 2001). Although this treatment did not directly target increasing social support, it is conceptually related in that it utilized the client-therapist relationship to resolve interpersonal problems as a means of treating SI (Guthrie et al., 2001). Compared to treatment as usual, individuals who received interpersonal-psychodynamic therapy were significantly less likely to attempt suicide during the 6-month follow-up period.
Of clinical importance, not only does social support interact with PTSD/depression to buffer against SI risk, but data also suggest that social support moderates response to treatment for PTSD (Price et al., 2011). Specifically, individuals who reported higher levels of perceived emotional and informational social support had greater symptom reduction following PTSD treatment. Conversely, conflict and lack of positive interactions with significant others may impede recovery from PTSD (Robinaugh et al., 2011). Thus, in order to more fully address suicide risk, clinicians may need to assess social support and intervene not only by treating disorders that increase risk for SI, but also by directly target social support in treatment. However, not all forms of social support are equivalent in terms of playing a protective role (e.g., perceived social support is more potent in comparison to actual support), and the mechanisms underlying differences in perceived social support remain unclear (Marroquin, 2011). Thus, when treating suicidal Veterans, thorough assessment of the quantity and quality of social support, perceptions of social support, and utilization of available social support is suggested.
4.1 Study Limitations
While the current study has several strengths, including the use of clinical diagnostic interviews and widely used, validated self-report measures, findings should be interpreted within the context of several limitations. First, all participants were enrolled in VA health care. Thus, the degree to which these findings generalize to OEF/OIF Veterans who are not seeking VA healthcare, or to non-Veteran populations, is unclear. Second, given the cross-sectional nature of the study, prospective, longitudinal research is needed to validate these findings.
4.2 Future Directions
Given that social support has been shown to moderate the influence of PTSD and depression on SI in multiple cross-sectional studies, future research should evaluate whether social support prospectively predicts SI and risk for suicide, and whether changes in social support is a more sensitive measure of suicide risk. Future research should continue to examine the most effective methods for assisting people with low social support (Hogan et al., 2002) and whether incorporating social support interventions into existing empirically-supported treatments for PTSD and depression reduces SI and risk for suicide. To maximize the impact of social support interventions, additional research is necessary to investigate the impact of differing forms of social support on SI, as well as precise mechanisms of social support that contribute to SI. For example, low social support is a robust risk factor for suicide (Van Orden et al., 2010). However, specific mechanisms that contribute to low social support and the development of social support systems remain unclear. One potential candidate is social cognition, or the ability to perceive, interpret, and respond to others when in social interactions (Green et al., 2005). Social cognition offers mechanisms, such as emotion perception, social perception, attributional style and theory of mind that are ripe for study within mental health population and among those who may be suicidal (Couture et al., 2006; Nietlisbach and Maercker, 2009; Sharp et al., 2012). Elucidating mechanisms to increase social support systems, as well as perceptions of social support, could provide fruitful targets for SI intervention in at-risk populations of returning Veterans who are attempting to reintegrate into civilian life following warzone deployments.
Acknowledgments
This research was supported by the Department of Veterans Affairs (VA) VISN 17 Center of Excellence for Research on Returning War Veterans, a Merit Award (I01RX000304) to Sandra B. Morissette, Ph.D. from the Rehabilitation Research and Development (RR&D) Service of the VA Office of Research and Development entitled, “Functional Outcomes in OEF/OIF Veterans with PTSD and Alcohol Misuse,” a VA VISN 17 New Investigator Award to Nathan A. Kimbrel, Ph.D. entitled, “Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse,” and a VA VISN 17 New Investigator Award to Eric C. Meyer, Ph.D. entitled, “Experiential Avoidance, Neurocognition, and Functional Outcomes in PTSD.” Dr. Kimbrel was supported by a Career Development Award-2 (1IK2CX000525-01A1) from the Clinical Science Research and Development Service of the VA Office of Research and Development. We would also like to acknowledge the contributions of our Veteran participants and research staff: Ellis Blackmore, Roberta Chrestman, Samantha Collum, Yolanda Evans, Christina Fay, Zachary Harned, Olivia Hobden, Ericka Saenz, Laurie Steffen, Skyy Walton, and Matthew Woodward. We would also like to thank Taylor Boss, Lindsey Jenkins and Samantha Synett for their help preparing this manuscript.
Footnotes
A second post-hoc regression analysis was also conducted in which we used categorical PTSD and MDD diagnoses in the analyses instead of a continuous PTSD-depression factor. Gender, age, education level, and race were entered in step 1. Centered social support scores and centered PTSD and MDD diagnosis (no = −.5, yes = .5) were entered in step 2. Finally, social support × PTSD diagnosis and social support × MDD diagnosis interaction terms were entered in step 3. The only significant predictor of SI in this model was social support. Neither PTSD nor depression diagnosis was predictive of SI in step 2. In addition, neither diagnosis interacted with social support to predict SI in step 3. This was likely due to decreased statistical power associated with using dichotomous instead of continuous predictors.
References
- Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: Follow-up over 34–38 years. Journal of Affective Disorders. 2002;68:167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R. Manual for the Beck Scale for Suicidal Ideation. San Antonio, TX: Psychological Corporation; 1991. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories – IA and –II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory – II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Steer RA, Garbin MGJ. Psychometric properties of the Beck Depression Inventory twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Steer RA, Ranieri WF. Scale for suicide ideation: Psychometric properties of a self-report version. Journal of Clinical Psychology. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Gusman FD, Charney DS, Keane T. Development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blow FC, Bohnert ASB, IIgen MA, Ignacio R, McCarthy JF, Valenstein MM, Knox KL. Suicide mortality among patients treated by the Veteran Health Administration from 2000 to 2007. American Journal of Public Health. 2012;102:98–104. doi: 10.2105/AJPH.2011.300441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner LA, Ignacio RV, Blow FC. Suicide and traumatic brain injury among individuals seeking Veterans Health Administration services. Journal of Head Trauma Rehabilitation. 2011;4:257–264. doi: 10.1097/HTR.0b013e31821fdb6e. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Corso KA. Depression, PTSD, and suicidal ideation among active duty Veterans in an integrated primary care clinic. Psychological Services. 2011;8:94. [Google Scholar]
- Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: A review. Schizophrenia Bulletin. 2006;32:S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) San Antonio, TX: The Psychological Corporation; 1994. [Google Scholar]
- Elhai JD, Biehn TL, Armour C, Klopper JJ, Frueh BC, Palmieri PA. Evidence for a unique PTSD construct represented by PTSD's D1–D3 symptoms. Journal of Anxiety Disorders. 2011;25:340–345. doi: 10.1016/j.janxdis.2010.10.007. [DOI] [PubMed] [Google Scholar]
- Forbes D, Creamer M, Biddle D. The validity of the PTSD checklist as a measure of symptomatic change in combat-related PTSD. Behaviour Research and Therapy. 2001;39:977–986. doi: 10.1016/s0005-7967(00)00084-x. [DOI] [PubMed] [Google Scholar]
- Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social cognition in schizophrenia: Recommendations from the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophrenia Bulletin. 2005;31:882–887. doi: 10.1093/schbul/sbi049. [DOI] [PubMed] [Google Scholar]
- Gros DF, Price M, Magruder KM, Frueh BC. Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Research. 2012;196:267–270. doi: 10.1016/j.psychres.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra VS, Calhoun PS. Examining the relation between posttraumatic stress disorder and suicidal ideation in OEF/OIF Veteran sample. Journal of Anxiety Disorders. 2011;25:12–18. doi: 10.1016/j.janxdis.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthrie E, Kapur N, Mackway-Jones K, Chew-Graham C, Moorey J, Mendel E, Marino-Francis F, Sanderson S, Turpin C, Boddy G, Tomenson B. Randomised controlled trial of a brief psychological intervention after deliberate self poisoning. British Medical Journal. 2001;323:1–5. doi: 10.1136/bmj.323.7305.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan B, Linden W, Najarian B. Social support interventions: Do they work? Clinical Psychology Review. 2002;22:383–442. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic Stress Disorder as a risk factor for suicidal ideation in Iraq and Afghanistan War Veterans. Journal of Traumatic Stress. 2009;22:303–306. doi: 10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Vannoy S, Imel Z, Cook JW, Fontana A, Rosenheck R, McFall M. Does PTSD moderate the relationship between social support and suicide risk in Iraq and Afghanistan War Veterans seeking mental health treatment? Depression and Anxiety. 2010;27:1001–1005. doi: 10.1002/da.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. Journal of the American Medical Association. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and Veterans. Military Psychology. 2006;18:89. [Google Scholar]
- Koenen KC, Fu QJ, Ertel K, Lyons MJ, Eisen SA, True WR, Goldberg J, Tsuang MT. Common genetic liability to major depression and posttraumatic stress disorder in men. Journal of Affective Disorders. 2008;105:109–115. doi: 10.1016/j.jad.2007.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulka R, Schlenger W, Fairbank J, Jordan B, Hough R, Marmar C, Weiss D. Assessment of posttraumatic disorder in the community: Prospects and pitfalls from recent studies of Vietnam Veterans. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:547–560. [Google Scholar]
- Lemaire CM, Graham DP. Factors associated with suicidal ideation in OEF/OIF veterans. Journal of Affective Disorders. 2011;132:231–238. doi: 10.1016/j.jad.2010.10.021. [DOI] [PubMed] [Google Scholar]
- Marroquin B. Interpersonal emotion regulation as a mechanism of social support in depression. Clinical Psychology Review. 2011;31:1276–1290. doi: 10.1016/j.cpr.2011.09.005. [DOI] [PubMed] [Google Scholar]
- McCarthy JF, Valenstein M, Kim HM, Ilgen M, Zivin K, Blow FC. Suicide mortality among patients receiving care in the Veterans Health Administration health system. American Journal of Epidemiology. 2009;169:1033–1038. doi: 10.1093/aje/kwp010. [DOI] [PubMed] [Google Scholar]
- Meyer EC, Morissette SB, Kimbrel NA, Kruse MI, Gulliver SB. Acceptance and Action Questionnaire – II scores as a predictor of posttraumatic stress disorder symptoms among war Veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:521–528. [Google Scholar]
- Miller MW, Fogler JM, Wolf EJ, Kaloupek DG, Keane TM. The internalizing and externalizing structure of psychiatric comorbidity in combat veterans. Journal of Traumatic Stress. 2008;21:58–65. doi: 10.1002/jts.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nietlisbach G, Maercker A. Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression, Maltreatment and Trauma. 2009;18:382–402. [Google Scholar]
- Oquendo MA, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum MF, Malone KM, Mann JJ. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. American Journal of Psychiatry. 2003;160:580–582. doi: 10.1176/appi.ajp.160.3.580. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, Southwick SM. Risk and protective factors associated with suicidal ideation in Veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders. 2010;123:102–107. doi: 10.1016/j.jad.2009.08.001. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Russo AH, Ling Q, Southwick SM. Suicidal ideation in treatment-seeking Veterans of Operation Enduring Freedom and Iraqi Freedom: The role of coping strategies, resilience, and social support. Journal of Psychiatric Research. 2011;45:720–726. doi: 10.1016/j.jpsychires.2010.11.015. [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF, Strachan M, Ruggerio KJ, Acierno R. The role of social support in exposure therapy for Operation Iraq Freedom/Operation Enduring Freedom Veterans: A preliminary investigation. Psychology Trauma: Theory, Research, Practice, and Policy. 2011;5:93–100. doi: 10.1037/a0026244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pukay-Martin ND, Pontoski KE, Maxwell MA, Calhoun PS, Dutton CE, Clancy CP, Hertzberg MA, Collie CF, Beckham JC. The influence of depressive symptoms on suicidal ideation among US Vietnam-Era and Afghanistan/Iraq-Era Veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2012;25:578–582. doi: 10.1002/jts.21741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh DJ, Marques L, Traegar LN, Marks EH, Sung SC, Beck JG, Pollack MH, Simon NM. Understanding the relationship of perceived social support to post-trauma cognitions and posttraumatic stress disorder. Journal of Anxiety Disorders. 2011;25:1072–1078. doi: 10.1016/j.janxdis.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider B, Philipp M, Muller MJ. Psychopathological predictors of suicide in patients with major depression during a 5-year follow-up. European Psychiatry. 2001;16:283–288. doi: 10.1016/s0924-9338(01)00579-x. [DOI] [PubMed] [Google Scholar]
- Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: Mental health disorders among 103,788 US Veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Archives of Internal Medicine. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Sharp C, Fonagy P, Allen JG. Posttraumatic stress disorder: A social-cognitive perspective. Clinical Psychology: Science and Practice. 2012;19:229–240. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Steer R, Kumar G, Beck A. Self-reported suicidal ideation in adolescent psychiatric inpatients. Journal of Consulting and Clinical Psychology. 1993;61:1096–1099. doi: 10.1037//0022-006x.61.6.1096. [DOI] [PubMed] [Google Scholar]
- Tsai J, Harpaz-Rotem I, Pietzak RH, Southwick SM. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry: Interpersonal Biological Processes. 2012;75:135–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. Facts about Veteran suicide. 2012 Retrieved from http://www.dcoe.health.mil/Content/Navigation/Documents/VA_Suicide_Prevention_Fact_Sheet.pdf. [Google Scholar]
- U.S. Department of Veterans Affairs, Mental Health Services, Suicide Prevention Program. Suicide Data Report. 2013 Retrieved from: http://www.va.gov/opa/docs/Suicide-Data-Report-2012-final.pdf.
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15:391–402. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]