Abstract
Many Veterans from the conflicts in Iraq and Afghanistan return home with physical and psychological impairments that impact their ability to enjoy normal life activities and diminish their quality of life (QoL). The present research aimed to identify predictors of QoL over an eight‐month period using Bayesian model averaging (BMA), which is a statistical technique useful for maximizing power with smaller sample sizes. A sample of 117 Iraq and Afghanistan Veterans receiving care in a southwestern health care system was recruited, and BMA examined the impact of key demographics (e.g. age, gender), diagnoses (e.g. depression), and treatment modalities (e.g. individual therapy, medication) on QoL over time. Multiple imputation based on Gibbs sampling was employed for incomplete data (6.4% missingness). Average follow‐up QoL scores were significantly lower than at baseline (73.2 initial versus 69.5 four‐month and 68.3 eight‐month). Employment was associated with increased QoL during each follow‐up, while post‐traumatic stress disorder and Black race were inversely related. Additionally, predictive models indicated that depression, income, treatment for a medical condition, and group psychotherapy were strong negative predictors of four‐month QoL but not eight‐month QoL. Copyright © 2014 John Wiley & Sons, Ltd.
Keywords: quality of life, Veterans, Bayesian analysis, mental health
Introduction
As a result of the conflicts in Iraq and Afghanistan (i.e. Operations Enduring Freedom, Iraqi Freedom, and New Dawn, or OEF/OIF), many deployed service members are returning home with physical and psychological impairments (Baker et al., 2009; Copeland et al., 2011; Gros et al., 2011; Morissette et al., 2011). Soldiers are surviving traumatic combat‐related injuries at much greater rates compared to their predecessors due to more advanced body armor and faster transfer to advanced treatment facilities (Weaver et al., 2009). However, this has led to a greater prevalence of serious injuries among returning troops, including traumatic brain injury (TBI), amputations, or hearing and vision impairments. After returning home, these Veterans must learn to cope with their physical injuries, which can adversely affect their ability to lead a comfortable and enjoyable life (Schnurr et al., 2009). Deployment‐related mental health disorders, such as post‐traumatic stress disorder (PTSD) and depression are also common and may further decrease Veterans' quality of life (QoL) (Hoge et al., 2006; Pittman et al., 2012). Approximately 18% of returning troops display diagnosable levels of either PTSD or major depression (Tanielian et al., 2008). In a study of 3671 US soldiers returning home from combat duty in Iraq or Afghanistan, 12–20% met screening criteria for PTSD, 14–15% for depression, 16–18% for anxiety, and 24–35% for alcohol misuse (Hoge et al., 2004). Moreover, the prevalence of such disorders has been shown to increase over the months following return from war (Milliken et al., 2007). Veterans with PTSD appear to be less resilient to post‐deployment psychological stressors and are at increased risk for developing depression and alcohol use disorders (Pietrzak and Southwick, 2011). Furthermore, co‐occurring substance use disorders may impede treatment response for persons with PTSD and depression (Burnett‐Zeigler et al., 2011). Thus, identification of both malleable and fixed factors associated with post‐deployment QoL may provide information vital to the successful rehabilitation and reintegration of returning Veterans into civilian life.
Changing demographics in today's military may also influence post‐deployment rehabilitation and QoL. Because of the unprecedented reliance on Reservists and the National Guard, American OEF/OIF Veterans tend to be older than previous post‐deployment cohorts (Griffith and West, 2010; Keane, 2011). In addition to the more than 1.8 million US troops that have been deployed to Iraq and Afghanistan, it is estimated that an additional 2.7 million family members have also been directly affected by these deployments, suggesting the importance of addressing family and interpersonal functioning in post‐deployment rehabilitation (Hayes et al., 2010; Sheppard et al., 2010; Khaylis et al., 2011). Veterans may experience significant challenges during post‐deployment, including high rates of unemployment and marital problems, leading to further decreases in QoL (Khaylis et al., 2011). While marriage may increase resilience by buffering the effects of deployment, physical and mental ailments may lead to poorer relationship functioning and greater difficulty with reintegration upon return to civilian life (Schnurr et al., 2009; Finley et al., 2010; Zeber et al., 2010; Caska and Renshaw, 2011; Pietrzak and Southwick, 2011). Spirituality is another social factor associated with resilience in Veterans (Pietrzak et al., 2010; Pietrzak and Southwick, 2011). OEF/OIF Veterans who demonstrate less psychological resilience – particularly Veterans with elevated PTSD symptoms – tend to be younger and single, while psychologically‐resilient Veterans tend to be older, married, and more spiritual (Pietrzak and Southwick, 2011).
QoL refers to the ability to enjoy normal life activities, encompassing physical, mental, and social well‐being (World Health Organization, 1948). Factors adversely affecting QoL may become more prevalent over time and may not even become apparent until several months after a Veteran's initial assessment (Department of Veteran Affairs, 2007). In Hoge's landmark 2004 study, 81–86% of the soldiers who met screening criteria for a mental health disorder acknowledged they had a psychological problem. Of these, less than half (38–45%) were interested in receiving mental care, and even fewer (13–27%) had received treatment from a mental health professional in the previous year (Hoge et al., 2004). This delay in obtaining appropriate treatment in a timely manner may further erode Veterans' QoL over time. Consequently, as time from deployment increases, the need for treatment to improve unaddressed conditions may also grow. Multiple factors may influence QoL over the post‐deployment period, including physical symptoms and healing, rehabilitation efforts and related outcomes, psychological adjustment, support networks, and social interactions. OEF/OIF Veterans' QoL provides a broad measure of their overall post‐deployment physical, mental, and social well‐being. As such, identification of factors associated with changes in Veterans' QoL during post‐deployment reintegration could provide significant insight into specific areas of dysfunction needing greater attention in order to improve QoL and daily functioning.
Bayesian model averaging (BMA)
A standard data analysis approach to examining factors associated with a change in QoL would select a subset of measured predictors guided by theory for inclusion in a multiple regression model; however, a shortcoming of this approach is a dependence on inference about the set of predictors selected for model inclusion. This occurs because an alternative model with a different subset of predictors may fit the data equally well and also provide reasonable inference (Hoeting et al., 1999). Although both models may seem reasonable given the data, they may lead to different conclusions about the questions of interest. Thus, conditioning reliance upon a single selected model ignores the uncertainty in the model, which leads to over‐confidence in the conclusions drawn regarding the quantified associations (Raftery, 1995; Raftery et al., 1997). A remedy for this dilemma that provides optimal predictive ability (Madigan and Raftery, 1994) is to account for model uncertainty through Bayesian model averaging (BMA). BMA averages effects over many different competing models, incorporating model uncertainty into inferences about specific parameters and prediction so that the most appropriate model is selected (Raftery et al., 1997; Candolo et al., 2003). In approach, it is analogous to bootstrapping, but BMA samples from the predictors to generate estimated associations rather than sampling from the cases. An additional advantage of BMA is that its approach to variable inclusion allows conservation of power without entirely omitting variables from the analysis. In a corresponding multiple regression model, this would not be possible: to gain any information about a predictor, it must be included in the model. Furthermore, when the sample size is small, few predictors can be included. Accordingly, for this study we used BMA to identify factors related to changes in QoL scores in a small sample of OEF/OIF Veterans, from an initial baseline assessment to four‐month and eight‐month follow‐up assessments.
Study objectives and hypotheses
Because few studies have assessed physical, mental, and social factors associated with longitudinal changes in QoL for Veterans returning from military combat in Iraq and Afghanistan, the aim of the present research was to employ BMA techniques for identifying potential predictors of OEF/OIF Veterans' QoL. The BMA facilitates this for small, data‐rich samples such as ours. One particular study objective was to explore the association of several key mental health conditions with QoL over several months. It was hypothesized that PTSD, depression, alcohol use disorders, and TBI would each be uniquely associated with lower QoL at follow‐up assessments. We further suspected that spouses and significant others play a key role during post‐deployment reintegration. Consequently, it was predicted that older age, married status, treatment involvement (e.g. counseling, medication use), and greater use of religious or spiritual counseling services would be associated with an increase in QoL over time, whereas unemployment would be inversely related to QoL.
Methods
Sample and study design
Data for the current study were obtained from a longitudinal, prospective cohort pilot study that was part of a program of research called Project SERVE (Study Evaluating Returning Veterans Experiences [Project SERVE]; see acknowledgments) designed to identify risk and resilience factors for psychopathology and functioning among returning OEF/OIF Veterans. Given that only 55% of OEF/OIF Veterans seek treatment in the US Department of Veterans Affairs health care system (VA), the sample of participants obtained from the SERVE study is representative of VA treatment‐seeking Veterans and not necessarily Veterans in general (Veterans Health Administration, 2012). This is an important Veteran population given the number of Veterans who reside in the central Texas area due to the close proximity to the military post, Fort Hood. All study procedures were reviewed and approved by the local Institutional Review Board prior to data collection. Multiple recruitment methods were utilized to reach out to as many Veterans in the area as possible (e.g. flyers posted locally, randomly stratified mailings to Veterans enrolled in the VA Central Texas Veterans Health Care System). Participants were recruited through advertisement at enrollment sites, Veteran networks and service organizations, in‐service presentations to VA primary care and mental health staff, and from targeted recruitment letters. Recruited patients had to be at least 18 years of age and English‐speaking OEF/OIF Veterans enrolled (or willing to enroll) in VA services within the health care system where the study was conducted. Participants agreed to be contacted for follow‐up assessments, and, if receiving mental health treatment, had to be stable on psychotropic medications and/or in psychotherapy prior to their baseline assessment. Participants were excluded if they planned to relocate out of the catchment area within four months of study initiation, had a psychotic disorder, or reported current suicidal or homicidal risk warranting crisis intervention. The recruitment plan was designed to over‐sample Veterans experiencing mental health problems. A total of 117 Veterans met eligibility criteria and completed a baseline QoL assessment. Participants were then mailed a follow‐up QoL assessment at four months and eight months; 95 Veterans completed both follow‐ups (81% response rate). A total of 79 Veterans (68% of total participants) had complete data on subsequent QoL assessments, demographics, diagnoses, and treatment involvement. Missing data on these measures for the remaining 38 participants were imputed to keep a study sample size of 117 Veterans, and results from the imputed and non‐imputed samples were compared.
Measures
Baseline measures included participants' demographics (age, gender, race/ethnicity, marital status), socio‐economic status (education, income, employment), diagnoses, treatment for medical and psychiatric conditions, prescription medication use, and time since last deployment. Marital status was dichotomized as married (1‐Yes/0‐No). Responses for race were reclassified into three indicators for White, Black, and other non‐White (1‐Yes/0‐No) due to small representation of other races, ethnicity was measured by a dichotomous variable for Hispanic status (1‐Yes/0‐No). Annual income was categorized into six levels, representing household income of < $15,000 to ≥ $90,000 with $15,000 intervals.
Indicators denoting medical and psychiatric conditions included current and lifetime diagnoses of PTSD, major depressive disorder (MDD), and alcohol use disorder (AUD), lifetime diagnoses for other substance use disorders (SUDs), and TBI. Clinical diagnoses were assessed using state‐of‐the art assessments, including Clinician Administered PTSD Scale (CAPS), the Anxiety Disorders Interview Schedule‐IV (ADIS‐IV), and the Structured Clinical Interview for DSM‐IV (SCID). All psychological disorders were diagnosed using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM‐IV‐TR) (American Psychiatric Association, 2000). The Defense and Veterans Brain Injury Center TBI screen and a TBI screening interview developed by Vasterling and colleagues were used to assess TBI (Vasterling, 2008). Treatment measures included self‐reported current receipt of physical, mental, and psychosocial treatment involvement factors assessed at baseline and dichotomously defined as: (1) hospital or doctor visits for a physical condition; (2) individual psychotherapy; (3) group psychotherapy; and (4) spiritual counseling. Current pharmacological treatment for a psychological condition was similarly defined and obtained in order to assess the impact of medication management on QoL. These variables served as candidate independent variables in the analyses.
The outcome variable of interest was Veterans' post‐deployment QoL, which was assessed at baseline, four months, and eight months. We measured QoL with the 16‐item Quality of Life Scale (QoLS), developed by Burckhardt et al. (1989). This measure was adapted from the original 15‐item instrument developed by Flanagan (1978) for use in chronically ill patients (Flanagan, 1978; Burckhardt and Anderson, 2003). It has demonstrably high reliability and validity across diverse patient groups and cultures (Burckhardt and Anderson, 2003; Burckhardt et al., 2003). The original version of the QoLS has demonstrated good internal consistency (Cronbach's α = 0.82–0.92) and high test–retest reliability over three weeks (r = 0.78–0.84). Similar findings have been reported for the 16‐item scale (Burckhardt and Anderson, 2003).
The adapted 16‐item QoLS contains items assessing satisfaction with various aspects of life including physical and material well‐being, personal development and fulfillment, relationships with others, participation in social, community and civic activities, and recreation (Burckhardt et al., 1989; Burckhardt and Anderson, 2003). Respondents rated their satisfaction on a seven‐point Likert scale ranging from Terrible (assigned a value of one) to Delighted (assigned a value of seven). The QoLS yields a total score, ranging from 16 to 112, where higher scores indicate better QoL. Although the 16‐item QoLS was initially developed for patients with chronic illnesses, including patients with PTSD, the instrument is also used to gather quantitative QoL information from healthy samples (Burckhardt and Anderson, 2003; Burckhardt et al., 2003). The average total score for healthy populations is approximately 90, where a mean of 61 was reported among a cohort of patients with PTSD admitted for mixed reasons: combat reactions, vehicle and work‐related accidents, terrorist incidents (Amir et al., 1997; Burckhardt and Anderson, 2003). The QoLS has three sub‐domains: (1) relationships and material well‐being (five items); (2) health and functioning (four items); and (3) personal, social and community commitment (seven items) (Burckhardt et al., 2003). High internal consistency for the QoLS total score was observed in the current study (range 0.93–0.94) across the three time points. Internal consistency ranged 0.78–0.83 for relationships and material well‐being, 0.80–0.85 for health and functioning, and 0.88–0.92 for personal, social and community commitment.
Data analysis
Multiple imputation using Gibbs sampling was performed for the incomplete multivariate data (6.4% missingness) utilizing the function in the MICE (Multivariate Imputations by Chained Equations) package of the statistical software, R. Multiple imputation by chained equations was performed using all available data, including complete and incomplete variables. This included patient characteristics found in Table 1, such as demographics, current and lifetime diagnoses, TBI, and treatment involvement measures, as well as baseline QoL and items from the QoLS at four months and eight months for use in the evaluation of the QoLS sub‐domains. Missing data for an incomplete variable were generated using the other variables in the data. For predictor variables that are also incomplete, the most recently generated imputed estimates were used to complete the predictors prior to imputation of the target variable. Imputation models included predictive mean matching for continuous variables, logistic regression for dichotomous variables, and polytomous logistic regression for variables containing more than two levels, using 50 imputations.
Table 1.
Descriptive characteristics of the sample (N = 117)
| Patient characteristics | Mean (SD)/Median (min–max) | Frequency (%) |
|---|---|---|
| Age (in years) | 37.2 (10.1) / 35.0 (22–61) | |
| Years of education | 14.0 (2.2) / 13.0 (11–20) | |
| Months since deployment | 43.4 (31.3) / 40.0 (0–174) | |
| Female | 16 (13.7%) | |
| Race | ||
| White | 76 (65.0%) | |
| Black | 21 (18.0%) | |
| Other | 20 (17.1%) | |
| Hispanic | 31 (26.5%) | |
| Married | 82 (70.1%) | |
| Employed | 56 (47.9%) | |
| Annual income | ||
| < $15,000 | 15 (12.8%) | |
| $15,000–29,999 | 22 (18.8%) | |
| $30,000–44,999 | 37 (31.6%) | |
| $45,000–59,999 | 21 (18.0%) | |
| $60,000–74,999 | < 11 | |
| $75,000–89,999 | < 11 | |
| > $90,000 | < 11 | |
| Diagnosesa | ||
| PTSD Lifetime; Current | 77 (65.8%); 51 (43.6%) | |
| MDD Lifetime; Current | 61 (52.1%); 36 (30.8%) | |
| AUD Lifetime; Current | 61 (52.1%); 28 (23.9%) | |
| SUD Lifetime | 18 (15.4%) | |
| TBI | 53 (45.3%) | |
| Current treatment involvement | ||
| Physical condition | 83 (70.9%) | |
| Individual psychotherapy | 42 (35.9%) | |
| Group psychotherapy | 27 (23.1%) | |
| Spiritual counseling | 21 (18.0%) | |
| Medication management | 56 (47.9%) |
Diagnoses are not mutually exclusive.
Means and frequencies were calculated for patient characteristics and QoL measures. Analyses employing BMA examined participant factors associated with changes in total QoLS scores and in the three QoLS sub‐domains over four‐month and eight‐month periods. These factors included demographic and socio‐economic characteristics, current mental health diagnoses and diagnosis of TBI, time since last deployment, and treatment involvement. The BMA procedure employed did not handle repeated outcomes; therefore, we did not model the three time points in any single model.
In BMA, model uncertainty is accounted for by averaging over the best models in the model class within a Bayesian framework. Let M = (M 1, …, MJ) for j = 1, …, J be the set of models under consideration. Suppose one were interested in a future observation or a model parameter, denoted by Δ. Then, the posterior distribution of Δ given data Y is an average of the posterior predictive distribution for Δ under each of the models considered, weighted by the corresponding posterior model probability p(Mj|Y), and is defined by the law of total probability formula,
The posterior probability for model Mj, serving as a weight in the previous formula, is derived using the posterior probabilities of the competing models and is given by
where p(Mj) is the prior probability that model Mj is the true model,
is the marginal likelihood for model Mj, p(θj |Mj) is the prior probability distribution assigned to the parameters of model Mj, and p(Y|θj, Mj) is the likelihood of Y under model Mj. Parameter estimates resulting from the BMA approach can then be obtained from
where denotes the posterior mean for model Mj with standard deviations similarly obtained (Hoeting et al., 1999).
Bayesian model selection is frequently based on Bayes factors. For any two candidate models, say Mj and Mk, the ratio of their corresponding marginal likelihoods gives the Bayes factor, defined as
This number is used to compare competing models and determine which model is most favored as representing the data. If BF jk > 1, then evidence would support Mj as the superior model for the data. In BMA, Bayes factors can be used to construct model posterior probabilities, where Bayesian Information Criterion (BIC) can approximate p(Y|M j) with
Then, BIC approximation to the Bayes factor becomes
Given model posterior probabilities can be expressed in terms of Bayes factors,
can be approximated with
Therefore, in this study, BIC approximation was used to construct the prior probabilities on the regression coefficients (Raftery et al., 2010; St‐Louis et al., 2012). This approximation corresponds most closely to the unit information prior, which is often a rational choice in the absence of strong prior information or beliefs (Raftery, 1999). This prior is relatively non‐informative and diffuse, making BIC approximation a more conservative approach than other alternative priors that are more likely to find evidence of an effect. Model priors were assumed to have a uniform distribution set to 1/2K, where K was the total number of variables included in the analysis (Clyde and George, 2004).
When J is large, a Bayesian model selection algorithm is used called “Occam's Window”, which involves averaging over a reduced set of models. Each post‐baseline QoLS score was separately assessed and modeled using a set of candidate independent variables, including baseline QoLS results. Potential models were determined using Occam's window and their posterior probabilities and the posterior means and standard deviations of the regression coefficients. The Occam's window approach entails the exclusion of (1) models that are N 0 times less likely a posteriori than the maximum posterior model (N 0 = 20 for this study) and (2) models with posterior probabilities smaller than their simpler counterparts. All remaining models fall in Occam's window (Raftery, 1995).
For the BMA procedure, all possible models composed of the candidate independent variables (including the null model) were evaluated according to model fit. BIC and derived posterior model probabilities were used to compare competing models (Schwarz, 1978). The model with the lowest BIC and largest posterior probability was deemed the best model. When BMA is applied to all proposed predictors, the posterior distribution of the outcome variable is a weighted average of the posterior distributions of the outcome for each likely model, making BMA a suitable method for analyses involving a large number of predictors (Raftery et al., 2005; Horvath, 2011). Other fit indices assessed included the coefficient of determination (R 2) and adjusted R 2. For each candidate independent variable, the posterior effect probability was calculated by summing up the posterior model probabilities of each model in which the explanatory variable is included and used to determine the relative importance of the variable. From this, the BMA posterior distribution mean and standard deviation of each regression coefficient can be calculated from the weighted average of coefficients under each separate model, where weights were assigned using the posterior model probabilities (Peters and Okalo, 2009). Analyses were performed using the bicreg() function contained in the BMA package of R. This function uses a BIC approximation to perform Bayesian model selection, accounting for model uncertainty in linear regression models, from which BMA estimates of the regression coefficients and their posterior standard deviations can be obtained (Lamon III et al., 2008). In this paper, we use a posterior probability cutoff for variable inclusion of 20% when reporting the posterior effects of potential variables associated with QoL.
Modest differences were observed between analysis results using the imputed and non‐imputed samples. Results from the imputed sample resembled those from the non‐imputed sample with the exception of income, Black race, and visits for a medical condition as prominent predictors (>20% posterior probability) and AUD no longer a prominent predictor for four‐month QoL. At eight‐months, the two best‐fit models for QoL with the imputed sample contained the same subset of predictors as the two best‐fit models with the non‐imputed sample. For this reason, the authors have chosen to include results from the imputed sample only. Results from the non‐imputed sample are available upon request. Models using lifetime diagnoses instead of current diagnoses of mental health conditions were also examined. Similar results were observed for the four‐month and eight‐month QoL BMA analysis with the exception of lifetime MDD included and lifetime PTSD excluded in most eight‐month models. These results are also available upon request.
Results
Cohort characteristics
Consistent with VA demographics, the sample of 117 OEF/OIF Veterans were predominantly male (86%), white (65%), and married (70%) with a mean age of 37 years (standard deviation [SD] = 10; Table 1). At initial assessment, the number of months since Veterans' last deployment averaged 43 months (SD = 31). Approximately half (48%) of the participants were currently employed (full‐time or part‐time), and 32% reported a household income under $30,000. A TBI diagnosis (primarily mild TBI, based on loss of consciousness lasting no more than 30 minutes and/or post‐traumatic amnesia lasting no more than 24 hours) was observed among 45% of the study participants.
The most frequently observed lifetime mental health condition was PTSD (66%; 44% current), followed by MDD (52%; 31% current) and AUD (52%; 24% current). A total of 96 (82%) Veterans had at least one lifetime mental health disorder (PTSD, MDD, AUD, or SUD) and 73 (62%) had more than one such lifetime condition. Similarly, 67 (57%) of participants had at least one and 37 (32%) had more than one current diagnosis of PTSD, MDD, AUD, or SUD. Of these 67 Veterans, 38 (57%) were currently attending individual or group psychotherapy sessions, 43 (64%) were receiving medication management, 34 (51%) were receiving both psychotherapy and medication, and 20 (30%) were receiving neither psychotherapy nor medication management. Baseline QoLS averaged 73.2 (SD = 19; Table 2).
Table 2.
QoLS total and sub‐domains (N = 117)
| Sub‐domains | Baseline | Four‐month | Eight‐month |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Median (min–max) | Median (min–max) | Median (min–max) | |
| Relationships and Material Well‐being | 24.1 (6.3) | 22.9 (6.1) | 22.5 (6.4) |
| 25.0 (8–35) | 23.0 (8–35) | 23.0 (9–35) | |
| Health and Functioning | 17.9 (5.3) | 17.0 (5.4) | 16.3 (5.9) |
| 18.0 (5–28) | 17.0 (5–28) | 16.0 (4–27) | |
| Personal, Social and Community Commitment | 31.3 (9.4) | 29.6 (9.0) | 29.5 (9.0) |
| 32.0 (10–49) | 30.0 (10–49) | 28.0 (11–49) | |
| Totala | 73.2 (19.1) | 69.5 (18.7) | 68.3 (19.3) |
| 74.0 (32–109) | 68.0 (30–112) | 65.0 (30–109) |
Significant change between baseline QoLS and follow‐up QoLS at four‐months (p = 0.01) and eight‐months (p < 0.01), assuming α = 0.05 significance level.
QoL assessment at four months
Veterans reported significantly lower QoL at four months (mean = 69.5, SD = 19; p = 0.01) compared to baseline. This corresponded to a mean decrease of 3.7 (SD = 16), yielding a small effect size (Cohen's d = 0.24) (Cohen, 1988). For the BMA approach, potential predictors excluded from all 45 selected models for modeling four‐month QoL are denoted by a zero posterior effect probability (Prob = 0%) for model inclusion and a zero posterior mean (Table 3).
Table 3.
BMA results showing the five best (BIC and posterior model probabilities) models for four‐month follow‐up QoLS (N = 117)
| Four‐month predictors | Prob (%) | Posterior Mean (SD) | Model 1a | Model 2 | Model 3 | Model 4 | Model 5 |
|---|---|---|---|---|---|---|---|
| Intercept | 100.0 | 43.16 (7.07) | 42.87 | 42.85 | 44.78 | 40.96 | 46.38 |
| QoL baseline | 100.0 | 0.47 (0.08) | 0.47 | 0.48 | 0.49 | 0.50 | 0.46 |
| Black | 98.2 | –9.33 (3.38) | –9.84 | –9.48 | –10.38 | –8.95 | –9.65 |
| PTSDb | 86.9 | –7.45 (4.06) | –9.18 | –8.68 | –9.53 | –9.29 | –8.73 |
| Group psychotherapy | 63.7 | –4.45 (4.14) | –8.03 | –6.17 | –7.29 | — | –7.34 |
| Income | 46.5 | –0.89 (1.13) | — | –1.97 | –1.40 | –2.33 | — |
| Employed | 44.9 | 2.60 (3.42) | — | 5.51 | — | 6.52 | — |
| MDD | 34.2 | –2.28 (3.76) | — | — | — | — | — |
| Physical treatment | 27.2 | –1.31 (2.56) | — | — | — | — | –4.52 |
| Female | 3.6 | –0.15 (1.03) | — | — | — | — | — |
| TBI | 2.7 | –0.06 (0.56) | — | — | — | — | — |
| Hispanic | 1.6 | –0.04 (0.48) | — | — | — | — | — |
| Time from deployment | 0.8 | <0.01 (<0.01) | — | — | — | — | — |
| Age | 0.6 | <0.01 (0.01) | — | — | — | — | — |
| Education | 0.6 | <0.01 (0.06) | — | — | — | — | — |
| Married | 0.0 | 0.0 | — | — | — | — | — |
| Other race | 0.0 | 0.0 | — | — | — | — | — |
| AUD | 0.0 | 0.0 | — | — | — | — | — |
| Medication management | 0.0 | 0.0 | — | — | — | — | — |
| Individual psychotherapy | 0.0 | 0.0 | — | — | — | — | — |
| Spiritual counseling | 0.0 | 0.0 | — | — | — | — | — |
| Fit indices | |||||||
| Number of variables | 4 | 6 | 5 | 5 | 5 | ||
| R b | 0.55 | 0.58 | 0.57 | 0.57 | 0.56 | ||
| Adjusted R b | 0.54 | 0.56 | 0.55 | 0.55 | 0.54 | ||
| BIC | –75.14 | –73.55 | –73.52 | –73.48 | –73.38 | ||
| Posterior probability | 0.122 | 0.055 | 0.054 | 0.053 | 0.051 |
Posterior means reported for Models 1–5.
Model includes current diagnoses of PTSD, MDD, and AUD. Similar results were obtained for lifetime diagnoses.
Adjusting for baseline QoLS results, the strongest predictors of four‐month QoL included Black race (Prob = 98.2%; BMA posterior mean of −9.3), current PTSD (Prob = 86.9%; −7.5), group psychotherapy (Prob = 63.7%; −4.5), income (Prob = 46.5%; −0.9), employment (Prob = 44.9%; 2.6), current MDD (Prob = 34.2%; −2.3), and treatment for a physical condition (Prob = 27.2%; −1.3). Thus, a current diagnosis of PTSD was associated with an average drop of 7.5 in QoL at four months compared to study participants without PTSD. Corresponding posterior standard deviations are also displayed in Table 3. The effects of other variables appeared minimal due to their small posterior probabilities. Posterior density plots for each coefficient derived from BMA are shown in Figure 1. The posterior probability that a coefficient is zero is represented by a solid line at zero with a height corresponding to this probability. Variables with a spike at zero appeared least influential in the models of post‐deployment QoL, suggesting their coefficients are centered on, and are approximately, zero. The non‐zero part of the distribution is scaled so that the maximum height is equal to the probability that the coefficient is non‐zero. Variables with posterior probabilities of being non‐zero greater than 20% are further outlined in Figure 1. These plots similarly convey the same subset of variables as contributing most to four‐month QoL assessments.
Figure 1.
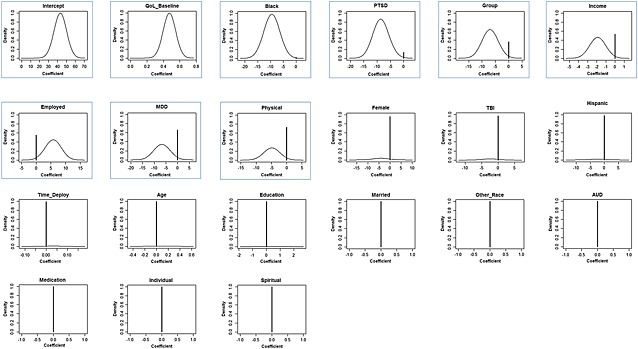
Posterior density plots of predictors for four‐month QoLS with posterior probabilities of being non‐zero > 20% outlined below (N = 117).
The five best models predicting four‐month QoL, defined by lowest BIC and largest posterior probability, are displayed in Table 3. These models have a cumulative posterior probability of 0.33. With each model, the number of predictors, R 2, and adjusted R 2 are also provided. The first model (Model 1) appeared to be the model of best fit because it had the lowest BIC (−75.1) and the largest posterior probability (0.12). Consequently, this model was selected as our final predictive model of four‐month QoL. The selected model indicated that race, current PTSD, and group psychotherapy were the strongest predictors of four‐month QoL.
Analyses were also performed to determine the strongest predictors of QoLS sub‐domains. When modeling QoL results from baseline to four months for the single sub‐domain Relationships and Material Well‐being, three prominent predictors in addition to baseline QoL included group psychotherapy (Prob = 100%; −3.9), Black race (Prob = 67.7%; −1.8), and income (Prob = 29.8%; −0.2). Married status, employment, non‐Black minority race, and time since deployment were associated with increased QoL for this sub‐domain while female gender, age, Hispanic ethnicity, medical treatment, and current PTSD, MDD or AUD were associated with decreased QoL. The strongest predictors of QoL in the sub‐domain Health and Functioning included employment (Prob = 92.4%; 2.2), current PTSD (Prob = 85.2%; −2.2), Black race (Prob = 73.6%; −1.9), and income (Prob = 32.0%; −0.2). Education and other minority race were associated with increased QoL in Health and Functioning while age, female gender, marital status, MDD, TBI, medical treatment, group psychotherapy, and spiritual counseling were associated with decreases. For Personal, Social, and Community Commitment, Black race (Prob = 91.7%; −4.3), current MDD (Prob = 80.9%; −3.6) and PTSD (Prob = 66.4%; −2.8), and TBI (Prob = 54.3%; −1.6) were the strongest predictors.
QoL assessment at eight months
A significant decrease in Veterans' QoL at eight months from baseline was observed (mean = 68.3, SD = 23; p < 0.01). A mean decrease of 4.9 (SD = 15) was observed, yielding a small effect size (Cohen's d = 0.32). Among the 32 selected models for modeling eight‐month QoL with the BMA approach (Table 4), prominent predictors included baseline QoL along with employment (Prob = 99.0%; 8.2), Black race (Prob = 34.6%; −2.2), and current PTSD (Prob = 32.1%; −1.9). Posterior density plots in Figure 2 further demonstrate these results. Cumulative posterior probability was 0.41 for the five best models. In addition to baseline QoL, the best‐fit model for eight‐month QoL (Model 1) contained only employment status, which was strongly associated with greater QoL for Veterans over the eight‐month period.
Table 4.
BMA results showing the five best (BIC and posterior model probabilities) models for eight‐month follow‐up QoLS (N = 117)
| Eight‐month predictors | Prob (%) | Posterior Mean (SD) | Model 1a | Model 2 | Model 3 | Model 4 | Model 5 |
|---|---|---|---|---|---|---|---|
| Intercept | 100.0 | 21.99 (7.11) | 17.02 | 25.47 | 19.22 | 15.25 | 21.34 |
| QoL baseline | 100.0 | 0.61 (0.08) | 0.64 | 0.57 | 0.63 | 0.65 | 0.63 |
| Employed | 99.0 | 8.15 (2.78) | 8.79 | 7.86 | 8.04 | 8.81 | 8.66 |
| Black | 34.6 | –2.17 (3.57) | — | — | –5.99 | — | — |
| PTSDb | 32.1 | –1.85 (3.18) | — | –5.88 | — | — | — |
| TBI | 12.5 | –0.53 (1.67) | — | — | — | — | — |
| Income | 11.4 | –0.15 (0.51) | — | — | — | — | — |
| Physical treatment | 9.8 | –0.40 (1.49) | — | — | — | — | –4.28 |
| Other race | 9.7 | 0.53 (1.93) | — | — | — | 5.41 | — |
| Group psychotherapy | 8.1 | –0.35 (1.47) | — | — | — | — | — |
| Medication management | 7.4 | –0.31 (1.34) | — | — | — | — | — |
| Spiritual counseling | 7.3 | –0.32 (1.44) | — | — | — | — | — |
| MDD | 2.0 | –0.06 (0.58) | — | — | — | — | — |
| Hispanic | 1.0 | –0.07 (0.73) | — | — | — | — | — |
| Age | 0.0 | 0.0 | — | — | — | — | — |
| Female | 0.0 | 0.0 | — | — | — | — | — |
| Married | 0.0 | 0.0 | — | — | — | — | — |
| Education | 0.0 | 0.0 | — | — | — | — | — |
| AUD | 0.0 | 0.0 | — | — | — | — | — |
| Individual psychotherapy | 0.0 | 0.0 | — | — | — | — | — |
| Time from deployment | 0.0 | 0.0 | — | — | — | — | — |
| Fit indices | |||||||
| Number of variables | 2 | 3 | 3 | 3 | 3 | ||
| R b | 0.52 | 0.53 | 0.53 | 0.53 | 0.53 | ||
| Adjusted R b | 0.51 | 0.52 | 0.52 | 0.51 | 0.51 | ||
| BIC | –75.46 | –74.73 | –74.08 | –73.43 | –73.13 | ||
| Posterior probability | 0.141 | 0.098 | 0.071 | 0.051 | 0.044 |
Posterior means reported for Models 1–5.
Model includes current diagnoses of PTSD, MDD, and AUD. Similar results were obtained for lifetime diagnoses, except for the inclusion of lifetime MDD as a prominent predictor instead of lifetime PTSD.
Figure 2.
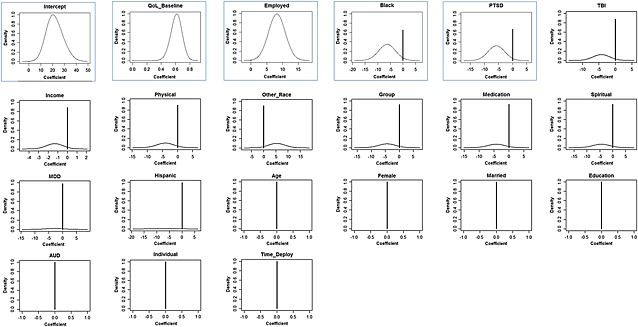
Posterior density plots of predictors for eight‐month QoLS with posterior probabilities of being non‐zero > 20% outlined below (N = 117).
The strongest predictors for the sub‐domain Relationships and Material Well‐being included Black race (Prob = 81.7%; −2.7), employment (Prob = 39.9%; 0.8), group psychotherapy (Prob = 37.6%; −0.9), and current PTSD (Prob = 21.3%; −0.4), in addition to baseline QoLS. While married status, non‐Black minority race, and individual psychotherapy were associated with increased QoL in this sub‐domain, Hispanic ethnicity, income, current AUD and MDD, and medication use were associated with decreased QoL. Prominent predictors for Health and Functioning included employment (Prob = 100%; 3.2), spiritual counseling (Prob = 74.0%; −1.9), treatment for a physical condition (Prob = 61.5%; −1.2), and minority non‐Black race (Prob = 32.2%; 0.6). For the Personal, Social and Community Commitment sub‐domain, TBI (Prob = 26.4%; −0.6) and employment (Prob = 64.6%; 1.9) were most associated with Veterans' QoL over eight months.
Discussion
The aim of the present research was to use BMA methods to identify prospective predictors of Iraq and Afghanistan Veterans' QoL across an eight‐month time period. A significant decline in QoL was observed during the eight‐month period which serves to underscore the importance of understanding factors that may influence Veterans' long‐term post‐deployment QoL, even years after returning from deployment. During this timeframe, average QoLS scores ranged from 68.3 to 73.2, roughly a 7% reduction from baseline. This is far below the average of 90 observed among healthy populations but above the average of 61 observed in a previous study of patients with PTSD (Burckhardt and Anderson, 2003). The fact that this study's average QoLS scores fall in this range is likely due to the fact that only 67 (57%) of participants met criteria for a current mental health condition at the time of the baseline assessment. The reduction in QoLS at four months corresponded to a small effect (Cohen's d = 0.24), which increased to d = 0.32 at eight months. If this trend continues, a much larger effect could be observed over a longer period of time, highlighting the need to appropriately treat Veterans during post‐deployment in order to improve their QoL. Further study of Veterans' QoL over a longer period of time is needed to determine if this trend in QoL continues, stabilizes, or reverses.
A significant strength of the study was the use of BMA techniques, which has the benefit of combining predictions from several models weighted by factors related to model performance and incorporating model and parameter uncertainty. In addition to baseline QoL (positive association), the best‐fitting model of four‐month QoL also included Veterans' race, current diagnosis of PTSD, and group psychotherapy. Each was negatively related to four‐month QoLS scores. At eight‐months, the best‐fitting model included baseline QoL and employment (both positively associated). In both cases, the best‐fitting models were parsimonious (i.e. included 2–4 predictors) while still accounting for a significant amount of variance (52–55%) in QoLS scores. The second model (Model 2) for eight‐month QoL did not vary from the first model (Model 1), except for the inclusion of current PTSD (negatively associated) as a predictor.
Regarding our hypotheses, neither age nor marital status was a strong predictor in the models of overall QoL. However, age was negatively associated with QoL in the sub‐domain, Health and Functioning, which makes intuitive sense given increased age is associated with declining health QoL. Also, marital status was positively associated with QoL in Relationships and Material Well‐being and negatively associated with QoL in Health and Functioning and Personal, Social, and Community Commitment. These differential effects of marital status on these subscales may have canceled out their effects when examining overall QoL. The relationships of QoL with treatment involvement were reversed from our hypotheses. While group psychotherapy and medical treatment were negatively associated with four‐month QoL, neither was strongly associated with eight‐month QoL. It is possible that there is a delayed impact of treatment on QoL. Here, participants in our sample may have had increased involvement in treatment due to more physical and mental health conditions, which were in turn associated with lower QoL. However, it is unclear why these factors were not associated with QoL at eight months. Consistent with our hypotheses, being employed full‐time or part‐time was associated with increased QoL. In addition, the averaged effects of Black race demonstrated a negative association with QoL for each time point. Although minimal, Hispanic ethnicity tended to have a negative relationship and minority non‐Black races a positive relationship with QoL for eight‐month QoL assessments. These findings are consistent with the larger literature on QoL in ethnic and racial minorities. Consistent with the mental health literature, a current diagnosis of PTSD or MDD were prominent predictors of decreased QoL at four‐months. At eight‐months, PTSD remained predictive of QoL, highlighting the lingering effects that mental health diagnoses can have on future QoL.
Limitations
There are several limitations with interpreting the findings of our study. First, QoL was measured via self report. It is widely known that mental health conditions can negatively affect perceptions, including of QoL, and there was no objective measure of whether QoL actually changed or whether it was merely perceived to change. Nonetheless, measurement of perceptions of QoL is clinically intuitive and can impact overall life satisfaction and well‐being. An additional limitation of the current investigation is the interpretation of the effects for treatment involvement measures. This observed negative association is noteworthy as it may indicate that the more intractable patients' symptoms are, the greater the likelihood of receiving these treatments, causing treatment to become a proxy for patients' symptomology and disease severity. For example, treatment for a physical condition could serve a proxy for a physical condition unaccounted for in the BMA models. In this case, a negative effect is likely to be observed. Although not available in this study, medical records could have provided more accurate detail on Veterans' treatment involvement, including the types of treatment and their frequency, as well as the use of various medications (e.g. antidepressants, antipsychotics). Another limitation was the substantial variability in the amount time elapsed from Veterans' last deployment, which was rarely selected in the BMA models but positive when chosen.
The selection of a subset of predictors remains a fundamental issue in linear regression modeling for situations involving a large number of predictors or small sample size. While models using different subsets of predictors may fit the data equally well and provide reasonable inference, these models may lead to different conclusions. BMA offers a coherent approach to accounting for model uncertainty by averaging over many different competing models and incorporating this uncertainty into inferences about parameters and prediction.
Although some variables may not be included in the best‐fitting BMA model (Model 1), they may be included in other models that had similarly good fit. BMA has the advantage of reducing a high‐dimensionality problem of too many potentially influential covariates. While BMA provides an averaged effect for a multitude of variables, it is not intended to yield a single best model. Theory should still dictate the correct model. Thus, while the BMA procedure may prove beneficial in identifying prominent associations in instances of a limited sample size or too many predictors, in our opinion, a clinician's perspective is still a necessary step for determining the appropriateness of such models.
Conclusions
The method of BMA appears to be a suitable analysis approach for studies involving a large number of predictors with a small sample. Through BMA, we were able to identify factors associated with changes in Veterans' QoL during long‐term post‐deployment reintegration over four and eight months following study entry. These factors (e.g. race, unemployment, PTSD) may be useful targets for intervention aimed at assisting Veterans in achieving meaningful functional recovery following warzone service and provide insight into the specific areas of dysfunction needing greater attention that will increase Veterans' QoL over time.
Findings from the current investigation have several clinical implications. First, it is imperative to continue to develop more effective treatments for commonly‐occurring mental health conditions among OEF/OIF Veterans, as not all Veterans respond to current best practices for PTSD and depression. Yet, PTSD and depression have clear impacts on long‐term QoL, and clearly impact other factors that were demonstrated in our models to influence QoL (e.g. unemployment). The finding that unemployment negatively predicted QoL was not surprising, and is in keeping with VA's efforts to develop supported employment and education programs for returning Veterans. It seems reasonable to incorporate these treatments into the context of treatments that directly target mental health disorders. Such treatment programs are vital for Veterans who are returning to a struggling economy and attempting to successfully reintegrate following warzone service. Second, despite Veterans having an average time since deployment of 43 months, meaningful fluctuations in QoL were still observed. That is, different factors were associated with fluctuations in QoL over time. This finding suggests the importance of evaluating long‐term QoL, as well as having a malleable treatment approach that is flexible to the changing needs of Veterans over time to improve their QoL. Interestingly, involvement in individual treatment was not predictive of QoL; in some models group psychotherapy was associated with QoL, but negatively so. Clearly, additional research is needed to identify factors that are associated with particular modalities and characteristics of treatment, and how they may influence QoL over time.
Declaration of interest statement
The authors have no competing interests.
Acknowledgments
This study was supported by the Department of Veterans Affairs (VA) VISN 17 Center of Excellence for Research on Returning War Veterans and its support for Project SERVE (Study Evaluating Returning Veterans Experiences) awarded to Sandra B. Morissette, PhD; a Merit Award (I01RX000304) to Dr Morissette from the Rehabilitation Research and Development Service of the VA Office of Research and Development entitled, “Functional Outcomes in OEF/OIF Veterans with PTSD and Alcohol Misuse”; the Central Texas Veterans Health Care System (CTVHCS); the Center for Applied Health Research; the Scott and White Healthcare System; VA VISN 17 New Investigator Award (“Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse”) and Career Development Award (1IK2CX000525‐01A1, “Gene x Environment Effects on PTSD”) to Dr Nathan Kimbrel from the Clinical Science Research and Development Service of the VA Office of Research and Development; and a VA VISN 17 New Investigator Award (“Experiential Avoidance, Neurocognition, and Functional Outcomes in PTSD”) to Dr Meyer. The authors would also like to acknowledge the contributions of our Veteran participants and research staff: Ellis Blackmore, Roberta Chrestman, Samantha Collum, Lianna Evans, PsyD, Yolanda Evans, Christina Fay, Brad Gary, Zachary Harned, Olivia Hobden, Marc Kruse, PhD, Ericka Saenz, Laurie Steffen, Skyy Walton, and Matthew Woodward.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the US Government, or Texas A&M Health Science Center.
Stock E. M., Kimbrel N. A., Meyer E. C., Copeland L. A., Monte R., Zeber J. E., Gulliver S. B. and Morissette S. B. (2014), A Bayesian model averaging approach to examining changes in quality of life among returning Iraq and Afghanistan Veterans, International Journal of Methods in Psychiatric Research, 23, pages 345–358, doi: 10.1002/mpr.1442
References
- American Psychiatric Association . (2000) Diagnostic and statistical manual of mental disorders (4th ed, Text Revision), Washington, DC, American Psychiatric Association. [Google Scholar]
- Amir M., Kaplan Z., Neumann L., Sharabani R., Shani N., Buskila D. (1997) Posttraumatic stress disorder, tenderness and fibromyalgia. Journal of Psychosomatic Research, 42(6), 607–613. [DOI] [PubMed] [Google Scholar]
- Baker D.G., Heppner P., Afari N., Nunnink S., Kilmer M., Simmons A., et al (2009) Trauma exposure, branch of service, and physical injury in relation to mental health among U.S. veterans returning from Iraq and Afghanistan. Military Medicine, 174(8), 773–778. [PubMed] [Google Scholar]
- Burckhardt C.S., Anderson K.L. (2003) The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health and Quality of Life Outcomes, 1, 60 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC269997/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burckhardt C.S., Woods S.L., Schultz A.A., Ziebarth D.M. (1989) Quality of life of adults with chronic illness: a psychometric study. Research in Nursing and Health, 12(6), 347–354. [DOI] [PubMed] [Google Scholar]
- Burckhardt C.S., Anderson K.L., Archenholtz B., Hagg O. (2003) The Flanagan Quality Of Life Scale: evidence of construct validity. Health and Quality of Life Outcomes, 1, 59 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC269996/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett‐Zeigler I., Ilgen M., Valenstein M., Zivin K., Gorman L., Blow A., et al (2011) Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addict Behavior, 36(8), 801–806. [DOI] [PubMed] [Google Scholar]
- Candolo C., Davison A., Demetrio C. (2003) A note on model uncertainty in linear regression. Journal of the Royal Statistical Society. Series D (The Statistician), 52(2), 165–177. [Google Scholar]
- Caska C.M., Renshaw K.D. (2011) Perceived burden in spouses of National Guard/Reserve service members deployed during Operations Enduring and Iraqi Freedom. Journal of Anxiety Disorders, 25(3), 346–351. [DOI] [PubMed] [Google Scholar]
- Clyde M., George E.I. (2004) Model uncertainty. Statistical Science, 19(1), 81–94. [Google Scholar]
- Cohen J. (1988) Statistical Analysis for the Behavioral Sciences, Hillsdale, NJ, Laurence Erlbaum Associates. [Google Scholar]
- Copeland L.A., Zeber J.E., Bingham M.O., Pugh M.J., Noel P.H., Schmacker E.R., et al (2011) Transition from military to VHA care: psychiatric health services for Iraq/Afghanistan combat‐wounded. Journal of Affective Disorders, 130(1–2), 226–230. [DOI] [PubMed] [Google Scholar]
- Department of Veteran Affairs . (2007) Health Effects of Serving in Afghanistan and Iraq. http://www.ptsd.va.gov/public/pages/overview-mental-health-effects.asp [14 February 2012]
- Finley E.P., Zeber J.E., Pugh M.J., Cantu G., Copeland L.A., Parchman M.L., et al (2010) Postdeployment health care for returning OEF/OIF military personnel and their social networks: a qualitative approach. Military Medicine, 175(12), 953–957. [DOI] [PubMed] [Google Scholar]
- Flanagan J.C. (1978) A research approach to improving our quality of life. American Psychologist, 33(2), 138–147. [Google Scholar]
- Griffith J., West C. (2010) The Army National Guard in OIF/OEF: relationships among combat exposure, postdeployment stressors, social support, and risk behaviors. Applied and Preventive Psychology, 14(1–4), 86–94. [Google Scholar]
- Gros D.F., Strachan M., Ruggiero K.J., Knapp R.G., Frueh B.C., Egede L.E., et al (2011) Innovative service delivery for secondary prevention of PTSD in at‐risk OIF‐OEF service men and women. Contempory Clinical Trials, 32(1), 122–128. [DOI] [PubMed] [Google Scholar]
- Hayes J., Wakefield B., Andresen E.M., Scherrer J., Traylor L., Wiegmann P., et al (2010) Identification of domains and measures for assessment battery to examine well‐being of spouses of OIF/OEF veterans with PTSD. Journal of Rehabilitation Research and Development, 47(9), 825–840. [DOI] [PubMed] [Google Scholar]
- Hoeting J., Madigan D., Raftery A., Volinsky C. (1999) Bayesian model averaging: a tutorial. Statistical Science, 14(4), 382–401. [Google Scholar]
- Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. (2004) Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. [DOI] [PubMed] [Google Scholar]
- Hoge C.W., Auchterlonie J.L., Milliken C.S. (2006) Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA, 295(9), 1023–1032. [DOI] [PubMed] [Google Scholar]
- Horvath R. (2011) Research & development and growth: a Bayesian model averaging analysis. Economic Modelling, 28(6), 2669–2673. [Google Scholar]
- Keane T.M. (2011) Responding to the psychological needs of OEF‐OIF military: a commentary on progress in treatment development. Cognitive and Behavioral Practice, 18(1), 144–148. [Google Scholar]
- Khaylis A., Polusny M.A., Erbes C.R., Gewirtz A., Rath M. (2011) Posttraumatic stress, family adjustment, and treatment preferences among National Guard soldiers deployed to OEF/OIF. Military Medicine, 176(2), 126–131. [DOI] [PubMed] [Google Scholar]
- Lamon E. III, Malve O., Pietilainen O. (2008) Lake classification to enhance prediction of eutrophication endpoints in Finnish lakes. Environmental Modelling & Software, 23(7), 938–947. [Google Scholar]
- Madigan D., Raftery A. (1994) Model selection and accounting for model uncertainty in graphical models using Occam's Window. Journal of the American Statistical Association, 89(428), 1535–1546. [Google Scholar]
- Milliken C.S., Auchterlonie J.L., Hoge C.W. (2007) Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA, 298(18), 2141–2148. [DOI] [PubMed] [Google Scholar]
- Morissette S.B., Woodward M., Kimbrel N.A., Meyer E.C., Kruse M.I., Dolan S., et al (2011) Deployment‐related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabilitation Psychology, 56(4), 340–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M., Okalo B. (2009) Severe declines of ant‐following birds in African rainforest fragments are facilitated by a subtle change in army ant communities. Biological Conservation, 142(10), 2050–2058. [Google Scholar]
- Pietrzak R.H., Southwick S.M. (2011) Psychological resilience in OEF‐OIF Veterans: application of a novel classification approach and examination of demographic and psychosocial correlates. Journal of Affective Disorders, 133(3), 560–568. [DOI] [PubMed] [Google Scholar]
- Pietrzak R.H., Goldstein M.B., Malley J.C., Rivers A.J., Johnson D.C., Southwick S.M. (2010) Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders, 123(1–3), 102–107. [DOI] [PubMed] [Google Scholar]
- Pittman J.O., Goldsmith A.A., Lemmer J.A., Kilmer M.T., Baker D.G. (2012) Post‐traumatic stress disorder, depression, and health‐related quality of life in OEF/OIF veterans. Quality of Life Research, 21(1), 99–103. [DOI] [PubMed] [Google Scholar]
- Raftery A. (1995) Bayesian Model Selection in Social Research. Sociological Methodology, 25, 111–163. http://www.stat.washington.edu/raftery/Research/PDF/socmeth1995.pdf [Google Scholar]
- Raftery A. (1999) Bayes Factors and BIC. Sociological Methods & Research, 27(3), 411–427. [Google Scholar]
- Raftery A., Madigan D., Hoeting J. (1997) Bayesian model averaging for linear regression models. Journal of the American Statistical Association, 92(437), 179–191. [Google Scholar]
- Raftery A., Painter I., Volinsky C. (2005) BMA: An R package for Bayesian model averaging. R News, 5(2), 2–8. [Google Scholar]
- Raftery A., Hoeting J., Volinsky C., Painter I., Yeung K.Y. (2010) BMA: Bayesian Model Averaging. R Package, version 3.13. http://CRAN.R-project.org/package=BMA
- Schnurr P.P., Lunney C.A., Bovin M.J., Marx B.P. (2009) Posttraumatic stress disorder and quality of life: extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review, 29(8), 727–735. [DOI] [PubMed] [Google Scholar]
- Schwarz G. (1978) Estimating the dimension of a model. Annals of Statistics, 6(2), 461–464. [Google Scholar]
- Sheppard S.C., Malatras J.W., Israel A.C. (2010) The impact of deployment on U.S. military families. American Psychology, 65(6), 599–609. [DOI] [PubMed] [Google Scholar]
- St‐Louis V., Clayton M.K., Pidgeon A.M., Radeloff V.C. (2012) An evaluation of prior influence on the predictive ability of Bayesian model averaging. Oecologia, 168, 719–726. [DOI] [PubMed] [Google Scholar]
- Tanielian T., Jaycox L.H., Schell T.L., Marshall G.N., Burnam M.A., Eibner C., Karney B.R., Meredith L.S., Ringel J.S., Vaiana M.E. (2008) Invisible Wounds of War: Summary and Recommendations for Addressing Psychological and Cognitive Injuries. Santa Monica, CA, RAND. [Google Scholar]
- Vasterling J.J. (2008) TBI screening interview [Unpublished measure]. Boston, MA, VA Boston Healthcare System. [Google Scholar]
- Veterans Health Administration . (2012) Analysis of VA Health Care Utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans. http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtr3.pdf [6 February 2013].
- Weaver F.M., Burns S.P., Evans C.T., Rapacki L.M., Goldstein B., Hammond M.C. (2009) Provider perspectives on soldiers with new spinal cord injuries returning from Iraq and Afghanistan. Archives of Physical Medicine and Rehabilitation, 90(3), 517–521. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (1948) Constitution of the World Health Organization, Geneva, World Health Organization. [Google Scholar]
- Zeber J.E., Noel P.H., Pugh M.J., Copeland L.A., Parchman M.L. (2010) Family perceptions of post‐deployment healthcare needs of Iraq/Afghanistan military personnel. Mental Health in Family Medicine, 7(3), 135–143. [PMC free article] [PubMed] [Google Scholar]


