Abstract
Objective
A substantial proportion of the more than 2 million service members who have served in Operations Enduring Freedom and Iraqi Freedom (OEF/OIF) have experienced a traumatic brain injury (TBI). Understanding the long-term impact of TBI is complicated by the non-specific nature of postconcussive symptoms (PCS) and the high rates of co-occurrence among TBI, posttraumatic stress disorder (PTSD), and depression. The goal of the present research was to examine the relations among TBI, persistent PCS, and symptoms of PTSD and depression among returning OEF/OIF Veterans.
Design
Two-hundred and thirteen OEF/OIF Veterans (87% male) completed a semi-structured screening interview assessing deployment-related TBI and current, persistent PCS. Participants also completed self-report measures of combat exposure and current symptoms of PTSD and depression.
Results
Nearly half (46%) of sampled Veterans screened positive for TBI, the majority of whom (85%) reported at least one persistent PCS after removing PCS that overlapped with PTSD and depression. Veterans with deployment-related TBI reported higher levels of combat exposure and symptoms of PTSD and depression. Structural equation modeling was used to assess the fit of three models of the relationships among TBI, combat exposure, persistent PCS, PTSD, and depression. Consistent with hypotheses, the best fitting model was one in which the effects of TBI on both PTSD and depression were fully mediated by non-overlapping persistent PCS.
Implications
These findings highlight the importance of addressing persistent PCS in order to facilitate the functional recovery of returning war Veterans.
Understanding the long-term effects of traumatic brain injury (TBI) has important public health implications. Estimates suggest that one to two million Americans sustain a TBI annually (Faul, Xu, Wald, & Coronado, 2010; Gerberding & Binder, 2003; Sosin, Sniezek, & Thurman, 1996; Thurman, Alverson, Dunn, Guerrero, & Sniezek, 1999; Thurman & Guerrero, 1999). Moreover, the large number of Veterans of the wars in Iraq and Afghanistan add to the global incidence of TBI. Since the inception of the current conflicts in Iraq and Afghanistan, more than two million U.S. troops have been deployed as part of Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF; Defense Manpower Data Center, 2009). Due to the increased use of improvised explosive devices (IEDs) by enemy combatants as well as improvements in the protective equipment of military personnel, OEF and OIF Veterans are more likely than previous generations of Veterans to experience and survive a TBI during deployment (Vasterling, Verfaellie, & Sullivan, 2009). Data from the Armed Forces Health Surveillance Center (2011) has identified 212,742 cases of TBI in all Armed Forces members, with 76.7% classified as mild, 16.8% classified as moderate, and 1.1% classified as severe. This is consistent with the proportion of TBIs classified as mild among civilians, which is estimated to be approximately 80% (Thurman et al., 1999). Due to its high incidence rate, most research to date concerning TBI among OEF/OIF Veterans has focused on mild traumatic brain injury (mTBI). For example, Hoge et al. (2008) found that 15% of a sample of 2,500 returning soldiers reported injuries consistent with mTBI.
Sequelae associated with sustaining a TBI vary significantly and may include cognitive problems, physical pain and impairment, as well as mental health problems such as depression and posttraumatic stress disorder (PTSD; Hoge et al., 2008). Self-reported, post-injury cognitive, affective, and somatic symptoms are collectively referred to as postconcussive symptoms (PCS). PCS include headaches, dizziness, memory problems, balance problems, sleep difficulties, and irritability. Although the majority of individuals who sustain a mTBI recover—even without targeted intervention (Dikman Machamer, & Temkin, 2001; Hessen, Nestvold, & Anderson, 2007)—approximately 6-15% experience persistent or permanent symptoms or disabilities (Stein & McAllister, 2009; Thurman et al., 1999; Vanderploeg, Curtiss, Luis, & Salazar, 2007; Zaloshnja, Miller, Langlois, & Selassie, 2008).
In general, following sports-related mTBI, post-injury cognitive effects (i.e., performance on neuropsychological tests) tend to resolve within 5-7 days (Guskiewicz et al., 2003), and PCS generally resolve within 2 weeks (Carroll et al., 2004). For mTBIs arising from non-sports-related events, post-injury cognitive effects tend to resolve within several weeks to 3 months (e.g., Belanger, Curtis, Demery, Lebowitz, & Vanderploeg, 2005; Carroll et al., 2004); however, PCS following mTBI may persist for one year post-injury or longer in adult civilian (Carroll et al., 2004) and Veteran (Stein & McAllister, 2009) samples. Despite the expectation of full recovery in most cases, a study of 609 individuals with mild to severe TBI demonstrated that, on average, life satisfaction declined over the first five years following TBI (Resch et al., 2009). Further, the rate of decline in life satisfaction was more pronounced among those with greater functional impairment, even though injury severity was only modestly correlated (r = .20) with functional impairment (Resch et al., 2009). Evidence also suggests that the onset of depression following TBI plays an important role in life satisfaction during the first five years post-injury (Underhill et al., 2003).
Understanding the long-term impact of TBI on functioning of military personnel and Veterans is a high priority within the Departments of Defense and Veterans Affairs (Jaffee & Meyer, 2009). However, understanding the specific long-term effects of TBI on persistent PCS and functional impairment is complicated by several factors. First, sleep problems and irritability—two of the most common PCS—directly overlap with the diagnostic features of PTSD and depression (APA, 2000). Second, the etiology of persistent PCS is unclear, as PCS are often associated with injuries other than head injuries (Lees-Haley, Fox, & Courtney, 2001; Meares et al, 2011), chronic pain (Iverson & McCracken, 1997), headaches (Hollnagle & Norrelund, 1980), depression (Iverson, 2006), and posttraumatic stress (Meares et al., 2011). For example, a recent study of 120 consecutive admissions to a trauma hospital found equivalent rates of PCS between people who had experienced a mTBI and non-brain-injured controls immediately post-injury and at 3-month follow-up (Meares et al., 2011). This study found that new PCS emerged during the follow-up period for 39% of the sample and that the relationship between PCS and PTSD symptoms strengthened over time (Meares et al., 2011). Third, high rates of psychopathology have been observed among people with mTBI. Carlson et al. (2010) found that 80% of OEF/OIF Veterans with a TBI had a psychiatric diagnosis. Moreover, mTBI is associated with elevated rates of PTSD in OEF and OIF Veterans. Whereas the overall prevalence of probable co-occurring mTBI and PTSD among OEF/OIF Veterans is 5-7%, the rate of probable PTSD among those with probable mTBI is 33-39% (Carlson et al., 2011). Notably, the overall prevalence of PTSD in OEF/OIF military personnel is estimated to be 6-25%, and PTSD has been associated with a range of functional difficulties, including occupational and social impairment, physical health problems, neuropsychological impairment, and substance use (Brenner et al., 2010; Hoge et al., 2004; Miliken, Auchterlonie, & Hoge, 2007; Thomas et al., 2010). In addition, it is important to keep in mind that the published prevalence estimates of PTSD, as well as other mental health conditions, may be underestimates given that only 50% of separated OEF/OIF Veterans obtain health care services within the VA (VHA Office of Public Health and Environmental Hazards, 2010).
Hoge et al. (2008) reported significantly elevated rates of major depression among Soldiers returning from deployment to Iraq who sustained mTBI with loss of consciousness (22.9%) compared to those with other injuries (6.6%). In this study, there was not a significantly elevated risk of depression among those with mTBI with alterations in, but not loss of, consciousness (8.4%; Hoge et al., 2008). Among civilians, estimates of depression following TBI range widely from 10-77% (see review by Alderfer, Arciniegas, & Silver, 2005). A prospective, longitudinal study found that 33-42% of people who sustained a TBI met criteria for major depressive disorder within one year post-injury (Jorge et al., 1993; 2004). In a more recent study, the incidence of new-onset depression was 18% within the first year following mTBI (Rao et al., 2010). Although the risk of developing depression was greatest during the first year following a TBI, the risk of developing depression remained elevated for decades (Alderfer et al., 2005). Additionally, depression following TBI is associated with elevated rates of self-reported PCS (Fann, Katon, Uomoto, & Esselman, 1995; Rapoport, McCullah, Streiner, & Feinstein., 2003), as well as aggression, suicidality, and cognitive impairment (Fann et al., 1995; Fann, Uomoto, & Katon, 2001; Hibbard, Uysal, Kepler, Bogdany, & Silver, 1998; Rapoport, McCullagh, Shammi, & Feinstein, 2005). Conversely, perceptions of impaired functioning following TBI may lead to worsening of depressive symptoms (Pagulayan, Hoffman, Temkin, Machamer, & Dikmen, 2008).
Further complicating matters is the finding that TBI and psychopathology may develop following exposure to the same critical event and that war Veterans are often exposed to multiple critical events, making the relations among these problems particularly challenging to disentangle (Stein & McAllister, 2009). Hoge and colleagues (2008) found that, although mTBI predicted greater PCS and a range of health problems and functional outcomes among OEF/OIF Veterans, these relations, except for the associations between mTBI and headache, became nonsignificant after controlling for symptoms of PTSD and depression. Similarly, in a sample of 2,235 OEF/OIF Veterans, PTSD proved to be a better predictor of PCS than mTBI, even after overlapping symptoms of PTSD and PCS were removed (Schneiderman, Braver, & Kang, 2008). Belanger, Kretzmer, Vanderploeg and French (2010) likewise found that TBI was significantly related to PCS, but the association disappeared after controlling for PTSD severity, suggesting that symptom complaints in mTBI may be related to emotional distress. Conversely, in a separate study, these authors found that mTBI was associated with PCS even after controlling for PTSD and suggested that PTSD and mTBI have independent additive contributions to the presentation of PCS, with PTSD having a stronger effect on current symptoms (Vanderploeg, Belanger, & Curtiss, 2009). Notably, the presence of a mTBI was associated with lower likelihood of recovery from PTSD over time (Vanderploeg et al., 2009). Finally, although there is clear evidence that mTBI is associated with greater risk for PTSD and other mood disturbances following trauma exposure (see Vasterling, Verfaellie & Sullivan, 2009 for a review), few studies have evaluated possible mechanisms that could account for why mTBI increases this risk.
Study Objectives
Because PCS are associated with a range of injuries and conditions, more research is needed to understand what factors are associated with the presence of persistent PCS in the months and years following TBIs when most PCS would be expected to have resolved (Howe 2009). Whether persistent PCS reflect a subtle neurological injury or the development of psychiatric sequelae remains a largely open question (Peskind et al., 2011; Schneiderman et al., 2008). Thus, characterizing the relations among TBI, persistent PCS, and psychopathology has important implications for understanding how best to assess and treat returning war Veterans. Accordingly, the primary goal of the present research was to examine and test the fit of different models of the associations among TBI, persistent PCS, PTSD, and depression in a sample of returning OEF/OIF Veterans. Based on the proximal association between TBI and PCS (i.e., sustaining a TBI is the first criterion to be met when diagnosing a post-concussional disorder; APA, 2000) and data supporting a strong association between persistent PCS, PTSD, and depression, we hypothesized that the influence of TBI on PTSD and depression would be fully mediated by persistent PCS. That is, we predicted that the influence of TBI on PTSD and depression symptoms would no longer be significant after accounting for the effects of PCS. To examine this hypothesis, this primary full mediation model was compared with a partial mediation model in which TBI was allowed to have both direct and indirect effects on PTSD and depression, and an alternative full mediation model in which we examined whether PTSD and depression symptoms mediated the effects of TBI on PCS to determine which model provided the best overall fit to the data within this sample of returning war Veterans.
Method
Participants
Participants in the current report were 213 OEF/OIF returning war Veterans who were recruited for one of two assessment studies. Data were collected between May of 2009 and August of 2010 (n = 132), and from August of 2010 until April of 2011 (n = 81), respectively. Exclusion criteria were identical for the two studies and included: (1) meeting diagnostic criteria for a bipolar or psychotic disorder; (2) being identified as currently at risk for suicide or homicide; or (3) having initiated psychiatric medications or psychotherapy within the preceding three months. The percentage of participants who screened positive for TBI did not differ significantly between the first (47.0%; 62/132) and second (44.4%; 36/81) studies, χ2 (1) = 0.13, ns. Consequently, data were collapsed across the two studies to form the final sample of 213 Veterans.
The combined sample was predominantly male (87%) with 60% self-identifying as White, 24% as Hispanic/Latino, 23% as African-American, 4% as American Indian/Alaska Native, 2% as Asian-American (2%), 1% as Hawaiian/Pacific-Islander, and 10% as “Other” (racial/ethnic categories were not mutually exclusive). Participants averaged 38.0 years of age (SD = 10.2) and reported completing 14.0 years of education (SD = 2.3). The majority of participants were Army Veterans (84.0%), with 14.1% reporting service in the National Guard, 7.3% in the Marine Corps, and 4.4% each in the Air Force and Navy (categories were not mutually exclusive). The majority of Veterans reported having served as part of active duty service (97.1%), with 2.9% reporting reserve service only, and 31.1% reporting both active duty and reserve service. Veterans reported being deployed on average 2.0 times (SD = 1.2; range 1-7) in support of OEF/OIF, with 94.7% reporting military service in Iraq, 15.0% in Afghanistan, and 29.7% in other countries (e.g., Kuwait, Germany). A large percentage (70.6%) of Veterans reported being awarded a service-connected disability due to a physical injury; 33.8% reported receiving a mental health-related service-connected disability.
Procedures
All procedures were reviewed and approved by the local Institutional Review Board prior to data collection. Participants were recruited through direct mailings, advertisements at enrollment sites and Veterans’ service organizations, and through in-service presentations to primary care, mental health, and OEF/OIF program staff. Recruitment was targeted toward over-sampling Veterans with mental health diagnoses. Following informed consent, participants completed the study procedures in private offices within the VA medical center. Interviews were used to assess for TBI and persistent PCS. Self-report measures were used to assess basic demographic information, combat exposure, and symptoms of PTSD and depression.
Measures
Assessment of Traumatic Brain Injury
Veterans were screened for possible deployment-related TBI using either the Brief Traumatic Brain Injury Screen (BTBIS; Schwab et al., 2006) utilized by the Defense and Veterans Brain Injury Center (DVBIC; n = 132) or the TBI screening interview developed by Vasterling (Vasterling, 2008; n = 81). These semi-structured screening interviews were conducted by trained clinicians. Veterans screened positive for TBI based on endorsement of a head injury during deployment (e.g., from a blast, vehicular accident, fall, bullet, fragment) that led to an alteration of consciousness (e.g., being disoriented, “dazed”, or confused, seeing “stars”), loss of consciousness, or post-traumatic amnesia. As two prior studies of OEF/OIF Veterans and service members found that blast-related TBI did not lead to greater reports of PCS than TBI following nonblast mechanisms (Lippa, Pastorek, Benge, & Thornton, 2010; Wilk et al., 2010), we did not differentiate TBIs according to different mechanisms of injury. In most cases, information obtained from follow-up questions was used to make post hoc determinations of the severity of TBIs in accordance with the American Congress of Rehabilitation Medicine (ACRM) guidelines (Mild Traumatic Brain Injury Committee, 1993). Specifically, deployment-related TBIs were classified as mild based on: (a) alteration of consciousness, (b) loss of consciousness lasting less than 30 minutes, and/or (c) the presence of post-traumatic amnesia lasting for less than 24 hours. TBIs were classified as moderate based on loss of consciousness for longer than 30 minutes but less than one week or post-traumatic amnesia for longer than 24 hours but less than one week. TBIs were categorized as severe based on loss of consciousness or post-traumatic amnesia lasting longer than one week. As the BTBIS is designed to identify service members who would benefit from additional evaluation for TBI (Schwab et al., 2006) and does not directly assess post-traumatic amnesia or loss of consciousness for longer than 30 minutes, Veterans who screened positive for a TBI but endorsed either not remembering the injury and/or reported loss of consciousness for longer than 20 minutes on this assessment were not classified in this study due to insufficient information to make a severity rating.
Persistent Postconcussive Symptoms
The presence of five persistent PCS was evaluated for each Veteran who screened positive for TBI: dizziness or balance problems, headaches, memory difficulties, sleep problems, and irritability. These five symptoms were selected based on their inclusion in both of the TBI assessment tools described above. PCS were scored as present if the Veteran reported that s/he currently experiences the symptom. In order to minimize overlap between persistent PCS and symptoms of PTSD and depression, sleep problems and irritability were not included in the persistent PCS summary variable. Thus, the final persistent PCS summary variable ranged from 0 (no endorsement of PCS) to 3 (endorsement of all three PCS: headaches, balance problems or dizziness, and memory problems). With the exception of sleep problems, these final 3 symptoms are consistent with results from Vanderploeg et al. (2009) who demonstrated that mTBI was associated with headaches, memory problems and fainting, after controlling for PTSD and other psychiatric problems. Internal consistency (Chronbach's alpha) for this three-item persistent PCS scale was .81 in this sample.
PTSD Symptoms
The PTSD Checklist - Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993) is a widely-used self-report measure of military-related PTSD symptoms experienced during the past month. The 17 items of the PCL-M assess the 17 symptoms of PTSD identified in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychiatric Association, 2000). The PCL-M has demonstrated excellent internal consistency and validity in prior research (Blanchard, Jones-Alexander, Buckley, and Forneris, 1996; Weathers et al., 1993). Across studies of Veterans, PCL cut off scores to screen for PTSD range from 28-60, with lower scores tending to be observed among studies of women or within primary care settings (Keen, Kutter, Niles & Krinsley, 2008). Generally, a cut-off score of 50 is used among studies of male Vietnam Veterans (Forbes, Creamer & Biddle, 2001; Weathers et al., 1993). In the current study, internal consistency for the PCL-M was .97.
Depression
The Beck Depression Inventory - II (BDI-II; Beck, Steer, & Brown, 1996) assessed depressive symptoms during the past two weeks. The BDI-II is a widely-used self-report measure that contains 21 items rated on a 4-point Likert scale. Scores of 0-10 are considered to be within the normal range, scores of 11-16 indicate mild mood disturbance, 17-20 indicate borderline clinical depression, 21-30 indicate moderate depression, 31-40 indicate severe depression, and scores greater than 40 indicate extreme depression. The BDI-II has demonstrated excellent psychometric properties in prior research (e.g., Beck, Steer, Ball, & Ranieri, 1996; Beck, Steer, & Brown, 1996). Internal consistency for the BDI-II in the current study was .95.
Combat Exposure
The Full Combat Exposure Scale (FCES; Hoge et al., 2004) is an 18-item self-report measure of combat experiences during land combat situations. A wide range of combat scenarios are assessed by the FCES, including elements of combat exposure (e.g., being attacked or ambushed, handling human remains, receiving incoming mortars) that are highly relevant to the OEF/OIF conflicts. Internal consistency of the FCES in the current study was .92.
Results
Participant Characteristics
Of the 98 (46.0%) Veterans who screened positive for a TBI based on the most severe head injury they experienced during deployment, the majority of TBIs were classified post-hoc as mild (85.7%, n = 84). Two (2.0%) were classified as moderate TBIs based on self-reported loss of consciousness for longer than 30 minutes. Twelve (12.2%) TBIs were not classified due to insufficient information to rule out loss of consciousness for longer than 30 minutes or determine whether the Veteran experienced post-traumatic amnesia. Among those who screened positive for a deployment-related TBI, 15.3% denied any current PCS that did not overlap with PTSD or depression, 25.5% reported one current non-overlapping PCS, 19.4% reported two current non-overlapping PCS, and 39.8% endorsed all three current non-overlapping PCS.
Group Comparisons
Between-groups analyses were conducted to examine potential differences between participants who screened positive and negative for TBI (see Table 1). Male Veterans were significantly more likely to screen positive for TBI (50.8% vs. 14.3%), χ2 = 13.061, p < .001, and there was a non-significant trend suggesting that White Veterans were also more likely endorse TBI (51.2% vs. 37.2%), χ2 = 3.861, p = .051. Although the reason for the non-significant racial trend is not clear, the difference in TBI screen status between males and females may be attributable to lower levels of self-reported combat exposure among female Veterans relative to male Veterans, F (1, 206) = 5.85, p = .016. Whites and non-Whites did not, however, differ in terms of combat exposure, F (1, 200) = 1.49, p = .22. Whereas there were no significant group differences on age, F (1, 211) = 2.03, p = .16; Veterans who screened positive for TBI reported significantly lower levels of education, F (1, 203) = 5.47, p = .020, higher levels of combat exposure, F (1, 206) = 75.508 p < .001, more symptoms of PTSD, F (1, 200) = 42.02, p < .001, and more symptoms of depression, F (1, 201) = 16.08 p < .001, than did Veterans who screened negative for TBI.
Table 1.
Sample Demographic Characteristics
| No TBI (n = 115) | TBI (n = 98) | Test Statistic | |
|---|---|---|---|
| Gender (% male) | 79.1% | 95.9% | χ2 (1) = 13.061, p < .001 |
| Race (% White) | 55.9% | 69.1% | χ2 (1) = 3.816, p = .051 |
| Age | 38.9 (10.9) | 36.9 (9.4) | F (1, 211) = 2.029, ns |
| Years of Education | 14.3 (2.6) | 13.6 (1.8) | F (1, 203) = 5.469, p < .05 |
| PCI-M | 36.7 (17.7) | 53.2 (17.8) | F (1, 200) = 42.019, p < .001 |
| BDI-II | 13.2 (12.0) | 21.2 (13.4) | F (1, 201) = 16.084 p < .001 |
| Combat Exposure | 16.1 (9.8) | 32.2 (15.6) | F (1, 206) = 75.508 p < .001 |
Structural Equation Modeling
Structural equation modeling (SEM) was used to examine the hypothesis that persistent PCS fully mediate the effects of TBI exposure on symptoms of PTSD and depression in a sample of returning OEF/OIF Veterans. SEM was conducted with AMOS (Arbuckle, 2006). Consistent with best practices, maximum likelihood estimation was used to estimate parameters (Enders, 2010). The proportion of missing data was relatively low (3.9%). There were no missing data for TBI or PCS.
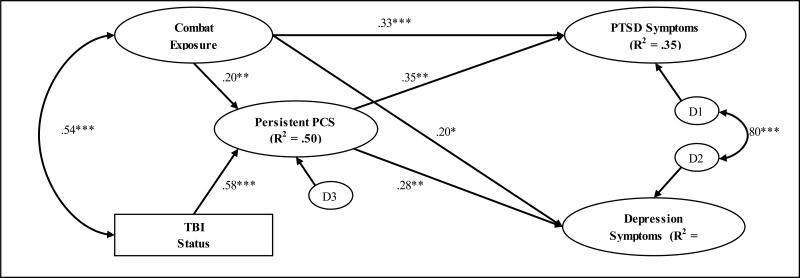
A simplified version of the hypothesized full mediation model is displayed in Figure 1. Partial disaggregation (i.e., using item parcels as indicators) was used to optimize the fit of the measurement models for the PTSD, depression, and combat exposure latent variables, as this technique is appropriate for relatively smaller sample sizes and is less prone to measurement error and sample specificity (Bagozzi & Heatherton, 1994; Leone, Perugini, Bagozzi, Pierro, & Manneti, 2001). The indicators for the PTSD latent variable were the sums of PCL scores on the Cluster B/Re-experiencing (items 1 - 5), Cluster C/Avoidance/Numbing (items 6 - 12), and Cluster D/Hyperarousal (13 - 17) symptoms. The depression latent variable was comprised of three parcels of seven items each from the BDI-II that were created by summing every third item on the measure (i.e., the first parcel was the sum of items 1, 4, 7, 10, 13, 16, & 19; the second was the sum of items 2, 5, 8, 11, 14, 17, & 20; and the third was the sum of items 3, 6, 9, 12, 15, 18, & 21). The combat exposure latent variable was composed of three parcels of six items each from the FCES which were also created by summing every third item (e.g., the first parcel was created by summing items 1, 4, 7, 10, 13, & 16). The three PCS symptoms (headaches, balance problems, memory problems) were used as indicators on the PCS latent variable. TBI status was modeled as an observed categorical variable (0 = no TBI, 1 = sustained TBI). With respect to the structural aspects of the hypothesized model, combat exposure and TBI status were allowed to freely covary as were the disturbance terms for PTSD and depression symptoms, as positive relationships between both were expected. To account for the effects of combat exposure, a well-known and robust predictor of the variables of interest, combat exposure was modeled as a predictor of persistent PCS, PTSD, and depression. Finally, PCS was regressed onto TBI, and, in turn, both PTSD and depression were regressed onto PCS.
Figure 1.
Hypothesized structural equation model (Model 1) designed to test the hypothesis that persistent PCS fully mediate the effects of TBI on PTSD and depression symptoms. Standardized maximum likelihood estimates are shown (N = 213).
As can be seen in Table 2, the hypothesized full mediation model (Model 1) showed close fit to the data (e.g., Kline, 2005; Hu & Bentler, 1999): χ2 (58) = 84.796, p = .012 (higher p-values indicate better fit, although close fitting models with large samples often lead to p-values < .05); Root Mean Square Error of Approximation (RMSEA) = .047 (close fit ≤ .05; adequate fit ≤ .08); Comparative Fit Index (CFI) = .988 (close fit ≥ .95; adequate fit ≥ .90); Tucker-Lewis Indices (TLI) = .981 (close fit ≥ .95; adequate fit ≥ .90); and Akaike Information Criterion (AIC) = 176.796 (lower score preferred). All factor loadings were high ( > .75) and statistically significant (p < .001), suggesting good measurement model fit. In addition, each of the hypothesized pathways was statistically significant (p < .01). Specifically, both TBI status, β = .58, p < .001, and combat exposure, β = .20, p < .01, had significant direct effects on persistent PCS, combining to account for 50% of the variance in this latent variable. In turn, persistent PCS was a significant predictor of symptoms of PTSD, β = .35, p < .001, and depression, β = .28, p < .01. Together, persistent PCS and combat exposure accounted for 35% of the variance in PTSD symptoms and 18% of the variance in depression symptoms. As hypothesized, TBI status had significant indirect effects on symptoms of PTSD, β = .20, p < .001, and depression, β = .16, p < .01, via persistent PCS, providing support for the hypothesis that the effects of TBI on PTSD and depression are fully mediated by persistent PCS.
Table 2.
Goodness-of-Fit Indices for the Different Structural Equation Models
| Full Sample (N = 213) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | χ 2 | df | p | CFI | TLI | AIC | RMSEA | RMSEA Lower 90% CI | RMSEA Upper 90% CI |
| Model 1: Hypothesized Full Mediation Model | 84.796 | 58 | .012 | .988 | .981 | 176.796 | .047 | .022 | .067 |
| Model 2: Partial Mediation Model | 84.682 | 56 | .008 | .987 | .979 | 180.682 | .049 | .026 | .070 |
| Model 3: Alternative Mediation Model | 130.770 | 57 | <.001 | .966 | .946 | 224.770 | .078 | .061 | .096 |
| Remaining Sample after Excluding Moderate and Possibly Moderate TBIs (n = 199) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | χ 2 | df | p | CFI | TLI | AIC | RMSEA | RMSEA Lower 90% CI | RMSEA Upper 90% CI |
| Model 1: Hypothesized Full Mediation Model | 85.744 | 58 | .010 | .986 | .978 | 177.744 | .049 | .024 | .070 |
| Model 2: Partial Mediation Model | 85.660 | 56 | .007 | .985 | .975 | 181.660 | .052 | .028 | .073 |
| Model 3: Alternative Mediation Model | 130.046 | 57 | <.001 | .963 | .940 | 224.046 | .080 | .062 | .099 |
Note: df = degrees of freedom; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; AIC = Akaike Information Criterion; RMSEA = Root Mean Square Error of Approximation; CI = confidence interval.
The hypothesized full mediation model (Model 1) was also compared with a partial mediation model (Model 2) in which direct paths from TBI to PTSD and depression symptoms were added to the model. As can be seen in Table 2, the addition of the direct paths from TBI to PTSD and depression actually resulted in slightly worse model fit, χ2 (56) = 84.682, p = .008; RMSEA = .049; CFI = .987; TLI = .979; AIC = 180.682. Moreover, the paths from TBI to PTSD, β = .03, ns, and from TBI to depression, β = .01, ns, were both non-significant, and a chi-square difference test indicated that adding these paths did not improve overall model fit, χ2D = 0.114 (2), ns. Accordingly, the partial mediation model (Model 2) was rejected.
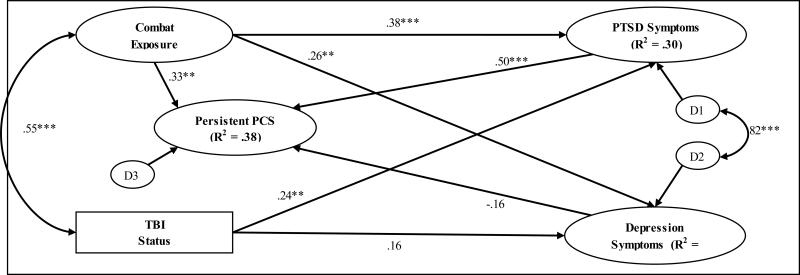
The hypothesized full mediation model (Model 1) was also compared to a model designed to test the competing hypothesis that PTSD and depression symptoms mediate the effects of TBI status on persistent PCS (Model 3). Model 3 was constructed to be identical to Model 1 with the following exceptions: (a) the direct paths from TBI to PCS, PCS to PTSD, and PCS to depression were removed; and (b) direct paths from TBI to PTSD, TBI to depression, PTSD to PCS, and depression to PCS were added (Figure 2). As summarized in Table 2, Model 3 demonstrated considerably worse fit to the data compared with Model 1 χ2 (57) = 130.770, p < .001; RMSEA = .078; CFI = .966; TLI = .946; AIC = 224.770. Further, the paths from TBI to depression, β = .16, p = .052, and from depression to persistent PCS, β = −.16, p = .244, both failed to reach statistical significance. Notably, Model 3 accounted for substantially less variance in persistent PCS (38% vs. 50%), PTSD (30% vs. 35%), and depression (14% vs. 18%) symptoms than Model 1, despite the fact that the same variables were used in both models. Because Models 1 & 3 were not nested (i.e., non-hierarchical), the chi-square difference test was not an appropriate statistic to use for comparison purposes (Kline, 2005); however, examination of AIC values for the two models revealed that Model 1 (AIC = 176.796) provided substantially better fit to the data than Model 3 (AIC = 224.770).
Figure 2.
Alternative structural equation model (Model 3) designed to test the competing hypothesis that PTSD and depression symptoms fully mediate the effects of TBI on persistent PCS. Standardized maximum likelihood estimates are shown (N = 213).
Finally, all three models were re-run after removing the fourteen participants identified with either moderate (n = 2) or possible moderate (n = 12) TBIs. As detailed in Table 2, the results from these analyses (n = 199) were nearly identical to those from the full dataset (N = 213) with the exception that the fit indices were predictably slightly worse given the 6.6% reduction in sample size (Kline, 2005). Moreover, the hypothesized full mediation model (Model 1) continued to demonstrate the best overall fit to the data, χ2 (58) = 85.744, p = .010; RMSEA = .049; CFI = .986; TLI = .978; AIC = 177.744, suggesting that the pattern of findings was not influenced by the inclusion of participants who experienced potentially more moderate TBIs.
Discussion
Consistent with the designation of TBI as one of the signature injuries of the war theatres in Iraq and Afghanistan, 46% of the returning Veterans recruited for this project screened positive for a deployment-related TBI. Further, of those who screened positive for a TBI, nearly 85% reported that they currently experienced at least one of the three persistent, non-overlapping post-concussive symptoms assessed in the study: headaches, balance problems/dizziness, and/or memory problems. As predicted, the presence of persistent PCS fully mediated the effects of TBI on current levels of PTSD and depression symptoms and better accounted for the relations among these variables compared to the two alternative hypotheses tested. Interestingly, despite debate in the literature as to whether persistent PCS are better explained by PTSD or other psychological disorders, Model 3, in which we examined whether PTSD and depression symptoms drove the relationship between TBI and persistent PCS, demonstrated significantly worse fit to the data than did Model 1. Moreover, comparison of these models revealed that whereas TBI and combat exposure combined to account for 50% of the variance in persistent PCS in Model 1, combat exposure, PTSD, and depression combined to account for less than 40% of the variance in persistent PCS in Model 3. These data strongly suggest that there is a direct relationship between TBI and persistent PCS that is not simply due to the frequent co-occurrence of TBI, PTSD, and depression. Indeed, the DSM-IV-TR (APA, 2000) explicitly states that a causal relationship must exist between TBI and PCS to diagnose post-concussional disorder. While data from other studies (Belanger et al., 2010; Schneidermann et al., 2008) support a model in which the relationship between mTBI and PCS is mediated by PTSD symptoms, our results suggest that PCS, as a mediator, is related to TBI in spite of self-reported symptoms of PTSD and depression.
The current findings add to a growing literature indicating that TBI confers increased risk for PTSD and depression among war Veterans (e.g., Carlson et al., 2011; Hoge et al., 2008; Vasterling et al., 2009) by evaluating mechanisms of action to explain this relationship. To our knowledge, this is the first published study to use SEM to directly compare competing models of the relations among TBI, persistent PCS, PTSD, and depression. Our findings provide insight into the nature of the associations among these variables and offer several important clinical and research implications. First, these findings suggest that it is the persistent experience of non-overlapping neurobehavioral symptoms that were reported to be either caused or exacerbated by the TBI, and not simply the experience of TBI exposure itself, that was predictive of current levels of psychopathology. This is particularly noteworthy in that, for the vast majority of individuals who experience a TBI, post-concussive symptoms are generally transient and are believed to resolve quickly (within days to a few months) and without direct clinical intervention. The current findings, however, suggest that within a sample of Veterans receiving care at VHA the experience of persistent PCS following TBI may be more common than previously reported in the literature. Further, the experience of persistent PCS appears to be an important mediator of the association between TBI exposure and reported symptoms of psychopathology. Moreover, persistent neurobehavioral sequelae of TBI (e.g., memory problems, headaches) may lead to worse long-term functional outcomes (e.g., occupational, social) among returning war Veterans. For example, they may contribute to poorer treatment outcomes by leading to increased symptoms of psychopathology (e.g., impaired concentration, irritability) and interfere with response to psychological treatments. In addition to increasing awareness of the importance of assessing for TBI and PCS, these findings highlight the potential benefits of evaluating and treating persistent PCS in Veterans with mental health difficulties.
An important caveat in interpreting the results is that our models were based on cross-sectional data. Well-designed longitudinal studies are needed to improve our understanding of the complex relations among TBI, persistent PCS, and psychopathology. Studies that evaluate military personnel prior to and following deployment may be of particular benefit. In this manner, the relations among persistent PCS, mental health problems, and functioning could be evaluated over time, including examining trajectories of functional recovery. Whereas relatively few published studies have focused on the impact of persistent PCS on depression in OEF/OIF Veterans to date, the high rates of suicide among Veterans (Bullman & Kang, 1996; Kang & Bullman, 2008) further highlight the importance of conducting research aimed at improving our understanding of the complex relations among these variables.
Several additional limitations of the current study should be noted. First, due to limitations in the BTBIS screening assessment, we were not able to classify all participants as having mild, moderate, or severe TBI. However, this limitation should be viewed within the context that there is considerable discussion in the field regarding how best to define criteria for both TBI and PCS (Barth, Ruff & Espe-Pfeifer, 2006) and the fact that the pattern of results were the same whether or not Veterans with moderate or possible moderate TBIs were included in the analyses. Second, to control for overlapping PCS and mental health symptoms we did not evaluate the predictive value of all possible symptoms that have been identified as PCS in the literature (e.g., ringing in the ears, sensitivity to bright light). Thus, this study reflects a subset of symptoms (headaches, balance/dizziness, memory difficulties) of the broader construct of post-concussive symptoms. Notably, the extremely high prevalence of ringing in the ears among war Veterans regardless of TBI status (Veterans Benefits Administration, 2010) would have been problematic in the current analyses. Furthermore, an advantage of the current study is that overlapping symptoms between TBI and psychopathology (i.e., irritability and sleep problems) were excluded to gain a better sense of the unique contribution of persistent PCS to PTSD and depression. Of note, memory difficulties were considered as a non-overlapping symptom in these analyses because they are not part of the diagnostic criteria for either PTSD or depression. In spite of this distinction, patients with PTSD and depression can certainly have cognitive and memory complaints (Burt, Zembar & Niederehe, 1995; Qureshi et al., 2011), although data do not necessarily support an exacerbating effect of PTSD on cognitive functioning in Veterans with mTBI (Gordon, Titzpatrick & Hilsabeck, 2011). Third, self-report measures of PTSD and depression symptoms were used. Whether the current findings would hold for clinical diagnoses of PTSD and depression is an important area for future research. Fourth, it is likely that the rates of TBI reported in the current study are inflated because our procedures included over-sampling for Veterans experiencing PTSD and depression, both of which co-occur at high rates with TBI among returning OEF/OIF Veterans (Hoge et al., 2004; 2008). In addition, because we did not assess the presence of symptoms included as PCS for Veterans who sustained injuries other than TBIs and who did not screen positive for TBI, we were not able to compare rates of these symptoms between Veterans who were exposed to TBI with those who were not. Such comparisons would be useful in examining the specific causal role of TBI in relation to PCS, particularly in light of findings demonstrating equivalent levels of PCS among individuals with TBI and non-brain-injured controls (Meares et al., 2011). Finally, lifetime history of head injuries, including injuries that occurred outside of, or prior to entry into the military, was not assessed. Therefore, the potential additive effects of non-military head injuries could not be evaluated within the current data set.
Collectively, these findings highlight the importance of routinely evaluating TBI and persistent PCS in the context of clinical management of mental health disorders. Due to the prevalence of these conditions in returning OEF/OIF Veterans, the Department of Veterans Affairs (DVA) has made significant efforts to better identify Veterans who have experienced a TBI, or who are struggling with PTSD or depression. For example, across medical and mental health clinics, DVA providers conduct a mandatory screening for these conditions. Moreover, co-located, collaborative mental health care has been embedded within many Primary Care Clinics (e.g., Pomerantz et al., 2010) to address these needs in a timely manner or to make referrals to specialty clinics, as appropriate. Identification within non-mental health care settings is important due to the significant stigma associated with mental health care among returning OEF/OIF Veterans (Wright et al., 2009). Moreover, frequent assessment as part of routine evaluations is critical given the potential for delayed onset or recognition of PTSD and depression. Specifically, most soldiers who meet criteria for PTSD or depression seven months following injury did not meet criteria for either disorder one month following injury (Grieger et al., 2006). Thus, it is imperative to assess and re-assess these conditions and whether they occur in the context of persistent PCS, especially given that our data, consistent with other studies of OEF/OIF Veterans (e.g., Carlson et al., 2011; Hoge et al., 2008), suggests that an alarming number of combat Veterans have sustained a TBI that may lead to persistent PCS, PTSD, and depression.
Although empirically-supported treatments for PTSD and depression are now widely available for Veterans across VA medical centers, these treatments have yet to be adapted for Veterans who are simultaneously struggling with persistent PCS, which is an important focus for future research (Najavits, Highley, Dolan & Fee, in press). To better understand the psychological and pathophysiological relationships among these conditions, future studies should incorporate structural and functional imaging techniques. For example, studies have demonstrated changes in neural activity following cognitive-behavioral treatments (CBT; e.g., Porto et al. e, 2009). The impact of CBT on the brain and treatment outcomes for PTSD and depression when the patient has a head injury has not been extensively studied to date, although evidence suggests that CBT is effective in treating acute stress disorder following mild TBI (Bryant, Moulds, Guthrie, & Nixon, 2003). Perhaps if PCS can be alleviated or prevented from becoming persistent, lower levels of PTSD and depressive symptoms would be observed over time. Unfortunately, treatments for PCS are limited and the timing, intensity and need for various treatment components remain unclear (Snell, Surgenor, Hay-Smith & Siegert, 2009). Moreover, although educational efforts may be beneficial if administered close in time with the injury (Snell et al., 2009), less is known about treatments for persistent PCS. Clearly, if persistent PCS (particularly headaches, balance problems or dizziness, and memory problems) are the mechanism accounting for the relationship between TBI and PTSD/depression, then improved treatments for persistent PCS need to be developed in order to better serve returning Veterans and others who have sustained TBIs.
Acknowledgements
This research was supported by the Department of Veterans Affairs (DVA) VISN 17 Center of Excellence for Research on Returning War Veterans, a Merit Award (I01RX000304) to Sandra B. Morissette, Ph.D. from the Rehabilitation Research and Development Service of the VA Office of Research and Development entitled, “Functional Outcomes in OEF/OIF Veterans with PTSD and Alcohol Misuse,” a DVA VISN 17 New Investigator Award to Nathan A. Kimbrel, Ph.D. entitled, “Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse,” and a DVA VISN 17 New Investigator Award to Eric C. Meyer, Ph.D. entitled, “Experiential Avoidance, Neurocognition, and Functional Outcomes in PTSD.” We would also like to acknowledge the contributions of our Veteran participants and research staff: Ellis Blackmore, Roberta Chrestman, Samantha Collum, Yolanda Evans, Christina Fay, Zachary Harned, Ericka Saenz, and Laurie Steffen.
References
- Alderfer BS, Arciniegas DB, Silver JM. Treatment of depression following traumatic brain injury. Journal of Head Trauma and Rehabilitation. 2005;20:544–562. doi: 10.1097/00001199-200511000-00006. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Revised 4th ed. Author; Washington, DC: 2000. [Google Scholar]
- Arbuckle J. Amos 7.0 User's Guide. Amos Development Corporation; Spring House, PA: 2006. [Google Scholar]
- Armed Forces Health Surveillance Center DoD numbers for traumatic brain injury [data file] 2011 Retrieved from http://www.dvbic.org/TBI-Numbers.aspx.
- Bagozzi RP, Heatherton TF. A general approach to representing multifaceted personality constructs: Application to state self-esteem. Structural Equation Modeling. 1994;1:35–67. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barth JT, Ruff R, Espe-Pfeifer P. Mild traumatic brain injury: Definitions. In: Young G, Kane AW, Nicholson K, editors. Psychological knowledge in court: PTSD, pain, and TBI. Springer Science + Business Media; New York, NY: 2006. pp. 271–278. doi:10.1007/0-387-25610-5_15. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories–IA and –II in psychiatric outpatients. Journal of Personality Assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. doi:10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 2nd ed. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Belanger HG, Curtiss G, Demery JA, Lebowitz BK, Vanderploeg RD. Factors moderating neuropsychological outcomes following mild traumatic brain injury: A meta-analysis. Journal of the International Neuropsychological Society. 2005;11:215–227. doi: 10.1017/S1355617705050277. [DOI] [PubMed] [Google Scholar]
- Belanger HG, Kretzmer T, Vanderploeg RD, French LM. Symptom complaints following combat-related traumatic brain injury: Relationship to traumatic brain injury severity and posttraumatic stress disorder. Journal of the International Neuropsychological Society. 2010;16(1):104–100. doi: 10.1017/S1355617709990841. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Brenner LA, Ivins BJ, Schwab K, Warden D, Nelson LA, Jaffee M, Terrio H. Traumatic brain injury, posttraumatic stress disorder, and postconcussive symptom reporting among troops returning from Iraq. The Journal of Head Trauma Rehabilitation. 2010;25(5):307–312. doi: 10.1097/HTR.0b013e3181cada03. doi:10.1097/HTR.0b013e3181cada03. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds M, Guthrie R, Nixon RD. Treating acute stress disorder following mild traumatic brain injury. The American Journal of Psychiatry. 2003;160:585–587. doi: 10.1176/appi.ajp.160.3.585. [DOI] [PubMed] [Google Scholar]
- Bullman TA, Kang HK. The risk of suicide among wounded Vietnam veterans. American Journal of Public Health. 1996;86:662–667. doi: 10.2105/ajph.86.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt DB, Zember MJ, Niederebe G. Depression and memory impairment: A meta-analysis of the association, its pattern, and specificity. Psychological Bulletin. 1995;117:285–305. doi: 10.1037/0033-2909.117.2.285. [DOI] [PubMed] [Google Scholar]
- Carlson KF, Kehle SM, Meis L, Greer N, MacDonald R, Rutks I, Sayer NA, Dobscha SK, Wilt TJ. Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: A systematic review of the evidence. Journal of Head Trauma and Rehabilitation. 2011;26:103–115. doi: 10.1097/HTR.0b013e3181e50ef1. [DOI] [PubMed] [Google Scholar]
- Carlson KF, Nelson D, Orazem RJ, Nugent S, Cifu DX, Sayer NA. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. Journal of Traumatic Stress. 2010;23(1):17–24. doi: 10.1002/jts.20483. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Peloso PM, Borg J, von Holst H, Holm L, et al. Prognosis for mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine. 2004;43:84–105. doi: 10.1080/16501960410023859. [DOI] [PubMed] [Google Scholar]
- Defense Manpower Data Center . OEF/OIF deployments since September 11th 2001 by component, gender, race, marital status, casualty status, deployment count and deployment days. Ezekiel Budda; Seaside, CA. Author: Dec 29, 2009. [Google Scholar]
- Dikman S, Machamer J, Temkin N. Mild head injury: Facts and artifacts. Journal of Clinical and Experimental Neuropsychology. 2001;23:729–738. doi: 10.1076/jcen.23.6.729.1019. [DOI] [PubMed] [Google Scholar]
- Enders CK. Applied missing data analysis. Guilford Press; New York: 2010. [Google Scholar]
- Fann JR, Katon WJ, Uomoto JM, Esselman PC. Psychiatric disorders and functional disability in outpatients with traumatic brain injuries. American Journal of Psychiatry. 1995;152:1493–1499. doi: 10.1176/ajp.152.10.1493. [DOI] [PubMed] [Google Scholar]
- Fann JR, Uomoto JM, Katon WJ. Cognitive improvement with treatment of depression following mild traumatic brain injury. Psychosomatics. 2001;42:48–54. doi: 10.1176/appi.psy.42.1.48. [DOI] [PubMed] [Google Scholar]
- Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. Retrieved from http://www.cdc.gov/traumaticbraininjury/tbi_ed.html. [Google Scholar]
- Forbes D, Creamer M, Biddle D. The validity of the PTSD checklist as a measure of symptomatic change in combat-related PTSD. Behaviour Research & Therapy. 2001;39:977–86. doi: 10.1016/s0005-7967(00)00084-x. [PMID: 11480838] [DOI] [PubMed] [Google Scholar]
- Gerberding JL, Binder S. National Center for Inquiry Prevention and Control. Centers for Disease Control and Prevention; Atlanta: 2003. Report to Congress on mild traumatic brain injury in the United States: Steps to prevent a serious public health problem. [Google Scholar]
- Gordon SN, Fitzpatrick PJ, Hilsabeck RC. No effect of PTSD and other psychiatric disorders on cognitive functioning in veterans with mild TBI. The Clinical Neuropsychologist. 2011;25(3):337–347. doi: 10.1080/13854046.2010.550634. Doi: 10.1080/13854046.2010.550634. [DOI] [PubMed] [Google Scholar]
- Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, Wain HJ. Posttraumatic stress disorder and depression in battle-injured soldiers. The American Journal of Psychiatry. 2006;163(10):1777–1783. doi: 10.1176/ajp.2006.163.10.1777. doi:10.1176/appi.ajp.163.10.1777. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: The NCAA Concussion Study. Journal of the American Medical Association. 2003;290:2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- Hessen E, Nestvold K, Anderson V. Neuropsychological function 23 years after mild traumatic brain injury: A comparison of outcome after pediatric and adult head injuries. Brain Injury. 2007:963–979. doi: 10.1080/02699050701528454. [DOI] [PubMed] [Google Scholar]
- Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J. Axis I psychopathology in individuals with traumatic brain injury. Journal of Head Trauma and Rehabilitation. 1998;13:24–39. doi: 10.1097/00001199-199808000-00003. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Coffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas J, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. The New England Journal of Medicine. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. doi:10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Hollnagel H, Norrelund N. Headache among 40-year olds in Glostrup: An epidemiological study. Ugeskr Laeger. 1980;142:3071–3077. [PubMed] [Google Scholar]
- Howe LLS. Giving context to post-deployment post-concussive-like symptoms: Blast-related potential mild traumatic brain injury and comorbidities. The Clinical Neuropsychologist.Special Issue: Injured Military Veterans. 2009;23(8):1315–1337. doi: 10.1080/13854040903266928. doi:10.1080/13854040903266928. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Iverson GL. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Archives of Clinical Neuropsychology. 2006;21(4):303–310. doi: 10.1016/j.acn.2005.12.008. doi:10.1016/j.acn.2005.12.008. [DOI] [PubMed] [Google Scholar]
- Iverson GL, Mccracken LM. Postconcussive symptoms in persons with chronic pain. Brain Injury. 1997;11(11):783–790. doi: 10.1080/026990597122990. doi:10.1080/026990597122990. [DOI] [PubMed] [Google Scholar]
- Jaffee MS, Meyer KS. A brief overview of traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) within the department of defense. The Clinical Neuropsychologist. Special Issue: Injured Military Veterans. 2009;23(8):1291–1298. doi: 10.1080/13854040903307250. doi:10.1080/13854040903307250. [DOI] [PubMed] [Google Scholar]
- Jorge RE, Robinson RG, Arndt SV, Starkstein SE, Forrester AW, Geisler F. Depression following traumatic brain injury: A 1 year longitudinal study. Journal of Affective Disorders. 1993;27:233–243. doi: 10.1016/0165-0327(93)90047-n. [DOI] [PubMed] [Google Scholar]
- Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S. Major depression following traumatic brain injury. Archives of General Psychiatry. 2004;61:42–50. doi: 10.1001/archpsyc.61.1.42. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among U.S. Veterans after returning from the Iraq or Afghanistan War Zones. Journal of the American Medical Association. 2008;300:653–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Keen SM, Kutter CJ, Niles BL, Krinsley KE. Psychometric properties of PTSD Checklist in a sample of male veterans. Journal of Rehabilitation Research and Development. 2008;45:465–474. doi: 10.1682/jrrd.2007.09.0138. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. Guilford Press; New York: 2005. [Google Scholar]
- Leone L, Perugini M, Bagozzi RP, Pierro A, Mannetti L. Construct validity and generalizability of the Carver-White Behavioural Inhibition System/Behavioural Activation System Scales. European Journal of Personality. 2001;15:373–390. [Google Scholar]
- Lees-Haley PR, Fox DD, Courtney JC. A comparison of complaints by mild brain injury claimants and other claimants describing subjective experiences immediately following their injury. Archives of Clinical Neuropsychology. 2001;16(7):689–695. doi:10.1016/S0887-6177(00)00092-5. [PubMed] [Google Scholar]
- Lippa SM, Pastorek NJ, Benge JF, Thornton G. Postconcussive Symptoms After Blast and Nonblast-Related Mild Traumatic Brain Injuries in Afghanistan and Iraq War Veterans. Journal of the International Neuropsychological Society. 2010;16(5):856–866. doi: 10.1017/S1355617710000743. doi:10.1017/S1355617710000743. [DOI] [PubMed] [Google Scholar]
- Meares S, Chores EA, Taylor AJ, Batchelor J, Bryant RA, Baguley IJ, Marosszeky JE. The prospective course of postconcussion syndrome: The role of mild traumatic brain injury. Neuropsychology. Advance online publication. 2011 May 16; doi: 10.1037/a0022580. Doi: 10.1037/a0022580. [DOI] [PubMed] [Google Scholar]
- Mild Traumatic Brain Injury Committee, A. C. O. R. M., Head Injury Interdisciplinary Special Interest Group Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation. 1993;8(3):86–87. [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA: Journal of the American Medical Association. 2007;298(18):2141–2148. doi: 10.1001/jama.298.18.2141. doi:10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Highley J, Dolan SL, Fee F. In: Substance use disorder, PTSD, and traumatic brain injury. Vasterling J, Keane T, Bryant R, editors. Guilford Press; in press. [Google Scholar]
- Pagulayan KF, Hoffman JM, Temkin NR, Machamer JE, Dikmen SS. Functional limitations and depression after traumatic brain injury: Examination of the temporal relationship. Archives of Physical Medicine and Rehabilitation. 2008;89:1887–1892. doi: 10.1016/j.apmr.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Peskind ER, Petrie EC, Cross DJ, Pagulayan K, McCraw K, Hoff D, et al. Cerebrocerebellar hypometabolism associated with repetitive blast exposure mild traumatic brain injury in 12 Iraq war veterans with persistent post-concussive symptoms. NeuroImage. 2011;54(Suppl 1; Supplement):S76–S82. doi: 10.1016/j.neuroimage.2010.04.008. doi:10.1016/j.neuroimage.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz AS, Shiner B, Watts BV, Detzer MJ, Kutter C, Street B, Scott D. The White River Model of Colocated Collaborative Care: A Platform for Mental and Behavioral Health Care in the Medical Home. Families, Systems, & Health. 2010;28:114–129. doi: 10.1037/a0020261. [DOI] [PubMed] [Google Scholar]
- Porto PR, Oliveira L, Mari J, Volchan E, Figueira I, Ventura P. Does cognitive behavioral therapy change the brain? A systematic review of neuroimaging in anxiety disorders? Journal of Neuropsychiatry and Clinical Neuroscience. 2009;21:114–125. doi: 10.1176/jnp.2009.21.2.114. [DOI] [PubMed] [Google Scholar]
- Qureshi SU, Long ME, Bradshaw MR, Pyne JM, Magruder KM, Kimbrell T, Hudson TJ, Jawaid A, Schulz PE, Kunik ME. Does PTSD impair cognition beyond the effect of trauma? The Journal of Neuropsychiatry and Clinical Neurosciences. 2011;23(1):16–28. doi: 10.1176/jnp.23.1.jnp16. [DOI] [PubMed] [Google Scholar]
- Rao V, Bertrand M, Rosenberg P, Makley M, Schretlen DJ, Brandt J, Mielke MM. Predictors of new-onset depression after mild traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences. 2010;22:100–104. doi: 10.1176/appi.neuropsych.22.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapoport MJ, McCullagh S, Streiner D, Feinstein A. The clinical significance of major depression following mild traumatic brain injury. Psychosomatics. 2003;44:31–37. doi: 10.1176/appi.psy.44.1.31. [DOI] [PubMed] [Google Scholar]
- Rapoport MJ, McCullagh S, Shammi P, Feinstein A. Cognitive impairment associated with major depression following mild and moderate traumatic brain injury. Journal of Neuropsychiatry and Clinical Neuroscience. 2005;17:61–65. doi: 10.1176/jnp.17.1.61. [DOI] [PubMed] [Google Scholar]
- Resch JA, Villarreal V, Johnson CL, Elliott TR, Kwok O, Berry JW, Underhill AT. Trajectories of life satisfaction in the first 5 years following traumatic brain injury. Rehabilitation Psychology. 2009;54(1):51–59. doi: 10.1037/a0015051. doi:10.1037/a0015051. [DOI] [PubMed] [Google Scholar]
- Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology. 2008;167(12):1446–1452. doi: 10.1093/aje/kwn068. [DOI] [PubMed] [Google Scholar]
- Schwab KA, Baker G, Ivins B, Sluss-Tiller M, Lux W, Warden D. The Brief Traumatic Brain Injury Screen (BTBIS): Investigating the validity of a self-report instrument for detecting traumatic brain injury (TBI) in troops returning from deployment in Afghanistan and Iraq. Neurology. 2006;65(5)(Supp. 2):A235. [Google Scholar]
- Snell DL, Surgenor LJ, Hay-Smith JC, Siegert RJ. A systematic review of psychological treatments for mild traumatic brain injury: An update on the evidence. Journal of Clinical and Experimental Neuropsychology. 2009;31(1):20–38. doi: 10.1080/13803390801978849. Doi: 10.1080/13803390801978849. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- Sosin D, Sniezek J, Thurman D. Incidence of mild and moderate brain injury in the United States, 1991. Brain Injury. 1996;10(1):47–54. doi: 10.1080/026990596124719. [DOI] [PubMed] [Google Scholar]
- Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. The American Journal of Psychiatry. 2009;166(7):768–776. doi: 10.1176/appi.ajp.2009.08101604. doi:10.1176/appi.ajp.2009.08101604. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry. 2010;67(6):614–623. doi: 10.1001/archgenpsychiatry.2010.54. doi:10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Thurman D, Alverson C, Dunn K, Guerrero J, Sniezek J. Traumatic brain injury in the United States: A public health perspective. Journal of Head Trauma and Rehabilitation. 1999;14(6):602–615. doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. Journal of the American Medical Association. 1999;282:954–957. doi: 10.1001/jama.282.10.954. [DOI] [PubMed] [Google Scholar]
- Underhill AT, Lobello SG, Stroud TP, Terry KS, Devivo MJ, Fine PR. Depression and life satisfaction in patients with traumatic brain injury: A longitudinal study. Brain Injury. 2003;17:973–982. doi: 10.1080/0269905031000110418. [DOI] [PubMed] [Google Scholar]
- Vanderploeg RD, Belanger HG, Curtiss G. Mild traumatic brain injury and posttraumatic stress disorder and their associations with health symptoms. Archives of Physical Medicine and Rehabilitation. 2009;90:1084–1093. doi: 10.1016/j.apmr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- Vanderploeg RD, Curtiss G, Luis CA, Salazar AM. Long-term morbidities following self-reported mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2007;29:585–598. doi: 10.1080/13803390600826587. [DOI] [PubMed] [Google Scholar]
- Vasterling JJ. TBI screening interview. Unpublished measure. VA Boston Healthcare System; Boston, MA.: 2008. [Google Scholar]
- Vasterling JJ, Verfaellie M, Sullivan KD. Mild traumatic brain injury and posttraumatic stress disorder in returning veterans: Perspectives from cognitive neuroscience. Clinical Psychology Review. 2009;29(8):674–684. doi: 10.1016/j.cpr.2009.08.004. doi:10.1016/j.cpr.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Veterans Benefits Administration Annual Benefits Report. 2010 http://www.vba.va.gov/REPORTS/abr/index.asp.
- VHA Office of Public Health and Environmental Hazards . Analysis of VA health care utilization among us Global War on Terrorism (GWOT) Veterans, 4th quarter, Fiscal Year 2010. US Department of Veterans Affairs; Washington, DC: Dec, 2010. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist: Reliability, validity, and diagnostic utility.. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX.. Oct, 1993. [Google Scholar]
- Wilk JE, Thomas JL, McGurk DM, Riviere LA, Castro CA, Hoge CW. Mild traumatic brain injury (concussion) during combat: Lack of association of blast mechanism with persistent postconcussive symptoms. Journal of Head Trauma Rehabilitation. 2010;25(1):9–14. doi: 10.1097/HTR.0b013e3181bd090f. [DOI] [PubMed] [Google Scholar]
- Wright KM, Cabrera OA, Bliese PD, Adler AB, Hoge CW, Castro CA. Stigma and barriers to care in soldiers postcombat. Psychological Services. 2009;6:108–116. [Google Scholar]
- Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. Journal of Head Trauma and Rehabilitation. 2005:394–400. doi: 10.1097/01.HTR.0000341435.52004.ac. [DOI] [PubMed] [Google Scholar]