Abstract
Background:
With the aim of addressing the relative scarcity of information on youth-onset diabetes in India, the Indian Council of Medical Research (ICMR) decided to establish the Registry of People with Diabetes with Young Age at Onset (YDR) in 2006. The major objectives of YDR are to generate information on disease pattern or types of youth-onset diabetes including their geographical variations within India and to estimate the burden of diabetes complications.
Methods:
YDR is an observational multicenter clinic based registry enlisting physician diagnosed diabetes in individuals below 25 years of age. Diabetes was classified using symptom based clinical criteria. YDR data collection is coordinated through regional collaborating centers and their interacting reporting centers across India. A baseline and an annual follow-up proformas are used to obtain information on sociodemographic details, clinical profile, and anthropometric and laboratory measurements of the patients.
Results:
In phase 1, the registry has enrolled 5546 patients, in which type 1 diabetes mellitus (T1DM) was the most prevalent (63.9%), followed by youth-onset type 2 diabetes mellitus (T2DM) (25.3%).
Conclusion:
This registry provides a unique opportunity to study the natural history of youth-onset diabetes in India.
Keywords: diabetes registry, youth-onset diabetes, type 1 diabetes, type 2 diabetes
Long-term prospective patient registries are critical epidemiological tools to build a knowledge base for chronic diseases. Both population and hospital based registries have contributed immensely to the epidemiology of chronic diseases such as cancers.1-3 Registries are able to track trends in the incidence of diseases in defined geographical areas.4 Linkage of registry data to census information and Global Positioning System (GPS) data could help to identify potential clusters and spatial distribution of the disease of interest.5 In addition to this, registries could act as a platform for nested studies to test the safety and effectiveness of treatment strategies including health care interventions.6 Moreover, registry data allow policy makers to set public health priorities and also help them in evidence based decision making.6,7
In the developed world, registries play a pivotal role in the health system to assess the quality of care delivered to chronic conditions such as diabetes, which require continuous long-term care. One of the central components of the “chronic care model” is the use of registries to improve patient outcomes and this has been substantiated by recent research studies.8-10
Due to an exponential increase in the global burden of diabetes, even well-established health systems are unable to deliver efficient patient monitoring as well as optimal care to the burgeoning population of patients.11,12 This emphasizes the relevance of information technology tools including electronic health records, registries and decision support systems in diabetes management.13 From a provider’s perspective, diabetes registries not only help physicians and health workers to track patients, increase follow-up rate, and identify high risk patients,14 but also facilitate the use of evidence based guidelines in management. The registry and risk stratification system of the Joslin Diabetes Center is one such model that showed promising results in terms of quality of care and patient outcomes.15 For patients, the registry summary narrates their health/disease status over time to assess improvement and identifies areas or concerns. It also enables them to compare their clinical parameters and health outcomes with other patients seeking care from the same health facility.
The utility of such registries targeting children and adolescents with diabetes has been recognized over the past couple of decades. Current literature on youth-onset diabetes, particularly type 1 diabetes (T1DM) has been contributed mainly by registry collaborations such as World Health Organization’s DIAMOND project, EURODIAB study, and national registries such as the SEARCH for diabetes in youth study in the United States. These registries reported an increase in the incidence of youth-onset diabetes with definite variation across ethnic groups.16-18 Registry data are useful in studying the burden and risk factors of complications among children and adolescents with diabetes (Table 1). However, such data are not available from developing countries.
Table 1.
An Overview of Childhood and Adolescent Onset Diabetes Registries.
| Number | Name | Location (start year) | Type of registry | Type of diabetes | Age at onset/diagnosis | Major outcomes |
|---|---|---|---|---|---|---|
| 1 | SEARCH for Diabetes in Youth19 | Cincinnati, Colorado, Seattle, South Carolina, USA (2000) | Population based | T1DM, T2DM, and other hybrid types | <20 years | Burden, pathogenesis, frequency of the complications, quality of care, and health utilization for diabetes |
| 2 | Pittsburgh Insulin Dependent Diabetes Mellitus Registry20 | Allegheny County, Pittsburgh, USA (1965) | Population based | T1DM | <20 years | Incidence of diabetes and diabetes complications |
| 3 | Belgium Diabetes Registry (BDR)21 | Belgium (1989) | Population based | T1DM | <40 years | Incidence of diabetes, causes and markers of diabetes |
| 4 | Irish Childhood Diabetes National Register (ICDNR)22 | Ireland (2008) | Population based | T1DM | <15 years | Incidence of diabetes |
| 5 | Norwegian Childhood Diabetes Registry (NCDR)23 | Norway (2006) | Population based | All childhood onset diabetes | <15 years | Incidence of diabetes, mortality, quality of diabetes care |
| 6 | National Diabetes Register (NDR), Australia24 | Australia (1999) | Population based | All insulin treated diabetes categories | <15 years | Incidence of diabetes |
| 7 | Finnish Childhood Diabetes Registry25 | Finland (1987) | Population based | T1DM | <15 years | Incidence of diabetes |
| 8 | Baden-Württemberg Diabetes Incidence Registry (DIARY)26 | Germany (1987) | Population based | T1DM | <15 years | Incidence of diabetes |
| 9 | Swedish Childhood Diabetes Registry (SWEDIABKIDS)27 | Sweden (2000) | Population based | T1DM | 0-18 years | Quality of care |
| 10 | Manitoba Diabetes Education Resource for Children and Adolescents (DER-CA) Registry28 | Manitoba, Canada (1986) | Population based | All categories of youth-onset diabetes | 1-18 years | Quality of care |
| 11 | Registry of Type 1 Diabetes Mellitus in Italy (RIDI)29 | North, central, south, and insular regions, Italy (1996) | Population based | T1DM | <15 years | Geographic variation in the incidence of diabetes |
| 12 | Diabetes in Children and Adolescents Registry (DiCARE)30 | Malaysia (2006) | Hospital based | All categories of youth-onset diabetes | ≤18 years | Number and time trend of diabetes, sociodemographic profile of diabetes patients |
| 13 | Israel Juvenile Diabetes Registry31 | Israel (1997) | Population based | All categories of youth-onset diabetes | 0-17 years | Incidence of diabetes |
In India, there is a substantial gap in the existing literature relating to the burden and natural history of youth-onset diabetes. To date, there are no national registers to record data of people with youth-onset diabetes. Since most published studies are from isolated clinics,32,33 the national distribution of this emerging public health problem is largely unknown. Moreover, there are limited data on long-term clinical outcomes including the burden and risk factors of chronic diabetes complications among children and adolescents with diabetes. Given the complexity of Indian health care system, only a national level clinic based registry involving public and private hospitals can describe the clinical profile and practice patterns of youth-onset diabetes. Recognizing these needs as well as evidence gaps, the Indian Council of Medical Research (ICMR) decided to establish the Registry of People with Diabetes with Young Age at Onset (YDR). Here, we describe the objectives, methods, and current recruitment status of the YDR registry.
Objectives—YDR
The primary objective of the YDR was to understand the disease pattern or types of youth-onset diabetes including their geographical variations within the country and to estimate the burden of diabetes complications. The secondary objectives were (1) to facilitate research in the areas of basic, clinical (including patterns of care and survival), epidemiological, genetic, and molecular levels pertain to young-onset diabetes; (2) to help promote awareness about the magnitude of problem among professionals and public health partners; (3) to help in diabetes monitoring programs; (4) to assist in the development of disease management guidelines; and (5) to develop human resources in diabetes epidemiology.
Timeline
The official commencement of prospective data collection in YDR was on September 1, 2006. However, the registry included retrospective data from 2000 to 2006. Hence, the phase 1 period of the registry spans from January 1, 2000, to July 31, 2011. Subsequently, recruitment for phase 2 of the registry has commenced and is currently on-going.
YDR Organizational Structure
Registry Administration
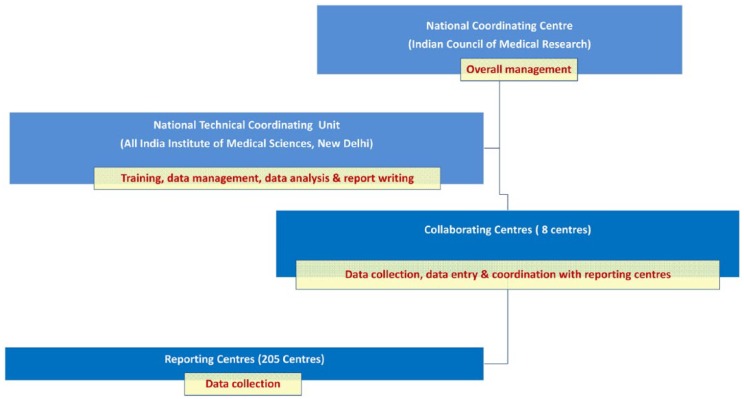
YDR is centrally managed by the Division of Noncommunicable Diseases (NCD) of the ICMR. An expert group consisting of eminent clinicians, clinical researchers, and academicians, constituted by the ICMR, is responsible for periodic review of registry activities, selection of new centers, drafting registry plan and procedures. A Technical Coordinating Unit (TCU) housed at the All India Institute Medical Sciences, New Delhi, was given the responsibility to compile, collate, and analyze the data. TCU is also responsible for the preparation of reports and manuscripts from the registry data.
Participating Centers
YDR is implemented through regional collaborating centers (RCCs) which coordinate data collection with reporting centers. The registry started with 5 RCCs and 3 more were added in the year 2009. These centers are tertiary care public or private institutions with proven track record of conducting multicenter clinical trials and translational research projects in the field of diabetes. RCCs were selected on the basis of the anticipated quantum of enrolled patients with young-onset diabetes.
Each RCC recruited patients attending clinics in their institution, hailing from an assigned geographical area. In addition, these centers also coordinated data collection from their interacting reporting centers located within the assigned area. Reporting centers ranged from single physician clinics to multispecialty hospitals including both private and public funded facilities. During phase 1, there were 205 reporting centers (3 to 83 centers per RCC) that collected and relayed data to their respective RCCs. The detailed organogram of the registry is shown in Figure 1.
Figure 1.
Organogram YDR.
Methods
Selection Criteria and Case Definitions
YDR registry recruited all cases of diabetes reporting on/after January 1, 2000, with the age equal to or less than 25 years at the time of diagnosis of diabetes (defined as fasting plasma glucose ≥126 mg/dl and/or 2 hr postload plasma glucose ≥200 mg/dl) and residing within the assigned geographical area. Both previously treated and untreated cases were included. YDR patients were classified into various diabetes categories based on the assessment of the principal investigator at the reporting center using symptom-based clinical criteria agreed on by the registry expert group prior to initiation of data collection in 2006 (Table 2).
Table 2.
Criteria for Classification of Diabetes Used in YDR.
| Type of diabetes | Case definition |
|---|---|
| T1DM | • The diagnosis of T1DM can be made throughout childhood but it is more likely below 15 years of age • The onset is usually acute and severe and insulin is required for survival • Family history of diabetes is rare • Presence of features of associated autoimmunity (other autoimmune disorders, vitiligo, etc) and absence of obesity, acanthosis nigricans • Urine ketones positive |
| T2DM | • The diagnosis of T2DM can be made at any age but peaks after puberty • The onset is usually insidious and may be mild to severe • Family history is usually positive and strong and obesity, metabolic syndrome and acanthosis nigricans are usually seen in these patients • There is no evidence of autoimmunity • There is no insulin dependence till late in the course of illness |
| Latent auto immune diabetes of adults (LADA) | • Generally above 15 years of age • Slower onset • Family history usually negative • Absence of ketosis • Absence of obesity and acanthosis nigricans |
| Maturity onset diabetes of the young (MODY) | • The age of onset of MODY is usually <25 years of age • The onset is usually insidious • A family history is strongly positive for 3 generations with an autosomal dominant mode of inheritance • No insulin requirement for metabolic control for 5 years after diagnosis is one of the criteria for diagnosis • The presence of obesity is variable and there is no autoimmunity or acanthosis nigricans |
| Malnutrition modulated diabetes mellitus | • Early onset of diabetes—often below 30 years of age • Insulin is required to obtain adequate glycemic control • Not ketosis prone • Absence of imaging evidence of pancreatic calculi or ductal dilatation • Low BMI (often below 17 kg/m2 at presentation) with other clinical features of malnutrition and often with growth retardation |
| Gestational diabetes | • Diabetes detected for the first time during pregnancy |
| Drug-induced diabetes | Diabetes associated with the use of; • Corticosteroids • Oral contraceptive agents • Thiazide diuretics • Non selective β adrenoceptor antagonists • Pentamidine • Nicotinic acid • Dilantin • Thyroid hormone • Diuretics like furosemide and chlorthiazide • Others |
| Chronic pancreatitis | • Evidence of exocrine pancreatic insufficiency—steatorrhoea • Chronic diarrhea • Evidence of malabsorption • History of chronic alcoholism or gallstones |
| Fibro calculous pancreatic diabetes | • Occurrence in a tropical country • Diabetes by standard criteria • Evidence of chronic pancreatic disease- pancreatic calculi on x-ray or any 3 of the following: • Abnormal pancreatic morphology with ductal dilatation detected by sonography, CT scan, or ERCP • Abnormal exocrine pancreatic function tests • Chronic recurrent abdominal pain since childhood • Steatorrhoea • Absence of other causes of chronic pancreatitis, eg, alcoholism, hepatobiliary disorders, hyperparathyroidism, etc |
Data Collection
A baseline proforma was used to obtain information from participants at registration (Supplementary File 1). Data from the period 2000-2006 were collected retrospectively in a structured format from medical records. The follow-up data of individuals registered in YDR was captured annually using an annual follow-up proforma (Supplementary File 2). If a participant had more than 1 visit during a calendar year, the details of the first visit were entered.
YDR recorded demographic, socioeconomic, clinical, and phenotypic profile of participants at registration and follow-up. Anthropometric measurements were done at the respective reporting centers using standardized instruments. Data on biochemical parameters were taken from the medical records. A list of core variables and the method of data collection are given in Table 3.
Table 3.
Core Variables and Methods of Data Collection.
| Domain/variable | Methods |
|---|---|
| Demographic | |
| Contact info, date of birth, sex, religion, residence (PIN code, district, state), mother tongue | 2b |
| Socioeconomic | |
| Parental/patient education | 2b |
| Socioeconomic status (low, middle, high) | 2b |
| Place of birth (parents/ child) | 2b |
| Clinical | |
| Diagnosis date, diabetes duration | 2a,b |
| Type of diabetes | 2d |
| Insulin use (yes/no), dose, type, start date | 1a,b |
| Oral diabetes medications (yes/no, type) | 1a,b |
| Alternate systems of medicine (yes/no, type) | 1b |
| Mode of presentation | 2b |
| Family history | 2b |
| Hospitalization (yes/no, reasons) | 1b |
| Complications of diabetes (yes/no, treatment, if any) | 1a,b |
| Comorbidities (yes/no, treatment, if any) | 1a,b |
| Phenotypic | |
| Height, weight | 1c |
| Waist and hip circumference | 1c |
| Blood pressure | 1c |
| Acanthosis nigricans, urine ketones | 2a |
| Fasting plasma glucose, HbA1c | 1a |
| Standard lipids (cholesterol, LDL, HDL, triglycerides) | 1a |
| Islet cell autoantibodies | 2a |
| Fasting C peptide | 2a |
| Urine albumin/creatinine | 3a |
| Birth weight | 2b |
1-Available at baseline and follow-up. 2-Available at baseline only. 3-Available at follow-up only. aMedical record. bSelf-report. cResearch measure. dClinical criteria.
Since many centers did not have access to a computer and internet, data were entered manually in printed pro formas. This was subsequently transcribed in the software created for the YDR in each RCC, before eventual transmission to the TCU. Paper copies of all pro formas were retained at the RCCs. Exact and adequate patient identifier characteristics (a combination of full name, age, gender and postal code) were used to prevent duplication of data.
Quality Control Measures
A uniform registry protocol, training manuals and pro formas were developed and adopted across all reporting centers. Trained staff assisted the reporting center investigators in collecting data. Uniform guidelines were followed to collect data on clinical characteristics as well as treatment practices. The overall coordination and supervision of data collection and entry were done by the TCU. Data were checked for missing values and entry errors. Incomplete pro formas were sent back to the respective RCCs for necessary action. Personal identifiers were matched to avoid duplication of data.
Apart from routine data collection exercises, annual training workshops were organized at RCCs. In these sessions, investigators from reporting centers were given training on data collection as well as data entry procedures. Operational difficulties in data collection and entry were also discussed in the workshops.
Ethical Considerations
Anonymous data has been acquired from the medical records and routine patient visits based on the baseline and follow-up pro forma prepared for the study. The ethics committee approvals were obtained from all RCCs—but not from the reporting centers as they did not have institutional ethics committees. Furthermore, there was no blood sampling as part of the registry related activities. In view of this, the YDR registry steering committee and the RCC ethics committees did not instruct for an individual consenting process. However the privacy and confidentiality of the participants were maintained during data collection. Personal identifiers of the patients were removed before transferring the data to TCU for final analysis.
Results—Recruitment Status
During phase 1, 5546 young diabetes patients were enrolled in the registry. Baseline data of 3488 patients were collected prospectively, while data of 2058 patients were collected retrospectively from their medical records. The details of data collection including the RCC wise and diabetes category wise details of patient recruitment are given in Table 4 and Figure 2.
Table 4.
Regional Collaborating Center Wise Recruitment of YDR Cases.
| Name of collaborating center | Start year | Number of reporting centers | Number of cases recruited |
|---|---|---|---|
| All India Institute of Medical Sciences (AIIMS), New Delhi | 2006 | 21 | 1266 |
| University College of Medical Sciences (UCMS), Delhi | 2006 | 14 | 709 |
| Madras Diabetes Research Foundation (MDRF), Chennai | 2006 | 26 | 1784 |
| S.C.B. Medical College Hospital, Cuttack | 2006 | 83 | 266 |
| Assam Medical College (AMC), Dibrugarh | 2006 | 27 | 569 |
| KEM Hospital, Mumbai | 2009 | 19 | 439 |
| P.D. Hinduja National Hospital, Mumbai | 2009 | 12 | 388 |
| Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh | 2009 | 3 | 125 |
Figure 2.
Diabetes category wise distributions of YDR cases.
Discussion
This is the first national-level multicentric clinic-based registry of youth-onset diabetes from India. The centers that collected data for this registry were treatment facilities ranging from single physician clinics to government hospitals to private super specialty centers. This heterogeneity will help to better understand the national distribution of youth-onset diabetes.
Most of the childhood diabetes registries from the west are population based and one of their major outcomes was to estimate the prevalence or Incidence of diabetes (Table 1). Being a hospital based registry, the YDR estimates may not reflect the actual population burden of youth-onset diabetes India. The ascertainment rate of the YDR has not been identified, but the process in which cases are registered and the manner in which youth with diabetes typically receive care in India suggest that only a few cases are likely to have been missed from the population. If methodological tools such as capture-recapture technique are used, the issue of under-ascertainment can be corrected in the future and the burden of disease can be estimated.34 However, the registry methodology is sound enough to gauge the types of diabetes seen, natural history and their complications and practice patterns across the country.
Till now, there are no gold standard definitions for various diabetes types presenting in younger age groups. The EURODIAB collaborative study, which included most of the European prospective registries, defined T1DM cases on the basis of a clinical diagnosis of idiopathic diabetes by a doctor.17 Registries like SEARCH adopted a pathogenesis based approach to classify diabetes.19 Since most of the reporting centers did not have facility to test auto antibodies, YDR used symptom based clinical criteria to classify diabetes. This may leave some chance for misclassification due to the overlap of clinical phenotypes at onset.
Unlike registries in Europe, YDR included all categories of youth-onset diabetes including Gestational Diabetes. This was to address the changing pattern of distribution of youth-onset diabetes. Until recently; the most common form of diabetes in the younger age group was T1DM. However, with the increasing burden of childhood overweight and obesity, the young people are increasingly being diagnosed with T2DM. A clinic based study from south India reported significant increase in the proportion of T2DM cases among children and adolescents between 1992 and 2009.35 In countries like Japan, T2DM is more common than T1DM and it accounts for 80% of childhood diabetes.36 The SEARCH registry also reported a higher proportion of young-onset T2DM among the non-white population.37 Furthermore, clinical reports from many countries, including India suggest an increase in proportion of other previously less prevalent variants of young-onset diabetes such as maturity onset diabetes of young (MODY), latent autoimmune diabetes in adults (LADA), and gestational diabetes.38-40 This was further confirmed by the distribution of cases in the YDR.
Different registries have used varied age at onset/diagnosis cutoffs to recruit cases (Table 1). Those recruiting T1DM alone followed a lower cutoff, while registries like SEARCH enrolled patients with age at onset/diagnosis less than 20 years. Since most of the adult onset diabetes studies from India included participants with age greater than or equal to 25 years, YDR has chosen this age as its upper cutoff to recruit cases.
Since the data from the period 2000-2006 were collected retrospectively from available medical records, the information on socio-economic status, family history, birth weight, lifestyle practices may not be complete for all the participants. Phase 1 does not mandate collection of blood/urine samples and the data on biochemical parameters were collected from the medical records. In the next phase of the project, collection of biosample is planned. These data should be interpreted with caution as there is a possibility of nonuniformity in analytical methods followed by the reporting centers.
Conclusion
Despite its limitations, YDR registry provides a unique opportunity to study the natural history of youth-onset diabetes in India. Furthermore, the data generated by this registry would serve as a strong platform for formulating treatment guidelines and designing interventions for improving the clinical outcomes as well as quality of life of youth-onset diabetes patients in India.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: GPS, Global Positioning System; ICMR, Indian Council of Medical Research; LADA, latent autoimmune diabetes in adults; MODY, maturity onset diabetes of young; NCD, noncommunicable diseases; RCC, regional collaborating center; TCU, Technical Coordinating Unit; T1DM, type 1 diabetes; T2DM, type 2 diabetes; YDR, Registry of People with Diabetes in India with Young Age at Onset.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Indian Council of Medical Research, India.
Supplemental Material: The supplementary material is available at http://dst.sagepub.com/supplemental
References
- 1. Satyanarayana L, Asthana S, Labani S P. Childhood cancer incidence in India: a review of population-based cancer registries. Indian Pediatr. 2014;51(3):218-220. [DOI] [PubMed] [Google Scholar]
- 2. Muir CS. The cancer registry in cancer control—a review. Arch Geschwulstforsch. 1984;54(6):491-497. [PubMed] [Google Scholar]
- 3. Parkin DM. The role of cancer registries in cancer control. Int J Clin Oncol. 2008;13(2):102-111. [DOI] [PubMed] [Google Scholar]
- 4. Agency for Healthcare Research and Quality. Registries for Evaluating Patient Outcomes: A User’s Guide. Vol 1 Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 5. Blakely T. O3-2.2 Linkage of census with mortality and cancer data in New Zealand. J Epidemiol Community Heal. 2011;65(suppl 1):A33-A33. [Google Scholar]
- 6. Dreyer N, Garner S. Registries for robust evidence. JAMA. 2009;302(7):790-791. [DOI] [PubMed] [Google Scholar]
- 7. Blommestein HM, Franken MG, Uyl-de Groot CA. A practical guide for using registry data to inform decisions about the cost effectiveness of new cancer drugs: lessons learned from the PHAROS registry. Pharmacoeconomics. 2015;33(6):551-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McEvoy P, Laxade S. Patient registries: a central component of the chronic care model. Br J Community Nurs. 2008;13(3):127-128, 130-133. [DOI] [PubMed] [Google Scholar]
- 9. Nutting PA, Dickinson WP, Dickinson LM, et al. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Fam Med. 2007;5(1):14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Minkman M, Ahaus K, Huijsman R. Performance improvement based on integrated quality management models: what evidence do we have? A systematic literature review. Int J Qual Health Care. 2007;19(2):90-104. [DOI] [PubMed] [Google Scholar]
- 11. Fox KM, Gerber R, Bolinder B, Chen J, Kumar S. Prevalence of inadequate glycemic control among patients with type 2 diabetes in the United Kingdom general practice research database: A series of retrospective analyses of data from 1998 through 2002. Clin Ther. 2006;28(3):388-395. [DOI] [PubMed] [Google Scholar]
- 12. Resnick HE, Foster GL, Bardsley J, Ratner RE. Achieve-ment of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999-2002: The National Health and Nutrition Examination Survey. Diabetes Care. 2006;29(3):531-537. [DOI] [PubMed] [Google Scholar]
- 13. Bu D, Pan E, Johnston D, et al. The value of information technology-enabled diabetes management. Diabetes Care. 2007;30(5):1137-1142. [DOI] [PubMed] [Google Scholar]
- 14. Chamany S, Silver LD, Bassett MT, et al. Tracking diabetes: New York City’s A1C Registry. Milbank Quart. 2009;87(3):547-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Russell KG, Rosenzweig J. Improving outcomes for patients with diabetes using Joslin Diabetes Center’s Registry and Risk Stratification system. J Healthc Inf Manag. 2007;21(2):26-33. [PubMed] [Google Scholar]
- 16. Karvonen M. Incidence and trends of childhood type 1 diabetes worldwide 1990-1999. Diabet Med. 2006;23(8):857-866. [DOI] [PubMed] [Google Scholar]
- 17. Green A, Gale EA, Patterson CC. Incidence of childhood-onset insulin-dependent diabetes mellitus: the EURODIAB ACE Study. Lancet. 1992;339(8798):905-909. [DOI] [PubMed] [Google Scholar]
- 18. Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pettitt DJ, Bell R, Dabelea D, et al. SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25(5):458-471. [DOI] [PubMed] [Google Scholar]
- 20. Fishbein HA, LaPorte RE, Orchard TJ, Drash AL, Kuller LH, Wagener DK. The Pittsburgh insulin-dependent diabetes mellitus registry: seasonal incidence. Diabetologia. 1982;23(2):83-85. [DOI] [PubMed] [Google Scholar]
- 21. Gorus FK. The importance of diabetes registries and clinical biology for the study and treatment of type 1 (insulin-dependent) diabetes mellitus. Verh K Acad Geneeskd Belg. 1996;58(5):539-586. [PubMed] [Google Scholar]
- 22. Roche EF, McKenna A, Ryder K, Brennan A, O’Regan M, Hoey H. The incidence of childhood type 1 diabetes in Ireland and the National Childhood Diabetes Register. Ir Med J. 2014;107(9):278-281. [PubMed] [Google Scholar]
- 23. Gagnum V, Stene LC, Sandvik L, et al. All-cause mortality in a nationwide cohort of childhood-onset diabetes in Norway 1973-2013. Diabetologia. 2015;58(8):1779-1786. [DOI] [PubMed] [Google Scholar]
- 24. Catanzariti L, Faulks K, Moon L, Waters AM, Flack J, Craig ME. Australia’s national trends in the incidence of type 1 diabetes in 0-14-year-olds, 2000-2006. Diabet Med. 2009;26(6):596-601. [DOI] [PubMed] [Google Scholar]
- 25. Karvonen M, Pitkäniemi J, Tuomilehto J. The onset age of type 1 diabetes in Finnish children has become younger. The Finnish Childhood Diabetes Registry Group. Diabetes Care. 1999;22(7):1066-1070. [DOI] [PubMed] [Google Scholar]
- 26. Ehehalt S, Dietz K, Willasch AM, Neu A. Epidemiological perspectives on type 1 diabetes in childhood and adolescence in germany: 20 years of the Baden-württemberg Diabetes Incidence Registry (DIARY). Diabetes Care. 2010;33(2):338-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hanberger L, Samuelsson U, Lindblad B, Ludvigsson J. A1C in children and adolescents with diabetes in relation to certain clinical parameters: The Swedish Childhood Diabetes Registry SWEDIABKIDS. Diabetes Care. 2008;31(5):927-929. [DOI] [PubMed] [Google Scholar]
- 28.Child Health Program. Diabetes education resource for children & adolescents (DER-CA)—annual report. Available at: https://umanitoba.ca/faculties/health_sciences/medicine/units/pediatrics/media/DER_CA_Annual_Report_2011.pdf.
- 29. Carle F, Gesuita R, Bruno G, et al. Diabetes incidence in 0- to 14-year age-group in Italy: a 10-year prospective study. Diabetes Care. 2004;27(12):2790-2796. [DOI] [PubMed] [Google Scholar]
- 30. Zain FM, Hua JHY, Ling WL, eds. 2nd Report of Diabetes in Children and Adolescence Registry (DiCARE) 2006-2008. Kuala Lumpur; 2012. [Google Scholar]
- 31. Koton S, Israel IDDM Registry Study Group. Incidence of type 1 diabetes mellitus in the 0- to 17-yr-old Israel population, 1997-2003. Pediatr Diabetes. 2007;8(2):60-66. [DOI] [PubMed] [Google Scholar]
- 32. Amutha A, Datta M, Unnikrishnan IR, et al. Clinical profile of diabetes in the young seen between 1992 and 2009 at a specialist diabetes centre in south India. Prim Care Diabetes. 2011;5(4):223-229. [DOI] [PubMed] [Google Scholar]
- 33. Unnikrishnan AG, Bhatia E, Bhatia V, et al. Type 1 diabetes versus type 2 diabetes with onset in persons younger than 20 years of age: results from an Indian multicenter study. Immunol Diabetes V Ann NY Acad Sci. 2008;1150:239-244. [DOI] [PubMed] [Google Scholar]
- 34. Chao A, Tsay PK, Lin SH, Shau WY, Chao DY. The applications of capture-recapture models to epidemiological data. Stat Med. 2001;20(2000):3123-3157. [DOI] [PubMed] [Google Scholar]
- 35. Amutha A, Datta M, Unnikrishnan R, Anjana RM, Mohan V. Clinical profile and complications of childhood- and adolescent-onset type 2 diabetes seen at a diabetes center in south India. Diabetes Technol Ther. 2012;14(6):497-504. [DOI] [PubMed] [Google Scholar]
- 36. Pinhas-Hamiel O, Zeitler P. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr. 2005;146(5):693-700. [DOI] [PubMed] [Google Scholar]
- 37. Liu LL, Yi JP, Beyer J, et al. Type 1 and type 2 diabetes in Asian and Pacific Islander U.S. youth: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(suppl 2):S133-S140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004;52:707-711. [PubMed] [Google Scholar]
- 39. Britten AC, Jones K, Törn C, et al. Latent autoimmune diabetes in adults in a South Asian population of the U.K. Diabetes Care. 2007;30(12):3088-3090. [DOI] [PubMed] [Google Scholar]
- 40. Harron KL, Feltbower RG, McKinney PA, Bodansky HJ, Campbell FM, Parslow RC. Rising rates of all types of diabetes in south Asian and non-south Asian children and young people aged 0-29 years in West Yorkshire, U.K., 1991-2006. Diabetes Care. 2011;34(3):652-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.