Abstract
Objectives
In recent years, Lean manufacturing principles have been applied to health care quality improvement efforts to improve wait times. In Ontario, an emergency department (ED) process improvement program based on Lean principles was introduced by the Ministry of Health and Long‐Term Care as part of a strategy to reduce ED length of stay (LOS) and to improve patient flow. This article aims to describe the hospital‐based teams’ experiences during the ED process improvement program implementation and the teams’ perceptions of the key factors that influenced the program's success or failure.
Methods
A qualitative evaluation was conducted based on semistructured interviews with hospital implementation team members, such as team leads, medical leads, and executive sponsors, at 10 purposively selected hospitals in Ontario, Canada. Sites were selected based, in part, on their changes in median ED LOS following the implementation period. A thematic framework approach as used for interviews, and a standard thematic coding framework was developed.
Results
Twenty‐four interviews were coded and analyzed. The results are organized according to participants’ experience and are grouped into four themes that were identified as significantly affecting the implementation experience: local contextual factors, relationship between improvement team and support players, staff engagement, and success and sustainability. The results demonstrate the importance of the context of implementation, establishing strong relationships and communication strategies, and preparing for implementation and sustainability prior to the start of the project.
Conclusions
Several key factors were identified as important to the success of the program, such as preparing for implementation, ensuring strong executive support, creation of implementation teams based on the tasks and outcomes of the initiative, and using multiple communication strategies throughout the implementation process. Explicit incorporation of these factors into the development and implementation of future similar interventions in health care settings could be useful.
Emergency department (ED) crowding is a widespread problem in Canada and other countries.1, 2 Crowding is most often experienced in urban, high‐volume, and/or trauma centers3 and is associated with poor patient experience, low hospital staff morale, and adverse patient outcomes.2, 4 Efforts to reduce crowding and mitigate ED wait times frequently focus on reducing internal process inefficiencies assumed to lead to delays. Methods based on Lean manufacturing are frequently used to achieve improvements.1
In 2008, the Ontario Ministry of Health and Long‐Term Care (the Ministry) launched the Emergency Department Wait Time Strategy in an attempt to improve ED wait times and reduce crowding.2 The Ministry worked with hospitals and regional health authorities in an effort to achieve wait time improvements, which included systemwide interventions such as a pay‐for‐performance incentive program for eligible hospitals, funding for hospital‐level interventions such as clinical decision units to manage short‐stay patients,5 and a Lean‐based quality improvement (QI) initiative known as the ED Process Improvement Program.2
A separate quantitative analysis found the Lean program to be associated with a modest decrease in ED length of stay (LOS) at participating hospitals, compared with control hospitals that did not implement it but were exposed to other initiatives in the policy.6 Prior studies found mixed evidence that Lean and six‐sigma can be successful at improving ED LOS metrics.1, 7
While Lean is thought to offer significant improvement opportunities,8 important questions remain about how Lean can best be implemented in health care settings.8 While recent qualitative evaluations of the implementation of Lean and improvement initiatives have begun to explore the specific mechanisms associated with successful implementation,9, 10, 11 to date most QI and Lean implementation research has focused on strategies, lessons learned, and barriers.11
Further, the context of improvement initiative implementation has also been identified as an important factor ripe for empirical investigation.12 For example, in a multisite study of infection control improvement initiatives,13 four key categories of contextual factors associated with successful QI implementation were identified: structural, political, emotional, and cultural. The authors called for further qualitative research to better understand how these contextual factors intersect in complex health care environments.
Lean implementation teams can provide valuable insight into the factors associated with the overall implementation process. As such, this study was conducted from the standpoint of the implementation team. Understanding the experiences of implementation teams is an important first step toward explicating the social processes involved so that future interventions can be better designed to take local context into account. This article aims to describe the hospital‐based implementation teams’ experiences during program implementation, and the team's perceptions of the key factors that influenced the program's success or failure.
Methods
Study Design
Using a descriptive qualitative design,14 we conducted semistructured interviews with Ontario hospital staff between November 2010 and September 2011. We obtained approval for this study from the Research Ethics Board of Sunnybrook Health Sciences Research Centre, as well as from each participating hospital. We also obtained written informed consent from all participants.
Study Setting and Population
Hospitals were selected for interviews based on the change in ED wait times, defined as the median ED LOS in the 6 months following the program implementation period, compared with the same period in the 2 years prior to program implementation.15 We selected the three hospitals with the greatest improvement and the two hospitals with the least improvement in ED LOS for interviews from each of wave 2 and wave 3. Figure 1 illustrates the relative change in ED LOS across all participating sites. Participants were members or senior‐level sponsors of the improvement teams at participating hospitals.
Figure 1.
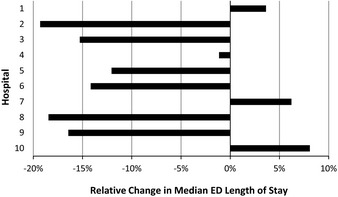
Relative change in ED length of stay in the 6 months following the ED process improvement program implementation period compared with the same period in the 2 years prior to program implementation for each participating site.
Study Protocol
The Ontario ED Process Improvement Program was launched in three waves between March 2009 and December 2010 within 36 hospitals across Ontario. The program used a Lean improvement approach modeled on pilot programs implemented in several Ontario hospitals. Dedicated hospital improvement teams, composed of senior leaders, managers, and staff from a variety of departments within participating hospitals, led the implementation of the Lean program at each hospital. These teams were responsible for identifying potential opportunities to improve patient flow from arrival in the ED to discharge from an inpatient unit, developing and implementing identified solutions. More detail regarding the program can be found elsewhere.6
Our sampling approach used a maximum variation method;15 we aimed to interview five respondents per hospital to obtain a wide range of perspectives, including physicians, nurses, clinical managers and directors, and senior administrators. We purposively selected hospitals from waves 2 and 3 (wave 1 was excluded as it was a pilot composed of a small number of hospitals). Characteristics of the participating hospitals are outlined in Table 1. This sampling technique was chosen to maximize the range of implementation experiences, not to compare experiences. We completed interviews within 6 to 8 months of program completion to allow us to determine whether ED wait times had improved while minimizing the effects of recall bias and hospital staff turnover.
Table 1.
Characteristics of Participating Hospitals
| Site | Average Annual ED Volume (N) | High‐Acuitya Patient Volume (%) | Admitted Patients (%) | Median ED LOSb (Hours) | 90th Percentile ED LOSb (hours) |
|---|---|---|---|---|---|
| Hospital 1 | 44,865 | 74.6 | 19.8 | 4.4 | 15.9 |
| Hospital 2 | 44,224 | 64.3 | 13.9 | 2.9 | 14.4 |
| Hospital 3 | 48,313 | 76.8 | 12.5 | 4.1 | 13.8 |
| Hospital 4 | 70,527 | 68.7 | 11.9 | 3.6 | 10.7 |
| Hospital 5 | 37,232 | 54.7 | 11.5 | 5.1 | 13.9 |
| Hospital 6 | 38,964 | 54.5 | 9.3 | 2.4 | 6.4 |
| Hospital 7 | 71,523 | 58.2 | 11.0 | 3.4 | 9.9 |
| Hospital 8 | 55,935 | 60.8 | 13.1 | 4.0 | 12.0 |
| Hospital 9 | 44,790 | 69.9 | 11.9 | 3.0 | 10.8 |
| Hospital 10 | 27,967 | 40.1 | 5.1 | 2.3 | 5.6 |
LOS = length of stay.
High‐acuity = Canadian Triage and Acuity Scale levels 1, 2, or 3
ED LOS is calculated for all patients regardless of ED disposition.
Semistructured interview guides were developed by the research team based on a review of the QI literature and consultation with the Ministry. Interview guides addressed barriers and enablers to program implementation, as well as perceptions of organizational factors related to achieving improved hospital and ED performance. All interviews were audiorecorded, transcribed, and anonymized for analysis. The order in which transcripts were reviewed was designed to ensure sufficient sampling of improved and unimproved hospitals, as well as hospital type (teaching vs. nonteaching) and location (north vs. south). We used the thematic analysis approach as outlined by Braun and Clarke16 to guide the analysis process. This approach involves looking for patterns of meaning in the data, developing themes to represent the identified patterns, and iteratively moving between the themes and the overall data set to develop an understanding of the phenomena under study.
Data Analysis
Four researchers independently reviewed the same four transcripts to develop a coding framework, and two researchers (ES, LR) then used NVIVO Version 8 (QSR International, Burlington, MA) coding software to apply the framework to the remaining transcripts. The research team continued to meet throughout the coding process to discuss emerging patterns and adjust the coding framework. Through consensus, the codes were organized into themes that represented the emerging patterns in the data related to the experience of the study participants. Review and coding of transcripts stopped after thematic saturation was reached.17
Results
Characteristics of the study participants are outlined in Table 2. We have organized our results according to participants’ experience of the various stages of the projects, beginning with a description of the process of implementing the process improvement program. Their experiences are grouped into four themes that were identified as significantly affecting the implementation experience: relational context, relationship between improvement team and support players, staff engagement, and success and sustainability. Participant quotes are displayed by theme in Tables 3 through 4, 5, 6.
Table 2.
Characteristics of Participants, by Site and Role
| Site | Participants | ||
|---|---|---|---|
| Executive Sponsora | Physician Leadb (Inpatient and ED) | Team Leadc (Inpatient and ED) | |
| Hospital 1 | 1 | 2 | 2 |
| Hospital 2 | 2 | 1 | 2 |
| Hospital 3 | 1 | 2 | 2 |
| Hospital 4 | 0 | 3 | 2 |
| Hospital 5 | 1 | 2 | 2 |
| Hospital 6 | 2 | 2 | 3 |
| Hospital 7 | 1 | 2 | 3 |
| Hospital 8 | 1 | 2 | 2 |
| Hospital 9 | 0 | 2 | 3 |
| Hospital 10 | 1 | 1 | 2 |
Executive sponsor = each hospital had to identify a senior member of the hospital executive who would act as the individual who was accountable to senior leadership for the implementation of the ED process improvement program.
Physician lead (inpatient and ED) = each hospital established an ED and inpatient team to implement Lean‐type interventions, and a lead physician was identified to help ensure effective physician engagement.
Team lead (inpatient and ED) = each hospital established an ED and in‐patient team to implement Lean‐type interventions, and a lead hospital staff member was identified.
Table 3.
Local Contextual Factors
| Theme | Quotes |
|---|---|
| Culture and past experience: Most facilities lacked substantial experience with QI prior to the implementation of PIP, which slowed momentum and had an institutional culture that saw QI as a dream or vision, not a reality. Often there were pockets of change but most improvement initiatives were disjointed or isolated. |
… I've had a number of different roles in different organizations and this place by a country mile, you know, sort of is the most collegial of all places and friendly; but at the same time, it really hadn't done that much along the way in terms of process improvements (inpatient physician). I'm not sure if there was a culture around improvement per se. I think that … I don't think there was … I don't think the concept was there in terms of as PIP would view it, in terms of ongoing quality assurance and look back and plan‐do‐check‐act cycle. I didn't see any of that, so I'd say there wasn't (ED physician lead). |
| Executive leadership: Visible and consistent support from senior management and executives was seen as crucial. |
The CEO's support was invaluable and his priority becomes everybody's priority. So it was a very important thing for all of us (inpatient team lead). So I found that was really positive and I think that's a top down thing. That's the message coming from Senior Admin to the Managers in the different departments that this is important and it didn't matter if it was DI or lab or whatever … They were hearing the message from the top not just from another department, like laterally (ED physician lead). I should point out that other than very initial meetings and some vague high profile statements, there was almost no presence of the CEO at the front line. And I think … and that is now reaping him negative results because people are saying ‘where the heck is he?’ (ED physician lead). I think they were genuinely interested in making, in facilitating the project for the group and for the hospital. I think that their role was quite positive as well (inpatient physician lead). [Executive sponsor] would sit down and figure out what exactly our issues were that we could go forward then and he would come with us as a support for us to the VP and to the CEO (ED team lead). |
DI = diagnostic imaging; PIP = process improvement program; QI = quality improvement.
Table 4.
Relationship Between Improvement Team and Support Players
| Theme | Quotes |
|---|---|
| Team selection: The selection of team members was often pointed to as critical to implementation success. Some felt that upfront information was lacking to inform team selection. |
I mean, it's a little hurried upfront and you're not given a lot of instruction as to what the exact roles might be. So it made picking a team a little bit harder (ED team lead). Get the right people on your team. Engage those managers and get the physicians … figure out a physician strategy. Know them, understand your stakeholders, understanding physician stakeholders because they can make or break (inpatient team lead). There's got to be some preparation; I know they do it in the eight months. But there's got to be some preparation for people like myself who's making the decisions initially to set it up (executive sponsor). |
| Team composition: Multiprofessional and equally representing implementation teams were considered important to program success. |
You just want to make sure the team and the team leadership is equitably comprised to represent people. Make it an equitable team and what I mean by, that is, have adequate representation from all the stakeholders involved (ED physician lead). I think it was quite well balanced, charge nurses, some support staff, clerical staff, who else, some RPNs. We had a good mix of people from the inpatient ward staff, as well (inpatient physician lead). |
| External coaches: Participants saw varying value in the external coach role. |
Well, I mean they certainly supported the people that we identified as the boots on the ground in the organization, supported them, pointed them in the right direction, you know, talked to them about what other best practice organizations were doing, mentored them, did all of those things. They were invaluable … (executive sponsor). Yeah so the coach was pulled out (…) and apparently replaced because of some conflict between the coach and some of the participants (executive sponsor). |
RPN = registered practical nurse.
Table 5.
Staff Engagement
| Theme | Quotes |
|---|---|
| Initial impressions and engagement: Frontline staff were often described as initially resistant to change, with some sense of cynicism and doubt about the program viability. | ‘Please don't step on my toes, I just want to come in and do what I have to do and get through my day and provide patient care as best I can and not get beat up by irate patients and go home and, you know, feed my family’ (steering committee sponsor). |
| Strategies to enhance engagement: Emphasizing patient‐centeredness, holding the course, and communication. |
We really took a focus from the beginning that this was all about the patient. So, keeping all of our improvement ideas and any of our projects patient‐focused; it's pretty hard to argue against that. Even if it means a bit of extra upfront work, I don't think there are too many people across the organization that can argue that improving the patient's journey has been a bad thing (ED team lead). And just holding your course; when you decide on a project and you're in the beginning phases of it, you can meet with a lot of resistance, but if you know that you've planned well and that it's going to work, to really stick with it because that initial pushback can be really strong and we certainly experienced it. So, holding the course, waiting for the flow to improve and for the staff to see the improvements (ED team lead). A lot of communication. They spent a lot of time talking with the staff, they spent a lot of time going step by step through the change that they wanted to see happen, but they also tried to ask them for a lot of feedback. ‘How would this form work if we did this?’ Bullet rounds, we took it to the staff many times about ‘how can we get more participation, how can we get doctors here at the bullet rounds?’ So there was a lot of collaboration with their peers (executive sponsor). |
| Physician engagement: Physicians were often described as skeptical about the program and in many cases seen to question the purpose, process, and motivation behind proposed change efforts. Effective leadership was critical to engagement efforts. |
So I think physicians were probably in their own mind right to keep asking why, why are we doing this? You know, why are we doing this? Who is making the decision? (ED team lead). I think they were slow to buy into the whole process. They tend to be skeptical at first (inpatient physician lead). So the credibility from the physician lead, the nurses that you choose to be on your team need to have credibility amongst their peers (ED team lead). Our medicine physician lead was phenomenal, continues to be phenomenal … She was very successful with quite a lot of initiatives and she was a phenomenal ally, but she's still having that discussion with us, how do I move them? Physicians are just a totally different beast and she's the Chief of Medicine, like she … but she gets it and she's trying to figure out how to move her own team (inpatient team lead). |
Table 6.
Success and Sustainability
| Theme | Quotes |
|---|---|
| Perceptions of success: The program was also viewed as enhancing frontline staff engagement in QI and problem solving, improved understanding of their own department's processes, and the broader hospital system. |
And handover, with using S‐BAR, certainly decreases a lot of patient safety issues as well, so appropriate handover of care improved (executive sponsor). It's gotten people talking more, what can we do about it, what are some ideas; it's got people brainstorming a little bit more and people bringing things forward, which is one of the main things to start. And that's been good, because that has been impacted and people are taking more onus … staff members are taking more onus on saying, you know what, this isn't working; we need to identify this. So that's a good thing (inpatient team lead). |
| Sustainability: Participants were able to describe some sustainability of improvements, such as changes in culture and improvements to care. |
I'd say at least halfway through. I mean, I think that it was more addressed honestly as we started to do and saw some change. I think once you see your metrics go up and see some positive results that's when you go okay, now I want to keep that … so I think that's when people started to be excited and they realized that we had improved in such a way that it really was worthy of ongoing and sustaining (inpatient team lead). The staff now know it's not over. You know, it just wasn't an eight‐month thing. We've talked about it, it's forever now (steering committee sponsor). I think we did surprising well actually. I was a bit skeptical in the beginning that this would be short couple months and then back to normal. But things are still happening and there's involvement from the senior team, CEO is still quite involved and quite committed, I think, honestly to quality care, to improving the flow through the hospital. So I think that's what's held is the support from the senior team from the start. And I think that's what's going to sustain it for the whole hospital (inpatient team lead). |
| Limited sustainability: Challenges to sustainability were discussed by many of the participants, citing issues such as workload, organizational structures, and lack of accountability. |
We tried not to make it stop, but at the end of the day, people go back to their jobs, they go back to doing what they have to do (executive sponsor). We had some sustainability plans but we were undergoing huge organizational change. We have been over the last year, so we've had a completely unstable senior management team and we've had director changes. We've had management changes. We've had staff … It's just been … and the entire organization was asked to refocus on 100‐day action plan. So we were asked to pretty much drop everything and only focus on getting our budget back in line (inpatient team lead). I had the buy‐in, the majority were on board and were almost enjoying it by the end, you know; they were proud that they were meeting their targets. Unfortunately, when they don't see it sustained, you lose trust, which is the bottom line and the basis to everything, so it just falls apart. So we've got a lot of burnt‐out people from that now, unfortunately (inpatient team lead). |
Local Contextual Factors
Participants described the study hospitals as having varying degrees of previous experience and success with QI implementation. Most participants believed that prior to the program, their organizations lacked the structure, resources, and past experience for successful QI implementation. Some participants described QI within their hospitals as a “dream” or “vision” rather than a reality. Others described past ad hoc improvements or “pockets of change” in some units; however, these were perceived as disjointed or isolated. Although past experience with QI initiatives, change management, and Lean processes were noted as helpful in the implementation of the process improvement program, few of these initiatives were described as positive or successful QI experiences.
While visible and consistent support for the program from senior management and executives was not uniformly reported at the study hospitals, it was seen by many as crucial to demonstrate the importance of the program as a corporate priority and ensure alignment between senior and middle management. Positive accounts of CEO involvement described leaders as being “huge into quality,” “big on change and Lean,” “visibly supportive,” and consistent and direct in their support. One participant explained that when the CEO supported the program as a key priority, it became a priority throughout the hospital. Similarly, another participant perceived the CEO as “absent” throughout the program and felt that this negatively affected implementation.
Relationship Between Improvement Team and Support Players
The selection and composition of the improvement teams varied across hospitals. Nursing staff and physicians were always included; however, the presence of other members such as allied health, porter and environmental services, diagnostic imaging, and labs was variable. Team leads also varied, with some hospitals selecting management‐level staff and others seconding frontline clinical staff. One hospital hired staff from outside the hospital to serve as team lead to provide Lean experience; however, these individuals were seen by some participants as lacking insight into the particular hospital's history, organizational structure, and politics.
Team selection was most often based on skills, motivation, individual characteristics, and interest in change and QI, rather than position in the ED or inpatient unit. While respondents frequently stated the importance of selecting individuals who were enthusiastic about the change process, views were mixed on including staff with “negative” attitudes on teams; some found it beneficial while others felt that negative attitudes affected others on the team and tended to persist. Equitable representation across the ED and inpatient units was seen to be important for ensuring subject matter expertise and staff buy‐in and to avoid perceived power imbalances between departments. Ensuring that team members also had organizational credibility was a common suggestion from participants. Several participants felt they were not provided with enough information about the program to guide the selection of their teams, and some said they would have chosen the teams differently given more information. Two specific changes included the relative representation from different hospital units and including more clinical frontline staff members. For example, many of the participants explained that they were told to ensure representation from across the organization, but felt that the majority of changes impacted nursing workflow, so including more frontline nurses would have been more effective.
Executive sponsors acted as senior team representatives, ensured communication with leadership, addressed operational barriers, and provided support to the teams. Some participants perceived them as being too detached, while engaged executive sponsors were seen as important to overall success. This was particularly true in smaller hospitals, which often lacked resources and infrastructure to support the initiatives.
On‐site support from external coaches was seen as integral to implementation success by providing a valuable external perspective and Lean expertise. Participants shared examples of the coaches helping teams understand implementation tools, as well as developing local solutions appropriate to that hospital. Some respondents indicated that coaches provided added credibility to the program, while others said that coaches did not provide the expected level of facilitation and leadership in terms of leading meetings and setting the agenda for planning sessions. While having the coaches challenge the implementation team and keep the project on track was, for the most part, seen as advantageous, in a limited number of cases the coach was perceived as pushing team members to complete tasks in an unrealistic timeline, sometimes resulting in conflict within the teams.
Staff Engagement
Frontline staff were often described by the improvement team members as initially resistant, cynical, and doubtful about the program, which was attributed to their past experiences with unsuccessful change initiatives. Participants shared conversations they had with frontline staff, who described their feelings as “we've been here before” or “this will never work.” According to study participants, frontline staff initially viewed the process improvement program as “just another initiative” and potentially more work. Physicians were often described as skeptical, frequently questioning the purpose and motivation behind proposed change efforts and not eager to participate. Once implementation commenced, the extent of engagement and involvement varied among hospitals. In general, frontline staff were involved in identifying areas for potential improvement and providing feedback on solutions design. Less involvement was reported in prioritizing improvement opportunities and the actual design and implementation of the solutions. Efforts to solicit input from frontline staff also varied, with most team members describing the use of multiple methods such as suggestion boxes, e‐mail, meetings, and focus groups. Participants described face‐to‐face discussions, implementation of frontline staff suggestions, and providing ongoing feedback to staff as the most effective strategies for staff engagement.
Initial physician engagement was reported as a challenge across most hospitals. Some hospitals noted differences between emergency and inpatient physicians, with emergency physicians generally perceived as more engaged. In some cases this perceived difference was attributed to characteristics of the physician group (e.g., natural cohesion among ED physicians who share shifts and handover patients) and, in others, to the quality of physician leadership. Overall, the active involvement of physician leads was seen to enhance program credibility and was critical to engaging other frontline physicians.
Success and Sustainability
Following program implementation, most participants described improvements in quality of care, decreased wait times, fewer patient complaints, and increased patient satisfaction. Overall, participation in the program was perceived as a positive experience. Specifically, standardization of care and improved communication were identified as key factors that could potentially have an effect on quality and safety of patient care in the future. The program was also viewed as enhancing frontline staff engagement in QI and problem solving and improving understanding of their own departments’ processes and the broader hospital systems. Many participants reported that it was only well into the implementation phase that staff began to embrace its concepts and the resulting process changes. These participants stressed the importance of “holding your course” long enough for the frontline staff to see positive benefits, since “real” staff buy‐in came only after initial improvements could be demonstrated.
Although many participants described positive outcomes, sustaining the changes was seen as challenging following the end of the program. Some participants described this as “slippage,” a common challenge with QI initiatives, while others saw specific impediments to sustainability such as increasing patient volumes, reduced hospital prioritization of Lean, and changes in other areas of the hospital that directly affected process changes. Ensuring accountability at operational and administrative levels was described as the most important factor in sustaining improvements. In some facilities, operational accountability (“process ownership”) took the form of continued staffing of improvement team positions, whereas in others department managers were responsible for maintaining the process changes. At the administrative level, explicit accountability for performance metrics was identified as key to sustaining process improvements. Promoting the change initiatives associated with the program to staff and team members as a means to sustain meaningful improvements, not simply for short‐term gains, was also identified as helpful in enhancing sustainability. Some participants described their hospitals as not being able to sustain improvements resulting from the program, but indicated that the experience prompted further QI efforts. Specifically, a number of participants described how their hospitals were continuing to refine program initiatives or were moving forward with improvements that were not addressed within the program timeline.
Discussion
The context in which QI and Lean initiatives are implemented in health care has been identified as important to their overall success.12, 18, 19 Across the hospitals, many participants felt that QI was not entrenched, and staff were skeptical and resistant to proposed change initiatives that originated externally. Organizational readiness for change, defined as an organization's members shared resolve for change and a belief that change is possible, is seen as critical to the implementation of complex changes in health care institutions.20 Many of the participants in our study described a lack of structures, resources, and experience with QI or Lean implementation, all of which affect the hospital's readiness for change.
Our study echoes current implementation literature demonstrating the clear importance of leadership in improvement efforts. Effective and engaged leadership was another important characteristic noted by respondents and one that has been shown to be a critical aspect of successful QI in other studies.12, 21, 22, 23, 24 CEOs and senior administrative personnel need to be engaged, motivating, and seen to be supporting frontline staff activities.21 We found that more successful hospitals tended to have more positive views of leadership and executive support and more positive experiences when executive sponsors were involved in and aware of all aspects of the wider program and the individual improvement initiatives, and the CEOs were visible and consistent in their support of the program.
A recurring challenge for hospitals in our study was the creation of strong and effective implementation teams, partly as a result of limited information about the program prior to team selection. Effective improvement teams are important to QI success.12, 25, 26, 27 Although the behaviors, skills, and knowledge of team members are important factors, many other factors also influence improvement team effectiveness, such as task design, team processes, team psychological traits and outcomes,28 and organizational context.27, 29 The results of this study pointed to the need to provide hospitals with more detailed preparatory information to ensure that the most effective teams were assembled based on the tasks, outcomes, and environment. External consultants or coaches commonly work with teams as part of Lean QI initiatives, but few studies have explicitly studied their value.23 Our respondents expressed mostly positive views on their value in supporting implementation teams.
The preparation for and process of implementation also plays into the success of QI initiatives.30 Actively engaging frontline staff is both necessary and a challenge in QI.31, 32 In this study, it was especially true in the initial stages. Using multiple methods and face‐to‐face strategies to communicate with staff were seen as most effective. This echoes other reports demonstrating that ongoing and candid communications are essential to maintain staff involvement.33 Frontline staff often feel that QI initiatives are not in line with their workflow and will consume valuable time and resources,31, 32 however, when given the opportunity they effectively address areas for improvement in their work areas.34 In this study, frontline staff were often not engaged in identifying areas for improvement or solutions, even though many of the implementation team members described the importance of frontline staff empowerment in Lean initiatives. Enhanced efforts and opportunities for frontline staff involvement or input in all aspects of improvement initiatives may not only enhance staff engagement, but may also improve the design and implementation of the initiatives in the local context. The concept of frontline staff resistance is common in QI implementation research;32, 33, 34 however, the causes are not well understood. Our study points to a potential relationship between this resistance and how feedback is collected from the frontline staff.
A particular challenge identified was physician engagement. Physicians are often seen as resistant,33, 35 relating to skepticism about quality problems and measurement, inadequate time to engage in quality initiatives, a lack of training and leadership in quality,36 and fear of change.33 Participants reported that a key factor enabling physician engagement was the presence of a credible and respected physician lead. To ensure strong physician leadership, however, respondents believed that system‐ and hospital‐level changes are needed. Specific system changes discussed in the literature include building QI into medical education, providing specific QI training to physicians, ensuring adequate resources, and providing incentives for QI work.35, 37, 38
Overall, the participants were able to identify improvements related to the program, such as improved wait times and a better understanding of hospital‐wide processes by staff. However, the sustainability of improvements was unclear, and a long‐term focus on clinical improvement appears necessary.23, 39 While external factors can influence sustainability, internal accountability, including the need for ongoing process ownership, was cited as a more important factor. Yet such accountability cannot rely on a few enthusiastic staff members; the organization as a whole must adopt a culture of long‐term accountability.23 Further, improvements in performance measures such as LOS may not be sustained by a single initiative. Widespread and focused interventions with built in flexibility, staff contributions, and sustainability processes are likely needed to maintain improvements.31, 40 Including a specific plan for sustainability at the outset of a change initiative has also been shown to enhance overall long‐term success.41, 42
Limitations
This study was conducted from the standpoint of the implementation team to explore their perceptions of key factors associated with implementation success. We did not interview frontline staff, which would have provided a more complete picture of hospital experience. However, to the best of our knowledge, no other qualitative study has explored Lean through the standpoint of the implementation team. Doing so extends our knowledge of the experiences of these key players in any QI project. Although we included participants from hospitals that were either successful or unsuccessful in reducing ED LOS to ensure a variety of perspectives on program implementation, the results of this study are not a direct comparison of these hospitals. Due to the small number of hospitals included in this study, we were unable to identify factors that were present in successful hospitals but not in unsuccessful ones. Instead we present all participant perceptions of the factors associated with successes and the challenges of program implementation.
Conclusions
This study adds to the current literature by identifying several key factors in the implementation of Lean, which have implications for practice. First, addressing organizational readiness prior to implementation will help set the stage for implementation. Second, leadership and support is critical. CEOs must prioritize and visibly support the initiative to achieve hospital‐wide engagement, and the implementation teams need committed executive support to ensure resources are available throughout the implementation. Third, a clear understanding of the tasks, outcomes, and environment are needed to enhance implementation team development and effectiveness. Fourth, ongoing and multimodal communication strategies are needed to engage and inform frontline staff, incorporating their insights and preexisting relationships in all aspects of the implementation process, and sharing ongoing successes to encourage engagement. Finally, having a sustainability plan that specifies responsibility or ownership for processes and changes brought about during the improvement initiative is important to helping ensuring long‐term and sustained improvements. Explicit incorporation of these factors into the development and implementation of similar interventions in hospital‐based settings may enhance implementation success.
The authors thank Ashif Kachra for research administrative support, study coordination, and assistance with manuscript preparation.
Appendix A. ED Investigator team
M. Afilalo, Emergency Department, Jewish General Hospital, McGill University, Montreal, Quebec, Canada; G. Anderson, Institute for Clinical Evaluative Sciences and Institute for Health Policy, Management and Evaluation, University of Toronto, Toronto, Ontario; D. Carew, Trauma, Emergency and Critical Care Program, Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada; M. Carter, Mechanical and Industrial Engineering, University of Toronto, Toronto, Ontario, Canada; M. Cooke, Division of Health Sciences, University of Warwick, Coventry, UK; B. Golden, Rotman School of Management, University of Toronto, Toronto, Ontario, Canada; T. Rutledge, Department of Family and Community Medicine, University of Toronto, North York General Hospital, Toronto, Ontario, Canada; T. Stukel, Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada, and Dartmouth Institute for Health Policy and Clinical Practice, Giesel School of Medicine at Dartmouth, Hanover, NH.
Academic Emergency Medicine 2015;22:720–729 © 2015 The Authors. Academic Emergency Medicine published by Wiley Periodicals, Inc. on behalf of Society for Academic Emergency Medicine.25996451
ED Investigator Team members are listed in Appendix A.
Presented at the Canadian Association for Health Services and Policy Research (CAHSPR), Vancouver, BC, Canada, May 2013; and the Canadian Association of Emergency Physicians (CAEP) Vancouver, BC, Canada, June 2013.
This study was funded by the Ontario Ministry of Health and Long Term Care and the Canadian Foundation for Healthcare Improvement. Astrid Guttmann is supported by a Canadian Institutes for Health Research (CIHR) Applied Chair in Child Health Policy and Services Research. Brian H. Rowe is supported by the CIHR as Tier I Canada Research Chair in Evidence Based Emergency Medicine. Michael J. Schull is supported by a CIHR Applied Chair in Health Services and Policy Research.
Disclaimer: This study was supported by the Institute for Clinical Evaluative Sciences, a nonprofit research institute funded by the Ontario Ministry of Health and Long‐Term Care. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by Institute for Clinical Evaluative Sciences or the Ontario Ministry of Health and Long‐Term Care is intended or should be inferred.
All authors declare no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
Due to the nature of our agreement with the Ontario Ministry of Health and Long‐Term Care and our privacy policies, data sharing is not possible.
A related article appears on page 750.
References
- 1. Ng D, Vail G, Thomas S, Schmidt N. Applying the Lean principles of the Toyota Production System to reduce wait times in the emergency department. CJEM 2010;12:50–7. [DOI] [PubMed] [Google Scholar]
- 2. Ovens H. ED overcrowding: the Ontario approach. Acad Emerg Med 2011;18:1242–5. [DOI] [PubMed] [Google Scholar]
- 3. Ontario Hospital Association OMA , Ontario Ministry of Health. Improving Access to Emergency Care: Addressing System Issues. Available at: http://www.health.gov.on.ca/en/common/ministry/publications/reports/improving_access/improving_access.pdf. Accessed Mar 3, 2015.
- 4. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009;16:1–10. [DOI] [PubMed] [Google Scholar]
- 5. Schull MJ, Vermeulen MJ, Stukel TA, et al. Evaluating the effect of clinical decision units on patient flow in seven Canadian emergency departments. Acad Emerg Med 2012;19:828–36. [DOI] [PubMed] [Google Scholar]
- 6. Vermeulen MJ, Stukel TA, Guttmann A, et al. Evaluation of an emergency department Lean process improvement program to reduce length of stay. Ann Emerg Med 2014;64:427–38. [DOI] [PubMed] [Google Scholar]
- 7. Mazzocato P, Holden RJ, Brommels M, et al. How does Lean work in emergency care? A case study of a Lean‐inspired intervention at the Astrid Lindgren Children's hospital, Stockholm. Sweden. BMC Health Serv Res 2012;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Holden RJ. Lean thinking in emergency departments: a critical review. Ann Emerg Med 2011;57:265–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. de Souza LB, Pidd M. Exploring the barriers to lean health care implementation. Public Money Manage 2011;31:59–66. [Google Scholar]
- 10. Kim CS, Spahlinger DA, Kin JM, Coffey RJ, Billi JE. Implementation of Lean thinking: one health system's journey. Jt Comm J Qual Patient Saf 2009;35:406–13. [DOI] [PubMed] [Google Scholar]
- 11. Jeffs LP, Lo J, Beswick S, Campbell H. Implementing an organization‐wide quality improvement initiative: insights from project leads, managers, and frontline nurses. Nurs Adm Q 2013;37:222–30. [DOI] [PubMed] [Google Scholar]
- 12. Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: a multi‐center qualitative study. Soc Sci Med 2010;71:1692–701. [DOI] [PubMed] [Google Scholar]
- 14. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 15. Patton MQ. Qualitative Research & Evaluation Methods, 3rd ed Thousand Oaks, CA: Sage Publications Inc, 2002. [Google Scholar]
- 16. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 17. Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. Thousand Oaks, CA: Sage Publications, 1998. [Google Scholar]
- 18. Stevens DP, Shojania KG. Tell me about the context, and more. BMJ Qual Saf 2011;20:557–9. [DOI] [PubMed] [Google Scholar]
- 19. Ovretveit J. Understanding the conditions for improvement: research to discover which context influences affect improvement success. BMJ Qual Saf 2011;20(Suppl 1):i18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weiner BJ. A theory of organizational readiness for change. Implement Sci 2009;4:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kaplan HC, Provost LP, Froehle CM, Margolis PA. The model for understanding success in quality (MUSIQ): building a theory of context in health‐care quality improvement. BMJ Qual Saf 2012;21:13–20. [DOI] [PubMed] [Google Scholar]
- 22. Barron WM, Krsek C, Weber D, Cerese J. Critical success factors for performance improvement programs. Jt Comm J Qual Saf 2005;31:220–6. [DOI] [PubMed] [Google Scholar]
- 23. Dixon‐Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation's programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Solberg LI, Taylor N, Conway WA, Hiatt RA. Large multispecialty group practices and quality improvement: what is needed to transform care? JACM 2007;30:9–17. [DOI] [PubMed] [Google Scholar]
- 25. Shortell SM, Marsteller JA, Lin M, et al. The role of perceived team effectiveness in improving chronic illness care. Med Care 2004;42:1040–8. [DOI] [PubMed] [Google Scholar]
- 26. Meltzer D, Chung J, Khalili P, et al. Exploring the use of social network methods in designing healthcare quality improvement teams. Soc Sci Med 2010;71:1119–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Strating MM, Nieboer AP. Explaining variation in perceived team effectiveness: results from eleven quality improvement collaboratives. J Clin Nurs 2012;22:1692–706. [DOI] [PubMed] [Google Scholar]
- 28. Lemieux‐Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev 2006;63:263–300. [DOI] [PubMed] [Google Scholar]
- 29. Mills PD, Weeks WB. Characteristics of successful quality improvement teams: lessons from five collaborative projects in the VHA. Jt Comm J Qual Saf 2004;30:152–62. [DOI] [PubMed] [Google Scholar]
- 30. Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Greenfield D, Nugus P, Travaglia J, Braithwaite J. Factors that shape the development of interprofessional improvement initiatives in health organisations. BMJ Qual Saf 2011;20:332–7. [DOI] [PubMed] [Google Scholar]
- 32. Davies H, Powell A, Rushmer R. Why don't clinicians engage with quality improvement? J Health Serv Res Policy 2007;12:129–30. [DOI] [PubMed] [Google Scholar]
- 33. Gollop R, Whitby E, Buchanan D, Ketley D. Influencing sceptical staff to become supporters of service improvement: a qualitative study of doctors’ and managers’ views. Qual Saf Health Care 2004;13:108–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Davies H, Powell A, Rushmer R. Healthcare Professionals’ Views on Clinician Engagement in Quality Improvement: A Literature Review. London, UK: The Health Foundation, 2007. [Google Scholar]
- 35. Taitz JM, Lee TH, Sequist TD. A framework for engaging physicians in quality and safety. BMJ Qual Saf 2012;21:722–8. [DOI] [PubMed] [Google Scholar]
- 36. Shekelle PG. Why don't physicians enthusiastically support quality improvement programmes? Qual Saf Health Care 2002;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hockey PM, Marshall MN. Doctors and quality improvement. J R Soc Med 2009;102:173–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pronovost PJ, Miller MR, Wachter RM, Meyer GS. Perspective: physician leadership in quality. Acad Med 2009;84:1651–6. [DOI] [PubMed] [Google Scholar]
- 39. Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM. Improving service quality by understanding emergency department flow: a White Paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med 2010;38:70–9. [DOI] [PubMed] [Google Scholar]
- 40. Glasgow JM, Davies ML, Kaboli PJ. Findings from a national improvement collaborative: are improvements sustained? BMJ Qual Saf 2012;21:663–9. [DOI] [PubMed] [Google Scholar]
- 41. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM). Jt Comm J Qual Saf 2008;34:228–43. [DOI] [PubMed] [Google Scholar]
- 42. Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci 2012;7:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]


