Abstract
Objective
To investigate the association between adverse childhood experiences (ACE) and pain with onset during pregnancy.
Design
Cross‐sectional study.
Setting
Eighteen antenatal clinics in southern Mid‐Sweden.
Sample
Of 293 women invited to participate, 232 (79%) women agreed to participate in early pregnancy and were assessed in late pregnancy.
Methods
Questionnaires were distributed in early and late pregnancy. The questionnaires sought information on socio‐demography, ACE, pain location by pain drawing and pain intensity by visual analogue scales. Distribution of pain was coded in 41 predetermined areas.
Main outcome measures
Pain in third trimester with onset during present pregnancy: intensity, location and number of pain locations.
Results
In late pregnancy, 62% of the women reported any ACE and 72% reported any pain location with onset during the present pregnancy. Among women reporting any ACE the median pain intensity was higher compared with women without such an experience (p = 0.01). The accumulated ACE displayed a positive association with the number of reported pain locations in late pregnancy (r s = 0.19, p = 0.02). This association remained significant after adjusting for background factors in multiple regression analysis (p = 0.01). When ACE was dichotomized the prevalence of pain did not differ between women with and without ACE. The subgroup of women reporting physical abuse as a child reported a higher prevalence of sacral and pelvic pain (p = 0.0003 and p = 0.02, respectively).
Conclusions
Adverse childhood experiences were associated with higher pain intensities and larger pain distributions in late pregnancy, which are risk factors for transition to chronic pain postpartum.
Keywords: adverse childhood experiences, pregnancy, pain, childhood physical abuse, antenatal care
Abbreviations
- ACE
adverse childhood experiences
- CPA
childhood physical abuse
Key Message.
Adverse childhood experiences were associated with higher pain intensities and larger pain distributions in third trimester of pregnancy.
Introduction
Adverse childhood experience (ACE) is a concept where a wide range of traumatic events during the first 18 years in life is assessed 1. Adverse childhood experience includes measures of emotional, sexual and physical abuse and also different forms of household dysfunction. ACE is believed to impair a person's social, emotional and cognitive functions with associated increased risk of developing health problems, certain diseases and premature death 2, 3, 4. Among both genders associations have been shown between accumulated ACE and stress, smoking habits, depression, anxiety, alcoholism, drug use, sexually transmitted disease, obesity, stroke, diabetes, ischemic cardiac disease, cancer and premature death, often in a dose–response relation 1, 5, 6, 7.
Adult survivors of childhood physical abuse (CPA) and sexual abuse have also been shown to have more health problems and chronic pain 8. Among pregnant women exposed to childhood sexual abuse more obstetrical complications, backache, headache and leg cramps were reported during pregnancy and their risk of being hospitalized or of giving birth preterm was increased 9, 10. In a small case–control study childhood abuse, including sexual and physical abuse, was reported to influence obstetric and neonatal complications such as preterm birth, depression and suicidal ideation 11. In the same study and in two large cohort studies it was reported that among pregnant women childhood sexual abuse was a traumatic event with greater negative long‐term effects than other traumatic events 9, 12, 13.
During pregnancy, development of pain, especially of the low back and pelvis, is common. Disabling pain of the low back and pelvis has been reported by up to one in three women during pregnancy 14, 15, 16, with severity and duration of pain as suggested prognostic factors of pelvic pain besides emotional distress 17. However, the impact of the cumulative exposure of ACE on pain development during pregnancy is unknown. Searches on PubMed using words like “Adverse childhood experiences”, “pregnancy” and “pain” did not yield any articles.
The aim of the present study was to examine the association between accumulated ACE and pain developed during pregnancy. We hypothesized that ACE was positively associated with pain intensity, pain location and the number of reported pain areas in late pregnancy.
Material and methods
In Sweden, pregnant women have free antenatal health care at local antenatal clinics and more than 95% of women make use of this offer. This cross‐sectional study was conducted at 18 antenatal clinics in southern Mid‐Sweden. The antenatal clinics were selected by convenience: bigger cities as well as smaller towns were represented. Women were eligible for the study if they were able to understand and speak Swedish, were pregnant and came for enrolment at the antenatal clinic. Each clinic consecutively assessed women for eligibility until they had enrolled a certain amount of women (n = 3 to n = 28). Women were enrolled between October 2011 and April 2012. During the data acquisition, 392 pregnant women visited for enrolment at the antenatal clinics and 293 women were invited to participate. Language difficulties (n = 46), forgetting to ask (n = 26) and time constraints (n = 10) were the most common reasons why the midwives did not ask women about participation. Following informed consent, 232 (79%) women agreed to participate and answered the first questionnaire and 142 (61%) women answered the second.
The participating women were asked to reply to two separate questionnaires, the first in early pregnancy (mean 9.6 completed weeks of pregnancy, 5th and 95th centiles 6 and 13 weeks) and the second in late pregnancy (mean 32.7 completed weeks of pregnancy, 5th and 95th centiles 31 and 36 weeks). The first questionnaire was distributed by the midwife and filled out in the clinic's waiting room or at the woman's home. The second questionnaire was distributed by post to the participants, including two reminders, and was returned in a postage free envelope.
The first questionnaire collected information about age, level of education, occupation, household monthly income, country of birth, partner or not, smoking habits, number of previous pregnancies and gestational week. The second questionnaire collected detailed information about ACEs according to the Adverse Childhood Experience Study group 18. The questionnaire was translated by our research group from English to Swedish, and back‐translated to English again to validate the translation. It was also face‐validated by professionals and lay people. The 19 items used to identify ACEs involved questions within eight categories: emotional abuse, physical abuse, sexual abuse, mother being treated violently, household mental illness, living with a drug user/alcoholic/risk consumer of alcohol, parental separation, and incarcerated household member. All questions about ACE referred to the respondents’ first 18 years of life. The ACEs score was calculated as the sum of each experienced category of ACE, ranging from 0 to 8, with 0 meaning no reported ACE.
Both the first and second questionnaires included a drawing of the body to indicate any location of pain and time of onset of such pain. Indicated pain locations with onset before the present pregnancy were excluded. Furthermore, the women were requested to report the present pain intensity and the worst pain intensity during the past week using visual analogue scales, which ranged from 0 (no pain) to 100 mm (worst possible pain). Only the pain intensities reported in third trimester were used for analysis in this study. The distribution of pain on the pain drawing was coded by using 41 predetermined areas, not shown to the women (Figure 1). If the woman reported pain that extended over two or more of the predetermined areas, each involved area was counted as one pain area. If a woman drew more than one pain location within the same predetermined area, it was counted as one pain area. Having pain was defined as marking one or more pain areas (no/yes).
Figure 1.
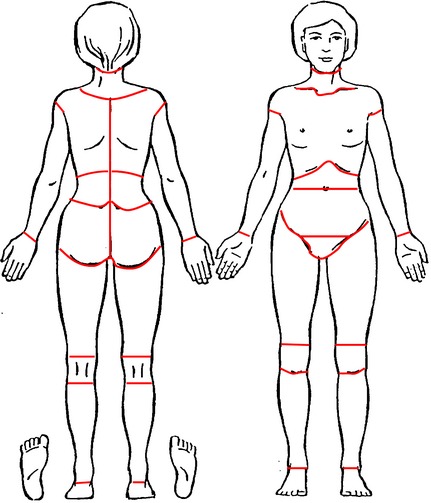
Pain drawing of a female body. The pain location area borders were not shown to the women.
Personal data were handled in accordance with the Personal Data Act 9. The study was approved by the regional ethics committee (Dnr 2010/085). In the information letter the women were asked to contact the researchers responsible for the study or contact the midwives if they felt in need of support.
Statistical analyses
Summary statistics were computed using standard methods. Possible relations based on ordinal data were tested using Spearman's correlation coefficient. For tests based on nominal data the chi‐squared test was used. The General Linear Model and logistic regression were used for regression analyses. The scale assigned for categorization of nominal and ordinal factors used in the regression analyses was: Sweden as country of birth (yes/no) and highest completed education (none/primary school/secondary school/high school/university). Only two‐tailed tests were used. A value of p < 0.05 was considered significant. Statistical analysis was performed using the sas program package version 9.3 (SAS Institute, Cary, NC, USA).
Results
Characteristics of participating women in early pregnancy are presented in Table 1. The women were on average 30.7 years of age, 74% had completed university education, all had a partner, 15% were born outside Sweden, 45% reported pain with onset during present pregnancy and the mean monthly income was 25 000 SEK.
Table 1.
Characteristics in early pregnancy of the women included in the study.
| Characteristic | n | Mean (95% CI) or n (%) |
|---|---|---|
| Age (years) | 140 | 30.7 (30.0–31.4) |
| Completed university education (%) | 142 | 105 (74) |
| Having a partner (%) | 141 | 141 (100) |
| Born outside Sweden (%) | 142 | 15 10 |
| Reported pain in early pregnancy | 142 | 63 (45) |
| Monthly individual income (SEK) | 133 | 25 443 (23 568–27 319) |
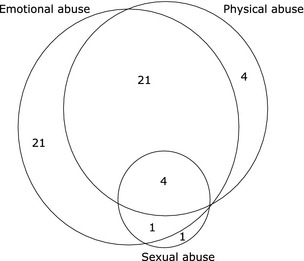
Six of ten women (88/142) reported any kind of ACE with a score ranging from 1 to 5 with a median of 2. The two most commonly reported ACE items were emotional abuse (33%) and parental separation (32%). Physical abuse was reported by 20% and the two least reported were sexual abuse (4%) and incarcerated household member (1%) (Table 2). The combinations of reported emotional, physical or sexual abuse are presented in Figure 2.
Table 2.
The number and proportion of women reporting a particular adverse childhood experience category (more than one experience could be reported).
| Adverse childhood experience | n | % |
|---|---|---|
| Emotional abuse | 47 | 33 |
| Physical abuse | 29 | 20 |
| Sexual abuse | 6 | 4 |
| Mother treated violently | 7 | 5 |
| Household mental illness | 22 | 16 |
| Living with a drug user/alcohol risk consumer | 17 | 12 |
| Parental separation | 45 | 32 |
| Incarcerated household member | 2 | 1 |
Figure 2.
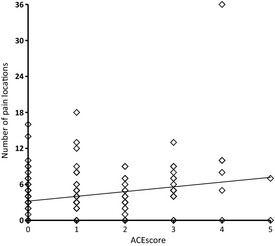
The number of women who reported emotional, physical or sexual abuse, separately or in combination, during childhood. Number of pain locations in late pregnancy by reported number of adverse childhood experiences.
In late pregnancy, any pain location was reported by 102 women (72%) and the prevalence of back pain, sacral pain, pelvic pain and leg pain was 37, 43, 57 and 46%, respectively. Among women reporting pain the median number of pain locations was 5 (range 1–36), the median pain intensity at present was 24 mm (range 0–79) and the median pain intensity as worst during the past week was 59 mm (range 0–98).
In late pregnancy, among women reporting any ACE, the median pain intensity described as worst during the past week was 48 mm, which was different compared with the 23 mm reported by women without any such experience (p = 0.01). Pain intensity at present showed no such difference between the groups (p = 0.13). In addition, the accumulated ACE score displayed a positive association with the number of reported pain locations in late pregnancy (r s = 0.19, p = 0.02) (Figure 3). The prevalence of any reported pain, back pain, sacral pain, pelvic pain or leg pain among women reporting any ACE was not different from that of women without ACE, both including and excluding parental separation as an ACE category.
Figure 3.
Number of pain locations in late pregnancy by reported number of adverse childhood experiences. The number of women who reported emotional, physical or sexual abuse, separately or in combination, during childhood.
Among women reporting the ACE category CPA the prevalence of reported sacral pain was 72% and that of pelvic pain 76%, compared with 35% and 52% among women with no reported child physical abuse (p = 0.0003 and p = 0.02, respectively). The proportions of any reported pain (83% vs. 69%, p = 0.14), back pain (52% vs. 33%, p = 0.06) and leg pain (62% vs. 42%, p = 0.06) were not significantly different. No other separate ACE category showed differences in reported pain locations.
Possible associations between factors reported in early pregnancy and the number of pain locations reported in late pregnancy are displayed in Table 3. In the simple regression analyses, the ACE score and reported pain in early pregnancy were positively, and country of birth was inversely, associated with the number of pain locations. A multivariable regression analysis was performed to find factors that were independently associated with the reported number of pain locations in late pregnancy, with significant factors from the simple regression analyses included as independent variables (Table 3). ACE score and reported pregnancy‐related pain in early pregnancy were positively and independently associated with the number of pain locations in late pregnancy. The R 2 of the model was 0.17 and p < 0.0001.
Table 3.
Association between factors reported in early pregnancy and the number of pain locations reported in late pregnancy.
| Characteristic | Simple linear regression | Multiple linear regression | |||
|---|---|---|---|---|---|
| β‐coefficient | R2 | p | β‐coefficient | p | |
| ACE score (0–8) | 0.79 | 0.05 | 0.007 | 0.75 | 0.007 |
| Reported pain in early pregnancy (no/yes) | 3.00 | 0.11 | <0.0001 | 2.7 | 0.0002 |
| Country of birth (Sweden/other country) | −2.74 | 0.04 | 0.02 | −2.2 | 0.05 |
| Age (years) | −0.17 | 0.03 | 0.05 | ||
| Education (< 12 years/> 12 years) | −0.56 | 0.01 | 0.16 | ||
| Individual income (SEK) | 0.00 | 0.00 | 0.82 | ||
ACE, adverse childhood experience.
R 2 of the full model was 0.17, p < 0.0001.
Possible associations of factors reported in early pregnancy and sacral pain in late pregnancy were investigated in simple and multivariable logistic regression analyses with sacral pain in late pregnancy as the dependent variable and CPA, age, level of education, income and country of birth as independent variables. CPA was the only factor that significantly and independently was associated with sacral pain in late pregnancy with an odds ratio of 4.4 (95% CI 1.7–11.4), p = 0.002 and a concordance of 67 in the multiple analysis.
Discussion
Adverse childhood experience was commonly reported and associated with higher intensity and larger distribution of pain developed during pregnancy. This suggests that information about accumulated ACE in early pregnancy could be useful to identify women who are at risk of developing pain with higher intensity and large distributions later on, as these are known risk factors for transition to chronic pain 19, 20, 21. In addition, among women with pain during pregnancy, information about ACE is warranted because of previously described unfavorable pregnancy outcomes 9, 11.
As this was a cross‐sectional study, we were not able to make any causal inferences but only study the associations between accumulated ACE and pain development. The limited number of participants with small numbers of women within the ACE subgroups suggests that the results have to be interpreted with caution. In addition, the generalizability is limited because of selection bias, such as from high educational levels and high degrees of partnership. Possibly some women with no reported ACE will have experienced, but not remembered, ACE, which would lead to underestimation of the suggested association; whereas the differential recall of ACE among those who developed pain and those who did not might have given the opposite effect. Methodological strengths of this study include consecutive recruitment of the women, use of a back and forth translated version of the validated and extensively used original ACE questionnaire 1 and pain drawings for pain evaluation.
It has earlier been shown that ACEs increase the risk for suffering from a wide range of physical or mental health problems in adulthood 1, 5, 13. In previous studies the prevalence of any ACE could stretch to about two‐thirds of the population, which is close to the 62% prevalence in this study 5. To the best of our knowledge, no previous study has investigated the relation between cumulative ACE and the development of pain during pregnancy or pain in general, while no etiologic role was shown for ACE on the development of rheumatoid arthritis 22. Onset of chronic widespread musculoskeletal pain has been linked to dysfunction of the hypothalamic–pituitary–adrenal stress axis 23, suggesting that a potential mechanism for the effect of ACE on pain development during pregnancy might be through a persistent autonomic nervous system hyper‐reactivity as a consequence of ACE 24. Since victims of CPA and child sexual abuse are at higher risk for re‐victimization 25, 26, 27, 28, it may be likely that participants with ACE have experienced abuse to a greater extent than women without ACE. We had no information about abuse in adulthood in this study.
The finding that CPA had a strong association with pain during pregnancy corresponds well with previous research showing that the experience of CPA is associated with poor health status among young people 29 and that the association persists or presents in adulthood 30. Previous studies show that childhood abuse and post‐traumatic stress have an impact on the occurrence of chronic pain in general and childhood sexual abuse with chronic pelvic pain in particular 31, 32, 33.
Conclusions
Adverse childhood experiences were commonly reported and were associated with pain development during pregnancy in this population of pregnant women. Information about ACE in early pregnancy could be useful to identify women at risk of developing pain of higher intensity and larger distribution, which are in turn known risk factors for transition to chronic pain after childbirth.
Funding
The study had financial support from the Uppsala County Council.
Drevin J, Stern J, Annerbäck E‐M, Peterson M, Butler S, Tydén T, et al. Adverse childhood experiences influence development of pain during pregnancy. Acta Obstet Gynecol Scand 2015; 94: 840–846.
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
References
- 1. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. [DOI] [PubMed] [Google Scholar]
- 2. Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37:268–77. [DOI] [PubMed] [Google Scholar]
- 3. Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–60. [DOI] [PubMed] [Google Scholar]
- 4. Corso PS, Edwards VJ, Fang X, Mercy JA. Health‐related quality of life among adults who experienced maltreatment during childhood. Am J Public Health. 2008;98:1094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37:389–96. [DOI] [PubMed] [Google Scholar]
- 7. Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache. 2010;50:1473–81. [DOI] [PubMed] [Google Scholar]
- 8. Sachs‐Ericsson N, Kendall‐Tackett K, Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Survey. Child Abuse Negl. 2007;31:531–47. [DOI] [PubMed] [Google Scholar]
- 9. Leeners B, Stiller R, Block E, Gorres G, Rath W. Pregnancy complications in women with childhood sexual abuse experiences. J Psychosom Res. 2010;69:503–10. [DOI] [PubMed] [Google Scholar]
- 10. Lukasse M, Schei B, Vangen S, Oian P. Childhood abuse and common complaints in pregnancy. Birth. 2009;36:190–9. [DOI] [PubMed] [Google Scholar]
- 11. Leeners B, Rath W, Block E, Gorres G, Tschudin S. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med. 2014;42:171–8. [DOI] [PubMed] [Google Scholar]
- 12. Boden JM, Fergusson DM, Horwood LJ. Experience of sexual abuse in childhood and abortion in adolescence and early adulthood. Child Abuse Negl. 2009;33:870–6. [DOI] [PubMed] [Google Scholar]
- 13. Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long‐term psychosocial consequences, and fetal death. Pediatrics. 2004;113:320–7. [DOI] [PubMed] [Google Scholar]
- 14. Kristiansson P, Svardsudd K, von Schoultz B. Back pain during pregnancy: a prospective study. Spine (Phila Pa 1976). 1996;21:702–9. [DOI] [PubMed] [Google Scholar]
- 15. Ostgaard HC, Andersson GB, Karlsson K. Prevalence of back pain in pregnancy. Spine (Phila Pa 1976). 1991;16:549–52. [DOI] [PubMed] [Google Scholar]
- 16. Zib M, Lim L, Walters WA. Symptoms during normal pregnancy: a prospective controlled study. Aust N Z J Obstet Gynaecol. 1999;39:401–10. [DOI] [PubMed] [Google Scholar]
- 17. Bjelland EK, Eskild A, Johansen R, Eberhard‐Gran M. Pelvic girdle pain in pregnancy: the impact of parity. Am J Obstet Gynecol. 2010;203:146 e1–6. [DOI] [PubMed] [Google Scholar]
- 18. Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282:1652–8. [DOI] [PubMed] [Google Scholar]
- 19. Ostgaard HC, Roos‐Hansson E, Zetherstrom G. Regression of back and posterior pelvic pain after pregnancy. Spine (Phila Pa 1976). 1996;21:2777–80. [DOI] [PubMed] [Google Scholar]
- 20. Brynhildsen J, Hansson A, Persson A, Hammar M. Follow‐up of patients with low back pain during pregnancy. Obstet Gynecol. 1998;91:182–6. [DOI] [PubMed] [Google Scholar]
- 21. Eisenach JC, Pan PH, Smiley R. Lavand'homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Carette S, Surtees PG, Wainwright NW, Khaw KT, Symmons DP, Silman AJ. The role of life events and childhood experiences in the development of rheumatoid arthritis. J Rheumatol. 2000;27:2123–30. [PubMed] [Google Scholar]
- 23. McBeth J, Silman AJ, Gupta A, Chiu YH, Ray D, Morriss R, et al. Moderation of psychosocial risk factors through dysfunction of the hypothalamic–pituitary–adrenal stress axis in the onset of chronic widespread musculoskeletal pain: findings of a population‐based prospective cohort study. Arthritis Rheum. 2007;56:360–71. [DOI] [PubMed] [Google Scholar]
- 24. Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. Pituitary–adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–7. [DOI] [PubMed] [Google Scholar]
- 25. Cannon EA, Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Adult health and relationship outcomes among women with abuse experiences during childhood. Violence Vict. 2010;25:291–305. [DOI] [PubMed] [Google Scholar]
- 26. Becker KD, Stuewig J, McCloskey LA. Traumatic stress symptoms of women exposed to different forms of childhood victimization and intimate partner violence. J Interpers Violence. 2010;25:1699–715. [DOI] [PubMed] [Google Scholar]
- 27. Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse, adolescent sexual behaviors and sexual revictimization. Child Abuse Negl. 1997;21:789–803. [DOI] [PubMed] [Google Scholar]
- 28. Coid J, Petruckevitch A, Feder G, Chung W, Richardson J, Moorey S. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross‐sectional survey. Lancet. 2001;358:450–4. [DOI] [PubMed] [Google Scholar]
- 29. Annerback EM, Sahlqvist L, Svedin CG, Wingren G, Gustafsson PA. Child physical abuse and concurrence of other types of child abuse in Sweden‐Associations with health and risk behaviors. Child Abuse Negl. 2012;36:585–95. [DOI] [PubMed] [Google Scholar]
- 30. Bonomi AE, Cannon EA, Anderson ML, Rivara FP, Thompson RS. Association between self‐reported health and physical and/or sexual abuse experienced before age 18. Child Abuse Negl. 2008;32:693–701. [DOI] [PubMed] [Google Scholar]
- 31. Lampe A, Doering S, Rumpold G, Solder E, Krismer M, Kantner‐Rumplmair W, et al. Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res. 2003;54:361–7. [DOI] [PubMed] [Google Scholar]
- 32. Finestone HM, Stenn P, Davies F, Stalker C, Fry R, Koumanis J. Chronic pain and health care utilization in women with a history of childhood sexual abuse. Child Abuse Negl. 2000;24:547–56. [DOI] [PubMed] [Google Scholar]
- 33. Arguelles LM, Afari N, Buchwald DS, Clauw DJ, Furner S, Goldberg J. A twin study of posttraumatic stress disorder symptoms and chronic widespread pain. Pain. 2006;124:150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


