Abstract
Objective
Improving the quality and safety of health care in Australia is imperative to ensure the right treatment is delivered to the right person at the right time. Achieving this requires appropriate clinical governance and support for health professionals, including professional supervision. This study investigates the usefulness and effectiveness of and barriers to supervision in rural and remote Queensland.
Design
As part of the evaluation of the Allied Health Rural and Remote Training and Support program, a qualitative descriptive study was conducted involving semi‐structured interviews with 42 rural or remote allied health professionals, nine operational managers and four supervisors. The interviews explored perspectives on their supervision arrangements, including the perceived usefulness, effect on practice and barriers.
Results
Themes of reduced isolation; enhanced professional enthusiasm, growth and commitment to the organisation; enhanced clinical skills, knowledge and confidence; and enhanced patient safety were identified as perceived outcomes of professional supervision. Time, technology and organisational factors were identified as potential facilitators as well as potential barriers to effective supervision.
Conclusions
This research provides current evidence on the impact of professional supervision in rural and remote Queensland. A multidimensional model of organisational factors associated with effective supervision in rural and remote settings is proposed identifying positive supervision culture and a good supervisor–supervisee fit as key factors associated with effective arrangements.
Keywords: allied health, clinical supervision, professional development for rural health professionals, professional supervision, rural health workforce
What is already known on this subject.
Professional supervision has reported benefits to organisations, professionals and patients in metropolitan settings although research lacks rigour.
There is a lack of peer‐reviewed supervision research in rural, remote and regional settings.
What this study adds.
Using a qualitative descriptive methodology, this study explored usefulness, impact and barriers to non‐metropolitan allied health professional supervision.
Multiple stakeholder perspectives including managers, professional supervisors and supervisees are reported.
Based on literature and study findings, a model is proposed to support the implementation of effective supervision arrangements in non‐metropolitan settings.
Introduction
In Australia, disparities in health status between metropolitan residents and those residing outside the bigger centres have been well documented.1 Recruitment and retention of staff in rural and remote areas continue to be challenging, with issues of professional isolation, limited resources, complex service demands and time and distance barriers to accessing support.2, 3, 4 Professional supervision, henceforth referred to as supervision, is one method to support health professionals that has demonstrated widespread benefits to health professionals, patients and organisations in metropolitan settings.5, 6, 7 There have been repeated calls for coordinated professional support programs8, 9, 10 and there are known initiatives being evaluated across the nation11, 12, 13, 14; however, there remains a lack of peer‐reviewed, published literature relevant to rural and remote allied health services.15
A review of the supervision literature demonstrates that a ‘one size fits all’ approach does not hold true in rural and remote services with supervision in these contexts influenced by multiple factors.8 The significance of factors such as the supervisory relationship, supervisor–supervisee matching and organisational support in promoting effective supervision has been highlighted in studies of the wider health workforce.16, 17, 18 As a range of additional factors influence workforce issues in rural and remote areas,8 research is needed to investigate the factors that contribute to effective supervision.
The Allied Health Rural and Remote Training and Support (AHRRTS) program coordinated by the Cunningham Centre, Darling Downs Hospital and Health Service was designed to provide capability‐based clinical education, training and professional support to the allied health workforce in non‐metropolitan Queensland Health. The intention of the AHRRTS initiative was to provide a holistic program of development and support strategies specifically focused on building requisite capabilities, such as evidence‐based practice and professional skills. The AHRRTS program coordinated professional support activities including supervision matching, whereby a rural/remote clinician was matched up with an appropriate supervisor from another area in the state. It also made funding available for face‐to‐face supervision meetings and incentives for rural/remote supervisors who were providing support.
The AHRRTS program was formally evaluated between 2010 and 2012 (S. Kumar et al., unpublished, 2012). As part of this evaluation, a qualitative study of the usefulness and impact of supervision on professional practice and service delivery was conducted through interviewing supervisees, supervisors and operational managers. The current paper reports findings from one element of this evaluation, factors that underpin effective supervisory practice in rural and remote allied health services, based on multiple stakeholder reports.
Method
Theoretical framework and design
Schoo et al.8 proposed a conceptual model for recruitment and retention of allied health workforce in rural Victoria, Australia. This multidimensional model illustrates that a range of factors are associated with the recruitment and retention of this group in rural areas. Organisational factors and availability of professional support and supervision have been identified as key factors that influence retention. Using this model as the theoretical framework, the current study investigated relevant multidimensional aspects of effective supervision in rural and remote areas.
A qualitative, descriptive research design was used, whereby participants' experiences were captured in their own words.19 Participants were invited to provide feedback on the usefulness and impact of supervision, as well as any barriers to participation. While wording used slightly varied based on whether supervisors, operational managers or supervisees were being interviewed, questions for supervisees were specifically:
-
1.
What are the most useful aspects of supervision?
-
2.
What effect has supervision had on your practice (if any)?
-
3.
What are the barriers to participating effectively in supervision?
Ethics
Ethical approval was obtained from both Queensland Health and University of South Australia (UniSA) Human Research and Ethics Committees.
Participant selection
Participants were employees of Queensland Health and included 42 rural and remote allied health professionals (shown in Table 1), nine operational managers and four supervisors (two physiotherapists, an occupational therapist and a social worker). Purposive sampling was chosen in order to ensure diversity of participants,20 and a range of disciplines with various levels of rural experience, management and supervision responsibilities were represented from across the state. The greatest proportion of participants were from rural areas of the Darling Downs region (33%), followed by the South West region (24%), equal representation from Central Queensland and Central West (14% each) and smaller numbers from Townsville, Mackay and Wide Bay regions (5% each). Professional and regional spread was diverse and closely matched demographics of participants in the wider AHRRTS program.
Table 1.
Allied health professions in the study
| Allied health discipline | Number of study participants |
|---|---|
| Dietetics | 4 |
| Medical radiation professionals | 2 |
| Nutrition | 7 |
| Occupational therapy | 8 |
| Physiotherapy | 6 |
| Psychology | 1 |
| Social work | 11 |
| Speech pathology | 3 |
Data collection
Following informed consent, researchers conducted individual telephone interviews lasting 20–40 min. Recognising the importance of trustworthiness in qualitative research, a number of key processes were employed to ensure rigour.19, 20, 21 These strategies included use of trained interviewers from the AHRRTS program and UniSA, adherence to standardised data collection protocol including a semi‐structured interview protocol, audio‐taping interviews and transcribing verbatim by an independent typist with subsequent validation by the interviewee, monitoring interviews for consistency of methods including either an independent observer monitoring the process or a second review of the recording to ensure adherence to the protocol, coding by more than one coder, and cross‐checking between coders. Any differences between the coders were discussed until consensus was reached. Thick descriptions in the form of meaningful quotations to represent important themes were included. Data were de‐identified to ensure participant confidentiality.
Data analysis
Data were categorised using thematic analysis.19 The process of thematic analysis involved continually revisiting the data and reviewing the categorisation of data until the researchers were sure that the themes and categories used to summarise and describe the findings were truthful and accurate reflection of the data. A qualitative data management system, Nvivo9 software,22 was utilised to manage the data throughout the process.
Results
As presented below, supervisees, supervisors and operational managers described their perspectives on the usefulness and effect of supervision on professional practice and service delivery. Specific facilitators of and barriers to effective supervision were identified.
A number of themes were corroborated across rural and remote supervisees, supervisors and operational managers. These have been broadly grouped into usefulness/effects of supervision and facilitators of effective supervision.
Usefulness/effects of supervision
These included enhanced clinical skills, knowledge and confidence; reduced professional isolation; increased growth and professional enthusiasm; and increased evidence‐based practice and patient safety as a result of supervision.
Enhanced clinical skills, knowledge and confidence
Supervisees reported value from their experience in supervision including enhanced confidence, knowledge and clinical skills.
I feel more confident and calmer. Because you are by yourself and you're having to make all the decisions, it can be really, really stressful and sometimes it's really good to just get rid of that stress, or even just to have a bit of a vent about things and then you can approach things calmly. … It helps me think outside the box a bit more … change my approaches …
Supervisors had similar views about the impact of the supervision in rural and remote practice, including noticing increasing confidence, clinical reasoning and improved application of techniques in their supervisees.
Reduced professional isolation
Participants reflected on the advantages of having expert assistance and support when needed, thus reducing professional isolation. A rural new graduate supervisee commented on the benefits of having an expert to support clinical decision making.
I think for me, as a new graduate, it's having that clinical support there and being able to, when you get a difficult case, be able to have someone really clearly identify this is the person you can call when you're having an issue clinically in this case.
Supervisors also highlighted the importance of supervision to provide professional connections and support across distance.
Enhanced professional enthusiasm
Enthusiasm, growth and organisational commitment were identified by supervisors and supervisees. One supervisor commented:
… we did an evaluation just when we had our face to face meeting, she said that she's more enthusiastic about her position, she's more motivated, she's more organised and she's been encouraged to do more skills development activities.
Patient safety
Improved evidence‐based practice, best practice, patient safety and clinical governance were identified by managers, supervisors and clinicians. An operational manager reiterated the critical role of supervision to support evidence‐based practice and patient safety:
… and, we really do need to ensure that our clinicians are doing the best practice, that they are supported to develop the skills they need for the role they do, and to have someone to support them to do that, not just measure them against it …
Usefulness for supervisors
Data analysis from supervisor interviews identified benefits they gained from providing supervision.
… I think the experience I've gained now I owe to a lot of individual physiotherapists who spent time with me over the years … So that's the main driver for me to continue with the program and I get a lot of enjoyment from it because of that …
Facilitators of and barriers to effective supervision
Supervision culture
Participants reported a number of facilitators of and barriers to effective supervision including time, travel, technology and organisational factors which come under the broad banner of supervision culture. Time was often reported as a significant barrier, for example:
Time is the biggest one … and my time management. Because my supervisor only works part‐time and I'm on outreach almost all the time and he's on outreach all the time, finding time when we can both access a phone … and have the internet in front of us is tricky.
Supervisors specifically highlighted the issue of travel time as a barrier. Some commented that being physically present with their supervisee might be beneficial but could recognise the limitations on travel, including the extra time, costs and resources involved. Utilising innovative means to facilitate distance supervision, including videoconferencing, email and teleconference were seen as facilitators by some respondents. However, some supervisees discussed use of technology as a barrier due to the limited access and at times limited functionality of such resources. Some suggested that they experienced difficulties meeting their supervision needs over the phone; for example, when observation was needed to address novel client presentations.
As with time, travel and technology, organisational factors were also considered both as a facilitator and barrier. When there were organisational drivers, such as management support and supervision policies and procedures in place, supervision was prioritised. One supervisee commented:
I don't know that I have too many barriers at the moment with my supervision. (My manager) is quite strict on supervision and the fact that it does take priority in your workload.
When organisational drivers were not in place, some supervisees reported that supervision arrangements had not progressed or been prevented from being initiated.
Supervisor–supervisee fit
Finally, supervisor and supervisee fit was reported to be of critical importance. When supervision was ineffective it was often attributed to a poor match. Many supervisees and supervisors discussed their positive relationship, that it was often reciprocal and that a good match was directly related to perceived usefulness. One supervisee who was matched with a supervisor through the AHRRTS program demonstrated this:
I've found it great. The two people who I have been matched up with over the last eighteen months have both come from very similar caseloads in terms of smaller towns and using an outreach model. They've have also come from similar multi‐disciplinary teams where they've either been the sole OT or working with only one other OT. It's been really good.
Discussion
Despite a lack of rigorous published research, increasing evidence supports the important role of supervision in non‐metropolitan allied health settings.6 Given the continued pressure on these services,2, 3, 4, 8, 9, 10 it is important that allied health professionals are provided with avenues for ongoing support including effective supervision. The results of this research highlight the important contribution of supervision to health service delivery in rural and remote areas. These findings concur with previous research in metropolitan settings showing supervisees' positive experiences with supervision including enhanced confidence, clinical skills and knowledge.5, 6 Important benefits unique to rural and remote allied health settings included reduced professional isolation and enhanced professional enthusiasm. In accordance with previous studies,6, 23 stakeholders reported organisational benefits to supervision implementation including improved clinical governance and enhanced staff retention. Similar to the few studies that have directly investigated outcomes on patients,7, 24 our findings were that key stakeholders also viewed supervision to be important for best practice outcomes and patient safety.
In accordance with study findings on barriers and enablers, and utilising a multidimensional framework,8 The Y model of effective supervision in rural and remote settings is proposed (Fig. 1). Positive supervision culture and supervisee–supervisor fit appear to be key factors that are associated with useful supervision as reported by supervisees, supervisors and operational managers. Positive supervision culture includes optimal and effective use of technology to manage geographical barriers, finding time for supervision, valuing the role of supervision in improving patient care, organisational commitment to supervision and support for supervisor. Supervisee–supervisor fit strengthens the supervisory relationship that has been shown in empirical studies to be the single most important factor that influences the quality of supervision.23, 24, 25, 26, 27
Figure 1.
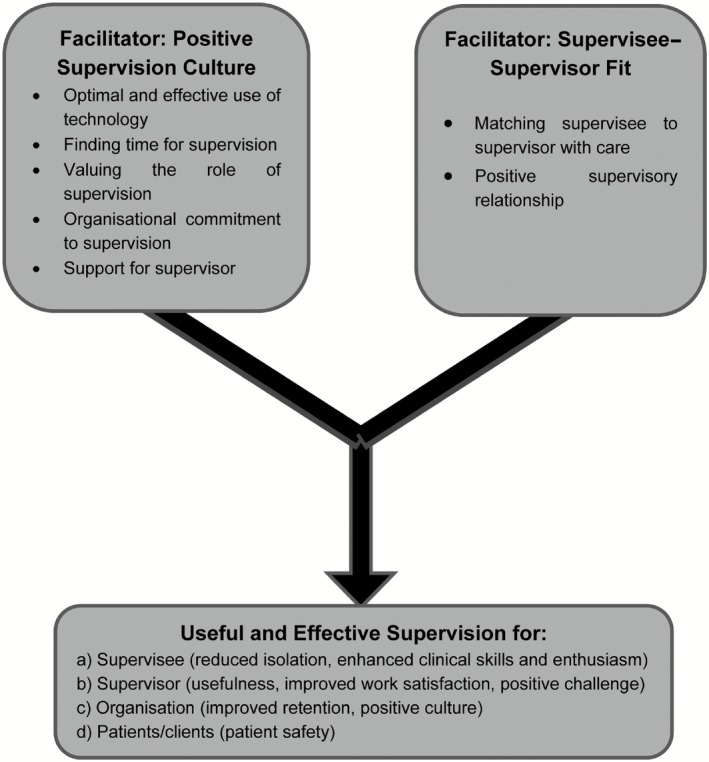
The Y model of effective supervision in rural and remote settings.
Some limitations of this study must be acknowledged. Although a strength of this study was the wide range of stakeholders' sampled leading to diverse perspectives, this may also be considered a weakness as discipline‐specific information was not investigated. Some interviews were conducted by AHRRTS program officers, which may have inhibited respondents from revealing all perspectives on the program. As data collected by program officers and independent researchers did not differ, this is not considered a significant limitation.
Despite its usefulness, barriers to effective supervision continue to exist. Unless organisational factors are addressed (e.g. through recognised, implemented policies supporting supervision), barriers such as time, competing clinical priorities and lack of dedicated resources will deter potential benefits. It is recommended that key elements of the Y model of effective supervision including support for a positive supervision culture and appropriate supervisor–supervisee fit are implemented in rural and remote allied health settings to ensure that supervision arrangements are effective.
Conclusion
Evidence indicates that despite supervision being considered as useful with a range of positive influences, there appear to be numerous barriers that could blunt its impact in rural and remote settings. Health care organisations and stakeholders should take this into consideration when implementing supervision in practice. Further research could also consider the parameters of effective supervision (such as content, frequency and duration) in rural and remote contexts as this is a gap in the current literature.
References
- 1. Health Workforce Australia . HWA Annual Report 2011–2012, Australian Government. 2012. [Cited 2 September 2014]. Available from URL: https://hwa.gov.au/sites/uploads/HWA‐Annual‐Report‐2011‐2012_0.pdf
- 2. Battye KM, McTaggart K. Development of a model for sustainable delivery of outreach allied health services to remote north‐west Queensland, Australia. Rural and Remote Health 2003; 3: 194. [PubMed] [Google Scholar]
- 3. Lindsay R, Hanson L, Taylor M, McBurney L. Workplace stressors experienced by physiotherapists working in regional public hospitals. The Australian Journal of Rural Health 2008; 16: 194–200. [DOI] [PubMed] [Google Scholar]
- 4. McAuliffe T, Barnett F. Factors influencing occupational therapy students' perceptions of rural and remote practice. Rural and Remote Health 2009; 9: 1078. [PubMed] [Google Scholar]
- 5. Martin P, Copley J, Tyack Z. Twelve tips for effective clinical supervision based on a narrative literature review and expert opinion. Medical Teacher 2014; 36: 201–207. [DOI] [PubMed] [Google Scholar]
- 6. Dawson M, Phillips B, Leggat S. Clinical supervision for allied health professionals: a systematic review. Journal of Allied Health 2013; 42: 65–73. [PubMed] [Google Scholar]
- 7. Farnan JM, Petty LA, Georgitis E et al A systematic review: the effect of clinical supervision on patient and residency education outcomes. Academic Medicine 2012; 87: 1–15. [DOI] [PubMed] [Google Scholar]
- 8. Schoo AM, Stagnitti KE, Mercer C, Dunbar J. A conceptual model for recruitment and retention: allied health workforce enhancement in Western Victoria, Australia. Rural and Remote Health 2005; 5: 477. [PubMed] [Google Scholar]
- 9. Stagnitti KE, Schoo AM, Dunbar J, Reid C. An exploration of issues of management and intention to stay. Journal of Allied Health 2006; 35: 226–232. [PubMed] [Google Scholar]
- 10. Rourke J. WHO recommendations to improve retention of rural and remote health workers – important for all countries. Rural and Remote Health 2010; 10: 1654. [PubMed] [Google Scholar]
- 11. WA Country Health Service . Professional Support: Clinical Supervision for Allied Health Professionals. Perth: Department of Health, 2008. [Cited 2 September 2014] Available from URL: http://www.wacountry.health.wa.gov.au/fileadmin/sections/allied_health/WACHS_R_AH_ProSupport_ClinSupervision.pdf [Google Scholar]
- 12. NSW Institute of Rural Clinical Services and Teaching . A report: clinical supervision for allied health professionals in rural NSW. Sydney: IRCST, 2008. [Cited 2 September 2014]. Available from URL: http://www.ruralheti.health.nsw.gov.au/__documents/initiatives/rural‐allied‐health‐project/rural_nsw_allied_health_clinical_supervision_paper_final.pdf
- 13. The Allied & Scientific Health Office . SA health allied health clinical supervision framework. Adelaide: SA Health, 2014. [Cited 2 September 2014]. Available from URL: http://www.sahealth.sa.gov.au/wps/wcm/connect/ad788900438bd2b689308dfd37f1549d/ASH+Clin+Super+Framework+2014.pdf?MOD=AJPERES&CACHEID=ad788900438bd2b689308dfd37f1549d
- 14. Hall F, Bell K. Professional support framework: improving access to professional support for professionals. Australian Health Review 2013; 37: 560–565. [DOI] [PubMed] [Google Scholar]
- 15. Ducat WH What do we really know about best practice allied health supervision? Proceedings of the 12th National Rural Health Conference, Adelaide: National Rural Health Alliance, 2013. [Cited 2 September 2014]. Available from URL: http://nrha.org.au/12nrhc/wp‐content/uploads/2013/06/Ducat‐Wendy_ppr.pdf
- 16. Dawson M, Phillips B, Leggat SG. Effective clinical supervision for regional allied health professionals – the supervisee's perspective. Australian Health Review 2012; 36: 92–97. [DOI] [PubMed] [Google Scholar]
- 17. Edwards D, Cooper L, Burnard P et al Factors influencing the effectiveness of clinical supervision. Journal of Psychiatric and Mental Health Nursing 2005; 12: 405–414. [DOI] [PubMed] [Google Scholar]
- 18. Hall F, Bell K. Professional support framework: improving access to professional support for professionals. Australian Health Review 2013; 37: 560–565. [DOI] [PubMed] [Google Scholar]
- 19. Rice P, Ezzy D. Qualitative Research Methods: A Health Focus. Oxford: Oxford University Press, 1999. [Google Scholar]
- 20. Patton M. Qualitative Research and Evaluation Methods, 3rd edn Thousand Oaks, CA: Sage Publications, 2002. [Google Scholar]
- 21. Barbour RS. Education and debate: checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ (Clinical Research Ed.) 2001; 322: 1115–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nvivo9 softwareTM QSR International Pty Ltd . NVivo qualitative data analysis software; QSR International Pty Ltd. 2010. [Cited March 2011]. Available from URL: http://www.qsrinternational.com/
- 23. Hyrkäs K. Clinical supervision, burnout and job satisfaction among mental health psychiatric nurses in Finland. Issues in Mental Health Nursing 2005; 26: 531–556. [DOI] [PubMed] [Google Scholar]
- 24. Bambling M, King R, Raue P, Schweitzer R, Lambert W. Clinical supervision: its influence on client‐rated working alliance and client symptom reduction in the brief treatment of major depression. Psychotherapy Research 2006; 16: 317–331. [Google Scholar]
- 25. Cox DL, Araoz G. The experience of therapy supervision within a UK multi‐centre randomized controlled trial. Learning in Health and Social Care 2009; 8: 301–314. [Google Scholar]
- 26. Herkt JA, Hocking C. Supervision in New Zealand: professional growth or maintaining competence? New Zealand Journal of Occupational Therapy 2007; 54: 24–30. [Google Scholar]
- 27. Kavanagh DJ, Spence SH, Strong J, Wilson H, Sturk H, Crow N. Supervision practices in Allied Mental Health: relationships of supervision characteristics to perceived impact and job satisfaction. Mental Health Services Research 2003; 5: 187–195. [DOI] [PubMed] [Google Scholar]


