Abstract
Purpose
Although typically not painful, preventive dental care can be distressing to young children. A greater understanding of how adults perceive child distress may enable clinicians to improve the patient/parent experience through alignment of values and facilitation of shared decision-making. This study examined the association between parent, dentist, and independent observer (IO) ratings of child distress during preventive dental procedures.
Methods
65 children under 3 years of age were seen for preventive dental care at a university-based dental clinic. Parents, dentists, and an IO rated intensity of child distress (0 = none; 5 = extreme) during 4 phases of the dental visit: pre-exam, positioning, prophylaxis/exam/fluoride, and post-exam.
Results
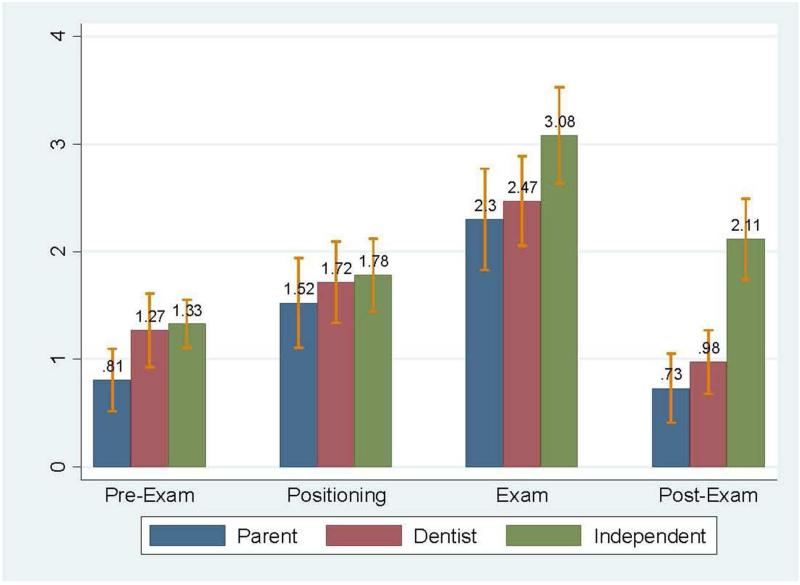
The average age of the children was 24.4 months (SD 7.2). The prophylaxis/exam/fluoride phase was judged to be most distress inducing. Mean distress ratings for this phase were: 2.30 (parents), 2.47 (dentists), and 3.08 (IO). This difference was statistically significant (p = .04). The IO ratings were significantly different from parents (for 3 phases) and dentists (for 1 phase); no statistically significant differences were noted between parent and dentist ratings for any phase.
Conclusions
There was a strong agreement between parents’ and dentists’ ratings of child distress during preventive dental procedures.
Keywords: pain, stress, psychological, infant
Introduction
The American Academy of Pediatric Dentistry and American Academy of Pediatrics recommend that children establish a dental home by age one.1, 2 Despite these recommendations, many parents have not developed a habit of routine preventive dental care for their young children. Initiation of dental care at a young age is associated with greater use of preventive services and with lower dentally-related costs.3, 4 Early initiation of dental care is particularly important for low-income children who have poorer dental attendance and are more likely to develop tooth decay than are children of higher income families5-9
While the reasons for poor dental attendance by low-income children are varied, factors such as an unpleasant first dental visit and dissatisfaction with dentists and office staff have been associated with less than optimal pediatric dental attendance.10, 11 More than 30 years of research has shown that exhibiting characteristics such as empathy and encouragement greatly improves relations and communication between clinicians and parents. Parents that feel supported, in turn, are reassured about their children’s health, and it is inferred that these parents have better compliance with future medical recommendations.12 Child behavior during the visit is also important. Some parents avoid taking their child to the dentist because they perceive their child’s crying and distress behaviors at the dental office as distressing.13, 14 As a result of these findings, parent attitudes and psychosocial motivation to pursue care have become major foci of health interventions.15-19
Preventive dental care for young children consists of relatively “benign” procedures including an examination of the oral cavity and the application of fluoride varnish. While the dental provider may perceive these services to be non-painful and therefore non-invasive, the visit may not necessarily be viewed by parents in the same way. In fact, a previous study, reported that over half of parents felt that their child experienced moderate to severe distress during these procedures.27
Recognizing children’s discomfort is key to understanding clinical interactions from the perspectives of the patient and parent. The term stress relates to factors that cause physical or mental tension, while distress refers to suffering related to excess stress. Pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage.”20 Experts in pediatric pain assessment suggest that there is considerable overlap in the measure of pain and distress. 35, 36 For example, facial grimace, cry, and scream can relate to pain experienced during an injection or distress related to a non-painful exam.37 Therefore, it is important to consider that these physical signs may represent a continuum of the stress reaction. In practice, the two terms “stress” and “distress” are used interchangeably.
Historically medical pain has been underrecognized and undertreated in very young children.21-26
Underestimation of patient discomfort by clinicians has been referred to as “pain blindness.”28, 29 The literature suggests that medical and dental providers do not assess children’s discomfort accurately and are often at odds with parents’ and independent observers’ (IO) perceptions of children’s pain.25, 26, 29, 30
Today’s model of shared decision-making in healthcare implies that parents, dentists, and pediatric patients must align values and share an element of trust and accountability.31, 32 This requires a certain amount of agreement among the triad regarding pain or distress during the dental visit. Therefore, accurate assessment of child pain and discomfort is an important step in developing rapport with families and improving the parent and patient experience.
In this study, parents, dentists, and an IO rated young children’s behavior during a dental examination and preventive treatment. The objective was to determine if dentists’ perception of child distress at sequential stages of the dental visit was similar to that of the other observers.
Methods
This study was approved by the study university’s Institutional Review Board, and each participating parent underwent the informed consent process prior to entering the study. A convenience sample of 65 parents of children presenting to a university-based pediatric dental clinic for preventive care from April 2012 to March 2014 was chosen. The parents and children were selected from the patient pool of 21 faculty, and resident, dentist participants. Inclusion criteria required that the parents were fluent in English, the patient was enrolled in the federal Medicaid program for low-income children, in good overall health, and was 6 to 36 months of age.
After check-in with the clinic reception desk, parents were approached by a member of the research team and invited to participate in the study. Consenting parents then completed a socio-demographic questionnaire that included questions about the child’s dental health status and if the child had seen a dentist any time in the past. Standard of care preventive procedures, including a prophylaxis, visual oral examination, and fluoride varnish treatment were performed and video recorded. The majority of children were examined in the knee-to-knee position. The video recordings were archived for analysis by a developmental psychologist IO-who was not present at the clinic.
Parents rated the child’s distress on a 10 point numeric rating scale (0 = “no distress” and 10 = “distress as bad as it could be”) during or immediately following each of 4 phases of the visit:
Phase I-Pre-exam, dentist entered the room
Phase II-Positioning, parent reclined the child into the knee-to-knee position or dentist lowered the child’s chair
Phase III-Prophylaxis/exam/fluoride, dentist conducted a prophylaxis, visual exam, and applied fluoride varnish
Phase IV-Post-exam, child returned to an upright position until dentist left the room or 3 minutes after returned to start position
To facilitate the flow of procedures the treating dentist rated the child’s distress using the same 10-point scale, but did so at the conclusion of the visit. This measure was derived from metrics used in clinical studies of pain responses to medical procedures in which the terms “pain” and behavioral “distress” are used interchangeably. 33, 34
At a later time, an IO (CH) reviewed the video recording of each child’s visit and rated distress according to the Behavioral Approach-Avoidance and Distress Scale (BAADS; Hubert, Jay, Saltoun and Hayes, 1988).
The BAADS scale consists of two subscales, one assessing approach-avoidance and the other assessing distress. Each subscale is scored using 5-point behaviorally anchored ratings. In this study, we rated child behavior on the distress subscale. The ratings range from 1, indicating no distress, a calm appearance, and not crying to scores of 2 to 4, indicating moderate distress, some crying, or moderate muscle tension. The most extreme rating is 5 and indicates extreme distress, agitation, screaming or extreme muscle tension. In this study, we report the BAADS distress subscale scores for the same dental visit phases rated by the parents and dentists. Each of the four phases received a single BAADS distress score of 1 to 5.
Descriptive statistics (means, standard deviations, counts, and percentages) were calculated for all variables. Numerical scores provided by parents and dentists were scaled proportionally (reduced by ½) to allow for direct comparison with the BAADS distress score. Differences in distress ratings between the three raters for each of the four phases of the dental visit were determined using ANOVA. After the ANOVA, a post-hoc analysis using a Bonferroni comparison was performed to calculate the associations between distress ratings of two observers in each phase. The significance level was pre-set to 0.05.
Results
Caregivers in the sample largely consisted of mothers who identified as white and Asian, the majority of whom had attended at least some college. The average age of children enrolled was 24.4 ± 7.2 months. The majority of parents reported that their child had previously visited a dentist (72.3%), and most indicated that their child had good to excellent dental health (80%). The demographics of this convenience sample are consistent with the clinic as a whole and with populations that participated in previous research projects at the study institution. (Table 1)
Table 1.
| Demographic Characteristics of Adults and Child Participants |
N = 65 |
| Mean (SD*) | |
| Child Age (months) | |
| 24.4 (7.2) | |
| N (%) | |
| Relation to Child | |
| Mother | 53 (81.6%) |
| Father | 10 (15.4%) |
| Other | 1 (1.5%) |
| Missing | 1 (1.5%) |
| Ethnic Origin | |
| White | 34 (52.3%) |
| Black | 2 (3.1%) |
| Asian | 14 (21.5%) |
| Other/Multiple | 8 (12.3%) |
| Missing | 7 (10.8%) |
| Education | |
| High school or less | 14 (21.5%) |
| Some College | 23 (35.4%) |
| 4 year College or more | 26 (40.0%) |
| Missing | 2 (3.1%) |
| Child Has Been to a Dentist Previously | |
| Yes | 47 (72.3%) |
| No | 18 (27.7%) |
| Parent Rating of Child’s Dental Health | |
| Excellent | 12 (18.5%) |
| Very Good | 17 (26.1%) |
| Good | 23 (35.4%) |
| Fair | 5 (7.7%) |
| Poor | 2 (3.1%) |
| Don’t know | 4 (6.1%) |
| Missing | 2 (3.1%) |
SD = Standard Deviation
Elapsed time for the four dental visit phases was calculated. The mean exam time was 11.28 minutes. As expected, the quickest exam phase was positioning, averaging 12 seconds (mean = 0.20 minutes, SD 0.31). The prophylaxis/exam/fluoride phase was longer at just over 3 minutes (mean = 3.08 minutes, SD 3.12). The pre-exam times showed wide variation, due in part to alterations of camera start time. Post-exam times showed little variation because recordings were truncated 3 minutes after the dentist left the room. (Table 2)
Table 2.
Duration of Dental Visit Phases (In Minutes)
| N | Mean | SD | Min | Max | |
|---|---|---|---|---|---|
| Pre-Exam* | 61 | 6.07 | 5.26 | 0.32 | 25.98 |
| Positioning | 60 | 0.20 | 0.31 | 0.02 | 1.82 |
| Prophylaxis/Exam/Fluoride | 63 | 3.08 | 3.12 | 0.35 | 17.28 |
| Post-Exam** | 61 | 2.20 | 0.90 | 0.42 | 3.00 |
| Total Time | 63 | 11.28 | 6.13 | 2.53 | 32.47 |
Pre-Exam: limited to period that was video recorded
Post-Exam: truncated to a max of 3 minutes
Parents, dentists, and the IO judged the prophylaxis/exam/fluoride phase to be the most distressing. The mean distress ratings given for this phase were highest for the IO (3.08), followed by the dentists (2.47) and parents (2.30).The IO evaluated the post-exam period to be the next most distressing phase, while parents and dentists rated the second most distressing phase to be positioning. On average, parents assessed their child as experiencing less distress than the dentists and IO, and this was true for each of the four phases. Overall, the mean distress scores for child participants were in the mild to moderate range. (Figure 1)
Mean Distress Rating By Reviewer and Exam Phase
There were no statistically significant differences between parent and dentist ratings for any phase of the dental visit. Statistically significant differences were found when comparing parent and dentist ratings with the IO. Differences between raters were greatest during the pre-exam (p = .02) and post-exam (p <.001) phases. IO ratings were significantly greater than parents for the pre-exam (mean .52, p = .04), prophylaxis/exam/fluoride (mean .78, p = 0.04), and post-exam (mean 1.38, p <.001) phases. IO ratings were significantly greater than dentists for the post-exam (mean 1.14, p <.001) phase. (Table 3)
Table 3.
Associations between Distress Rating and Observer Type
| Pre-Exam | Positioning | Prophylaxis/ Exam/Fluoride |
Post-Exam | |||||
|---|---|---|---|---|---|---|---|---|
| Pairwise Comparison |
Mean Difference |
p-value | Mean Difference |
p-value | Mean Difference |
p-value | Mean Difference |
p-value |
| Overall | 0.02* | 0.61* | 0.04* | <0.001* | ||||
| Dentist vs Parent |
0.46 | 0.07** | 0.20 | >0.999** | 0.17 | >0.999** | 0.25 | 0.87** |
| Independent Observer vs Parent |
0.52 | 0.04** | 0.26 | >0.999** | 0.78 | 0.04** | 1.38 | <0.001** |
| Independent Observer vs Dentist |
0.06 | >0.999** | 0.06 | >0.999** | 0.61 | 0.17** | 1.14 | <0.001** |
P-value testing overall association between distress rating and observer type calculated using one-way ANOVA
P-value testing the association between distress ratings of two observers calculated using a post-hoc Bonferroni comparison
Fifteen of the 65 videos were re-coded (23%) to determine intra-rater reliability (IRR) of the IO. Pearson correlation for evaluating the IRR was found to be 0.998 when comparing the total distress score for all four phases. When comparing the distress score in the prophylaxis/exam/fluoride phase there was perfect agreement in the IO ratings between the two time periods (Pearson correlation = 1.00).
The majority of children were rated very similarly by their parents and dentists; however there was a subset for which the parent and dentist ratings differed considerably. These cases were examined to determine if they differed systematically from the other children. We defined two groups with significant differences in the prophylaxis/exam/fluoride phase as “mismatches.” One group was the children for whom the parent and dentist ratings that differed by >2 points on the 10 point scale (N = 17). The second was the cases with rating differences greater than 1.5 times the standard deviation from the mean (N = 8). We compared each of these groups with the larger group of children (N = 48 and 57 respectively) and found no statistically significant differences for variables listed in Table 1. (Data not shown)
Discussion
Beginning at age 4-5 years, children can reliably self-report pain.30 Before that age, accurate assessment of pain observed by others may be difficult because estimations rely on physiologic and behavioral responses.25, 26, 38 Pain assessment in this group is complicated further by the fact that children, parents, and providers vary in their assessment of actual pain and discomfort.25, 29, 39, 40 A variety of instruments have been used to report patient fear and distress behavior during dental treatment. A recent systematic review indicates that Likert scales have been used frequently to describe child pain and distress behavior. One of the most common instruments is a simple 5 point Likert scale derived from Weinstein et al, 1982.41 Versloot employed a similar instrument, using a 4 point scale ranging from (1) no pain to (4) a lot of pain.29 The medical literature also commonly features instruments based upon Likert or visual analog scales completed by children, parents, and providers.30, 42-45 Others have described child behavior during dental care with more detailed scales such as the St Andrews Behavioral Interaction Coding Scheme (SABICS), which includes 48 behavioral codes.46, 47
In this study parents and dentists rated pain on a 10 point Likert scale. We chose this scale for real-time ratings performed by parents and dentists because it is reliable and simple to use. The IO rated behavior using the BAADS rating scale. The BAADS was developed as an observational scale of children’s behavioral response to preparation for bone marrow aspiration procedures.48 We selected the BAADS for use in this study because it is a cost-efficient, reliable and valid observational measure of young children’s stress and coping with medical stressors. The BAADS requires expertise in observational ratings of child behavior, which was true of the IO but not true of the dentist or parent participants. Also, it seemed possible that ratings based on video recordings, rather than done “live,” would more accurately reflect the child’s state, independent of any shared experience of the child’s distress.
Providers may underrate discomfort as a result of “pain blindness” that occurs when administering medical care to patients. For example, dentists may not accurately assess pain experienced during dental injection because they are focused on administering anesthetic, not the child’s reaction.28, 29 It is thought that while parents do not perfectly assess their child’s pain, they may are more accurate than a treating clinician.25, 30, 49
If dentists were blind to a child’s distress during preventive care, we would expect them to rate the pre-exam phase similarly to other observers, while rating exam procedures lower. In contrast to findings in the pain literature, the results of the present study suggest that dentists rate child distress during preventive care similarly to parents. Average distress measurements were within the moderate range for all observers, and interestingly, parents provided the lowest mean distress scores at all time points. Perhaps parents identified the distress behavior as typical for their child, while providers and IOs gauged it according to their experience with other children.
For all treatment phases, the IO’s average rating was greater than both dentists and parents. This may be because parents and dentists used context-specific cues to interpret the meaning of the child’s behavior, whereas the IO rated observed behaviors only. For example, maximum distress was coded for any phase that included screaming, strong back arch, or kicking. It is also possible that parents and dentists mentally averaged these short behavioral spikes in their assessment, arriving at a lower overall score. In contrast, for example the parents’ and dentists’ ratings might have been lower for this phase because the dentist (the distressing stimulus) was no longer in contact with the child and both the dentist and the parent knew the dentist would not reinitiate contact. In fact, parents’ comments to their children supported this view; with reassurances such as “It’s okay, all done.”
In this study we determined that parents and dentists often have a similar perception of the distress that a child experiences during preventive care. It may be that for procedures that are not generally thought to be painful there is better agreement between the dentist and parent than for those procedures that are typically considered to be painful (e.g. injections, restorative dentistry, suturing, etc.). We reported previously that a large proportion of children experience moderate to severe distress when receiving pediatric preventive dental care.27 While most children return quickly to baseline after examination, the child’s experience over the course of the visit may leave a more lasting impression on parents. This has important implications for pediatric oral health because parent satisfaction with the dental experience can affect follow-through with routine preventive care. 50 These results suggest that when dentists perceive that young patients are experiencing distress, it is quite likely that the parent feels the same way. We therefore suggest that practitioners attempt to determine which children are at highest risk for distress behavior, and counsel parents appropriately.27
Limitations of this study included the fact that examination procedures were performed by twenty-one separate dental providers at a university-based dental clinic. A recent systematic review showed that sample sizes of 25-30 practitioners of varying experience have been commonly reported in this type of study. While not an uncommon practice, it must be recognized that enrolling a variety of providers may have affected results.41 Parent interactions with providers and individual variation in practitioner style and experience may have affected the children’s responses and parents’ impression of distress experienced by their child. Parents and dentists also rated distress on a scale that was similar but not the same as the IO. The scores were scaled to facilitate comparison, however this may partially explain why dentist and parent distress ratings were more similar for some time points.
Conclusions
The results of this study suggest that:
There was no statistically significant difference between distress scores provided by dentists and parents of children receiving preventive dental care at any exam phase.
On average, parents provided the lowest ratings of child distress for all phases.
The Prophylaxis/Examination/Fluoride treatment phase was judged to be most distressing by parents, dentists and the IO.
Acknowledgments
This research was supported by grant U54DE019346, National Institute of Health, National Center for Dental and Craniofacial Research.
Contributor Information
Travis M. Nelson, Department of Pediatric Dentistry, University of Washington, 6222 NE 74th Street, Seattle, WA 98115, USA.
Colleen E. Huebner, School of Public Health and Adjunct Professor of Pediatric Dentistry, School of Dentistry, University of Washington, Box 357230, Seattle, WA 98195, USA. colleenh@uw.edu.
Amy Kim, Department of Pediatric Dentistry, University of Washington, 6222 NE 74th Street, Seattle, WA 98115, USA. akim3@uw.edu.
JoAnna M. Scott, Department of Pediatric Dentistry, University of Washington, 6222 NE 74th Street, Seattle, WA 98115, USA. elorra@uw.edu.
References
- 1.Hale KJ. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 Pt 1):1113–6. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- 2.Guideline on infant oral health care. Pediatr Dent. 2012;34(5):148–52. [PubMed] [Google Scholar]
- 3.Savage MF, Lee JY, Kotch JB, Vann WF., Jr. Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418–23. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- 4.Nowak AJ, Casamassimo PS, Scott J, Moulton R. Do early dental visits reduce treatment and treatment costs for children? Pediatr Dent. 2014;36(7):489–93. [PubMed] [Google Scholar]
- 5.Kaste LM, Drury TF, Horowitz AM, Beltran E. An evaluation of NHANES III estimates of early childhood caries. J Public Health Dent. 1999;59(3):198–200. doi: 10.1111/j.1752-7325.1999.tb03269.x. [DOI] [PubMed] [Google Scholar]
- 6.Vargas CM, Crall JJ, Schneider DA. Sociodemographic distribution of pediatric dental caries: NHANES III, 1988-1994. J Am Dent Assoc. 1998;129(9):1229–38. doi: 10.14219/jada.archive.1998.0420. [DOI] [PubMed] [Google Scholar]
- 7.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 2007;11(248):1–92. [PubMed] [Google Scholar]
- 8.Badri P, Saltaji H, Flores-Mir C, Amin M. Factors affecting children’s adherence to regular dental attendance: a systematic review. J Am Dent Assoc. 2014;145(8):817–28. doi: 10.14219/jada.2014.49. [DOI] [PubMed] [Google Scholar]
- 9.Alio AP, Salihu HM. Maternal determinants of pediatric preventive care utilization among blacks and whites. J Natl Med Assoc. 2005;97(6):792–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Brickhouse TH, Farrington FH, Best AM, Ellsworth CW. Barriers to dental care for children in Virginia with autism spectrum disorders. J Dent Child (Chic) 2009;76(3):188–93. [PubMed] [Google Scholar]
- 11.Leroy R, Bogaerts K, Hoppenbrouwers K, Martens LC, Declerck D. Dental attendance in preschool children - a prospective study. Int J Paediatr Dent. 2013;23(2):84–93. doi: 10.1111/j.1365-263X.2012.01227.x. [DOI] [PubMed] [Google Scholar]
- 12.Wasserman RC, Inui TS, Barriatua RD, Carter WB, Lippincott P. Pediatric clinicians’ support for parents makes a difference: an outcome-based analysis of clinician-parent interaction. Pediatrics. 1984;74(6):1047–53. [PubMed] [Google Scholar]
- 13.Bitar King B, Huebner C, Slayton R, Leggott P. Barriers to obtaining needed dental treatment for Head Start children in Washington. University of Washington; 2011. unpublished data. [Google Scholar]
- 14.Song B, Pickrell J. Research Day Presentation. University of Washington; Seattle, WA: Sep, 2010. Managing Children’s Dental Fear: Current Practices in a Latino Population. [Google Scholar]
- 15.Schor EL. The influence of families on child health. Family behaviors and child outcomes. Pediatr Clin North Am. 1995;42(1):89–102. doi: 10.1016/s0031-3955(16)38910-6. [DOI] [PubMed] [Google Scholar]
- 16.Kataoka-Yahiro MR, Munet-Vilaro F. Barriers to preventive health care for young children. J Am Acad Nurse Pract. 2002;14(2):66–72. doi: 10.1111/j.1745-7599.2002.tb00093.x. [DOI] [PubMed] [Google Scholar]
- 17.Amin MS. Utilization of dental services by children in low-income families in Alberta. J Can Dent Assoc. 2011;77:b57. [PubMed] [Google Scholar]
- 18.Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children’s oral health. J Am Dent Assoc. 2005;136(3):364–72. doi: 10.14219/jada.archive.2005.0179. quiz 81. [DOI] [PubMed] [Google Scholar]
- 19.Goettems ML, Ardenghi TM, Demarco FF, Romano AR, Torriani DD. Children’s use of dental services: influence of maternal dental anxiety, attendance pattern, and perception of children’s quality of life. Community Dent Oral Epidemiol. 2012;40(5):451–8. doi: 10.1111/j.1600-0528.2012.00694.x. [DOI] [PubMed] [Google Scholar]
- 20.International Association for the Study of Pain Task Force on Taxonomy. Announcement: modification of pain definition. IASP Newsletter. 2001;2:2. [Google Scholar]
- 21.Coleman MM, Solarin K, Smith C. Assessment and management of pain and distress in the neonate. Adv Neonatal Care. 2002;2(3):123–36. doi: 10.1053/adnc.2002.32040. quiz 37-9. [DOI] [PubMed] [Google Scholar]
- 22.Friedland LR, Pancioli AM, Duncan KM. Pediatric emergency department analgesic practice. Pediatr Emerg Care. 1997;13(2):103–6. doi: 10.1097/00006565-199704000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Schechter NL, Allen DA, Hanson K. Status of pediatric pain control: a comparison of hospital analgesic usage in children and adults. Pediatrics. 1986;77(1):11–5. [PubMed] [Google Scholar]
- 24.Beyer JE, Wells N. The assessment of pain in children. Pediatr Clin North Am. 1989;36(4):837–54. doi: 10.1016/s0031-3955(16)36724-4. [DOI] [PubMed] [Google Scholar]
- 25.Xavier Balda R, Guinsburg R, de Almeida MF, et al. The recognition of facial expression of pain in full-term newborns by parents and health professionals. Arch Pediatr Adolesc Med. 2000;154(10):1009–16. doi: 10.1001/archpedi.154.10.1009. [DOI] [PubMed] [Google Scholar]
- 26.Pillai Riddell RR, Craig KD. Judgments of infant pain: the impact of caregiver identity and infant age. J Pediatr Psychol. 2007;32(5):501–11. doi: 10.1093/jpepsy/jsl049. [DOI] [PubMed] [Google Scholar]
- 27.Nelson TM, Huebner CE, Kim A, Scott JM, Pickrell JE. Parent-reported distress in children under 3 years old during preventive medical and dental care. Eur Arch Paediatr Dent. 2015 Jun;16(3):283–90. doi: 10.1007/s40368-014-0161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murtomaa H, Milgrom P, Weinstein P, Vuopio T. Dentists’ perceptions and management of pain experienced by children during treatment: a survey of groups of dentists in the USA and Finland. Int J Paediatr Dent. 1996;6(1):25–30. doi: 10.1111/j.1365-263x.1996.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 29.Versloot J, Veerkamp JS, Hoogstraten J. Assessment of pain by the child, dentist, and independent observers. Pediatr Dent. 2004;26(5):445–9. [PubMed] [Google Scholar]
- 30.Singer AJ, Gulla J, Thode HC., Jr. Parents and practitioners are poor judges of young children’s pain severity. Acad Emerg Med. 2002;9(6):609–12. doi: 10.1111/j.1553-2712.2002.tb02298.x. [DOI] [PubMed] [Google Scholar]
- 31.Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- 32.Fiks AG, Jimenez ME. The promise of shared decision-making in paediatrics. Acta Paediatr. 2010;99(10):1464–6. doi: 10.1111/j.1651-2227.2010.01978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen LL. Reducing infant immunization distress through distraction. Health Psychol. 2002;21(2):207–11. [PubMed] [Google Scholar]
- 34.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 35.von Baeyer CL, Spagrud LJ. Systematic review of observational (behavioral) measures of pain for children and adolescents aged 3 to 18 years. Pain. 2007;127(1-2):140–50. doi: 10.1016/j.pain.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 36.Cohen LL, Lemanek K, Blount RL, et al. Evidence-based assessment of pediatric pain. J Pediatr Psychol. 2008;33(9):939–55. doi: 10.1093/jpepsy/jsm103. discussion 56-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blount RL, Loiselle KA. Behavioural assessment of pediatric pain. Pain Res Manag. 2009;14(1):47–52. doi: 10.1155/2009/348184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho K, Spence J, Murphy MF. Review of pain-measurement tools. Ann Emerg Med. 1996;27(4):427–32. doi: 10.1016/s0196-0644(96)70223-8. [DOI] [PubMed] [Google Scholar]
- 39.Dahlquist LM, Power TG, Carlson L. Physician and parent behavior during invasive pediatric cancer procedures: relationships to child behavioral distress. J Pediatr Psychol. 1995;20(4):477–90. doi: 10.1093/jpepsy/20.4.477. [DOI] [PubMed] [Google Scholar]
- 40.Mahoney L, Ayers S, Seddon P. The association between parent’s and healthcare professional’s behavior and children’s coping and distress during venepuncture. J Pediatr Psychol. 2010;35(9):985–95. doi: 10.1093/jpepsy/jsq009. [DOI] [PubMed] [Google Scholar]
- 41.Zhou Y, Cameron E, Forbes G, Humphris G. Systematic review of the effect of dental staff behaviour on child dental patient anxiety and behaviour. Patient Educ Couns. 2011;85(1):4–13. doi: 10.1016/j.pec.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 42.McMurtry CM, Chambers CT, McGrath PJ, Asp E. When “don’t worry” communicates fear: Children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain. 2010;150(1):52–8. doi: 10.1016/j.pain.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 43.McMurtry CM, McGrath PJ, Asp E, Chambers CT. Parental reassurance and pediatric procedural pain: a linguistic description. J Pain. 2007;8(2):95–101. doi: 10.1016/j.jpain.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 44.Felber M, Schabmann A, Inschlag N, et al. Effects of parental soothing behavior on stress levels of 2-8 year old children during voiding cystourethrograms by phase of procedure. J Clin Psychol Med Settings. 2011;18(4):400–9. doi: 10.1007/s10880-011-9260-5. [DOI] [PubMed] [Google Scholar]
- 45.Blount RL, Devine KA, Cheng PS, Simons LE, Hayutin L. The impact of adult behaviors and vocalizations on infant distress during immunizations. J Pediatr Psychol. 2008;33(10):1163–74. doi: 10.1093/jpepsy/jsn030. [DOI] [PubMed] [Google Scholar]
- 46.Zhou Y, Forbes GM, Humphris GM. The behaviour of preschool children receiving fluoride varnish application in a community setting. Br Dent J. 2013;215(7):E11. doi: 10.1038/sj.bdj.2013.990. [DOI] [PubMed] [Google Scholar]
- 47.Zhou Y, Humphris GM. Reassurance and Distress Behavior in Preschool Children Undergoing Dental Preventive Care Procedures in a Community Setting: a Multilevel Observational Study. Ann Behav Med. 2013 doi: 10.1007/s12160-013-9566-7. 10.1007/s12160-013-9566-7. [DOI] [PubMed] [Google Scholar]
- 48.Bachanas PJ, Blount RL. The Behavioral Approach-Avoidance and Distress Scale: an investigation of reliability and validity during painful medical procedures. J Pediatr Psychol. 1996;21(5):671–81. doi: 10.1093/jpepsy/21.5.671. [DOI] [PubMed] [Google Scholar]
- 49.Rajasagaram U, Taylor DM, Braitberg G, Pearsell JP, Capp BA. Paediatric pain assessment: differences between triage nurse, child and parent. J Paediatr Child Health. 2009;45(4):199–203. doi: 10.1111/j.1440-1754.2008.01454.x. [DOI] [PubMed] [Google Scholar]
- 50.Grembowski D, Milgrom PM. Increasing access to dental care for medicaid preschool children: the Access to Baby and Child Dentistry (ABCD) program. Public Health Rep. 2000;115(5):448–59. doi: 10.1093/phr/115.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]