Abstract
We describe the neuroimaging findings of an 11-year-old boy who presented with mild occipital headache and precocious puberty. This child was found to have a combination of various midline anomalies including a Chiari type 1 malformation, corpus callosum agenesis and patent craniopharyngeal canal with adjacent intracranial dermoid cyst.
Keywords: Chiari type 1 malformation, corpus callosum agenesis, craniopharyngeal canal, magnetic resonance imaging, children, brain
Introduction
Although several incidental or presumed associated cerebral malformations have been described in Chiari type 1 malformations, they are more commonly seen in Chiari type 2 or 3 malformations.1 Corpus callosum anomalies are occasionally described in Chiari type 1 malformation.2 There are, however, no reports on a combined presence of a patent craniopharyngeal canal. The simultaneous occurrence of a patent craniopharyngeal canal could possibly give valuable clues about the timing and etiology of the Chiari type 1 malformation, which is still not fully understood.1
Case report
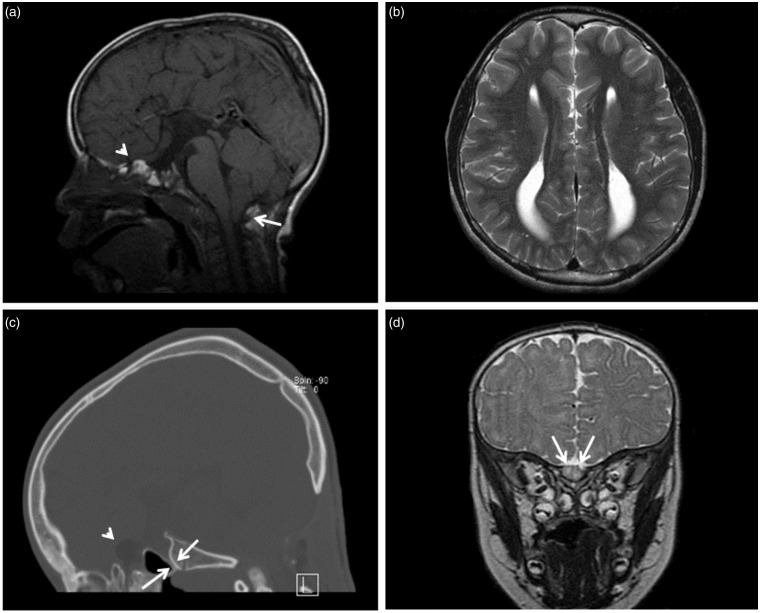
We present the clinical and neuroimaging findings of an 11-year-old boy who was diagnosed with a Chiari type 1 malformation in his first year of life and had undergone two posterior fossa decompressions because of cervical syringomyelia. The child presented with occipital headache and precocious puberty. In addition to the classical stigmata of a Chiari type 1 malformation, the neuroimaging studies showed several additional midline malformations including (1) a classical corpus callosum agenesis with the typical trident-shaped frontal horns on coronal imaging, parallel lateral ventricles on axial imaging and colpocephaly, (2) a dysplasia of the anterior skull base with a small patent craniopharyngeal canal without meningocele formation, and (3) a focal mass lesion just anterior/superior to the craniopharyngeal canal that was identified with signal characteristics consistent with a dermoid cyst and remained stable for several years of neuroimaging (Figure 1).
Figure 1.
(a) Sagittal T1-weighted MR image shows tonsillar herniation more than 5 mm below the foramen magnum, consistent with Chiari type 1 malformation (white arrow). A dermoid cyst is noted at the anterior skull base as a focal mass with high T1-signal (white arrowhead). There is complete agenesis of the corpus callosum. (b) Axial T2-weighted MR image shows findings consistent with agenesis of the corpus callosum including parallel lateral ventricles and colpocephaly. (c) Sagittal CT image in bone algorithm shows a persistent craniopharyngeal canal (white arrows). The fat signal of the dermoid cyst can also be noted (white arrowhead). (d) Coronal T2-weighted MR image confirms the dermoid cyst at the anterior skull base with heterogeneous intermediate signal intensity.
MR: magnetic resonance; CT: computed tomography.
Discussion
Chiari type 1 malformation is defined as cerebellar tonsillar ectopia or herniation through the foramen magnum (≥5 mm). The precise mechanism/etiology causing this herniation is not yet fully understood, but the general hypothesis is that the condition is mainly due to ‘overcrowding’ of the posterior fossa due to underdevelopment of the occipital bone.1,3,4 Chiari type 1 malformation can be accompanied by other cranial, cerebral and spinal anomalies. The most common include syringomyelia (30%–70%) and hydrocephalus (about 10%).1,2,5 Dysgenesis of the corpus callosum is not commonly associated with Chiari type 1 malformation, but has occasionally been described in the literature.2
According to recent insight the formation of the corpus callosum starts around the 13th gestational week. The corpus callosum is initially small and short, but anatomically complete by the 14th gestational week, with a progressively dorsal expansion reaching into the 20th week.6–8 Agenesis of the corpus callosum can be an isolated finding, but in the majority of cases a corpus callosum agenesis is associated with other malformations within a broad spectrum of congenital syndromes.7 Furthermore the corpus callosum can be injured/disrupted as early as during the fetal life with resultant thinning or focal defects, which makes corpus callosum abnormalities in general a heterogeneous disorder.7,8
A patent craniopharyngeal canal is believed to result from a defect in the fusion of the Rathke pouch.9,10 In the embryologic development of the hypophysis, the adenohypophysis migrates through a canal (Rathke pouch) extending from the nasopharynx to the floor of the sella turcica. Normally, this canal is obliterated by the cartilaginous sphenoid skull base development. Defective fusion results in a residual canal, called the craniopharyngeal canal.9,10 Ossification progresses in an orderly pattern but not strictly according to age. Progressive and finally complete ossification/closure of the canal occurs between the 13th and 24th gestational weeks.10 Small incidental canals are found to be benign in most cases, but especially the larger craniopharyngeal canals may be associated with other craniofacial abnormalities such as holoprosencephaly, cleft lip and palate, orbital hypoplasia and agenesis of the corpus callosum.9,11,12 Although there are several disagreements regarding the development of the pituitary gland and the timing of the closure of the craniopharyngeal canal, the combined presence with the corpus callosum agenesis could suggest an embryological event around the 13th–14th week of gestation in this case.13
Sener described the association of Chiari type 1, callosal dysgenesis and ectopic neurohypophysis.14 Several authors described the association between (1) corpus callosum agenesis and Chiari type 1 malformation, or (2) corpus callosum agenesis and the craniopharyngeal canal. To our knowledge, the combined presence of Chiari type 1 malformation, craniopharyngeal canal and agenesis of the corpus callosum has not yet been documented in the literature. We cannot differentiate between a rare, causative association of midline brain anomalies or a chance event with unrelated midline anomalies. The simultaneous occurrence of several findings that are all located within the midline of the skull and brain suggests, however, a causative link between these findings. Consequently, we conclude that radiologists should pay special attention to the skull base in children who present with various combinations of Chiari type 1 malformations and corpus callosum agenesis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Poretti A, Boltshauser E, Huisman TA. Chiari malformations and syringohydromyelia in children. Semin Ultrasound CT MRI 2016; 37: 129–142. [DOI] [PubMed] [Google Scholar]
- 2.Galarza M, Martínez-Lage JF, Ham S, et al. Cerebral anomalies and Chiari type 1 malformation. Pediatr Neurosurg 2010; 46: 442–449. [DOI] [PubMed] [Google Scholar]
- 3.Milhorat TH, Chou MW, Trinidad EM, et al. Chiari I malformation redefined: Clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 1999; 44: 1005–1017. [DOI] [PubMed] [Google Scholar]
- 4.Nishikawa M, Sakamoto H, Hakuba A, et al. Pathogenesis of Chiari malformation: A morphometric study of the posterior fossa. J Neurosurg 1997; 86: 40–47. [DOI] [PubMed] [Google Scholar]
- 5.Loukas M, Shayota BJ, Oelhafen K, et al. Associated disorders of Chiari I malformations: A review. Neurosurg Focus 2011; 31: E3. [DOI] [PubMed] [Google Scholar]
- 6.Rakic P, Yakovlev PI. Development of the corpus callosum and cavum septi in man. J Comp Neurol 1968; 132: 45–72. [DOI] [PubMed] [Google Scholar]
- 7.Edwards TJ, Sherr EH, Barkovich AJ, et al. Clinical, genetic and imaging findings identify new causes for corpus callosum development syndromes. Brain 2014; 137: 1579–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raybaud C. The corpus callosum, the other great forebrain commissures, and the septum pellucidum: Anatomy, development, and malformation. Neuroradiology 2010; 52: 447–477. [DOI] [PubMed] [Google Scholar]
- 9.Abele TA, Salzman KL, Harnsberger HR, et al. Craniopharyngeal canal and its spectrum of pathology. AJNR Am J Neuroradiol 2014; 35: 772–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nemzek WR, Brodie HA, Hecht ST, et al. MR, CT, and plain film imaging of the developing skull base in fetal specimens. AJNR Am J Neuroradiol 2000; 21: 1699–1706. [PMC free article] [PubMed] [Google Scholar]
- 11.Kjaer I, Fischer-Hansen B. Human fetal pituitary gland and holoprosencephaly and anencephaly. J Craniofac Genet Dev Biol 1995; 15: 222–229. [PubMed] [Google Scholar]
- 12.Currarino G, Maravilla KR, Salyer KE. Transsphenoidal canal (large craniopharyngeal canal) and its pathologic implications. AJNR Am J Neuroradiol 1985; 6: 39–43. [PMC free article] [PubMed] [Google Scholar]
- 13.Mehemed TM, Fushimi Y, Okada T, et al. MR imaging of the pituitary gland and postsphenoid ossification in fetal specimens. AJNR Am J Neuroradiol. Epub ahead of print 28 April 2016. DOI: 10.3174/ajnr.A4808. [DOI] [PMC free article] [PubMed]
- 14.Sener RN. Chiari I malformation associated with callosal dysgenesis and ectopic neurohypophysis. Comput Med Imaging Graph 1995; 19: 487–489. [DOI] [PubMed] [Google Scholar]