Abstract
Although the occurrence of sudden cardiac death (SCD) in a young person is a rare event, it is traumatic and often widely publicized. In recent years, SCD in this population has been increasingly seen as a public health and safety issue. This review presents current knowledge relevant to the epidemiology of SCD and to strategies for prevention, resuscitation and identification of those at greatest risk. Areas of active research and controversy include the development of best practices in screening, risk stratification approaches and post-mortem evaluation, and identification of modifiable barriers to providing better outcomes after resuscitation of young SCD victims. Institution of a national registry of SCD in the young will provide data that will help to answer these questions.
Introduction
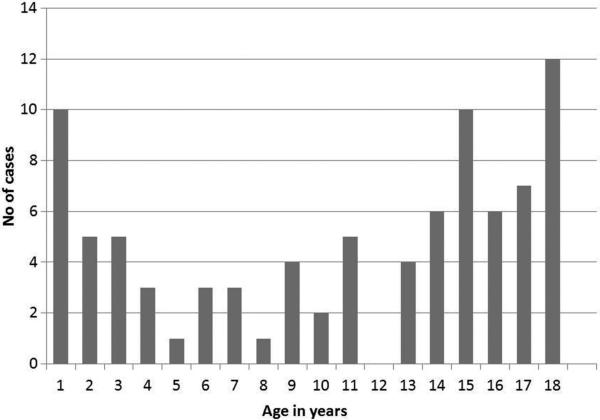
Few medical events are more traumatic than the sudden, unanticipated death of a young person. Sudden cardiac death (SCD) is statistically uncommon in the young, but its dramatic presentation and cascading effects in the family and community make it a newsworthy event. Widely publicized cases of SCD in athletes personify the metaphor of hidden vulnerability lurking in the body of a vigorous, healthy young person. There is a high degree of concern regarding the risk of SCD in children and teenagers amongst the lay public, in comparison to other much more prevalent deadly risks of childhood, such as accident, injury, suicide, and violence (Figure 1). Nonetheless, it is fair to consider SCD in the young as a public health issue, and to develop strategies based on evidence and expert consensus to mitigate it.
Figure 1.
Causes of death in American children
This review will examine the current state of knowledge and practice regarding SCD in the young. This will include the pathophysiology of SCD, the disease processes which predispose to it – especially among asymptomatic youth – and strategies for resuscitation and identification of those at risk. Because many major etiologies of SCD in the young are congenital and/or genetic, the sudden death of a young person must often be studied within the context of the family. Advances in cardiovascular genetics have added both molecular insight and new levels of complexity and ambiguity to our understanding of affected families. Both pre-mortem and post-mortem genetic testing now promise disease specific risk assessment and therapy for the surviving relatives of the SCD victim. Finally, SCD in the young is an event that affects the community. These events demand public health policy responses to provide rational and effective strategies to protect our youth against rare but dramatic events. Such strategies might include programs of cardiovascular screening, innovations in deployment of public access defibrillation, the development of standards for post-mortem investigation of SCD, and the institution of regional and national registries of SCD in the young.
Given such broad scope, this review will be limited in depth in general and particularly with respect to the various SCD-predisposing cardiac etiologies (including congenital heart disease). An exception to this will occur in the sections on the science, epidemiology and outcomes of resuscitation. These will focus on the phenomena around out-of-hospital cardiac arrest, and will be drawn from and more widely applicable to the larger topic of pediatric sudden death in the community. Conversely, the basic knowledge of cardiac etiologies associated with SCD in the young is widely available and will be reviewed succinctly. Pathophysiology and prevention of Sudden Infant Death Syndrome, (SIDS), defined as an infant death unexplained after a thorough case investigation,1 is also outside the scope of this review, although it includes some deaths attributable to cardiac causes such as channelopathies.2 Finally, it is not the intention of this review to repeat or summarize expert consensus recommendations relevant to this broad topic that have been published in several recently published guideline documents. These guideline statements include cardiopulmonary resuscitation,3-6 ICD implantation,7 evaluation and management of cardiomyopathies8, 9 and channelopathies,10, 11 stimulant medication use,12, 13 screening14, 15 and sports eligibility.10, 16-19
1. Epidemiology and etiologies of SCD in the young
Epidemiology
SCD is uncommon in children, and in general it requires carefully designed, regional and/or multi-center studies to generate accurate statistics regarding incidence and risk factors. Table 1 presents the incidence of SCD in a variety of younger populations and settings. This highlights the variation inherent in these estimates, and also clearly indicates that the rate of SCD in children is 1 to 2 orders of magnitude less than that seen in the adult population, with incidence ranging from <1 – 10 deaths/100,000 population/year (with exclusion of infants and persons >18 years of age, <1 – 4 deaths/100,000 population/year). The burden of SCD in terms of lost life-years is disproportionately larger for children, due to their greater life expectancy. These statistics are necessary to formulate useful public health policy for early detection, prevention and delivery of therapies. Relevant factors include age, gender, the presence of comorbid disease, geographic region, and participation in athletic activity.
Table 1.
Population based estimates of SCD incidence in the young
| Study | Patient group | Age range (yrs) | SCD incidence (per 100,000 patient years) | Comments |
|---|---|---|---|---|
| Molander et al22 | All unexpected deaths, southern Sweden | 1 - 20 yrs | 0.7 | Approximately 15% SCD |
| Driscoll et al23 | Death certificate survey, Olmsted Co.,Minnesota | 1 - 22 yrs | 1.3 | >50% sudden death cardiac related |
| Gerein et al24 | Cardiopulmonary arrest victims, Ontario, Canada | <17 yrs | 1.5 (9.1 all arrests) | 16% deemed attributable to cardiac causes |
| Puranik et al25 | Forensic office review of sudden death, Eastern Sydney, Australia | 5 - 35 yrs | 1.0 | 29% autopsy negative |
| Chugh et al26 | Sudden death survey, Multnomah Co., Oregon | 1 - 17 yrs | 1.7 | Same study included infants, accounting for 76% of all events |
| Park et al27 | Out-of-hospital cardiac arrest, Korea | <19 yrs | 4.2 | Includes ~25% infants ~30% deemed cardiac |
| Papadakis et al28 | Sudden deaths, England & Wales | 1 - 34 yrs | 1.8 | 14% classified as SCD |
| Hendrix et al29 | Death certificate survey, 12 Dutch provinces | 1 - 40 yrs | 1.6 | Increased rate in patients >30 yrs |
| Winkel et al30 | Sudden deaths, Denmark | 1 - 35 yrs | 1.9 - 2.8 | Dependent on assignment of non-autopsy cases |
| Margey et al31 | Sudden death statistics, Republic of Ireland | 15 - 35 yrs | 2.9 | Sudden unexplained death 27%, hypertrophic cardiomyopathy 15% |
| Wren et al32 | All deaths, one English health region | 1 - 20 yrs | 2.5 | Half of SCD associate with prior known diagnosis |
| Winkel et al33 | All deaths, Denmark | 1 - 18 yrs | 1.5 | No prior medical history in 2/3 of cases |
| Bardai et al34 | Out-of-hospital, province in the Netherlands | <21 yrs | 3.2 (9.0 all arrests) | 39% cardiac etiology |
| Meyer et al35 | Out-of-hospital, King Co., Washington | <35 yrs | 2.3 | In patients >25 yrs, coronary artery disease primary cause |
| Atkins et al36 | Out-of-hospital, multiple US districts | 1-11 yrs | 3.73 | Resuscitation Outcomes Consortium |
| Atkins et al36 | Out-of-hospital, multiple US districts | 12-18 yrs | 6.4 | Resuscitation Outcomes Consortium |
| Kitamura et al37 | Out-of-hospital, Japan | <12 yrs | 2.4 (female) 3.3 (male) | Nationwide registry of OHCA |
| Daya et al38 | Out-of-hospital, USA | <18 yrs | 10.1 | Includes infant sudden death |
Population-based studies with a large, well defined denominator are the gold standard for determining SCD incidence. Because SCD is infrequent in the young, such studies must survey national or regional populations over a extended periods. Most have been based on retrospective analyses of administrative databases, utilization of EMS databases, or ad hoc means such as internet searches or news media review.20 This introduces ascertainment uncertainty, with respect to both over- and under-diagnosis. A prospective, analysis of SCD in patients of all ages suggested that ascertainment based on death certificates tended to overestimate SCD events.21 Case series of SCD allow excellent ascertainment of affected cases, and are useful for defining etiology and mechanisms. They also provide an estimate of the absolute magnitude of the problem, but cannot reliably quantify the denominator population.
Recently, voluntary prospective registries have been developed to monitor the occurrence of SCD in the young over an extended period in stable populations. This approach addresses some of the specific weaknesses of prior techniques, by utilizing a prospective and problem-specific approach to ensure relative accuracy and completeness of data available for review. A national registry is in development by the National Institutes of Health in conjunction with the Centers for Disease Control for sudden unexpected deaths in a young population in a number of regions, an effort likely to be broadened in the future.39 Much of our current knowledge has been generated from local data collection or research registries which are inclusive of all ages and causes.37, 40-42
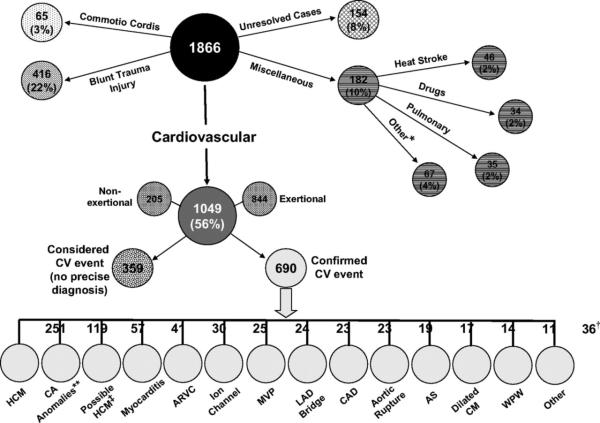
Important demographic characteristics relevant to the occurrence of SCD in young populations can be derived from available data. First, the prevalence of sudden unexpected death in general and SCD in particular is age dependent. After an initial period of higher risk of unexpected death in early infancy (due largely to non-cardiac causes and SIDS), the prevalence of SCD falls in early childhood and begins to rise again in adolescence. An example of this from one large national study identifying 114 cases of SCD in children ages 1 – 18 comprising nearly 8 million patient-years of observation is presented (Figure 2). Similar findings have been observed in an comprehensive surveys from Ontario and 10 North American sites comprising the Resuscitation Outcomes Consortium.36, 43
Figure 2.
Age distribution of SCD in the Danish population, 2000 – 200633 (used with permission)
These studies also confirm that SCD is significantly more prevalent in young males, by a factor of approximately 2:1.33, 35, 43 Less clear is whether ethnicity is associated with increased overall risk or differing patterns of age and gender dependence of SCD in the young. African-American newborns and infants have an elevated risk of post-neonatal mortality associated with a variety of non-cardiac causes, including SIDS,44 and race is also appears to be a risk factor in SCD in adults45 and in NCAA athletes.46, 47 However, etiologies underlying SCD in these other age groups are different from those responsible for SCD in youth. It may thus be incorrect to infer similar ethnic disparities until further population based research is performed.
SCD associated with identifiable cardiovascular disorders
Case series methodology has been used effectively to classify cardiovascular diseases that underlie SCD in the young. Knowledge of the relative prevalence of the underlying diseases also allows for estimation of the relative risks of cardiac arrest. General etiologic categories include heritable and acquired cardiomyopathies and arrhythmia syndromes, (channelopathies), structural congenital heart diseases, myocarditis, and coronary abnormalities. In any given patient, these underlying diagnoses may be known, or they may be undiagnosed and pre-symptomatic. The proportion of detected versus undetected risk of SCD varies by diagnosis, as does our ability to mitigate risk of cardiac arrest by prophylactic therapy and other preventative measures. These two factors strongly affect the utility of diagnostic screening in asymptomatic individuals, a topic which will later be discussed at greater length in this paper.
Heritable and acquired cardiomyopathies and channelopathies
The heritable cardiomyopathies including hypertrophic cardiomyopathy (HCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), dilated cardiomyopathy, and left ventricular non-compaction cardiomyopathy and the heritable channelopathies including long QT syndrome (LQTS), short QT syndrome, Brugada syndrome (BrS), and catecholaminergic polymorphic ventricular tachycardia are potentially lethal but highly treatable genetic heart diseases. The estimated incidence for each of these entities varies, but is thought for the more common diagnoses to be about 1:500 persons for HCM48 and about 1:2000 persons for LQTS.49
Structural congenital heart disease (CHD)
In the United States, ~40,000 children are born annually with CHD. The presence of ventricular dysfunction in combination with scarring, hypertrophy and fibrosis increases the likelihood of SCD in many patients with severe and, to a lesser degree, mild forms of CHD.50 Patients with CHD have an elevated risk of SCD compared to the general population, particularly as they age into early adulthood, and SCD accounts for 15 – 25% of deaths in these patients.51, 52
The diversity of CHD makes it a difficult to construct an aggregated risk estimate, but overall the incidence of SCD in CHD patients appears much lower than that observed in acquired heart diseases such as dilated or ischemic cardiomyopathy. Patients with tetralogy of Fallot, a form of CHD which is well-studied due to its relative prevalence and the availability of long follow-up after surgical palliation, have SCD rates that average 0.1 - 0.2% / year,53-57 although there are other lesions and subgroups of patients likely to be at considerably higher risk for SCD (see below). It is likely that ventricular tachycardia, atrial arrhythmia, and heart block with paroxysmal bradycardia all may contribute to some degree, and the prevalence of each of all arrhythmia subtypes increases with age (Figure 3).
Figure 3.
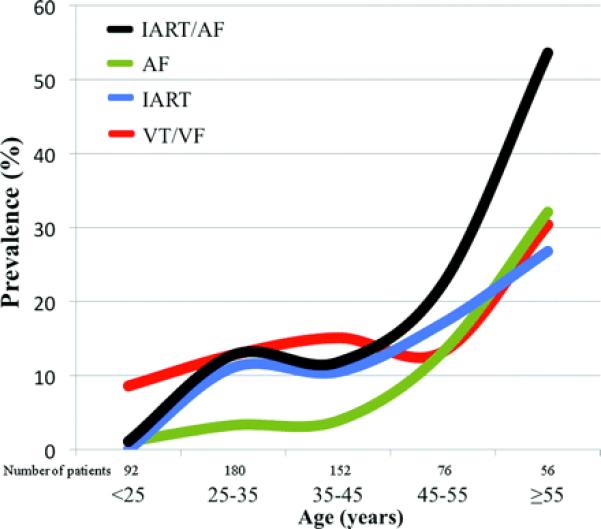
Prevalence of different arrhythmia types as a function of age in patients with tetralogy of Fallot.58 (Used with permission)
SCD in athletes
Athletes are an important subpopulation of young individuals who have a high public profile, and they have been studied carefully with respect to the incidence of SCD. In the United States, youth participation in sports is prevalent, with more than 40,000,000 participants and 7.5 – 8 million teenagers enrolled in organized high school sports.59 Occurrence of SCD in young athletes receives media attention, and it is often assumed that sports participation was a direct cause of SCD. Estimates of SCD in athletes varies by more than 100-fold, ranging from 1:3,000/yr in NCAA Division 1 male basketball athletes47 to 1:917,000/yr among high school athletes in Minnesota.60 Studies of college athletes have suggested that they have an annual incidence between 1:43,000 to 1:67,000. 46, 61 This risk is two to three times greater than that cited above for the general population, but this difference may in part be related to demographic factors correlated with sports participation (gender, age, ethnicity).47
Etiologies of SCD in the young athlete
An early paper investigating the etiology of SCD in the young athlete was a case series published from Italy identifying ARVC in 22 young athletes suffering SCD.62 A more extensive autopsy study of young adult athletes from this region showed that ARVC and coronary artery disease accounted for more than half of the nearly 200 cases studied who had identifiable heart disease, with valvular heart disease, nonatherosclerotic coronary artery malformations, myocarditis and abnormalities of the conduction system accounting for most of the rest.63
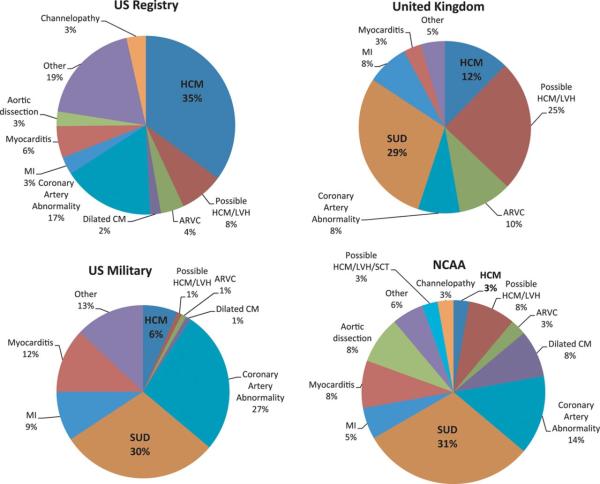
Case studies of SCD in the athlete performed in the United States suggested a more prominent role for HCM as the principal pathology underlying this event.64, 65 A registry of 1,866 episodes of SCD in athletes maintained over more than 25 years revealed that 1,049 were due to cardiovascular causes. Of these, the majority could be assigned a specific diagnosis. In this study, HCM and congenital abnormalities of the coronary arteries were most frequently identified (Figure 4),66 but other series have identified autopsy negative sudden death as the most frequent finding.67
Figure 4.
Distribution of causes of death among young US athletes.66 (Used with permission)
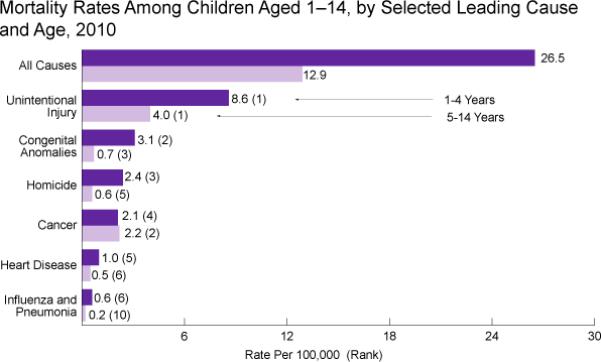
Noncardiac causes of sudden death are also frequent in athletes, including heat stroke and traumatic injury. A recent review of all deaths occurring in college athletes in the US (both on and off the field) revealed the most common cause of death to be accidental (typically motor vehicle), accounting for 50% of all deaths, with non-cardiac medical causes such as homicide, suicide, cancer and drug and alcohol overdose accounting for another 26%.68 An important feature of all studies investigating the etiology of SCD in young athletes is the variability in the findings obtained by different investigators, which likely reflects a mix of ascertainment bias, regional variation in forensic practice and some element of true clinical variation among populations living in different regions of the world (Figure 5).28, 69-73
Figure 5.
Comparison of four studies of SCD etiology.71 (Used with permission)
The significant role of sport in society has generated interest in prophylactic identification of individuals at risk, institution of policies intended to protect those individuals, and investment of community resources to respond promptly to cardiac arrests occurring at athletic events. Comprehensive recommendations have been put forward in several revisions by American and European professional societies (the “Bethesda Guidelines” and the European Society of Cardiology Consensus Recommendations).74, 75 These documents are based on review of available current and historical data, but differ in certain respects and have resulted in a wide variety of public mandated and voluntary policies for cardiovascular screening of athletes and recommendations regarding competitive eligibility. New guidelines addressing these issues were released in late 2015.10 These largely reiterate the recommendations from a decade ago, although a significant change has occurred with respect to the cardiac channelopathies. In contrast to the prior stance which resulted in de facto disqualification most sports, it is now acknowledged that there may be shared decision making and respect for patient/family autonomy and well informed decisions to compete. This is also consistent with 2013 guidelines for management of LQTS which identify as a class I recommendation that athletes with LQTS who desired to compete should see an expert.11
Recent reports highlight difficulties in application of these guidelines to individuals designated at increased risk for SCD and therefore proscribed from certain athletic activities. Anecdotal evidence exists that many patients with increased risk of SCD compete in both recreational and competitive sports which are formally proscribed by these guidelines. High profile legal cases have been tried regarding the right of athletes to compete despite disqualification due to medical diagnosis.76 Prospective review is now underway regarding the consequences of allowing patients with ICDs and diseases like LQTS, HCM and ARVC to participate in competitive activities currently proscribed by guidelines.77, 78 NIH-funded prospective studies (Lifestyle and Exercise in Patients with HCM or LIVE-HCM and Lifestyle and Exercise in Patients with LQTS or LIVE-LQTS) began patient enrollment in early 2015 (NIH Clinical Trial NCT02549664). The goal is to test the hypothesis that those patients with LQTS or HCM who are the most active will have a higher quality of life compared to those who are least active without making their disease substrate more arrhythmic.
It is unclear whether sports participation is a modifiable risk factor for SCD. Adrenergic stimulation associated with athletic activity may plausibly act as a proximate cause for cardiac events in patients with HCM,79 LQTS,80 ARVC,81 anatomical abnormalities of the coronary artery.82 The epidemiology of SCD in young people indirectly suggests that active participation in sports itself is a cause of SCD.83 However, noncompetitive athletes with similar conditions appear to be at similar risk,84 and SCD is as likely to occur during periods of recreational play (which may be as vigorous as competitive activity in young patients),85, 86 as well as in quiet time and sleep.87 Historical epidemiological studies are inconclusive: an Italian study identified an beneficial effect of national policy mandating cardiovascular screening of athletes in reducing SCD,88 while studies from Israel, Denmark, and the United States have failed to support that finding.69, 89, 90 No well-designed studies have demonstrated that sports proscription reduces incidence of SCD. This raises the question as to whether athletes are “singled out” for cardiovascular scrutiny and intervention, while possibly having neither higher risk of SCD nor a clearly effective intervention.
SCD associated with chest trauma
SCD is also rarely associated in the normal juvenile heart with blunt chest trauma, a condition referred to as commotio cordis. The frequency of this event is difficult to determine, but studies of SCD at intercollegiate NCAA events indicate that autopsy negative SCD is a relatively frequent finding,71 and some can clearly be related as trauma-related by history.91 Animal studies have identified a putative mechanism of commotio cordis, related to serendipitously timed precordial chest trauma that affects the ventricle during a vulnerable repolarization interval.92 Certain sports are more likely to experience these events, both in competitive and in recreational settings (baseball and cricket, lacrosse, soccer, hockey football, and martial arts).91, 93, 94
SCD associated with use of medications
In contrast to the debate surrounding the management of SCD risk in athletes, concerns regarding the effects of stimulant medications on SCD risk in the young have largely been settled by recent-population based studies. In 2003, 2.5 million children in the US were treated with stimulant medications for attention deficit and hyperactivity disorder (ADHD) and similar disorders of school and social function.95 Many of these medicines have sympathomimetic effects of small but measurable degree. 96, 97 An apparent cluster of SCD events in patients receiving stimulants for ADHD led to the suspension of one such drug (a methylphenidate preparation) in Canada, release of a public health advisory, and a so-called “black box” warning regarding the use of stimulant drugs by the FDA, and recommendation for pretreatment electrocardiographic evaluation prior to starting therapy.12 Subsequently, however, several epidemiological studies conducted using large administrative databases clearly show that such medications have no effect, and possibly even a negative, “healthy-user” effect of these medications on SCD prevalence.98, 99
Counterbalancing this are specific, recent data developed from a large LQTS registry relating to the use of stimulant medications in patients with LQTS, which suggest that use of these medications was associated with increased risk of cardiac events, particularly in males.100 A concurrent, smaller retrospective study found no such effect,101 indicating that in LQTS consensus regarding the safety of stimulant medication has not yet been reached.
2. Identification of young patients at risk for SCD
Prodromal signs and screening
Prodromal symptoms/signs/events – value of warning signs
Certain prodromal symptoms and clinical events identify groups of patients at increased risk for SCD. Their specific predictive power can be incorporated into calculations regarding the desirability of interventions such as diagnostic screening or, in the case of known disease, primary prevention by medical therapy and/or ICD implantation.
The most reliable presenting symptom which specifically indicates both the likely presence of a primary cardiac diagnosis is aborted or resuscitated sudden cardiac arrest. The likelihood of recurrent episode of cardiac arrest in these patients is so well-recognized that it constitutes a significant fraction of ICD implantations performed in young patients,102 even in cases for which a specific diagnosis may not be established and the patient receives the default classification of idiopathic ventricular fibrillation.
Other prodromal symptoms commonly associated with risk of SCD are those of non-sustained arrhythmia: palpitations, chest pain, syncope and seizure, representing transient fluctuations in pulse and blood pressure caused by brief arrhythmic episodes. Studies of unexpected SCD in apparently healthy children suggest that a significant fraction, perhaps ¼ to ½, may have experienced an antecedent symptoms, frequently syncope or seizure.33 However, palpitation, chest pain and syncope are prevalent in healthy children,103 and thus of limited diagnostic value as an isolated finding. An exception to this may be exertional syncope, which is associated with considerably greater likelihood of cardiac disease.104 When taken in combination with other findings of cardiac disease, however, any of these symptoms may be indicative of increased risk.
Screening for SCD in the young
Many have proposed screening programs for SCD, either on a societal basis or for subpopulations (like athletes) perceived to be at high risk. This has been the recent subject of study by a working group at the National Heart Lung and Blood Institute.105 This topic can be approached by applying general principles used to determine whether a screening test is clinically useful. First, the test must be diagnostically sensitive for the target disease. The disease should not be exceedingly rare, and should pose a risk of a life-threatening manifestation as a first event. The cost of the test and the potential costs of a false positive diagnosis should be low. Finally, effective therapies should be available.106, 107 The utility of a screening test is measured in relation to threshold values that are societally accepted ($50,000 - $100,000 for each life year saved in the US).
Various cardiovascular screening strategies have been proposed, including ECG, history and physical examination, and echocardiogram singly and in combination.108-112 The sensitivity, specificity and positive and negative predictive values of tests used for cardiac screening depends on the disease in question and its prevalence in the screened population. Analyses of differing screening approaches have been published in community populations,113 and in age-defined populations (e.g., in neonates for the diagnosis of LQTS)49 and those identified by athletic participation114, 115 or by the use of stimulant medications.116, 117 This literature suggests that the ECG is a sensitive and efficient screening test for most diagnoses that cause SCD in young people and may be prophylactically treated, including LQTS, WPW, HCM, and BrS.118 Various coding systems have been developed in efforts to optimize the utility of the ECG in this screening function.119, 120
Cost-effectiveness studies of screening in asymptomatic youth have been performed, with selected results presented below. (Table 2). All such studies are sensitive to underlying assumptions and provide a range of possible findings on sensitivity analysis. However, they suggest that ECG screening in most settings is cost-ineffective or marginally cost-effective, with sensitivity to initial assumptions regarding baseline disease prevalence and efficacy of available therapies. Cost-effectiveness could be increased by targeting groups that have a particularly high risk of SCD (e.g., NCAA Division 1 athletes47) if effective measures could be taken to mitigate those risks, or groups that may stand to gain significant additional protection by early identification of arrhythmic disease (e.g., screening for LQTS in infancy49, 121).
Table 2.
Cost-effectiveness studies on ECG-based cardiovascular screening in young
| Study | Patient group | Age range (yrs) | Cost per life-year saved | Comments |
|---|---|---|---|---|
| Fuller, et al122 | Preparticipation sports screening | Teenagers | Hx and physical: $84,000 ECG: $44,000 Echocardiogram: $200,000 |
Designed as means to compare different screening modalities |
| Zupancic et al123 | LQTS screening in newborns | Newborns | $28,400 - $118,900 | Assumes that most SIDS not preventable by LQTS treatment, and identification of “high-risk” population |
| Quaglini et al124 | LQTS screening in newborns | Newborns | €11,700 | Includes identification of other cardiac diseases and assumes high treatment effect on LQTS |
| Denchev et al125 | Screening for ADHA medications use | School-aged children | Incremental cost of adding ECG to HX and physical: $27,200 - $39,300 | Cost of total strategy not modeled, most of benefit based on assumption of restriction from sports activity, not ADHD meds |
| Wheeler et al126 | Preparticipation sports screening | Teenagers and college students | Incremental cost of adding ECG to HX and physical: $21,200 - $71,300 Total cost: $62,000 - $130,00 |
ECG / history and physical Sensitive to effective of intervention and cost of screening |
| Schoenbaum et al127 | Preparticipation sports screening | Teenagers | Incremental cost of adding ECG to HX and physical: $37,300 - $68,800 | Cost of total strategy not modeled, with most of cost driven by evaluation of false-positive findings |
| Leslie et al117 | Screening for ADHD medications use Preparticipation sports screening | School-aged children and adolescents | $91,000 - $204,000 | ECG only Sensitive of prevalence, mortality and effectiveness of interventions |
| Halkin et al128 | 20-yr ECG screening model at Medicare reimbursement rates | High school and college athletes | $10,600,000 - $14,400,000 per life saved (cost / life-year not calculated) | Modeled according to Italian screening program using US statistics |
There is widespread community-based interest in cardiac screening, often based on application of existing guidelines12, 14, 15 by self-organized advocacy groups. Many such groups have demonstrated a high level of proficiency in structuring these programs. Although cardiovascular screening has been adopted as public policy and met with widespread acceptance in some countries,49, 88, 129 practical concerns have limited enthusiasm for mandated screening in the US and elsewhere.130 Chief among these are 1) the impact of false-positive findings, which include unnecessary work-up, proscription from sport or other desired, healthful or necessary activity, and possible creation of psychological harms,115, 116 2) the effect of inaccuracy in diagnosis to discount the potential value of cardiovascular screening in actual use131-133 , and 3) the willingness of patients with positive screening tests to pursue further diagnosis and management.114
Effective yield of screening tests can be increased by limiting testing to relatives of disease probands. For heritable arrhythmias, this markedly increases the pre-test probability regarding the potential prevalence (i.e. 50%) of disease in the tested population, enhancing the positive predictive value. This approach, termed cascade screening, is useful in families with known disease causing mutations and phenotypes,134, 135 such as LQTS, as well as in cases of sudden unexplained death,135-139 employing electrocardiographic, genetic or other techniques as appropriate. In one study employing a national registry, an average of 2.1 new cases were identified per each LQTS proband,134 and observational studies have noted a high diagnostic yield of affected family members of victims of SCD and unexplained cardiac arrest,137 although this has not been a uniform finding.140
SCD in the young and the affected family
Several challenges relevant to the health of surviving family members must be confronted immediately following an event of SCD in the young. First, the occurrence and quality of a postmortem evaluation (i.e. autopsy) hinges on the specific state, county, and city in which the SCD occurred, as there is a wide range of competency with respect to postmortem cardiac diagnosis, as well as the availability of specialized cardiac examination.141 Second, the scope of cardiac evaluations among first degree relatives following an SCD event is not standardized. In the absence of a standard of care for clinical investigation of families affected by SCD, the response of physicians confronted with this presentation may range from simple inquiry as to symptoms, to obtaining a broad range of noninvasive and, in some cases, invasive cardiac testing on each individual, and then repeating such testing at frequent intervals. Third, the occurrence and quality of postmortem genetic testing (also referred to as the molecular autopsy) is unsettled at the present time, with the emergence of new genetic technology and increasingly subtle understanding of the significance of different genetic markers and point mutations, and thus also varies tremendously.142-146 Application of genetic testing of the SCD victim, potentially valuable and specific tool for clinical investigation when performed within the construct of wider familial investigations, is also often confronted by challenges with reimbursement for tests performed on deceased individuals.
As a consequence, the ability of the clinician to provide useful diagnostic information to families of young SCD victims is at present in a state of transition. In the best case scenario, phenotypic and in some cases genotypic information obtained both from the affected individual and close relations will be considered together to provide both a specific diagnosis, identification of other family members at risk and actionable clinical information of value to the survivors.
Presently, there are no consensus guidelines/recommendations as to what a comprehensive post-mortem investigation of a youthful SCD victim must entail and what the minimum pre-mortem investigation of the surviving first degree relatives ought to include. At minimum, standard operating procedures from medical examiner's offices need to include obtaining so-called “DNA friendly tissue” (blood in EDTA, frozen nucleated tissue, or blood spot cards) to permit post-mortem genetic testing if indicated.147, 148 For the surviving first degree relatives, cardiologic testing should be tailored according to the autopsy findings of the decedent but a 12-lead electrocardiogram, 24-hour Holter monitor, treadmill stress test, and an echocardiogram comprise a reasonable set of initial tests. It remains to be determined whether such post-mortem investigations of the decedent and pre-mortem investigations of the living should be pursued in parallel or whether a sequential investigation starting with a molecular autopsy of the decedent may be more cost effective.
Risk stratification in specific individual diseases
A small but significant fraction (12 – 18%) of young patients experiencing SCD has a prior known cardiac diagnosis.33, 43 Once a specific high risk diagnosis has been established, the presence of arrhythmia symptoms or other findings can be used to identify subpopulations at increased risk of SCD. Risk stratification is limited to conditions that are prevalent and well-studied in multiple independent groups of patients; this criterion is met perhaps most notably the case for patients diagnosed with hypertrophic cardiomyopathy and certain channelopathies such as long QT syndrome, for whom explicit guidelines have been written.8, 11 However, the studies available to inform risk stratification strategies specific to young populations in this and other SCD predisposing diseases are generally retrospective in design, and many variables identified as associating with patients at increased risk are also associated with one another. Thus, risk stratification schema for SCD in the young are less explicitly prescriptive than many of the validated risk assessment tools used in adult cardiology, and risk factor assessment must be applied cautiously, and in conjunction with individualized clinical assessment and judgment.
3. Prophylaxis and secondary therapy of SCD in the young
Primary prevention and SCD
For patients who have been identified as being at high risk for SCD, it may be appropriate to consider placement of an ICD for primary prevention. This is a principal which has long been widely accepted in adult populations, based on studies of ischemic cardiomyopathy and left ventricular dysfunction in which the benefits of ICD implantation are clearly demonstrated.149-151 In children with SCD-predisposing diseases and syndromes, the risk to benefit relationship that pertains to ICD use is less clearly developed. From the point of view of risk of ICD, children clearly have a relatively high rate of complications associated with devices, including frequency of inappropriate shocks, lead malfunctions and difficulties in ICD placement related to intracardiac anatomy and small size.152, 153 Conversely, from the point of view of potential benefits associated with primary prophylaxis, children may stand to gain relatively less from ICD implantation. In particular, the known rate of sudden death associated with congenital heart disease and a variety of arrhythmic cardiomyopathies is considerably lower than that observed in adult populations in whom ICD is seen to be useful (e.g., as mentioned above for adults tetralogy of Fallot, in whom these rates range from 0.1 – 0.2%/yr). Guidelines relating to indications for implantation of ICDs for the purpose of primary prevention in children and young people with CHD and other SCD-predisposing illnesses are written with considerable latitude, compared to those used in adults with acquired heart disease.7 However, recognizing the difficulties associated with ICDs in this population, clinicians specializing in pediatric patients at risk for SCD have generally applied conservative algorithms to the decision-making process regarding whether or not to implant these devices.
Resuscitation of SCD
Relation between resuscitation and SCD
It is unfortunate that the epidemiology and clinical diagnosis of SCD-predisposing conditions are not typically addressed in conjunction with the science and practice of resuscitation. For this reason, the literature and knowledge base in these two fields is to a great extent non-overlapping, although they are well connected around the shared topic of defibrillation. Given the dismal rates of survival of out-of-hospital arrest (OHCA), all components of resuscitation science can legitimately be considered as relevant to an integrated approach to the prophylaxis and management of SCD in the young. An understanding of clinical characteristics of SCD in the young informs resuscitation strategies and deployment of services in the community. Conversely, continuous improvement and measurement of the efficacy and availability of effective bystander and EMS response to SCD improves survival and changes the risk to benefit calculations useful in planning for individual clinical decisions in patients known to have an SCD-predisposing condition.
Definition of sudden cardiac arrest (SCA)
From the perspective of resuscitation, the concept of SCA is more useful than SCD, by virtue of its specificity. SCA is defined as “malfunction or cessation of the electrical and mechanical activity of the heart, resulting in almost instantaneous loss of consciousness and collapse”.154 This definition focuses on primary cardiovascular causes and does not specify an outcome. Prior definitions such as “non-traumatic death occurring instantaneously or within ... 24 hours of the onset of acute symptoms”23 are better termed sudden unexpected death because the underlying etiology is broader and the defined outcome is death.
Pathophysiology of SCA and principles of management
Rhythms in young people experiencing OHCA include asystole, pulseless electrical activity, and ventricular fibrillation (VF). In epidemiologic studies of out of hospital cardiac arrest (OHCA) in youth, asystole is more common than ventricular arrhythmias.36, 155 However, these studies include patients with comorbidities, intercurrent illness, drowning, and suffocation. In SCA in the population discussed here, the primary arrhythmia is often VF.35
The pathophysiology of SCA induced by pulseless ventricular tachycardia (pVT) and/or VF is time-dependent, with 3 phases distinguished by cardiac rhythm and metabolic consequences of low-flow and hypoxia. These phases define appropriate therapies and predict probability of survival and neurologic disability. 156 The initial electrical phase lasts approximately 4 minutes and is defined by the presence of shockable rhythms. During this period, the heart is responsive to defibrillation, as established by outcomes of ICD implantation and deployment of public access defibrillation program studies.157-159
The circulatory phase is characterized by onset of tissue hypoxemia and emergence of asystole. Cardiopulmonary resuscitation (CPR) to provide oxygen delivery is crucial during this phase.160 Defibrillation is less effective, but may be enhanced by pre-shock epinephrine administration and effective CPR.161-164,165 The metabolic phase commences approximately 10 minutes after SCA, distinguished by asystole, worsening hypoxia and circulating metabolic factors resulting in cell death and end organ dysfunction. Survival during the metabolic phase is unlikely and often associated with severe functional disability.
Components of CPR
CPR has 4 components in both children and adults: chest compression, defibrillation, ventilation, and pharmacologic agents. Although all are thought to be important, effective chest compression and early defibrillation have been most clearly linked to increased survival.
Chest compression
Chest compressions generate forward blood flow by causing intrathoracic pressure changes166, 167 and by direct cardiac compression.168 Standard CPR produces 30-40% of normal cardiac output with variations between vascular beds: cerebral flow may be as high as 60%, but myocardial flow is substantially lower at 10-30%.166, 169 Restoration of cerebral function is dependent on the former,170, 171 while cardiac resuscitation depends on adequate coronary perfusion pressure.166, 172-174
Perfusion pressures increase over a period of 5-7 compressions during CPR but fall rapidly during pauses. Thus, time for coronary and cerebral perfusion is curtailed during ventilatory pauses.175 Effective CPR also requires complete chest recoil to allow venous return into the thorax,176-179 and excessive compression rates compromise coronary blood flow and compression depth.180-182 On balance, compression fractions of <80% appear associated with decreased survival,183-185 and current recommendations emphasize short, infrequent pauses.
Defibrillation
Early defibrillation is a significant determinant of survival from VF arrest. It was hypothesized originally that the electric current terminated fibrillation by depolarization of a critical mass of myocardium.186 Recently, the importance of preventing re-initiation of fibrillation after defibrillation has been recognized.187 Determinants of defibrillation success are current delivery, waveform shape and transthoracic impedance. Biphasic waveforms have a high success rate for VF termination and have replaced monophasic devices in practice.188-191
Airway management and ventilation
Assisted ventilation was initially considered essential for successful resuscitation.192 However, when cardiac arrest is abrupt, oxygen content within the vascular space is adequate to permit a period of compression without ventilation. Positive pressure ventilation increases intrathoracic pressure and may decrease cardiac output and coronary perfusion pressure.176, 193 Optimal compression:ventilation ratios have not been determined, but recent guidelines trended toward a greater emphasis on chest compression.194
Pharmacologic agents
Vasopressive and antiarrhythmic agents are widely used in resuscitation, but no drug has been shown in prospective trial to improve long-term survival from cardiac arrest.195 Administration of epinephrine during cardiac arrest has been accepted as a standard of care, but its use remains controversial; although epinephrine has been shown to improve ROSC, no improvement in long-term survival has yet been demonstrated.196 Vasopressin has been used as an alternative, but trials comparing epinephrine to either vasopressin or placebo have failed to show superiority to hospital discharge or long-term survival.194, 197, 198 Further clinical trials are needed on this topic, as all studies to date have been underpowered to draw conclusions with respect to survival outcomes.199
Similarly, limited evidence is available to guide the use of antiarrhythmics agents during cardiac arrest. In one randomized out-of-hospital trial, amiodarone improved survival to hospital admission compared to placebo,200 and this drug has been recommended for treatment of shock-resistant or recurrent pVT/VF since 2005. However, no randomized trial testing the efficacy of amiodarone or lidocaine for OHCA has demonstrated improved survival to discharge.201 An study in hospitalized young patients showed that survival to hospital discharge is improved with lidocaine compared to amiodarone202 and guided the 2015 AHA recommendations to downgrade amiodarone during cardiac arrest in children.4 The Resuscitation Outcomes Consortium is currently conducting a study of antiarrhythmic use during CPR.203
High Quality CPR
It has become apparent that high quality CPR is a major determinant of survival.4, 160, 184, 204, 205 In practice, CPR performance is often sub-optimal by both EMS and hospital providers.181, 206, 207 Metrics of the quality of CPR include maintenance of appropriate chest compression rate and depth, adequacy of chest recoil, fraction of time during CPR that chest compressions are being performed and maintenance of appropriate ventilation rate. Multiple studies have shown the positive effect on outcomes when these parameters are measured and monitored.183, 208-210
Major emphasis is now placed on chest compression, and animal and human studies172, 174, 211-215 have shown equivalent survival with chest compression only. In 2008, the AHA recommended chest compression only CPR for bystanders who witnessed the sudden collapse of a victim,216 and in 2010, the American Heart Association revised the ABC of CPR (Airway - Breathing - Chest Compression) to CAB (Chest Compression - Airway - Breathing).217 This recommendation was made based on the data that demonstrate effectiveness and the need to increase the frequency and quality of bystander CPR and to reduce obstacles to lay-persons performing CPR. 36, 218, 219,220 In practice studies, delay of intubation until after 4 cycles of chest compression, defibrillation and administration of epinephrine by EMS providers has result in doubling of survival in patients with witnessed arrest and shockable rhythms and OHCA survival increased by 40%.167 A recent, population–based study from Japan suggests that broad dissemination of chest-compression only CPR for bystanders was associated with a substantial increase in neurologically favorable survival.221
CPR techniques for young children
The basic physiological principles of CPR apply to babies and children, but there are differences in technique to accommodate age related differences in body size, elasticity of chest wall and differing primary causes of arrest. Thus, the AHA guidelines recommend different compression-ventilation ratios and less compression depth for infants .3, 194 Current guidelines also do not recommend chest compression only CPR for young children, based on two Japanese studies in which children who received chest compression-only had worse neurologic outcomes. However, chest compression-only CPR was as effective as conventional CPR in children presumed to have arrest from a cardiac etiology.222
Chain of Survival
Survival from cardiac arrest depends on immediate initiation of treatment, with likelihood of survival decreasing 10% with every minute delay in initiation of CPR.223 The Chain of Survival construct has guided practical deployment of resuscitation principles in the field.
Wide disparities exist in survival of OHCA in the United States. Data from 10 North American sites revealed survival rates ranging from 7.7 to 39.9%.204 Although differences in patient demographics, education and health status account for some of this difference, it is likely that community and health care system factors accounted for much of this variability. 224 Several communities have undertaken to improve their survival statistics, including the Seattle/King County, Arizona, Denver, and Wake County, North Carolina.225-231 Each has observed a doubling or tripling of survival from OHCA, and their experiences have provided direction for system improvement in other communities. Critical factors include strong leadership robust community engagement, an efficient, well-supported EMS system, and hospitals capable of providing excellent post-arrest care.
Leadership
Leadership in the high-performing communities has established a culture of excellence, with continuous data collection, analysis and reporting so that progress associated with the implementation of new strategies could be measured. 225-232 Examples of successful new approaches have included changing CPR protocols to minimize chest compression pauses during defibrillation, continuous chest compression for several minutes and delayed ventilations and intubation, and use of the impedance threshold devices.
Community Engagement
The first three links of the chain (early EMS activation, early CPR and early defibrillation) require community response and acceptance of civic duty to respond and deliver basic life support. Bystander CPR improves the response of the heart to defibrillation233 and can double or triple survival to hospital discharge and improve neurological outcome.234-237,238-240 However, only 4% of the US population has received any CPR training,241 and of the 15-20% of OHCA, only 20-30% receive bystander CPR or defibrillation242-245
CPR training has been supported by the American Heart Association and the American Red Cross for decades, but CPR courses are an inefficient and expensive method to train large numbers of responders, with rural areas and communities with high proportion of Hispanic and African-American residents particularly difficult to reach. Alternative methods to provide training to all members of society include school-based training, or as a prerequisite for civil activity such as obtaining a driver's license. School-based training has been endorsed by the World Health Organization246 and the AHA.247 Legislatures in 27 states have enacted legislation to require or support CPR training as a graduation requirement.
A Danish program to expand public CPR response included mandatory training in schools and prior to receipt of a driver's license, distribution of CPR self-instruction kits, improved dispatch CPR training and increased number of AEDs.248 Bystander CPR rates increased from <20% to 40-70% and survival from OHCA increased from 2.9% to 10.2%. In the US, the Take Heart America Program also increased bystander CPR rates and hospital discharge.249 Targeting family members of persons at high-risk for training (e.g., those with inherited arrhythmia syndromes or CHD) also has merit, with instruction shown to improve self-confidence to perform CPR and increase the number of trained personnel by inclusion of other family members, caregivers and friends.250-253
Public Access Defibrillation
The development of automated external defibrillators (AEDs) which allow minimally trained persons to use a defibrillator has led to the establishment of Public Access Defibrillation (PAD) sites over the last 20 years. Outcome improvements have been demonstrated in selected sites such as government buildings, airports and transportation centers, and casinos.224 The Public Access Defibrillation Trial demonstrated a twofold improvement in adult survival with good neurologic function when victims were resuscitated with CPR and AEDs compared to only CPR.159
PAD sites require an organizational structure to maintain effectiveness.254 PAD programs which have appropriate leadership, with AEDs placed in locations of highest-risk with ongoing maintenance, have a cost per quality-adjusted life-year of $30,000-100,000.255-257 However, in programs where one or more of these elements is absent, the cost per QALY can be substantially higher.258, 259 Practical problems encountered with PAD programs include expired disposable equipment, limited access to the AED and poorly marked locations.260 School-based AED programs have strong support, due to the social prominence of sports events in that setting and concern for prevention of sudden death in athletes.261, 262 Despite the rarity of an event, school programs appear to be effective.263, 264
Because the many cardiac arrests occur in the home, home AEDs could be potentially useful. Successful AED use has been reported for young children,265, 266 but randomized trials placing AEDs in homes of older high-risk individuals have not shown benefit,267 possibly due to low proportion of witnessed events, and low use of the AED despite its availability.
Hospitals and Post Arrest Care
The final link in the chain of survival is early post-resuscitation care in hospitals. Post-cardiac arrest syndrome is recognized as a complex clinical condition encompassing several pathophysiologic processes.268, 269 Myocardial dysfunction, neurologic injury, systemic ischemic injury, and reperfusion injury dictate both rapid assessment and therapeutic needs in order to stabilize a patient and prevent further injury. Patients may develop systemic inflammatory and septic shock syndromes which further affect disability-free outcomes.270, 271 Multidisciplinary care is focused on hemodynamic and ventilatory support, neurologic preservation and prevention of further injury and secondary comorbidities.
Targeted temperature management (TTM) has been applied with a goal of slowing pathophysiologic events and biochemical systems which cause cellular damage. Early randomized studies used targeted temperatures of 32-34°C and reported improved neurologic outcomes for patients with VF arrests.272 However, questions remain about optimal target temperature, specific populations, duration of hypothermia and methods for induction, maintenance and reversal. A recent multi-center, randomized trial of TTM in young OHCA victims observed no difference in neurologic outcomes at 1 year.273 Despite this seemingly negative response, TTM remains a therapeutic option for patients < 18 years, has been rapidly incorporated into standard clinical practice and is still recommended for patients with shockable rhythms.274 Extracorporeal membrane oxygenation (ECMO or eCPR) may be of potential use for patients with underlying congenital heart disease or where a reversible disease process is present and where existing protocols, personnel and equipment are established and readily available.4, 275, 276 No data are available for ECMO for OHCA where institution of cardiovascular support is markedly delayed, although it has been demonstrated to be effective following prolonged CPR after in-hospital CA in children.277, 278
Conclusions
Over the past decade, there has been a proliferation of data to guide the identification and management of children and young adults who are at risk for sudden cardiac death. The prevalence of this problem is low but its consequences are great, and a stepwise approach can be used to identify targets for prophylaxis and therapy. By organizing and placing into perspective relevant literature in each of these areas, outstanding deficiencies of knowledge relevant to these topics ban be more readily identified. Urgent questions that must be addressed include the following.
How can we use our knowledge of the epidemiology of SCD in the young to guide the further development of effective clinical and health policy interventions? Should ECG screening be used to identify youth at risk? If so, should screening be universal or should it be focused on subgroups perceived to be at higher risk of SCD?
How should post-mortem evaluation be performed following SCD, both of the victim and of his or her living relatives, and what is the utility of post-mortem genetic testing (i.e., the molecular autopsy)?
Is it possible to reduce the prevalence of SCD in the young by prophylactic lifestyle restrictions? Which conditions might benefit from that approach, what types of activities should be restricted and how could the effects of such interventions be measured?
Which young patients actually benefit from primary prevention ICDs? Can improvements in ICD design and implant techniques improve the risk to benefit ratio in children and make them more useful technology in patients known to be at high risk?
Are there modifiable barriers to improving resuscitation of the young in the community? How can emergency medical services and post-resuscitation care be better organizing to improve survival outcomes after out of hospital cardiac arrest in the young?
Management of SCD in the young includes both preemptive mitigation of its risk and effective response to cardiac arrest by the community. Steps toward these goals may include the informed and appropriate use of screening programs to identify patients at risk, risk stratification for patients with SCD-predisposing diseases, provision of appropriate prophylactic therapy and advice regarding lifestyle, wide deployment of resuscitation expertise and technology, and services for diagnostic evaluation and provision of aftercare to affected families. The institution and use of a national registry of SCD in the young will be a major source of data that will help to answer some of the most pressing questions in this area.
Figure 6.
The Chain of Survival rubric.
Acknowledgements
The authors would like to acknowledge and express appreciation for the critical reading of this manuscript and editorial remarks of Dr. Dominic Abrams.
Dr. Michael Ackerman is supported in part by the Mayo Clinic Windland Smith Rice Comprehensive Sudden Cardiac Death Program. He is a consultant for Boston Scientific, Gilead Sciences, Medtronic, and St. Jude Medical. Mayo Clinic and Dr. Ackerman receive sales based royalties from Transgenomic for their FAMILION-LQTS and FAMILION-CPVT genetic tests.
Dr. John Triedman is supported in part by NIH 1U10HL109816. He is a consultant for Biosense Webster.
Footnotes
Conflict of Interest Disclosures
Dr. Dianne Atkins has no disclosures.
References
- 1.Willinger M, James LS, Catz C. Defining the sudden infant death syndrome (sids): Deliberations of an expert panel convened by the national institute of child health and human development. Pediatr Pathol. 1991;11:677–684. doi: 10.3109/15513819109065465. [DOI] [PubMed] [Google Scholar]
- 2.Moon RY, Syndrome TFoSID Sids and other sleep-related infant deaths: Expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128:1030–1039. doi: 10.1542/peds.2011-2284. [DOI] [PubMed] [Google Scholar]
- 3.Atkins DL, Berger S, Duff JP, Gonzales JC, Hunt EA, Joyner BL, Meaney PA, Niles DE, Samson RA, Schexnayder SM. Part 11: Pediatric basic life support and cardiopulmonary resuscitation quality: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S519–525. doi: 10.1161/CIR.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 4.de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, Sutton RM, Tijssen JA, Topjian A, van der Jagt É , Schexnayder SM, Samson RA. Part 12: Pediatric advanced life support: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S526–542. doi: 10.1161/CIR.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JM, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O'Connor RE, Samson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF. Part 1: Executive summary: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S315–367. doi: 10.1161/CIR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 6.Link MS, Myerburg RJ, Estes NA, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 12: Emergency action plans, resuscitation, cardiopulmonary resuscitation, and automated external defibrillators: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e334–338. doi: 10.1161/CIR.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 7.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Foundation ACoC, Guidelines AHATFoP, Society HR 2012 accf/aha/hrs focused update incorporated into the accf/aha/hrs 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the american college of cardiology foundation/american heart association task force on practice guidelines and the heart rhythm society. Circulation. 2013;127:e283–352. doi: 10.1161/CIR.0b013e318276ce9b. [DOI] [PubMed] [Google Scholar]
- 8.Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW, Guidelines ACoCFAHATFoP, Surgery AAfT, Echocardiography ASo, Cardiology ASoN, America HFSo, Society HR, Interventions SfCAa, Surgeons SoT 2011 accf/aha guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation. 2011;124:2761–2796. doi: 10.1161/CIR.0b013e318223e230. [DOI] [PubMed] [Google Scholar]
- 9.Maron BJ, Udelson JE, Bonow RO, Nishimura RA, Ackerman MJ, Estes NA, Cooper LT, Link MS, Maron MS, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 3: Hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e273–280. doi: 10.1161/CIR.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 10.Ackerman M, Zipes D, Kovacs R, Maron B. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 10: The cardiac channelopathies. Circulation. 2015;132:e326–9. doi: 10.1161/CIR.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 11.Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, Blom N, Brugada J, Chiang CE, Huikuri H, Kannankeril P, Krahn A, Leenhardt A, Moss A, Schwartz PJ, Shimizu W, Tomaselli G, Tracy C. Hrs/ehra/aphrs expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: Document endorsed by hrs, ehra, and aphrs in may 2013 and by accf, aha, paces, and aepc in june 2013. Heart Rhythm. 2013;10:1932–1963. doi: 10.1016/j.hrthm.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Vetter VL, Elia J, Erickson C, Berger S, Blum N, Uzark K, Webb CL, Committee AHACoCDitYCCD, Nursing AHACoC Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: A scientific statement from the american heart association council on cardiovascular disease in the young congenital cardiac defects committee and the council on cardiovascular nursing. Circulation. 2008;117:2407–2423. doi: 10.1161/CIRCULATIONAHA.107.189473. [DOI] [PubMed] [Google Scholar]
- 13.Estes NA, Kovacs RJ, Baggish AL, Myerburg RJ, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 11: Drugs and performance-enhancing substances: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e330–333. doi: 10.1161/CIR.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 14.Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, Dimeff R, Douglas PS, Glover DW, Hutter AM, Krauss MD, Maron MS, Mitten MJ, Roberts WO, Puffer JC, American Heart Association Council on Nutrition PyA, and Metabolism Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: A scientific statement from the american heart association council on nutrition, physical activity, and metabolism: Endorsed by the american college of cardiology foundation. Circulation. 2007;115:1643–1455. doi: 10.1161/CIRCULATIONAHA.107.181423. [DOI] [PubMed] [Google Scholar]
- 15.Maron BJ, Friedman RA, Kligfield P, Levine BD, Viskin S, Chaitman BR, Okin PM, Saul JP, Salberg L, Van Hare GF, Soliman EZ, Chen J, Matherne GP, Bolling SF, Mitten MJ, Caplan A, Balady GJ, Thompson PD, Clinical Cardiology AHACo, Committee AC, in the Young Council on CD, Anesthesia CoCSa, Prevention CoEa, Biology CoFGaT, Council on Quality of Care and Outcomes Research aACof C Assessment of the 12-lead electrocardiogram as a screening test for detection of cardiovascular disease in healthy general populations of young people (12-25 years of age): A scientific statement from the american heart association and the american college of cardiology. J Am Coll Cardiol. 2014;64:1479–1514. doi: 10.1016/j.jacc.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Levine BD, Baggish AL, Kovacs RJ, Link MS, Maron MS, Mitchell JH, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 1: Classification of sports: Dynamic, static, and impact: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e262–266. doi: 10.1161/CIR.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 17.Maron BJ, Zipes DP, Kovacs RJ, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Preamble, principles, and general considerations: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e256–261. doi: 10.1161/CIR.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 18.Van Hare GF, Ackerman MJ, Evangelista JA, Kovacs RJ, Myerburg RJ, Shafer KM, Warnes CA, Washington RL, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 4: Congenital heart disease: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e281–291. doi: 10.1161/CIR.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 19.Zipes DP, Link MS, Ackerman MJ, Kovacs RJ, Myerburg RJ, Estes NA, American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology CoCDitY, Council on Cardiovascular and Stroke Nursing, C.uncil on Functional Genomics and Translational Biology, and the American College of Cardiology Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 9: Arrhythmias and conduction defects: A scientific statement from the american heart association and american college of cardiology. Circulation. 2015;132:e315–325. doi: 10.1161/CIR.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 20.Maron BJ, Murphy CJ, Haas TS, Ahluwalia A, Garberich RF. Strategies for assessing the prevalence of cardiovascular sudden deaths in young competitive athletes. Int J Cardiol. 2014;173:369–372. doi: 10.1016/j.ijcard.2014.02.021. doi: 310.1016/j.ijcard.2014.1002.1021. Epub 2014 Feb 1022. [DOI] [PubMed] [Google Scholar]
- 21.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: Multiple source surveillance versus retrospective death certificate-based review in a large u.S. Community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 22.Molander N. Sudden natural death in later childhood and adolescence. Arch Dis Child. 1982;57:572–576. doi: 10.1136/adc.57.8.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Driscoll DJ, Edwards WD. Sudden unexpected death in children and adolescents. J Am Coll Cardiol. 1985;5:118B–121B. doi: 10.1016/s0735-1097(85)80540-4. [DOI] [PubMed] [Google Scholar]
- 24.Gerein RB, Osmond MH, Stiell IG, Nesbitt LP, Burns S, Group OS. What are the etiology and epidemiology of out-of-hospital pediatric cardiopulmonary arrest in ontario, canada? Acad Emerg Med. 2006;13:653–658. doi: 10.1197/j.aem.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 25.Puranik R, Chow CK, Duflou JA, Kilborn MJ, McGuire MA. Sudden death in the young. Heart Rhythm. 2005;2:1277–1282. doi: 10.1016/j.hrthm.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Chugh SS, Reinier K, Balaji S, Uy-Evanado A, Vickers C, Mariani R, Gunson K, Jui J. Population-based analysis of sudden death in children: The oregon sudden unexpected death study. Heart Rhythm. 2009;6:1618–1622. doi: 10.1016/j.hrthm.2009.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park CB, Shin SD, Suh GJ, Ahn KO, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Pediatric out-of-hospital cardiac arrest in korea: A nationwide population-based study. Resuscitation. 2010;81:512–517. doi: 10.1016/j.resuscitation.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Papadakis M, Sharma S, Cox S, Sheppard MN, Panoulas VF, Behr ER. The magnitude of sudden cardiac death in the young: A death certificate-based review in england and wales. Europace. 2009;11:1353–1358. doi: 10.1093/europace/eup229. doi: 1310.1093/europace/eup1229. Epub 2009 Aug 1321. [DOI] [PubMed] [Google Scholar]
- 29.Hendrix A, Vaartjes I, Mosterd A, Reitsma JB, Doevendans PA, Grobbee DE, Bots ML. Regional differences in incidence of sudden cardiac death in the young. Neth J Med. 2010;68:274–279. [PubMed] [Google Scholar]
- 30.Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, Bundgaard H, Svendsen JH, Haunso S, Tfelt-Hansen J. Nationwide study of sudden cardiac death in persons aged 1-35 years. Eur Heart J. 2011;32:983–990. doi: 10.1093/eurheartj/ehq428. doi: 910.1093/eurheartj/ehq1428. Epub 2010 Dec 1092. [DOI] [PubMed] [Google Scholar]
- 31.Margey R, Roy A, Tobin S, O'Keane CJ, McGorrian C, Morris V, Jennings S, Galvin J. Sudden cardiac death in 14- to 35-year olds in ireland from 2005 to 2007: A retrospective registry. Europace. 2011;13:1411–1418. doi: 10.1093/europace/eur161. doi: 1410.1093/europace/eur1161. Epub 2011 Jul 1428. [DOI] [PubMed] [Google Scholar]
- 32.Wren C, O'Sullivan JJ, Wright C. Sudden death in children and adolescents. Heart. 2000;83:410–413. doi: 10.1136/heart.83.4.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winkel BG, Risgaard B, Sadjadieh G, Bundgaard H, Haunso S, Tfelt-Hansen J. Sudden cardiac death in children (1-18 years): Symptoms and causes of death in a nationwide setting. Eur Heart J. 2014;35:868–875. doi: 10.1093/eurheartj/eht509. doi: 810.1093/eurheartj/eht1509. Epub 2013 Dec 1015. [DOI] [PubMed] [Google Scholar]
- 34.Bardai A, Berdowski J, van der Werf C, Blom MT, Ceelen M, van Langen IM, Tijssen JG, Wilde AA, Koster RW, Tan HL. Incidence, causes, and outcomes of out-of-hospital cardiac arrest in children. A comprehensive, prospective, population-based study in the netherlands. J Am Coll Cardiol. 2011;57:1822–1828. doi: 10.1016/j.jacc.2010.11.054. [DOI] [PubMed] [Google Scholar]
- 35.Meyer L, Stubbs B, Fahrenbruch C, Maeda C, Harmon K, Eisenberg M, Drezner J. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: A 30-year review. Circulation. 2012;126:1363–1372. doi: 10.1161/CIRCULATIONAHA.111.076810. doi: 1310.1161/CIRCULATIONAHA.1111.076810. Epub 072012 Aug 076810. [DOI] [PubMed] [Google Scholar]
- 36.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA, Investigators ROC Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The resuscitation outcomes consortium epistry-cardiac arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kitamura T, Iwami T, Nichol G, Nishiuchi T, Hayashi Y, Nishiyama C, Sakai T, Kajino K, Hiraide A, Ikeuchi H, Nonogi H, Kawamura T, Project UO. Reduction in incidence and fatality of out-of-hospital cardiac arrest in females of the reproductive age. Eur Heart J. 2010;31:1365–1372. doi: 10.1093/eurheartj/ehq059. [DOI] [PubMed] [Google Scholar]
- 38.Daya M, Schmiker R, May S, Morrison L. Current burden of cardiac arrest in the united states: report from the resuscitation outcomes consortium. 2015 [Google Scholar]
- 39.Mitka M. Jama. United States: 2013. Us registry for sudden death in the young launched by the nih and cdc. p. 2495. [DOI] [PubMed] [Google Scholar]
- 40.Cobb LA, Weaver WD, Hallstrom AP, Copass MK. Cardiac resuscitation in the community. The seattle experience. Cardiologia. 1990;35:85–90. [PubMed] [Google Scholar]
- 41.Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R, Munkley DP, Lyver MB, Luinstra LG, Campeau T, Maloney J, Dagnone E. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: Opals study phase ii. Ontario prehospital advanced life support. JAMA. 1999;281:1175–1181. doi: 10.1001/jama.281.13.1175. [DOI] [PubMed] [Google Scholar]
- 42.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A, Prevention CfDCa Out-of-hospital cardiac arrest surveillance --- cardiac arrest registry to enhance survival (cares), united states, october 1, 2005--december 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 43.Pilmer CM, Kirsh JA, Hildebrandt D, Krahn AD, Gow RM. Sudden cardiac death in children and adolescents between 1 and 19 years of age. Heart Rhythm. 2014;11:239–245. doi: 10.1016/j.hrthm.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 44.Kitsantas P, Gaffney KF. Racial/ethnic disparities in infant mortality. J Perinat Med. 2010;38:87–94. doi: 10.1515/jpm.2010.014. [DOI] [PubMed] [Google Scholar]
- 45.Steinhaus DA, Vittinghoff E, Moffatt E, Hart AP, Ursell P, Tseng ZH. Characteristics of sudden arrhythmic death in a diverse, urban community. Am Heart J. 2012;163:125–131. doi: 10.1016/j.ahj.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in u.S. College athletes. J Am Coll Cardiol. 2014;63:1636–1643. doi: 10.1016/j.jacc.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 47.Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in national collegiate athletic association athletes. Circulation. 2011;123:1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622. [DOI] [PubMed] [Google Scholar]
- 48.Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the cardia study. Coronary artery risk development in (young) adults. Circulation. 1995;92:785–789. doi: 10.1161/01.cir.92.4.785. [DOI] [PubMed] [Google Scholar]
- 49.Schwartz PJ, Stramba-Badiale M, Crotti L, Pedrazzini M, Besana A, Bosi G, Gabbarini F, Goulene K, Insolia R, Mannarino S, Mosca F, Nespoli L, Rimini A, Rosati E, Salice P, Spazzolini C. Prevalence of the congenital long-qt syndrome. Circulation. 2009;120:1761–1767. doi: 10.1161/CIRCULATIONAHA.109.863209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khairy P, Harris L, Landzberg MJ, Viswanathan S, Barlow A, Gatzoulis MA, Fernandes SM, Beauchesne L, Therrien J, Chetaille P, Gordon E, Vonder Muhll I, Cecchin F. Implantable cardioverter-defibrillators in tetralogy of fallot. Circulation. 2008;117:363–370. doi: 10.1161/CIRCULATIONAHA.107.726372. [DOI] [PubMed] [Google Scholar]
- 51.Nieminen HP, Jokinen EV, Sairanen HI. Causes of late deaths after pediatric cardiac surgery: A population-based study. J Am Coll Cardiol. 2007;50:1263–1271. doi: 10.1016/j.jacc.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 52.Verheugt CL, Uiterwaal CS, van der Velde ET, Meijboom FJ, Pieper PG, van Dijk AP, Vliegen HW, Grobbee DE, Mulder BJ. Mortality in adult congenital heart disease. Eur Heart J. 2010;31:1220–1229. doi: 10.1093/eurheartj/ehq032. [DOI] [PubMed] [Google Scholar]
- 53.Nollert G, Fischlein T, Bouterwek S, Böhmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol. 1997;30:1374–1383. doi: 10.1016/s0735-1097(97)00318-5. [DOI] [PubMed] [Google Scholar]
- 54.Murphy JG, Gersh BJ, Mair DD, Fuster V, McGoon MD, Ilstrup DM, McGoon DC, Kirklin JW, Danielson GK. Long-term outcome in patients undergoing surgical repair of tetralogy of fallot. N Engl J Med. 1993;329:593–599. doi: 10.1056/NEJM199308263290901. [DOI] [PubMed] [Google Scholar]
- 55.Gatzoulis MA, Balaji S, Webber SA, Siu SC, Hokanson JS, Poile C, Rosenthal M, Nakazawa M, Moller JH, Gillette PC, Webb GD, Redington AN. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of fallot: A multicentre study. Lancet. 2000;356:975–981. doi: 10.1016/S0140-6736(00)02714-8. [DOI] [PubMed] [Google Scholar]
- 56.Silka MJ, Hardy BG, Menashe VD, Morris CD. A population-based prospective evaluation of risk of sudden cardiac death after operation for common congenital heart defects. J Am Coll Cardiol. 1998;32:245–251. doi: 10.1016/s0735-1097(98)00187-9. [DOI] [PubMed] [Google Scholar]
- 57.Valente AM, Gauvreau K, Assenza GE, Babu-Narayan SV, Schreier J, Gatzoulis MA, Groenink M, Inuzuka R, Kilner PJ, Koyak Z, Landzberg MJ, Mulder B, Powell AJ, Wald R, Geva T. Contemporary predictors of death and sustained ventricular tachycardia in patients with repaired tetralogy of fallot enrolled in the indicator cohort. Heart. 2014;100:247–253. doi: 10.1136/heartjnl-2013-304958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khairy P, Aboulhosn J, Gurvitz MZ, Opotowsky AR, Mongeon FP, Kay J, Valente AM, Earing MG, Lui G, Gersony DR, Cook S, Ting JG, Nickolaus MJ, Webb G, Landzberg MJ, Broberg CS, (AARCC) AfARiCC Arrhythmia burden in adults with surgically repaired tetralogy of fallot: A multi-institutional study. Circulation. 2010;122:868–875. doi: 10.1161/CIRCULATIONAHA.109.928481. [DOI] [PubMed] [Google Scholar]
- 59.Associations NFoSHS High school sports participation statistics, 2013 - 2014. 2014:2015. [Google Scholar]
- 60.Roberts WO, Stovitz SD. Incidence of sudden cardiac death in minnesota high school athletes 1993-2012 screened with a standardized pre-participation evaluation. J Am Coll Cardiol. 2013;62:1298–1301. doi: 10.1016/j.jacc.2013.05.080. [DOI] [PubMed] [Google Scholar]
- 61.Drezner JA, Rogers KJ, Zimmer RR, Sennett BJ. Use of automated external defibrillators at ncaa division i universities. Med Sci Sports Exerc. 2005;37:1487–1492. doi: 10.1249/01.mss.0000177591.30968.d4. [DOI] [PubMed] [Google Scholar]
- 62.Corrado D, Thiene G, Nava A, Rossi L, Pennelli N. Sudden death in young competitive athletes: Clinicopathologic correlations in 22 cases. Am J Med. 1990;89:588–596. doi: 10.1016/0002-9343(90)90176-e. [DOI] [PubMed] [Google Scholar]
- 63.Corrado D, Basso C, Thiene G. Sudden cardiac death in young people with apparently normal heart. Cardiovasc Res. 2001;50:399–408. doi: 10.1016/s0008-6363(01)00254-1. [DOI] [PubMed] [Google Scholar]
- 64.Maron BJ, Roberts WC, McAllister HA, Rosing DR, Epstein SE. Sudden death in young athletes. Circulation. 1980;62:218–229. doi: 10.1161/01.cir.62.2.218. [DOI] [PubMed] [Google Scholar]
- 65.Maron BJ, Epstein SE, Roberts WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol. 1986;7:204–214. doi: 10.1016/s0735-1097(86)80283-2. [DOI] [PubMed] [Google Scholar]
- 66.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: Analysis of 1866 deaths in the united states, 1980-2006. Circulation. 2009;119:1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. doi: 1010.1161/CIRCULATIONAHA.1108.804617. Epub 802009 Feb 804616. [DOI] [PubMed] [Google Scholar]
- 67.Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, Pearse LA, Virmani R. Sudden death in young adults: A 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141:829–834. doi: 10.7326/0003-4819-141-11-200412070-00005. [DOI] [PubMed] [Google Scholar]
- 68.Harmon KG, Asif IM, Maleszewski JJ, Owens DS, Prutkin JM, Salerno JC, Zigman ML, Ellenbogen R, Rao A, Ackerman MJ, Drezner JA. Incidence, etiology, and comparative frequency of sudden cardiac death in NCAA athletes: A decade in review. Circulation. 2015;132:10–9. doi: 10.1161/CIRCULATIONAHA.115.015431. doi: 10.1161/CIRCULATIONAHA.115.015431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Holst AG, Winkel BG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, Svendsen JH, Haunso S, Prescott E, Tfelt-Hansen J. Incidence and etiology of sports-related sudden cardiac death in denmark--implications for preparticipation screening. Heart Rhythm. 2010;7:1365–1371. doi: 10.1016/j.hrthm.2010.05.021. doi: 1310.1016/j.hrthm.2010.1305.1021. Epub 2010 May 1315. [DOI] [PubMed] [Google Scholar]
- 70.Solberg EE, Gjertsen F, Haugstad E, Kolsrud L. Sudden death in sports among young adults in norway. Eur J Cardiovasc Prev Rehabil. 2010;17:337–341. doi: 10.1097/HJR.0b013e328332f8f7. [DOI] [PubMed] [Google Scholar]
- 71.Harmon KG, Drezner JA, Maleszewski JJ, Lopez-Anderson M, Owens D, Prutkin JM, Asif IM, Klossner D, Ackerman MJ. Pathogeneses of sudden cardiac death in national collegiate athletic association athletes. Circ Arrhythm Electrophysiol. 2014;7:198–204. doi: 10.1161/CIRCEP.113.001376. [DOI] [PubMed] [Google Scholar]
- 72.de Noronha SV, Sharma S, Papadakis M, Desai S, Whyte G, Sheppard MN. Aetiology of sudden cardiac death in athletes in the united kingdom: A pathological study. Heart. 2009;95:1409–1414. doi: 10.1136/hrt.2009.168369. [DOI] [PubMed] [Google Scholar]
- 73.Suárez-Mier MP, Aguilera B, Mosquera RM, Sánchez-de-León MS. Pathology of sudden death during recreational sports in spain. Forensic Sci Int. 2013;226:188–196. doi: 10.1016/j.forsciint.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 74.Maron BJ, Chaitman BR, Ackerman MJ, Bayes de Luna A, Corrado D, Crosson JE, Deal BJ, Driscoll DJ, Estes NA, 3rd, Araujo CG, Liang DH, Mitten MJ, Myerburg RJ, Pelliccia A, Thompson PD, Towbin JA, Van Camp SP. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109:2807–2816. doi: 10.1161/01.CIR.0000128363.85581.E1. [DOI] [PubMed] [Google Scholar]
- 75.Pelliccia A, Fagard R, Bjørnstad HH, Anastassakis A, Arbustini E, Assanelli D, Biffi A, Borjesson M, Carrè F, Corrado D, Delise P, Dorwarth U, Hirth A, Heidbuchel H, Hoffmann E, Mellwig KP, Panhuyzen-Goedkoop N, Pisani A, Solberg EE, van-Buuren F, Vanhees L, Blomstrom-Lundqvist C, Deligiannis A, Dugmore D, Glikson M, Hoff PI, Hoffmann A, Horstkotte D, Nordrehaug JE, Oudhof J, McKenna WJ, Penco M, Priori S, Reybrouck T, Senden J, Spataro A, Thiene G, Physiology SGoSCotWGoCRaE, Cardiology WGoMaPDotESo Recommendations for competitive sports participation in athletes with cardiovascular disease: A consensus document from the study group of sports cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the european society of cardiology. Eur Heart J. 2005;26:1422–1445. doi: 10.1093/eurheartj/ehi325. [DOI] [PubMed] [Google Scholar]
- 76.Paterick TE, Paterick TJ, Fletcher GF, Maron BJ. Medical and legal issues in the cardiovascular evaluation of competitive athletes. JAMA. 2005;294:3011–3018. doi: 10.1001/jama.294.23.3011. [DOI] [PubMed] [Google Scholar]
- 77.Lampert R, Olshansky B, Heidbuchel H, Lawless C, Saarel E, Ackerman M, Calkins H, Estes NA, Link MS, Maron BJ, Marcus F, Scheinman M, Wilkoff BL, Zipes DP, Berul CI, Cheng A, Law I, Loomis M, Barth C, Brandt C, Dziura J, Li F, Cannom D. Safety of sports for athletes with implantable cardioverter-defibrillators: Results of a prospective, multinational registry. Circulation. 2013;127:2021–2030. doi: 10.1161/CIRCULATIONAHA.112.000447. [DOI] [PubMed] [Google Scholar]
- 78.Johnson JN, Ackerman MJ. Competitive sports participation in athletes with congenital long qt syndrome. JAMA. 2012;308:764–765. doi: 10.1001/jama.2012.9334. [DOI] [PubMed] [Google Scholar]
- 79.Lim PO, Morris-Thurgood JA, Frenneaux MP. Vascular mechanisms of sudden death in hypertrophic cardiomyopathy, including blood pressure responses to exercise. Cardiol Rev. 2002;10:15–23. doi: 10.1097/00045415-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 80.Sakaguchi T, Shimizu W, Itoh H, Noda T, Miyamoto Y, Nagaoka I, Oka Y, Ashihara T, Ito M, Tsuji K, Ohno S, Makiyama T, Kamakura S, Horie M. Age- and genotype-specific triggers for life-threatening arrhythmia in the genotyped long qt syndrome. J Cardiovasc Electrophysiol. 2008;19:794–799. doi: 10.1111/j.1540-8167.2008.01138.x. [DOI] [PubMed] [Google Scholar]
- 81.Zorzi A, ElMaghawry M, Rigato I, Cardoso Bianchini F, Crespi Ponta G, Michieli P, Migliore F, Perazzolo Marra M, Bauce B, Basso C, Schiavon M, Thiene G, Iliceto S, Corrado D. Exercise-induced normalization of right precordial negative t waves in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. 2013;112:411–415. doi: 10.1016/j.amjcard.2013.03.048. [DOI] [PubMed] [Google Scholar]
- 82.Shimizu T, Iwaya S, Suzuki S, Sakamoto N, Sugimoto K, Nakazato K, Suzuki H, Nishimura T, Takahashi Y, Saito S, Takeishi Y. Sudden cardiac arrest associated with an anomalous aortic origin of the left coronary artery from the opposite sinus of valsalva. Intern Med. 2014;53:2601–2604. doi: 10.2169/internalmedicine.53.2676. [DOI] [PubMed] [Google Scholar]
- 83.De Giorgi A, Achilli F, Fabbian F, Pala M, Menegatti AM, Malagoni AM, Manfredini F, Manfredini R. Sudden death in competitive athletes: Does a circadian variation in occurrence exist? Am J Emerg Med. 2012;30:1306–1309. doi: 10.1016/j.ajem.2012.04.027. doi: 1310.1016/j.ajem.2012.1304.1027. Epub 2012 Jul 1312. [DOI] [PubMed] [Google Scholar]
- 84.Risgaard B, Winkel BG, Jabbari R, Glinge C, Ingemann-Hansen O, Thomsen JL, Ottesen GL, Haunsø S, Holst AG, Tfelt-Hansen J. Sports-related sudden cardiac death in a competitive and a noncompetitive athlete population aged 12 to 49 years: Data from an unselected nationwide study in denmark. Heart Rhythm. 2014;11:1673–1681. doi: 10.1016/j.hrthm.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 85.Gow RM, Borghese MM, Honeywell CR, Colley RC. Activity intensity during free-living activities in children and adolescents with inherited arrhythmia syndromes: Assessment by combined accelerometer and heart rate monitor. Circ Arrhythm Electrophysiol. 2013;6:939–945. doi: 10.1161/CIRCEP.113.000514. [DOI] [PubMed] [Google Scholar]
- 86.Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276:199–204. [PubMed] [Google Scholar]
- 87.Maron BJ, Semsarian C, Shen WK, Link MS, Epstein AE, Estes NA, 3rd, Almquist A, Giudici MC, Haas TS, Hodges JS, Spirito P. Circadian patterns in the occurrence of malignant ventricular tachyarrhythmias triggering defibrillator interventions in patients with hypertrophic cardiomyopathy. Heart Rhythm. 2009;6:599–602. doi: 10.1016/j.hrthm.2009.02.007. doi: 510.1016/j.hrthm.2009.1002.1007. Epub 2009 Feb 1012. [DOI] [PubMed] [Google Scholar]
- 88.Corrado D, Basso C, Schiavon M, Pelliccia A, Thiene G. Pre-participation screening of young competitive athletes for prevention of sudden cardiac death. J Am Coll Cardiol. 2008;52:1981–1989. doi: 10.1016/j.jacc.2008.06.053. [DOI] [PubMed] [Google Scholar]
- 89.Steinvil A, Chundadze T, Zeltser D, Rogowski O, Halkin A, Galily Y, Perluk H, Viskin S. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death proven fact or wishful thinking? J Am Coll Cardiol. 2011;57:1291–1296. doi: 10.1016/j.jacc.2010.10.037. doi: 1210.1016/j.jacc.2010.1210.1037. [DOI] [PubMed] [Google Scholar]
- 90.Maron BJ, Haas TS, Ahluwalia A, Rutten-Ramos SC. Incidence of cardiovascular sudden deaths in minnesota high school athletes. Heart Rhythm. 2013;10:374–377. doi: 10.1016/j.hrthm.2012.11.024. doi: 310.1016/j.hrthm.2012.1011.1024. Epub 2012 Dec 1011. [DOI] [PubMed] [Google Scholar]
- 91.Maron BJ, Gohman TE, Kyle SB, Estes NA, Link MS. Clinical profile and spectrum of commotio cordis. JAMA. 2002;287:1142–1146. doi: 10.1001/jama.287.9.1142. [DOI] [PubMed] [Google Scholar]
- 92.Link MS. Pathophysiology, prevention, and treatment of commotio cordis. Curr Cardiol Rep. 2014;16:495. doi: 10.1007/s11886-014-0495-2. doi: 410.1007/s11886-11014-10495-11882. [DOI] [PubMed] [Google Scholar]
- 93.Maron BJ, Doerer JJ, Haas TS, Estes NA, Hodges JS, Link MS. Commotio cordis and the epidemiology of sudden death in competitive lacrosse. Pediatrics. 2009;124:966–971. doi: 10.1542/peds.2009-0167. doi: 910.1542/peds.2009-0167. Epub 2009 Aug 1510. [DOI] [PubMed] [Google Scholar]
- 94.Maron BJ, Ahluwalia A, Haas TS, Semsarian C, Link MS, Estes NA. Global epidemiology and demographics of commotio cordis. Heart Rhythm. 2011;8:1969–1971. doi: 10.1016/j.hrthm.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 95.(CDC) CfDCaP Mental health in the united states. Prevalence of diagnosis and medication treatment for attention-deficit/hyperactivity disorder--united states, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:842–847. [PubMed] [Google Scholar]
- 96.Findling RL, Short EJ, Manos MJ. Short-term cardiovascular effects of methylphenidate and adderall. J Am Acad Child Adolesc Psychiatry. 2001;40:525–529. doi: 10.1097/00004583-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 97.Samuels JA, Franco K, Wan F, Sorof JM. Effect of stimulants on 24-h ambulatory blood pressure in children with adhd: A double-blind, randomized, cross-over trial. Pediatr Nephrol. 2006;21:92–95. doi: 10.1007/s00467-005-2051-1. [DOI] [PubMed] [Google Scholar]
- 98.Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, Murray KT, Quinn VP, Stein CM, Callahan ST, Fireman BH, Fish FA, Kirshner HS, O'Duffy A, Connell FA, Ray WA. Adhd drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896–1904. doi: 10.1056/NEJMoa1110212. doi: 1810.1056/NEJMoa1110212. Epub 1112011 Nov 1110211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schelleman H, Bilker WB, Strom BL, Kimmel SE, Newcomb C, Guevara JP, Daniel GW, Cziraky MJ, Hennessy S. Cardiovascular events and death in children exposed and unexposed to adhd agents. Pediatrics. 2011;127:1102–1110. doi: 10.1542/peds.2010-3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang C, Kutyifa V, Moss AJ, McNitt S, Zareba W, Kaufman ES. Long-qt syndrome and therapy for attention deficit/hyperactivity disorder. J Cardiovasc Electrophysiol. 2015;26:1039–1044. doi: 10.1111/jce.12739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rohatgi RK, Bos JM, Ackerman MJ. Stimulant therapy in children with attention-deficit/hyperactivity disorder and concomitant long qt syndrome: A safe combination? Heart Rhythm. 2015;12:1807–1812. doi: 10.1016/j.hrthm.2015.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Berul CI. Implantable cardioverter defibrillator criteria for primary and secondary prevention of pediatric sudden cardiac death. Pacing Clin Electrophysiol. 2009;32:S67–70. doi: 10.1111/j.1540-8159.2009.02388.x. doi: 10.1111/j.1540-8159.2009.02388.x. [DOI] [PubMed] [Google Scholar]
- 103.Friedman KG, Alexander ME. Chest pain and syncope in children: A practical approach to the diagnosis of cardiac disease. J Pediatr. 2013;163:896–901.e891-893. doi: 10.1016/j.jpeds.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tretter JT, Kavey RE. Distinguishing cardiac syncope from vasovagal syncope in a referral population. J Pediatr. 2013;163:1618–1623.e1611. doi: 10.1016/j.jpeds.2013.07.023. [DOI] [PubMed] [Google Scholar]
- 105.Kaltman JR, Thompson PD, Lantos J, Berul CI, Botkin J, Cohen JT, Cook NR, Corrado D, Drezner J, Frick KD, Goldman S, Hlatky M, Kannankeril PJ, Leslie L, Priori S, Saul JP, Shapiro-Mendoza CK, Siscovick D, Vetter VL, Boineau R, Burns KM, Friedman RA. Screening for sudden cardiac death in the young: Report from a national heart, lung, and blood institute working group. Circulation. 2011;123:1911–1918. doi: 10.1161/CIRCULATIONAHA.110.017228. doi: 1910.1161/CIRCULATIONAHA.1110.017228. [DOI] [PubMed] [Google Scholar]
- 106.Mahle WT, Sable CA, Matherne PG, Gaynor JW, Gewitz MH. Key concepts in the evaluation of screening approaches for heart disease in children and adolescents: A science advisory from the american heart association. Circulation. 2012;125:2796–2801. doi: 10.1161/CIR.0b013e3182579f25. doi: 2710.1161/CIR.2790b2013e3182579f3182525. Epub 3182012 Apr 3182530. [DOI] [PubMed] [Google Scholar]
- 107.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D, Methods Work Group TiUPSTF Current methods of the us preventive services task force: A review of the process. Am J Prev Med. 2001;20:21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 108.Anderson JB, Grenier M, Edwards NM, Madsen NL, Czosek RJ, Spar DS, Barnes A, Pratt J, King E, Knilans TK. Usefulness of combined history, physical examination, electrocardiogram, and limited echocardiogram in screening adolescent athletes for risk for sudden cardiac death. Am J Cardiol. 2014;114:1763–1767. doi: 10.1016/j.amjcard.2014.09.011. doi: 1710.1016/j.amjcard.2014.1709.1011. Epub 2014 Sep 1717. [DOI] [PubMed] [Google Scholar]
- 109.Chandra N, Bastiaenen R, Papadakis M, Panoulas VF, Ghani S, Duschl J, Foldes D, Raju H, Osborne R, Sharma S. Prevalence of electrocardiographic anomalies in young individuals: Relevance to a nationwide cardiac screening program. J Am Coll Cardiol. 2014;63:2028–2034. doi: 10.1016/j.jacc.2014.01.046. [DOI] [PubMed] [Google Scholar]
- 110.Coris EE, Sahebzamani F, Curtis A, Jennings J, Walz SM, Nugent D, Reese E, Zwygart KK, Konin JG, Pescasio M, Drezner JA. Preparticipation cardiovascular screening among national collegiate athletic association division i institutions. Br J Sports Med. 2013;47:182–184. doi: 10.1136/bjsports-2012-091356. [DOI] [PubMed] [Google Scholar]
- 111.Charboneau ML, Mencias T, Hoch AZ. Cardiovascular screening practices in collegiate student-athletes. PM R. 2014;6:583–586. doi: 10.1016/j.pmrj.2013.12.014. quiz 586. [DOI] [PubMed] [Google Scholar]
- 112.Fudge J, Harmon KG, Owens DS, Prutkin JM, Salerno JC, Asif IM, Haruta A, Pelto H, Rao AL, Toresdahl BG, Drezner JA. Cardiovascular screening in adolescents and young adults: A prospective study comparing the pre-participation physical evaluation monograph 4th edition and ecg. Br J Sports Med. 2014;48:1172–1178. doi: 10.1136/bjsports-2014-093840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vetter VL, Dugan N, Guo R, Mercer-Rosa L, Gleason M, Cohen M, Vogel RL, Iyer R. A pilot study of the feasibility of heart screening for sudden cardiac arrest in healthy children. Am Heart J. 2011;161:1000–1006.e1003. doi: 10.1016/j.ahj.2011.01.022. doi: 1010.1016/j.ahj.2011.1001.1022. Epub 2011 Mar 1012. [DOI] [PubMed] [Google Scholar]
- 114.Zeltser I, Cannon B, Silvana L, Fenrich A, George J, Schleifer J, Garcia M, Barnes A, Rivenes S, Patt H, Rodgers G, Scott W. Lessons learned from preparticipation cardiovascular screening in a state funded program. Am J Cardiol. 2012;110:902–908. doi: 10.1016/j.amjcard.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 115.Asif IM, Price D, Harmon KG, Salerno JC, Rao AL, Drezner JA. The psychological impact of cardiovascular screening in young athletes: Perspectives across age, race, and gender. Clin J Sport Med. 2015;25:464–71. doi: 10.1097/JSM.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 116.Baggish AL, Hutter AM, Wang F, Yared K, Weiner RB, Kupperman E, Picard MH, Wood MJ. Cardiovascular screening in college athletes with and without electrocardiography: A cross-sectional study. Ann Intern Med. 2010;152:269–275. doi: 10.7326/0003-4819-152-5-201003020-00004. [DOI] [PubMed] [Google Scholar]
- 117.Leslie LK, Cohen JT, Newburger JW, Alexander ME, Wong JB, Sherwin ED, Rodday AM, Parsons SK, Triedman JK. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125:2621–2629. doi: 10.1161/CIRCULATIONAHA.111.087940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rodday AM, Triedman JK, Alexander ME, Cohen JT, Ip S, Newburger JW, Parsons SK, Trikalinos TA, Wong JB, Leslie LK. Electrocardiogram screening for disorders that cause sudden cardiac death in asymptomatic children: A meta-analysis. Pediatrics. 2012;129:e999–1010. doi: 10.1542/peds.2011-0643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Riding NR, Sheikh N, Adamuz C, Watt V, Farooq A, Whyte GP, George KP, Drezner JA, Sharma S, Wilson MG. Comparison of three current sets of electrocardiographic interpretation criteria for use in screening athletes. Heart. 2015;101:384–390. doi: 10.1136/heartjnl-2014-306437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pickham D, Zarafshar S, Sani D, Kumar N, Froelicher V. Comparison of three ecg criteria for athlete pre-participation screening. J Electrocardiol. 2014;47:769–774. doi: 10.1016/j.jelectrocard.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 121.Saul JP, Schwartz PJ, Ackerman MJ, Triedman JK. Rationale and objectives for ecg screening in infancy. Heart Rhythm. 2014;11:2316–2321. doi: 10.1016/j.hrthm.2014.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fuller CM. Cost effectiveness analysis of screening of high school athletes for risk of sudden cardiac death. Med Sci Sports Exerc. 2000;32:887–890. doi: 10.1097/00005768-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 123.Zupancic JA, Triedman JK, Alexander M, Walsh EP, Richardson DK, Berul CI. Cost-effectiveness and implications of newborn screening for prolongation of qt interval for the prevention of sudden infant death syndrome. J Pediatr. 2000;136:481–489. doi: 10.1016/s0022-3476(00)90011-8. [DOI] [PubMed] [Google Scholar]
- 124.Quaglini S, Rognoni C, Spazzolini C, Priori SG, Mannarino S, Schwartz PJ. Cost-effectiveness of neonatal ecg screening for the long qt syndrome. Eur Heart J. 2006;27:1824–1832. doi: 10.1093/eurheartj/ehl115. [DOI] [PubMed] [Google Scholar]
- 125.Denchev P, Kaltman JR, Schoenbaum M, Vitiello B. Modeled economic evaluation of alternative strategies to reduce sudden cardiac death among children treated for attention deficit/hyperactivity disorder. Circulation. 2010;121:1329–1337. doi: 10.1161/CIRCULATIONAHA.109.901256. [DOI] [PubMed] [Google Scholar]
- 126.Wheeler MT, Heidenreich PA, Froelicher VF, Hlatky MA, Ashley EA. Cost-effectiveness of preparticipation screening for prevention of sudden cardiac death in young athletes. Ann Intern Med. 2010;152:276–286. doi: 10.1059/0003-4819-152-5-201003020-00005. doi: 210.7326/0003-4819-7152-7325-201003020-201000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Schoenbaum M, Denchev P, Vitiello B, Kaltman JR. Economic evaluation of strategies to reduce sudden cardiac death in young athletes. Pediatrics. 2012;130:e380–389. doi: 10.1542/peds.2011-3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Halkin A, Steinvil A, Rosso R, Adler A, Rozovski U, Viskin S. Preventing sudden death of athletes with electrocardiographic screening: What is the absolute benefit and how much will it cost? J Am Coll Cardiol. 2012;60:2271–2276. doi: 10.1016/j.jacc.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 129.Menafoglio A, Di Valentino M, Segatto JM, Siragusa P, Pezzoli R, Maggi M, Romano GA, Moschovitis G, Wilhelm M, Gallino A. Costs and yield of a 15-month preparticipation cardiovascular examination with ecg in 1070 young athletes in switzerland: Implications for routine ecg screening. Br J Sports Med. 2014;48:1157–1161. doi: 10.1136/bjsports-2013-092929. [DOI] [PubMed] [Google Scholar]
- 130.Skinner JR, Van Hare GF. Routine ecg screening in infancy and early childhood should not be performed. Heart Rhythm. 2014;11:2322–2327. doi: 10.1016/j.hrthm.2014.09.046. [DOI] [PubMed] [Google Scholar]
- 131.Hill AC, Miyake CY, Grady S, Dubin AM. Accuracy of interpretation of preparticipation screening electrocardiograms. J Pediatr. 2011;159:783–788. doi: 10.1016/j.jpeds.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 132.Berte B, Duytschaever M, Elices J, Kataria V, Timmers L, Van Heuverswyn F, Stroobandt R, De Neve J, Watteyne K, Vandensteen E, Vandekerckhove Y, Tavernier R. Variability in interpretation of the electrocardiogram in young athletes: An unrecognized obstacle for electrocardiogram-based screening protocols. Europace. 2015;17:1435–40. doi: 10.1093/europace/euu385. [DOI] [PubMed] [Google Scholar]
- 133.Brosnan M, La Gerche A, Kumar S, Lo W, Kalman J, Prior D. Modest agreement in ecg interpretation limits the application of ecg screening in young athletes. Heart Rhythm. 2015;12:130–136. doi: 10.1016/j.hrthm.2014.09.060. [DOI] [PubMed] [Google Scholar]
- 134.Earle N, Crawford J, Smith W, Hayes I, Shelling A, Hood M, Stiles M, Maxwell F, Heaven D, Love DR, Skinner JR. Community detection of long qt syndrome with a clinical registry: An alternative to ecg screening programs? Heart Rhythm. 2013;10:233–238. doi: 10.1016/j.hrthm.2012.10.043. doi: 210.1016/j.hrthm.2012.1010.1043. Epub 2012 Nov 1011. [DOI] [PubMed] [Google Scholar]
- 135.Baruteau AE, Baruteau J, Joomye R, Martins R, Treguer F, Baruteau R, Daubert JC, Mabo P, Roussey M. Role of congenital long-qt syndrome in unexplained sudden infant death: Proposal for an electrocardiographic screening in relatives. Eur J Pediatr. 2009;168:771–777. doi: 10.1007/s00431-009-0951-y. [DOI] [PubMed] [Google Scholar]
- 136.Behr ER, Dalageorgou C, Christiansen M, Syrris P, Hughes S, Tome Esteban MT, Rowland E, Jeffery S, McKenna WJ. Sudden arrhythmic death syndrome: Familial evaluation identifies inheritable heart disease in the majority of families. Eur Heart J. 2008;29:1670–1680. doi: 10.1093/eurheartj/ehn219. [DOI] [PubMed] [Google Scholar]
- 137.Kumar S, Peters S, Thompson T, Morgan N, Maccicoca I, Trainer A, Zentner D, Kalman JM, Winship I, Vohra JK. Familial cardiological and targeted genetic evaluation: Low yield in sudden unexplained death and high yield in unexplained cardiac arrest syndromes. Heart Rhythm. 2013;10:1653–1660. doi: 10.1016/j.hrthm.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 138.Tan HL, Hofman N, van Langen IM, van der Wal AC, Wilde AA. Sudden unexplained death: Heritability and diagnostic yield of cardiological and genetic examination in surviving relatives. Circulation. 2005;112:207–213. doi: 10.1161/CIRCULATIONAHA.104.522581. [DOI] [PubMed] [Google Scholar]
- 139.Wong LC, Roses-Noguer F, Till JA, Behr ER. Cardiac evaluation of pediatric relatives in sudden arrhythmic death syndrome: A 2-center experience. Circ Arrhythm Electrophysiol. 2014;7:800–806. doi: 10.1161/CIRCEP.114.001818. [DOI] [PubMed] [Google Scholar]
- 140.van der Werf C, Stiekema L, Tan HL, Hofman N, Alders M, van der Wal AC, van Langen IM, Wilde AA. Low rate of cardiac events in first-degree relatives of diagnosis-negative young sudden unexplained death syndrome victims during follow-up. Heart Rhythm. 2014;11:1728–1732. doi: 10.1016/j.hrthm.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 141.Wilms HR, Midgley DJ, Morrow P, Stables S, Crawford J, Skinner JR. Evaluation of autopsy and police reports in the investigation of sudden unexplained death in the young. Forensic Sci Med Pathol. 2012;8:380–389. doi: 10.1007/s12024-012-9340-3. doi: 310.1007/s12024-12012-19340-12023. Epub 12012 May 12022. [DOI] [PubMed] [Google Scholar]
- 142.Basso C, Carturan E, Pilichou K, Rizzo S, Corrado D, Thiene G. Sudden cardiac death with normal heart: Molecular autopsy. Cardiovasc Pathol. 2010;19:321–325. doi: 10.1016/j.carpath.2010.02.003. doi: 310.1016/j.carpath.2010.1002.1003. Epub 2010 Apr 1019. [DOI] [PubMed] [Google Scholar]
- 143.Tester DJ, Ackerman MJ. The molecular autopsy: Should the evaluation continue after the funeral? Pediatr Cardiol. 2012;33:461–470. doi: 10.1007/s00246-012-0160-8. doi: 410.1007/s00246-00012-00160-00248. Epub 02012 Feb 00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ackerman MJ. State of postmortem genetic testing known as the cardiac channel molecular autopsy in the forensic evaluation of unexplained sudden cardiac death in the young. Pacing Clin Electrophysiol. 2009;32:S86–89. doi: 10.1111/j.1540-8159.2009.02393.x. doi: 10.1111/j.1540-8159.2009.02393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Tester D, Ackerman M. Forensic pathology of infancy and childhood. Springer Publishing; New York, NY: 2014. [Google Scholar]
- 146.Glengarry JM, Crawford J, Morrow PL, Stables SR, Love DR, Skinner JR. Long qt molecular autopsy in sudden infant death syndrome. Arch Dis Child. 2014;99:635–640. doi: 10.1136/archdischild-2013-305331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Loporcaro CG, Tester DJ, Maleszewski JJ, Kruisselbrink T, Ackerman MJ. Confirmation of cause and manner of death via a comprehensive cardiac autopsy including whole exome next-generation sequencing. Arch Pathol Lab Med. 2014;138:1083–1089. doi: 10.5858/arpa.2013-0479-SA. [DOI] [PubMed] [Google Scholar]
- 148.Carturan E, Tester DJ, Brost BC, Basso C, Thiene G, Ackerman MJ. Postmortem genetic testing for conventional autopsy-negative sudden unexplained death: An evaluation of different dna extraction protocols and the feasibility of mutational analysis from archival paraffin-embedded heart tissue. Am J Clin Pathol. 2008;129:391–397. doi: 10.1309/VLA7TT9EQ05FFVN4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 150.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The antiarrhythmics versus implantable defibrillators (avid) investigators. N Engl J Med. 1997;337:1576–1583. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 151.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, Investigators SCDiHFTS-H Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 152.Berul CI, Van Hare GF, Kertesz NJ, Dubin AM, Cecchin F, Collins KK, Cannon BC, Alexander ME, Triedman JK, Walsh EP, Friedman RA. Results of a multicenter retrospective implantable cardioverter-defibrillator registry of pediatric and congenital heart disease patients. J Am Coll Cardiol. 2008;51:1685–1691. doi: 10.1016/j.jacc.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 153.DeWitt ES, Triedman JK, Cecchin F, Mah DY, Abrams DJ, Walsh EP, Gauvreau K, Alexander ME. Time dependence of risks and benefits in pediatric primary prevention implantable cardioverter-defibrillator therapy. Circ Arrhythm Electrophysiol. 2014;7:1057–1063. doi: 10.1161/CIRCEP.114.001569. [DOI] [PubMed] [Google Scholar]
- 154.Medicine Io . Strategies to improve cardiac arrest survival: a time to act. The National Academies Press; Washington, DC: 2015. [PubMed] [Google Scholar]
- 155.Johnson MA, Grahan BJ, Haukoos JS, McNally B, Campbell R, Sasson C, Slattery DE. Demographics, bystander cpr, and aed use in out-of-hospital pediatric arrests. Resuscitation. 2014;85:920–926. doi: 10.1016/j.resuscitation.2014.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: A 3-phase time-sensitive model. JAMA. 2002;288:3035–3038. doi: 10.1001/jama.288.23.3035. [DOI] [PubMed] [Google Scholar]
- 157.Myerburg RJ, Fenster J, Velez M, Rosenberg D, Lai S, Kurlansky P, Newton S, Knox M, Castellanos A. Impact of community-wide police car deployment of automated external defibrillators on survival from out-of-hospital cardiac arrest. Circulation. 2002;106:1058–1064. doi: 10.1161/01.cir.0000028147.92190.a7. [DOI] [PubMed] [Google Scholar]
- 158.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–1247. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 159.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M, Investigators PADT Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 160.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, Abella BS, Kleinman ME, Edelson DP, Berg RA, Aufderheide TP, Menon V, Leary M, CPR Quality Summit Investigators tAHAECCC, and the Council on Cardiopulmonary, Critical Care, P.rioperative and Resuscitation Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the american heart association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 161.Garcia LA, Allan JJ, Kerber RE. Interactions between cpr and defibrillation waveforms: Effect on resumption of a perfusing rhythm after defibrillation. Resuscitation. 2000;47:301–305. doi: 10.1016/s0300-9572(00)00244-6. [DOI] [PubMed] [Google Scholar]
- 162.Cobb LA, Fahrenbruch CE, Walsh TR, Copass MK, Olsufka M, Breskin M, Hallstrom AP. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA. 1999;281:1182–1188. doi: 10.1001/jama.281.13.1182. [DOI] [PubMed] [Google Scholar]
- 163.Yu T, Weil MH, Tang W, Sun S, Klouche K, Povoas H, Bisera J. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation. 2002;106:368–372. doi: 10.1161/01.cir.0000021429.22005.2e. [DOI] [PubMed] [Google Scholar]
- 164.Eftestøl T, Wik L, Sunde K, Steen PA. Effects of cardiopulmonary resuscitation on predictors of ventricular fibrillation defibrillation success during out-of-hospital cardiac arrest. Circulation. 2004;110:10–15. doi: 10.1161/01.CIR.0000133323.15565.75. [DOI] [PubMed] [Google Scholar]
- 165.Olasveengen TM, Lund-Kordahl I, Steen PA, Sunde K. Out-of hospital advanced life support with or without a physician: Effects on quality of cpr and outcome. Resuscitation. 2009;80:1248–1252. doi: 10.1016/j.resuscitation.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 166.Halperin HR, Tsitlik JE, Guerci AD, Mellits ED, Levin HR, Shi AY, Chandra N, Weisfeldt ML. Determinants of blood flow to vital organs during cardiopulmonary resuscitation in dogs. Circulation. 1986;73:539–550. doi: 10.1161/01.cir.73.3.539. [DOI] [PubMed] [Google Scholar]
- 167.Rudikoff MT, Maughan WL, Effron M, Freund P, Weisfeldt ML. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation. 1980;61:345–352. doi: 10.1161/01.cir.61.2.345. [DOI] [PubMed] [Google Scholar]
- 168.KOUWENHOVEN WB, JUDE JR, KNICKERBOCKER GG. Closed-chest cardiac massage. JAMA. 1960;173:1064–1067. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 169.Michael JR, Guerci AD, Koehler RC, Shi AY, Tsitlik J, Chandra N, Niedermeyer E, Rogers MC, Traystman RJ, Weisfeldt ML. Mechanisms by which epinephrine augments cerebral and myocardial perfusion during cardiopulmonary resuscitation in dogs. Circulation. 1984;69:822–835. doi: 10.1161/01.cir.69.4.822. [DOI] [PubMed] [Google Scholar]
- 170.Eleff SM, Kim H, Shaffner DH, Traystman RJ, Koehler RC. Effect of cerebral blood flow generated during cardiopulmonary resuscitation in dogs on maintenance versus recovery of atp and ph. Stroke. 1993;24:2066–2073. doi: 10.1161/01.str.24.12.2066. [DOI] [PubMed] [Google Scholar]
- 171.Eleff SM, Schleien CL, Koehler RC, Shaffner DH, Tsitlik J, Halperin HR, Rogers MC, Traystman RJ. Brain bioenergetics during cardiopulmonary resuscitation in dogs. Anesthesiology. 1992;76:77–84. doi: 10.1097/00000542-199201000-00012. [DOI] [PubMed] [Google Scholar]
- 172.Berg RA, Sanders AB, Kern KB, Hilwig RW, Heidenreich JW, Porter ME, Ewy GA. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104:2465–2470. doi: 10.1161/hc4501.098926. [DOI] [PubMed] [Google Scholar]
- 173.Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M, Nowak RM. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA. 1990;263:1106–1113. [PubMed] [Google Scholar]
- 174.Kern KB, de la Guardia B, Ewy GA. Myocardial perfusion during cardiopulmonary resuscitation (cpr): Effects of 10, 25 and 50% coronary stenoses. Resuscitation. 1998;38:107–111. doi: 10.1016/s0300-9572(98)00089-6. [DOI] [PubMed] [Google Scholar]
- 175.Ewy GA. Cardiocerebral resuscitation: The new cardiopulmonary resuscitation. Circulation. 2005;111:2134–2142. doi: 10.1161/01.CIR.0000162503.57657.FA. [DOI] [PubMed] [Google Scholar]
- 176.Yannopoulos D, McKnite S, Aufderheide TP, Sigurdsson G, Pirrallo RG, Benditt D, Lurie KG. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64:363–372. doi: 10.1016/j.resuscitation.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 177.Zuercher M, Hilwig RW, Ranger-Moore J, Nysaether J, Nadkarni VM, Berg MD, Kern KB, Sutton R, Berg RA. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit Care Med. 2010;38:1141–1146. doi: 10.1097/CCM.0b013e3181ce1fe2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Glatz AC, Nishisaki A, Niles DE, Hanna BD, Eilevstjonn J, Diaz LK, Gillespie MJ, Rome JJ, Sutton RM, Berg RA, Nadkarni VM. Sternal wall pressure comparable to leaning during cpr impacts intrathoracic pressure and haemodynamics in anaesthetized children during cardiac catheterization. Resuscitation. 2013;84:1674–1679. doi: 10.1016/j.resuscitation.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 179.Niles DE, Sutton RM, Nadkarni VM, Glatz A, Zuercher M, Maltese MR, Eilevstjønn J, Abella BS, Becker LB, Berg RA. Prevalence and hemodynamic effects of leaning during cpr. Resuscitation. 2011;82(Suppl 2):S23–26. doi: 10.1016/S0300-9572(11)70147-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wolfe JA, Maier GW, Newton JR, Glower DD, Tyson GS, Spratt JA, Rankin JS, Olsen CO. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988;95:523–532. [PubMed] [Google Scholar]
- 181.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, Bigham B, Morrison LJ, Larsen J, Hess E, Vaillancourt C, Davis DP, Callaway CW, Investigators ROCR What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40:1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Monsieurs KG, De Regge M, Vansteelandt K, De Smet J, Annaert E, Lemoyne S, Kalmar AF, Calle PA. Excessive chest compression rate is associated with insufficient compression depth in prehospital cardiac arrest. Resuscitation. 2012;83:1319–1323. doi: 10.1016/j.resuscitation.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 183.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D, Aufderheide TP, Idris A, Stouffer JA, Stiell I, Berg R, Investigators ROC Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Vaillancourt C, Everson-Stewart S, Christenson J, Andrusiek D, Powell J, Nichol G, Cheskes S, Aufderheide TP, Berg R, Stiell IG, Investigators ROC The impact of increased chest compression fraction on return of spontaneous circulation for out-of-hospital cardiac arrest patients not in ventricular fibrillation. Resuscitation. 2011;82:1501–1507. doi: 10.1016/j.resuscitation.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sutton RM, Case E, Brown SP, Atkins DL, Nadkarni VM, Kaltman J, Callaway C, Idris A, Nichol G, Hutchison J, Drennan IR, Austin M, Daya M, Cheskes S, Nuttall J, Herren H, Christenson J, Andrusiek D, Vaillancourt C, Menegazzi JJ, Rea TD, Berg RA, Investigators R A quantitative analysis of out-of-hospital pediatric and adolescent resuscitation quality - a report from the roc epistry-cardiac arrest. Resuscitation. 2015;93:150–157. doi: 10.1016/j.resuscitation.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zipes DP, Fischer J, King RM, Nicoll A deB, Jolly WW. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. doi: 10.1016/0002-9149(75)90865-6. [DOI] [PubMed] [Google Scholar]
- 187.Shibata N, Chen PS, Dixon EG, Wolf PD, Danieley ND, Smith WM, Ideker RE. Influence of shock strength and timing on induction of ventricular arrhythmias in dogs. Am J Physiol. 1988;255:H891–901. doi: 10.1152/ajpheart.1988.255.4.H891. [DOI] [PubMed] [Google Scholar]
- 188.van Alem AP, Chapman FW, Lank P, Hart AA, Koster RW. A prospective, randomised and blinded comparison of first shock success of monophasic and biphasic waveforms in out-of-hospital cardiac arrest. Resuscitation. 2003;58:17–24. doi: 10.1016/s0300-9572(03)00106-0. [DOI] [PubMed] [Google Scholar]
- 189.Morrison LJ, Dorian P, Long J, Vermeulen M, Schwartz B, Sawadsky B, Frank J, Cameron B, Burgess R, Shield J, Bagley P, Mausz V, Brewer JE, Lerman BB, Steering Committee CVC, S.fety and Efficacy Committee Out-of-hospital cardiac arrest rectilinear biphasic to monophasic damped sine defibrillation waveforms with advanced life support intervention trial (orbit). Resuscitation. 2005;66:149–157. doi: 10.1016/j.resuscitation.2004.11.031. [DOI] [PubMed] [Google Scholar]
- 190.Kudenchuk PJ, Cobb LA, Copass MK, Olsufka M, Maynard C, Nichol G. Transthoracic incremental monophasic versus biphasic defibrillation by emergency responders (timber): A randomized comparison of monophasic with biphasic waveform ascending energy defibrillation for the resuscitation of out-of-hospital cardiac arrest due to ventricular fibrillation. Circulation. 2006;114:2010–2018. doi: 10.1161/CIRCULATIONAHA.106.636506. [DOI] [PubMed] [Google Scholar]
- 191.Schneider T, Martens PR, Paschen H, Kuisma M, Wolcke B, Gliner BE, Russell JK, Weaver WD, Bossaert L, Chamberlain D. Multicenter, randomized, controlled trial of 150-j biphasic shocks compared with 200- to 360-j monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized response to cardiac arrest (orca) investigators. Circulation. 2000;102:1780–1787. doi: 10.1161/01.cir.102.15.1780. [DOI] [PubMed] [Google Scholar]
- 192.Safar P, Brown TC, Holtey WJ. Failure of closed chest cardiac massage to produce pulmonary ventilation. Dis Chest. 1962;41:1–8. doi: 10.1378/chest.41.1.1. [DOI] [PubMed] [Google Scholar]
- 193.Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, von Briesen C, Sparks CW, Conrad CJ, Provo TA, Lurie KG. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 194.Kleinman ME, de Caen AR, Chameides L, Atkins DL, Berg RA, Berg MD, Bhanji F, Biarent D, Bingham R, Coovadia AH, Hazinski MF, Hickey RW, Nadkarni VM, Reis AG, Rodriguez-Nunez A, Tibballs J, Zaritsky AL, Zideman D, Collaborators PBaALSC Part 10: Pediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122:S466–515. doi: 10.1161/CIRCULATIONAHA.110.971093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: A randomized trial. Jama. 2009;302:2222–2229. doi: 10.1001/jama.2009.1729. [DOI] [PubMed] [Google Scholar]
- 196.Lin S, Callaway CW, Shah PS, Wagner JD, Beyene J, Ziegler CP, Morrison LJ. Adrenaline for out-of-hospital cardiac arrest resuscitation: A systematic review and meta-analysis of randomized controlled trials. Resuscitation. 2014;85:732–740. doi: 10.1016/j.resuscitation.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 197.Wenzel V, Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH, Group ERCVdCRS A comparison of vasopressin and epinephrine for out-of-hospital cardiopulmonary resuscitation. N Engl J Med. 2004;350:105–113. doi: 10.1056/NEJMoa025431. [DOI] [PubMed] [Google Scholar]
- 198.Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011;82:1138–1143. doi: 10.1016/j.resuscitation.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 199.Perkins GD, Cottrell P, Gates S. Is adrenaline safe and effective as a treatment for out of hospital cardiac arrest? BMJ. 2014;348:g2435. doi: 10.1136/bmj.g2435. [DOI] [PubMed] [Google Scholar]
- 200.Kudenchuk PJ, Cobb LA, Copass MK, Cummins RO, Doherty AM, Fahrenbruch CE, Hallstrom AP, Murray WA, Olsufka M, Walsh T. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;341:871–878. doi: 10.1056/NEJM199909163411203. [DOI] [PubMed] [Google Scholar]
- 201.Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002;346:884–890. doi: 10.1056/NEJMoa013029. [DOI] [PubMed] [Google Scholar]
- 202.Valdes SO, Donoghue AJ, Hoyme DB, Hammond R, Berg MD, Berg RA, Samson RA, Investigators AHAGWTG-R Outcomes associated with amiodarone and lidocaine in the treatment of in-hospital pediatric cardiac arrest with pulseless ventricular tachycardia or ventricular fibrillation. Resuscitation. 2014;85:381–386. doi: 10.1016/j.resuscitation.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Kudenchuk PJ, Brown SP, Daya M, Morrison LJ, Grunau BE, Rea T, Aufderheide T, Powell J, Leroux B, Vaillancourt C, Larsen J, Wittwer L, Colella MR, Stephens SW, Gamber M, Egan D, Dorian P, Investigators ROC Resuscitation outcomes consortium-amiodarone, lidocaine or placebo study (roc-alps): Rationale and methodology behind an out-of-hospital cardiac arrest antiarrhythmic drug trial. Am Heart J. 2014;167:653–659.e654. doi: 10.1016/j.ahj.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I, Investigators ROC Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, Hoffman P, Tynus K, Vanden Hoek TL, Becker LB. Chest compression rates during cardiopulmonary resuscitation are suboptimal: A prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 206.Idris AH, Guffey D, Pepe PE, Brown SP, Brooks SC, Callaway CW, Christenson J, Davis DP, Daya MR, Gray R, Kudenchuk PJ, Larsen J, Lin S, Menegazzi JJ, Sheehan K, Sopko G, Stiell I, Nichol G, Aufderheide TP, Investigators ROC Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015;43:840–848. doi: 10.1097/CCM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 207.Lammers RL, Willoughby-Byrwa M, Fales WD. Errors and error-producing conditions during a simulated, prehospital, pediatric cardiopulmonary arrest. Simul Healthc. 2014;9:174–183. doi: 10.1097/SIH.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 208.Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, Powell J, Daya M, Bigham BL, Atkins DL, Berg R, Davis D, Stiell I, Sopko G, Nichol G, Investigators ROCR Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125:3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Cheskes S, Schmicker RH, Verbeek PR, Salcido DD, Brown SP, Brooks S, Menegazzi JJ, Vaillancourt C, Powell J, May S, Berg RA, Sell R, Idris A, Kampp M, Schmidt T, Christenson J, investigators ROCR The impact of peri-shock pause on survival from out-of-hospital shockable cardiac arrest during the resuscitation outcomes consortium primed trial. Resuscitation. 2014;85:336–342. doi: 10.1016/j.resuscitation.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Aufderheide TP, Lurie KG. Death by hyperventilation: A common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32:S345–351. doi: 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 211.Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: Improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002;105:645–649. doi: 10.1161/hc0502.102963. [DOI] [PubMed] [Google Scholar]
- 212.Ewy GA, Zuercher M, Hilwig RW, Sanders AB, Berg RA, Otto CW, Hayes MM, Kern KB. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation. 2007;116:2525–2530. doi: 10.1161/CIRCULATIONAHA.107.711820. [DOI] [PubMed] [Google Scholar]
- 213.Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. N Engl J Med. 2000;342:1546–1553. doi: 10.1056/NEJM200005253422101. [DOI] [PubMed] [Google Scholar]
- 214.Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H. Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation. 2007;116:2900–2907. doi: 10.1161/CIRCULATIONAHA.107.723411. [DOI] [PubMed] [Google Scholar]
- 215.Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116:2908–2912. doi: 10.1161/CIRCULATIONAHA.107.710194. [DOI] [PubMed] [Google Scholar]
- 216.Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD, Committee AHAECC Hands-only (compression-only) cardiopulmonary resuscitation: A call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: A science advisory for the public from the american heart association emergency cardiovascular care committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 217.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk PJ, Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, Link MS, Morrison LJ, O'Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD, Vanden Hoek TL. Part 1: Executive summary: 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S640–656. doi: 10.1161/CIRCULATIONAHA.110.970889. [DOI] [PubMed] [Google Scholar]
- 218.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. Cpr training and cpr performance: Do cpr-trained bystanders perform cpr? Acad Emerg Med. 2006;13:596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 219.Stiell I, Nichol G, Wells G, De Maio V, Nesbitt L, Blackburn J, Spaite D, Group OS Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation. 2003;108:1939–1944. doi: 10.1161/01.CIR.0000095028.95929.B0. [DOI] [PubMed] [Google Scholar]
- 220.Ewy GA, Bobrow BJ. Cardiocerebral resuscitation: An approach to improving survival of patients with primary cardiac arrest. J Intensive Care Med. 2014;31:24–33. doi: 10.1177/0885066614544450. [DOI] [PubMed] [Google Scholar]
- 221.Iwami T, Kitamura T, Kiyohara K, Kawamura T. Dissemination of chest compression-only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation. 2015;132:415–422. doi: 10.1161/CIRCULATIONAHA.114.014905. [DOI] [PubMed] [Google Scholar]
- 222.Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, Berg RA, Hiraide A, Agency iwgfA-JURotFaDM Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: A prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347–1354. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- 223.Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: A graphic model. Ann Emerg Med. 1993;22:1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 224.Becker LB, Aufderheide TP, Graham R. Strategies to improve survival from cardiac arrest: A report from the institute of medicine. JAMA. 2015;314:223–224. doi: 10.1001/jama.2015.8454. [DOI] [PubMed] [Google Scholar]
- 225.Rea TD, Helbock M, Perry S, Garcia M, Cloyd D, Becker L, Eisenberg M. Increasing use of cardiopulmonary resuscitation during out-of-hospital ventricular fibrillation arrest: Survival implications of guideline changes. Circulation. 2006;114:2760–2765. doi: 10.1161/CIRCULATIONAHA.106.654715. [DOI] [PubMed] [Google Scholar]
- 226.Rea TD, Eisenberg MS, Becker LJ, Lima AR, Fahrenbruch CE, Copass MK, Cobb LA. Emergency medical services and mortality from heart disease: A community study. Ann Emerg Med. 2003;41:494–499. doi: 10.1067/mem.2003.149. [DOI] [PubMed] [Google Scholar]
- 227.Eisenberg MS, Horwood BT, Cummins RO, Reynolds-Haertle R, Hearne TR. Cardiac arrest and resuscitation: A tale of 29 cities. Ann Emerg Med. 1990;19:179–186. doi: 10.1016/s0196-0644(05)81805-0. [DOI] [PubMed] [Google Scholar]
- 228.Spaite DW, Bobrow BJ, Stolz U, Berg RA, Sanders AB, Kern KB, Chikani V, Humble W, Mullins T, Stapczynski JS, Ewy GA, Consortium ACRC Statewide regionalization of postarrest care for out-of-hospital cardiac arrest: Association with survival and neurologic outcome. Ann Emerg Med. 2014;64:496–506.e491. doi: 10.1016/j.annemergmed.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 229.Braithwaite S, Friesen JE, Hadley S, Kohls D, Hinchey PR, Prather M, Karonika M, Myers B, Holland WD, Eason CM, Carhart J. A tale of three successful ems systems. How coordinated “Pit crew” Procedures have helped improve cardiac arrest resuscitations in the field. JEMS. 2014;(Suppl):28–35. [PubMed] [Google Scholar]
- 230.Hinchey PR, Myers JB, Lewis R, De Maio VJ, Reyer E, Licatese D, Zalkin J, Snyder G, Consortium CCR. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 aha guidelines for compressions, ventilations, and induced hypothermia: The wake county experience. Ann Emerg Med. 2010;56:348–357. doi: 10.1016/j.annemergmed.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 231.Sasson C, Haukoos JS, Ben-Youssef L, Ramirez L, Bull S, Eigel B, Magid DJ, Padilla R. Barriers to calling 911 and learning and performing cardiopulmonary resuscitation for residents of primarily latino, high-risk neighborhoods in denver, colorado. Ann Emerg Med. 2015;65:545–552.e542. doi: 10.1016/j.annemergmed.2014.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA. Chest compression-only cpr by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 233.Nordberg P, Hollenberg J, Herlitz J, Rosenqvist M, Svensson L. Aspects on the increase in bystander cpr in sweden and its association with outcome. Resuscitation. 2009;80:329–333. doi: 10.1016/j.resuscitation.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 234.Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, Bloomingdale M, Subido C, Romines S, Eisenberg MS. Cpr with chest compression alone or with rescue breathing. N Engl J Med. 2010;363:423–433. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- 235.Akahane M, Ogawa T, Tanabe S, Koike S, Horiguchi H, Yasunaga H, Imamura T. Impact of telephone dispatcher assistance on the outcomes of pediatric out-of-hospital cardiac arrest. Crit Care Med. 2012;40:1410–1416. doi: 10.1097/CCM.0b013e31823e99ae. [DOI] [PubMed] [Google Scholar]
- 236.Akahane M, Tanabe S, Ogawa T, Koike S, Horiguchi H, Yasunaga H, Imamura T. Characteristics and outcomes of pediatric out-of-hospital cardiac arrest by scholastic age category. Pediatr Crit Care Med. 2013;14:130–136. doi: 10.1097/PCC.0b013e31827129b3. [DOI] [PubMed] [Google Scholar]
- 237.Yasunaga H, Horiguchi H, Tanabe S, Akahane M, Ogawa T, Koike S, Imamura T. Collaborative effects of bystander-initiated cardiopulmonary resuscitation and prehospital advanced cardiac life support by physicians on survival of out-of-hospital cardiac arrest: A nationwide population-based observational study. Crit Care. 2010;14:R199. doi: 10.1186/cc9319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Haukoos JS, Witt G, Gravitz C, Dean J, Jackson DM, Candlin T, Vellman P, Riccio J, Heard K, Kazutomi T, Luyten D, Pineda G, Gunter J, Biltoft J, Colwell C, Group CCARCS, Directors DMEM Out-of-hospital cardiac arrest in denver, colorado: Epidemiology and outcomes. Acad Emerg Med. 2010;17:391–398. doi: 10.1111/j.1553-2712.2010.00707.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kaji AH, Hanif AM, Bosson N, Ostermayer D, Niemann JT. Predictors of neurologic outcome in patients resuscitated from out-of-hospital cardiac arrest using classification and regression tree analysis. Am J Cardiol. 2014;114:1024–1028. doi: 10.1016/j.amjcard.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 240.Mahapatra S, Bunch TJ, White RD, Hodge DO, Packer DL. Sex differences in outcome after ventricular fibrillation in out-of-hospital cardiac arrest. Resuscitation. 2005;65:197–202. doi: 10.1016/j.resuscitation.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 241.Anderson ML, Cox M, Al-Khatib SM, Nichol G, Thomas KL, Chan PS, Saha-Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, Peterson ED. Rates of cardiopulmonary resuscitation training in the united states. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Weisfeldt ML, Everson-Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, Bigham B, Brooks SC, Foerster C, Gray R, Ornato JP, Powell J, Kudenchuk PJ, Morrison LJ, Investigators ROC Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Bagai A, McNally BF, Al-Khatib SM, Myers JB, Kim S, Karlsson L, Torp-Pedersen C, Wissenberg M, van Diepen S, Fosbol EL, Monk L, Abella BS, Granger CB, Jollis JG. Temporal differences in out-of-hospital cardiac arrest incidence and survival. Circulation. 2013;128:2595–2602. doi: 10.1161/CIRCULATIONAHA.113.004164. [DOI] [PubMed] [Google Scholar]
- 244.Urban J, Thode H, Stapleton E, Singer AJ. Current knowledge of and willingness to perform hands-only cpr in laypersons. Resuscitation. 2013;84:1574–1578. doi: 10.1016/j.resuscitation.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 245.Lester CA, Donnelly PD, Assar D. Lay cpr trainees: Retraining, confidence and willingness to attempt resuscitation 4 years after training. Resuscitation. 2000;45:77–82. doi: 10.1016/s0300-9572(00)00170-2. [DOI] [PubMed] [Google Scholar]
- 246.Böttiger BW, Van Aken H. Kids save lives -: Training school children in cardiopulmonary resuscitation worldwide is now endorsed by the world health organization (who). Resuscitation. 2015;94:A5–7. doi: 10.1016/j.resuscitation.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 247.Cave DM, Aufderheide TP, Beeson J, Ellison A, Gregory A, Hazinski MF, Hiratzka LF, Lurie KG, Morrison LJ, Mosesso VN, Jr., Nadkarni V, Potts J, Samson RA, Sayre MR, Schexnayder SM. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: A science advisory from the american heart association. Circulation. 2011;123:691–706. doi: 10.1161/CIR.0b013e31820b5328. doi: 610.1161/CIR.1160b1013e31820b35328. Epub 32011 Jan 31810. [DOI] [PubMed] [Google Scholar]
- 248.Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang-Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp-Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 249.Lick CJ, Aufderheide TP, Niskanen RA, Steinkamp JE, Davis SP, Nygaard SD, Bemenderfer KK, Gonzales L, Kalla JA, Wald SK, Gillquist DL, Sayre MR, Osaki Holm SY, Oski Holm SY, Oakes DA, Provo TA, Racht EM, Olsen JD, Yannopoulos D, Lurie KG. Take heart america: A comprehensive, community-wide, systems-based approach to the treatment of cardiac arrest. Crit Care Med. 2011;39:26–33. doi: 10.1097/CCM.0b013e3181fa7ce4. [DOI] [PubMed] [Google Scholar]
- 250.Potts J, Lynch B. The american heart association cpr anytime program: The potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26:346–354. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 251.Blewer AL, Leary M, Decker CS, Andersen JC, Fredericks AC, Bobrow BJ, Abella BS. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: A feasibility trial. J Hosp Med. 2011;6:428–432. doi: 10.1002/jhm.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Knight LJ, Wintch S, Nichols A, Arnolde V, Schroeder AR. Saving a life after discharge: Cpr training for parents of high-risk children. J Healthc Qual. 2013;35:9–16. doi: 10.1111/j.1945-1474.2012.00221.x. quiz17. [DOI] [PubMed] [Google Scholar]
- 253.Pierick TA, Van Waning N, Patel SS, Atkins DL. Self-instructional cpr training for parents of high risk infants. Resuscitation. 2012;83:1140–1144. doi: 10.1016/j.resuscitation.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 254.Hazinski MF, Idris AH, Kerber RE, Epstein A, Atkins D, Tang W, Lurie K, Committee AHAEC, Council on Cardiopulmonary Pr, and Critical Care, Cardiology CoC Lay rescuer automated external defibrillator (“Public access defibrillation”) programs: Lessons learned from an international multicenter trial: Advisory statement from the american heart association emergency cardiovascular committee; the council on cardiopulmonary, perioperative, and critical care; and the council on clinical cardiology. Circulation. 2005;111:3336–3340. doi: 10.1161/CIRCULATIONAHA.105.165674. [DOI] [PubMed] [Google Scholar]
- 255.Moran PS, Teljeur C, Masterson S, O'Neill M, Harrington P, Ryan M. Cost-effectiveness of a national public access defibrillation programme. Resuscitation. 2015;91:48–55. doi: 10.1016/j.resuscitation.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 256.Winkle RA. The effectiveness and cost effectiveness of public-access defibrillation. Clin Cardiol. 2010;33:396–399. doi: 10.1002/clc.20790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Gold LS, Eisenberg M. Cost-effectiveness of automated external defibrillators in public places: Pro. Curr Opin Cardiol. 2007;22:1–4. doi: 10.1097/HCO.0b013e32801173c1. [DOI] [PubMed] [Google Scholar]
- 258.Folke F, Lippert FK, Nielsen SL, Gislason GH, Hansen ML, Schramm TK, Sørensen R, Fosbøl EL, Andersen SS, Rasmussen S, Køber L, Torp-Pedersen C. Location of cardiac arrest in a city center: Strategic placement of automated external defibrillators in public locations. Circulation. 2009;120:510–517. doi: 10.1161/CIRCULATIONAHA.108.843755. [DOI] [PubMed] [Google Scholar]
- 259.Chan TC, Li H, Lebovic G, Tang SK, Chan JY, Cheng HC, Morrison LJ, Brooks SC. Identifying locations for public access defibrillators using mathematical optimization. Circulation. 2013;127:1801–1809. doi: 10.1161/CIRCULATIONAHA.113.001953. [DOI] [PubMed] [Google Scholar]
- 260.Haskell SE, Post M, Cram P, Atkins DL. Community public access sites: Compliance with american heart association recommendations. Resuscitation. 2009;80:854–858. doi: 10.1016/j.resuscitation.2009.04.033. [DOI] [PubMed] [Google Scholar]
- 261.Drezner J, Pluim B, Engebretsen L. Prevention of sudden cardiac death in athletes: New data and modern perspectives confront challenges in the 21st century. Br J Sports Med. 2009;43:625–626. doi: 10.1136/bjsm.2009.064592. doi: 610.1136/bjsm.2009.064592. [DOI] [PubMed] [Google Scholar]
- 262.Berger S. Automated external defibrillators utility, rational, and controversies. Pacing Clin Electrophysiol. 2009;32(Suppl 2):S75–79. doi: 10.1111/j.1540-8159.2009.02390.x. [DOI] [PubMed] [Google Scholar]
- 263.Kovach J, Berger S. Automated external defibrillators and secondary prevention of sudden cardiac death among children and adolescents. Pediatr Cardiol. 2012;33:402–406. doi: 10.1007/s00246-012-0158-2. [DOI] [PubMed] [Google Scholar]
- 264.Swor R, Grace H, McGovern H, Weiner M, Walton E. Cardiac arrests in schools: Assessing use of automated external defibrillators (aed) on school campuses. Resuscitation. 2013;84:426–429. doi: 10.1016/j.resuscitation.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 265.Divekar A, Soni R. Successful parental use of an automated external defibrillator for an infant with long-qt syndrome. Pediatrics. 2006;118:e526–529. doi: 10.1542/peds.2006-0129. [DOI] [PubMed] [Google Scholar]
- 266.Bar-Cohen Y, Walsh EP, Love BA, Cecchin F. First appropriate use of automated external defibrillator in an infant. Resuscitation. 2005;67:135–137. doi: 10.1016/j.resuscitation.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 267.Bardy GH, Lee KL, Mark DB, Poole JE, Toff WD, Tonkin AM, Smith W, Dorian P, Packer DL, White RD, Longstreth WT, Anderson J, Johnson G, Bischoff E, Yallop JJ, McNulty S, Ray LD, Clapp-Channing NE, Rosenberg Y, Schron EB, Investigators H Home use of automated external defibrillators for sudden cardiac arrest. N Engl J Med. 2008;358:1793–1804. doi: 10.1056/NEJMoa0801651. [DOI] [PubMed] [Google Scholar]
- 268.Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW, Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP, American Heart Association Emergency Cardiovascular Care Committee CoC, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, C.uncil on Clinical Cardiology, and Council on P Strategies for improving survival after in-hospital cardiac arrest in the united states: 2013 consensus recommendations: A consensus statement from the american heart association. Circulation. 2013;127:1538–1563. doi: 10.1161/CIR.0b013e31828b2770. [DOI] [PubMed] [Google Scholar]
- 269.Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-cardiac arrest syndrome: Epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the international liaison committee on resuscitation (american heart association, australian and new zealand council on resuscitation, european resuscitation council, heart and stroke foundation of canada, interamerican heart foundation, resuscitation council of asia, and the resuscitation council of southern africa); the american heart association emergency cardiovascular care committee; the council on cardiovascular surgery and anesthesia; the council on cardiopulmonary, perioperative, and critical care; the council on clinical cardiology; and the stroke council. Circulation. 2008;118:2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 270.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL, Association AH. Part 9: Post-cardiac arrest care: 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768–786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 271.Callaway CW, Soar J, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, Donnino MW, Drajer S, Kloeck W, Morley PT, Morrison LJ, Neumar RW, Nicholson TC, Nolan JP, Okada K, O'Neil BJ, Paiva EF, Parr MJ, Wang TL, Witt J, Collaborators ALSC Part 4: Advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S84–S145. doi: 10.1161/CIR.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 272.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 273.Moler FW, Silverstein FS, Holubkov R, Slomine BS, Christensen JR, Nadkarni VM, Meert KL, Clark AE, Browning B, Pemberton VL, Page K, Shankaran S, Hutchison JS, Newth CJ, Bennett KS, Berger JT, Topjian A, Pineda JA, Koch JD, Schleien CL, Dalton HJ, Ofori-Amanfo G, Goodman DM, Fink EL, McQuillen P, Zimmerman JJ, Thomas NJ, van der Jagt EW, Porter MB, Meyer MT, Harrison R, Pham N, Schwarz AJ, Nowak JE, Alten J, Wheeler DS, Bhalala US, Lidsky K, Lloyd E, Mathur M, Shah S, Wu T, Theodorou AA, Sanders RC, Dean JM, Investigators TT Therapeutic hypothermia after out-of-hospital cardiac arrest in children. N Engl J Med. 2015;372:1898–1908. doi: 10.1056/NEJMoa1411480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Donnino MW, Andersen LW, Berg KM, Reynolds JC, Nolan JP, Morley PT, Lang E, Cocchi MN, Xanthos T, Callaway CW, Soar J, Force atIAT Temperature management after cardiac arrest: An advisory statement by the advanced life support task force of the international liaison committee on resuscitation and the american heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Circulation. 2015;132:2448–56. doi: 10.1161/CIR.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 275.Lowry AW, Morales DL, Graves DE, Knudson JD, Shamszad P, Mott AR, Cabrera AG, Rossano JW. Characterization of extracorporeal membrane oxygenation for pediatric cardiac arrest in the united states: Analysis of the kids’ inpatient database. Pediatr Cardiol. 2013;34:1422–1430. doi: 10.1007/s00246-013-0666-8. [DOI] [PubMed] [Google Scholar]
- 276.Otani T, Sawano H, Oyama K, Morita M, Natsukawa T, Kai T. Resistance to conventional cardiopulmonary resuscitation in witnessed out-of-hospital cardiac arrest patients with shockable initial cardiac rhythm. J Cardiol. 2015;S0914-5087(15):00285–3. doi: 10.1016/j.jjcc.2015.08.020. doi: 10.1016/j.jjcc.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 277.Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V, Bhutta A, Investigators AHAsGWtGR Outcomes after in-hospital cardiac arrest in children with cardiac disease: A report from get with the guidelines--resuscitation. Circulation. 2011;124:2329–2337. doi: 10.1161/CIRCULATIONAHA.110.013466. [DOI] [PubMed] [Google Scholar]
- 278.Mattke AC, Stocker CF, Schibler A, Alphonso N, Johnson K, Karl TR. A newly established extracorporeal life support assisted cardiopulmonary resuscitation (ecpr) program can achieve intact neurological outcome in 60 % of children. Intensive Care Med. 2015;41(12):2227–8. doi: 10.1007/s00134-015-4036-2. [DOI] [PubMed] [Google Scholar]