Abstract
BACKGROUND
Given the dramatic increase in adolescent overweight and obesity, models are needed for implementing weight management treatment through readily accessible venues. We evaluated the acceptability and efficacy of a school-based intervention consisting of school nurse-delivered counseling and an afterschool exercise program in improving diet, activity, and body mass index (BMI) among overweight and obese adolescents.
METHODS
A pair-matched cluster-randomized controlled school-based trial was conducted in which 8 public high schools were randomized to either a 12-session school nurse-delivered cognitive-behavioral counseling intervention plus school-based after school exercise program, or 12-session nurse contact with weight management information (control). Overweight or obese adolescents (N = 126) completed anthropometric and behavioral assessments at baseline and 8-month follow-up. Main outcome measures included diet, activity, and BMI. Mixed effects regression models were conducted to examine differences at follow-up.
RESULTS
At follow-up, students in intervention compared with control schools were not different in BMI, percent body fat, and waist circumference. Students reported eating breakfast (adjusted mean difference 0.81 days; 95% confidence interval [CI] 0.11–1.52) on more days/week; there were no differences in other behaviors targeted by the intervention.
CONCLUSIONS
While a school-based intervention including counseling and access to an after-school exercise program is theoretically promising with public health potential, it was not effective in reducing BMI or key obesogenic behaviors. Our findings are important in highlighting that interventions targeted at the individual level are not likely to be sufficient in addressing the adolescent obesity epidemic without changes in social norms and the environment.
Keywords: obesity, adolescents, school-based program, diet, physical activity
Adolescent overweight and obesity have increased dramatically in recent decades, with 34% of adolescents currently overweight or obese.1 Adolescent obesity has negative physical and mental health consequences,2–4 and is strongly linked with obesity during adulthood.5 Adolescence provides an opportunity to promote healthy lifestyles affecting physical and psychosocial outcomes during adolescence and into adulthood, yet adolescent obesity has been understudied compared with adults and preadolescents.6 One systematic review7 found that comprehensive behavioral interventions including diet and physical activity counseling and behavioral management training8 are efficacious for decreasing youth body mass index (BMI), but they were focused on preadolescents and conducted in specialty clinics with limited access by youth.7
Models for implementing expert recommendations for weight management interventions9 with adolescents require development and testing. The school setting provides a uniquely practical venue for translating promising treatment approaches into the community,9–13 as they have the facilities and staff to deliver a physical activity program, school nurses with the skills to provide counseling, and are easily accessible by adolescents, because 95% attend school.14 However, only 1 study has utilized school nurses to deliver a weight management intervention to obese adolescents in the high school setting, a randomized controlled school-based trial of a brief school nurse-delivered counseling intervention that found minimal dietary changes and no improvements in BMI.15 The purpose of the present trial was to expand on that study by testing the acceptability and efficacy of school nurse-delivered weight management counseling extended over the full academic year plus after-school exercise program, compared with an information-only control condition, to reduce BMI and improve diet and activity among overweight and obese adolescents.
METHODS
Participants
A pair-matched cluster-randomized controlled school-based trial was conducted with a convenience sample of 8 public high schools in Massachusetts. The total student enrollment at these schools ranged from 673 to 1467; the student populations were predominately white (61.8% to 94.4%) in 7 schools, and Hispanic (42.7%) in 1 school. The percent of students considered low income ranged from 5.7% to 59.7%. Schools were pair matched on enrollment, and 1 school from each pair was randomly assigned to the intervention or control condition. Data were collected from September 2012 to June 2013. Clinical Trial Registration # NCT01463124.
Adolescents in grades 9 to 12 were eligible to participate if they had a BMI ≥ 85th percentile for age and sex, provided assent and had parental consent, and had at least 1 English-speaking parent. Exclusions included plans to move out of the area; a medical condition that precluded adherence to the intervention; diagnosis of a serious psychiatric illness; genetic or endocrine cause of obesity; taking a medication associated with weight gain; or weighing ≥ 300 pounds. Students were recruited to a study about “healthy living,” in an attempt to reduce the potential for stigma, through school announcements, flyers and posters, going into classes, setting up an information table in the cafeteria, and school nurse encounters.
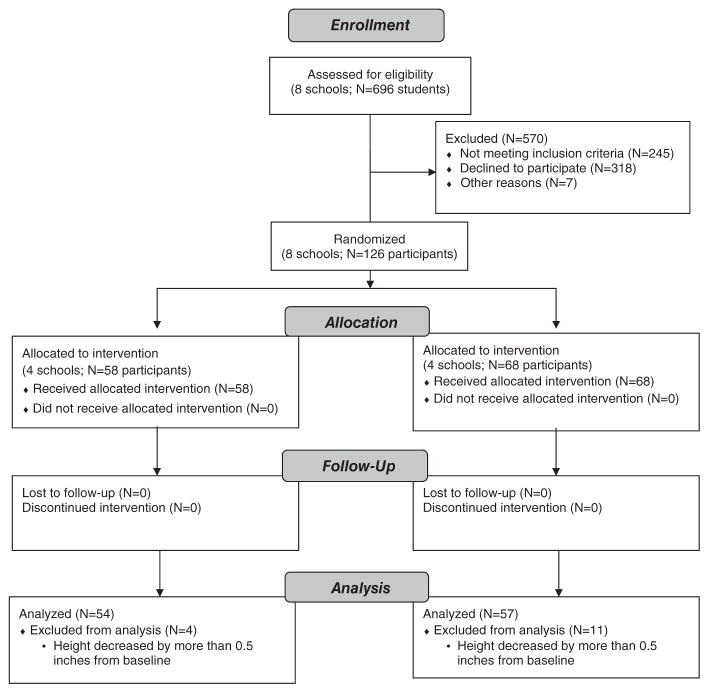
Assessments were completed at baseline and 8 months later by trained research assistants. Participants received a $25 gift card at assessments. Six hundred and ninety-six students were screened for eligibility; 126 students participated in the study (Figure 1). The study retained 100% of participants at follow-up.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) Flow Diagram
Study Conditions
Lookin’ Good Feelin’ Good: school nurse intervention and after-school exercise program
The Lookin’ Good Feelin’ Good condition involved 2 components—a school nurse-delivered counseling intervention, and an after school exercise program. The school nurse-delivered counseling component expanded upon the prior study intervention15 and consisted of an intensive phase of 6-weekly 30-minute individual sessions followed by a maintenance phase of 6 monthly sessions and brief weekly weigh-ins.
Each visit was conducted during the school day during nonacademic periods and included the following: (1) a weigh-in; (2) review of diet and physical activity log; (3) assessment of progress toward behavioral goals with a review of successes and strategies used and problem-solving challenges experienced; (4) discussion of the session’s topics using a student booklet; (5) assessment of current behavior related to topics and discussion of challenges and strategies for improving; and (6) structured goal setting for the coming week. Although a weight loss goal and caloric requirements were set at the start of the program given the primary goal of reduction in BMI, the stated program goals and focus of the counseling were on eating healthy and being more physically active. A Food and Activity Tracking Log was provided to support the adolescent in making these healthy behavior changes.
The dietary component of the counseling intervention was consistent with expert recommendations for the prevention and treatment of child and adolescent overweight and obesity for addressing pediatric overweight and obesity,8–16 with particular attention to the unique needs of adolescents.17 This includes eating 5 or more servings of fruits and vegetables a day; limiting consumption of soda and sugar-sweetened drinks; eating 3 structured meals a day, including a healthy breakfast and limiting unhealthy snacks and desserts, replacing with healthy alternatives; decreasing consumption of foods high in glycemic index, saturated fats, and calories; limiting eating out; eating when hungry, stopping when satisfied (hunger and appetite); and choosing appropriate portion sizes. Tools such as the Rate your Plate and visuals to depict caloric balance and how it relates to weight loss were used.
The physical activity component of the school nurse-delivered counseling intervention was consistent with expert recommendations for obesity management,18 encouraging at least 1 hour of exercise most days of the week. Students were provided with a pedometer for themselves and a support person and instructed in its use to support their goal of increasing physical activity. They were instructed in the F.I.T.T. principles (frequency, intensity, time, and type of activity) and how to apply these to their efforts. The intervention also targeted reduction in sedentary behavior, for a goal of less than 2 hours/day of screen time (eg, TV, video, and computer).
Additional topics included problem solving strategies, how to handle slips, stopping negative thoughts that get in the way of making healthy choices, changing problem food and activity cues, how to handle stressful events, problem social cues, getting support for healthy behavior change, handling social events such as parties, holidays and vacations, taking charge of one’s environment, sleep hygiene, and ways to stay motivated. A student booklet was used to guide the discussion, with sections adapted from Group Lifestyle Balance™ materials. The intervention was based on Social Cognitive Theory19 and school nurses tailored the intervention to the student’s needs using patient centered counseling, which involves asking students questions about their unique experiences with each topic and how they may practically apply the strategies discussed in their lives. School nurses were trained on the protocol in a daylong group training session.
The after school exercise program component consisted of 3 sessions per week for 8 months structured to increase exercise enjoyment20 delivered by existing school staff with training and experience in delivering physical activity education to youth (eg, physical education teachers, school nurses and administrative staff with prior experience in providing physical activity instruction). Sessions were modeled on the CANFIT (Communities, Adolescents, Nutrition, and Fitness) program, which includes fun group sports, games, and noncompetitive fitness activities such as dance, with efficacy for increasing exercise in adolescents.21 Each session included a warm-up, instructions, moderate-to-vigorous activity, and cool-down. During the cool-down, strategies for incorporating physical activity into their daily routines were discussed, such as walking/bicycling to school, and parking farther away. The CANFIT program was designed to be delivered by facilitators with a wide range of experience and includes clear, simple instructions on engaging youth in the physical activities and creating a positive physical activity environment for youth. The staff delivering the after school exercise program participated in a 2-hour training program conducted by the study’s physical activity expert that included (1) review of each of the study protocol activities, including discussion of strategies found effective in implementing the activities and (2) hands-on instruction and practice with each of the warm-up and cool-down exercises.
Control condition
Participants in the control schools had 12 individual visits with the school nurse during nonacademic periods over the same time frame as the intervention condition to be weighed, review behavior changes, read weight management pamphlets (from ETR Associates and Journeyworks http://www.journeyworks.com/ with appropriate content for adolescents), and have questions answered. School nurses received an individual orientation to the protocol.
Assessments
All assessments were conducted by 1 trained Research Coordinator at baseline and 8-month follow-up. Height and weight were measured using standard methodology, wearing light clothing and no shoes. BMI, the primary outcome measure, was calculated as weight (kg)/height squared (in meters) for age and sex using the CDC BMI charts. Waist circumference was measured as the average of 2 measurements midway between the rib cage and superior border of the iliac crest. A Tanita Scale measured body weight and body fat using the leg-to-leg bioelectric impedance analysis (BIA) system.
Dietary intake was assessed with a 24-hour dietary recall interview22 using the Interactive Nutrition Data System (NDS, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). Recalls were unannounced and conducted by trained, licensed dieticians by phone on 1 randomly selected day of the week. An 8-item instrument developed by Ammerman et al23 was used to assess dietary behaviors targeted by the intervention. Physical activity was assessed by accelerometer using the ActiGraph Model GT1M for a 7-day period; average daily minutes of light, moderate, and vigorous activity were calculated using published cut points.24 Sedentary behavior, TV watching, and playing computer or video games on an average school day was measured using 2 items from the Youth Risk Behavior Survey.25 Self-efficacy or confidence in making weight-related behavior changes was assessed with an 11-item questionnaire adapted from the Go Girls study (Cronbach alpha = .90).26 Barriers to eating healthy and exercising was assessed by 5 items adapted from New Moves (Cronbach alpha = .84; test-retest r = .89)27 and 2 items from Motl et al.28
Intervention fidelity was assessed by student report on a Patient Exit Interview Survey and school nurses completing a checklist after each visit. The number of counseling and exercise sessions attended by each student were documented by the school nurse and exercise class facilitator, respectively. Student acceptability of the counseling intervention was assessed by rating the perceived helpfulness of the nurse intervention and level of comfort in discussing weight with the school nurse. Students also rated their level of satisfaction with the after school exercise program and barriers to their participation.
Data Analysis
Baseline means were compared using t tests. Chi-square tests were used to compare categorical variables. Continuous and dichotomous outcomes of physiologic measures, physical activity, diet, and psychosocial measures were compared using mixed effects regression models. The same methods were used in post hoc, exploratory analyses that compared the characteristics and predictors of those with favorable and unfavorable changes in BMI, irrespective of intervention condition. To account for the cluster randomized design, school was included as a random effect in the mixed effects regression models. Models were adjusted for baseline level of the outcome. Four students from the intervention and 11 from the control condition were excluded from the analyses because their measured height at follow-up decreased by more than 0.5 inches from baseline and was, therefore, inconsistent. All analyses were conducted at the student level and carried out using SAS version 9.3. A 2-tailed p < .05 was considered statistically significant. Study data were collected and managed using REDCap electronic data capture tools hosted at University of Massachusetts Medical School (UMMS).29
Sample size
The number of schools was determined as the maximum feasible, given the budget of the study. We assumed a cluster randomized approach to determine the number of participants per condition and, thus, per school, assuming an intraclass correlation of 0.027 (from preliminary data), yielding a design effect of 1.38. Thus, with a sample size of 15 per school, we had 80% power to detect a difference in the primary outcome of change in BMI of 0.6 standard deviations, which is considered to be a moderate size difference using Cohen’s criteria.30
Randomization
We created 4 pairs of schools (1 for each condition) matching on approximate number of students. The schools were each assigned a random number and the school with the lowest random number in each pair was assigned to the Lookin’ Good Feelin’ Good condition. We used a random start for the random number sequence31 and used the sequence of random numbers from that point. Because this was a cluster randomized trial, there was no need to conceal the sequence. The school nurse and staff at each school were trained in the appropriate study procedures for that condition. The random allocation sequence was generated by the study biostatistician (B.B.).
RESULTS
Baseline Participant Characteristics
Baseline sociodemographic characteristics of participants were generally comparable between the 2 conditions (Table 1). Control schools had fewer students that were of black race and more students that were mixed race when compared with intervention schools (15.8% vs 24.1% black race and 21.1% vs 5.6% mixed race, respectively; p = .018). Anthropometric measures did not differ significantly between conditions.
Table 1.
Characteristics of Student Population at Baseline
| Variable | Control (N = 57) | Intervention (N = 54) | p-value* |
|---|---|---|---|
| Mean (SD) age (years) | 16.3 (1.20) | 16.5 (1.23) | .320 |
| %Female | 61.4 | 63.0 | .866 |
| Race | |||
| %White | 63.2 | 63.0 | .018 |
| %Black | 15.8 | 24.1 | |
| %Other | 0 | 7.4 | |
| %Mixed | 21.1 | 5.6 | |
| %Hispanic ethnicity | 38.6 | 24.1 | .100 |
| %participate in free or reduced school meals | 63.2 | 51.9 | .228 |
| Hours play video/computer games or watching TV on average school day in past 7days | |||
| %None | 3.5 | 5.6 | .948 |
| %<1hour/day | 1.8 | 1.9 | |
| %1hour/day | 17.5 | 13.0 | |
| %2hours/day | 12.3 | 11.1 | |
| %3hours/day or more | 64.9 | 68.5 | |
| %Servings of fruits and vegetables on a typical day in past 7days | |||
| %None | 7.0 | 1.9 | .336 |
| %1 serving | 5.3 | 1.9 | |
| %2 servings | 3.5 | 7.4 | |
| %3 servings or more | 84.2 | 88.9 | |
| Times drink soda on a typical day in past 7days | |||
| None | 24.6 | 35.2 | .348 |
| 1 time | 29.8 | 31.5 | |
| 2 times | 22.8 | 11.1 | |
| 3 or more times | 22.8 | 22.2 | |
| Times eat fast food in past 7days | |||
| None | 24.6 | 48.1 | .072 |
| 1 time | 43.9 | 31.5 | |
| 2 times | 17.5 | 9.3 | |
| 3 or more times | 14.0 | 11.1 | |
| Mean number of days eat breakfast in past 7days | 3.5 (2.44) | 4.9 (2.44) | .003 |
| Barriers to healthy behaviors (%strongly agree to agree) | |||
| %Too busy to exercise | 29.8 | 29.6 | .982 |
| %Do not like feel when exercise | 42.1 | 35.2 | .454 |
| %Feel embarrassed exercising with others | 50.9 | 44.4 | .498 |
| %Do not feel safe walking in neighborhood | 14.0 | 13.0 | .869 |
| %Eating healthy costs too much | 24.6 | 27.8 | .700 |
| %Healthy food does not taste good | 19.3 | 16.7 | .718 |
| %Healthy food is not available | 12.3 | 11.1 | .848 |
| Confident can do the following (%very confident) | |||
| %Lose weight | 50.9 | 57.4 | .490 |
| %Eat healthier | 52.6 | 59.3 | .482 |
| %Exercise most days | 57.9 | 48.1 | .304 |
| %of time spent in MVPA each day† | 31.9 (8.76) | 30.9 (11.82) | .676 |
| Mean number days physically active in past 7days (range 0 to 7) | 3.6 (2.14) | 3.4 (2.11) | .724 |
| Mean total energy intake (range 119 to 4178 calories) | 1797.5 (800.90) | 1822.6 (901.54) | .925 |
| Mean BMI kg/m2 (range 23.6 to 50.8) | 31.6 (5.20) | 30.7 (5.35) | .242 |
| Mean Body fat (%) (range 13.3 to 51.1) | 35.0 (9.56) | 34.4 (9.41) | .672 |
| Mean BMI percentile (range 76.3%to 99.9%) | 95.6 (4.37) | 93.9 (5.77) | .172 |
| Mean BMI Z-score (range 0.72 to 3.05) | 1.9 (0.48) | 1.7 (0.52) | .172 |
| Mean waist circumference (cm) (range 39.0 to 133.8) | 96.8 (12.02) | 94.0 (14.77) | .234 |
BMI Z, body mass index Z-score; MVPA, moderate to vigorous activity.
The p-values derived from the Student’s independent t test for comparison of 2 means and chi-square test for independence for comparison of responses to categorical variables between intervention and control conditions.
Accelerometer data were available for only 49 students in the intervention condition.
Intervention Effects
Students in the intervention compared with control schools showed no significant differences in anthropometric variables including BMI, percent body fat, and waist circumference at follow-up (Table 2). Students in intervention compared with control schools reported eating breakfast on significantly more days/week at follow-up, adjusted mean 4.65 vs 3.84 days, respectively (adjusted mean difference 0.81 days; 95% confidence interval [CI] 0.11–1.52). The mean number of days students reported being physically active in the past 7 days was similarly higher in intervention compared with control schools at follow-up, adjusted mean 4.53 days vs 3.64 days, respectively (adjusted mean difference 0.89 days; 95% CI 0.25–1.53). There were no statistically significant differences between conditions on other behaviors targeted by the intervention such as TV watching, fruit and vegetable intake, drinking soda, eating fast food, and moderate to vigorous activity (MVPA). The proportion of students in intervention and control schools reporting barriers to exercise and healthy eating were similar at baseline and follow-up (data not shown).
Table 2.
Effects of Intervention on Anthropometric Variables and Lifestyle Factors
| Variable | Treatment Condition | Unadjusted BL Mean (SD) | Unadjusted FUP Mean (SD) | Unadjusted Mean Change (FUP-BL) | Adjusted FUP Mean* (95% CI) | Adjusted Mean Difference I-C* (95% CI) | p-value |
|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | Control | 31.65 (0.69) | 31.61 (0.69) | −0.04 | 31.14 (30.48–31.80) | −0.14 (−1.09–0.81) | .731 |
| Intervention | 30.66 (0.73) | 30.52 (0.78) | −0.15 | 31.00 (30.31–31.69) | |||
| BMI Z-score | Control | 1.89 (0.06) | 1.88 (0.07) | −0.02 | 1.80 (1.72–1.88) | −0.03 (−0.15–0.09) | .601 |
| Intervention | 1.74 (0.07) | 1.69 (0.08) | −0.05 | 1.77 (1.68–1.86) | |||
| Waist circumference (cm) | Control | 96.81 (1.59) | 94.66 (1.98) | −2.15 | 93.74 (88.01–99.48) | 1.40 (−6.82–9.62) | .693 |
| Intervention | 93.98 (2.01) | 94.25 (2.15) | 0.27 | 95.14 (89.26–101.03) | |||
| Body fat (%) | Control | 35.04 (1.27) | 35.46 (1.19) | 0.42 | 35.20 (32.87–37.54) | −1.62 (−4.98–1.74) | .281 |
| Intervention | 34.40 (1.28) | 33.39 (1.41) | −1.02 | 33.58 (31.16–36.00) | |||
| Number of servings of fruits and vegetables in past 7days | Control | 3.44 (0.24) | 3.68 (0.24) | 0.25 | 3.73 (2.95–4.52) | 0.52 (−0.60–1.65) | .276 |
| Intervention | 3.67 (0.22) | 4.39 (0.17) | 0.72 | 4.26 (3.45–5.06) | |||
| Number days eat breakfast in past 7days | Control | 3.47 (0.32) | 3.37 (0.33) | −0.11 | 3.84 (3.36–4.32) | 0.81 (0.11–1.52) | .024 |
| Intervention | 4.89 (0.33) | 5.15 (0.32) | 0.26 | 4.65 (4.16–5.15) | |||
| Number times drink soda in past 7days | Control | 1.63 (0.19) | 1.30 (0.16) | −0.33 | 1.26 (0.96–1.56) | −0.11 (−0.54–0.33) | .628 |
| Intervention | 1.35 (0.20) | 1.11 (0.17) | −0.24 | 1.15 (0.84–1.46) | |||
| Number times eat fast food in past 7days | Control | 1.28 (0.15) | 1.09 (0.15) | −0.19 | 1.04 (0.59–1.48) | −0.07 (−0.72–0.59) | .791 |
| Intervention | 0.85 (0.14) | 0.93 (0.16) | 0.07 | 0.97 (0.49–1.45) | |||
| Hours play video/computer games or watching TV on average school day in past 7days | Control | 2.38 (0.12) | 2.19 (0.13) | −0.18 | 2.21 (1.92–2.50) | −0.01 (−0.43–0.41) | .937 |
| Intervention | 2.42 (0.13) | 2.20 (0.14) | −0.21 | 2.19 (1.89–2.50) | |||
| Number days physically active in past 7days | Control | 3.58 (0.28) | 3.68 (0.29) | 0.11 | 3.64 (3.19–4.08) | 0.89 (0.25–1.53) | .007 |
| Intervention | 3.43 (0.29) | 4.48 (0.28) | 1.06 | 4.47 (3.79–5.16) | |||
| %Time spent in MVPA each day† | Control | 31.93 (1.16) | 30.07 (1.43) | −1.85 | 29.79 (27.32–32.26) | −0.76 (−4.63–3.10) | .695 |
| Intervention | 30.93 (1.69) | 27.87 (1.80) | −3.06 | 29.02 (26.06–31.99) | |||
| Total energy (calories) | Control | 1797.47 (106.08) | 1534.42 (87.90) | −263. | 1537.62 (1384.24–1691.00) | −52.81 (−272.72–167.10) | .635 |
| Intervention | 1822.63 (122.68) | 1488.19 (78.43) | −334. | 1484.81 (327.23–1642.39) |
BL, baseline; BMI, body mass index; CI, confidence interval; FUP, follow-up; MVPA, moderate to vigorous activity.
Adjusted means from mixed effects regression models adjusted for school and baseline measurement of each variable; Adjusted Mean Difference I-C (Adjusted FUP Mean BMI for Intervention—Adjusted FUP Mean BMI for Control).
Accelerometer data available on only 49 control and 34 intervention students at baseline and follow-up.
In exploratory analyses, we examined the dietary and lifestyle factors associated with favorable (decrease in BMI) vs unfavorable (no change or increase in BMI) changes in BMI, irrespective of school condition. Among the 51 participants with a favorable BMI change, there was a 1.46 unit average decrease in BMI compared with a 1.08 unit average increase in BMI among the 60 participants with unfavorable changes in BMI (adjusted mean difference −2.58; 95% CI −3.03 to 2.13). Students with favorable vs unfavorable changes in BMI also had significantly greater decreases in waist circumference and % body fat, were more likely to be of non-Hispanic ethnicity (78.4% vs 60%, respectively; p = .037), and somewhat more likely to be male (47.1% vs 30%, respectively; p = .065). The 2 groups were comparable on age, race, plans to lose weight, and dietary and physical activity behaviors at baseline (data not shown). The only statistically significant dietary or lifestyle factor change associated with a favorable change in BMI at follow-up was soda intake (Table 3). Students with a favorable change in BMI reported drinking soda fewer times in the last 7 days than those with unfavorable changes in BMI, adjusted mean 0.83 times vs 1.53 times, respectively (adjusted mean difference −0.71 days; 95% CI −1.12 to −0.30).
Table 3.
Association Between Changes in Dietary and Lifestyle Factors and Favorable vs Unfavorable Changes in BMI
| Variable | BMI Change | Unadjusted BL Mean (SD) | Unadjusted FUP Mean (SD) | Unadjusted Mean Change FUP-BL | Adjusted FUP Mean* (95% CI) | Adjusted Mean Difference* (95% CI) | p-value |
|---|---|---|---|---|---|---|---|
| Totals energy (calories) | Unfavorable | 1534.46 (82.90) | −208. | 1552.28 (1402.81–1701.76) | −87.83 (−308.79–133.12) | .432 | |
| Favorable | 1888.60 (127.64) | 1485.42 (83.85) | −403. | 1464.45 (1302.28–1626.63) | |||
| Servings in fruits and vegetables in past 7days | Unfavorable | 3.68 (0.21) | 4.25 (0.18) | 0.57 | 4.15 (3.58–4.72) | −0.36 (−0.92–0.21) | .212 |
| Favorable | 3.39 (0.24) | 3.76 (0.25) | 0.37 | 3.79 (3.22–4.37) | |||
| Days eat breakfast in past 7days | Unfavorable | 4.08 (0.33) | 4.28 (0.34) | 0.20 | 4.34 (3.76–4.91) | −0.21 (−0.93–0.50) | .558 |
| Favorable | 4.25 (0.36) | 4.18 (0.36) | −0.08 | 4.13 (3.53–4.72) | |||
| Days drink soda in past 7days | Unfavorable | 1.50 (0.19) | 1.53 (0.17) | 0.03 | 1.53 (1.25–1.81) | −0.71 (−1.12–−0.30) | .001 |
| Favorable | 1.49 (0.20) | 0.82 (0.14) | −0.67 | 0.83 (0.52–1.13) | |||
| Times eat fast food in past 7days | Unfavorable | 1.13 (0.16) | 1.20 (0.16) | 0.07 | 1.19 (0.85–1.53) | −0.40 (−0.84–0.03) | .07 |
| Favorable | 1.00 (0.14) | 0.78 (0.15) | −0.22 | 0.78 (0.43–1.13) | |||
| Days physically active in past 7days | Unfavorable | 3.62 (0.27) | 4.22 (0.29) | 0.60 | 4.14 (3.56–4.72) | −0.14 (−0.82–0.53) | .675 |
| Favorable | 3.37 (0.30) | 3.90 (0.29) | 0.53 | 3.99 (3.40–4.59) | |||
| %Time spent in MVPA each day† | Favorable | 31.78 (1.32) | 28.90 (1.70) | −2.88 | 29.12 (26.41–31.82) | 0.71 (−3.10–4.51) | .713 |
| Unfavorable | 31.12 (1.51) | 29.36 (1.47) | −1.76 | 29.82 (27.15–32.49) | |||
| Hours spent watching TV or video games | Unfavorable | 2.37 (0.13) | 2.27 (0.14) | −0.10 | 2.29 (2.06–2.52) | −0.19 (−0.51–0.12) | .233 |
| Favorable | 2.43 (0.12) | 2.12 (0.13) | −0.31 | 2.10 (1.85–2.34) |
CI, confidence interval; BMI, body mass index; MVPA, moderate to vigorous activity.
Adjusted means from mixed effects regression models adjusted for school and baseline measurement of each variable; Adjusted Mean Difference (Adjusted FUP Mean for Favorable BMI Change—Adjusted FUP Mean for Unfavorable BMI Change).
Accelerometer data available for only 83 students at baseline and follow-up.
Treatment Fidelity and Acceptability
School nurses reported the majority of students in control schools attended all 12 visits; 100% attended all of the first 6 visits, 99% attended the last 6 visits. Attendance in intervention schools was lower; 91% of students attended all of the first 6 visits, 74% attended all of the last 6 visits. Students reported on the Patient Exit Interview Survey generally moderate to high levels of interest, helpfulness and comfort in working with the school nurse to lose weight. On a scale of 1 (not at all ) to 5 (very), mean ratings for each of these constructs at each visit ranged from 4.2 to 4.7 in intervention schools and 3.6 to 4.5 in control schools. Participation in the after school exercise program was low, with 50% of students attending none of the classes. Among the students who attended at least 1 exercise class, mean attendance was 8.6 (SD 10.4) classes; 74% were slightly or very satisfied with the helpfulness of the class leader and the length of the classes; 67% were slightly or very satisfied with the class activities and with their ability to reach their physical activity goals. Barriers to attending the after school exercise program identified as important or somewhat important by all students (both those participating in the after school program and those not able to participate) included having homework to complete (81%), after school responsibilities such as taking care of a sibling (65%), already participating in sports (52%) or had sport practice after school conflicting with the exercise class (44%), do not like to exercise in a group (46%), had no transportation home after the class (45%), or had an after school job (43%).
DISCUSSION
This study found that a school-based intervention consisting of school nurse-delivered counseling plus the availability of an after school exercise program improves a limited number of self-reported dietary and physical activity behaviors, but not BMI, other anthropometric outcomes, or key obesogenic behaviors. The school nurse counseling component is feasible for school nurses to deliver with high fidelity and is acceptable to overweight and obese adolescents. However, an after school exercise component is not as well received or feasible for students, with 50% of students not attending any of the classes held during the school year. The most commonly cited barriers to participation in the after school exercise program were academic and other personal after-school responsibilities or extracurricular activities as well as not liking to exercise in a group setting.
Recent findings from a systematic review suggest that comprehensive behavioral interventions consistent with expert recommendations8 of fairly high-intensity (26 to 75+ hours) are needed for effective weight loss.7 The intervention tested in this study provided the opportunity for moderate contact time (6 hours of counseling plus brief weekly check-ins and thrice-weekly exercise classes) integrated within the easily accessible school setting, leveraging existing school resources and reducing barriers to adolescents seeking and receiving treatment. While it had the potential to be more intensive than the prior school-based study,15 it did not reach the level of moderate-to high-intensity of the effective interventions provided within the specialty clinics and poor participation in the after school exercise program further limited the intensity of the intervention and hence potentially the outcomes. The lack of an intervention effect on BMI and only minimal positive changes in self-reported obesogenic behaviors is consistent with the finding of mixed results from less comprehensive and intensive programs similar to our intervention.7
Unlike other pediatric weight management programs that found reductions in sedentary behaviors when targeted as part of the intervention, the present study found no such improvements. A meta-analysis of interventions targeting screen time reduction found such interventions had a statistically significant although small effect in children, including adolescents.32 In the present study, it appears that the problem-solving conducted as part of the counseling intervention was not more effective in helping teens reduce their screen time than the provision of written information. It may be that students are unable to effectively develop strategies to overcome barriers to physical activity, which might serve as a replacement for time spent in sedentary activity. This is consistent with the finding of no change in barriers to engaging in physical activity found in the current study.
In post hoc analyses, our study found that adolescents with favorable BMI changes had an average 7.0 pound weight loss while those with unfavorable changes had an average 8.2 pound increase in weight. Those with favorable BMI changes were more likely to be of non-Hispanic ethnicity, and drank less soda. Drinking less soda also has been reported to be a successful weight control strategy by overweight adolescents who have lost weight.33
Limitations
Our study had a number of limitations. Both conditions involved 12 one-on-one sessions with the school nurse to control for contact, regular weighing, and discussions about weight management. While the strong control condition was a strength, it served in many ways as another intervention and the intensity of the control intervention may have made it difficult to identify a statistically significant improvement from the intervention condition. Had we tested the intervention against usual care for the school health clinic, which may consist of only BMI screening and parent notification of results, we may have been able to see statistically significant differences in improvements in anthropometric measures and/or behavioral measures. Another limitation is poor participation in the after school exercise program. Reliance on self-report measures of behavior change inherent in weight management trials may have affected the reliability of student responses. Although we used a cluster randomized design, the small number of schools located in 1 geographical area limits the generalizability of our findings. Significant strengths of the current study are the randomized design, relatively large sample of students, and 100% retention. Additional strengths include the carefully designed intervention based on current recommendations tailored for adolescents and extensive formative work, and use of real-world providers to deliver the intervention.
Conclusions
This study found that a school-based intervention including nurse-delivered counseling and access to an after school exercise program was feasible for nurses to deliver with high fidelity and acceptable to overweight and obese adolescents, but the majority of adolescents did not participate in the after school exercise program. While such a program delivering weight management counseling to overweight and obese adolescents within the school setting is theoretically appealing and has tremendous public health potential, it was not found to be effective in improving BMI or key obesogenic behaviors. This study’s findings highlight that individual interventions are not likely to be sufficient in addressing the adolescent obesity epidemic without changes within the family and community. Change in social norms and environment, similar to what has been done with tobacco use, must be part of the solution in addressing overweight and obesity in adolescents.
IMPLICATIONS FOR SCHOOL HEALTH
The school and school health setting is an excellent venue for tackling the challenging problem of adolescent obesity. School nurses have the skills needed to provide weight-related behavior change counseling, and are easily accessible to adolescents, the vast majority of whom (over 95%) attend school.14 In addition, about half of high schools in the United States have a full-time registered nurse and another one third have a part-time nurse.34 The position of the National Association of School Nurses (NASN) is that “school nurses have the knowledge and expertise to promote the prevention of overweight and obesity and address the needs of overweight and obese youth in schools” and that it is their role to “assist students who are overweight and obese to . . . [learn] good-decision-making skills related to nutrition and physical activity to develop and achieve healthy lifestyles.”35 The leveraging of existing infrastructure by capitalizing on the placement of skilled health care providers in the highly accessible school setting along with facilities and staff to deliver an after-school exercise program has tremendous public health significance compared with specialty clinics, which have limited reach due to access and the expense of intensive resources required, including the cost to the family in terms of transportation, copayments and time.
However, the present study demonstrated that, while a weight management program within the school setting was feasible for school nurses to deliver, the after-school exercise program was not. Although theoretically appealing with strong public health potential, this program was not found to be effective in improving BMI or key obesogenic behaviors. This finding suggests that interventions focused on the individual adolescent that do not include changes at the family and community level are not likely to be effective in reducing adolescent overweight and obesity. The implication is that such school-based programs targeting the individual adolescent need to be integrated into a larger social norms campaign within schools and communities, and engage families to help implement diet and physical activity into the adolescent’s home environment. Another possible direction is to focus on ways to bring effective, high-intensity interventions to more accessible venues for adolescents as part of a more comprehensive approach. For example, a combination of in-school intervention plus evening programming at the school for adolescents and their families for more intensive intervention may be worthy of investigation. An additional approach would be to tailor the physical activity intervention component to best meet the individual adolescent’s needs and preferences, as opposed to relying on a structured group program. For instance, adolescents could be supported in engaging in physical activities that are more likely to transfer to their everyday lives, such as becoming involved in activities in their natural environments including their home and neighborhood. Should such integrated interventions be found to be effective in helping adolescents reduce their BMI, there would be tremendous implications for the ability of school health to contribute to the reduction of adolescent obesity at a public health level.
Human Subjects Approval Statement
The University of Massachusetts Medical School (UMMS) Human Subjects Institutional Review Board approved the study protocol.
Acknowledgments
We gratefully acknowledge support for this research by grant R21 HL110208 fromthe National Institutes of Health, National Heart, Lung and Blood Institute. We thank the Active Living Research Programof the Robert Wood Johnson Foundation for the loan of accelerometer equipment used in this study. We also wish to thank the research assistants who collected the data and the schools and school nurses who graciously took part in this study. To the adolescents who participated, we extend our deepest appreciation.
Contributor Information
Lori Pbert, Email: lori.pbert@umassmed.edu.
Susan Druker, Email: susan.druker@umassmed.edu.
Bruce Barton, Email: bruce.barton@umassmed.edu.
Kristin L. Schneider, Email: kristin.schneider@rosalindfranklin.edu.
Barbara Olendzki, Email: barbara.olendzki@umassmed.edu.
Mary A. Gapinski, Email: Mary.Gapinski@state.ma.us.
Stephen Kurtz, Email: stephen.kurtz@umassmed.edu.
Stavroula Osganian, Email: stavroula.osganian@tch.harvard.edu.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136(5):664–672. doi: 10.1067/mpd.2000.105141. [DOI] [PubMed] [Google Scholar]
- 3.Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996;128(5 Pt 1):608–615. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 4.Willie SM, Wojciechowski B, Garvey T. Insulin resistance and defective glucose-insulin coupling in ketosis-prone type 2 diabetes at African-American children. Diabetes. 1998;46:A306. [Google Scholar]
- 5.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–2047. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitlock EA, O’Connor EP, Williams SB, Beil TL, Lutz KW. Effectiveness of Weight Management Programs in Children and Adolescents. Rockville, MD: Agency for Healthcare Research and Quality; 2008. (Report No.: 08-E014) [PubMed] [Google Scholar]
- 7.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–e418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 8.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 9.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 10.Montalto NJ. Implementing the guidelines for adolescent preventive services. Am Fam Physician. 1998;57(9):2181–2190. [PubMed] [Google Scholar]
- 11.Lyznicki JM, Young DC, Riggs JA, Davis RM. Obesity: assessment and management in primary care. Am Fam Physician. 2001;63(11):2185–2196. [PubMed] [Google Scholar]
- 12.Gidding SS, Leibel RL, Daniels S, Rosenbaum M, Van Horn L, Marx GR. Understanding obesity in youth. A statement for healthcare professionals from the Committee on Atherosclerosis and Hypertension in the Young of the Council on Cardiovascular Disease in the Young and the Nutrition Committee, American Heart Association. Writing Group. Circulation. 1996;94(12):3383–3387. doi: 10.1161/01.cir.94.12.3383. [DOI] [PubMed] [Google Scholar]
- 13.Kubik MY, Story M, Davey C. Obesity prevention in schools: current role and future practice of school nurses. Prev Med. 2007;44(6):504–507. doi: 10.1016/j.ypmed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Department of Commerce. Historical statistics of the United States Colonial Times to 1970; Current population reports, Serios P-20, various years; and current population survey, October, 1970 through 2008 (This table was prepared August 2009) [Accessed February 20, 2015]; Available at: http://nces.ed.gov/programs/digest/d09/tables/dt09_007.asp.
- 15.Pbert L, Druker S, Gapinski MA, et al. A school nurse-delivered intervention for overweight and obese adolescents. J Sch Health. 2013;83(3):182–193. doi: 10.1111/josh.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans. 6. Washington, DC: 2005. [Accessed January 11, 2016]. Available at: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm. [Google Scholar]
- 17.Adolescent Health Care: A Practical Guide. 5. Philadelphia, PA: Lippincott Williams and Wilkins; 2005. [Google Scholar]
- 18.Carrel AL, Bernhardt DT. Exercise prescription for the prevention of obesity in adolescents. Curr Sports Med Rep. 2004;3(6):330–336. doi: 10.1007/s11932-996-0008-1. [DOI] [PubMed] [Google Scholar]
- 19.Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 20.Rukavina PB, Li W. School physical activity interventions: do not forget about obesity bias. Obes Rev. 2008;9(1):67–75. doi: 10.1111/j.1467-789X.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- 21.McCall A, Raj R. Exercise for prevention of obesity and diabetes in children and adolescents. Clin Sports Med. 2009;28(3):393–421. doi: 10.1016/j.csm.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Lytle LA, Nichaman MZ, Obarzanek E, et al. Validation of 24-hour recalls assisted by food records in third-grade children. The CATCH Collaborative Group. J Am Diet Assoc. 1993;93(12):1431–1436. doi: 10.1016/0002-8223(93)92247-u. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow RE, Ory MG, Klesges LM, Cifuentes M, Fernald DH, Green LA. Practical and relevant self-report measures of patient health behaviors for primary care research. Ann Fam Med. 2005;3(1):73–81. doi: 10.1370/afm.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(suppl 11):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 25.Grunbaum JA, Kann L, Kinchen SA, et al. Youth risk behavior surveillance - United States, 2001. Morb Mortal Wkly Rep Surveill Summ. 2002;51(4):1–62. [PubMed] [Google Scholar]
- 26.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13(10):1739–1748. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 27.Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: a school-based obesity prevention program for adolescent girls. Prev Med. 2003;37(1):41–51. doi: 10.1016/s0091-7435(03)00057-4. [DOI] [PubMed] [Google Scholar]
- 28.Motl RW, Dishman RK, Ward DS, et al. Perceived physical environment and physical activity across one year among adolescent girls: self-efficacy as a possible mediator? J Adolesc Health. 2005;37(5):403–408. doi: 10.1016/j.jadohealth.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 31.Rand I. A Million Random Digits with 100,000 Normal Deviates. Pittsburgh, PA: American Book Publishers; 2001. [Google Scholar]
- 32.Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children’s screen time for reduction. Pediatrics. 2011;128(7):e193–e210. doi: 10.1542/peds.2010-2353. [DOI] [PubMed] [Google Scholar]
- 33.Boutelle KN, Libbey H, Neumark-Sztainer D, Story M. Weight control strategies of overweight adolescents who successfully lost weight. J Am Diet Assoc. 2009;109(12):2029–2035. doi: 10.1016/j.jada.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 34.National Association of School Nurses. School Nursing in the United States Quantitative Study. Burkhardt Research Services; 2007. [Accessed February 20, 2015]. Available at: http://www.nasn.ore/portals/0/2007/_Burkhardt_Report.pdf. [Google Scholar]
- 35.National Association of School Nurses. [Accessed February 20, 2015];Overweight and obesity in youth in schools - The role of the school nurse. 2012 Available at: http://www.nasn.org/PolicyAdvocacy/PositionPapersandReports/NASNPositionStatementsFullView/tabid/462/ArticleId/39/Overweight-and-Obesity-in-Youth-in-Schools-The-Role-of-the-School-Nurse-Revised-2011.