Abstract
Vitamin D deficiency and insufficiency may further increase fracture risk in patients with decreased bone mineral density. A cross-sectional study on serum vitamin D concentrations in medical inpatients was conducted at Bassetlaw District General Hospital between April 2014 and January 2015 (10 months), and the relationship of serum vitamin D concentrations with calcium and alkaline phosphatase was evaluated. 25-Hydroxyvitamin D immunoassays were used and analyzed in the local laboratory. The total number of patients analyzed was 200, age range 18–99 years, with mean age of 76 years. The most common presentation was found to be fall/collapse. The following cutoff points for serum vitamin D were used: levels ≤30 nmol/L for severe deficiency, >30–50 nmol/L for moderate deficiency, >50–75 nmol/L for mild deficiency, and anything above 75 nmol/L as normal. Of the 209 participants examined, 78 (37.3%) participants had mild vitamin D deficiency, 54 (25.8%) participants had moderate vitamin D deficiency, 68 (32.5%) participants had severe vitamin D deficiency, and 9 (4.3%) participants with low vitamin D levels died during their admission. Of the 122 moderate/severe patients, 70 (57.4%) patients had their vitamin D deficiency treated, according to local Trust guidelines. The study found no relationship between serum calcium levels and vitamin D deficiency, whereas patients’ alkaline phosphatase levels were found to be higher with increased severity of vitamin D deficiency. The study examined the implications of untreated severe/moderate vitamin D deficiency compared to treated deficiency, in terms of the frequency of readmission with similar complaints. It was found that the rate of readmission within one year in patients who were not treated was 57%, compared to 48% in patients whose vitamin D deficiency was treated. Presenting after falls was a recurring theme. It was concluded that even if moderate vitamin D deficiency can be asymptomatic, it is important to correct it as it can have an impact on morbidity and readmission rates in the long term.
Keywords: vitamin D deficiency, insufficiency, calcium, alkaline phosphatase
Introduction
Vitamin D plays an important role in bone mineral regulation and bone health. Deficiency of vitamin D, which manifests as bone disease, is characterized by impaired bone mineralization. In recent years, the term insufficiency has been used to describe low levels of serum vitamin D that may be associated with other disease outcomes.1
Interest in vitamin D deficiency is driven by its common occurrence and its wide range of effects. Sun exposure is responsible for the conversion of vitamin D to active form, and it is also obtained from dietary sources. People at risk of deficiency are those with poor nutritional intake, insufficient exposure to sun, and/or defective intestinal absorption. Daily intake of vitamin D in the general population does not often meet the level needed to maintain optimum Vitamin D concentrations. Deficient patients are often offered supplements, but clinicians may be unsure of the optimal dose and how best to monitor the therapy.
Vitamin D deficiency leads to decreased intestinal absorption of calcium, which further leads to increased bone turnover, resulting in secondary hyperparathyroidism. It has been shown that vitamin D supplementation helps to decrease the number of reported falls in elderly populations and to improve muscle strength and prevent fragility fractures as a consequence of the falls.2 Therefore, patients who are at risk of falls and known to have fragility fractures should be investigated for vitamin D deficiency.3
Clinicians should routinely test for vitamin D deficiency in patients who present with symptoms of generalized weakness, muscle aches, and other musculoskeletal complaints, as these are often misdiagnosed as chronic fatigue, depression, fibromyalgia, etc.4 Some studies have established that 80%–90% of individuals with musculoskeletal pain and weakness are vitamin D deficient.5 Moreover, low levels of vitamin D can indicate poor general nutritional status in a patient, or secondary or chronic illness, and hence decreased outdoor activities. In such individuals, a placebo-controlled trial showed that vitamin D supplementation does not improve symptom control, as various other factors are in play.6 This study has tried to explore the relationship between vitamin D and other variables, such as levels of alkaline phosphatase and serum calcium, and the impact of vitamin D deficiency on elderly patients’ morbid status and their readmission rates in Bassetlaw Hospital, UK, which has 300 beds in the district general hospital. Each year, the hospital treats around 33,000 patients along with 38,000 emergencies in the A&E Department, thereby exploring whether treating moderate to severe vitamin D deficiency would decrease the rate of their readmissions with recurring presenting complaints.
Aim
The aim of the study was to determine vitamin D deficiency in at-risk elderly inpatients in medical wards in Bassetlaw Hospital, UK, by measuring blood serum levels and studying the relationship with serum calcium and alkaline phosphatase levels. We also examined the consequences of untreated severe vitamin D deficiency compared to treated deficiency.
Methods
Retrospective data were collected from a random cross-sectional sample of 209 patients admitted to the medical wards who had their vitamin D levels checked over a period of 10 months between April 2014 and January 2015. The data collected specifically included age, sex, sample day, laboratory number, location, specific identifier number, vitamin D levels grouped according to their severity, corrected calcium levels, alkaline phosphatase levels, if treated or not, reason for admission, diagnosis, number of readmissions in the following year, and reason for readmissions. Random selection was used to yield a patient sample population treated by different medical subspecialties, such as gastroenterology, endocrinology, stroke rehabilitation, and general medical wards. The research was exempted from Research Ethics Committee review as it comprised a secondary use of anonymized data previously collected in the course of normal care.
An Excel spreadsheet was created to ensure concise data collection. Each junior doctor collected approximately 50 sets of data, and a total of 200 completed datasets and results were analyzed. Quantitative methodology was employed, and the data were further examined using a correlational statistical analysis.
Patients whose blood levels of vitamin D, calcium, and alkaline phosphatase had been measured were identified with the help of a list obtained from pathology (biochemistry laboratory), and an electronic order request system was used to retrieve the biochemical data. Results were reviewed, and patients were categorized as having adequate levels (>75 nmol/L), mild deficiency (50–73 nmol/L), moderate deficiency (30–50 nmol/L), and severe deficiency (<30 nmol/L). Treatment given was identified by using E-Prescribing and Medicines Administration, the administration charts and medication prescribed on the system. Discharge letters and rates of readmission over the next year were reviewed using the same system as described earlier.
Results
The total number of patients was 200, of which 62% were female. The average age was 76 years. Patient demographics are further outlined in Figure 1.
Figure 1.
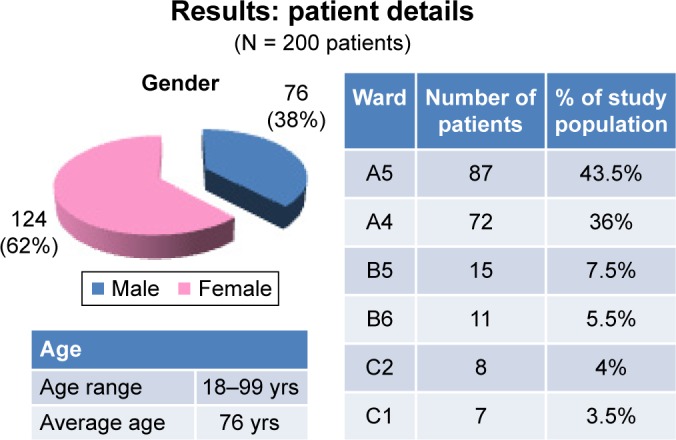
Patient demographics.
Of the 209 participants (Fig. 2), 37.3% had mild vitamin D deficiency, 25.8% had moderate vitamin D deficiency, and 32.5% had severe vitamin D deficiency. The final results exclude 4.3% who died during their admission. Furthermore, 57.4% of the moderate/severe patients had their vitamin D deficiency treated, according to local Trust guidelines.
Figure 2.
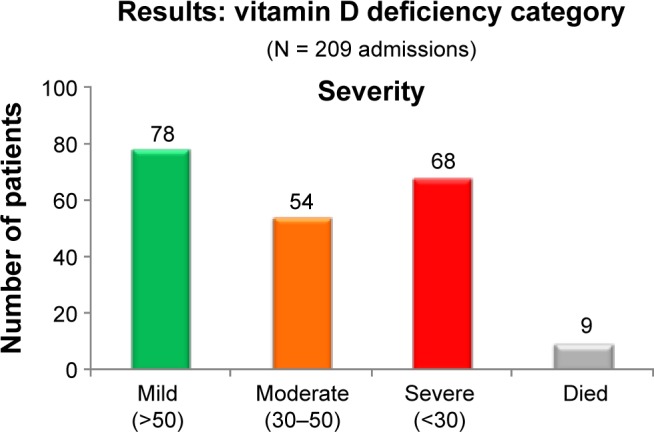
Severity of vitamin D deficiency.
Mann–Whitney U test was applied to compare the data, and no relationship was identified between vitamin D deficiency and serum calcium levels. One finding of note was that serum alkaline phosphatase level rose with the severity of vitamin D deficiency as depicted in Figures 3 and 4.
Figure 3.
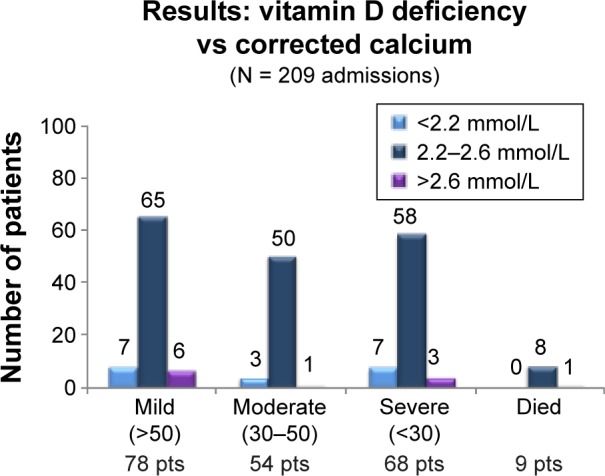
Vitamin D deficiency and corrected calcium levels.
Note: Pts is used as an abbreviation for patients in this and subsequent figures.
Figure 4.
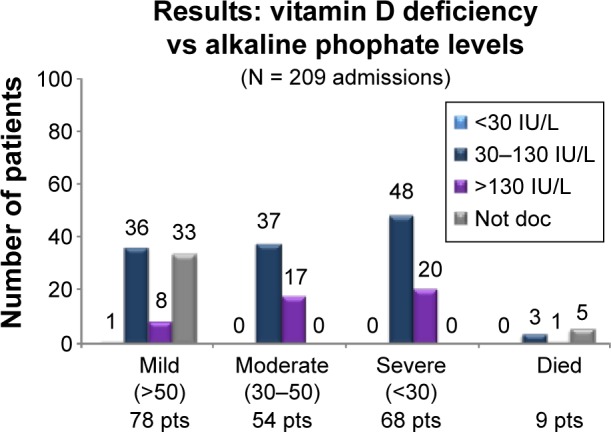
Vitamin D and alkaline phosphatase levels.
The most common presenting complaint in patients with moderate/severe vitamin D deficiency was found to be falls/collapse. Other common presentations are outlined in Figures 5 and 6 in their descending order.
Figure 5.
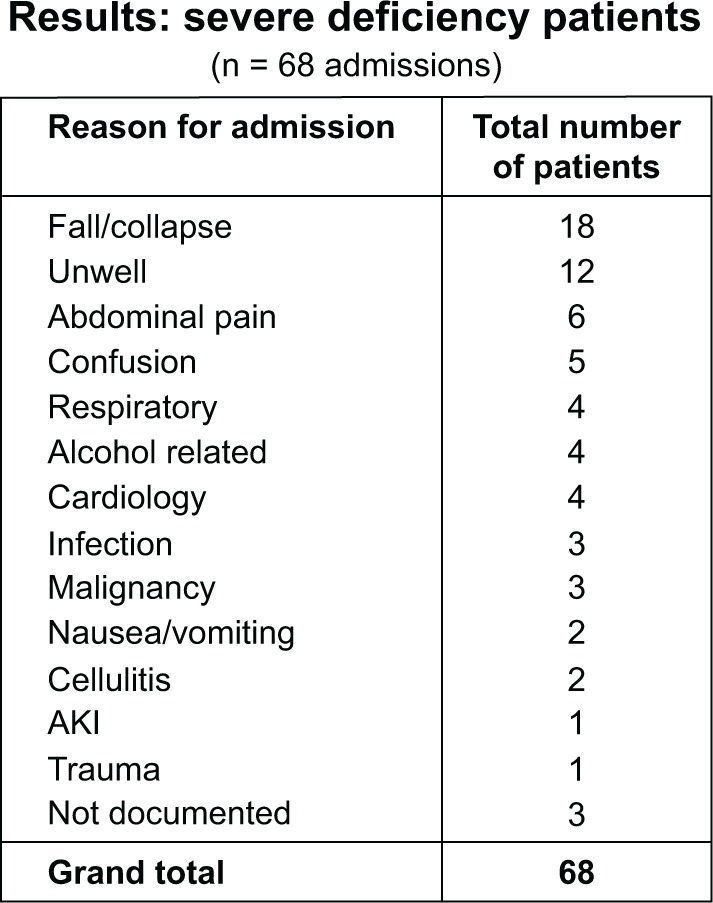
Reasons for admission in severe vitamin D deficiency patients.
Figure 6.
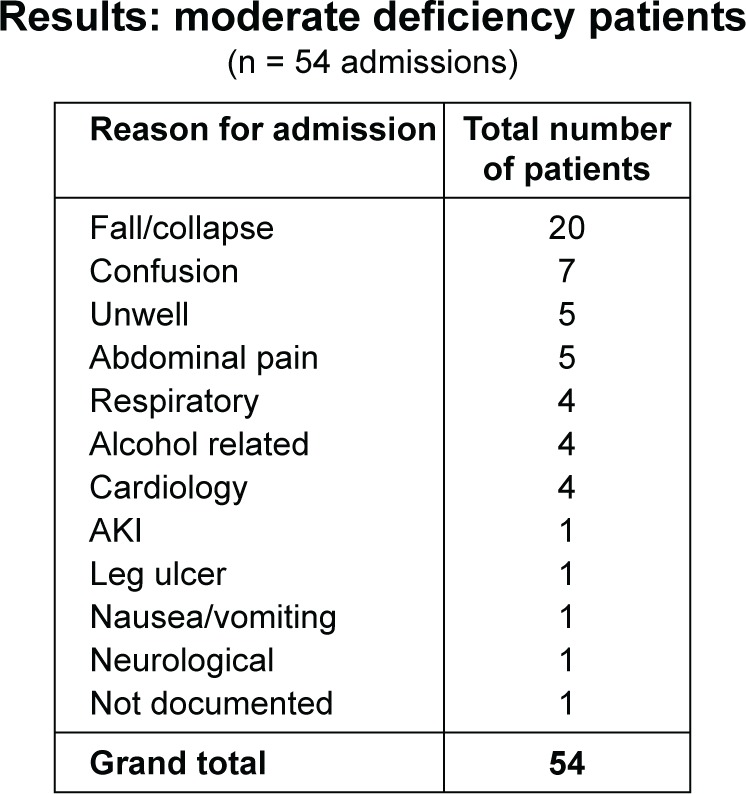
Reasons for admission in moderate vitamin D deficiency patients.
Of patients who were not treated for their vitamin D deficiencies, 57% were readmitted over the next year, whereas the rate of readmission in patients treated was found to be 48%, with falls as a recurring theme for readmissions. Besides falls being the most common presentation, other reasons for admission identified was patients being generally unwell as the second commonest in severe deficiency and confusion in moderate. Respiratory causes were mainly lower respiratory tract infection or infective exacerbations of underlying lung disease. Cardiological causes were mainly chest pains-ACS, bradyarrythmias, or tachyarrythmias.
Discussion
Subclinical vitamin D deficiency or vitamin D insufficiency is common and is defined as a lower than normal vitamin D level that has no visible signs or symptoms. However, vitamin D insufficiency is often associated with a reduced bone density (osteopenia or osteoporosis) in some cases a mild decrease in the blood calcium level, an elevated parathyroid hormone (which accelerates bone resorption), and an increased risk of falls, all of which can seriously affect a person’s quality of life.7 Thus, identifying and treating vitamin D insufficiency or deficiency is important to maintain bone strength. Treatment may even improve the health of other body systems, such as the immune, muscular, and cardiovascular systems, although more research is needed in these areas.
In view of the above findings revealed by this study, it may be warranted to check vitamin D levels in patients with raised alkaline phosphatase. No relationship was identified between vitamin D deficiency and serum calcium levels, a finding consistent with a recent study by Ferreira et al.8 According to some studies, adverse effects of low vitamin D levels are seen below 50 nmol/L,9 whereas a higher threshold was suggested by other studies. One such study conducted by Lips10 has classed levels between 50 and 25 nmol/L as insufficiency, whereas levels below 25 nmol/L would be classed as deficiency. Proximal myopathy and increased bone turnover may be found in levels between 25 and 12 nmol/L,11 whereas in osteomalacia, levels can be below 10 and 12 nmol/L.12
There is a lack of research on the topic of what levels of vitamin D should be classed as low. Plasma vitamin D levels often reflect a lifestyle of indoor or outdoor activities or geographical variations in terms of sun exposure rather than an average vitamin D status. However, it is seen that as age advances, dermal vitamin D production decreases.13 In a study by Thacher and Clarke,14 it was argued whether the threshold levels for serum vitamin D should be lowered, and it was found that levels are generally lower in people who have experienced a fracture.
A survey performed in 2001 by Lips,15 in various locations including the USA, Australia, Europe, and others, found vitamin D insufficiency to be frequent among elderly institutionalized patients. Patients living in nursing homes and care homes for the elderly, according to the study, “had plasma 25OHD levels of 9–37 nmol/L in Europe compared with 53–45 nmol/L in the USA and 26–40 nmol/L in Australia. Geriatric patients had mean levels of 3–29 nmol/L in Europe compared with 45–71 nmol/L in the USA.”16 In this study with medical inpatients, where the average age of the patients was 76 years, 58.3% of patients had levels lower than 50 nmol/L, of which 32.5% had levels between 3 and 29 nmol/L.
It was found in an Australian cross-sectional study that falls risk in the elderly was directly proportional to vitamin D status;17 treatment improved myopathy but did not improve the muscle strength.18 It is obvious that vitamin D deficiency leads to muscle weakness and impaired muscle function, which is reversible with vitamin D supplementation.19 In this study, it was identified that patients with moderate and severe vitamin D deficiency treated with 100,000 units of colecalciferol per month for three months and then daily supplementation onward at a lower dose had a readmission rate of 9 percentage points lower than that of patients who were not treated for vitamin D deficiency. The most recurring reason for readmission was found to be falls in the untreated group. For those whose vitamin D deficiency was treated, most readmissions were attributed to other comorbidities. It was established by a meta-analysis on the effect of vitamin D and its relationship to falls that vitamin D supplementation reduces the risk of falls by 20% in older individuals with stable health.20 Hence it can be concluded that even if moderate vitamin D deficiency can be asymptomatic, it is important to correct it as it can have an important impact on morbidity and readmission rates in the long term. This study has tried to establish the rate of readmissions for untreated vitamin D deficiency versus treated in medical inpatients in UK, and we have established two important things that raised alkaline phosphatase in elderly should trigger checking their vitamin D levels and that treated vitamin D deficiency would help reducing the number of readmissions in elderly with falls. Impact on readmission of corrected vitamin D deficiency versus untreated over a longer period can be evaluated in future studies.
Footnotes
ACADEMIC EDITOR: Joseph Zhou, Editor in Chief
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 2109 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: SAHZ, GS, OO, RK, MA, SS, FB, CR. Analyzed the data: SAHZ, GS, OO, RK, MA, SS, FB, CR. Wrote the first draft of the manuscript: SAHZ, GS, OO, RK, MA, SS, FB, CR. Contributed to the writing of the manuscript: SAHZ, GS, OO, RK, MA, SS, FB, CR. Agree with manuscript results and conclusions: SAHZ, GS, OO, RK, MA, SS, FB, CR. Jointly developed the structure and arguments for the paper: SAHZ, GS, OO, RK, MA, SS, FB, CR. Made critical revisions and approved final version: SAHZ, GS, OO, RK, MA, SS, FB, CR. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Bischoff HA, Stahelin HB, Dick W, et al. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res. 2003;18:343–351. doi: 10.1359/jbmr.2003.18.2.343. [DOI] [PubMed] [Google Scholar]
- 3.Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293:2257–2264. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 4.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–373. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 5.Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003;78:1463–1470. doi: 10.4065/78.12.1463. [DOI] [PubMed] [Google Scholar]
- 6.Arvold DS, Odean MJ, Dornfeld MP, et al. Correlation of symptoms with vitamin D deficiency and symptom response to cholecalciferol treatment: a randomized controlled trial. Endocr Pract. 2009;15:203–212. doi: 10.4158/EP.15.3.203. [DOI] [PubMed] [Google Scholar]
- 7.Bischoff HA, Stahelin HB, Tyndall A, Theiler R. Relationship between muscle strength and vitamin D metabolites: are there therapeutic possibilities in the elderly? Z Rheumatol. 2000;29(suppl 1):39–41. doi: 10.1007/s003930070037. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira Tda S, Rocha TM, Klein MR, Sanjuliani AF. Vitamin d deficiency is associated with insulin resistance independent of intracellular calcium, dietary calcium and serum levels of parathormone, calcitriol and calcium in premenopausal women. Nutr Hosp. 2015;31(4):1491–1498. doi: 10.3305/nh.2015.31.4.8490. [DOI] [PubMed] [Google Scholar]
- 9.Lamberg-Allardt C, Brustad M, Meyer HE, et al. Vitamin D—a systematic literature review for the 5th edition of the Nordic Nutrition Recommendations. Food Nutr Res. 2013;3:57. doi: 10.3402/fnr.v57i0.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22:477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 11.Parfitt AM. Osteomalacia and related disorders. In: Avioli LV, Krane SM, editors. Metabolic Bone Diseases and Clinically Related Disorders. San Diego: Academic Press; 1998. pp. 327–386. [Google Scholar]
- 12.Holick MF. Vitamin D: photobiology, metabolism, mechanism of action and clinical application. In: Favus MJ, editor. Primer on the Metabolic Bone Diseases and Mineral Metabolism. 4th ed. Philadelphia: Lippincott, Williams & Wilkins; 1999. pp. 92–98. [Google Scholar]
- 13.Center JR, Nguyen TV, Sambrook PN, Eisman JA. Hormonal and biochemical parameters and osteoporotic fractures in elderly men. J Bone Miner Res. 2000;15:1405–1411. doi: 10.1359/jbmr.2000.15.7.1405. [DOI] [PubMed] [Google Scholar]
- 14.Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50–60. doi: 10.4065/mcp.2010.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22:477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 16.Bellido T, Boland R, Teresita BB, Ricardo BB. Effects of 1,25-dihydroxyvitamin D3 on phosphate accumulation by myoblasts. Horm Metab Res. 1991;23:113–116. [PubMed] [Google Scholar]
- 17.Pfeifer M, Begerow B, Minne HW, et al. Vitamin D status, trunk muscle strength, body sway, falls, and fractures among 237 postmenopausal women with osteoporosis. Exp Clin Endocrinol Diabetes. 2001;109:87–92. doi: 10.1055/s-2001-14831. [DOI] [PubMed] [Google Scholar]
- 18.Grady D, Halloran B, Cummings S, et al. 1,25-Dihydroxyvitamin D3 and muscle strength in the elderly in a randomised controlled trial. J Clin Endocrinol Metab. 1991;73:1111–1117. doi: 10.1210/jcem-73-5-1111. [DOI] [PubMed] [Google Scholar]
- 19.Glerup H, Mikkelsen K, Poulsen L, et al. Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited. J Intern Med. 2000;247:260–268. doi: 10.1046/j.1365-2796.2000.00595.x. [DOI] [PubMed] [Google Scholar]
- 20.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA. 2004;291:1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]


