Abstract
In response to the lack of therapeutics for internal bleeding following a traumatic event, we synthesized hemostatic dexamethasone nanoparticles (hDNP) to help alleviate internal hemorrhaging. hDNP consist of a block copolymer, poly(lactic-co-glycolic acid)-poly(l-lysine)-poly(ethylene glycol) conjugated to a peptide, glycine-arginine-glycine-aspartic acid-serine (GRGDS). These particles were evaluated as treatment for primary blast lung injury in a rodent model. Animals were randomly placed into test and control groups, exposed to blast and given immediate injection. Recovery was assessed using physiological parameters and immunohistochemistry. We found that dexamethasone-loaded hemostatic nanoparticles alleviate physiological deprivation caused by blast injury and reduce lung injury damage.
Keywords: nanoparticles, trauma, dexamethasone, synthetic platelets, hemostatic
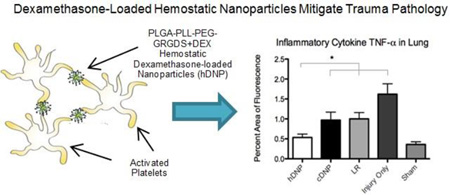
Graphical Abstract
Primary blast lung injury (PBLI) is a significant cause of death due to internal hemorrhage following detonation of improvised explosive devices (IEDs)1. Explosions cause the majority of injuries in the current conflicts, accounting for 79% of combat related injuries2. The need for a readily assessable treatment to decrease mortality of those who suffer from closed-chest lung trauma is obvious. Moreover, it is vital that treatment must occur within the first hours following injury to increase survival. Our blast trauma rodent model can be utilized as a tool to assess the novel nanotherapeutics3. There is a clear call for therapeutic intervention for treating severe lung injury, as well as internal hemorrhage, immediately after blast exposure4,5.
Several physiological parameters change following lung injury. Hypoxemia, monitored by a reduction in PAO2, was seen following PBLI. Reduced heart rate and presence of hypotension are also well-documented during pulmonary hemorrhage leading to a ventilation-perfusion mismatch6,7. It has been reported that blast injury can cause infiltration of red blood cells (RBCs) in the alveolar spaces, as well as biochemical changes in the lungs8. Inflammatory cytokines, such as TNF-α and IL-6, have been reported following PBLI. Knoferl, et al.6 demonstrated that levels of TNF-α and IL-6 were elevated three hours post-blast in blood plasma due to thoracic trauma. As such, these documented biological parameters can be used to confirm injury and monitor injury mediation following treatment.
Due to the lack of therapies that specialize in mitigating internal hemorrhage after trauma, our efforts focused on synthesizing functionalized nanoparticles to target and assist clotting to reduce internal bleeding. The functionalized nanoparticles were composed of a block copolymer, poly(lactic-co-glycolic acid)-poly(l-lysine)-poly(ethylene glycol) (a detailed description of the synthesis is described in the Supplementary Information). We conjugated the polymer with a peptide, glycine-arginine-glycine-aspartic acid-serine (GRGDS), to enable binding with the glycoprotein IIb/IIIa receptor found on activated platelets. (A control formulation conjugated of the peptide GRADSP was used to confirm the activity of these particles). These particles have proven to mitigate internal bleeding in several models of bleeding9–11. In a model of blast polytrauma, hemostatic nanoparticles (hNP) were shown to increase survival and reduce lung injury11. Because these particles are based on PLGA, they lend themselves to application as a drug delivery vehicle that leverages their entrapment in the clots for local delivery.
We determined that dexamethasone would be a suitable steroid-link for this hNP treatment due to its anti-inflammatory properties and non-effect on coagulation. It is a corticosteroid that has been shown to reduce programmed cellular death, or apoptosis, due to hemorrhage in the brain while also inhibiting inflammation after injury12. In lung injury models, dexamethasone in conjunction with targeting nanogels, has been shown to alleviate pulmonary inflammation one day after administration13. Sustained delivery of dexamethasone from coated nanoparticles has been shown to be necessary to elicit biological effects14. By reducing the effects of pro-inflammatory cytokines responsible for tissue damage after injury, dexamethasone is an attractive option for treatment of PBLI, and the drug lends itself to encapsulation in a hemostatic nanoparticle formulation to aid recovery following injury. This study focused on how well the fabricated nanoparticles reduced the initial hemorrhage within the lungs as well as the effectiveness of the local dexamethasone delivery at seven days following injury.
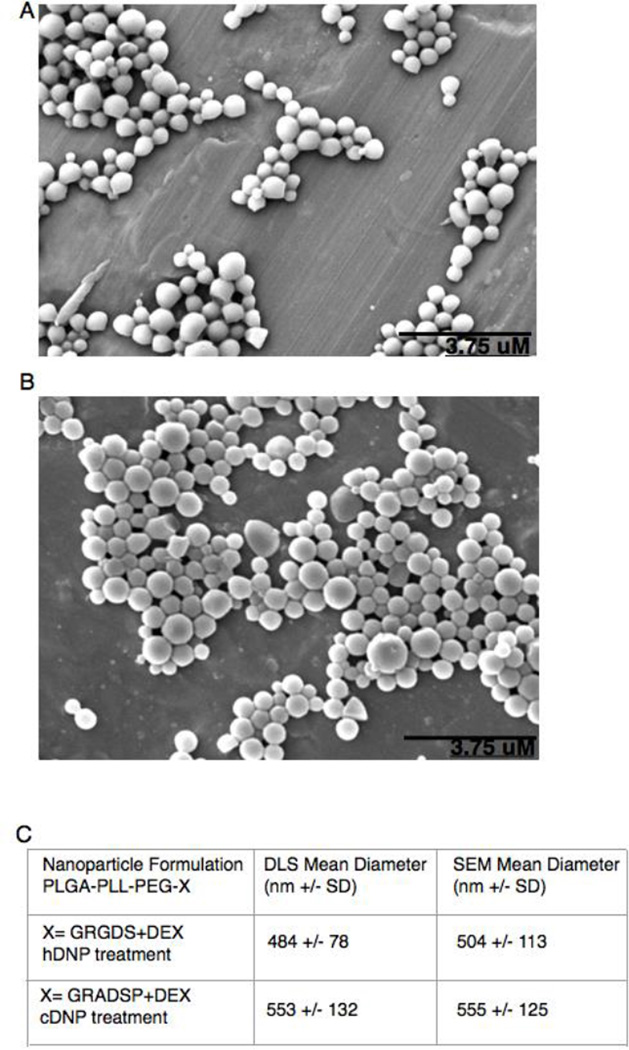
A representative scanning electron microscope (SEM) image of the particles (Figure 1A) shows that the treatment is a spherical nanoparticle of approximately 500 nm in size. This sizing measurement is confirmed by dynamic light scattering (DLS) measurement (Figure 1B).
Figure 1.
(A) SEM of hemostatic dexamethasone loaded nanoparticles (hDNPs) (B) SEM of control dexamethasone loaded nanoparticles (cDNPs) (C) Particle size as measured by SEM and DLS.
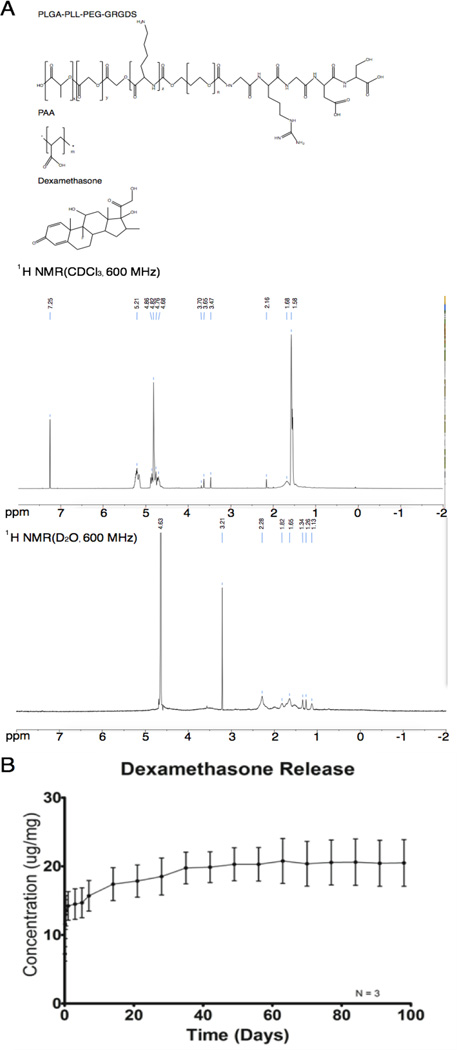
Nuclear magnetic resonance (NMR) data indicated that the poly(ethylene glycol) (PEG) arms form a corona when suspended in aqueous solution, indicated by in increased size of the PEG peak (δ = 3.21) in deuterated water (D2O) in relation to other peaks. In addition the dexamethasone peaks were visible in deuterated chloroform (CDCl3) indicating that the dexamethasone is encapsulated by the particles. Total loading of the dexamethasone is 22 ug/mg. Release data showed that the majority (65%) of the dexamethasone is released within the first 24 hours of incubation (Figure 2B). After 63 days, 95% of the loaded dexamethasone has been released.
Figure 2.
(A) Molecular structure of nanoparticles as well as dexamethasone. Characterization of the nanoparticles by NMR in deuterated chloroform and deuterated water, showing the presence of the PEG corona (B) Release of dexamethasone from hemostatic nanoparticles over time.
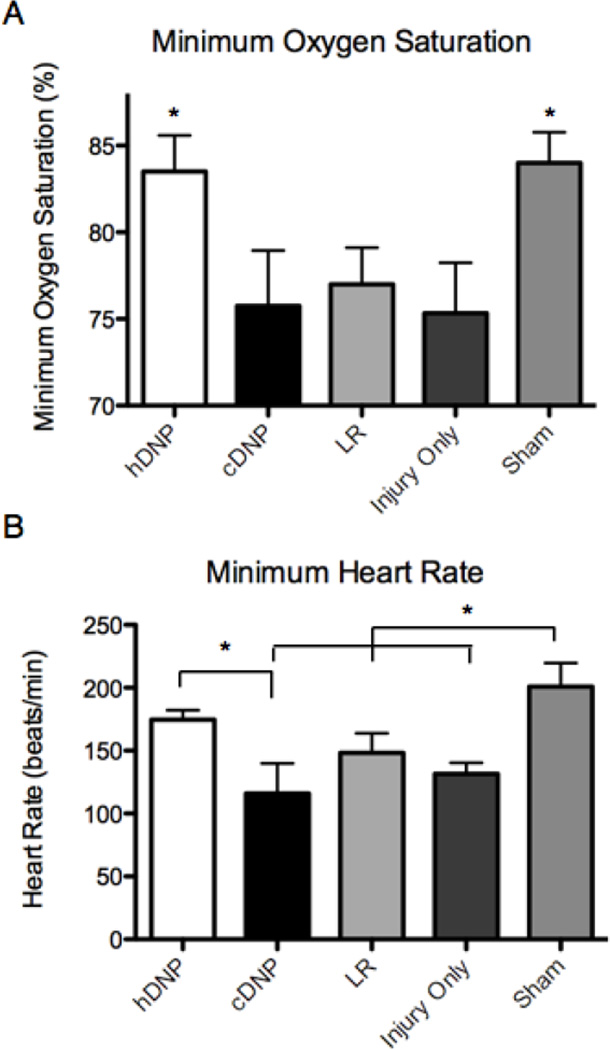
We found that treatment with hDNP improved outcomes in acute measures of injury. Reduced levels of oxygen saturation after lung trauma are harmful to survival as well as tissue health. There was a significant difference between the hDNP and the other blast groups (cDNP, LR, and IO) in terms of minimum oxygen saturation during the one-hour post-blast monitoring period (p-value < 0.05). (Figure 3A) This suggests that animals treated with hDNP experience a more immediate level of recovery in terms of lung functionality in supplying oxygen to the body. Characterization of the particles shows that they can deliver a burst of dexamethasone at an injury site during the few hours after injury, which may also reduce the longer-term effects of PBLI (see particle biodistribution in Supporting Information; Figure S2). As commented on in Brown, et al.15, the compensatory response during lung contusion of the undamaged areas of the lung plays an important role in combating hypotension and apnea after initial trauma16. When evaluating the acute heart rate response following injury, similar trends were observed as the hDNP group was higher when compared to the cDNP group. (Figure 3B)
Figure 3.
(A) Oxygen saturation in treatment groups after injury. (B) Minimum heart rate in treatment groups after injury. * p-value < 0.05
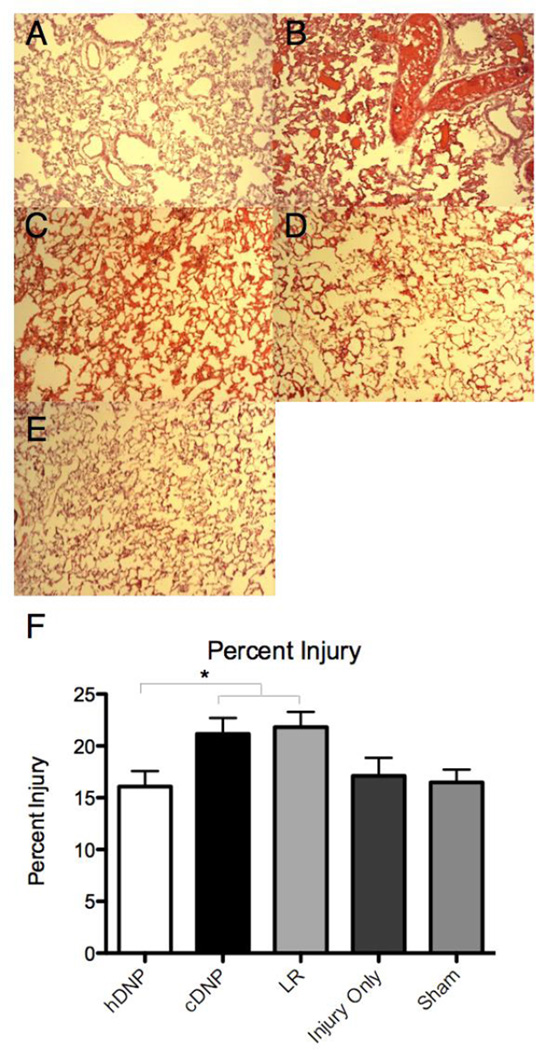
Previously, a PBLI model was shown to produce lesions in the left lobe as well as bilateral traumatic pulmonary hemorrhage17. Contusion and hemorrhaging in the left lobe has been correlated with a higher incidence of lethal outcomes in preliminary studies3. Figure 4A–E displays representative images of each group and the staining of RBCs in the lung cross-section. Figure 4F demonstrates that the hDNP treatment, as well as the uninjured sham group, had significance when compared to the cDNP and LR groups, which may also help account for a better outcome in oxygen saturation. Although percent injury in the IO group was higher than the hDNP group, there was not a significant difference. This could be due to variability in injury sustained from the blast, which can be influenced by factors including inhalation/respiration status. One mechanism of lung injury progression suggests that the amount of free actin in the circulation from dying cells that can obstruct circulation in the lungs and destroy pulmonary endothelium18. This mechanism could pose a delayed response of apoptosis in the lungs and can show how assuaging the injury in the acute stages can alleviate ensuing cellular degradation. Delayed pulmonary injury is indirectly due to extravasated blood components15,19.
Figure 4.
Representative H&E staining for (A) hDNP (B) cDNP (C) LR (D) IO and (E) Sham. (F) The hDNP and sham demonstrated a decreased lung injury level compared to the cDNP and LR groups (* p < 0.05) at seven days after blast.
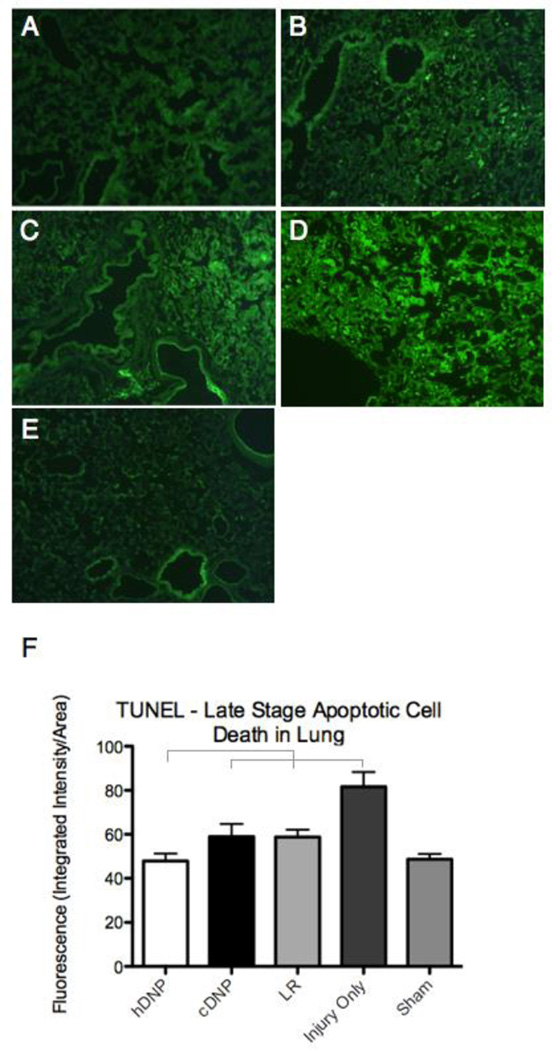
Apoptotic markers, such as terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) and cleaved caspase-3, were measured to provide a representation of various stages within the apoptosis cascade. Lee, et al. has shown that apoptosis is elevated in low oxygen environments20. As described in Seitz, et al.21, apoptosis of alveolar type-2 cells contributed to the loss of epithelial cells following lung contusion. Figure 5A–E shows representative images from the TUNEL assay on the lung tissue. The hDNP group had a significantly lower amount of late stage apoptosis compared to the other blast groups (cDNP, LR, and IO) at the seven day time point after injury (p<0.05). (Figure 5F)
Figure 5.
Representative TUNEL staining for (A) hDNP (B) cDNP (C) LR (D) IO and (E) Sham. (F) The hDNP group and sham group are significantly different compared to the cDNP, LR, and IO groups (* p<0.05) at seven days after injury.
Figure S3A–E (found in Supporting Information) shows representative images from cleaved caspase-3 immunofluorescence on the left lobe. The hDNP group, also, had a lower, though insignificant, amount of early stage apoptosis compared to the other blast groups (cDNP, LR, and IO) at the seven day time point after injury (Figure S3F; Supporting Information). Knowing that apoptosis of epithelial cells are a result of many post-injury mechanisms, decreased levels of early and late stage apoptotic signals with the hDNP group is a promising result, indicating that this treatment may have a protective effect on surviving cells after trauma.
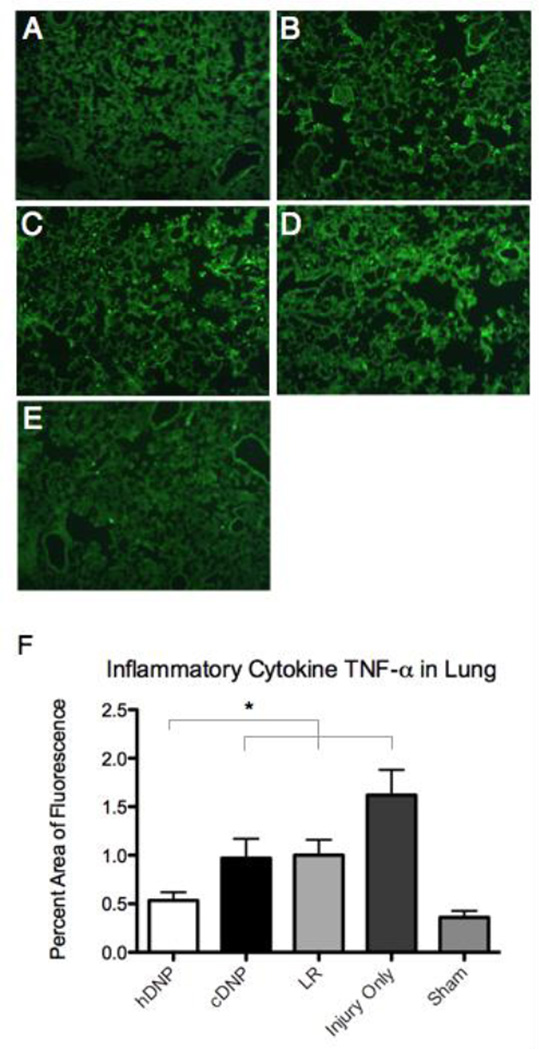
Injury-induced cytokines are known to contribute to tissue damage15. TNF-α has been shown to induce apoptosis leading to cleavage of DNA into fragments. In a study by Liener, et al.22, programmed cell death was identified as a cellular mechanism after pulmonary contusion. In a brain ischemia-induced lung injury model, TNF-α positive epithelial cells were seen in lung tissue three days after injury23. In a model of interleukin-2-induced microvascular lung injury, TNF-α was seen elevated in the lung tissue while having undetectable levels in blood serum indicating that local mechanisms are responsible for inflammation and injury progression24. In other models of lung disease, TNF-α protein levels in the tissue were seen at chronic time points (weeks)25. Figure 6A–E shows representative images from TNF-α targeting. For percent area of TNF-α fluorescence, the hDNP and sham group were significantly reduced compared to the other blast groups (cDNP, LR, and IO) at the seven day time point (p<0.05). (Figure 6F)
Figure 6.
Representative fluorescent images of TNF-α. (A) hDNP (B) cDNP (C) LR (D) IO and (E) Sham (F) The average percent area of the TNF-α fluorescence. (* - p<0.05)
Decreased TNF-α levels at seven days indicates that the hDNP group is effective at mitigating inflammation as well as cellular injury cascades compared to controls after injury.
Multiple administrations of dexamethasone as treatment for lung injury have resulted in therapeutic benefits, reducing percent injury of the hemorrhage and anatomical implications of emphysema26. These same curative effects can be seen in our study, but with only a single administration of hDNP. Targeting activated platelets creates efficiency of dexamethasone’s therapeutic effect11. Administration of hDNP has the potential to be a viable option for open field trauma care because of its effectiveness in reducing lung damage and improving oxygen exchange as well as ease of delivery. Treatment with hDNP significantly decreased acute hemorrhaging and alleviated cellular damage of lungs at a subactute stage. The lower levels of TNF-α, accompanied by reduced levels of apoptosis in the hDNP group show a therapeutic effect at a delayed time point. Findings of increased oxygen saturation and lower cell death in the lungs for the hDNP group demonstrate promising therapeutic roles in trauma care.
Results from Elsayed, et al.8 stress the need for initiating treatment within the first hour following blast exposure due to oxidative stress, pulmonary hemorrhage, and rupture of alveolar walls in the lungs. Due to the absence of therapeutics that target internal hemorrhage, we advocate that administered nanoparticles are a venue to produce this rapid response in cases of PBLI. The way hDNP affects the interplay between physiological parameters, percent hemorrhage, and apoptosis after injury is crucial for survival and healing. Examining the effects of nanoparticles on other inflammatory cytokines in the lungs and blood plasma as well as factors involved with oxidative stress can further validate their performance as a post-injury therapeutic. hDNP administration after traumatic injury can mitigate internal bleeding and improve lung pathologic outcomes.
Supplementary Material
Acknowledgments
The authors would like to thank Haiyan Zhang for assistance with histological techniques, as well as Shaylen Hall, Ryan Brady, Carly Norris and Bryce Dunn for assistance with microscopic imaging. Also, the authors would like to acknowledge the funding source: DOD CDMRP Program W81XWH-11-1-0014 and NIH Director’s New Innovator Award number DP20D007338
Footnotes
Associated Content
Supporting Information
Materials and methods, experimental details, and additional figures. This material is available free of charge via the Internet at http://pubs.acs.org.
References
- 1.Yeh DD, Schecter WP. World journal of surgery. 2012;36(5):966–972. doi: 10.1007/s00268-012-1500-9. [DOI] [PubMed] [Google Scholar]
- 2.Ramasamy A, Harrisson SE, Clasper JC, Stewart MPM. Journal of Trauma-Injury Infection and Critical Care. 2008;65(4):910–914. doi: 10.1097/TA.0b013e3181848cf6. [DOI] [PubMed] [Google Scholar]
- 3.Hubbard WB, Hall C, Sajja VS, Lavik E, VandeVord P. Biomedical sciences instrumentation. 2014 In Press. [PMC free article] [PubMed] [Google Scholar]
- 4.Huller T, Bazini Y. Archives of surgery. 1970;100(1):24–30. doi: 10.1001/archsurg.1970.01340190026008. [DOI] [PubMed] [Google Scholar]
- 5.Clifford CC. Military medicine. 2004;169(12 Suppl):8–10. 14. doi: 10.7205/milmed.169.12s.8. [DOI] [PubMed] [Google Scholar]
- 6.Knoferl MW, Liener UC, Seitz DH, Perl M, Bruckner UB, Kinzl L, Gebhard F. Shock. 2003;19(6):519–525. doi: 10.1097/01.shk.0000070739.34700.f6. [DOI] [PubMed] [Google Scholar]
- 7.Irwin RJ, Lerner MR, Bealer JF, Brackett DJ, Tuggle DW. The Journal of trauma. 1997;43(4):650–655. doi: 10.1097/00005373-199710000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Elsayed NM, Gorbunov NV. Toxicological sciences : an official journal of the Society of Toxicology. 2007;95(1):289–296. doi: 10.1093/toxsci/kfl138. [DOI] [PubMed] [Google Scholar]
- 9.Bertram JP, Williams CA, Robinson R, Segal SS, Flynn NT, Lavik EB. Science translational medicine. 2009;1(11):11ra22. doi: 10.1126/scitranslmed.3000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shoffstall AJ, Atkins KT, Groynom RE, Varley ME, Everhart LM, Lashof-Sullivan MM, Martyn-Dow B, Butler RS, Ustin JS, Lavik EB. Biomacromolecules. 2012;13(11):3850–3857. doi: 10.1021/bm3013023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lashof-Sullivan MM, Shoffstall E, Atkins KT, Keane N, Bir C, VandeVord P, Lavik EB. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(28):10293–10298. doi: 10.1073/pnas.1406979111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee IN, Cheng WC, Chung CY, Lee MH, Lin MH, Kuo CH, Weng HH, Yang JT. Journal of neuroscience research. 2014 doi: 10.1002/jnr.23454. [DOI] [PubMed] [Google Scholar]
- 13.Coll Ferrer MC, Shuvaev VV, Zern BJ, Composto RJ, Muzykantov VR, Eckmann DM. PloS one. 2014;9(7):e102329. doi: 10.1371/journal.pone.0102329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lo CT, Van Tassel PR, Saltzman WM. Biomaterials. 2010;31(13):3631–3642. doi: 10.1016/j.biomaterials.2010.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown RF, Cooper GJ, Maynard RL. International journal of experimental pathology. 1993;74(2):151–162. [PMC free article] [PubMed] [Google Scholar]
- 16.Irwin RJ, Lerner MR, Bealer JF, Mantor PC, Brackett DJ, Tuggle DW. The Journal of trauma. 1999;47(1):105–110. doi: 10.1097/00005373-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Gorbunov NV, Nath J, Parker JM, Zaucha GM. The Journal of trauma. 2003;54(3):574–583. doi: 10.1097/01.TA.0000043922.40376.38. [DOI] [PubMed] [Google Scholar]
- 18.Chavko M, Prusaczyk WK, McCarron RM. The Journal of trauma. 2006;61(4):933–942. doi: 10.1097/01.ta.0000233742.75450.47. [DOI] [PubMed] [Google Scholar]
- 19.Gorbunov NV, Elsayed NM, Kisin ER, Kozlov AV, Kagan VE. The American journal of physiology. 1997;272(2 Pt 1):L320–L334. doi: 10.1152/ajplung.1997.272.2.L320. [DOI] [PubMed] [Google Scholar]
- 20.Lee JH, Hanaoka M, Kitaguchi Y, Kraskauskas D, Shapiro L, Voelkel NF, Taraseviciene-Stewart L. Lung. 2012;190(1):69–82. doi: 10.1007/s00408-011-9326-z. [DOI] [PubMed] [Google Scholar]
- 21.Seitz DH, Perl M, Mangold S, Neddermann A, Braumuller ST, Zhou S, Bachem MG, Huber-Lang MS, Knoferl MW. Shock. 2008;30(5):537–544. doi: 10.1097/SHK.0b013e31816a394b. [DOI] [PubMed] [Google Scholar]
- 22.Liener UC, Knoferl MW, Strater J, Barth TF, Pauser EM, Nussler AK, Kinzl L, Bruckner UB, Gebhard F. Shock. 2003;20(6):511–516. doi: 10.1097/01.shk.0000095057.62263.fb. [DOI] [PubMed] [Google Scholar]
- 23.Liao F, Dan QQ, Du RF, Li JT, Zhang YH. Journal of Sichuan University. Medical science edition. 2012;43(6):914–917. [PubMed] [Google Scholar]
- 24.Rabinovici R, Feuerstein G, Abdullah F, Whiteford M, Borboroglu P, Sheikh E, Phillip DR, Ovadia P, Bobroski L, Bagasra O, Neville LF. Circulation research. 1996;78(2):329–336. doi: 10.1161/01.res.78.2.329. [DOI] [PubMed] [Google Scholar]
- 25.Rube CE, Wilfert F, Uthe D, Schmid KW, Knoop R, Willich N, Schuck A, Rube C. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2002;64(2):177–187. doi: 10.1016/s0167-8140(02)00077-4. [DOI] [PubMed] [Google Scholar]
- 26.Araz O, Demirci E, Yilmazel Ucar E, Calik M, Pulur D, Karaman A, Yayla M, Altun E, Halici Z, Akgun M. Multidisciplinary respiratory medicine. 2013;8(1):74. doi: 10.1186/2049-6958-8-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.