Abstract
Background
The burden of typhoid in sub-Saharan African (SSA) countries has been difficult to estimate, in part, due to suboptimal laboratory diagnostics. However, surveillance blood cultures at two sites in Nigeria have identified typhoid associated with Salmonella enterica serovar Typhi (S. Typhi) as an important cause of bacteremia in children.
Methods
A total of 128 S. Typhi isolates from these studies in Nigeria were whole-genome sequenced, and the resulting data was used to place these Nigerian isolates into a worldwide context based on their phylogeny and carriage of molecular determinants of antibiotic resistance.
Results
Several distinct S. Typhi genotypes were identified in Nigeria that were related to other clusters of S. Typhi isolates from north, west and central regions of Africa. The rapidly expanding S. Typhi clade 4.3.1 (H58) previously associated with multiple antimicrobial resistances in Asia and in east, central and southern Africa, was not detected in this study. However, antimicrobial resistance was common amongst the Nigerian isolates and was associated with several plasmids, including the IncHI1 plasmid commonly associated with S. Typhi.
Conclusions
These data indicate that typhoid in Nigeria was established through multiple independent introductions into the country, with evidence of regional spread. MDR typhoid appears to be evolving independently of the haplotype H58 found in other typhoid endemic countries. This study highlights an urgent need for routine surveillance to monitor the epidemiology of typhoid and evolution of antimicrobial resistance within the bacterial population as a means to facilitate public health interventions to reduce the substantial morbidity and mortality of typhoid.
Author Summary
Typhoid fever, a serious bloodstream infection caused by the bacterium Salmonella Typhi, is a major cause of disease and death around the world. There have been limited data on the epidemiology of typhoid in many countries in sub-Saharan African, including Nigeria. Recent evidence, however, showed that typhoid was an important cause of bacteraemia in children residing in two regions of Nigeria. Here, we analyzed the whole genome sequences of 128 S. Typhi isolates from two studies in order to elucidate the population structure and characterize the genetic components of antimicrobial resistance. We found that the multiple S. Typhi genotypes identified were closely related to other S. Typhi from neighboring regions of Africa and that multidrug resistance (MDR) was common among these isolates, and in many cases was associated with the IncHI1 plasmid known to cause MDR typhoid. These results provide evidence that typhoid was established in Nigeria as a result of several independent introductions into the country and that there has been extensive exchange of S. Typhi in and around the region of West Africa. This study emphasizes the importance of surveillance to improve our understanding of the epidemiology of typhoid, which is needed to underpin public health measures to reduce the spread of disease and facilitate patient management.
Introduction
Typhoid fever is a systemic infection caused by the Gram-negative bacterium Salmonella enterica serovar Typhi (S. Typhi) that continues to be a serious global health problem and a major cause of morbidity and mortality in low-middle income countries [1]. It is estimated that the yearly incidence of typhoid fever exceeds 20 million cases, with over 200,000 deaths [2, 3]. Defining the burden of typhoid fever is a challenge in settings where there are few diagnostic microbiology facilities, with diagnosis often based on clinical history of fever, malaise, and abdominal pain. Unfortunately, these symptoms have considerable overlap with several other febrile illnesses and clinical diagnosis is therefore inaccurate [4].
Nigeria is one of the most densely populated countries in Africa with large areas of urban development. Thus, it is perhaps surprising that little reliable data are available on microbial culture of the etiologic agents of bacteremia in children or adults. This poses a challenge for data comparison with other regions, including other sub-Saharan African countries where such data are available [5–7]. In general, febrile illnesses among children in Nigeria are presumed by clinicians to be caused by malaria, which is still very common in many parts of the country. Only if fever persists following an empiric course of anti-malarials, is typhoid then considered as a potential cause of infection [8]. In studies from central and northwest Nigeria [9], we found that S. Typhi was the commonest cause of bloodstream infections in children, particularly in those living in the proximity of Abuja city located in central Nigeria.
Until recently, molecular epidemiological studies on S. Typhi were compromised by a lack of genetic resolution, limiting the ability to define the population structure of the bacteria and identify transmission patterns. This is because S. Typhi is a relatively monomorphic pathogen with limited genome variation [10]. However, sequencing-based approaches have facilitated the stratification of S. Typhi into multiple genotypes [11] (see Wong et al. 2016, under review in Nature Communications, NCOMMS-15-25823, manuscript included). Whole genome sequencing in particular can unequivocally identify phylogenetic relationships with important genetic traits such as antimicrobial resistance [12]. Here we report whole genome-based analysis of 128 bloodstream isolates of S. Typhi from children residing in two regions of Nigeria, and compared these with data from other countries in Africa, including the West African subregion.
Methods
Settings
Nigeria has a population of approximately 177 million people making it the most populous country in sub-Saharan Africa [13]. The two study sites in Nigeria were the Federal Capital Territory (FCT) and Kano. The FCT is a federal territory in central Nigeria and covers a land area of 8,000 square kilometers. It is the home of the capital city Abuja, a “planned” city, built in the 1980s. It was officially made Nigeria’s capital in 1991 replacing the previous capital in Lagos. In 2006, the population was estimated at 1.7 million [14]. The FCT continue to experience rapid population growth; it has been reported that some areas around Abuja have been growing at an annual rate of 20–30%, and the current population may be as high as 5.7 million [14]. The rapid spread of squatter settlements and shantytowns in and around the city limits contribute to this rapid growth. The rainy season begins in April and ends in October. Within this period there is a brief interlude of Harmattan, occasioned by the Northeast Trade Wind, with the main features of dust haze, intensified coldness and dryness. The annual total rainfall for the FCT is in the range of 1,100 to 1,600 mm. The population is diverse, with increasing representation from the major ethnic groups of Hausa, Yoruba, and Igbos following the development of the FCT and relocation of the federal capital [15]. Of note, there is also perennial malaria transmission, mostly due to Plasmodium falciparum, and the HIV prevalence is 7.5% amongst pregnant women attending antenatal clinics [16].
Kano is the capital of Kano state in northwest Nigeria. According to the 2006 census, Kano state has a population of 9.38 million, which is comprised predominantly of Hausa and Fulani ethnic groups [17]. It is recognized as one of the fastest growing cities in Nigeria with a population density of about 1,000 inhabitants per km2. It lies within the Sahel savannah region with daily mean temperature of about 30–33°C during the dry months of March to May and 10°C during the autumn months of September to February. Rainy season varies from year to year, but typically commences in May and ends in October, with an average annual rainfall of 600mm. The dry season starts from November to April [18]. The entire state is within the meningococcal disease belt and malarial transmission is seasonal [17]. HIV prevalence among women attending antenatal clinic is 1.3% [16].
Enrolment sites
The enrolment sites at FCT are as previously described [9, 15]. Briefly, children aged less than 5 years were enrolled from primary, secondary and tertiary healthcare facilities on presentation with an acute febrile illness and symptoms suggestive of sepsis. In Kano, we enrolled children from Aminu Kano Teaching Hospital (AKTH), Hasiya Bayero Pediatric Hospital and Murtala Specialist Hospital. While AKTH serves as a tertiary referral center, the other two facilities provide primary and secondary healthcare services. The combined outpatient attendance for children at these three facilities is about 1,000 daily. Both study sites included patients from the newer settlements on the outskirt of Abuja and around Kano where the level of sanitation is poor and access to potable water limited.
Data collection
A structured questionnaire was used to collate the clinical information. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Nebraska Medical Center [19]. IBM SPSS for statistics was used for data analysis. Dichotomous variables were analyzed using χ2 or χ2 for trend tests [20].
Ethics statement
Clinical information was collected using a structured questionnaire after obtaining a signed informed consent from the child’s parent or legal guardian. This study was approved by the ethics committees of the FCT, National Hospital Abuja, Zankli Medical Center, Federal Medical Center Keffi, Aminu Kano Teaching Hospital, and UNMC, Omaha Institutional Review Board.
Blood culture processing
Blood sampling and processing were as previously described [9, 15]. Briefly, we utilized only aerobic blood culture bottles and held cultures in the Bactec 9050 incubator for a maximum of 5 days. Bacteria were identified by a combination of colony morphology and biochemical assays. For example, the API 20E system (bioMérieux, France) was used to identify Enterobacteriacae. Antimicrobial susceptibility profiles of the bacteria were determined by the Kirby-Bauer disk diffusion test using standard interpretative criteria [21] for locally available antimicrobials (amoxicillin, co-amoxiclav, ceftazidime, ceftriaxone, nalidixic acid, ciprofloxacin, ofloxacin, sulfamethoxazole, trimethoprim-sulfamethoxazole, chloramphenicol, tetracycline, streptomycin, gentamicin, kanamycin, azithromycin, imipenem) in order to provide immediate management of patients. Bacterial isolates were stored in skimmed milk at -70°C and further characterized at the Clinical Microbiology Laboratory of the University of Nebraska Medical Center (UNMC).
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed at the UNMC Microbiology laboratory using the Epsilometer test (Etest; bioMérieux, France) according to standard methods. Minimum inhibitory concentration (MIC) values were interpreted according to Clinical Laboratory Standards Institute (CLSI) standards [21]. Due to the lack of CLSI standards, a streptomycin MIC of ≥16 mg/L was considered resistant in these studies.
Salmonella serotyping
All Salmonella isolates were identified to the serotype level using the Bioplex 200 (Bio-Rad) as previously described using the CDC standard Salmonella molecular serotyping protocol [22–24]. A total of 128 S. Typhi isolates were identified in these studies for whole genome sequencing.
DNA sequencing
S. Typhi DNA was prepared using the Wizard Genomic DNA Kit (Promega, Madison, WI, USA) as per manufacturer’s instructions. Index-tagged paired end Illumina sequencing libraries were prepared as previously described [25]. These were combined into pools each containing 96 uniquely tagged libraries and sequenced on the Illumina Hiseq2000 or Miseq platforms (Illumina, San Diego, CA, USA) according to manufacturer’s protocols to generate tagged 100 or 150 base pair (bp) paired-end reads with an insert size of 300–400 bp. Sequence reads were deposited in the European Nucleotide Archive under accession ERP005877 and a full list of accession numbers for each sample is available in S1 Table. Sequence data from 1,831 additional S. Typhi isolates from 63 countries, generated previously in the same manner (Wong et al. 2015) [12], were also included in the study (reads are available in the European Read Archive under accession ERP001718).
Read alignment and SNP detection
For analysis of single nucleotide polymorphisms (SNPs), the paired-end reads were mapped to the reference genome of S. Typhi CT18 (accession number AL513382), including the chromosome and plasmids pHCM1 and pHCM2 [26], using SMALT (version 0.7.4) (http://www.sanger.ac.uk/resources/software/smalt/). SNPs were identified as previously described, using samtools mpileup [27] and filtering with a minimum mapping quality of 30 and a quality ratio cut-off of 0.75 [25]. The allele at each locus in each isolate was determined by reference to the consensus base in that genome, using samtools mpileup [27] and removing low confidence alleles with consensus base quality ≤20, read depth ≤5 or a heterozygous base call. SNPs called in phage regions, repetitive sequences (354 kbp; ~7.4% of bases in the S. Typhi CT18 reference chromosome, as defined previously [10]) or recombinant regions (~180 kbp; <4% of CT18 reference chromosome, identified using an approach described previously [25, 28]) were excluded, resulting in a final set of 23,300 chromosomal SNPs.
Phylogenetic analysis
The maximum likelihood (ML) phylogenetic tree was built from 23,300 SNP alignment of 1,961 isolates, including one S. Paratyphi A (accession number ERR326600) to provide an outgroup for tree rooting. We used RAxML (version 7.0.4) [29] with the generalized time-reversible model and a Gamma distribution to model site-specific rate variation (the GTR+ substitution model; GTRGAMMA in RAxML). Support for the ML phylogeny was assessed via 100 bootstrap pseudo-replicate analyzes of the alignment data. The ML trees were displayed and annotated using iTOL [30, 31].
In silico resistance plasmid and resistance gene analysis
Plasmids and acquired antimicrobial resistance genes were detected, and their precise alleles determined, using the mapping-based allele typer SRST2 [32] together with the ARG-Annot database of antimicrobial resistance genes [33] and the PlasmidFinder database of plasmid replicons [34]. SRST2 was also used to identify mutations in the gyrA, gyrB, parC and parE genes that have been associated with resistance to quinolones in Salmonella and other Gram-negative bacteria [35–38].
Results
Typhoid surveillance
Blood cultures were performed for the evaluation of 10,133 acutely ill children, aged 0–60 months, from September 2008 until April 2015, in the FCT (including Abuja) and Kano located in central and northwest Nigeria, respectively [9]. At FCT 6,082 children were enrolled between June 2012 and March 2015, of whom 457 (8%) had clinically significant bacteremia. Of these 110 (24%) had invasive salmonellosis, consisting of S. Typhi in 84 cases and non-typhoidal salmonellae (NTS) in 26 cases. In Kano from January 2014 until April 2015 clinically significant bacteremia was detected in 609 (15%) of 4,051 children: salmonellae accounted for 364 (60%) of 609 cases, of which 296 were S. Typhi and 68 were NTS. Across both regions Salmonella species accounted for 24–60% of bacteremia with S. Typhi being the most common serovar isolated with a total of 380 isolates (76–79%) [9].
Phylogenetic analysis of Nigerian S. Typhi
A selection of one hundred and twenty-two S. Typhi from the FCT and six from Kano, all isolated between 2008–2013, were randomly selected and sequenced via Illumina HiSeq and MiSeq (see Methods). The genomes of the Nigerian isolates were compared to that of the S. Typhi CT18 reference strain and a previously published global collection of approximately 2,000 S. Typhi isolates [12]. A phylogeny was built by extracting single nucleotide polymorphisms (SNPs) from the whole genome sequences, excluding likely recombination events and repetitive sequences that could confound phylogenetic analysis as described in Methods. The SNP data were also used to assign each isolate to one of 62 previously defined genotypes; details of the source and genotype of all Nigerian isolates is given in Table 1 and S1 Table. The distribution of the 128 Nigerian S. Typhi within the global phylogenetic tree is shown in S1 Fig. This global phylogeny includes 238 isolates from other countries in Africa, and the Nigerian isolates all cluster with other African isolates. Detailed phylogenetic relationships amongst the 366 African isolates are shown in Fig 1, and an interactive version of the phylogeny and map are available for exploration online at http://microreact.org/project/styphi_nigeria.
Table 1. Summary of genotypes of Nigerian S. Typhi.
| Laboratory name | Year of isolation | Location | Roumagnac haplotype* | Primary clade | Clade | Subclade |
|---|---|---|---|---|---|---|
| PO_30 | 2008 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_601 | 2009 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| PO_132 | 2009 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| PO_107 | 2009 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| PO_1057 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1060 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1063 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_187 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_227 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_293 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_351 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_355 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_771 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_812 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_919 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_575 | 2009 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_260 | 2009 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| PO_1102 | 2010 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| PO_1131 | 2010 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| 3135STDY5861198 | 2010 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| 3135STDY5861206 | 2010 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| 3135STDY5861239 | 2010 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| 3135STDY5861254 | 2010 | Abuja | Untypeable | 2 | 2.1 | 2.1.0 |
| PO_1255 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1098 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1101 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1210 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1242 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| PO_1265 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861190 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861230 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861262 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861271 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861184 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861208 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861216 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861224 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861232 | 2010 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861183 | 2010 | Abuja | H42 | 3 | 3.3 | 3.3.0 |
| PO_1232 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| 3135STDY5861222 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| 3135STDY5861246 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| 3135STDY5861270 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| 3135STDY5861199 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| 3135STDY5861247 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
| PO_1110 | 2010 | Abuja | H52 | 4 | 4.1 | 4.1.1 |
| PO_1256 | 2011 | Abuja | Untypeable | 1 | 1 | 0.0.3 |
| 3135STDY5861272 | 2011 | Abuja | Untypeable | 2 | 2.1 | 2.1.0 |
| 3135STDY5861209 | 2011 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861248 | 2011 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861256 | 2011 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861264 | 2011 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861193 | 2011 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861201 | 2011 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861233 | 2012 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861241 | 2012 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861273 | 2012 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861217 | 2012 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861225 | 2012 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861195 | 2012 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861211 | 2012 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861235 | 2012 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861243 | 2012 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861210 | 2013 | Kano | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861226 | 2013 | Kano | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861202 | 2013 | Kano | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861234 | 2013 | Kano | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861242 | 2013 | Kano | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861218 | 2013 | Kano | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861196 | 2013 | Abuja | Untypeable | 1 | 1 | 0.0.1 |
| 3135STDY5861244 | 2013 | Abuja | Untypeable | 1 | 1 | 0.0.1 |
| 3135STDY5861359 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861290 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861298 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861350 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861287 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861280 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861289 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861337 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861353 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861361 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861369 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861253 | 2013 | Abuja | Untypeable | 2 | 2.2 | 2.2.0 |
| 3135STDY5861342 | 2013 | Abuja | Untypeable | 2 | 2.3 | 2.3.1 |
| 3135STDY5861334 | 2013 | Abuja | Untypeable | 2 | 2.3 | 2.3.2 |
| 3135STDY5861294 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.0 |
| 3135STDY5861312 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861320 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861268 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861276 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861229 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861237 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861245 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861314 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861330 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861197 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861338 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861351 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861282 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861306 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861322 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861326 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861366 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861279 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861303 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861319 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861327 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861335 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861343 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861367 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861304 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861328 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861336 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861344 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861260 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861189 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861213 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861278 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861286 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861251 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861259 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861212 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861220 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861228 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861252 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861236 | 2013 | Abuja | H56 | 3 | 3.1 | 3.1.1 |
| 3135STDY5861368 | 2013 | Abuja | Untypeable | 3 | 3.1 | 3.1.1 |
| 3135STDY5861205 | 2013 | Abuja | H52 | 4 | 4.1 | 4.1.0 |
* Reference [11]
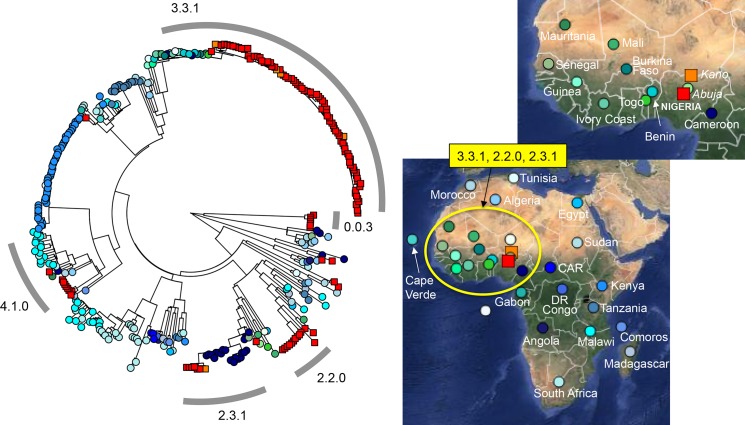
Fig 1. Distribution of Nigerian S. Typhi isolates in Africa in this study.
A maximum likelihood tree of 366 S. Typhi isolates constructed using 9,352 SNPs from whole genome sequence from 128 Nigerian isolates and 238 isolates from other regions of Africa is shown on the left. The geographical location of isolation is highlighted on the maps of Africa displayed on the right (http://microreact.org/showcase/). S. Typhi isolates from Abuja (122 isolates) and Kano (6) are denoted using red and orange squares, respectively. Colored circles on both the tree and maps represent isolates from other regions of Africa. The common genotypes of the Nigerian isolate are highlighted by a grey ring surrounding the tree with the corresponding geographical location marked on the map. Branch lengths are indicative of the estimated substitution rate per variable site.
The majority of Nigerian S. Typhi (84/128, 66%) belonged to genotype 3.1.1 (these isolates were assigned to H56 under the old typing scheme of Roumagnac et al (2006) [11]). This dominant genotype is relatively common across Africa, predominantly western and central countries (Fig 1). The Nigerian isolates formed a tight phylogenetically clustered subgroup within the 3.1.1 subclade (Fig 1), suggesting recent local expansion, and included isolates from both Abuja and Kano, suggesting intra-country transmission. Interestingly, in the wider African collection genotype 3.1.1 was represented by isolates from neighboring Cameroon and across West Africa (Benin, Togo, Ivory Coast, Burkina Faso, Mali, Guinea and Mauritania) suggesting long-term inter-country exchange within the region (Fig 1). Most of the remaining isolates belonged to four other genotypes, indicating that these are also established genotypes in circulation at the study sites in Nigeria. These genotypes, highlighted in Fig 1, are 2.2.0 (n = 13), 2.3.1 (n = 8), 4.1.0 (n = 8, H52 under the old scheme) and 0.0.3 (n = 7, H12). Nigerian isolates of genotypes 2.2.0 and 2.3.1 were closely related to isolates from neighboring Cameroon and West African countries and not found elsewhere, supporting regional transmission similar to the dominant genotype 3.1.1 (see map in Fig 1), while genotype 4.1.0 was more widespread across Africa. Interestingly genotype 0.0.3 (previously identified in India and Malaysia), which accounted for >5% of Nigerian isolates, maps very close to the root of the global S. Typhi tree, suggestive of older circulating isolates. A further six other genotypes were also detected amongst the Nigerian isolates, represented by 1–2 isolates each (Table 1). Of note, genotype 4.3.1 (H58), which has become dominant elsewhere in sub-Saharan Africa and accounts for the majority of antimicrobial resistant typhoid globally, was not detected in the Nigerian studies.
Antimicrobial resistant S. Typhi in Nigeria
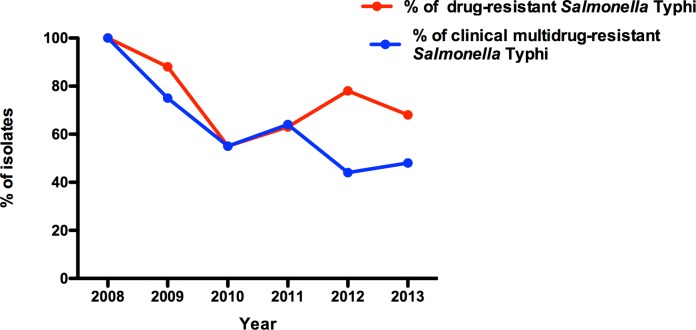
Fig 2 shows the proportion of S. Typhi isolates that were resistant to one or more antimicrobials, and the proportion that were multidrug-resistant (MDR; defined as resistance to ampicillin, chloramphenicol and trimethoprim-sulfamethoxazole), each year from 2008–2013. The majority of isolates were MDR throughout this period (Fig 2).
Fig 2. Presence of antimicrobial resistance of S. Typhi in the study areas.
The proportion of S. Typhi isolates that were resistant to one or more antimicrobials (red line) and were multidrug-resistant (MDR; defined as resistance to ampicillin, chloramphenicol and trimethoprim-sulfamethoxazole, blue line) are shown. Percentages are of the total S. Typhi isolated per year.
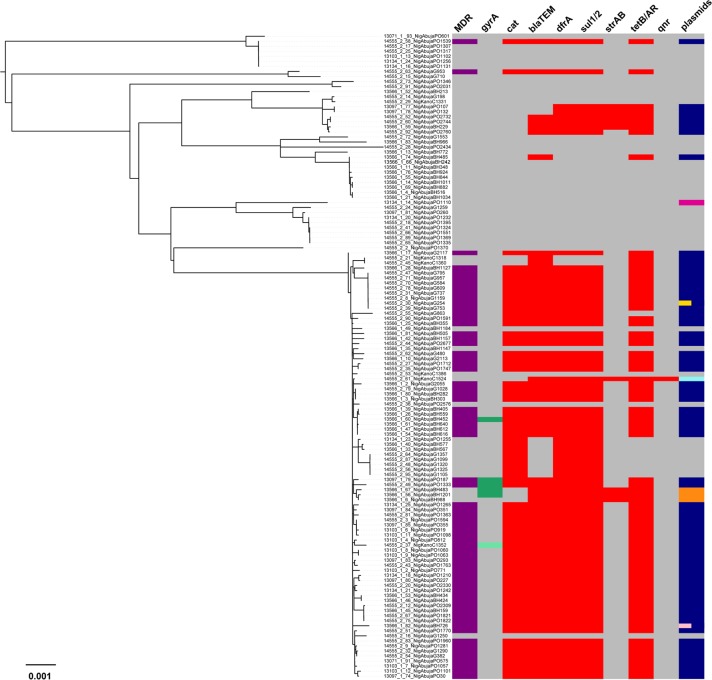
Fig 3 and Table 2 show the distribution of antimicrobial resistance determinants in the Nigerian isolates. Most of the 3.1.1 (H56) isolates carried genes encoding resistance to ampicillin, chloramphenicol, tetracycline and sulfamethoxazole (blaTEM-1, catA1, tetB, dfrA15, sul1). These were located on an IncHI1 plasmid, similar to that commonly found in MDR S. Typhi 4.3.1 (H58). The same profile was identified in a single isolate of 0.0.3, indicative of local plasmid transfer between the co-circulating genotypes. Genotype 2.3.1 isolates were found to carry IncHI1 plasmids encoding these resistance genes, as well as resistance determinants sul2 and strAB. An IncHI1 plasmid carrying blaTEM and tetB was also identified in one 2.2.0 isolate. Interestingly, nine genotype 3.1.1 isolates lacked the IncHI1 plasmid. However, four of these carried plasmids of other incompatibility groups. Three isolates (3135STDY5861338; 3135STDY5861351; 3135STDY5861282) harbored a novel IncY plasmid (blaTEM-198, catA1, tetB, dfrA14, sul1) and one (3135STDY5861242) harbored a plasmid-related to the Kpn3 plasmid (blaTEM-198, tetAR, dfrA14, sul1, sul2, strAB and also qnr-S, which mediates fluoroquinolone resistance). Thus, plasmid-mediated MDR is common in Nigerian S. Typhi from the regions under study.
Fig 3. Acquired multidrug-resistance in Nigerian S. Typhi isolates.
Maximum likelihood tree of 128 Nigerian S. Typhi isolates from 2,541 SNPs is shown on the left. On the right is a heatmap which shows, for each isolate, its multidrug-resistant (MDR) status (purple), the presence of gyrA mutations (dark green S83Y; light green S83F), resistance genes cat, blaTEM, dfrA, sul1/2, strAB, tetB/AR, qnr (red) and plasmids, including IncHI1 (dark blue), Kpn3 (light blue), IncY (orange), IncQ1 (light pink), IncFIIs (yellow) and Col(RNAI) (magenta). Different colored bars within the plasmid column show isolates that harbor multiple plasmids with each bar representing a plasmid type. The absence of a genotype or plasmid was displayed in grey. Branch lengths are indicative of the estimated substitution rate per variable site.
Table 2. Summary of drug resistance of Nigerian S. Typhi.
| Laboratory name | Subclade | Plasmids | Resistance genes | gyrA mutations | |
|---|---|---|---|---|---|
| 3135STDY5861196 | 0.0.1 | - | - | - | |
| 3135STDY5861244 | 0.0.1 | - | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_601 | 0.0.3 | - | - | - | |
| PO_1102 | 0.0.3 | - | - | - | |
| PO_1131 | 0.0.3 | - | - | - | |
| 3135STDY5861198 | 0.0.3 | - | - | - | |
| 3135STDY5861206 | 0.0.3 | - | - | - | |
| 3135STDY5861239 | 0.0.3 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1256 | 0.0.3 | - | - | - | |
| 3135STDY5861254 | 2.1.0 | - | - | - | |
| 3135STDY5861272 | 2.1.0 | - | - | - | |
| 3135STDY5861209 | 2.2.0 | - | - | - | |
| 3135STDY5861359 | 2.2.0 | IncHI1 | bla-TEM, tetB | - | |
| 3135STDY5861290 | 2.2.0 | - | - | - | |
| 3135STDY5861298 | 2.2.0 | - | - | - | |
| 3135STDY5861350 | 2.2.0 | - | - | - | |
| 3135STDY5861287 | 2.2.0 | - | - | - | |
| 3135STDY5861280 | 2.2.0 | - | - | - | |
| 3135STDY5861289 | 2.2.0 | - | - | - | |
| 3135STDY5861337 | 2.2.0 | - | - | - | |
| 3135STDY5861353 | 2.2.0 | - | - | - | |
| 3135STDY5861361 | 2.2.0 | - | - | - | |
| 3135STDY5861369 | 2.2.0 | - | - | - | |
| 3135STDY5861253 | 2.2.0 | - | - | - | |
| PO_132 | 2.3.1 | IncHI1 | dfrA, sul1, tetB, strA, strB, sul2, aad | - | |
| PO_107 | 2.3.1 | IncHI1 | dfrA, tetB, strA, strB, sul2, aad | - | |
| 3135STDY5861233 | 2.3.1 | IncHI1 | dfrA, sul1, bla-TEM, tetB, strA, strB, sul2, aad | - | |
| 3135STDY5861241 | 2.3.1 | IncHI1 | dfrA, sul1, bla-TEM, tetB, strA, strB, sul2, aad | - | |
| 3135STDY5861273 | 2.3.1 | IncHI1 | dfrA, sul1, bla-TEM, tetB, aad | - | |
| 3135STDY5861210 | 2.3.1 | - | - | - | |
| 3135STDY5861195 | 2.3.1 | - | - | - | |
| 3135STDY5861342 | 2.3.1 | IncHI1 | dfrA, sul1, bla-TEM, tetB, strA, strB, sul2, aad | - | |
| 3135STDY5861334 | 2.3.2 | - | - | - | |
| 3135STDY5861294 | 3.1.0 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_30 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1057 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1060 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1063 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_187 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | S83Y | |
| PO_227 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_293 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_351 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_355 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_771 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_812 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_919 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_575 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1255 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| PO_1098 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1101 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1210 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1242 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| PO_1265 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861190 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861230 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | S83Y | |
| 3135STDY5861262 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861271 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861184 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861208 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861216 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861224 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861232 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861248 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861256 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861264 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861193 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861201 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861217 | 3.1.1 | - | - | - | |
| 3135STDY5861225 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861226 | 3.1.1 | IncHI1 | bla-TEM, tetB | - | |
| 3135STDY5861202 | 3.1.1 | IncHI1 | bla-TEM, tetB | - | |
| 3135STDY5861234 | 3.1.1 | - | - | - | |
| 3135STDY5861242 | 3.1.1 | Kpn3 | bla-TEM, strA, strB, sul1, sul2, dfrA, tetA, tetR, qnrS | - | |
| 3135STDY5861218 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | S83F | |
| 3135STDY5861211 | 3.1.1 | IncHI1, IncFIIs | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861235 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861243 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861312 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861320 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861268 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861276 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861229 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861237 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861245 | 3.1.1 | - | cat, dfrA, sul1 | - | |
| 3135STDY5861314 | 3.1.1 | - | - | - | |
| 3135STDY5861330 | 3.1.1 | - | - | - | |
| 3135STDY5861197 | 3.1.1 | - | - | - | |
| 3135STDY5861338 | 3.1.1 | IncY | bla-TEM, strA, strB, sul1, dfrA, tetA, tetR | S83Y | |
| 3135STDY5861351 | 3.1.1 | IncY | bla-TEM, strA, strB, sul1, dfrA, tetA, tetR | S83Y | |
| 3135STDY5861282 | 3.1.1 | IncY | bla-TEM, strA, strB, sul1, dfrA, tetA, tetR | S83Y | |
| 3135STDY5861306 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861322 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861326 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861366 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861279 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861303 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861319 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861327 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861335 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861343 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861367 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861304 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861328 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861336 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861344 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861260 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861189 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861213 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861278 | 3.1.1 | IncHI1 | cat, dfrA, sul1, bla-TEM, tetB | - | |
| 3135STDY5861286 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861251 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861259 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861212 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861220 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861228 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861252 | 3.1.1 | IncHI1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861236 | 3.1.1 | IncHI1 | 4 | cat, dfrA, sul1, bla-TEM, | - |
| 3135STDY5861368 | 3.1.1 | IncHI1, IncQ1 | 5 | cat, dfrA, sul1, bla-TEM, tetB | - |
| 3135STDY5861183 | 3.3.0 | - | 0 | - | - |
| PO_260 | 4.1.0 | - | 0 | - | - |
| PO_1232 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861222 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861246 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861270 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861199 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861247 | 4.1.0 | - | 0 | - | - |
| 3135STDY5861205 | 4.1.0 | - | 0 | - | - |
| PO_1110 | 4.1.1 | Col(RNAI) | 0 | - | - |
We identified only six S. Typhi isolates with quinolone resistance-associated mutations in gyrA (one with S83F; five with S83Y). The affected isolates were all of the dominant genotype 3.1.1, including the three that carried IncY plasmids and three that carried IncHI1 plasmids. No other polymorphisms were detected in the quinolone resistance determining regions of the gyrA or parC genes of Nigerian S. Typhi isolates.
Discussion
Here, S. Typhi is shown to be a common cause of bacteremia and fever among children living in two geographically distinct regions of Nigeria. Studies on typhoid within Nigeria have been relatively rare, even though it is a country with a large population and extensive urbanization. Indeed, S. Typhi is the most common bacterial cause of bloodstream infections. Phylogenetic analysis identified distinct clusters of S. Typhi, with isolates of genotype 3.1.1 representing 66% of all isolates. Other common genotypes included 2.2.0 and 2.3.1, which have been previously reported in Africa, and genotypes 4.1.0 and 0.0.3, which were previously reported in Asia. The presence of multiple genotypes in these comparatively small regions suggests typhoid has been established for some time and that different waves of disease have entered the regions at different times. It is also interesting that the different clades of Nigerian isolates distributed across the phylogeny frequently map adjacent to other S. Typhi isolates from other African countries. For example, genotype 3.1.1 maps adjacent to S. Typhi isolates from both west and north Africa, with the Nigerian isolates located on a more recent phylogenetic branch. Similarly, genotypes 2.2.0 and 2.3.1 also map close to other African isolates. This general distribution indicates substantial exchange of S. Typhi between Nigeria and other parts of Africa. However, the phylogenetic analysis was limited to two sites within Nigeria, with only six S. Typhi isolates included in the analysis from Kano, over a five- year period, resulting in a selection bias towards strains from a single study site in Nigeria (Abuja). Therefore, a more comprehensive analysis involving a larger number of strains from multiple regions across Nigeria and surrounding countries over a wider time span would be required to further investigate transmission within the region.
It is notable that none of the Nigerian isolates were of the genotype 4.3.1 (H58), which is now expanding across many other regions with endemic typhoid and is associated with a MDR phenotype. This suggests that the recent expansion of H58 S. Typhi, estimated to date from the mid-1980s, has not yet reached Nigeria, unlike other African countries including Kenya, Tanzania, Malawi and South Africa. The absence of H58 isolates in the sampled area of Nigeria is an important finding. It has been postulated that H58 S. Typhi originally emerged in Asia, but subsequently entered Africa on a number of distinct occasions where they have gone on to cause large typhoid outbreaks [12]. Thus, it is likely that H58 S. Typhi will reach Nigeria in the future, potentially changing the epidemiology of the disease in the region and molecular surveillance could be used to monitor for this.
Nevertheless, MDR S. Typhi are common in the regions of study despite the absence of H58 microorganisms. This is an important observation, as the MDR phenotype in other regions of the world has been driven by the spread of MDR S. Typhi H58. Many of the Nigerian S. Typhi, including those of genotype 3.1.1, harbored IncHI1 plasmids that have been previously associated with S. Typhi of other genotypes, particularly H58 [12, 39]. This is consistent with a genetic compatibility between S. Typhi and such plasmids. Interestingly, genetic analysis indicates that an IncHI1 plasmid recently transferred between 3.1.1 and 0.0.3 Typhi within the study region. However, several other plasmids of distinct incompatibility types were also detected within the sampled S. Typhi and it will be interesting to see if any of these are common elsewhere in Nigeria or whether they solely persist within these study sites.
Mutations associated with resistance to quinolones were relatively rare within the sample set. This could be because fluoroquinolones are not commonly used to treat typhoid in these regions, or alternatively, it may be that such mutations have not become fixed in these non-H58 isolates. Further studies on the use of fluoroquinolones are warranted.
In conclusion, it is clear that typhoid associated with MDR S. Typhi is common in these parts of Nigeria and that the MDR phenotype is evolving independently of haplotype H58, which has emerged elsewhere in the world where typhoid is endemic.
Members of International Typhoid Consortium
Vanessa K. Wong1,2, Stephen Baker3,4,5, Derek Pickard1, Julian Parkhill1, Andrew J Page1, Nicholas A. Feasey6 Robert A. Kingsley1,7, Nicholas R. Thomson1,5, Jacqueline A. Keane1, François-Xavier Weill8, Simon Le Hello8, Jane Hawkey9,10,11, David J. Edwards9,11, Zoe A. Dyson9,11, Simon R. Harris1, Amy K. Cain1, James Hadfield1, Peter J. Hart12,13, Nga Tran Vu Thieu3, Elizabeth J. Klemm1, Robert F. Breiman14,15,16, Conall H. Watson17, Samuel Kariuki1,14, Melita A. Gordon18,19, Robert S. Heyderman20,19, Chinyere Okoro1,2, Jan Jacobs21,22, Octavie Lunguya23,24, W. John Edmunds17, Chisomo Msefula19,25, Jose A. Chabalgoity26, Mike Kama27, Kylie Jenkins28, Shanta Dutta29, Florian Marks30, Josefina Campos31, Corinne Thompson3,4, Stephen Obaro32,33,34, Calman A. MacLennan1,12,35, Christiane Dolecek3,4, Karen H. Keddy36, Anthony M. Smith36, Christopher M. Parry37,38, Abhilasha Karkey39, E. Kim Mulholland5,40, James I. Campbell3,4, Sabina Dongol39, Buddha Basnyat39, Amit Arjyal39, Muriel Dufour41, Don Bandaranayake42, Take N. Toleafoa43, Shalini Pravin Singh44, Mochammad Hatta45, Robert S. Onsare14, Lupeoletalalelei Isaia46, Guy Thwaites3,4, Paul Turner4,47,48, Sona Soeng48, John A. Crump49, Elizabeth De Pinna50, Satheesh Nair50, Eric J Nille51, Duy Pham Thanh3, Mary Valcanis52, Joan Powling52, Karolina Dimovski52, Geoff Hogg52, Thomas R. Connor53, Jayshree Dave54, Niamh Murphy54, Richard Holliman54, Armine Sefton55, Michael Millar55, Jeremy Farrar3,4, Alison E. Mather56, Ben Amos57, Grace Olanipekun58, Huda Munir59, Roxanne Alter60, Paul D. Fey60, Kathryn E Holt9,11 and Gordon Dougan1
The Wellcome Trust Sanger Institute, Hinxton, Cambridge, United Kingdom
Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge Biomedical Campus, Hills Road, Cambridge, United Kingdom
The Hospital for Tropical Diseases, Wellcome Trust Major Overseas Programme, Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam
Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Oxford University, Oxford, UK
Department of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom
Liverpool School of Tropical Medicine, Pembroke Place, Liverpool, United Kingdom
Institute of Food Research, Norwich Research Park, Colney, Norwich, United Kingdom
Institut Pasteur, Unité des Bactéries Pathogènes Entériques, Paris, France
Department of Biochemistry and Molecular Biology, Bio21 Molecular Science and Biotechnology Institute, University of Melbourne, Parkville, Victoria, Australia
Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Parkville, Victoria, Australia
Centre for Systems Genomics, University of Melbourne, Parkville, Victoria, Australia
Institute of Biomedical Research, School of Immunity and Infection, College of Medicine and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
St George’s University of London, London, United Kingdom
Kenya Medical Research Institute (KEMRI), Nairobi, Kenya
Centers for Disease Control and Prevention, Atlanta, Georgia, United States of America
Emory Global Health Institute, Atlanta, Georgia, United States of America
Centre for the Mathematical Modelling of Infectious Diseases, Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, Keppel Street, London, United Kingdom
Institute of Infection and Global Health, University of Liverpool, United Kingdom
Malawi-Liverpool-Wellcome-Trust Clinical Research Programme, College of Medicine, University of Malawi, Chichiri, Blantyre, Malawi
Division of Infection and Immunity, University College London, London, United Kingdom
Department of Clinical Sciences, Institute of Tropical Medicine, Antwerp, Belgium
KU Leuven, University of Leuven, Department of Microbiology and Immunology, Belgium
National Institute for Biomedical Research, Kinshasa, Democratic Republic of the Congo
University Hospital of Kinshasa, Kinshasa, Democratic Republic of the Congo
Microbiology Department, College of Medicine, University of Malawi, Malawi
Departamento de Desarrollo Biotecnologico, Instituto de Higiene, Facultad de Medicina, Avda A Navarro 3051, Montevideo, Uruguay
Ministry of Health, Toorak, Suva, Fiji
Fiji Health Sector Support Program, Suva, Fiji
National Institute of Cholera and Enteric Diseases, Scheme XM, Beliaghata, Kolkata, India
International Vaccine Institute, Department of Epidemiology, Kwanak, Republic of Korea
Enteropathogen Division, ANLIS-Carlos G Malbran Institute, CABA, Argentina
Division of Pediatric Infectious Diseases, University of Nebraska Medical Center, Omaha, Nebraska, United States of America
University of Abuja Teaching Hospital, Gwagwalada, FCT, Nigeria
Bingham University, Karu, Nassarawa State, Nigeria
The Jenner Institute, Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom
Centre for Enteric Diseases, National Institute for Communicable Diseases, Division in the National Health Laboratory Service and Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Department of Clinical Research, London School of Hygiene and Tropical Medicine, Keppel Street, London, United Kingdom
Graduate School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, Japan
Patan Academy of Health Sciences, Wellcome Trust Major Overseas Programme, Oxford University Clinical Research Unit, Kathmandu, Nepal
Murdoch Childrens Research Institute, Melbourne, Australia
Enteric and Leptospira Reference Laboratory, Institute of Environmental Science and Research Limited (ESR), New Zealand
National Centre for Biosecurity and Infectious Disease, Institute of Environmental Science and Research, Porirua, New Zealand
Samoa Ministry of Health, Apia, Samoa
National Influenza Center, World Health Organization, Center for Communicable Disease Control, Suva, Fiji
Department of Microbiology, Hasanuddin University, Makassar, Indonesia
National Health Services, Tupua Tamasese Meaole Hospital, Samoa
Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Cambodia-Oxford Medical Research Unit, Angkor Hospital for Children, Siem Reap, Cambodia
Centre for International Health, University of Otago, Dunedin, New Zealand
Salmonella Reference Service, Public Health England, Colindale, London, United Kingdom
Emerging Disease Surveillance and Response, Division of Pacific Technical Support, World Health Organization, Suva, Fiji
Microbiological Diagnostic Unit—Public Health Laboratory, Department of Microbiology and Immunology at the Peter Doherty Institute for Infection and Immunity, The University of Melbourne, Victoria, Australia
Cardiff University School of Biosciences, Cardiff University, Cardiff, United Kingdom
Public Health Laboratory London, Public Health England, London, United Kingdom
Division of Infection, Barts Health NHS Trust, London, United Kingdom
Department of Veterinary Medicine, University of Cambridge, Cambridge, United Kingdom
St Augustine’s Hospital, Muheza, Tanzania
International Foundation Against Infectious Diseases in Nigeria, Abuja, Nigeria
Department of Medical Microbiology, Aminu Kano Teaching Hospital, Kano, Nigeria
Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, Nebraska, United States of America
Supporting Information
A maximum likelihood tree of 1,960 S. Typhi isolates from 23,300 SNPs surrounded by colored rings representing the geographic origin of 502 African isolates, according to the legend. 128 Nigerian isolates are highlighted in black (122 = Abuja) and grey (6 = Kano); neighboring African countries labeled by black arrows. The genotypes of the Nigerian isolates are labeled in red with the old Roumagnac haplotypes [11] in parentheses (red * denotes untypeable Nigerian strains). The 4.3.1 (H58) subclade is indicated in red italics. Branch lengths are indicative of the estimated substitution rate per variable site.
(TIF)
(XLS)
Acknowledgments
We would like to thank the members of the Pathogen Informatics Team and the core sequencing teams at the Wellcome Trust Sanger Institute (Cambridge, UK). We are grateful to David Harris for his superb work in managing the sequence data.
Data Availability
All sequence read files are available from European Nucleotide Archive under accession number ERP005877.
Funding Statement
This work was supported by a number of organizations. The Wellcome Trust Sanger Institute authors were funded by Wellcome Trust Award 098051; NAF was supported by the Wellcome Trust Research Fellowship WT092152MA. NAF, RSH and this work were supported by a strategic award from the Wellcome Trust for the MLW Clinical Research Programme (101113/Z/13/Z). KEH was supported by the NHMRC of Australia (fellowship #1061409) and the Victorian Life Sciences Computation Initiative (VLSCI) (grant #VR0082). CAM was supported by a Clinical Research Fellowship from GlaxoSmithKline and PJH by a UK Medical Research Council PhD studentship. This work forms part of an EU FP7 Marie Curie Actions Industry Academia Partnerships and Pathways (IAPP) Consortium Programme, entitled GENDRIVAX (Genome-driven vaccine development for bacterial infections), involving the Wellcome Trust Sanger Institute, KEMRI Nairobi and Novartis Vaccines Institute for Global Health. The Institut Pasteur (IP) authors were funded by the IP, the Institut de Veille Sanitaire, and by the French Government “Investissement d'Avenir” program (Integrative Biology of Emerging Infectious Diseases” Laboratory of Excellence, grant no. ANR-10-LABX-62-IBEID). CO was supported by Society in Science, The Branco Weiss Fellowship, administered by the ETH Zurich. JJ was supported by the antibiotic resistance surveillance project in DR Congo, funded by Project 2.01 of the Third Framework Agreement between the Belgian Directorate General of Development Cooperation and the Institute of Tropical Medicine, Antwerp, Belgium. FM was supported by a research grant from the Bill & Melinda Gates Foundation. The findings and conclusions contained within this publication are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation. SK was supported by the NIH Grant Number R01 AI099525-02. SB is a Sir Henry Dale Fellow, jointly funded by the Wellcome Trust and the Royal Society (100087/Z/12/Z). SO was supported by the National Institute Of Allergy And Infectious Diseases (NIAID) of the National Institutes of Health (#R01AI097493). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346–53. Epub 2004/08/10. [PMC free article] [PubMed] [Google Scholar]
- 2.Crump JA, Mintz ED. Global trends in typhoid and paratyphoid Fever. Clin Infect Dis. 2010;50(2):241–6. 10.1086/649541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mogasale V, Maskery B, Ochiai RL, Lee JS, Mogasale VV, Ramani E, et al. Burden of typhoid fever in low-income and middle-income countries: a systematic, literature-based update with risk-factor adjustment. The Lancet Global health. 2014;2(10):e570–80. 10.1016/S2214-109X(14)70301-8 . [DOI] [PubMed] [Google Scholar]
- 4.Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N Engl J Med. 2002;347(22):1770–82. 10.1056/NEJMra020201 . [DOI] [PubMed] [Google Scholar]
- 5.Enwere G, Biney E, Cheung YB, Zaman SM, Okoko B, Oluwalana C, et al. Epidemiologic and clinical characteristics of community-acquired invasive bacterial infections in children aged 2–29 months in The Gambia. Pediatr Infect Dis J. 2006;25(8):700–5. 10.1097/01.inf.0000226839.30925.a5 . [DOI] [PubMed] [Google Scholar]
- 6.Berkley JA, Lowe BS, Mwangi I, Williams T, Bauni E, Mwarumba S, et al. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med. 2005;352(1):39–47. 10.1056/NEJMoa040275 . [DOI] [PubMed] [Google Scholar]
- 7.Isendahl J, Manjuba C, Rodrigues A, Xu W, Henriques-Normark B, Giske CG, et al. Prevalence of community-acquired bacteraemia in Guinea-Bissau: an observational study. BMC Infect Dis. 2014;14:3859 10.1186/s12879-014-0715-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arulogun OS, Adeniyi JD, Asa S, Adegbenro CA. Why actions for early treatment of febrile illnesses in children are delayed by caregivers. Int Q Community Health Educ. 2011;32(3):219–31. 10.2190/IQ.32.3.e . [DOI] [PubMed] [Google Scholar]
- 9.Obaro SK, Hassan-Hanga F, Olateju EK, Umoru D, Lawson L, Olanipekun G, et al. Salmonella Bacteremia Among Children in Central and Northwest Nigeria, 2008–2015. Clin Infect Dis. 2015;61 Suppl 4:S325–31. 10.1093/cid/civ745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holt KE, Parkhill J, Mazzoni CJ, Roumagnac P, Weill FX, Goodhead I, et al. High-throughput sequencing provides insights into genome variation and evolution in Salmonella Typhi. Nat Genet. 2008;40(8):987–93. Epub 2008/07/29. ng.195 [pii] 10.1038/ng.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roumagnac P, Weill FX, Dolecek C, Baker S, Brisse S, Chinh NT, et al. Evolutionary history of Salmonella typhi. Science. 2006;314(5803):1301–4. Epub 2006/11/25. 314/5803/1301 [pii] 10.1126/science.1134933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong VK, Baker S, Pickard DJ, Parkhill J, Page AJ, Feasey NA, et al. Phylogeographical analysis of the dominant multidrug-resistant H58 clade of Salmonella Typhi identifies inter- and intracontinental transmission events. Nat Genet. 2015;47(6):632–9. 10.1038/ng.3281 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The World Bank 2015. http://data.worldbank.org/country/nigeria. Accessed 18th November 2015.
- 14.Abuja, the Beautiful Capital city (21 January 2011).Available at: http://9ja-land.blogstop.com/2010/05/abuja-beautiful-capital-city.html. Accessed 18 November 2015.
- 15.Obaro S, Lawson L, Essen U, Ibrahim K, Brooks K, Otuneye A, et al. Community acquired bacteremia in young children from central Nigeria—a pilot study. BMC Infect Dis. 2011;11:137 10.1186/1471-2334-11-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Federal Republic of Nigeria NAftCoA, Global AIDS Response Country Progress Report 2014. Available at: http://www.unaids.org/sites/default/files/country/documents/NGA_narrative_report_2014.pdf. Accessed 11 November 2015.
- 17.Olayemi IK, Ande AT, Ayanwale AV, Mohammed AZ, Bello IM, Idris B, et al. Seasonal trends in epidemiological and entomological profiles of malaria transmission in North Central Nigeria. Pak J Biol Sci. 2011;14(4):293–9. . [DOI] [PubMed] [Google Scholar]
- 18.Federal Republic of Nigeria NBoSpc, Kano state statisical table: 2010. Available at: http://www.nigriast.gov.ng. Accessed 11 November 2015.
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IBM Corp. Released 2013. IBM SPSS Statistics for Macintosh VA, NY: IBM Corp.
- 21.Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Twentieth Informational Supplement M100-S20. Wayne, PA, USA: CLSI; 2014.
- 22.CDC standard protocol: molecular determination of serotype in Salmonella version 2.0 AawcucgciAN.
- 23.Herrera-Leon S, McQuiston JR, Usera MA, Fields PI, Garaizar J, Echeita MA. Multiplex PCR for distinguishing the most common phase-1 flagellar antigens of Salmonella spp. J Clin Microbiol. 2004;42(6):2581–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fitzgerald C, Collins M, van Duyne S, Mikoleit M, Brown T, Fields P. Multiplex, bead-based suspension array for molecular determination of common Salmonella serogroups. J Clin Microbiol. 2007;45(10):3323–34. 10.1128/JCM.00025-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Croucher NJ, Harris SR, Fraser C, Quail MA, Burton J, van der Linden M, et al. Rapid pneumococcal evolution in response to clinical interventions. Science. 2011;331(6016):430–4. Epub 2011/01/29. 10.1126/science.1198545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, Wain J, et al. Complete genome sequence of a multiple drug resistant Salmonella enterica serovar Typhi CT18. Nature. 2001;413(6858):848–52. Epub 2001/10/26. 10.1038/35101607 . [DOI] [PubMed] [Google Scholar]
- 27.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25(16):2078–9. Epub 2009/06/10. 10.1093/bioinformatics/btp352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Croucher NJ, Page AJ, Connor TR, Delaney AJ, Keane JA, Bentley SD, et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43(3):e15 10.1093/nar/gku1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stamatakis A. RAxML-VI-HPC: maximum likelihood-based phylogenetic analyses with thousands of taxa and mixed models. Bioinformatics. 2006;22(21):2688–90. Epub 2006/08/25. 10.1093/bioinformatics/btl446 . [DOI] [PubMed] [Google Scholar]
- 30.Letunic I, Bork P. Interactive Tree Of Life (iTOL): an online tool for phylogenetic tree display and annotation. Bioinformatics. 2007;23(1):127–8. 10.1093/bioinformatics/btl529 . [DOI] [PubMed] [Google Scholar]
- 31.Letunic I, Bork P. Interactive Tree Of Life v2: online annotation and display of phylogenetic trees made easy. Nucleic Acids Res. 2011;39(Web Server issue):W475–8. 10.1093/nar/gkr201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Inouye MD, H. Raven LA. Schultz M.B. Pope B.J. Tomita T. Zobel J. and Holt K. E. SRST2: Rapid genomic surveillance for public health and hospital microbiology labs. Genome Medicine. 2014;6(90). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta SK, Padmanabhan BR, Diene SM, Lopez-Rojas R, Kempf M, Landraud L, et al. ARG-ANNOT, a new bioinformatic tool to discover antibiotic resistance genes in bacterial genomes. Antimicrob Agents Chemother. 2014;58(1):212–20. 10.1128/AAC.01310-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carattoli A, Zankari E, Garcia-Fernandez A, Voldby Larsen M, Lund O, Villa L, et al. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother. 2014;58(7):3895–903. 10.1128/AAC.02412-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eaves DJ, Randall L, Gray DT, Buckley A, Woodward MJ, White AP, et al. Prevalence of mutations within the quinolone resistance-determining region of gyrA, gyrB, parC, and parE and association with antibiotic resistance in quinolone-resistant Salmonella enterica. Antimicrob Agents Chemother. 2004;48(10):4012–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baucheron S, Chaslus-Dancla E, Cloeckaert A, Chiu CH, Butaye P. High-level resistance to fluoroquinolones linked to mutations in gyrA, parC, and parE in Salmonella enterica serovar Schwarzengrund isolates from humans in Taiwan. Antimicrob Agents Chemother. 2005;49(2):862–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hooper DC. Quinolone mode of action—new aspects. Drugs. 1993;45 Suppl 3:8–14. . [DOI] [PubMed] [Google Scholar]
- 38.Song Y, Roumagnac P, Weill FX, Wain J, Dolecek C, Mazzoni CJ, et al. A multiplex single nucleotide polymorphism typing assay for detecting mutations that result in decreased fluoroquinolone susceptibility in Salmonella enterica serovars Typhi and Paratyphi A. J Antimicrob Chemother. 2010;65(8):1631–41. 10.1093/jac/dkq175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holt KE, Phan MD, Baker S, Duy PT, Nga TV, Nair S, et al. Emergence of a globally dominant IncHI1 plasmid type associated with multiple drug resistant typhoid. PLoS neglected tropical diseases. 2011;5(7):e1245 10.1371/journal.pntd.0001245 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A maximum likelihood tree of 1,960 S. Typhi isolates from 23,300 SNPs surrounded by colored rings representing the geographic origin of 502 African isolates, according to the legend. 128 Nigerian isolates are highlighted in black (122 = Abuja) and grey (6 = Kano); neighboring African countries labeled by black arrows. The genotypes of the Nigerian isolates are labeled in red with the old Roumagnac haplotypes [11] in parentheses (red * denotes untypeable Nigerian strains). The 4.3.1 (H58) subclade is indicated in red italics. Branch lengths are indicative of the estimated substitution rate per variable site.
(TIF)
(XLS)
Data Availability Statement
All sequence read files are available from European Nucleotide Archive under accession number ERP005877.