Abstract
Acute respiratory failure contributes significantly to nonrelapse mortality after allogeneic hematopoietic stem cell transplantation. Although there is a trend of improved survival over time, mortality remains unacceptably high. An understanding of the pathophysiology of early respiratory failure, opportunities for targeted therapy, assessment of the patient at risk, optimal use of noninvasive positive pressure ventilation, strategies to improve alveolar recruitment, appropriate fluid management, care of the patient with chronic lung disease, and importantly, a team approach between critical care and transplantation services may improve outcomes.
Key Words: Respiratory failure, Transplantation
Highlights
-
•
Outcomes from acute respiratory failure after hematopoietic stem cell transplantation remain unacceptably high.
-
•
The review focuses on strategies to improve these outcomes.
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is a curative modality for patients with certain hematologic malignancies and nonmalignant disorders. Post-transplantation pulmonary complications and acute respiratory failure (ARF) contribute significantly to the morbidity and mortality from this procedure [1]. Although the incidence of ARF after HSCT has decreased over time, mortality remains high, particularly for patients who require endotracheal intubation and mechanical ventilation [2]. Hence, a team approach between transplantation, intensive care, and ancillary services is essential to improve outcomes. This review will highlight an approach to ARF from this perspective, focus on identifying patients at risk for ARF before transplantation, update definitions of pulmonary complications, discuss newer insights into pathophysiology and novel therapeutic options, explore the role of brocho-alveolar lavage (BAL) in the context of newly developed infectious diagnostic arrays, and include post–intensive care (ICU) rehabilitation.
Lung injury occurs in 25% to 55% of HSCT recipients and accounts for approximately 50% of transplantation-related mortality [3]. Lung injury may be classified as noninfectious or infectious. Noninfectious lung injury may be acute idiopathic pneumonia syndrome (IPS) or chronic, leading to either obstructive lung disease (OLD) or restrictive lung disease (RLD). OLD is defined on the basis of Global Lung Initiative (GLI)-2012 equations endorsed by the American Thoracic Society and the European Respiratory Society [4], as forced expiratory volume in second (FEV1) over forced vital capacity (FVC) less than lower limits of normal. RLD is defined as total lung capacity less than 80% predicted.
Noninfectious Lung Injury
Acute IPS: Pathophysiology
In 1993, a National Institutes of Health (NIH) workshop proposed a broad definition of IPS that included widespread alveolar injury in the absence of active lower respiratory infection, cardiogenic causes, acute renal failure, or iatrogenic fluid overload after HSCT [5]. The diagnostic criteria of IPS have been updated based on an official American Thoracic Society Research Statement (Table 1 ) and classified into entities based on anatomical sites of inflammation as related either to interstitial, vascular and airway tissue, or unclassifiable (Table 2 ) [6]. Clinical symptoms include cough, dyspnea, and hypoxemia with or without fever. Chest radiography may show bilateral infiltrates. The incidence of IPS in the first 120 days after allogeneic HSCT with myeloablative conditioning is 3% to 15% 5, 7. Risk factors include total body irradiation, older recipient age, and acute graft-versus-host disease (GVHD) 3, 8, 9. The incidence of IPS is lower after nonmyeloablative conditioning; however, the clinical course resulting in ARF and death once the diagnosis was established is unchanged [8]. IPS-related mortality has been historically high (>50%) despite treatment with corticosteroids [7]. Noninfectious lung injury occasionally occurs after autologous HSCT [10].
Table 1.
|
CMV indicates cytomegalovirus; RSV, respiratory syncytial virus; HSV, herpes simplex virus; VZV, varicella zoster virus.
Table 2.
Salient Clinical Features of Lung Injury Syndromes Defined under IPS
| Parenchyma |
| Acute interstitial pneumonitis: onset day 0-100 after transplantation. Secondary to chemotoxicity (BCNU, bleomycin, busulfan). |
| ARDS: Noncardiogenic capillary leak syndrome with onset day 0-30 after transplantation. |
| Delayed pulmonary toxicity syndrome: presents months to years after auto HSCT for breast cancer. |
| Vascular endothelium |
| Peri-engraftment respiratory distress syndrome: present within 5-7 days of engraftment may progress to ARDS. |
| Diffuse alveolar hemorrhage: progressively bloodier BAL fractions, presents within 0-100 days after transplantation. |
| Airway epithelium [6] |
| BOS: Diminished FEV1, onset 3-24 months after transplantation. Chest radiography may be normal or show hyperinflation. Chest CT may show mosaic attenuation, air trapping, septal lines, centrilobular nodules or bronchiectasis. Histology reveals bronchiolar inflammation with luminal obstruction. |
| COP (formerly known as bronchiolitis obliterans organizing pneumonia or BOOP): restrictive findings on spirometry, impaired DLCO, onset 2-12 months after transplantation. Chest CT may show patchy airspace disease, or nodular opacities. Histology reveals intraluminal organizing fibrosis in distal airspaces with mild interstitial inflammation. |
BCNU indicates Carmustine; DLCO, diffusing capacity for carbon monoxide; CT, computed tomography.
Murine models of IPS support the lung as a target of T cell–mediated injury after HSCT [11]. Increased TNF-α is found in the BAL fluid of mice with IPS [12]. A causal role for TNF-α has been established by neutralizing this cytokine in experimental HSCT models [13].
TNF-α–independent pathways may also contribute to the pathophysiology of IPS. Lipopolysaccharide levels are increased in BAL fluid of mice with IPS [12]. Translocation of lipopolysaccharide across a gut mucosa damaged in the early post-transplantation period stimulates the release of cytokines that contribute to lung damage and development of acute GVHD [14]. The lung is also sensitive to reactive oxygen species, whose production is enhanced in this setting [15]. Changes in exhaled nitric oxide, a marker of airway inflammation, are useful to guide risk stratification for noninfectious lung injury after lung transplantation [16]. Surfactant dysfunction caused by decreased synthesis in alveolar type II cells or degradation by oxidants likely contributes to IPS [17]. Transtracheal instillation of human surfactant protein-A attenuated the manifestations of IPS in mice [18]. Keratinocyte growth factor is a growth factor for type II pneumocytes in vivo. Keratinocyte growth factor increases lung surfactant levels, may detoxify reactive oxygen species, lowers serum TNF-α levels, and diminishes lung injury in IPS mouse models [19].
Investigators have also found an increased expression of CC-chemokine ligand 2 ([CCL-2]MCP-1) in murine lung models of IPS that paralleled the recruitment of leukocytes and cellular expression of Chemokine receptor 2 (CCR2) [20]. IL-6 generated by lung parenchyma promotes IPS via induction of Th17 differentiation [21]. High plasma concentrations of IL-6 at time of diagnosis are associated with lack of response to TNF inhibition [21]. Blockade of IL-6 signaling with anti-IL-6R monoclonal antibody (Tocilizumab, Genetech, Inc., San Francisco, CA) reduced GVHD while preserving a graft-versus-tumor effect in mice [22]. In summary, inflammatory factors contributing to IPS have strong foundations in basic science, offering promising targets for therapy.
Acute IPS: Clinical Spectrum
Engraftment syndrome
IPS is a syndrome with a wide clinical spectrum depending on the site of disease (Table 2). Engraftment syndrome is defined by consensus according to the criteria outlined by Spitzer [23] and is mainly characterized by fever, rash, and noncardiogenic pulmonary edema occurring at the time of neutrophil recovery after HSCT. The risk was reported to be higher among male recipients, myeloablative conditioning with total body irradiation (TBI) ≥ 1200 cGy, and unrelated donor HSCT [24]. Patients with engraftment syndrome were at higher risk for developing GVHD, and biomarkers such as suppression of tumorigenicity 2, interleukin 2 receptor alpha (IL2Rα), and tumor necrosis factor receptor 1 are elevated, as described in patients with GVHD [24].
Diffuse alveolar hemorrhage
Diffuse alveolar hemorrhage (DAH) originates from the pulmonary microvasculature in response to alveolar injury, which may be noninfectious; secondary to chemotherapy, radiation, or immune-mediated events; or due to systemic or pulmonary infections [25]. Older age, allogeneic donor source, myeloablative conditioning, and acute severe GVHD were independently predictive of an increased risk of DAH. The probability of 60-day survival is poor with >50% mortality in both noninfectious and infection-associated DAH.
Lung injury syndromes not defined under IPS
Other noninfectious pulmonary complications not included under the classification of IPS include radiation pneumonitis, pulmonary alveolar proteinosis involving the lung parenchyma, pulmonary veno-occlusive disease [26], pulmonary cytolytic thrombi [27], transfusion-related acute lung injury, pulmonary arterial hypertension, and pulmonary thrombo-embolism, all involving the vascular endothelium (Table 3 ).
Table 3.
Salient Clinical Features of Lung Injury Syndromes not Defined Under IPS
| Parenchyma |
| Radiation pneumonitis: restrictive findings on spirometry. Impaired DLCO, onset 2-4 months after therapy. |
| Pulmonary alveolar proteinosis: may occur early or late (1-2 years) after transplantation. Chest radiography may show crazy paving pattern. BAL shows milky periodic-acid-Schiff–positive milky fluid. |
| Vascular endothelium |
| Pulmonary veno-occlusive disease: occurs 2-6 months after transplantation and results in pulmonary hypertension. Histology reveals fibrous intimal proliferation of pulmonary venules. |
| Pulmonary cytolytic thrombi: observed in pediatric HSCT recipients 2-3 months after HSCT. Chest CT may show pulmonary nodules. Histology reveals thrombi in small to medium distal pulmonary vessels, associated with pulmonary infarction. |
| Transfusion-related acute lung injury: Present with fever, chills, leukopenia, acute dyspnea, and hypotension within 6 hours of cellular product infusion. Histology reveals aggregation of leukocytes in pulmonary vasculature. |
| Pulmonary artery hypertension: insidious onset of dyspnea, within 0-6 months after transplantation. Detected by follow-up echocardiogram. Histology reveals intimal hyperplasia in small pulmonary vessels. |
| Pulmonary thrombo-embolism: acute onset of fever, dry cough and dyspnea due to embolus in a pulmonary vein detected by chest CT or lung angiography. |
Chronic Pneumonia Syndromes
Bronchiolitis obliterans syndrome (BOS) is a progressive, insidious lung disease manifesting as new fixed airflow obstruction due to progressive circumferential fibrosis and cicatrization of the small terminal airways [28]. The pathogenesis of BOS involves both alloimmune and nonalloimmune (infectious, chemo-radiotherapy injury) processes, but the association between chronic GVHD and BOS is well accepted [29].
Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia, is a Th1 inflammatory disease [29]. HLA disparity, female-to-male HSCT, peripheral blood stem cell transplantation, and TBI-based regimen are associated with increased risk of COP [30]. An association between acute and chronic GVHD and the subsequent development of COP has been noted [31]. Although COP and BOS have both been associated with chronic GVHD, and occur in similar time frame, patients with BOS present without fever and have wheezing, whereas patients with COP present with fever and have crackles on physical examination. Other notable differences are described in Table 2. A lung biopsy is recommended for diagnosis of COP.
BOS causing obstructive lung disease and COP/bronchiolitis obliterans organizing pneumonia causing RLD may not be used interchangeably, as they have clinical, radiological, pulmonary function, and histological differences, as described in Table 2.
Infectious Lung Injury
Diagnostic Utility of BAL
Although the syndrome of IPS excludes infection, infectious lung injury has a role the pathophysiology of DAH and exacerbations of BOS. BAL should strongly be considered in patients with diffuse lung infiltrates after transplantation. The availability of automated multiplexed PCR for rapid and accurate detection of respiratory pathogens has increased the assay sensitivity and specificity to 80% to 100% and 100%, respectively [32]. BiofireFilmArray Respiratory Panel (BioFire Diagnostics, Inc., Salt Lake City, UT, USA) targets 20 pathogens including 17 viruses and subtypes and 3 bacteria, and it is performed with minimal sample manipulation [32]. Although 33% of BAL specimens on HSCT patients between days 31 to 100 were positive for infection in a retrospective study performed from 2001 to 2007 [33], with improved diagnostic arrays, this yield may be higher. Procedural complications were noted in only 3.6% of cases, and only 2% of patients required intubation and mechanical ventilation within 48 hours after procedure. BAL data resulted in changes in medical management in approximately 60% of cases [33]. The diagnostic yield of BAL was as high as 75% when performed within 24 hours of clinical presentation [34]. Procedural complications occurred in only .6% of patients in this study. Pathogens detected in the lower respiratory tract with BAL often differ from those detected in the upper respiratory tract with a nasopharyngeal wash. In addition, assay for galactomannan in BAL has a 93% negative predictive value for diagnosing proven and probable invasive fungal infections (IFI) [35]. Further, institution of corticosteroid therapy for IPS may cause more harm than benefit in the context of an undiagnosed infection. The risks associated with empiric antimicrobial therapy, including medication side effects and development of resistance, compound the potential harm of delaying targeted management.
IFI
Isolated lung involvement alone accounts for 49.4% of deaths due to proven IFI after HSCT [36]. In a review of cases of aspergillosis over a 34-year period at our institution, no cases of isolated abdominal or pelvic disease were noted; the lung was the most common organ involved with concurrent abdominal disease [37]. IFI of the lung have decreased with better antifungal prophylaxis and pre-emptive screening with galactomannan 36, 37, 38, 39. The use of PCR and other molecular approaches, such as matrix-assisted laser desorption ionization, have proved promising in clinical trials and their use after standardization may reduce the need for antifungal therapy [40].
Viral Pathogens
Both prophylaxis and pre-emptive therapy based on surveillance molecular screening have substantially reduced the incidence of cytomegalovirus disease after transplantation [41]. Novel drugs, such as maribavir, letermovir, and brincidofovir, are undergoing clinical trials [41]. Adoptive cellular therapy promises to restore antiviral immunity in the absence of significant toxicity and with a low risk of induction of GVHD 42, 43, 44. DAS181, a novel sialidase fusion protein against parainfluenza virus [45], is undergoing randomized placebo-controlled clinical trial in older children and adults (NCT01644877). Treatment with oral GS-5806, a respiratory syncytial virus–entry inhibitor, reduced viral load and severity of disease in a double-blind, placebo-controlled study in healthy adults [46]. These approaches, when translated into clinical practice, may reduce infectious-associated lung injury after transplantation.
Approach to Patients with Pulmonary Dysfunction
Identification of Patients at Risk
Patients at risk for pulmonary dysfunction after transplantation should be identified on pretransplantation evaluation based on pulmonary function testing (PFT). Children with noninfectious and infectious pulmonary complications after transplantation had a significantly lower forced expiratory flow at 25% to 75% of vital capacity on pretransplantation PFT [47]. Lower FEV1, FVC, and RLD predicted worse overall survival [47]. Reduced pretransplantation FEV1 and FVC were associated with higher risk of early respiratory failure [48]. A worse lung function score, a combined measurement of FEV1 and single-breath diffusing capacity for carbon monoxide was associated with poor survival [49]. These patients may benefit from non TBI-based conditioning, lung shielding, prevention of GVHD, and close monitoring of PFT after transplantation. Patients receiving myeloablative conditioning had much greater declines in FEV1 compared with those receiving nonmyeloablative conditioning, with a higher mortality risk, especially if the pretransplantation FEV1 was less than 60% [50]. For patients with combined ventilation/diffusing capacity deficits before transplantation, reduction in lung TBI dose improved survival [51]. Further, for patients with abnormal pretransplantation lung function and others with evolving pulmonary dysfunction after transplantation, our approach is to conduct weekly multidisciplinary rounds in conjunction with the intensive care team to discuss strategies to prevent further respiratory compromise.
Acute IPS
Neutralization of TNF-α reduces lung injury after experimental allogeneic HSCT [13]. Etanercept (Enbrel; Immunex, Seattle, WA) is a dimeric protein consisting of 2 soluble p75 TNF receptors fused to the Fc portion of a type I IgG1 molecule. Significant improvements in day 28 survival were reported in several single-institutional, nonrandomized studies combining etanercept with corticosteroids 52, 53, 54. A randomized, multicenter, double-blind, placebo-controlled trial of etanercept for treatment of IPS after allogeneic HSCT in adults was halted because of accrual of only 34 subjects and precluded a definitive conclusion [55]. Etanercept administration was not associated with increased toxicity, increased incidence of opportunistic infections, or risk of relapse compared with placebo controls [55]. A multicenter phase II trial of etanercept with corticosteroids in children with IPS accrued 28 evaluable patients. Complete responses were seen in 20 (71%) patients, with a median time to response of 10 days. Response rates were higher in patients not requiring mechanical ventilation at study entry and overall survival at 1 year after therapy was 63%, comparing favorably with historical data [56]. Early recognition of the disorder, BAL to exclude infectious pathogens, and therapy with etanercept and corticosteroids may improve outcome after IPS.
Engraftment Syndrome
Corticosteroids are often dramatically effective in patients with engraftment syndrome. A dose of 1 m/kg/day for 3 days with no taper is suggested. Higher nonrelapse mortality and lower overall survival at 2 years in patients with engraftment syndrome was reported despite use of corticosteroids [24].
DAH
High-dose corticosteroids have not altered the poor outcome associated with DAH [25]. In a large retrospective study, patients with DAH who received steroids <250 mg/day had lower mortality compared with those receiving medium- and high-dose steroids [57]. Adjunctive treatment with aminocaproic acid did not produce difference in outcomes, and 100-day mortality was as high as 85% [57]. A previous study in a small group of 8 patients showed that the use of aminocaproic acid with corticosteroids was safe and had a favorable effect on survival [58]. Factor VIIa has also been used in addition to steroids to control the acute stage of DAH. However, in a recent retrospective study, the use of factor VIIa in combination with steroids did not improve the time of resolution of DAH, duration of mechanical ventilation, or hospital mortality compared with outcomes after steroids alone [59].
BOS
Avoidance of systemic steroids and treatment with inhaled budesonide/formoterol was shown to significantly improve FEV1 as early as 2 month after treatment initiation in a randomized, double-blind, placebo-controlled study in 32 patients with moderate to severe BOS [60]. A trial using fluticasone, azithromycin, and montelukast for BOS is ongoing (NCT01307462). A case series of 8 patients showed similar change in FEV1 compared to a historical group who received high-dose corticosteroids. Reducing systemic corticosteroid exposure reduced treatment-related morbidity in BOS with no change in efficacy [61]. Etanercept, in addition to its efficacy in IPS, may have a potential role in the treatment of subacute lung injury in patients at least 100 days after allogeneic HSCT. Etanercept was well tolerated in this population, and objective responses were seen in 32% of patients [62].
A randomized, double-blind, placebo-controlled trial of inhaled cyclosporine in addition to systemic immunosuppression after lung transplantation improved survival and extended periods of chronic rejection-free survival. Histologically, chronic rejection in lung transplantation presents as BOS [63]. The excellent negative predictive value of persistently low fractional exhaled nitric oxide for early diagnosis of BOS after lung transplantation suggests a value to exploring these novel diagnostic and therapeutic modalities to treat BOS after HSCT [16]. A placebo-controlled trial of azithromycin therapy given on alternate days for 12 weeks in patients with BOS after lung transplantation showed significant improvement in FEV1 [64].
Early identification and management of patients with evolving pulmonary dysfunction before development of symptoms is critical to improve outcomes. The NIH symptom-based lung score with score 0 (no symptoms), score 1 (shortness of breath with climbing stairs), score 2 (shortness of breath on flat ground), and score 3 (shortness of breath at rest or requiring oxygen) was associated with nonrelapse mortality and overall survival [65]. Even an NIH symptom-based lung score of 1 was associated with worse overall survival compared with those with a score of 0. Worsening of NIH symptom-based lung score was associated with increased mortality [65].
More frequent monitoring with PFT using GLI-2012 indices may detect changes before symptoms develop and guide management. The GLI-2012 equations are based on a very large reference population of ages 3 to 95 years and produces age-specific spirometric indices for lower limits of normal. Using fixed thresholds for FEV1/FVC < .70 could misdiagnose >20% of patients referred for PFT [66]. Computed tomography–based imaging biomarkers may provide a unique signature for diagnosis of small airway disease and disease progression [67]. Clinical biomarkers may aid early diagnosis and prognostication of patients with evolving pulmonary dysfunction. Serum levels of suppression of tumorigenicity 2 were significantly elevated in patients with acute exacerbations of idiopathic pulmonary fibrosis and these levels inversely correlated with PaO2/FiO2 [68].
COP
Symptoms typically respond to corticosteroids. Preventive azithromycin treatment reduced noninfectious lung injury and acute GVHD in a murine model of allogeneic HSCT [69]. Macrolides in patients with acute lung injury have been shown to improve survival and shorten the time to successful discontinuation of mechanical ventilation [70].
Novel Investigational Agents
Cell-based therapy with bone marrow–derived mesenchymal stem cells is a potentially attractive new therapeutic option for treating patients with acute respiratory distress syndrome (ARDS) [71] and has shown to be efficacious in repair of established injury in animals [72].
IL-6 plays a role in the pathophysiology of IPS [21]. Blockade of IL-6 with toclilizumab reduced GVHD in mouse models [22]. Addition of tocilizumab to standard GVHD prophylaxis for patients who received HLA-matched allogeneic HSCT was shown to be safe and associated with a very low incidence of significant acute GVHD [73]. Tocilizumab is available for clinical use and may be considered in research studies in combination with etanercept and corticosteroids.
Recently, preclinical studies have uncovered possible novel strategies to treat BOS. Ibrutinib is a Food and Drug Administration–approved reversible inhibitor of Bruton's tyrosine kinase and IL-2 inducible T cell kinase that targets Th2 cells and B cells. In an alloantibody-driven multiorgan-system chronic GVHD murine model that induces BOS, ibrutinib treatment ameliorated pulmonary fibrosis and curtailed the development of BOS in vivo as measured by pulmonary function parameters, including resistance, elastance, and compliance [74]. In another murine model with BOS as a prominent manifestation, lung pathology developed in an IL-17 and colony-stimulating factor-1R–dependent manner. Anti–colony-stimulating factor-1R antibody significantly improved all pulmonary function parameters and resulted in significant reduction in collagen deposition [75].
ICU Care
Noninvasive Positive Pressure Ventilation
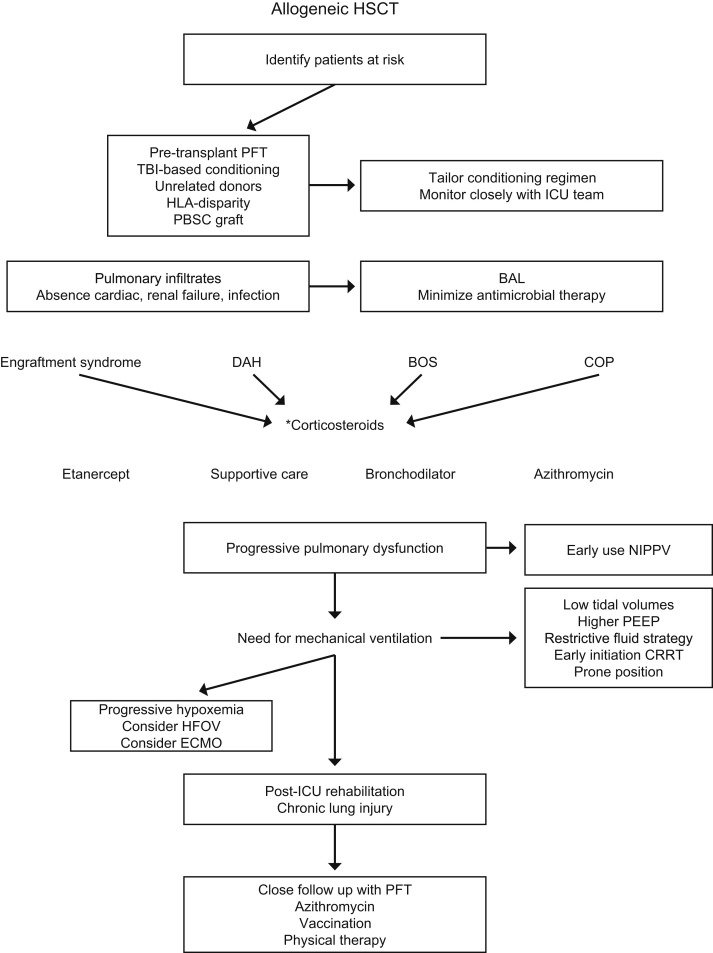
Noninvasive positive pressure ventilation (NIPPV) has been increasingly used in the last decade to support patients with ARF. In some instances, it helps avoid endotracheal intubation and invasive mechanical ventilation. It is of particular interest in patients who are highly susceptible to infections because it does not breach the respiratory barrier. In a recent survey that explored the variation in the care of critically ill pediatric HSCT patients in North America, all 33 centers included in the study reported the use of bontinuous positive airway pressure (CPAP)/bilevel positive airway pressure (BiPAP) before intubation [76]. A success rate (defined as the absence of subsequent endotracheal intubation) as high as 74.2% in 239 immune-compromised children has been reported [77]. Cardiovascular dysfunction was 1 of the predictive factors for NIPPV failure [77]. In a postallogeneic HSCT adult cohort, the early initiation of noninvasive ventilation was associated with better oxygenation but did not improve survival or need for mechanical ventilation [78]. The benefit from the NIPPV is usually seen early within few hours of its application. Therefore, evolving pulmonary dysfunction in patients at risk (Figure 1 ) should prompt escalation of therapy to the use of invasive mechanical ventilation.
Figure 1.
Approach to a patient with evolving pulmonary dysfunction after allogeneic HSCT. ∗A short course of corticosteroids without taper is suggested for engraftment syndrome. Doses ≤2 mg/kg/day may be used for DAH. Inhaled steroids are recommended for BOS. A prolonged course of steroids may be necessary for COP. PFT, pulmonary function test; BAL, broncho-alveolar lavage; DAH, diffuse alveolar hemorrhage; BOS, bronchiolitis obliterans syndrome; COP, cryptogenic organizing pneumonia; NIPPV, non-invasive positive pressure ventilation; PEEP, positive end-expiratory pressure; CRRT, continuous renal replacement therapy; HFOV, high-frequency ventilation; ECMO, extra-corporeal membrane oxygenation.
Ventilation Strategies: Conventional Mechanical Ventilation
Nearly one half of children admitted to the pediatric ICU after transplantation will require mechanical ventilation [79]. A common theme that is particularly true of post-transplantation patients with respiratory failure who require mechanical ventilation is the clear and early derecruitment of distal alveolar air space available for effective gas exchange. The pathophysiology of IPS involves loss of alveolar air space as a critical element leading to hypoxemia. Efforts aimed at minimizing alveolar derecruitment include judicious use of positive end-expiratory pressure (PEEP) with low tidal volume (TV) strategies (6 mL/kg). Likewise, goals of ventilation may need to be moderated toward maintaining pH > 7.25 and supporting oxygen saturation to >85%. A landmark study from the ARDS Network evaluated higher versus lower TV mechanical ventilation and demonstrated a reduction in mortality from 40% to 31% with 6 mL/kg ideal body weight TV, compared to 12 mL/kg ideal body weight TV [80]. To achieve optimal lung protection, the lowest plateau pressure and TV possible should be selected. Accumulating observational evidence suggests that TV should be limited in all mechanically ventilated patients—even in those who do not have ARDS. PEEP should be set to maximize alveolar recruitment while avoiding over-distention. Judicious use of higher PEEP may be needed in clinical settings of DAH or engraftment syndrome.
Ventilation Strategies: High-Frequency Oscillatory Ventilation
High-frequency oscillatory ventilation (HFOV) is an alternative technique of ventilation in which small TV are delivered at high frequencies (3 to 15 Hz) with an oscillatory pump [81]. Thus, high-frequency oscillation theoretically meets the goals of a strategy of lung protective ventilation with extremely small TV (1 to 4 mL/kg) and constant lung recruitment. The benefit of HFOV in treatment of ARDS is still controversial. In patients with ARDS, HFOV reduced hospital and 30-day mortality and resulted in improved oxygenation, as measured by the partial arterial oxygen saturation/inspired oxygen fraction (PaO2/FiO2) ratio [82]. However, a recent multicenter, randomized controlled trial of HFOV versus conventional mechanical ventilation in 548 adult patients with ARDS concluded that mortality was actually higher in patients receiving early HFOV [83]. Pediatric literature is also inconclusive, but many centers reported improved gas exchange with the use of HFOV [84]. Therefore, the use of HFOV may still be suitable as a rescue treatment in patients with refractory hypoxemia, when higher mean airway pressures or FiO2 are required to maintain oxygenation.
Prone Positioning
Prone positioning can improve ventilation perfusion mismatch and help to recruit dependent lung regions and drain tracheobronchial secretions. Although earlier studies failed to show survival benefit, recent evidence suggests that interval prone positioning in patients with severe ARDS can reduce mortality. In a recent multicenter randomized trial, 474 adult patients with severe ARDS (PaO2/FiO2 <150) were randomized either to standard supine or interval prone positioning with protective mechanical ventilation strategies implemented in both groups. Mortality was significantly lower in patients undergoing interval prone positioning compared with that for patients in supine position (24% versus 41%, P < .001) [85]. Although prone positioning may offer benefits in treating children with ARDS, it has to be done cautiously as it is associated with increased frequency of adverse events, such as airway obstruction, hypotension, vomiting, and accidental extubation [86].
Fluid Management
Recently, the ARDS Network Fluid and Catheter Treatment Trial reported that a conservative fluid management strategy, compared with a liberal fluid strategy, increased the mean number of ventilator-free days in adult patients with acute lung injury (15 versus 12 days respectively, P < .001) [87]. In addition to this beneficial effect on outcomes, the study found that the conservative fluid strategy did not increase the incidence of renal failure or the development of shock. There is growing evidence that fluid overload in critically ill children is associated with worse outcome. In a large series of 297 critically ill children receiving continuous renal replacement therapy (CRRT), children with fluid overload ≥20% had a higher adjusted mortality rate of 8.5 compared with those with <20% [88]. There was a 3% increase in mortality for each 1% increase in fluid overload at CRRT initiation. Children after transplantation are at higher risk of fluid overload. In addition, in many instances, they manifest capillary leak that renders fluid management more challenging. In a retrospective review of 26 children after transplantation children with acute renal failure and fluid overload, <10% fluid overload was associated with better survival [89]. Early initiation of CRRT for treatment of fluid overload when diuretic therapy fails may help to improve oxygenation and outcome. In a retrospective review in our institution that included 30 post-transplantation pediatric patients with acute lung injury who underwent CRRT from 1994 to 2006, CRRT was associated with significant improvement of oxygenation 24 and 48 hours after initiation of this therapy. PaO2/FiO2 increased significantly with median increase of 31 and 43 in the 24- and 48-hour intervals after initiation of CRRT compared with the 24-hour interval before CRRT. This improvement in PaO2/FiO2 was associated with the reduction of fluid balance after initiation of CRRT [90]. In a cohort of 51 pediatric stem cell recipients (both autologous and allogeneic) on CRRT, survivors had lower mean airway pressure at the end of CRRT compared to nonsurvivors receiving mechanical ventilation [91]. This suggests that the etiology of underlying pulmonary dysfunction may influence the beneficial effects of CRRT.
Corticosteroids and Surfactant Therapy in ARDS
The benefit of corticosteroids to treat acute lung injury has been controversial with some studies showing clear benefit, whereas other studies reporting increased mortality when used >13 days after the onset of ARDS. A meta-analysis of 5 randomized trials of the use of corticosteroid in ARDS showed that prolonged corticosteroid treatment was associated with significant improvement in PaO2/FiO2 ratio, as well as significant reduction in duration of mechanical ventilation and ICU stay [92]. When mortality was adjusted to include some of the variables that were not balanced between this and the control groups in the meta-analysis, 60-day mortality diminished from 28% to 11% and was not statistically significant [92].
Surfactant dysfunction likely contributes to IPS [17]. Transtracheal instillation of human surfactant protein-A attenuated the manifestations of IPS in mice [18]. A recent randomized, double-blinded, controlled study of the use of calfactant in children with ARDS did not show improvement in oxygenation, hospital-free days, or 90-day mortality rate [93]. A post hoc analysis of immune-compromised cohort of 52 children with acute lung injury suggested a potential benefit of calfactant in this population to reduce mortality and improve oxygenation [94]. This is being explored with an ongoing multicenter randomized trial investigating the use of calfactant in children after transplantation (NCT00999713).
Role of Extracorporeal Membrane Oxygenation
Extracorporeal membrane oxygenation (ECMO) is used in children with acute respiratory or cardiac failure when other conventional methods of treatment fail and the risk of mortality is high. The reported survival rate of children with respiratory failure requiring ECMO is 57% [95]. However, children after transplantation who have undergone ECMO have a significantly lower survival rate, ranging from 5% to 21% [96]. Factors that increase risk of mortality include longer duration from intubation to initiation of ECMO (median of 8 days), higher PEEP at 24 hours after initiating ECMO, as well as higher number of organ dysfunction [96]. ECMO requires anticoagulation, which can be challenging after transplantation. In a series of 19 children after transplantation who underwent ECMO, bleeding complications occurred in 53%. ECMO can be considered early in the course of severe respiratory failure; however, the prognosis is still poor.
Outcome of ARF
Mortality from ARF is high, ranging from 42% to 84% 79, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108 (Table 4 ). We have recently reported the largest single-institution retrospective review of outcomes for pediatric oncology and post-transplantation patients requiring invasive mechanical ventilation, documenting an encouraging and steady trend of improved survival over time [105]. A recent prospective multicenter study reported a 52% mortality rate; severe impairment in oxygenation, use of CRRT, and cytomegalovirus viremia were independent predictors of mortality [108].
Table 4.
Overview of Studies on Outcome after ARF for Children after Transplantation Requiring Mechanical Ventilation
| Study Design | Enrollment Period | Ventilated HSCT Patients, n | PICU Survival, % | Long-Term Survival | Factors Associated with Mortality | Reference |
|---|---|---|---|---|---|---|
| Retrospective | 1983-1996 | 121 | 16 | N/A | Respiratory failure, pulmonary dysfunction, >1 organ dysfunction | [97] |
| Retrospective | 1990-1999 | 86 | 41 | 20% 2 yr | Hepatic dysfunction, use of HFOV | [98] |
| Retrospective | 1991-2000 | 34 | 24 | N/A | Male gender, MOF ≥3, hemorrhagic cystitis, GVHD grades III-IV | [99] |
| Prospective | 1993-2001 | 24 | 21 | 17% 1 yr | MOF | [100] |
| Retrospective | 1994-1998 | 31 | 42 | 13% 6 mo | MV >48 hr | [101] |
| Retrospective | 1998-2001 | 13 | 15 | NR | MV >5 d | [102] |
| Retrospective | 1992-2004 | 65 | ∗59 | 54% 100 d | PaO2/FiO2 <300, PEEP >8 cm 24 hours, no survivor HFOV | [103] |
| Meta-analysis | 1973-2004 | 822 | 29 | N/A | Pulmonary infection | [104] |
| Retrospective | 1996-2004 | 206 | 45 | 18% 6 mo | Previous intubation within 6 months, hepatic/cardiac failure | [105] |
| Retrospective | 2000-2006 | 36 | 31 | 25% 6 mo | MV >7 d, CRRT >7 d, pressor support | [106] |
| Retrospective | 2002-2009 | 28 | 31 | N/A | †Oxygenation index ≥25 associated with100% mortality | [107] |
| Retrospective | 2004-2010 | 88 | 39 | N/A | CRRT | [108] |
PICU, pediatric intensive care-unit; N/A, not available; MOF, multi-organ failure; MV, mechanical ventilation; NR, not reported.
During the period 2000-2004.
Oxygenation index is defined as FiO2/PaO2 x mean airway pressure.
Mortality in patients with ARF after transplantation who require CRRT is high. Coordination of care between critical care, transplantation, pulmonary, nephrology, pharmacy, nutritional, and other services is imperative to improve outcome, counsel HSCT patients, and their families. Perspectives from team members in the different services may be at variance, albeit complimentary when put together.
Post-ICU Care and Management of Chronic Lung Disease
Patients with chronic lung disease require more frequent monitoring of symptoms, PFT, and a 6-minute walk test at each clinic visit to assess response to bronchodilator/steroid therapy [109]. Cardio-pulmonary exercise testing may be performed if indicated. Overnight pulse-oximetry may be considered to assess need for supplemental oxygen during sleep, as hypoxia may go unnoticed and lead to pulmonary hypertension. Development of pulmonary hypertension has been associated with BOS in lung transplant recipients [110]. Transthoracic echocardiography is an excellent screening tool for pulmonary hypertension. Seasonal influenza vaccine and protective pneumococcal titers may be beneficial, as respiratory viral infections are not uncommon late after allogeneic HSCT [111]. Physical therapy to build cardiorespiratory endurance and avoidance of active or passive smoking is important. Repair of impaired pulmonary function with recovery of diffusing capacity for carbon monoxide was observed 10 years after allogeneic HSCT [112].
Conclusions
Outcome of ARF can be improved with a team approach from both critical care and transplantation services by identifying patients at risk, early diagnosis of IPS with BAL, incorporating newer advances in targeted drug therapy, using noninvasive positive pressure ventilation with respiratory decompensation, minimizing alveolar derecruitment with mechanical ventilation, restricting fluids, early initiation of CRRT, use of HFOV and ECMO with progressive hypoxemia, possibly cellular therapy in the future, and close follow-up of the patient with chronic lung disease.
Acknowledgments
Financial disclosure statement: This work was supported by National Cancer Institute Cancer Center CORE Support Grant P30 CA 21765 and by the American Lebanese Syrian Associated Charities.
Conflict of interest statement: There are no conflicts of interest to report.
Authorship statement: L.E. and A.S. contributed equally to this work and should be considered as co-first authors.
Footnotes
Financial disclosure: See Acknowledgments on page 624.
References
- 1.Eikenberry M., Bartakova H., Defor T. Natural history of pulmonary complications in children after bone marrow transplantation. Biol Blood Marrow Transplant. 2005;11:56–64. doi: 10.1016/j.bbmt.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Clark J.G., Madtes D.K., Martin T.R. Idiopathic pneumonia after bone marrow transplantation: cytokine activation and lipopolysaccharide amplification in the bronchoalveolar compartment. Crit Care Med. 1999;27:1800–1806. doi: 10.1097/00003246-199909000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Crawford S.W., Hackman R.C. Clinical course of idiopathic pneumonia after bone marrow transplantation. Am Rev Resp Dis. 1993;147:1393–1400. doi: 10.1164/ajrccm/147.6_Pt_1.1393. [DOI] [PubMed] [Google Scholar]
- 4.Quanjer P.H., Stanojevic S., Cole T.J. ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3-95 yr age range: the Global Lung Function 2012 equations. Eur Respir J. 2012;40:1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark J.G., Hertz M.I., Parkman R. Idiopathic pneumonia syndrome after bone marrow transplantation. Am Rev Respir Dis. 1993;147:1601–1606. doi: 10.1164/ajrccm/147.6_Pt_1.1601. [DOI] [PubMed] [Google Scholar]
- 6.Panoskaltsis-Mortari A., Griese M., Madtes D.K. An official American Thoracic Society Research Statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med. 2011;183:1262–1279. doi: 10.1164/rccm.2007-413ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Afessa B., Litzow M.R., Tefferi A. Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;28:425–434. doi: 10.1038/sj.bmt.1703142. [DOI] [PubMed] [Google Scholar]
- 8.Fukuda T., Hackman R.C., Guthrie K.A. Risks and outcomes of idiopathic pneumonia syndrome after nonmyeloablative and conventional conditioning regimens for allogeneic hematopoietic stem cell transplantation. Blood. 2003;102:2777–2785. doi: 10.1182/blood-2003-05-1597. [DOI] [PubMed] [Google Scholar]
- 9.Weiner R.S., Bortin M.M., Gale R.P. Interstitial pneumonitis after bone marrow transplantation: assessment of risk factors. Ann Intern Med. 1986;104:168–175. doi: 10.7326/0003-4819-104-2-168. [DOI] [PubMed] [Google Scholar]
- 10.Afessa B., Tefferi A., Litzow M.R. Diffuse alveolar hemorrhage in hematopoietic stem cell transplant recipients. Am J Resp Crit Care Med. 2002;166:641–645. doi: 10.1164/rccm.200112-141cc. [DOI] [PubMed] [Google Scholar]
- 11.Panoskaltsis-Mortari A., Taylor P.A., Yaeger T.M. The critical early proinflammatory events associated with idiopathic pneumonia syndrome in irradiated murine allogeneic recipients are due to donor T cell infusion and potentiated by cyclophosphamide. J Clin Invest. 1997;100:1015–1027. doi: 10.1172/JCI119612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooke K.R., Kobzik L., Martin T.R. An experimental model of idiopathic pneumonia syndrome after bone marrow transplantation: I. The roles of minor H antigens and endotoxin. Blood. 1996;88:3230–3239. [PubMed] [Google Scholar]
- 13.Cooke K.R., Hill G.R., Gerbitz A. Tumor necrosis factor-alpha neutralization reduces lung injury after experimental allogeneic bone marrow transplantation. Transplantation. 2000;70:272–279. doi: 10.1097/00007890-200007270-00006. [DOI] [PubMed] [Google Scholar]
- 14.Cooke K.R., Hill G.R., Crawford J.M. Tumor necrosis factor-alpha production to lipopolysaccharide stimulation by donor cells predicts the severity of experimental acute graft-versus-host disease. J Clin Invest. 1998;102:1882–1891. doi: 10.1172/JCI4285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang S., Porter V.A., Cornfield D.N. Effect of oxidant stress on inflammation and survival of iNOS knockout mice after marrow transplantation. Am J Physiol Lung Cell Mol Physiol. 2001;281:L922–L930. doi: 10.1152/ajplung.2001.281.4.L922. [DOI] [PubMed] [Google Scholar]
- 16.Neurohr C., Huppmann P., Leushner S. Usefulness of exhaled nitric oxide to guide risk stratification for bronchiolitis obliterans syndrome after lung transplantation. Am J Transplant. 2011;11:129–137. doi: 10.1111/j.1600-6143.2010.03327.x. [DOI] [PubMed] [Google Scholar]
- 17.Gunther A., Siebert C., Schmidt R. Surfactant alterations in severe pneumonia, acute respiratory distress syndrome, and cardiogenic lung edema. Am J Respir Crit Care Med. 1996;153:176–184. doi: 10.1164/ajrccm.153.1.8542113. [DOI] [PubMed] [Google Scholar]
- 18.Yang S., Milla C., Panoskaltsis-Mortari A. Surfactant protein A decreases lung injury and mortality after murine marrow transplantation. Am J Respir Cell Mol Biol. 2002;27:297–305. doi: 10.1165/rcmb.2002-0035OC. [DOI] [PubMed] [Google Scholar]
- 19.Panoskaltsis-Mortari A., Ingbar D.H., Jung P. KGF pretreatment decreases B7 and granzyme B expression and hastens repair in lungs of mice after allogeneic BMT. Am J Physiol Lung Cell Mol Physiol. 2000;278:L988–L999. doi: 10.1152/ajplung.2000.278.5.L988. [DOI] [PubMed] [Google Scholar]
- 20.Hildebrandt G.C., Duffner U.A., Olkiewicz K.M. A critical role for CCR2/MCP-1 interactions in the development of idiopathic pneumonia syndrome after allogeneic bone marrow transplantation. Blood. 2004;103:2417–2426. doi: 10.1182/blood-2003-08-2708. [DOI] [PubMed] [Google Scholar]
- 21.Varelias A., Gartlan K.H., Kreijveld E. Lung parenchyma-derived IL-6 promotes IL-17A-dependent acute lung injury after allogeneic stem cell transplantation. Blood. 2015;125:2435–2444. doi: 10.1182/blood-2014-07-590232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tawara I., Koyama M., Liu C. Interleukin-6 modulates graft-versus-host responses after experimental allogeneic bone marrow transplantation. Clin Cancer Res. 2010;17:77–88. doi: 10.1158/1078-0432.CCR-10-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spitzer T.R. Engraftment syndrome following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27:893–898. doi: 10.1038/sj.bmt.1703015. [DOI] [PubMed] [Google Scholar]
- 24.Chang L., Frame D., Braun T. Engraftment syndrome following allogeneic hematopoietic cell transplantation predicts poor outcomes. Biol Blood Marrow Transplant. 2014;20:1407–1417. doi: 10.1016/j.bbmt.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Majhail N.S., Parks K., Defor T.E., Weisdorf D.J. Diffuse alveolar hemorrhage and infection-associated alveolar hemorrhage following hematopoietic stem cell transplantation: related and high-risk clinical syndromes. Biol Blood Marrow Transplant. 2006;12:1038–1046. doi: 10.1016/j.bbmt.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Troussard X., Bernaudin J.F., Cordonnier C. Pulmonary veno-occlusive disease after bone marrow transplantation. Thorax. 1984;39:956–957. doi: 10.1136/thx.39.12.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woodard J.P., Gulbahce E., Shreve M. Pulmonary cytolytic thrombi: a newly recognized complication of stem cell transplantation. Bone Marrow Transplant. 2000;25:293–300. doi: 10.1038/sj.bmt.1702137. [DOI] [PubMed] [Google Scholar]
- 28.Williams K.M., Chien J.W., Gladwin M.T., Pavletic S.Z. Bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. JAMA. 2009;302:306–314. doi: 10.1001/jama.2009.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwarer A.P., Hughes J.M., Trotman-Dickenson B. A chronic pulmonary syndrome associated with graft-versus-host disease after allogeneic marrow transplantation. Transplantation. 1992;54:1002–1008. doi: 10.1097/00007890-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Nakasone H., Onizuka M., Suzuki N. Pre-transplant risk factors for cryptogenic organizing pneumonia/bronchiolitis obliterans organizing pneumonia after hematopoietic cell transplantation. Bone Marrow Transplant. 2013;48:1317–1323. doi: 10.1038/bmt.2013.116. [DOI] [PubMed] [Google Scholar]
- 31.Freudenberger T.D., Madtes D.K., Curtis J.R. Association between acute and chronic graft-versus-host disease and bronchiolitis obliterans organizing pneumonia in recipients of hematopoietic stem cell transplants. Blood. 2003;102:3822–3828. doi: 10.1182/blood-2002-06-1813. [DOI] [PubMed] [Google Scholar]
- 32.Babady N.E. The FilmArray® respiratory panel: an automated, broadly multiplexed molecular test for the rapid and accurate detection of respiratory pathogens. Expert Rev Mol Diagn. 2013;13:779–788. doi: 10.1586/14737159.2013.848794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yanik G., Maslak J., Connelly J. Impact of broncho-alveolar lavage on the diagnosis and management of pulmonary complications post transplant. Biol Blood Marrow Transplant. 2008;14:33. [supplement] [Google Scholar]
- 34.Shannon V.R., Andersson B.S., Lei X. Utility of early versus late fiberoptic bronchoscopy in the evaluation of new pulmonary infiltrates following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2010;45:647–655. doi: 10.1038/bmt.2009.203. [DOI] [PubMed] [Google Scholar]
- 35.Affolter K., Tamm M., Jahn K. Galactomannan in bronchoalveolar lavage for diagnosing invasive fungal disease. Am J Respir Crit Care Med. 2014;190:309–317. doi: 10.1164/rccm.201403-0431OC. [DOI] [PubMed] [Google Scholar]
- 36.Alsharif M., Cameron S.E.H., Young J.A.H. Time trends in fungal infections as a cause of death in hematopoietic stem cell transplant recipients. Am J Clin Pathol. 2009;132:746–755. doi: 10.1309/AJCPV9DC4HGPANKR. [DOI] [PubMed] [Google Scholar]
- 37.Abbasi S., Shenep J.L., Hughes W.T., Flynn P.M. Aspergillosis in children with cancer: A 34-year experience. Clin Infect Dis. 1999;29:1210–1219. doi: 10.1086/313445. [DOI] [PubMed] [Google Scholar]
- 38.van Burik J.H., Leisenring W., Myerson D. The effect of prophylactic fluconazole on the clinical spectrum of fungal disease in bone marrow transplant recipients with special attention to hepatic candidiasis. An autopsy study of 355 patients. Medicine. 1998;77:246–254. doi: 10.1097/00005792-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Maron G.M., Hayden R.T., Rodriguez A. Voriconazole prophylaxis in children with cancer: changing outcomes and epidemiology of fungal infections. Pediatr Infect Dis J. 2013;32:e451–e455. doi: 10.1097/INF.0b013e3182a74233. [DOI] [PubMed] [Google Scholar]
- 40.Arvanitis M., Anagnostou T., Fuchs B.B. Molecular and nonmolecular diagnostic methods for invasive fungal infections. Clin Microbiol Rev. 2014;27:490–526. doi: 10.1128/CMR.00091-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boeckh M., Murphy W.J., Peggs K.S. Recent advances in cytomegalovirus: an update on pharmacologic and cellular therapies. Biol Blood Marrow Transplant. 2015;21:24–29. doi: 10.1016/j.bbmt.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 42.Leen A.M., Bollard C.M., Mendizabal A.M. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood. 2013;121:5113–5123. doi: 10.1182/blood-2013-02-486324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feucht J., Opherk K., Lang P. Adoptive T-cell therapy with hexon-specific Th1 cells as a treatment of refractory infection after HSCT. Blood. 2015;125:1986–1994. doi: 10.1182/blood-2014-06-573725. [DOI] [PubMed] [Google Scholar]
- 44.Saglio F., Hanley P.J., Bollard C.M. The time is now: moving toward virus-specific T cells after allogeneic hematopoietic stem cell transplantation as the standard of care. Cytotherapy. 2014;16:149–159. doi: 10.1016/j.jcyt.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chalkias S., Mackenzie M.R., Gay C. DAS181 treatment of hematopoietic stem cell transplant patients with parainfluenza virus lung disease requiring mechanical ventilation. Transpl Infect Dis. 2014;16:141–144. doi: 10.1111/tid.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeVincenzo J.P., Whtiley R.J., Mackman R.L. Oral GS-5806 activity in a respiratory syncytial virus challenge study. N Engl J Med. 2014;37:711–722. doi: 10.1056/NEJMoa1401184. [DOI] [PubMed] [Google Scholar]
- 47.Srinivasan A., Srinivasan S., Sunthankar S. Pre-hematopoietic stem cell transplant lung function and pulmonary complications in children. Ann Am Thor Soc. 2014;11:1576–1585. doi: 10.1513/AnnalsATS.201407-308OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaya Z., Weiner D.J., Yilmaz D. Lung function, pulmonary complications, and mortality after allogeneic blood and marrow transplantation in children. Biol Blood Marrow Transplant. 2009;15:817–826. doi: 10.1016/j.bbmt.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 49.Ginsberg J.P., Aplenc R., McDonough J. Pre-transplant lung function is predictive of survival following pediatric bone marrow transplantation. Pediatr Blood Cancer. 2010;54:454–460. doi: 10.1002/pbc.22337. [DOI] [PubMed] [Google Scholar]
- 50.Chien J.W., Maris M.B., Sandmaier B.M. Comparison of lung function after myeloablative and 2 Gy of total body irradiation-based regimens for hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005;11:288–296. doi: 10.1016/j.bbmt.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 51.Singh A.K., Karimpour S.E., Savani B.N. Pretransplant pulmonary function tests predict risk of mortality following fractionated total body irradiation and allogeneic peripheral blood stem cell transplant. Int J Radiat Oncol Biol Phys. 2006;66:520–527. doi: 10.1016/j.ijrobp.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 52.Yanik G., Hellerstedt B., Custer J. Etanercept (Enbrel) administration for idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2002;8:395–400. doi: 10.1053/bbmt.2002.v8.pm12171486. [DOI] [PubMed] [Google Scholar]
- 53.Yanik G.A., Ho V.T., Levine J.E. The impact of soluble tumor necrosis factor receptor etanercept on the treatment of idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Blood. 2008;112:3073–3081. doi: 10.1182/blood-2008-03-143412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tizon R., Frey N., Heitjan D.F. High-dose corticosteroids with or without etanercept for the treatment of idiopathic pneumonia syndrome after allo-SCT. Bone Marrow Transplant. 2012;47:1332–1337. doi: 10.1038/bmt.2011.260. [DOI] [PubMed] [Google Scholar]
- 55.Yanik G.A., Horowitz M.M., Weisdorf D.J. Randomized, double-blind, placebo- controlled trial of soluble tumor necrosis factor receptor: Enbrel (Etanercept) for the treatment of idiopathic pneumonia syndrome after allogeneic stem cell transplantation: Blood and Marrow Transplant Clinical Trials Network Protocol. Biol Blood Marrow Transplant. 2014;20:858–864. doi: 10.1016/j.bbmt.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yanik G.A., Grupp S.A., Pulsipher M.A. TNF-receptor inhibitor therapy for the treatment of children with idiopathic pneumonia syndrome. A joint Pediatric Blood and Marrow Transplant Consortium and Children's Oncology Group Study (ASCT0521) Biol Blood Marrow Transplant. 2015;21:67–73. doi: 10.1016/j.bbmt.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rathi N.K., Tanner A.R., Dinh A. Low-, medium-, and high dose steroids with or without aminocaproic acid in adult hematopoietic SCT patients with diffuse alveolar hemorrhage. Bone Marrow Transplant. 2015;50:420–426. doi: 10.1038/bmt.2014.287. [DOI] [PubMed] [Google Scholar]
- 58.Wanko S.O., Broadwater G., Folz R.J., Chao N.J. Diffuse alveolar hemorrhage: retrospective review of clinical outcome in allogeneic transplant recipients treated with aminocaproic acid. Biol Blood Marrow Transplant. 2006;12:949–953. doi: 10.1016/j.bbmt.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 59.Elinoff J.M., Bagci U., Moriyama B. Recombinant human factor VIIa for aleveolar hemorrhage following allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:969–978. doi: 10.1016/j.bbmt.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bergeron A., Chevret S., Chagnon K. Budesonide/formoterol for bronchiolitis obliterans after hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2015;191:1242–1249. doi: 10.1164/rccm.201410-1818OC. [DOI] [PubMed] [Google Scholar]
- 61.Norman B.C., Jacobsohn D.A., Williams K.M. Fluticasone, azithromycin and montelukast therapy in reducing corticosteroid exposure in bronchiolitis obliterans syndrome after allogeneic hematopoietic SCT: a case series of eight patients. Bone Marrow Transplant. 2011;46:1369–1373. doi: 10.1038/bmt.2010.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yanik G.A., Mineishi S., Levine J.E. Soluble tumor necrosis factor receptor: Enbrel (etanercept) for subacute pulmonary dysfunction following allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:1044–1054. doi: 10.1016/j.bbmt.2011.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Iacono A.T., Johnson B.A., Grgurich W.F. A randomized trial of inhaled cyclosporine in lung-transplant recipients. N Engl J Med. 2006;354:141–150. doi: 10.1056/NEJMoa043204. [DOI] [PubMed] [Google Scholar]
- 64.Corris P.A., Ryan V.A., Small T. A randomized controlled trial of azithromycin therapy in bronchiolitis obliterans syndrome (BOS) post lung transplantation. Thorax. 2015;70:442–450. doi: 10.1136/thoraxjnl-2014-205998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Palmer J., Williams K., Inamoto Y. Pulmonary symptoms measured by the National Institutes of Health Lung Score predict overall survival, nonrelapse mortality, and patient-reported outcomes in chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2014;20:337–344. doi: 10.1016/j.bbmt.2013.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miller M.R., Quanjer P.H., Swanney M.P. Interpreting lung function data using 80% predicted and fixed thresholds misclassifies more than 20% of patients. Chest. 2011;139:52–59. doi: 10.1378/chest.10-0189. [DOI] [PubMed] [Google Scholar]
- 67.Galban C.J., Han M.K., Boes J.L. Computed tomography-based biomarker provides unique signature for diagnosis of COPD phenotypes and disease progression. Nat Med. 2012;18:1711–1715. doi: 10.1038/nm.2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tajima S., Oshikawa K., Tominaga S., Sugiyama Y. The increase in serum soluble ST2 protein upon acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2003;124:1206–1214. doi: 10.1378/chest.124.4.1206. [DOI] [PubMed] [Google Scholar]
- 69.Radhakrishnan S.V., Palaniyandi S., Mueller G. Preventive azithromycin treatment reduces noninfectious lung injury and acute graft-versus-host disease in a murine model of allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2015;21:30–38. doi: 10.1016/j.bbmt.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 70.Walkey A.J., Wiener R.S. Macrolide antibiotics and survival in patients with acute lung injury. Chest. 2012;141:1153–1159. doi: 10.1378/chest.11-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wilson J.G., Liu K.D., Zhuo H. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3:24–32. doi: 10.1016/S2213-2600(14)70291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hayes M., Masterson C., Devaney J. Therapeutic efficacy of human mesenchymal stromal cells in the repair of established ventilator-induced lung injury in the rat. Anesthesiology. 2015;122:363–373. doi: 10.1097/ALN.0000000000000545. [DOI] [PubMed] [Google Scholar]
- 73.Kennedy G.A., Varelias A., Vuckovic S. Addition of interleukin-6 inhibition with tocilizumab to standard graft-versus-host disease prophylaxis after allogeneic stem-cell transplantation: a phase 1/2 trial. Lancet Oncol. 2014;15:1451–1459. doi: 10.1016/S1470-2045(14)71017-4. [DOI] [PubMed] [Google Scholar]
- 74.Dubovsky J.A., Flynn R., Du J. Ibrutinib treatment ameliorates murine chronic graft-versus-host disease. J Clin Invest. 2014;124:4867–4876. doi: 10.1172/JCI75328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alexander K.A., Flynn R., Lineburg K.E. CSF-1 dependent donor-derived macrophages mediate chronic graft-versus-host disease. J Clin Invest. 2014;124:4266–4280. doi: 10.1172/JCI75935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McArthur J., Petterson G., Jouvet P. The care of critically ill children after hematopoietic SCT: a North American survey. Bone Marrow Transplant. 2011;46:227–231. doi: 10.1038/bmt.2010.89. [DOI] [PubMed] [Google Scholar]
- 77.Pancera C.F., Hayashi M., Fregnani J.H. Noninvasive ventilation in immunocompromised pediatric patients: eight years of experience in a pediatric oncology intensive care unit. J Pediatr Hematol Oncol. 2008;30:533–538. doi: 10.1097/MPH.0b013e3181754198. [DOI] [PubMed] [Google Scholar]
- 78.Wemke M., Schiemanck S., Hoffken G. Respiratory failure in patients undergoing allogeneic hematopoietic SCT-a randomized trial on early non-invasive ventilation based on standard care hematology wards. Bone Marrow Transplant. 2012;47:574–580. doi: 10.1038/bmt.2011.160. [DOI] [PubMed] [Google Scholar]
- 79.Chima R.S., Daniels R.C., Kim M.O. Improved outcomes for stem cell transplant recipients requiring pediatric intensive care. Pediatr Crit Care Med. 2012;13:e336–e342. doi: 10.1097/PCC.0b013e318253c945. [DOI] [PubMed] [Google Scholar]
- 80.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 81.Slutsky A.S., Drazen J.M. Ventilation with small tidal volumes. N Engl J Med. 2002;347:630–631. doi: 10.1056/NEJMp020082. [DOI] [PubMed] [Google Scholar]
- 82.Sud S., Sud M., Friedrich J.O. High frequency oscillation in patients with acute lung injury and acute respiratory distress syndrome (ARDS): systematic review and meta-analysis. BMJ. 2010;340:c2327. doi: 10.1136/bmj.c2327. [DOI] [PubMed] [Google Scholar]
- 83.Ferguson N.D., Cook D.J., Guyatt G.H. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368:795–805. doi: 10.1056/NEJMoa1215554. [DOI] [PubMed] [Google Scholar]
- 84.Rizkalla N.A., Dominick C.L., Fitzgerald J.C. High-frequency percussive ventilation improves oxygenation and ventilation in pediatric patients with acute respiratory failure. J Crit Care. 2014;29:314.e1–314.e7. doi: 10.1016/j.jcrc.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 85.Guérin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 86.Taccone P., Pesenti A., Latini R. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302:1977–1984. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 87.National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Wiedemann H.P., Wheeler A.P. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 88.Sutherland S.M., Zappitelli M., Alexander S.R. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55:316–325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 89.Michael M., Kuehnle I., Goldstein S.L. Fluid overload and acute renal failure in pediatric stem cell transplant patients. Pediatr Nephrol. 2004;19:91–95. doi: 10.1007/s00467-003-1313-z. [DOI] [PubMed] [Google Scholar]
- 90.Elbahlawan L., West N.K., Avent Y. Impact of continuous renal replacement therapy on oxygenation in children with acute lung injury after allogeneic hematopoietic stem cell transplantation. Pediatr Blood Cancer. 2010;55:540–545. doi: 10.1002/pbc.22561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Flores F.X., Brophy P.D., Symons J.M. Continuous renal replacement therapy (CRRT) after stem cell transplantation. A report from the prospective pediatric CRRT Registry group. Pediatr Nephrol. 2008;23:625–630. doi: 10.1007/s00467-007-0672-2. [DOI] [PubMed] [Google Scholar]
- 92.Meduri G.U., Marik P.E., Chrousos G.P. Steroid treatment in ARDS: a critical appraisal of the ARDS network trial and the recent literature. Intensive Care Med. 2008;34:61–69. doi: 10.1007/s00134-007-0933-3. [DOI] [PubMed] [Google Scholar]
- 93.Willson D.F., Thomas N.J., Tamburro R. Pediatric Acute Lung and Sepsis Network. Pediatric calfactant in acute respiratory distress syndrome trial. Pediatr Crit Care Med. 2013;14:657–665. doi: 10.1097/PCC.0b013e3182917b68. [DOI] [PubMed] [Google Scholar]
- 94.Tamburro R.F., Thomas N.J., Pon S. for the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Post hoc analysis of calfactant use in immunocompromised children with acute lung injury: impact and feasibility of further clinical trials. Pediatr Crit Care Med. 2008;9:459–464. doi: 10.1097/PCC.0b013e3181849bec. [DOI] [PubMed] [Google Scholar]
- 95.Zabrocki L.A., Brogan T.V., Statler K.D. Extracorporeal membrane oxygenation for pediatric respiratory failure: Survival and predictors of mortality. Crit Care Med. 2011;39:364–370. doi: 10.1097/CCM.0b013e3181fb7b35. [DOI] [PubMed] [Google Scholar]
- 96.Gow K.W., Wulkan M.L., Heiss K.F. Extracorporeal membrane oxygenation for support of children after hematopoietic stem cell transplantation: the Extracorporeal Life Support Organization experience. J Pediatr Surg. 2006;41:662–667. doi: 10.1016/j.jpedsurg.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 97.Keenan H.T., Bratton S.L., Martin L.D. Outcome of children who require mechanical ventilatory support after bone marrow transplantation. Crit Care Med. 2000;28:830–835. doi: 10.1097/00003246-200003000-00036. [DOI] [PubMed] [Google Scholar]
- 98.Hagen S.A., Craig D.M., Martin P.L. Mechanically ventilated pediatric stem cell transplant recipients: effect of cord blood transplant and organ dysfunction on outcome. Pediatr Crit Care Med. 2003;4:206–213. doi: 10.1097/01.PCC.0000043293.83440.79. [DOI] [PubMed] [Google Scholar]
- 99.Lamas A., Otheo E., Ros P. Prognosis of child recipients of hematopoietic Stem cell transplantation requiring intensive care. Intensive Care Med. 2003;29:91–96. doi: 10.1007/s00134-002-1549-2. [DOI] [PubMed] [Google Scholar]
- 100.Diaz M.A., Vicent M.G., Prudencio M. Predicting factors for admission to an Intensive care unit and clinical outcome in pediatric patients receiving hematopoietic stem cell transplantation. Haematologica. 2002;87:292–298. [PubMed] [Google Scholar]
- 101.Jacobe S.J., Hassan A., Veys P. Outcome of children requiring admission to an intensive care unit after bone marrow transplantation. Crit Care Med. 2003;31:1299–1305. doi: 10.1097/01.CCM.0000060011.88230.C8. [DOI] [PubMed] [Google Scholar]
- 102.Tomaske M., Bosk A., Eyrich M. Risks of mortality in children admitted to the paediatric intensive care unit after haematopoietic stem cell transplantation. Br J Haematol. 2003;121:886–891. doi: 10.1046/j.1365-2141.2003.04390.x. [DOI] [PubMed] [Google Scholar]
- 103.Kache S., Weiss I.K., Moore T.B. Changing outcomes for children requiring intensive care following hematopoietic stem cell transplantation. Pediatr Transplant. 2006;10:299–303. doi: 10.1111/j.1399-3046.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- 104.van Gestel J.P., Bollen C.W., van der Tweel I. Intensive care unit mortality trends in children after hematopoietic stem cell transplantation: a meta-regression analysis. Crit Care Med. 2008;36:2898–2904. doi: 10.1097/CCM.0b013e318186a34a. [DOI] [PubMed] [Google Scholar]
- 105.Tamburro R.F., Barfield R.C., Shaffer M.L. Changes in outcomes (1996-2004) for pediatric oncology and hematopoietic stem cell transplant patients requiring invasive mechanical ventilation. Pediatr Crit Care Med. 2008;9:270–277. doi: 10.1097/PCC.0b013e31816c7260. [DOI] [PubMed] [Google Scholar]
- 106.Aspesberro F., Guthrie K.A., Woolfrey A.E. Outcome of pediatric hematopoietic stem cell transplant recipients requiring mechanical ventilation. J. Intensive Care Med. 2014;29:31–37. doi: 10.1177/0885066612457343. [DOI] [PubMed] [Google Scholar]
- 107.Rowan C.M., Hege K.M., Speicher R.H. Oxygenation index predicts mortality in pediatric stem cell transplant recipients requiring mechanical ventilation. Pediatr Transplant. 2012;16:645–650. doi: 10.1111/j.1399-3046.2012.01745.x. [DOI] [PubMed] [Google Scholar]
- 108.van Gestel J.P., Bierings M.B., Dauger S. Outcome of invasive mechanical ventilation after pediatric allogeneic hematopoietic SCT: results from a prospective, multicenter registry. Bone Marrow Transplant. 2014;49:1287–1292. doi: 10.1038/bmt.2014.147. [DOI] [PubMed] [Google Scholar]
- 109.ATS committee on proficiency standards for clinical pulmonary function laboratories ATS Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 110.Nathan S.D., Shlobin O.A., Ahmad S. Pulmonary hypertension in patients with bronchiolitis obliterans syndrome listed for retransplantation. Am J Transplant. 2008;8:1506–1511. doi: 10.1111/j.1600-6143.2008.02277.x. [DOI] [PubMed] [Google Scholar]
- 111.Srinivasan A., Wang C., Srivastava D.K. Timeline, epidemiology, and risk factors for bacterial, fungal, and viral infections in children and adolescents after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19:94–101. doi: 10.1016/j.bbmt.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jain N.A., Pophali P.A., Klotz J.K. Repair of impaired pulmonary function is possible in very-long-term allogeneic stem cell transplantation survivors. Biol Blood Marrow Transplant. 2014;20:209–213. doi: 10.1016/j.bbmt.2013.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]