Abstract
In Saudi Arabia, only 9% of dialysis patients are on peritoneal dialysis (PD), and this has been the case for years. A number of centers around the world have sought to understand the underutilization of PD by asking nephrologists directly. In this study, we aimed to gather information that will answer the question “Why is PD underutilized in Saudi Arabia?” hoping that a roadmap may be developed to overcome the hurdles the study underscores, allowing for more patients to utilize this valuable modality.
Keywords: Peritoneal dialysis, barriers, utilization
In Saudi Arabia, the prevalence of end-stage renal failure treated by dialysis at the end of 2014 was around 513 cases/per million population with a total number of 15,782 patients (1). Of these, 14,366 patients were on hemodialysis (HD) and the remaining 1,416 were on peritoneal dialysis (PD) (1). In other words, only 9% of dialysis patients in Saudi Arabia are on PD and that percentage has not changed over the years. Several worldwide centers have tried to address the reasons behind the underutilization of PD by acquiring feedback directly from nephrologists (2,3).
This is a survey-based, cross-sectional study. The survey (available as supplemental online material) consisted of 18 questions, of which 17 were closed-ended and required the respondent to respond to a binary or ordinal scale, while the 18th question was open-ended, requiring the respondent to give his/her personal view about how to improve PD utilization in Saudi Arabia. The survey was pre-tested on a sample of 2 nephrologists, and modifications were applied prior to distribution. After obtaining approval from the institutional review board of King Abdullah International Medical Research Center (KAIMRC), the survey was electronically distributed using SurveyMonkey (SurveyMonkey, CA, USA) to all adult nephrology consultants registered in the most recently updated list of the Saudi Center for Organ Transplantation (SCOT). The survey was first sent to participants on May 26, 2015 and closed on July 31, 2015. While the study was open, non-respondents received reminders every 2 weeks. Data were analyzed using SPSS for Windows software version 21 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were generated. Significance of differences of non-parametric variables (percentages and proportions) was calculated using Pearson chi-squared test (p value of ≤ 0.05 is considered as significant).
Results
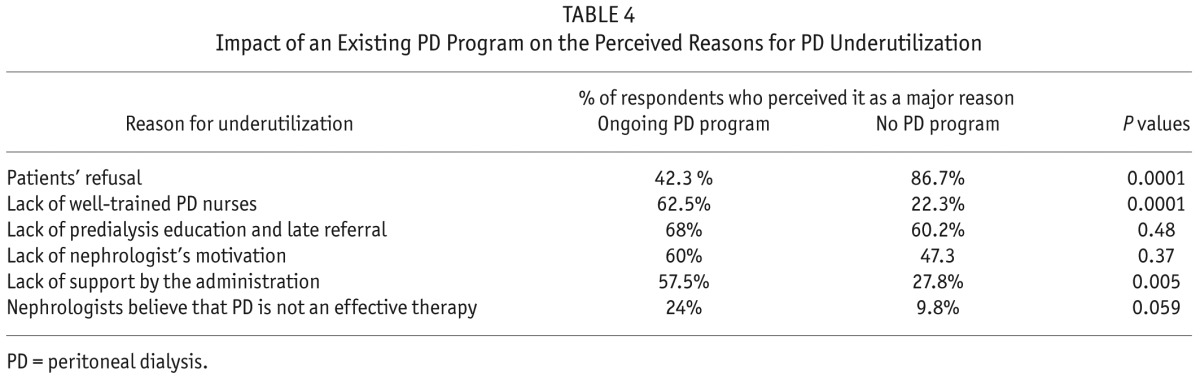
Two hundred and two physicians are registered as adult nephrology consultants in the SCOT list, 5 of whom were excluded: (1 being one of the authors, 2 retired, and 2 had left the country). Out of the 197 nephrologists who were eligible for the study and received the survey, 124 responded (63%), 7 declined (4%), and 66 did not respond (33%). The demographic data of respondents are summarized in Table 1. Most nephrologists were not satisfied with the current number of their PD patients and around 60% of them felt that 30% or more of their dialysis patients should be on PD. Eighty-eight percent of respondents believe that PD should be offered to patients as the first dialysis modality. Seventeen percent of participants reported the cessation of a previously existing PD program. Most of the participants (61%) had not attended any PD-related educational activity (e.g. lecture, course, or workshop) for more than a year and only 21% have attended 1 of these activities during the last 6 months. Figure 1 indicates participants' response to inquiries about the services available at their institutions to support their PD program. The top factors behind PD underutilization and patient refusal at participants' institutions as perceived by participants are summarized in Tables 2 and 3. When asked about the mode of dialysis nephrologists would opt for if dialysis were needed for themselves, 92 respondents (74%) chose PD. The 3 most common suggestions provided by respondents to improve utilization of PD in Saudi Arabia were: 1) a chronic kidney disease (CKD) clinic to allow proper predialysis patients' education, 2) early referral, and 3) increase nephrologists' motivation with continuous medical education (CME). We also looked into the possibility that some respondents' preferences may have affected the participants' reasoning of underutilization of PD at their institution. We found that neither sex, respondents' age, nor whether they work in a ministry of health (MOH) sector or another sector had an impact on their response. On the other hand, the existence of an ongoing PD program in their institution had an impact, as shown in Table 4.
TABLE 1.
Demographics of the (124) Participating Nephrologists
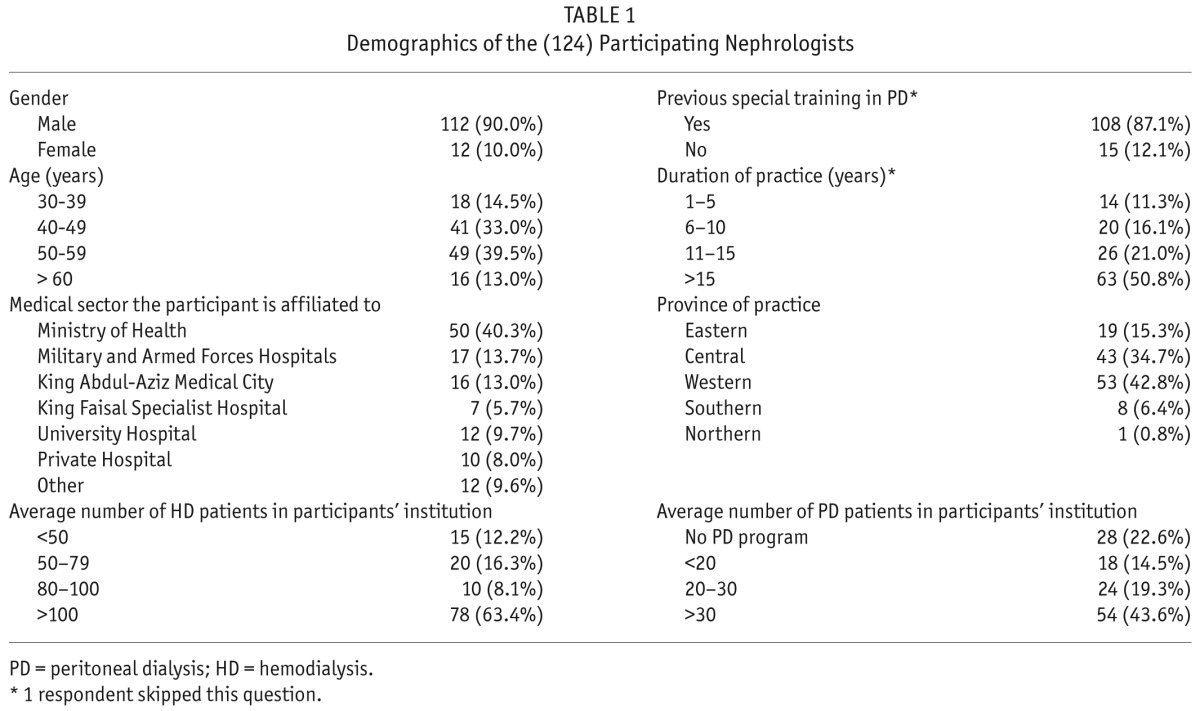
Figure 1 —
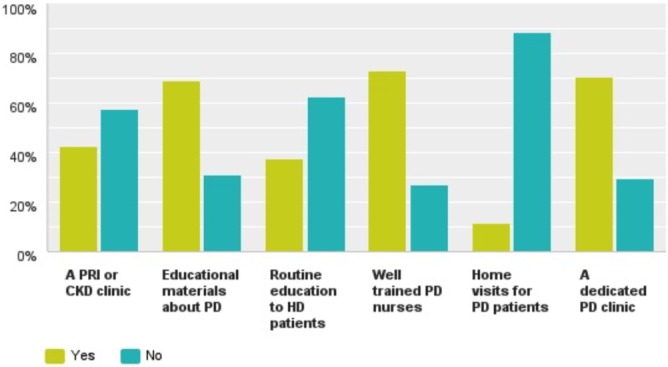
Responses to the question: As part of supporting the PD program, the following is/are currently available in your institution. PD = peritoneal dialysis; CKD = chronic kidney disease; PRI = progressive renal insufficiency; HD = hemodialysis.
TABLE 2.
Factors Leading to PD Underutilization According to Participants*
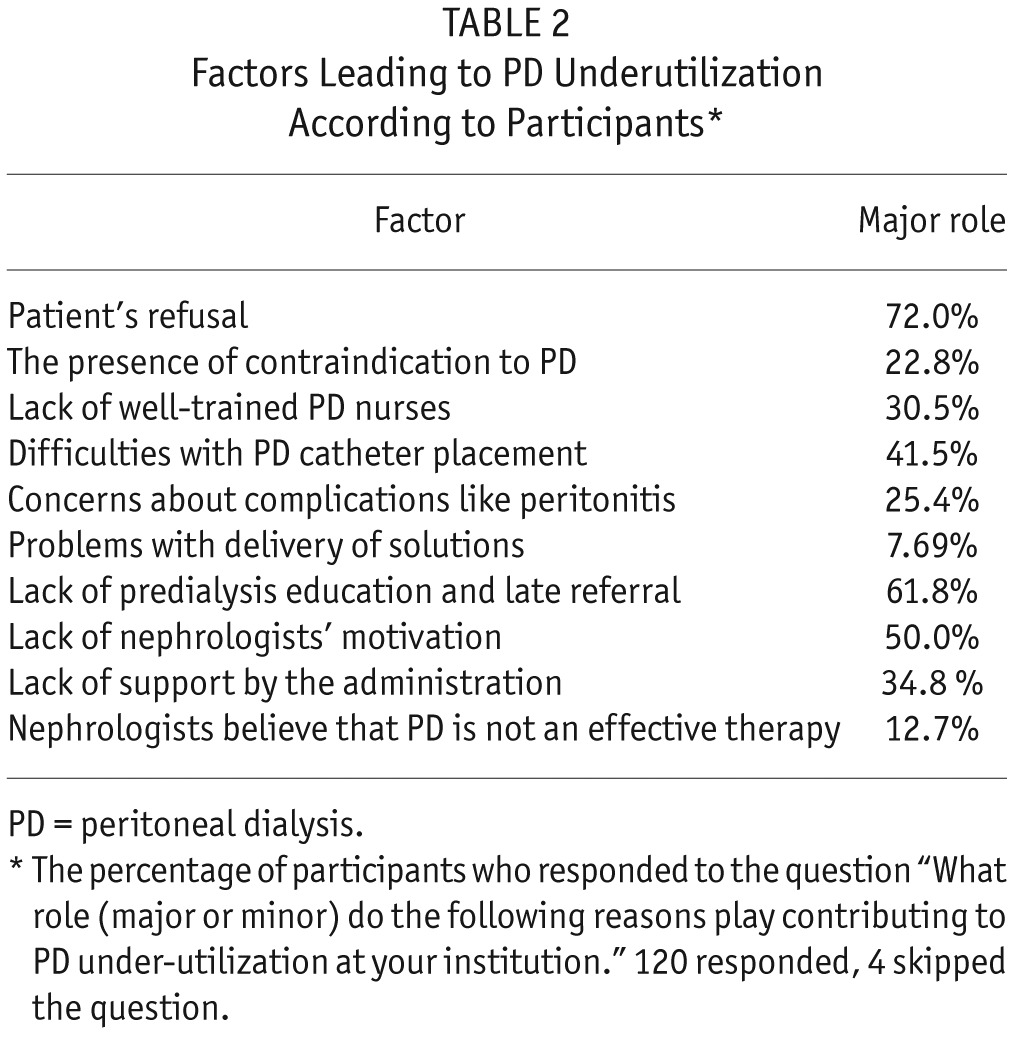
TABLE 3.
Factors Leading to patients' refusal of PD According to Participants*
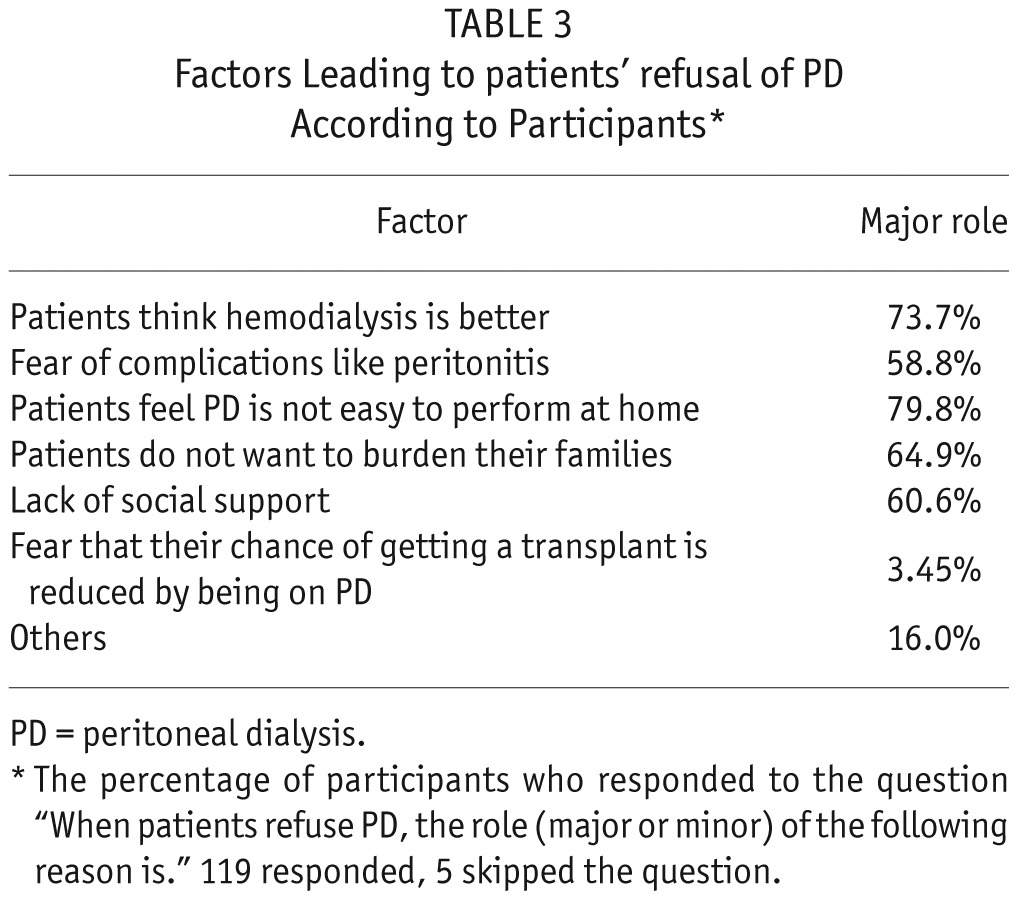
TABLE 4.
Impact of an Existing PD Program on the Perceived Reasons for PD Underutilization
Discussion
There has been clear evidence showing the positive impact of predialysis education on utilization of PD (4). The timing of the educational programs offered to patients in the course of their disease is crucial. Late referral, defined as less than 3 months from follow-up by a nephrologist before initiation of dialysis, with its resultant knowledge gap, will significantly lower the number of patients on PD (5). The fact that 88% of our nephrologists would offer PD as the first dialysis modality, and most of them would choose it if they were to undergo dialysis, indicates how strongly they believe in this modality. Despite the evident stance of nephrologists, patients' refusal of PD stands. This comes as no surprise because 60% of the nephrologists surveyed did not run a CKD clinic, where a multidisciplinary approach and counseling usually take place. In other words, the lack of efficient educational programs offered to patients in a timely manner is likely among the reasons behind patients' refusal of PD in Saudi Arabia. On the other hand, nephrologists who practice with an existing PD program at their institution were not as concerned about patients' refusal as those who had no existing PD program (Table 4). This may indicate the positive impact of the practice itself on nephrologists' educational skills, counseling, and their faith in this dialysis modality. Home-visit programs to PD patients provided by training centers has exhibited improved clinical outcomes including decreased technique failure, lower peritonitis rate, and a lower chance of hospitalization (6). Saudi Arabia and most Middle Eastern countries share distinct social cultures that may act as possible barriers to the home-visit program. This is probably why most PD programs in the kingdom abandoned home visits. Interestingly, some of these hospitals do run successful home-intravenous-antibiotics programs, which indicates the lack of awareness of the importance of PD home-visit programs by hospital administration, patients, and nephrologists. The fact that 87% of participants dedicated part of their training to PD, and yet their skills and knowledge are neither being utilized nor being maintained by CME, means that we are not only underutilizing a great therapeutic modality but also wasting a scientific wealth we should be maintaining and expanding.
In conclusion, during this era of expanding outsourced HD centers in the kingdom where more HD seats will be easily available to patients, it is crucial to address the abovementioned issues to improve PD utilization. We recommend that all nephrology programs increase their PD educational activities to both nephrologists and patients. Patients' education is probably best achieved through multidisciplinary predialysis CKD clinics. Support to existing PD patients and their caregivers should include easy access to a healthcare team, home-visit programs, and well-trained PD nurses. This is the first study to address the issue of underutilization of PD in a Middle East country. It is limited by the fact that nephrologists' views may not accurately reflect patients' views.
Disclosures
The authors have no financial conflicts of interest to declare.
Footnotes
Supplemental material available at www.pdiconnect.com
REFERENCES
- 1. Souqiyyeh MZ, Al-Attar MB, Zakaria H, Shaheen FA. Dialysis in the Kingdom of Saudi Arabia. Saudi J Kidney Dis Transplant 2015; 26(4):839–48. [PubMed] [Google Scholar]
- 2. Troidle L, Kliger A, Finkelstein F. Barriers to utilization of chronic peritoneal dialysis in network #1. New England Perit Dial Int 2006; 26(4):452–7. [PubMed] [Google Scholar]
- 3. Jung B, Blake PG, Mehta RL, Mendelssohn DC. Attitude of Canadian nephrologists toward dialysis modality selection. Perit Dial Int 1999; 19(3):263–8. [PubMed] [Google Scholar]
- 4. Ribitsch W, Haditsch B, Otto R, Schilcher G, Quehenberger F, Roob JM, et al. Effects of a pre-dialysis patient education program on the relative frequencies of dialysis modalities. Perit Dial Int 2013; 33(4):367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baer G, Lameire N, Van Biesen W. Late referral of patients with end-stage renal disease: an in-depth review and suggestions for further actions. NDT Plus 2010; 3(1):17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Martino F, Adıbelli Z, Mason G, Nayak A, Ariyanon W, Rettore E, et al. Home visit program improves technique survival in peritoneal dialysis. Blood Purif 2014; 37(4):286–90. [DOI] [PubMed] [Google Scholar]


