Abstract
Objective
For people living with HIV, treatment adherence self-efficacy is an important predictor of treatment adherence and therefore of clinical outcomes. Using experience sampling method (ESM), this study aimed to examine: (1) the within-person association between moment-to-moment changes in social support and HIV treatment self-efficacy; (2) the moderators of this within-person association, (3) the concordance between questionnaire and ESM measurement of treatment self-efficacy; and (4) the utility of each approach (ESM and questionnaire) in predicting adherence to medication, adherence to clinic visits, CD4 counts, and viral load.
Methods
109 men living with HIV responded to the same set of ESM questions 3 times a day for 7 days via a smart phone given to them for the study. They also completed cross-sectional questionnaires and their clinic data was extracted from medical records in order to examine predictors and consequences of state and trait treatment self-efficacy.
Results
In within-person hierarchical linear modeling (HLM) analyses, receipt of recent social support predicted higher current ESM treatment self-efficacy. This association was stronger for individuals reporting higher avoidance coping with HIV. The correlation between ESM and questionnaire measures of treatment self-efficacy was r = .37. ESM measure of average treatment self-efficacy predicted medication adherence, visit adherence, CD4 counts, and viral load, while questionnaire-based self-efficacy did not predict these outcomes.
Conclusion
Interventions aimed at improving treatment adherence may target social support processes, which may improve treatment self-efficacy and adherence.
Keywords: HIV, self-efficacy, adherence, social support, attachment, experience sampling, coping
Introduction
Treatment adherence self-efficacy is an important construct for understanding adherence to treatment recommendations in people living with HIV (PLWH). This construct, adapted from the concept of self-efficacy in other domains (Bandura, 1989), is defined as having confidence in one’s ability to adhere to a treatment regimen even in the presence of obstacles (e.g., side effects, treatment interferes with daily activities, etc.). The relationship between self-efficacy and better health outcomes has been reported in several other chronic diseases (e.g., diabetes (Gerber et al., 2005) and hypertension (Ogedegbe, Mancuso, Allegrante, & Charlson, 2003)). There is evidence that HIV treatment self-efficacy is also associated with better HIV outcomes (Ammassari et al., 2002; Johnson et al., 2007). This construct has significant public health implications, given that low adherence to antiretroviral therapy (ART) is linked to poorer disease outcomes for PLWH (e.g., higher viral loads), which in turn may result in the development of resistant strains of HIV (Bangsberg et al., 2006) and increased risk of HIV transmission to others (Quinn et al., 2000). Thus, research in this area is important, specifically research to: 1) determine psychosocial and interpersonal predictors of HIV treatment self-efficacy that may inform development of intervention strategies, and 2) determine the most accurate methods to measure this construct.
Predictors of HIV Treatment Self-Efficacy
There is a small body of literature on predictors of HIV treatment self-efficacy. Lower depression, greater problem solving skills, and higher general coping self-efficacy are associated with higher HIV treatment self-efficacy (Godin, Côté, Naccache, Lambert, & Trottier, 2005; Johnson et al., 2007). Self-efficacy is an intrapersonal resource. However, theory and research suggests that interpersonal processes such as social support are important to the development of self-efficacy (Bandura, 1989; Godin et al., 2005; Reitz, Motti-Stefanidi, & Asendorpf, 2015). According to attachment theory, mechanisms underlying the association between social support and self-efficacy include two key social support functions. First, at times of adversity, support from attachment figures provides a safe haven and a source of strength, which can have positive downstream effects on self-perceptions, appraisals of the situation, and ultimately health behaviors. Second, in the absence of adversity, social support may act as a secure base: a relational catalyst to increase positive emotions such as self-confidence and empowerment, resulting in downstream positive effects on outcomes (Bowlby, 2012; Feeney & Collins, 2015). The sociometer hypothesis also posits that a feeling of social belonging is an important predictor of self-esteem (Leary, Tambor, & Terdal, 1995).
Certain individual difference constructs (personality traits and psychosocial factors) may moderate the effects of social support on self-efficacy, such that this process is stronger for some people compared to others (Feeney & Collins, 2015; Fitzsimons & Finkel, 2010). One potentially important construct is coping (Vitaliano, Russo, Carr, Maiuro, & Becker, 1985). Individuals who use maladaptive coping strategies such as avoidance (disengaging from a stressor instead of directly addressing it), blaming self (focusing on self-blaming instead of actively trying to address the stressor), and who experience feelings of helplessness in the face of dealing with HIV may benefit more from social support, because they are at higher risk for poorer outcomes compared to individuals who do not use maladaptive coping strategies or who do not experience feelings of helplessness, and thus stand to gain more from social support. Indeed, studies suggest that individuals low in personal control (Dagan et al., 2011) benefit more from social support compared to individuals high in personal control. This may be due to those with high levels of personal control having ceiling functioning on outcomes, with not much room for improvement. Insecure attachment styles may also moderate the association between social support and HIV treatment self-efficacy. Modern measures of attachment styles assess two dimensions of insecure attachment: attachment-related avoidance (avoidance of intimacy and closeness) and attachment-related anxiety (worry about relationships and over-reliance on relationship partners) (Brennan, Clark, & Shaver, 1998)). Social support may interact with attachment styles to influence health outcomes (Medard & Kellett, 2014). High levels of social support may be able to overcome defensiveness associated with attachment-related avoidance by providing evidence of the availability and support of social relationships, whereas those who are low in attachment-related avoidance may experience better outcomes regardless of the level of social support they receive (Girme, Overall, Simpson, & Fletcher, 2015). However, it is also possible that individuals high in avoidance may not use social support effectively (Brennan et al., 1998). Individuals high in attachment-related anxiety may benefit more from social support because of their overreliance on partners. However, the opposite prediction can also be made, since they are usually not satisfied with the support they receive and communicate their low efficacy in dealing with stressors in order to justify their need for more support from partners (Brennan et al., 1998).
Lastly, stigma dimensions such as perceived stigma in the community (a person’s perceptions of the extent of stigmatizing attitudes against PLWH in the community) and internalized stigma (the degree to which PLWH accept these stigmatizing beliefs and feel inferior as a result) may also moderate the association between social support and self efficacy, as strong social networks may buffer the effects of stigma on outcomes (Bogart et al., 2015). Both types of stigma are associated with low self-efficacy (DiIorio et al., 2009). While PLWH with low levels of stigma may have high self-efficacy regardless of social support, receiving social support may be particularly beneficial for PLWH with high levels of stigma. Social support increases feelings of belonging (Baumeister & Leary, 1995), and may compensate for the negative effects of stigma on feelings of belonging.
Measurement of HIV Treatment Self-Efficacy
Currently, questionnaire measurement is the most common approach for measuring HIV treatment self-efficacy and has yielded valuable information in previous research (Ammassari et al., 2002; Johnson et al., 2007). However, questionnaire measures require respondents to take a mental average of their experiences and emotional tendencies over time and rely on respondents’ ability and willingness to report how they generally perceive, feel, and think across situations. To the best of our knowledge, the current study is the first in the area of HIV treatment self-efficacy to utilize the experience sampling method (ESM)—a method widely used in psychological and medical research (Affleck, Zautra, Tennen, & Armeli, 1999; Nezlek, 2007). In ESM, participants are asked multiple times a day during daily life about their experiences at the time (or close to the time) of these experiences. Thus, ESM attempts to avoid inaccuracies and biases associated with global judgments. ESM has an additional advantage: It allows within-person analyses to examine relevant processes that co-occur for a given person in real time. One can, for example, examine whether a participant’s perceived treatment self-efficacy is higher at times when that participant has just received support from others related to HIV. Previous research has not examined such within-person associations, which can have important theoretical and practical implications not revealed by studies that examine between-person effects (Affleck et al., 1999; Nezlek, 2007).
The Current Study
The current study utilizes both ESM and questionnaire-measures of treatment self-efficacy and examines a broad spectrum of predictors. The specific aims are to examine: 1) the within-person association between moment-to-moment changes in social support and HIV treatment self-efficacy; 2) moderators of this association, 3) the concordance between ESM and questionnaire measurement of treatment self-efficacy; and 4) the utility of each approach (ESM and questionnaire) in predicting adherence to ART, adherence to clinic visits, CD4 counts, and viral load.
Methods
Participants and Procedures
Men living with HIV (N = 109) who are on ART and not current substance users were recruited from an HIV clinic at a research university in Birmingham, AL as part of a larger study on psychosocial aspects of living with HIV. Each participant was given a smart phone and responded to a set of ESM questions three times throughout the day for seven days using the smart phone. Participants also completed questionnaires on psychosocial and interpersonal traits and other individual difference constructs during their in-person study visits. This protocol was approved by the Institutional Review Board of the university and all procedures were carried out with the adequate understanding and written consent of the participants.
Experience Sampling Method (ESM)
Participants received alerts to respond to the same ESM questions three times a day for seven consecutive days. ESM times were preset by the researchers spread out throughout the day (between 10 am and 8 pm, with at least 2 hours between sampling occasions). However, participants were told that ESM times were random so that they could not anticipate when the next prompt would be (which could potentially affect their responses). ESM questions included an item on HIV treatment self-efficacy (“Right now, how confident do you feel that you can stick to your treatment plan for your immune status?”) We used the term “immune status” instead of HIV for confidentiality purposes and told participants about this wording choice when we gave them their smart phones and explained the procedures. Response choices ranged from “1-not confident at all” to “5-extremely confident”. Another ESM item concerned recent acts of HIV-related social support (“Since last report, how much did someone give you support related to your immune status?”). Response choices ranged from “1-I received no support” at all to “5- I received a huge amount of support”.
HIV Visit Adherence, Viral Load, CD4, and hospital visits
Data on HIV clinic appointments in the past 24 months were extracted from clinic records to calculate adherence to HIV visits as the number of attended visits divided by the number of total scheduled visits (total scheduled visits = completed visits + no shows) that were not cancelled in advance (Mugavero, Davila, Nevin, & Giordano, 2010). Hospital visits in the last 12 months, most recent viral load and most recent CD4 data were extracted from clinic records. Most participants (n = 98) had undetectable viral load (<200 c/mL, which is the threshold for viral suppression according to current guidelines (Panel on Antiretroviral Guidelines for Adults and Adolescents, 2015)). Most participants (n = 99) had CD4 counts over 200. A CD4 count lower than 200 is the long-standing standard to define AIDS clinically, as well as a good predictor of virologic failure and opportunistic infections (Kaplan et al., 2009; Panel on Antiretroviral Guidelines for Adults and Adolescents, 2015)). Only 22 participants had hospital visits in the last 12 months.
Questionnaire Measures
ART adherence
Participants reported their ability to take all of their HIV medications using a 6-point rating scale ranging from “1-very poor” to “6-excellent”. Previous research suggests that this single item is a valid measure of ART adherence (Feldman et al., 2013; Lu et al., 2008). The scores on this measure were not normally distributed, with the majority of participants (n = 73)1 reporting excellent adherence. Therefore, this measure was dichotomized: Excellent adherence versus less than excellent adherence.
HIV treatment self-efficacy
The HIV Treatment Adherence Self-Efficacy Scale (Johnson et al., 2007) consists of 12 items with the stem: “How confident do you feel that you can do these things related to HIV?” A sample item is “Stick to your treatment schedule even when your daily routine is disrupted.” The response scale ranged from “1-cannot do it at all” to “10-certain can do it”. The mean of 12 items was used to reflect HIV treatment self-efficacy, with higher scores indicating higher self-efficacy. In the current data, Cronbach’s α was .93.
Coping with HIV
We used two subscales from the revised Ways of Coping List (Vitaliano et al., 1985). The avoidance subscale includes 10 items (e.g., “I go on as if nothing had happened”) and the blaming self subscale includes 3 items (e.g., “I blame myself”). Participants were asked to use a scale from “1-I don’t do this at all” to “5-I do this a lot” to rate how much they use each coping strategy in response to events that remind them of having HIV. Cronbach’s α was .77 for avoidance coping and .82 for blame coping.
Cognitions of helplessness due to HIV
We adapted the Illness Cognition Questionnaire for Chronic Diseases (Evers et al., 2001) to HIV as was done by Earnshaw et al. (Earnshaw, Smith, Chaudoir, Amico, & Copenhaver, 2013). This 18-item scale includes six items assessing helplessness (e.g., “My HIV controls my life”). Participants rated their agreement with the items using a 4-point scale, with higher scores reflecting greater helplessness. Cronbach’s α for helplessness was .81 in the current data.
Attachment styles
We used a shorter 18-item version of the most widely used attachment style measure: Experiences in Close relationships (ECR, Brennan et al., 1998). ECR assesses two dimensions of insecure attachment: anxiety (worry about relationships and over-reliance on partners) and avoidance (over-independence and avoidance of intimacy). A sample item of the anxiety scale is “I worry about being abandoned,” and a sample item of the avoidance scale is “I am nervous when partners get too close to me.” Participants rated each item on a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). In the present data, anxiety (Cronbach’s α = .88) and avoidance scales (Cronbach’s α = .90) showed good internal consistency. Attachment-related anxiety and attachment-related avoidance were correlated (r = .61).
Internalized HIV stigma and perceived HIV stigma in the community
Participants responded to a multi-dimensional HIV stigma scale developed by Berger et al. (2001) and revised by Bunn et al. (2007). This scale measures multiple dimensions of stigma associated with HIV. We focused on the 6-item subscale of concern with public attitudes (i.e., perceived stigma in the community; e.g., “Most people believe a person who has HIV/AIDS is dirty”) and the 7-item subscale of negative self-image (i.e., internalized stigma; e.g., “I feel guilty because I have HIV”). Participants rated each item from 1-strongly agree to 4-strongly disagree. The mean of the items in each scale was used to assess each type of stigma dimension, with scores reversed so that higher scores reflect higher stigma. These subscales showed good internal consistency in the present study (Cronbach’s α = .87 and Cronbach’s α = .88, respectively for concern with public attitudes and negative self-image subscales).
Appraisal of general social support
We used the 4-item subscale of appraisal of social support in the Interpersonal Support Evaluation List-Short Form (Payne et al., 2012). This subscale assesses perceived availability of supportive others to discuss personal issues. A sample item is “When I need suggestions on how to deal with a personal problem, I know someone I can turn to.” Participants rated each item to indicate how true it is for them using a 4-point rating scale (1-definitely false to 4-definitely true). Cronbach’s α was .77 in the current data.
Statistical Analyses
All variables (except for dichotomized variables) were treated as interval/continuous variables in analyses. Multi-level analyses were conducted using Hierarchical Linear Modeling (HLM) version 6.08 (Raudenbush, Bryk, & Congdon, 2004). All other analyses were conducted using SPSS (version 20). All HLM analyses included random effects for the intercepts as well as all slopes, all error terms were assumed to be normally distributed, Level 2 error terms were allowed to be correlated, and it was assumed that residuals for successive sampling occasions were independent of each other. Between-person Level 2 predictors were standardized before entering into analyses to aid interpretation of results. Similarly, within-person predictors were also standardized using pooled within-person standard deviations.
To examine aim 1 (within-person association between recent social support and state self-efficacy), we conducted the following HLM analysis. (Level 1 predictor was person-mean centered; Level 2 predictors were grand-mean centered).
| (1) |
| (2) |
| (3) |
At Level 1 (the within-person level), ESM-treatment self-efficacyti is treatment self-efficacy for participant i at time t. β0i is the Level 1 intercept reflecting the average level of state treatment self-efficacy for each participant across all sampling occasions. β1i is the slope of the within-person association between social support and treatment self-efficacy for each participant across all sampling occasions. The Level 2 equations (the between-person level) test the predictors of β0i and β1i. γ10 reflects the magnitude of the average within-person association between ESM-support and ESM-treatment self-efficacy (controlling for the covariates).
In order to examine between-person associations between social support and self-efficacy, we saved the intercepts from the empty Level 1 equation (average ESM-treatment self-efficacy across all sampling occasions) for each participant. We repeated the same procedure to obtain average ESM-social support across all sampling occasions (using ESM-social support as the dependent variable in the Level 1 equation with no predictors). We examined Pearson and partial correlations (controlling for age, race, SES, and time on ART) between these average measures of social support and treatment self-efficacy. Another method for calculating average ESM-treatment self-efficacy (or average social support) across all sampling occasions is simply to compute the arithmetic average of treatment self-efficacy (or social support) values across all sampling occasions. Therefore, we repeated the correlation analyses using these average values.
Analyses for aim 2 examined potential psychosocial moderators of the within-person association between social support and treatment self-efficacy by adding these moderators to both Level 2 equations (a separate analysis for each moderator that does not control for other moderators). A significant positive coefficient for the moderation effect indicates a stronger association between ESM social support and ESM treatment self-efficacy for individuals higher on the moderator variable. We also built a model simultaneously entering all Level 2 moderators that were significant when entered individually into the Level 2 equations (age, race, SES, and time on ART were also entered as control variables).
For aim 3, we tested the association between questionnaire and experience sampling measures of treatment self-efficacy (Q-treatment self-efficacy and ESM-treatment self-efficacy) using the following equations. (Level 2 variables were grand-mean centered.)
| (4) |
| (5) |
β0i is the Level 1 intercept reflecting the average level of (state) treatment self-efficacy for each participant across all sampling occasions. γ05 is the coefficient reflecting the magnitude of the association between Q-treatment self-efficacy and the average level of ESM-treatment self-efficacy (controlling for the covariates). We also examined this association using a different method—examining the correlation between ESM (intercepts saved from the empty HLM model reflecting average state self-efficacy across all sampling occasions or the arithmetic average) and questionnaire self-efficacy.
Finally, for aim 4 examining ESM and questionnaire treatment self-efficacy as predictors of clinical outcomes, we employed logistic regression and multiple linear regression analyses (controlling for the covariates age, race, SES, time on ART, as well as hospital visits as a measure of recent health) to predict medication adherence, visit adherence, viral load, and CD4.
Results
Preliminary Analyses
The sample included 50 white and 59 black participants with an average age of 41.36 years (SD = 10.94), from different socio-economic status (SES) levels (with 54 reporting middle class SES). In terms of sexual orientation, 17 participants reported being heterosexual, 72 participants reported being gay, 19 being bisexual, and one participant did not provide his sexual orientation. Descriptive statistics on the study variables are presented in Table 1. On average, participants responded to 15.78 (out of 21; SD = 4.79) ESM prompts. Preliminary analyses comparing the variance of the error terms at Level 1 and Level 2 suggested that the majority of the variance in momentary self-efficacy was between people (62%), with within-person variability and error accounting for 38% of the variability.
Table 1.
Descriptive statistics on the study variables (N = 109).
| Variable | Mean (SD) | Range | Possible Range |
|---|---|---|---|
| Age | 41.44 (10.96) | 24 – 68 | — |
| Time Since Starting ART Medication (Months) | 79.46 (56.06) | 12 – 227 | — |
| Visit Adherencea | .89 (.17) | .25 – 1.00 | 0 – 1 |
| Q Self-efficacy | 9.22 (1.28) | 2.50 – 10.00 | 1 −10 |
| Avoidance Coping | 2.10 (0.79) | 1.00 – 4.38 | 1 – 5 |
| Blame Coping | 2.24 (1.05) | 1.00 – 5.00 | 1 – 5 |
| Helplessness | 1.76 (0.65) | 1.00 – 3.50 | 1 – 4 |
| Attachment-related Avoidance | 2.95 (1.45) | 1.00 – 6.33 | 1 – 7 |
| Attachment-related Anxiety | 3.45 (1.52) | 1.00 – 7.00 | 1 – 7 |
| Internalized HIV Stigma | 1.95 (0.74) | 1.00 – 4.00 | 1 – 4 |
| Perceived HIV Stigma in the Community | 2.65 (0.66) | 1.00 – 4.00 | 1 – 4 |
| Appraisal of Social Support | 3.49 (0.59) | 1.00 – 4.00 | 1 – 4 |
| ESM self-efficacy | 4.74 (.52b) | 1.00 – 5.00 | 1 – 5 |
| ESM social support | 2.14 (1.27c) | 2.00 – 5.00 | 1 – 5 |
Note. ART = antiretroviral therapy.
n = 107
Average within-person standard deviation = 0.19
Average within-person standard deviation = 0.65
Aim 1 Results
In equation (3), γ10 was significant (coefficient = 0.09, t = 3.35, p = .001), indicating that on average recent support and current treatment self-efficacy were associated within-persons. This result suggests that when a person receives specific support about his HIV status, this may lead to increases in feelings of treatment self-efficacy.2 None of the covariates predicted (i.e., moderated) the Level 1 association between recent support and treatment self-efficacy (β1i).
The average measures of treatment self-efficacy and social support (intercepts saved from empty models) were not correlated (r = .09, p = .35 or rpartial = .14, p = .16 when controlling for age, race, SES, and time on ART). Average ESM-social support was also not correlated with Q-treatment self-efficacy (r = −.04, p = .65 or rpartial = −.05, p = .59 when controlling for the covariates). Using the arithmetic averages of treatment self-efficacy and social support values across all sampling occasions yielded very similar results for the association between average self-efficacy and average social support (r = .07, p = .47 or rpartial = .11, p = .26 when controlling for the covariates). Similarly, the association between average ESM-social support and Q-treatment self-efficacy was not significant (r = −.04, p = .68 or rpartial = −.05, p = .59 when controlling for the covariates). Thus, the association between social support and treatment self-efficacy was evident only in within-person analyses (and not in between-person analyses).
Aim 2 Results
Table 2 presents results of HLM analyses testing the moderating effects of psychosocial variables (see the column labeled “Interaction”). Avoidance coping with HIV, helplessness, attachment-related avoidance, and perceived stigma in the community yielded significant positive coefficients, which means that individuals higher on avoidance coping with HIV, helplessness, attachment-related avoidance, and perceived stigma in the community had stronger positive associations between recent support and treatment self-efficacy (i.e., stronger slopes for β1i) compared to individuals who have lower scores in these measures. Conversely, individuals higher on appraisal of general social support had weaker associations between recent HIV-related support and current treatment self-efficacy than individuals lower on appraisal of general social support. On the other hand, blame coping with HIV, attachment-related anxiety, and internalized stigma were not significant moderators.
Table 2.
Between-person psychosocial variables as predictors (a) of average state HIV treatment self-efficacy (main effect) and (b) of the within-person association between recent support and state treatment self-efficacy (cross-level interaction of between-person variables with recent social support). Between-person moderator variables are entered one by one (a separate analysis for each moderator that does not control for other moderators).
| Main Effect |
Interactiona |
|||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | t | p | Coefficient | SE | t | p | |
| Interceptb | 4.75 | 0.05 | 103.07 | .00 | 0.09 | 0.03 | 3.33 | .00 |
| SESb | 0.05 | 0.06 | 0.82 | .42 | −0.01 | 0.04 | −0.25 | .80 |
| Raceb | −0.18 | 0.09 | −1.96 | .05 | 0.03 | 0.07 | 0.44 | .66 |
| Ageb | −0.05 | 0.05 | −1.07 | .29 | 0.00 | 0.02 | 0.12 | .91 |
| Time on ARTb | 0.08 | 0.05 | 1.75 | .08 | −0.02 | 0.02 | −0.74 | .46 |
| Avoidance coping with HIV | −0.15 | 0.06 | −2.58 | .01 | 0.12 | 0.03 | 3.46 | .00 |
| Blame coping | −0.11 | 0.07 | −1.61 | .11 | 0.03 | 0.03 | 0.84 | .40 |
| Helplessness | −0.11 | 0.06 | −1.85 | .07 | 0.11 | 0.05 | 2.43 | .02 |
| Attachment-related avoidance | −0.10 | 0.05 | −2.24 | .03 | 0.05 | 0.02 | 2.22 | .03 |
| Attachment-related anxiety | −0.13 | 0.06 | −2.37 | .02 | 0.05 | 0.03 | 1.47 | .15 |
| Internalized stigma | −0.14 | 0.06 | −2.11 | .04 | 0.06 | 0.03 | 1.93 | .06 |
| Perceived stigma in the community | −0.08 | 0.05 | −1.64 | .10 | 0.06 | 0.03 | 2.10 | .04 |
| Appraisal of social support | 0.14 | 0.07 | 1.89 | .06 | −0.08 | 0.04 | −2.15 | .03 |
Note. Between-person predictors were standardized before entering into analyses to aid interpretation of results. Similarly, within-person predictor was also standardized using pooled within-person standard deviations.
Cross-level interaction of between-person variables with recent social support. A positive interaction terms indicates that participants higher in the between-person variable (e.g., avoidance coping) have stronger associations between recent social support and state self-efficacy.
The results for the Intercept, SES, race, age, and time on ART were very similar for each between-person predictor (slight variations due to missing data). Results shown are for the first between-person predictor (i.e., perceived stigma in the community).
As can be seen in Table 2 (the column labeled “Main Effect”), the majority of these Level 2 variables had associations with average state self-efficacy (β0i) in the opposite direction of their association with β1i (association between recent support and momentary treatment self-efficacy). For example, avoidance coping predicted lower average self-efficacy, but a stronger association between recent support and current treatment self-efficacy (see Table 2 the column labeled “Interaction”).
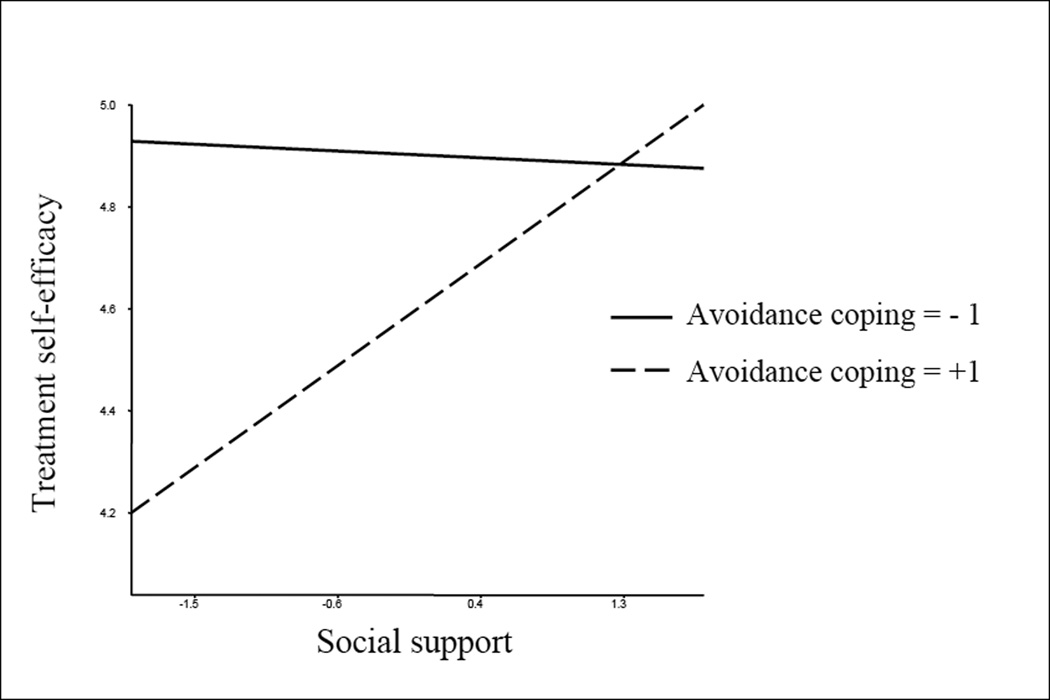
We also built a model simultaneously entering all Level 2 moderators that were significant when entered individually into the Level 2 equation (age, race, SES, and time on ART were also entered as control variables). In this analysis, avoidance coping with HIV was the only significant moderator of the within-person association between recent support and current treatment self-efficacy (coefficient = 0.10, t = 2.86, p = .006). The interaction for avoidance coping with HIV can be seen in Figure 1.
Figure 1.
Cross-level interaction between avoidance coping (at 1 SD below and 1SD above the mean) and ESM social support when predicting ESM treatment self-efficacy.
Aim 3 Results
In equation (5), γ05 was significant (coefficient = .182, t = 2.372, p = .020), suggesting that ESM-treatment self-efficacy and Q-treatment self-efficacy are associated. In order to obtain an effect size for this association, we saved the intercepts from the Level 1 equation (average ESM-treatment self-efficacy across all sampling occasions) for each participant, which showed a Pearson correlation of r = .371 (p < .001) with Q-treatment self-efficacy. When we calculated average ESM-treatment self-efficacy by simply taking the average value across all sampling occasions, the correlation between that average ESM-treatment self-efficacy and Q-treatment self-efficacy was very similar r = .355 (p < .001). Another way to examine this effect size is to compare the variances of the residual errors at Level 2 when Q-treatment self-efficacy is in the model versus when it is not. This analysis yielded an explained variance of .142.
Aim 4 Results
We examined whether Q-treatment self-efficacy or average ESM-treatment self-efficacy (intercepts saved from the Level 1 equation reflecting average ESM-treatment self-efficacy for each participant) predicted ART adherence and visit adherence. A logistic regression analysis (controlling for the covariates age, race, SES, time on ART, and hospital visits in the last 12 months, revealed that ESM-treatment self-efficacy was a significant predictor of better medication adherence (OR = 3.47, p = .026, 95% CI [1.16, 10.37]). A second (separate) logistic regression analysis (again controlling for the covariates) revealed that Q-treatment self-efficacy was not a significant predictor of medication adherence (OR = 1.50, p = .076, 95% CI [0.96, 2.35]). Similarly, a linear multiple regression analysis (controlling for the covariates) revealed that ESM-treatment self-efficacy was a significant predictor of visit adherence (β = 0.35, t = 3.89, p < .001). However, Q-treatment self-efficacy was not a significant predictor of visit adherence (β = 0.13, t = 1.37, p = .17).
Since nine participants had missing data on medication adherence, we repeated the analyses predicting medication adherence coding missing adherence data as non-adherence. These sensitivity analyses yielded very similar results: ESM-treatment self-efficacy was a significant predictor of better medication adherence (OR = 3.31, p = .028, 95% CI [1.14, 9.59], controlling for the covariates), whereas Q-treatment self-efficacy was not a significant predictor of medication adherence (OR = 1.45, p = .09, 95% CI [0.95, 2.23]).
We repeated these analyses using viral load (suppressed versus not suppressed) as the outcome. A logistic regression analysis (controlling for the covariates) revealed that ESM-treatment self-efficacy was a significant predictor of suppressed viral load (OR = 4.66, p = .015, 95% CI [1.34, 16.18]). A similar (separate) logistic regression analysis (again controlling for the covariates) revealed that Q-treatment self-efficacy was not a significant predictor of suppressed viral load (OR = 1.55, p = .151, 95% CI [0.85, 2.83]). Results were similar when CD4 (below versus above 200) was used as the outcome. ESM-treatment self-efficacy was a significant predictor of high CD4 (OR = 5.29, p = .005, 95% CI [1.64, 17.07]), but Q-treatment self-efficacy was not a significant predictor of high CD4 (OR = 1.29, p = .42, 95% CI [0.70, 2.38]).
Discussion
The goal of this study was to examine the utility of ESM in assessing HIV treatment self-efficacy in the moment, and to determine predictors and consequences of this clinically important variable in men living with HIV. We found that greater recent acts of HIV-related social support was a predictor of higher current (i.e., state) HIV treatment self efficacy, even when adjusting for important covariates such as age, SES, race, and time on ART. This finding supports our hypotheses and expands upon existing literature in other domains demonstrating that social support can affect self-efficacy (Feeney & Collins, 2015; Fitzsimons & Finkel, 2010) by showing that the positive effects of social support also generalize to the specific construct of HIV treatment self-efficacy. This is a promising finding, given that social support is a modifiable factor that might be enhanced through interventions. There are several studies in the literature providing support for the effectiveness of social support interventions, some of which use similar smart phone technology as ESM (i.e., mobile health) to deliver social support (Guillory et al., 2015).
We also found that several interpersonal and psychosocial variables moderated this relationship between HIV-related social support and treatment self-efficacy, including avoidance coping with HIV, helplessness, attachment-related avoidance, perceived stigma in the community, and perceptions of general social support. Specifically, the association between acts of HIV-related social support and increases in current (state) self-efficacy was stronger for individuals higher on avoidance coping with HIV, helplessness, attachment-related avoidance, perceived stigma in the community, and for individuals lower on perceived general social support. In an analysis that included all of the significant trait moderators, avoidance coping was the only significant moderator.
The main effect of the trait variables moderating the association between social support and state self-efficacy were in the opposite direction of the moderations. For example, higher avoidance coping predicted lower HIV treatment self-efficacy. Thus, our findings suggest that PLWH who are higher on avoidance coping (or higher on helplessness, attachment-related avoidance, perceived stigma, or lower on general social support) do not only have lower HIV treatment self-efficacy (as would be expected), but they may benefit more from specific acts of HIV-related social support in terms of boosting their low self-efficacy.
These findings are congruent with the literature suggesting that support from others can boost a person’s confidence to deal with stressors (Feeney & Collins, 2015; Fitzsimons & Finkel, 2010), as well as with the notion that individuals with certain traits benefit more from social support (Dagan et al., 2011; Girme et al., 2015). As such, these factors may be targeted in psychosocial intervention strategies to identify people living with HIV who may need enhanced social resources and who may be at risk for poorer HIV treatment self efficacy and resulting negative clinical outcomes. Such interventions can also be tailored to individual differences across participants to maximize efficacy.
For our third aim to examine the concordance between questionnaire and ESM measurement of treatment self-efficacy, we found a moderate association between these two formats, supporting that ESM measurement of this construct does map onto traditional questionnaire based measurement. However, aim 4 analyses suggested that the ESM measure of average treatment self-efficacy is a better predictor of clinical outcomes (i.e., medication adherence, visit adherence, viral load, and CD4 counts) than Q-treatment self-efficacy. Thus, it appears that ESM may offer a more valid approach to measuring this important construct in PLWH as it predicts important clinical outcomes. These findings support the use of ESM for the assessment of different constructs that may not be static from moment to moment in PLWH and that are subject to recall and interpretation biases. ESM may provide valuable data to determine psychosocial and interpersonal factors that may be amenable to interventions aiming to improve important clinical behaviors and outcomes in this population, as well as for people living with other chronic diseases. Interventions may target factors such as social support and coping to indirectly improve clinical outcomes via self-efficacy, in addition to targeting self-efficacy directly.
While this study highlights many strengths of ESM, there are some limitations to this approach in terms of feasibility and cost. Inherently, questionnaires are more cost effective than technological approaches. In addition, ESM approaches using smart phones may require familiarity with technology that some participants may not possess. Thus, training some participants extensively in the use of these methods prior to the study may be necessary. Future research should continue to examine the utility and feasibility of ESM in larger studies with other constructs and outcomes to further determine its utility.
While major strengths of this study include its novelty in using ESM to measure HIV treatment self-efficacy, collecting intensive data from each participant at multiple times during daily life, as well as including meaningful real-world treatment outcomes in PLWH, one limitation is the inclusion of only male participants. While this homogeneity was useful in drawing inferences in this initial study, future studies of larger samples should include both men and women (possibly from various geographical and cultural backgrounds) in order to ascertain potential differences in these relationships by gender and to examine generalizability. Another limitation was the use of a single self-reported item to assess adherence, which may lead to overestimation of adherence, and possibly to underestimation of the effect size of the association between self-efficacy and adherence. However, this method of assessing adherence could also lead to overestimation of the effect size of the association between self-efficacy and adherence if participants high in self-efficacy tend to overestimate their adherence. Future work may benefit from using electronic methods such as medication event monitoring systems (MEMS) to capture medication adherence. It should be noted that the present study also included objective clinical outcomes such as visit adherence, viral load, and CD4 counts. Our ESM measures of self-efficacy and social support also consisted of single items at each sampling occasion (in order to reduce participant burden), which is a limitation. Another limitation is the use of multiple tests without controlling for type I error. Finally, the ESM social support question directly asked participants about receiving social support, which deviates from the questionnaire items used to assess social support. Future studies, both interventional and observational, might examine the utility of ESM measured self-efficacy in predicting other outcomes in PLWH, such as practicing safe sex/risky sexual behaviors; tobacco, drug and alcohol cessation; depression; and engagement in other healthy behaviors (e.g., caloric restriction and physical activity).
Conclusion
People living with HIV deal with psychological and physical aspects of the disease and with the need to adhere to their treatment regimen every day. Research is needed to gain a finer understanding of what PLWH experience on a daily basis in order to help them to improve their health outcomes, since their daily experiences may affect not only their momentary mood, but may have long term effects on their mental and physical health. This study provides support for using ESM to understand predictors and consequences of HIV treatment self-efficacy in PLWH, with implications for clinical outcomes.
Table 3.
Pearson Correlations among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. ESM self-efficacy | — | 0.37** | ||||||||
| 2. Q self-efficacy | 0.37** | — | ||||||||
| 3. Avoidance coping | −0.33** | −.31** | — | |||||||
| 4. Blame coping | −0.25* | −.29** | 0.69** | — | ||||||
| 5. Helplessness | −0.23* | −.33** | 0.68** | 0.52** | — | |||||
| 6. Attachment-related avoidance |
−0.24* | −0.15 | 0.57** | 0.45** | 0.53** | — | ||||
| 7. Attachment-related anxiety | −0.30** | −0.22* | 0.64** | 0.63** | 0.46** | 0.61** | — | |||
| 8. Internalized HIV stigma | −0.30** | −.28** | 0.72** | 0.68** | 0.65** | 0.56** | 0.60** | — | ||
| 9. Perceived HIV stigma in the community |
−0.19* | −.30** | 0.59** | 0.37** | 0.55** | 0.43** | 0.47** | 0.58** | — | |
| 10. Appraisal of social support |
0.30** | 0.19* | −0.57** | −0.39** | −0.61** | −.57** | −0.55** | −.47** | −0.40** | — |
Note. ESM = experience sampling method. Q self-efficacy = Questionnaire self-efficacy
p < 0.01,
p < 0.05.
Acknowledgments
This research was supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research (CFAR), an NIH funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. Dr. Fazeli is supported by 1K99 AG048762-01 from NIA (P. Fazeli, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We would like to thank Christopher Helms, Maria Lechtreck, Wesley Browning, Christy Thai, and all the research assistants for their help in data collection.
Footnotes
Due to missing data on this variable the sample size was 99 for ART adherence.
Note that the time frame for the ESM question about support was “since your last report”, and the time frame for the ESM question about treatment self-efficacy was “right now”. Thus, in these analyses social support preceded self-efficacy in time. In further analyses, current treatment self-efficacy did not predict how much support participants reported receiving in the next sampling episode.
References
- Affleck G, Zautra A, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: a preface for the perplexed. Journal of Consulting and Clinical Psychology. 1999;67(5):746–754. doi: 10.1037//0022-006x.67.5.746. [DOI] [PubMed] [Google Scholar]
- Ammassari A, Trotta M, Murri R, Castelli F, Narciso P, Noto P, Antinori A. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. Journal of Acquired Immune Deficiency Syndromes (1999) 2002;31:S123–S127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- Bandura A. Human agency in social cognitive theory. American Psychologist. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Acosta EP, Gupta R, Guzman D, Riley ED, Harrigan PR, Deeks SG. Adherence-resistance relationships for protease and non-nucleoside reverse transcriptase inhibitors explained by virological fitness. AIDS. 2006;20(2):223–231. doi: 10.1097/01.aids.0000199825.34241.49. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The Need to Belong: Desire for Interpersonal Attachments as a Fundamental Human Motivation. Psychological Bulletin. 1995;117(3):497–529. [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in Nursing and Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Wagner GJ, Green HD, Jr, Mutchler MG, Klein DJ, McDavitt B. Social Network Characteristics Moderate the Association Between Stigmatizing Attributions About HIV and Non-adherence Among Black Americans Living with HIV: a Longitudinal Assessment. Annals of Behavioral Medicine. 2015:1–8. doi: 10.1007/s12160-015-9724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. The making and breaking of affectional bonds. New York: Routledge; 2012. [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. New York: Guilford Press; 1998. pp. 46–76. [Google Scholar]
- Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Education and Prevention. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- Dagan M, Sanderman R, Schokker MC, Wiggers T, Baas PC, van Haastert M, Hagedoorn M. Spousal support and changes in distress over time in couples coping with cancer: The role of personal control. Journal of Family Psychology. 2011;25(2):310–318. doi: 10.1037/a0022887. [DOI] [PubMed] [Google Scholar]
- DiIorio C, McCarty F, Depadilla L, Resnicow K, Holstad MM, Yeager K, Lundberg B. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS and Behavior. 2009;13(1):10–22. doi: 10.1007/s10461-007-9318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and Behavior. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers AW, Kraaimaat FW, van Lankveld W, Jongen PJ, Jacobs JW, Bijlsma JW. Beyond unfavorable thinking: the illness cognition questionnaire for chronic diseases. Journal of Consulting and Clinical Psychology. 2001;69(6):1026–1036. [PubMed] [Google Scholar]
- Feeney BC, Collins NL. A new look at social support A theoretical perspective on thriving through relationships. Personality and Social Psychology Review. 2015;19(2):113–147. doi: 10.1177/1088868314544222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman B, Fredericksen R, Crane P, Safren S, Mugavero M, Willig JH, Kitahata M. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS and Behavior. 2013;17(1):307–318. doi: 10.1007/s10461-012-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimons GM, Finkel EJ. Interpersonal influences on self-regulation. Current Directions in Psychological Science. 2010;19(2):101–105. [Google Scholar]
- Gerber B, Pagcatipunan M, Smith E, Jr, Basu S, Lawless K, Smolin L, Eiser A. The assessment of diabetes knowledge and self-efficacy in a diverse population using Rasch measurement. Journal of Applied Measurement. 2005;7(1):55–73. [PubMed] [Google Scholar]
- Girme YU, Overall NC, Simpson JA, Fletcher GJ. “All or nothing”: Attachment avoidance and the curvilinear effects of partner support. Journal of Personality and Social Psychology. 2015;108(3):450–475. doi: 10.1037/a0038866. [DOI] [PubMed] [Google Scholar]
- Godin G, Côté J, Naccache H, Lambert L, Trottier S. Prediction of adherence to antiretroviral therapy: a one-year longitudinal study. AIDS Care. 2005;17(4):493–504. doi: 10.1080/09540120412331291715. [DOI] [PubMed] [Google Scholar]
- Guillory J, Chang P, Henderson CR, Jr, Shengelia R, Lama S, Warmington M, Reid MC. Piloting a Text Message-based Social Support Intervention for Patients With Chronic Pain: Establishing Feasibility and Preliminary Efficacy. The Clinical Journal of Pain. 2015;31(6):548–556. doi: 10.1097/AJP.0000000000000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) Journal of Behavioral Medicine. 2007;30(5):359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents. MMWR: Recommendations and Reports. 2009;58(RR-4):1–207. [PubMed] [Google Scholar]
- Leary MR, Tambor ES, Terdal SK. Self-esteem as an interpersonal monitor: the sociometer hypothesis. Journal of Personality and Social Psychology. 1995;68:518–530. [Google Scholar]
- Lu M, Safren SA, Skolnik PR, Rogers WH, Coady W, Hardy H, Wilson IB. Optimal recall period and response task for self-reported HIV medication adherence. AIDS and Behavior. 2008;12(1):86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- Medard E, Kellett S. The Role of Adult Attachment and Social Support in Hoarding Disorder. Behavioural and Cognitive Psychotherapy. 2014;42(05):629–633. doi: 10.1017/S1352465813000659. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care and STDS. 2010;24(10):607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezlek JB. A multilevel framework for understanding relationships among traits, states, situations and behaviours. European Journal of Personality. 2007;21(6):789–810. [Google Scholar]
- Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. Journal of Clinical Epidemiology. 2003;56(6):520–529. doi: 10.1016/s0895-4356(03)00053-2. [DOI] [PubMed] [Google Scholar]
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. 2015 available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf.
- Payne TJ, Andrew M, Butler KR, Wyatt SB, Dubbert PM, Mosley TH. Psychometric evaluation of the interpersonal support evaluation list-short form in the ARIC study cohort. SAGE Open. 2012;2(3) 2158244012461923. [Google Scholar]
- Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, Gray RH. Viral load and heterosexual transmission of human immunodeficiency virus type 1. New England Journal of Medicine. 2000;342(13):921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 6 for Windows [Computer software] Skokie, IL: Scientific Software International: Inc; 2004. [Google Scholar]
- Reitz AK, Motti-Stefanidi F, Asendorpf JB. Me, Us, and Them: Testing Sociometer Theory in a Socially Diverse Real-Life Context. Journal of Personality and Social Psychology. 2015 doi: 10.1037/pspp0000073. Advance online publication. doi: http://dx.doi.org/10.1037/pspp0000073. [DOI] [PubMed]
- Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The ways of coping checklist: Revision and psychometric properties. Multivariate Behavioral Research. 1985;20(1):3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]