Abstract
Objective
To examine the associations among self-reported loss-of-control (LOC) eating, emotion dysregulation, body mass, and objective energy intake among youth. Emotion dysregulation may be one individual factor that promotes excess energy intake and increases in body mass among youth with LOC eating.
Methods
Children and adolescents (N=230; 8 to 17 years) enrolled in a non-intervention study completed a structured interview to determine the presence or absence of self-reported LOC eating. Children’s emotion dysregulation was assessed via parent-report with the Child Behavior Checklist. Youth also completed two test meals to capture “binge” and “normal” eating. Body composition was examined using air displacement plethysmography.
Results
After controlling for relevant covariates, youth with self-reported LOC eating had higher parent-reported emotion dysregulation than those without LOC. Parent-reported emotion dysregulation was also associated with greater observed energy intake (after accounting for body mass), as well as higher fat mass. Emotion dysregulation also moderated associations between LOC status/sex and body mass variables; among youth with self-reported LOC eating and girls, those with high parent-described emotion dysregulation (versus low) had significantly higher fat mass and BMIz.
Conclusions
Data from the current study suggest that emotion dysregulation may play a role in energy intake and obesity, particularly among youth with self-reported LOC eating and girls. Additional studies are needed to identify the prospective mechanisms linking poor emotion regulation and LOC eating. These mechanisms, in turn, may inform future interventions targeting excess energy intake and obesity in pediatric samples.
Keywords: emotion regulation, loss of control eating, binge eating, body mass, fat mass
Emotion regulation refers to the biopsychosocial processes involved in understanding and monitoring affective states, as well as the skills required to adjust the intensity and duration of one’s emotional reactions (Thompson, 1994). Adaptive emotion regulation strategies include refocusing on the positive, problem-solving, and seeking out social support, among others. In contrast, common characteristics of poor emotion regulation, or emotion dysregulation, include maladaptive cognitive coping strategies, such as rumination and catastrophic thinking, as well as ineffective behavioral responses, including aggressive action and social withdrawal. Emotion dysregulation has been shown to predict excess weight gain and obesity onset in youth (Graziano, Calkins, & Keane, 2010).
Some theoretical models suggest that youth with higher emotion dysregulation are also at greater risk for loss-of-control (LOC) eating (Kenardy, Arnow, & Agras, 1996), or the subjective experience of being unable to control what or how much is eaten, regardless of the amount of food consumed (Tanofsky-Kraff, Yanovski, & Yanovski, 2011). LOC eating is theorized to facilitate an emotional “trade off” in which one uncomfortable emotional state (e.g., depressed affect) is traded for another (e.g., guilt) (Kenardy et al., 1996). Similar to emotion dysregulation, self-reported LOC is predictive of excessive weight gain (Tanofsky-Kraff et al., 2006; Tanofsky-Kraff, Yanovski, et al., 2009). Although some theories (Kenardy et al., 1996) conceptualize LOC eating as a consequence of emotion dysregulation, a range of other individual factors are associated with increased risk for this eating behavior, such as exposure to parental problems (Hartmann, Czaja, Rief, & Hilbert, 2012). Relative to these other individual factors, youth whose LOC eating coincides with emotion dysregulation may be particularly prone to excess weight gain. Thus, rather than LOC eating fully explaining or mediating the association between emotion dysregulation and excess weight gain, the co-occurrence of these constructs – LOC eating and emotion dysregulation - may be most predictive of weight gain among youth.
LOC eating is conceptually similar to binge eating, the hallmark symptom of bulimia nervosa and binge eating disorder (American Psychiatric Association, 2013). While both eating behaviors entail a sense of loss of control over eating, binge eating requires the consumption of an objectively large amount of food. LOC eating (versus objective binge eating) has increasingly become the focus of clinical attention in youth, in part due to difficulties determining what constitutes an “unambiguously large” amount of food in growing boys and girls (Shomaker, Tanofsky-Kraff, Savastano, et al., 2010). Additionally, youth who engage in objectively versus subjectively large binge eating episodes differ very little in terms of comorbid psychological and physical symptoms (Goossens, Soenens, & Braet, 2009; Shomaker, Tanofsky-Kraff, Elliott, et al., 2010). Furthermore, self-reported LOC eating has been shown to be a precursor to partial- and full-syndrome binge eating disorder (Tanofsky-Kraff, Shomaker, et al., 2011) in youth.
Poor outcomes associated with self-reported LOC eating are thought to be due, in part, to the type and amount of food these youth consume. Data show that youth report that LOC meals are often comprised of highly palatable, calorically-dense foods (Theim et al., 2007). Moreover, youth with self-reported LOC report more frequent afternoon snacking (Matheson et al., 2012) and higher overall caloric intake (Hilbert, Rief, Tuschen-Caffier, de Zwaan, & Czaja, 2009) relative to their peers who do not endorse LOC eating. Laboratory assessments of energy intake suggest that, while youth with self-reported LOC tend to consume fewer calories from protein, and more calories from carbohydrate and highly palatable foods compared to those without LOC, the overall caloric intake of youth with and without LOC eating does not appear to differ (Hartmann, Rief, & Hilbert, 2012; Tanofsky-Kraff, McDuffie, et al., 2009). The absence of group differences in total intake raises questions regarding individual factors that might contribute to excess energy intake and associated gains in fat, body mass and metabolic problems among some youth with LOC eating. Furthermore, only about 50% of youth with self-reported LOC eating continue to experience persistent and/or exacerbated LOC eating patterns (Goldschmidt, Wall, Loth, Bucchianeri, & Neumark-Sztainer, 2013; Tanofsky-Kraff, Shomaker, et al., 2011). Identifying individual factors that distinguish LOC youth at greatest risk for poor outcomes (e.g. excess energy intake, weight gain, metabolic risk) is warranted.
As noted previously, one individual factor that may contribute to eating patterns and body mass gains among youth with LOC eating is emotion dysregulation. Indeed, cognitive emotion dysregulation, defined as difficulties understanding emotions, maladaptive expression of sadness and anger, and ruminative responses to distress, predicted increases in self-reported general disordered eating pathology, including LOC-like behavior (e.g., I have gone on eating binges where I feel that I might not be able to stop) over the course of seven months among 10–14 year olds (McLaughlin, Hatzenbuehler, Mennin, & Nolen-Hoeksema, 2011). Similarly, more behaviorally-oriented emotion dysregulation, defined as a tendency to give up, withdraw, perseverate, and engage in aggressive action, were more common among children with self-reported LOC eating relative to those without LOC (Czaja, Rief, & Hilbert, 2009). Emotion dysregulation is also positively associated with junk food intake among adolescent girls (Isasi, Ostrovsky, & Wills, 2013) and general disordered eating patterns, including self-reported LOC eating, among high school students (Mills, Newman, Cossar, & Murray, 2015). Emotion dysregulation also predicts 1-year increases in emotional and external eating among children (Harrist, Hubbs-Tait, Topham, Shriver, & Page, 2013). Data from these studies suggest that emotion dysregulation is associated with a range of self-reported eating behaviors characterized by excess energy intake, including self-reported LOC eating. While other individual factors may be salient to the development and maintenance of LOC eating specifically (e.g., dietary restraint; Goossens, Braet, & Bosmans, 2010), emotion dysregulation may be associated with continued LOC eating, as well as a general pattern of excess energy intake and weight gain. As such, individuals with LOC eating and concurrent emotion dysregulation may be at heightened risk for broad patterns of excess energy intake, as well as adverse physical and mental health outcomes.
In summary, youth with self-reported LOC eating are thought to be at higher risk for excess weight gain and poor health outcomes as a result of their eating patterns (Matheson et al., 2012; Tanofsky-Kraff, McDuffie, et al., 2009; Theim et al., 2007). Given the links between emotion dysregulation and excess energy intake (Czaja et al., 2009; McLaughlin et al., 2011; Mills et al., 2015), youth with LOC eating and concurrent difficulties with emotion regulation may be at highest risk for overeating and excess gains in fat and weight. However, this hypothesis has yet to be empirically evaluated. Further, prior studies have relied on self-report measures of eating behaviors. Using objective measures to identify individual factors associated with excess energy intake and body mass among youth with self-reported LOC eating is a first step in explicating why only some youth with LOC eating experience poor physical and mental health outcomes. We therefore examined the associations between self-reported LOC eating, emotion dysregulation, objective energy intake, and fat/body mass. We hypothesized that youth with self-reported LOC eating would have greater emotion dysregulation relative to youth who do not report LOC eating. We further expected that youth with higher emotion dysregulation, regardless of self-reported LOC status, would consume more energy in the laboratory, and have higher body and fat mass. Finally, we hypothesized that emotion regulation would moderate these associations, such that youth with self-reported LOC eating and higher emotion dysregulation would consume the most energy and have the highest fat and body mass. Interactions with sex were also examined given data suggesting that both emotion regulation strategies (Harrist et al., 2013) and prevalence of self-reported LOC eating (Tanofsky-Kraff, Yanovski, et al., 2011) differ for boys and girls.
Methods
Participants
Participants were a convenience sample of children and adolescents (8–17 years old) enrolled in a protocol investigating the eating behaviors of youth of a broad weight range (ClinicalTrials.gov Identifiers [ID]: NCT00320177). This protocol was approved by the Institutional Review Board at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Participants were recruited through physician referral, advertisements in local newspapers, and flyers posted on public bulletin boards at the National Institutes of Health (NIH), libraries, supermarkets, and school parent email listservs in the Washington, DC metropolitan area. Study flyers were also mailed to parents of children within the study’s age range. Youth enrolled in previous non-treatment studies were also invited to participate in the current study. Notices requested participation of children for a study investigating eating behaviors. Individuals were excluded if they (1) had a significant medical or psychiatric condition; (2) had abnormal hepatic, renal, or thyroid function; (3) were taking medications known to impact body weight; (4) experienced greater than five pounds of weight loss in the past three months; or (5) were undergoing weight loss treatment.
Procedures
Participants and a parent/guardian were seen during outpatient visits at the NIH Hatfield Clinical Research Center. Informed parental consent and child assent were obtained for all studies. Families understood that treatment would not be received, but that youth would be financially compensated for their participation ($100 per visit). Study procedures included anthropometric measurements and completion of several questionnaires and interviews. Research staff completed extensive training prior to administering interviews assessing self-reported LOC eating behavior. All study visits took place following an overnight fast, during which youth underwent the following procedures:
Physical Assessments
Body Composition
Participants’ height and weight were measured in a fasting state using calibrated electronic instruments. BMI standard deviation (BMIz) scores adjusted for age and sex were calculated according to the Centers for Disease Control and Prevention 2000 growth charts (Kuczmarski et al., 2002). Total fat mass and fat-free mass were measured by air displacement plethysmography (Bod Pod; Life Measurement Inc., Concord, CA) with participants wearing only underclothes or a form-fitting bathing suit (Nicholson et al., 2001).
Pubertal Stage
An endocrinologist or nurse practitioner performed a physical examination to determine pubertal stage (Bonat, Pathomvanich, Keil, Field, & Yanovski, 2002). In boys, testicular volume (mL) was estimated by using a set of orchidometer beads as standards according to Prader (Tanner, 1981). Breast development was assigned according to the five stages of Tanner (Marshall & Tanner, 1969). Testicular volume for males and Tanner breast staging for females were used to categorize youth as: pre-pubertal (stage 1), early-pubertal (stage 2), mid-pubertal (stage 3), late-pubertal (stage 4), or adult standard (stage 5). For cases in which the stage was discordant between the right and left testis/breast, the higher stage was assigned.
Psychological Assessments
Self-Reported LOC Eating
The Eating Disorder Examination (EDE), versions 12.0D (Fairburn & Cooper, 1993) or C.2 (Bryant-Waugh, Cooper, Taylor, & Lask, 1996), was used to determine the presence or absence of objective binge episodes (consumption of an unambiguously large amount of food with a sense of LOC) and subjective binge episodes (experience of LOC while consuming an ambiguously large amount of food) in the month prior to assessment. Consistent with prior research (Shomaker, Tanofsky-Kraff, Elliott, et al., 2010; Tanofsky-Kraff et al., 2007), the presence of LOC eating was coded if youth reported objective or subjective binge episodes in the past month. The child version differs from the adult EDE only in that its script has been edited to make it more accessible to children ages 8–14 years. Both versions generate the same eating episodes and subscales, and the child and adult interviews have been effectively combined (Tanofsky-Kraff et al., 2007; Tanofsky-Kraff, Han, et al., 2009; Tanofsky-Kraff, McDuffie, et al., 2009; Tanofsky-Kraff, Shomaker, et al., 2011). Inter-rater reliability for the presence of self-reported LOC eating among a subset of the current sample (7%, n = 33) was very good (Cohen’s kappa of 0.92). Group consensus determined the episode size when interviewers thought it was ambiguous, which is reflected in the excellent discriminant validity for differentiating episode size in the current study (Cohen’s kappa of 1.00).
Emotion Dysregulation
The Child Behavior Checklist, a 118-item survey designed for use in children between 6–18 (Achenbach & Elderbrock, 1991), was completed by parents to assess their perceptions of their child’s psychopathology and problem behaviors in the previous six months. An empirically-derived profile of the Child Behavior Checklist was used to assess emotion dysregulation. The Deficient Emotion Self-Regulation profile is calculated by summing the T-scores of the Anxious/Depressed, Aggression, and Attention Problems subscales (Biederman, Spencer, Lomedico, et al., 2012). This profile score captures core features of emotion dysregulation, including heightened emotional reactivity, deficits in self-regulating the physiological arousal arising from emotional reactions, difficulties inhibiting inappropriate behaviors in response to strong emotions, and problems shifting attention away from aversive emotions. The Deficient Emotion Self-Regulation profile has demonstrated good reliability, construct validity, and predictive validity in community samples and a profile score 180 indicates clinically elevated levels of emotion dysregulation (Biederman, Spencer, Petty, et al., 2012). It has been used to examine risk for bipolar disorder in pediatric samples, as well as to distinguish between children with attention deficit hyperactivity disorder and significant comorbid functional symptoms from those without such comorbid symptoms (Biederman et al., 2009; Spencer et al., 2011).
Laboratory Test Meals
All participants completed two laboratory test meals visits, as described previously (Tanofsky-Kraff, McDuffie, et al., 2009). Youth were asked to consume their lunch ad libitum from a buffet test meal on two separate days. In random order, youth participated in a “normal” meal (at which they were instructed to “eat as much as you would at a normal meal”) and a “binge” meal (at which they were instructed to “let yourself go and eat as much as you want”). Apart from the instructions, test meal conditions were identical. On the morning of each test meal, youth were provided with a standard 288-kcal breakfast (7% protein, 19% fat, 74% carbohydrate). Participants were observed for the next six hours to ensure no calorie-containing foods or beverages were consumed and no moderate-to-vigorous activity was performed. During this period, participants were permitted to engage in any non-energy intensive activities (e.g., complete homework, read magazines). In an effort to capture potential energy intake and expenditure activities which staff may have missed (e.g., eating during bathroom breaks), adherence to these instructions was assessed prior to each test meal by querying the participant. Each participant was then presented with a multiple-item, 9,835-kcal food array varied in macronutrient composition (51% carbohydrate, 12% protein, 37% fat, across all foods) and containing a wide assortment of foods (Mirch et al., 2006). These paradigms are standard, well-validated approaches in pediatric samples (Mirch et al., 2006; Tanofsky-Kraff, McDuffie, et al., 2009). All presented food items were weighed to the nearest 0.1 g before and after the test meal sessions. Total energy intake (kcal) and percent macronutrient content consumed (carbohydrate, fat, and protein) were calculated (Tanofsky-Kraff, McDuffie, et al., 2009).
Analytic Plan
Data were screened for normality. Extreme, but plausible, outliers were recoded to fall 1.5 times the interquartile range below or above the 25th or 75th percentile so they were no longer outliers (Behrens, 1997). This a priori strategy was used because it minimizes outliers’ influence on the characteristics of the distribution, minimally changes the distribution overall, and avoids potential bias associated with eliminating outliers (Behrens, 1997). No more than 3% of the data comprising any variable was considered an outlier. After adjusting outliers, skewness and kurtosis were confirmed to be satisfactory for all variables. Listwise deletion was employed for missing data. This approach is considered satisfactory when missing data are minimal (less than 5%) and random (Buhi, Goodson, & Neilands, 2008; Duffy, 2006). Further, Little’s Missing Completely at Random analyses confirmed that missing data were random, or not related to any primary independent or dependent variable of interest in the current study (ps>.05).
Participants were categorized into one of two groups based on the presence or absence of self-reported LOC eating within the previous month. For all models, covariates were selected a priori because of their association with their respective dependent variable. General linear models (GLM) were used to examine differences in parent-reported emotion dysregulation by LOC status. Covariates included age (Zimmermann & Iwanski, 2014), puberty (Crockett, Carlo, Wolff, & Hope, 2013), race (coded as non-Hispanic White or Other) (Chapman & Mullis, 2000), sex (Zimmermann & Iwanski, 2014), and fat mass (%, arcsine transformed) (Vandewalle, Moens, & Braet, 2014). GLM analyses were also used to examine the main and interaction effects of self-reported LOC status and parent-reported emotion dysregulation (centered based on the grand mean to reduce multicollinearity concerns) (Cohen, Cohen, West, & Aiken, 2003) on BMIz and fat mass. Covariates included age, puberty, race (Ogden, Carroll, Kit, & Flegal, 2014), sex (Crocker et al., 2014), and height (cm) (Kakinami, Henderson, Chiolero, Cole, & Paradis, 2014). Linear mixed models with repeated measures were used to examine the main and interaction effects of self-reported LOC status and emotion dysregulation on energy intake, including total kilocalories (log transformed to improve normality) and percent macronutrient content consumed (carbohydrate, fat, and protein). Significant interaction terms provide evidence of the moderating properties of emotion dysregulation. Because total energy intake did not significantly differ for youth with or without self-reported LOC eating at the “binge” or “normal” meal (Tanofsky-Kraff, McDuffie, et al., 2009), meal instruction was treated as a repeated measure in all models; covariates included age, puberty, race, sex, height, fat mass, and fat-free mass (kg) (Goulding, Taylor, Gold, & Lewis-Barned, 1996; Shomaker, Tanofsky-Kraff, Savastano, et al., 2010). Total energy intake was also included as a covariate in the models examining percent macronutrient. Meal type randomization was considered as a covariate but was removed because it did not significantly contribute to any model and did not improve overall model fit. Participant was treated as a random effect to allow for within-subject correlation and all other independent variables were treated as fixed effects.
Secondary analyses included sex as a two- and three-way interaction term with self-reported LOC status and emotion dysregulation in relevant models. For significant interactions, follow-up analyses were conducted to examine differences in the respective dependent variable at one standard deviation (SD) above and below the mean for the moderator (i.e., parent-reported emotion dysregulation), described as high and low, respectively. Results from unadjusted models (without covariates) are presented briefly. All analyses were performed with SPSS version 22 and all tests were two-tailed. To control for multiple comparisons, the Benjamini–Hochberg (1995) procedure for false discovery rate was applied to each family of analyses.
Results
Sample Characteristics
A total of 230 children and adolescents (8–17y) were studied. Participant characteristics by self-reported LOC status are presented in Table 1. In these unadjusted models, youth who self-reported recent LOC eating had significantly higher BMIz scores and fat mass relative to youth who did not report LOC eating (ps < .001). Relative to those who did not endorse LOC eating, a greater percentage of youth with self-reported LOC eating were female (p < .01).
Table 1.
Comparisons between youth with and without loss-of-control eating
| Characteristicsa | LOCb Eating Present (n=65) | LOC Eating Absent (n=156) |
|---|---|---|
| Age (y) | 14.0±2.5 (8.0–17.8) | 13.0±2.8 (8.1–17.9) |
| Height (cm) | 156.5±13.8 (126.6–181.5) | 156.0±15.8 (118.4–189.8) |
| Sex: female (%) | 69.2** | 44.2 |
| Race: White (%) | 58.5 | 56.4 |
| Pubertal status (median) | 3 (1–5) | 3 (1–5) |
| BMIzc score | 1.3±1.1 (−1.4–2.9)** | 0.7±1.1 (−2.2–3.2) |
| Weight status: overweight/obese (%) | 16.9/46.2* | 21.2/22.4 |
| Fat-free mass (kg) | 42.9±16.3 (20.6–97.9) | 42.0±14.8 (19.8–77.2) |
| Fat mass (kg) | 24.6±18.2 (2.9–99.8)** | 16.3±16.4 (1.1–110.9) |
| Fat mass (%) | 33.2±11.8 (10.7–54.9)** | 24.9±12.3 (1.6–59.1) |
Values presented are mean ± standard deviation (range), unless otherwise noted.
LOC = loss-of-control;
BMIz = body mass index z score; p < .001, p < .01
Primary Analyses – Body Mass and Adiposity
In adjusted models, youth with self-reported LOC eating (M=162.11±1.85) had significantly higher parent-reported emotion dysregulation scores compared to youth without LOC eating (M=157.20±1.17), F (1, 206) = 5.00, p < .03, partial eta2 = .02. The association between emotion dysregulation and BMIz was not statistically significant, F (1, 216) = 2.04, p = .16, partial eta2 = .01. However, emotion dysregulation was positively and significantly associated with fat mass, F (1, 215) = 5.04, p < .03, partial eta2 = .02.
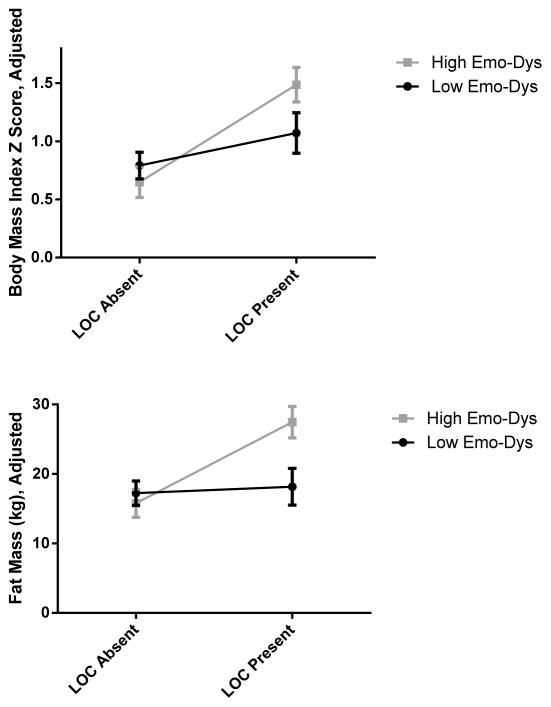
The interaction between self-reported LOC status and parent-reported emotion dysregulation was significant for both BMIz, F (1, 208) = 4.39, p < .04, partial eta2 = .02, and fat mass, F (1, 207) = 7.01, p < .01, partial eta2 = .03. These data suggest that parent-reported emotion dysregulation moderated the association between self-reported LOC status and adiposity. Follow-up analyses indicate that, at low levels of parent-reported emotion dysregulation, neither fat mass, F (1, 207) = .09, p = .77, partial eta2 = <.001, nor BMIz, F (1, 208) = 1.79, p = .18, partial eta2 = .01, differed for youth with or without self-reported LOC eating. However, at high levels of emotion dysregulation, youth with self-reported LOC eating had significantly higher BMIz, F (1, 208) = 16.91, p < .001, partial eta2 = .08, and fat mass, F (1, 207) = 14.17, p < .001, partial eta2 = .02, relative to youth without LOC (Figure 1). Results did not differ when analyses were run separately for “normal” and “binge” meals (data not shown).
Figure 1.
Emotion dysregulation moderated the link between LOC status and body mass variables such that youth with self-reported LOC eating and high parent-reported emotion dysregulation had significantly more body mass and fat mass
After controlling for age, sex, race, puberty, and height, the link between LOC status and BMIz did not differ significantly among those with low parent-reported emotion dysregulation, F (1, 208) = 1.79, p = .18, partial eta2 = .01, but did significantly differ among those with high parent-reported emotion dysregulation, F (1, 208) = 16.91, p < .001, partial eta2 = .08. Similarly, the link between LOC status and fat mass did not differ significantly among those with low parent-reported emotion dysregulation, F (1, 207) = .09, p = .77, partial eta2 = <.001, but did significantly differ among those with high parent-reported emotion dysregulation, F (1, 207) = 14.17, p < .001, partial eta2 = .02. Youth with LOC eating and high emotion dysregulation had significantly higher body mass and fat mass relative to those with low emotion dysregulation.
Primary Analyses – Energy Intake
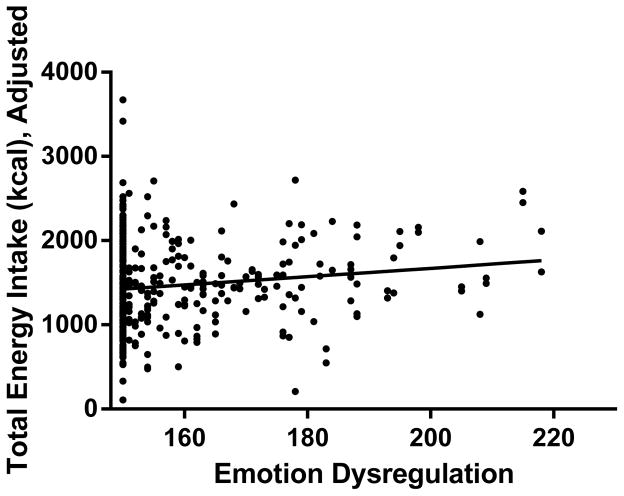
Emotion dysregulation was positively and significantly associated with total energy intake, F (1, 373) = 9.02, p < .003, partial eta2 = .031. Youth with greater parent-reported dysregulation scores consumed more total energy during their test meals, even after accounting for body mass (Figure 2). Emotion dysregulation was not significantly associated with macronutrient consumption for protein, F (1, 372) = .71, p = .39, fat, F (1, 372) = 2.38, p = .12, or carbohydrates, F (1, 372) = 3.14, p = .08.
Figure 2.
Greater parent-reported emotion dysregulation is associated with higher total energy intake
Emotion dysregulation was positively and significantly associated with total energy intake after controlling for age, puberty, race, sex, height, fat mass, and fat-free mass, F (1, 373) = 9.02, p < .003, partial eta2 = .03.
The interaction between self-reported LOC status and parent-reported emotion dysregulation was non-significant for total energy intake, F (1, 366) = .28, p = .60, protein consumption, F (1, 365) = .55, p = .46, fat consumption, F (1, 366) = .25, p = .62, and carbohydrate consumption, F (1, 366) = .01, p = .93. These data indicate that emotion dysregulation did not moderate the associations between self-reported LOC eating and energy intake. Results did not differ when analyses were run separately for the “normal” and “binge” meals (data not shown).
Follow-up Interactional Analyses by Sex – Body Mass and Adiposity
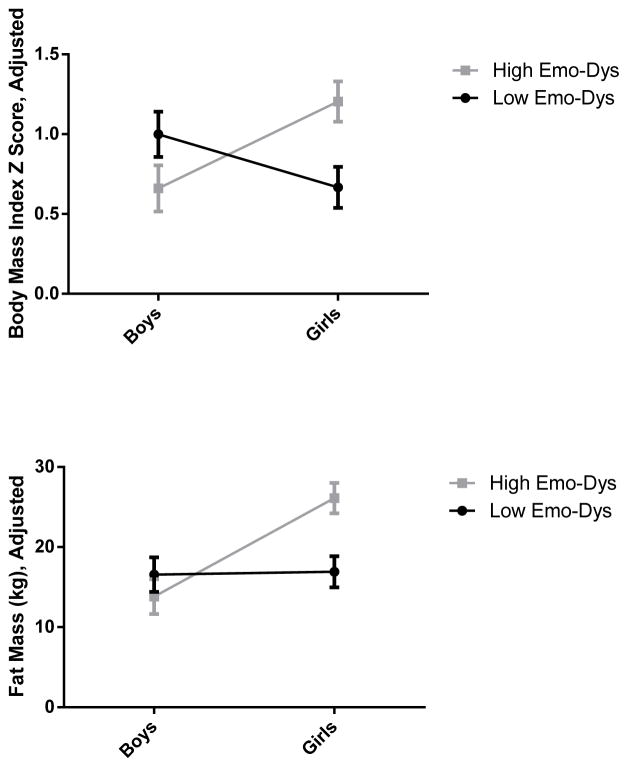
Interactions between parent-reported emotion dysregulation and sex were significant for BMIz, F (1, 215) = 11.16, p < .001, partial eta2 = .05, and fat mass, F (1, 214) = 9.05, p < .003, partial eta2 = .04. Follow-up analyses indicate that the link between sex and BMIz did not significantly differ among those with low emotion dysregulation, F (1, 215) = 2.90, p = .09, partial eta2 = .01, but did significantly differ among those with high emotion dysregulation, F (1, 215) = 7.83, p < .006, partial eta2 = .04. Similarly, the link between sex and fat mass did not significantly differ among those with low parent-reported emotion dysregulation, F (1, 214) = .01, p = .91, partial eta2 < .001, but did significantly differ among those with high emotion dysregulation, F (1, 214) = 17.49, p < .001, partial eta2 = .08 (Figure 3). These results indicate that, at low levels of emotion dysregulation, girls and boys did not significantly differ from one another in terms of their body mass or fat mass. However, at high levels of emotion dysregulation, both body and fat mass were significantly higher among girls relative to boys.
Figure 3.
Emotion dysregulation moderated the associations between sex and body mass, such that girls with higher parent-reported emotion dysregulation had more body mass and fat mass
After controlling for age, race, puberty, and height, the link between sex and BMIz did not significantly differ among those with low parent-reported emotion dysregulation, F (1, 215) = 2.90, p = .09, partial eta2 = .01, but did significantly differ among those with high parent-reported emotion dysregulation, F (1, 215) = 7.83, p < .006, partial eta2 = .04. Similarly, the link between sex and fat mass did not significantly differ among those with low parent-reported emotion dysregulation, F (1, 214) = .01, p = .91, partial eta2 < .001, but did significantly differ among those with high parent-reported emotion dysregulation, F (1, 214) = 17.49, p < .001, partial eta2 = .08. Compared to girls with low emotion dysregulation, girls with high dysregulation had significantly higher fat and body mass.
Three-way interactions between self-reported LOC status, parent-reported emotion dysregulation, and sex were not significant for BMIz, F (1, 205) = 1.99, p = .16, partial eta2 = .01, or fat mass, F (1, 204) = .12, p = .73, partial eta2 = .001.
Follow-up Interactional Analyses by Sex – Energy Intake
Interactions between emotion dysregulation and sex were non-significant for total energy intake, F (1, 372) = 2.00, p = .16, as well as protein, F (1, 371) = .03, p = .87, fat, F (1, 371) = .02, p = .90, and carbohydrate consumption, F (1, 371) = .00, p = .98. Three-way interactions between self-reported LOC status, parent-reported emotion dysregulation, and sex were not significant for any energy intake variable, including: total energy intake, F (1, 364) = 2.72, p = .10, protein consumption, F (1, 363) = .001, p = .97, fat consumption, F (1, 363) = .05, p = .82, or carbohydrate consumption, F (1, 363) = .02, p = .88.
Unadjusted Models
Results for unadjusted models, in which all covariates were removed, paralleled those for adjusted models (data not shown).
Discussion
Prior research has shown that self-reported LOC eating is associated with general patterns of overeating (Hilbert et al., 2009; Matheson et al., 2012; Theim et al., 2007) and excess weight and fat gains among pediatric samples (Tanofsky-Kraff et al., 2006; Tanofsky-Kraff, Yanovski, et al., 2009). However, not all youth with this type of eating behavior experience persistent concerns with eating and weight (Hartmann et al., 2012; Tanofsky-Kraff, McDuffie, et al., 2009; Goldschmidt et al., 2013; Hilbert et al., 2013; Tanofsky-Kraff, Shomaker, et al., 2011). As such, to pinpoint those at highest risk for chronic health concerns, it is important to identify individual factors which may be most salient to excess energy intake and elevated body mass among youth with LOC eating. Emotion dysregulation may be one such factor, given its links with self-reported overeating patterns, including LOC eating (Czaja et al., 2009; McLaughlin et al., 2011; Mills et al., 2015). However, this hypothesis has yet to be tested as prior studies have not evaluated LOC eating, emotion dysregulation, energy intake, and body mass concurrently. Moreover, prior research on emotion dysregulation and eating behavior has largely relied on self-report methods of energy intake. The current study addressed both of these limitations, thereby facilitating the explication of individual factors associated with excess energy intake and body mass among youth with self-reported LOC eating.
Consistent with prior research (Czaja et al., 2009), data from the current study indicates that children and adolescents with self-reported LOC eating demonstrated greater emotion dysregulation per their parents’ report relative to their peers without self-reported LOC eating. Youth with higher parent-reported emotion dysregulation also consumed more calories when presented with a buffet of food items, and had higher measured BMIz and fat mass. Importantly, parent-reported emotion dysregulation functioned as a moderator between self-reported LOC status, sex and body mass variables, such that youth with self-reported LOC eating and girls had significantly higher fat mass and BMIz when their parents described their children’s emotion dysregulation as high. There were no sex- or LOC-related differences in body or fat mass when emotion dysregulation was low.
Broadly, these data are consistent with prior cross-sectional (Czaja et al., 2009) and prospective studies (McLaughlin et al., 2011; Mills et al., 2015). These data lend further credence to emotion regulation models for LOC eating (Kenardy et al., 1996), which state that the overconsumption of palatable foods may function as a means of relieving negative emotions. Youth who tend to use ineffective strategies to manage negative emotions may be more prone to both excess energy intake and LOC eating as these behaviors offer relatively efficient (albeit maladaptive) means of coping with aversive affective states. These eating patterns, in turn, promote excessive gains in weight and fat mass (Tanofsky-Kraff et al., 2006; Tanofsky-Kraff, McDuffie, et al., 2009).
Emotion dysregulation and self-reported LOC eating may also be behavioral manifestations of the same impulsive disposition (Nederkoorn, Braet, Van Eijs, Tanghe, & Jansen, 2006), which appears to place vulnerable youth at risk for excessive weight gain (Graziano et al., 2010; van den Berg et al., 2011). From an early age, some children demonstrate difficulties regulating their behavior (Graziano et al., 2010) and these self-regulatory problems may manifest in both food and non-food contexts. Indeed, youth who present with both self-reported LOC eating and obesity demonstrate more behavioral impulsivity on a cognitive task than obese youth without LOC eating (Nederkoorn et al., 2006). Thus, higher levels of emotion dysregulation, self-reported LOC eating behavior, and body mass may all be the result of broad difficulties regulating behavior, rather than (or perhaps in addition to) using palatable foods to cope with difficult emotions.
Data from the current study suggest that parent-reported emotion regulation problems may play a more prominent role in elevated body mass and adiposity among girls and youth with self-reported LOC relative to boys and youth without LOC eating. These findings extend prior research which has not evaluated these constructs concurrently, and are consistent with hypotheses that emotion dysregulation may be an individual factor associated with greater body mass concerns among youth with LOC eating. However, contrary to hypotheses, these associations appear to be the result of factors other than energy intake (as such models were non-significant). Girls and youth with self-reported LOC are more likely than boys and youth who do not report LOC, respectively, to endorse a number of internalizing mood symptoms, such as depressive symptoms (Hilbert et al., 2013) and shape/weight concerns (Tanofsky-Kraff, Shomaker, et al., 2011). Girls also tend to attribute higher levels of stress to interpersonal conflict (Hampel & Petermann, 2006). As a result of these symptoms, girls and youth with self-reported LOC may be more inclined to social isolation and inactivity when a stressor arises, thereby contributing to an energy imbalance promoting body mass gains. Boys, in contrast, tend to engage in externalizing behaviors when stressed (Harrist et al., 2013). Alternatively, the methods used in the current study may not have captured energy intake associated with emotion dysregulation. While the current study examined self-reported LOC eating behavior and objective energy intake, we did not specifically assess eating in response to acute negative affect. Indeed, emotional eating has been linked to emotion dysregulation (Vandewalle et al., 2014). However, given that emotional eating has not been shown to predict excess weight or fat gain, we opted to study self-reported LOC eating, a construct that has been consistently associated with adverse outcomes (Tanofsky-Kraff et al., 2006; Tanofsky-Kraff et al., 2012; Tanofsky-Kraff, Yanovski, et al., 2009). Nevertheless, emotional eating may account for the link between emotion dysregulation and adiposity in girls and warrants future study. Further, energy intake was assessed in the laboratory, which may have been affected by demand characteristics. Energy intake assessed in the natural environment may yield differing results.
Potential explanations for the link between emotion dysregulation, energy intake, and adiposity are speculative given the cross-sectional nature of our data. Although the current study utilized objective measurements of body composition and energy intake, as well as a well-validated interview of self-reported LOC eating, prospective data are needed to elucidate the developmental nature of these variables, as well as potential mechanistic factors. It is frequently presumed that emotion dysregulation precedes LOC eating and subsequent weight gain (Kenardy et al., 1996); however, the onset and causes of these problems may differ across individuals. For instance, some adolescents describe initiating LOC eating to cope with the negative affect associated with weight-related teasing (Puhl & Luedicke, 2012). Therefore, elevated weight and adiposity may precede self-reported LOC eating. For others, the presence of early risk factors, such as chronic stressors, may lead to deteriorations in self-regulatory abilities, which ultimately promote obesogenic behaviors and significant gains in body mass (Evans, Fuller-Rowell, & Doan, 2012). Further clarification of the role of emotion regulation difficulties in promoting and/or maintaining LOC eating and excess weight gain in youth, particularly girls, is critical to the development of clinical interventions.
While a strength of the current study is its evaluation of a large, community-based sample of boys and girls, youth seeking weight management tend to endorse higher levels of disordered eating (Decaluwe, Braet, & Fairburn, 2003). Thus, additional studies are needed to determine if the current data generalize to clinical samples. Emotion dysregulation was also measured via parent-report, which may introduce additional biases. For instance, parents may lack awareness of their children’s ability to regulate emotions in situations outside of the home (e.g., school). Additionally, objective energy intake was captured at two time points in a laboratory setting. Observational methods in multiple settings would be ideal in characterizing the emotion regulation and eating patterns among youth. Further, while adherence to study procedures was closely observed across studies, participants may have engaged in energy intake or expenditure activities that our research team was not able to capture. Finally, some effects sizes for the current study’s findings were small. Replication with larger samples is needed to confirm the value of using these data to inform clinical interventions.
In summary, children and adolescents with self-reported LOC eating tend to engage in more maladaptive emotion regulation strategies than their peers without LOC eating. Emotion regulation difficulties may be one individual factor that contributes to the long-term health problems associated with persistent LOC eating among a subset of at-risk youth. Additional studies are needed to identify the prospective mechanisms linking poor emotion regulation and LOC eating and to determine whether these associations differ by sex.
Acknowledgments
Research support: USUHS grant R072IC (to MTK). Intramural Research Program, NIH, grant 1ZIAHD000641 from the NICHD with supplemental funding from NIMHD, the Bench to Bedside Program, the Office of Behavioral and Social Sciences Research (OBSSR) of the NIH (to JAY), and NIMH 5F31MH095348 (to LMR). AMA is supported by the Division of Nutrition Research Coordination, NIH.
Footnotes
Many limitations have been noted regarding effect sizes for linear mixed models (Nakagawa & Schielzeth, 2013). As such, for significant results, we present a partial eta2 calculated from GLMs in which an average intake score was created for each person from the two test meals.
Disclosures: J.A. Yanovski and M. Kozlosky are Commissioned Officers in the United States Public Health Service (PHS).
Disclaimer: The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the PHS, USUHS, or the United States Department of Defense.
References
- Achenbach TM, Elderbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. University of Vermont, Department of Psychiatry; Burlington: 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Behrens JT. Principles and procedures of exploratory data analysis. Psychological Methods. 1997;2(2):131–160. [Google Scholar]
- Benjamini Y, Hochberg T. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B, Statistical methodology Royal Statistical Society. 1995;57:289–300. [Google Scholar]
- Biederman J, Petty CR, Monuteaux MC, Evans M, Parcell T, Faraone SV, Wozniak J. The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. Journal of Clinical Psychiatry. 2009;70:732–740. doi: 10.4088/JCP.08m04821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Spencer T, Lomedico A, Day H, Petty CR, Faraone SV. Deficient emotional self-regulation and pediatric attention deficit hyperactivity disorder: a family risk analysis. Psychological Medicine. 2012;42(3):639–646. doi: 10.1017/S0033291711001644. [DOI] [PubMed] [Google Scholar]
- Biederman J, Spencer TJ, Petty C, Hyder LL, O’Connor KB, Surman CB, Faraone SV. Longitudinal course of deficient emotional self-regulation CBCL profile in youth with ADHD: prospective controlled study. Neuropsychiatric Disease and Treatment. 2012;8:267–276. doi: 10.2147/NDT.S29670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonat S, Pathomvanich A, Keil MF, Field AE, Yanovski JA. Self-assessment of pubertal stage in overweight children. Pediatrics. 2002;110(4):743–747. doi: 10.1542/peds.110.4.743. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: A pilot study. International Journal of Eating Disorders. 1996;19(4):391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Buhi ER, Goodson R, Neilands TB. Out of sight, not out of mind: Strategies for handling missing data. American Journal of Health Behavior. 2008;32:83–92. doi: 10.5993/AJHB.32.1.8. [DOI] [PubMed] [Google Scholar]
- Chapman PL, Mullis RL. Racial differences in adolescent coping and self-esteem. Journal of Genetic Psychology. 2000;161(2):152–160. doi: 10.1080/00221320009596702. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Crocker MK, Stern EA, Sedaka NM, Shomaker LB, Brady SM, Ali AH, … Yanovski JA. Sexual dimorphisms in the associations of BMI and body fat with indices of pubertal development in girls and boys. Journal of Clinical Endocrinology and Metabolism. 2014;99(8):E1519–E1529. doi: 10.1210/jc.2014-1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crockett LJ, Carlo G, Wolff JM, Hope MO. The role of pubertal timing and temperamental vulnerability in adolescents’ internalizing symptoms. Developmental Psychopathology. 2013;25(2):377–389. doi: 10.1017/S0954579412001125. [DOI] [PubMed] [Google Scholar]
- Czaja J, Rief W, Hilbert A. Emotion regulation and binge eating in children. International Journal of Eating Disorders. 2009;42(4):356–362. doi: 10.1002/eat.20630. [DOI] [PubMed] [Google Scholar]
- Decaluwe V, Braet C, Fairburn C. Binge eating in obese children and adolescents. International Journal of Eating Disorders. 2003;33:78–84. doi: 10.1002/eat.10110. [DOI] [PubMed] [Google Scholar]
- Duffy ME. Handling missing data: A commonly encountered problem in quantitative research. Clinical Nurse Specialist. 2006;20:273–276. doi: 10.1097/00002800-200611000-00005. [DOI] [PubMed] [Google Scholar]
- Evans GW, Fuller-Rowell TE, Doan SN. Childhood cumulative risk and obesity: The mediating role of self-regulatory ability. Pediatrics. 2012;129(1):e68–73. doi: 10.1542/peds.2010-3647. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Goldschmidt AB, Wall MM, Loth KA, Bucchianeri MM, Neumark-Sztainer D. The course of binge eating from adolescence to young adulthood. Health Psychology. 2014;33(5):457–460. doi: 10.1037/a0033508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, Braet C, Bosmans G. Relations of dietary restraint and depressive symptomatology to loss of control over eating in overweight youngsters. European Child and Adolescent Psychiatry. 2010;19(7):587–596. doi: 10.1007/s00787-010-008. [DOI] [PubMed] [Google Scholar]
- Goossens L, Soenens B, Braet C. Prevalence and characteristics of binge eating in an adolescent community sample. Journal of Clinical Child and Adolescent Psychology. 2009;38:342–353. doi: 10.1080/15374410902851697. [DOI] [PubMed] [Google Scholar]
- Goulding A, Taylor RW, Gold E, Lewis-Barned NJ. Regional body fat distribution in relation to pubertal stage: a dual-energy X-ray absorptiometry study of New Zealand girls and young women. American Journal of Clinical Nutrition. 1996;64(4):546–551. doi: 10.1093/ajcn/64.4.546. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. International Journal of Obesity. 2010;34:633–641. doi: 10.1038/ijo.2009.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel P, Petermann F. Perceived stress, coping, and adjustment in adolescents. Journal of Adolescent Health. 2006;38(4):409–415. doi: 10.1016/j.jadohealth.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Harrist AW, Hubbs-Tait L, Topham GL, Shriver LH, Page MC. Emotion regulation is related to children’s emotional and external eating. Journal of Developmental and Behavioral Pediatrics. 2013;34(8):557–565. doi: 10.1097/DBP.0b013e3182a5095f. [DOI] [PubMed] [Google Scholar]
- Hartmann AS, Czaja J, Rief W, Hilbert A. Psychosocial risk factors of loss of control eating in primary school children: A retrospective case-control study. International Journal of Eating Disorders. 2012;45(6):751–758. doi: 10.1002/eat.22018. [DOI] [PubMed] [Google Scholar]
- Hartmann AS, Rief W, Hilbert A. Laboratory snack food intake, negative mood, and impulsivity in youth with ADHD symptoms and episodes of loss of control eating. Where is the missing link? Appetite. 2012;58(2):672–678. doi: 10.1016/j.appet.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, Czaja J. Loss of control eating and psychological maintenance in children: An ecological momentary assessment study. Behavior Research and Therapy. 2009;47(1):26–33. doi: 10.1016/j.brat.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Isasi CR, Ostrovsky NW, Wills TA. The association of emotion regulation with lifestyle behaviors in inner-city adolescents. Eating Behavior. 2013;14(4):518–521. doi: 10.1016/j.eatbeh.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakinami L, Henderson M, Chiolero A, Cole TJ, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Archives of Disease in Childhood. 2014;99(11):1020–1024. doi: 10.1136/archdischild-2013-305163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, Agras WS. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australasian Psychiatry. 1996;30(6):839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Archives of Disease in Childhood. 1969;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson BE, Tanofsky-Kraff M, Shafer-Berger S, Sedaka NM, Mooreville M, Reina SA, … Yanovski JA. Eating patterns in youth with and without loss of control eating. International Journal of Eating Disorders. 2012;45(8):957–961. doi: 10.1002/eat.22063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behavior Research and Therapy. 2011;49(9):544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills P, Newman EF, Cossar J, Murray G. Emotional maltreatment and disordered eating in adolescents: Testing the mediating role of emotion regulation. Child Abuse & Neglect. 2015;39:156–166. doi: 10.1016/j.chiabu.2014.05.011. [DOI] [PubMed] [Google Scholar]
- Mirch MC, McDuffie JR, Yanovski SZ, Schollnberger M, Tanofsky-Kraff M, Theim KR, … Yanovski JA. Effects of binge eating on satiation, satiety, and energy intake of overweight children. American Journal of Clinical Nutrition. 2006;84(4):732–738. doi: 10.1093/ajcn/84.4.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S, Schielzeth H. A general and simplemethod for obtaining R2 from generalized linearmixed-effectsmodels. Methods in Ecology and Evolution. 2013;4:133–142. doi: 10.1111/j.2041-210x.2012.00261.x. [DOI] [Google Scholar]
- Nederkoorn C, Braet C, Van Eijs Y, Tanghe A, Jansen A. Why obese children cannot resist food: The role of impulsivity. Eating Behaviors. 2006;7(4):315–322. doi: 10.1016/j.eatbeh.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Nicholson JC, McDuffie JR, Bonat SH, Russell DL, Boyce KA, McCann S, … Yanovski JA. Estimation of body fatness by air displacement plethysmography in African American and white children. Pediatric Research. 2001;50(4):467–473. doi: 10.1203/00006450-200110000-00008. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA: Journal of the American Medical Association. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Luedicke J. Weight-based victimization among adolescents in the school setting: emotional reactions and coping behaviors. Journal of Youth and Adolescence. 2012;41(1):27–40. doi: 10.1007/s10964-011-9713-z. [DOI] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Elliott CA, Wolkoff LE, Columbo KM, Ranzenhofer LM, Yanovski JA. Salience of loss of control for pediatric binge episodes: Does size really matter? International Journal of Eating Disorders. 2010;43(8):707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Savastano DM, Kozlosky M, Columbo KM, Wolkoff LE, Yanovski JA. Puberty and observed energy intake: Boy, can they eat! American Journal of Clinical Nutrition. 2010;92(1):123–129. doi: 10.3945/ajcn.2010.29383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer TJ, Faraone SV, Surman CB, Petty C, Clarke A, Batchelder H, … Biederman J. Toward defining deficient emotional self-regulation in children with attention-deficit/hyperactivity disorder using the Child Behavior Checklist: a controlled study. Postgraduate Medicine. 2011;123(5):50–59. doi: 10.3810/pgm.2011.09.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner JM. Growth and maturation during adolescence. Nutrition Reviews. 1981;39(2):43–55. doi: 10.1111/j.1753-4887.1981.tb06734.x. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, … Yanovski JA. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117(4):1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, … Yanovski JA. A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology. 2007;75(6):901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Han JC, Anandalingam K, Shomaker LB, Columbo KM, Wolkoff LE, Yanovski JA. The FTO gene rs9939609 obesity-risk allele and loss of control over eating. American Journal of Clinical Nutrition. 2009;90(6):1483–1488. doi: 10.3945/ajcn.2009.28439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, Yanovski JA. Laboratory assessment of the food intake of children and adolescents with loss of control eating. American Journal of Clinical Nutrition. 2009;89(3):738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, Yanovski JA. A prospective study of pediatric loss of control eating and psychological outcomes. Journal of Abnormal Psychology. 2011;120(1):108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, Dellavalle D, … Yanovski JA. Children’s binge eating and development of metabolic syndrome. International Journal of Obesity. 2012;36:956–962. doi: 10.1038/ijo.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders. 2009;42(1):26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Loss of control over eating in children and adolescents. In: Striegel-Moore RH, Wonderlich SA, Walsh BT, Mitchell JE, editors. Developing an Evidence-Based Classification of Eating Disorders: Scientific Findings for DSM-5. Washington, DC: American Psychiatric Association Press; 2011. pp. 221–236. [Google Scholar]
- Theim KR, Tanofsky-Kraff M, Salaita CG, Haynos AF, Mirch MC, Ranzenhofer LM, … Yanovski JA. Children’s descriptions of the foods consumed during loss of control eating episodes. Eating Behavior. 2007;8(2):258–265. doi: 10.1016/j.eatbeh.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R. Emotion regulation: a theme in search of a definition. Emotion Regulation: Biological and Behavioral Considerations. In: Fox NA, editor. Monographs of the Society for Research in Child Development. Vol. 59. Chicago: University of Chicago Press; 1994. pp. 25–52. [PubMed] [Google Scholar]
- van den Berg L, Pieterse K, Malik JA, Luman M, Willems van Dijk K, Oosterlaan J, Delemarre-van de Waal HA. Association between impulsivity, reward responsiveness and body mass index in children. International Journal of Obesity. 2011;35(10):1301–1307. doi: 10.1038/ijo.2011.116. [DOI] [PubMed] [Google Scholar]
- Vandewalle J, Moens E, Braet C. Comprehending emotional eating in obese youngsters: the role of parental rejection and emotion regulation. International Journal of Obesity. 2014;38(4):525–530. doi: 10.1038/ijo.2013.233. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Iwanski A. Emotion regulation from early adolescence to emerging adulthood and middle adulthood: Age differences, gender differences, and emotion-specific developmental variations. International Journal of Behavioral Development. 2014:1–14. doi: 10.1177/0165025413515405. [DOI] [Google Scholar]