Abstract
Health-related quality of life (HRQOL) is an important determinant of prognosis in cirrhosis and hepatic encephalopathy (HE). However due to inherent cognitive dysfunction, insight into HRQOL severity in patients with liver disease may be impaired.
Aim
To assess insight into HRQOL using PROMIS tools compared to norms in cirrhotic patients.
Methods
PROMIS tools are validated HRQOL instruments that test the domains of anger, anxiety, depression, physical function, pain behavior/impact, sleep disturbances/impairment, and social activities/roles, compared to US-norms. Patients were administered the PROMIS tools, the results of which were reviewed using a visual comparison with thed norms. Then two Likert scales from 0–10 per domain were administered that inquired about (1) Surprise Intensity: 0–4: not surprised, 5–10: surprised; and (2) Expectancies: 0–4: results better than expected, 5:10: as/worse than expected. Comparisons between HE/no-HE were also performed.
Results
203 cirrhotic patients (57 yrs, 62% men, MELD 12, 83 HE) were included. All HE patients were controlled on therapy. Prior HE patients were significantly impaired on all PROMIS domains (p<0.01) except anger, compared to the rest. The majority (76–85%) were not surprised with their placement vis-à-vis the norms. Similarly, a majority (59–61%) thought their results were worse or as expected. However, a third of patients found that their PROMIS results were better than expected. Prior HE status did not significantly impact expectations or surprise based on placement with the norms.
Conclusions
The majority of cirrhotic patients, regardless of prior HE, have good insight regarding their HRQOL issues.
Keywords: PROMIS, health-related quality of life, cognition, sleep
Background
Patients with cirrhosis, especially those with hepatic encephalopathy (HE), have a multi-faceted impairment in their health-related quality of life (HRQOL)(Arguedas et al. 2003). This impaired HRQOL is an important patient-reported outcome (PRO) that determines daily function and prognosis, as well as burden on their caregivers and the healthcare system (Bajaj et al. 2011b; Kanwal et al. 2009). While PROs are subjective, their interpretation in the context of normative values is especially relevant in HE, where cognitive impairment may hinder insight (Riggio et al. 2011). This insight limitation has been reported earlier regarding driving capabilities (Bajaj et al. 2008). The Patient Reported Outcomes Measurement Information System (PROMIS) is a HRQOL evaluation that is based on extensive norms (Liu et al. 2010). These span several domains, and have been validated in cirrhosis (Bajaj et al. 2011a). PROMIS results are shown in a user-friendly, graphical format that can be readily interpreted in the context of age and gender-based US norms.
We hypothesized that prior HE patients will have poor insight into their HRQOL using the PROMIS results in the US-norms context. Our aim was to define patient insight regarding their HRQOL using the PROMIS norms.
Methods
Outpatients with cirrhosis were enrolled in at VCU and McGuire VA Medical Center after informed consent. Cirrhosis was diagnosed based on biopsy, radiological, or history of frank decompensation (HE, ascites, variceal bleeding). Patients who were unable to consent, had abused alcohol or illicit drugs within 3 months and those with a mini-mental status exam score of <25 were excluded. Patients were administered the Psychometric Hepatic Encephalopathy Score subtests (PHES) and based on our norms, covert HE (CHE) was diagnosed (Allampati et al. 2016; Vilstrup et al. 2014).
Demographic data, HE status, current medications and cirrhosis severity data were obtained. Prior HE was defined as ≥1 episode of overt HE grade 2 or higher that resulted in hospitalization and treatments such as lactulose and/or rifaximin therapy(Vilstrup et al. 2014). All patients then underwent the computerized adaptive format of PROMIS assessing HRQOL in 11 domains: anger, anxiety/fear, depression/sadness, physical function, pain behavior, pain impact, sleep disturbances, fatigue, sleep-related impairment, satisfaction with discretionary social activities and satisfaction with social roles. More details and a typical result printout of PROMIS CAT are in the supplementary data
They were asked to complete two 10-point Likert scales per PROMIS domain (one related to degree of surprise and second related to result “expectancy”) regarding their perception of HRQOL compared to the PROMIS profile results (Supplementary information). On the surprise question, scores between 0 and 4 indicated no surprise, while >5 represented a high intensity of surprise. On the “expectedness” question, 0–4 showed their placement was better than expected while 5–10 was as expected, or worse than expected. Sub-analyses between those with/without prior HE and with/without CHE were performed. Patients who were not surprised in all domains and whose results turned out to be better than expected in all domains were studied separately.
Statistical analysis was performed using t-tests between patients with and without prior HE on clinical and continuous PROMIS variables. Chi-square tests were used to compare proportion of patients surprised >5, those who had expected the results, and those whose results turned out to be better, were compared against patients with and without prior HE or CHE.
The protocol was approved by the VCU and VA Medical Center IRB.
Results
205 patients (83 with HE) were enrolled. As expected, there were significant differences in cirrhosis severity, CHE diagnosis and cognitive testing, cirrhosis-associated medication use and in most aspects of PROMIS in patients with a prior history of HE (Table 1). However, no significant differences in psychoactive or pain medications were noted.
Table 1.
Characteristics of patients with and without prior HE
| No-HE (n=122) | Prior HE (n=83) | |
|---|---|---|
| Age | 56.1±6.9 | 58.4±6.7* |
| Gender (M/F) | 67/55 | 59/24* |
| Education (yrs) | 13.9±5.3 | 13.6±2.4 |
| MELD score | 11.6±4.9 | 16.0±5.8*** |
| Serum sodium | 139.7±3.0 | 137.7±4.7*** |
| Serum albumin | 3.8±0.6 | 3.3±0.6*** |
| Lactulose only | - | 34 |
| Rifaximin only | - | 6 |
| Lactulose+Rifaximin | - | 33 |
| SSRI | 16 | 15 |
| Other anti-depressants | 11 | 10 |
| Anti-anxiety | 11 | 11 |
| Anti-seizure | 2 | 1 |
| Anti-psychotic | 2 | 2 |
| Opioids | 10 | 11 |
| NSAIDs | 10 | 9 |
| Non-selective beta-blockers | 29 | 38 |
| Cognitive testing | ||
| Number connection-A (sec) | 30.2±10.5 | 48.3±23.5*** |
| Number connection-B (sec) | 75.4±35.8 | 142.9±93.4*** |
| Digit Symbol test | 65.9±17.6 | 47.3±16.3*** |
| Line tracing errors | 26.8±26.9 | 33.6±29.2 |
| Line tracing time (sec) | 85.5±24.0 | 120.3±61.5*** |
| Serial dotting test (sec) | 56.2±14.0 | 88.3±97.5** |
| Total median PHES score | 0 | −5 |
| CHE n (%) | 37 (30%) | 52 (63%) |
| PROMIS results | ||
| Anger | 48.8±9.5 | 49.0±8.9 |
| Anxiety | 51.3±7.9 | 53.9±7.7* |
| Depression | 48.4±8.5 | 50.7±8.4* |
| Fatigue | 52.1±10.2 | 56.7±8.9** |
| Pain behavior | 49.3±10.2 | 55.1±8.0*** |
| Pain interference | 50.6±10.5 | 56.6±9.5*** |
| Physical Function | 46.2±9.7 | 38.3±6.5*** |
| Social activity | 53.9±37.4 | 43.6±7.1** |
| Social roles | 48.4±10.1 | 41.6±6.5*** |
| Sleep disturbance | 52.3±10.8 | 56.9±9.2** |
| Wake disturbance | 51.1±11.4 | 56.6±9.7*** |
| Better than expected? (no. of patients) | ||
| Anger | 40 | 30 |
| Anxiety | 39 | 25 |
| Depression | 45 | 35 |
| Fatigue | 52 | 27 |
| Pain behavior | 51 | 30 |
| Pain interference | 48 | 32 |
| Physical Function | 43 | 24 |
| Social activity | 48 | 31 |
| Social roles | 47 | 30 |
| Sleep disturbance | 49 | 32 |
| Wake disturbance | 52 | 33 |
| Surprised? (no. of patients) | ||
| Anger | 28 | 25 |
| Anxiety | 26 | 26 |
| Depression | 27 | 18 |
| Fatigue | 25 | 19 |
| Pain behavior | 18 | 19 |
| Pain interference | 15 | 17 |
| Physical Function | 20 | 11 |
| Social activity | 17 | 13 |
| Social roles | 17 | 13 |
| Sleep disturbance | 23 | 15 |
| Wake disturbance | 24 | 13 |
While the overall PROMIS scores were significantly worse in patients with prior HE, there was no significant impact of this status on the patients reaction to their scores respective to the US norms, high score on digit symbol test indicates good performance; low score on the remaining cognitive tests indicates the same;
p<0.05,
p<0.01,
p<0.001
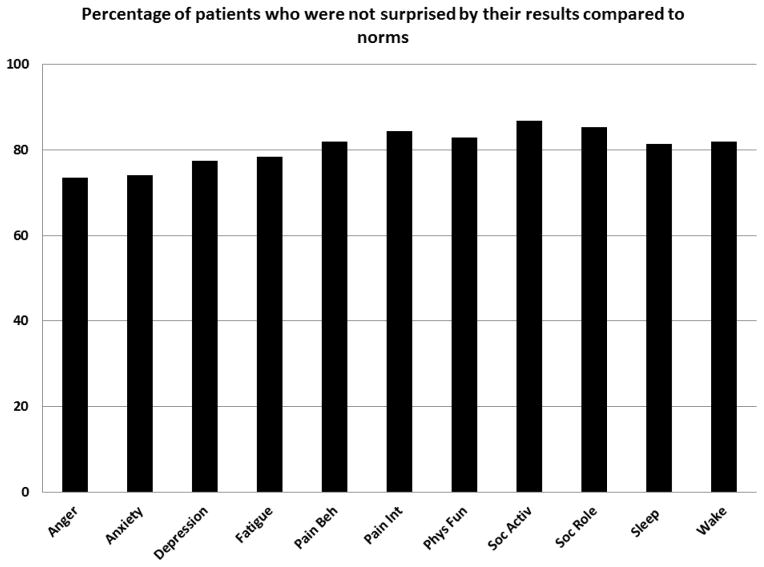
When asked about surprise at their PROMIS profile, the majority of subjects were not surprised (74–85% depending on domain, Figure 1A). The minority who did express surprise had the highest surprise regarding their PROMIS anger and anxiety scale scores; and the lowest regarding their social roles, activities and pain interference. None of the patients were surprised regarding their results in all 11 domains.
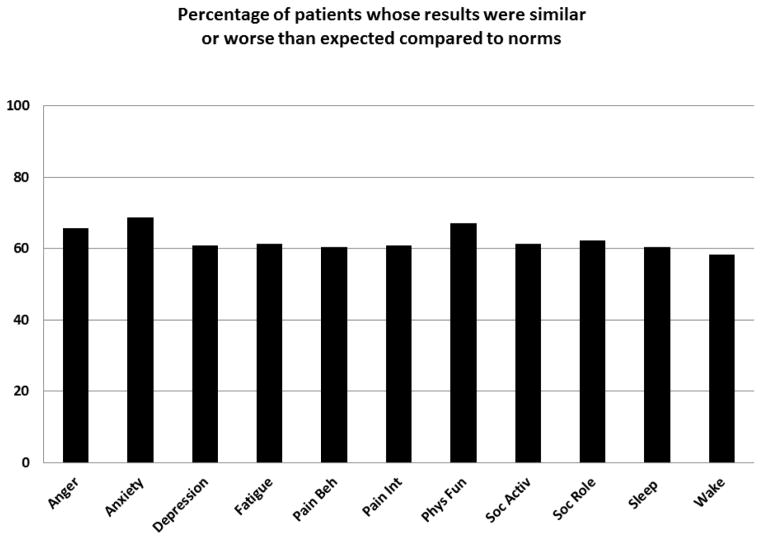
Figure 1.
Figure 1A: Percentage of patients that were surprised by their placement within the PROMIS norms
Figure 1B: Percentage of patients who found their results to be worse or as expected compared to the PROMIS norms
Pain Beh: pain behavior, Pain Int: Pain intereference, Soc Activ: Social Activity, Soc Role: Social Role, Sleep: Sleep disturbances, Wake: Sleep-related impairment.
When the subjects were asked whether they thought their results were either better or worse than expected compared to the US norms, the majority thought their PROMIS scale profile was what they expected or worse than they had anticipated (59–69%). However, almost a third of patients found that their HRQOL PROMIS profile was actually better than they had expected. Fifty-one patients (21 prior HE) found that their PROMIS performance on all domains was significantly better than norms. There was no significant difference in demographics, duration of HE or cirrhosis diagnosis, diagnosis of CHE, disease or medication use between those patients compared to the rest (Supplementary table 1).
The proportion of patients who expressed surprise and had over-estimated the HRQOL PROMIS profile compared to norms was statistically similar between those with/without prior HE and CHE (Supplementary table 1).
Discussion
Patient-reported outcomes are critically important in determining the course of the disease and potential acceptance of therapies. The PROMIS results parallel legacy instruments in cirrhosis across several aspects of HRQOL (Bajaj et al. 2011a). Due to the extensive US-based norms, a visual comparison of the personal responses in the context of the norms could potentially enhance insight regarding the extent of suffering (Liu et al. 2010).
Insight is a clinical construct that is useful to clinicians in understanding a patient’s difficulty in appreciating their illness and its consequences. Poor insight can be seen as a patient’s inability to match their perception of sickness impact with that of available objective medical data. Impaired illness insight has been linked to medication non-adherence and poor treatment outcomes (Amador et al. 1994; Buckley et al. 2007). However, investigation into the insight or a meaningful comparison of these PROs to a large normative sample has not been performed systematically in cirrhosis. We used a limited definition of insight manifested as surprise on comparison with norms. Studies directly comparing insight into PROMIS are lacking in healthy controls but since PROMIS instruments. Healthy subjects have good insight into most “legacy” instruments, which are correlated with PROMIS, but dedicated studies are needed.
When compared to a U.S. census-matched normative sample, most patients had robust insight and indeed were not surprised by their PROMIS scale elevations regardless of whether they had a history of HE or not. However, the PROMIS normative procedure also included a proportion of diseased individuals in selected domains. This inclusion could have tempered these findings, however, the remarkable consistency in the insight between all domains suggests that this impact may be minimal. Roughly a third of our study subjects over estimated their degree of lifestyle disruption and emotional suffering. Of these, 51 patients actually overestimated their HRQOL responses in all domains compared to the norms. This could be potentially due to a psychological tendency to excessively focus on the sensation or issue causing the problem (rumination), exaggerate its threat (magnification), and perceive oneself as being helpless to control the physical/emotional symptoms (Sullivan et al. 2001). This tendency to overestimate sickness impact could further impair the patients’ daily functioning and increase reliance on health services. Importantly, none of the clinical predictors could identify which subjects would consider themselves better, or worse off, then their objective PROMIS profile results. Therefore, while most cirrhotic patients have good insight regarding their HRQOL, the PROMIS, with its large U.S. census matched normative database represents a more reliable and valid methodology to assess HRQOL in liver disease patients.
Contrary to our hypothesis, we did not find any psychological insight differences in patients with and without prior HE or those with CHE. This indicates a personal assessment of quality of life domains using the PROMIS transcends the potential impact of cognitive impairment and greater disease severity or cognitive impairment inherent in these groups(Umapathy et al. 2014). The similarity in psychological insight between patients with and without a prior history of HE may be explained by the fact that no subjects had evidence of active HE at the time of testing, and all subjects had similar psychotropic medication profiles.
Since PROs are the sum total of the immediate and prior disease impact, along with the emotional response to the disease, simply putting these results in context with others may not facilitate a personal understanding of the issues at hand. However, the use of the PROMIS as an intervention tool could improve insight, and ultimately increase social function and treatment adherence. In support of the notion that real world feedback facilitates greater understanding of sickness impact, a prior study demonstrated improved psychological insight in cirrhotic patients when confronted by visual-motor planning and judgment errors associated with a driving simulation(Bajaj et al. 2012). Future studies focusing on repeat PROMIS administration may serve to clarify treatment response and improve allocation of medical resources.
We conclude that the majority of cirrhotic patients have good insight into the daily functional disturbances compared to the US norms, regardless of the prior HE status. However, almost a third of patients with cirrhosis overestimate their HRQOL concerns. The use of PROMIS tools in the US-norms context could help patients and clinicians facilitate an appreciation of their unique HRQOL profile, enhancing referral for appropriate treatments.
Supplementary Material
Supplementary Table 1: PROMIS Reaction between patients with and without covert HE
Acknowledgments
This work was partly supported by grants RO1DK089713 (NIDDK NIH) and CX10076 (VA Merit Review) awarded to JSB and from the McGuire Research Institute.
References
- Allampati S, et al. Diagnosis of Minimal Hepatic Encephalopathy Using Stroop EncephalApp: A Multicenter US-Based, Norm-Based Study. Am J Gastroenterol. 2016;111:78–86. doi: 10.1038/ajg.2015.377. [DOI] [PubMed] [Google Scholar]
- Amador XF, Flaum M, Andreasen NC, Strauss DH, Yale SA, Clark SC, Gorman JM. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994;51:826–836. doi: 10.1001/archpsyc.1994.03950100074007. [DOI] [PubMed] [Google Scholar]
- Arguedas MR, DeLawrence TG, McGuire BM. Influence of hepatic encephalopathy on health-related quality of life in patients with cirrhosis. Dig Dis Sci. 2003;48:1622–1626. doi: 10.1023/a:1024784327783. [DOI] [PubMed] [Google Scholar]
- Bajaj JS, Saeian K, Hafeezullah M, Hoffmann RG, Hammeke TA. Patients with minimal hepatic encephalopathy have poor insight into their driving skills. Clin Gastroenterol Hepatol. 2008;6:1135–1139. doi: 10.1016/j.cgh.2008.05.025. quiz 1065. [DOI] [PubMed] [Google Scholar]
- Bajaj JS, et al. Driving simulation can improve insight into impaired driving skills in cirrhosis. Dig Dis Sci. 2012;57:554–560. doi: 10.1007/s10620-011-1888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj JS, et al. PROMIS computerised adaptive tests are dynamic instruments to measure health-related quality of life in patients with cirrhosis. Aliment Pharmacol Ther. 2011a;34:1123–1132. doi: 10.1111/j.1365-2036.2011.04842.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj JS, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol. 2011b;106:1646–1653. doi: 10.1038/ajg.2011.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley PF, Wirshing DA, Bhushan P, Pierre JM, Resnick SA, Wirshing WC. Lack of insight in schizophrenia: impact on treatment adherence. CNS Drugs. 2007;21:129–141. doi: 10.2165/00023210-200721020-00004. [DOI] [PubMed] [Google Scholar]
- Kanwal F, et al. Health-related quality of life predicts mortality in patients with advanced chronic liver disease. Clin Gastroenterol Hepatol. 2009;7:793–799. doi: 10.1016/j.cgh.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Liu H, Cella D, Gershon R, Shen J, Morales LS, Riley W, Hays RD. Representativeness of the Patient-Reported Outcomes Measurement Information System Internet panel. J Clin Epidemiol. 2010;63:1169–1178. doi: 10.1016/j.jclinepi.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggio O, Ridola L, Pasquale C, Nardelli S, Pentassuglio I, Moscucci F, Merli M. Evidence of persistent cognitive impairment after resolution of overt hepatic encephalopathy. Clin Gastroenterol Hepatol. 2011;9:181–183. doi: 10.1016/j.cgh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. 2001;91:147–154. doi: 10.1016/s0304-3959(00)00430-9. [DOI] [PubMed] [Google Scholar]
- Umapathy S, Dhiman RK, Grover S, Duseja A, Chawla YK. Persistence of cognitive impairment after resolution of overt hepatic encephalopathy. Am J Gastroenterol. 2014;109:1011–1019. doi: 10.1038/ajg.2014.107. [DOI] [PubMed] [Google Scholar]
- Vilstrup H, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715–735. doi: 10.1002/hep.27210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: PROMIS Reaction between patients with and without covert HE