Abstract
Sober living houses (SLHs) are alcohol and drug-free living environments for individuals in recovery. The goal of this study was to map the distribution of SLHs in Los Angeles (LA) County, California (N=260) and examine neighborhood correlates of SLH density. Locations of SLHs were geocoded and linked to tract-level Census data as well as to publicly available information on alcohol outlets and recovery resources. Neighborhoods with SLHs differed from neighborhoods without them on measures of socioeconomic disadvantage and accessibility of recovery resources. In multivariate, spatially-lagged hurdle models stratified by monthly fees charged (less than $1400/month vs. $1400/month or greater), minority composition and accessibility of treatment were associated with the presence of affordable SLHs. Accessibility of treatment was also associated with the number of affordable SLHs in those neighborhoods. Higher median housing value and accessibility of treatment were associated with whether a neighborhood had high-cost SLHs, and lower population density was associated with the number of high-cost SLHs in those neighborhoods. Neighborhood factors are associated with the availability of SLHs, and research is needed to better understand how these factors affect resident outcomes, as well as how SLHs may affect neighborhoods over time.
Keywords: recovery housing, recovery residences, sober living houses, neighborhood characteristics, recovery resources
For many individuals with substance use disorders, attempts to recover from addiction often are undermined by precarious living arrangements or environments where substance use is highly prevalent (Evans, Li, Buoncristiani, & Hser, 2014; Havassy, Hall, & Wasserman, 1991; Linton, Celentano, Kirk, & Mehta, 2013). Sober living houses (SLHs) are an excellent option for these individuals because they offer affordable alcohol- and drug-free housing and social support for sustained abstinence (Polcin & Henderson, 2008).
In California, where many studies have been conducted, SLHs do not provide treatment or formal programming. However, residents are either encouraged or required to attend 12-step meetings to help maintain abstinence. Although SLHs typically have a staff member who is responsible for overseeing the day-to-day management of the house, a social model philosophy of recovery is promoted that emphasizes resident input into house operations and management, peer support for recovery, financial self-sufficiency, and resident responsibility for maintaining the facility (Borkman, Kaskutas, Room, Bryan, & Barrows, 1998; Kaskutas, 1998). Residents of SLHs can stay as long as they wish, provided they abide by house rules (such as maintaining abstinence from alcohol and drugs) and pay monthly fees that cover renting a room (often shared) in a furnished house, utilities, and other basic household expenses. SLHs can be used by persons in recovery at a variety of time points, including after residential treatment, during outpatient treatment, after release from incarceration, or as an alternative to formal treatment (Polcin, 2006; Polcin & Henderson, 2008).
There is growing evidence of the important role recovery residences such as SLHs play in promoting recovery from addiction (Jason, Mericle, Polcin, & White, 2013). For example, in a study tracking the functioning of 300 individuals residing in 20 different SLHs over an 18-month period, Polcin et al. (2010a; 2010b) found residents showed significant improvement on a wide variety of outcomes including reduced alcohol and drug use, alcohol- and drug-related problems, psychiatric symptoms, unemployment, and arrests. All improvements between baseline and 6-month follow-up were maintained at 12- and 18-month follow-up even though the vast majority of residents had left the SLHs by 18 months. Factors that predicted positive outcomes were social network characteristics and 12-step involvement, but factors pertaining to the neighborhoods in which the houses were located were not examined. This is an unfortunategap in knowledge. Analysis of neighborhood factors could lead to the identification of neighborhood-level risk and protective factors for resident relapse and to specification of best practice guidelines for where to locate SLHs and other types of recovery residences.
Relapse prevention interventions are predicated on helping individuals recognize and manage “high-risk situations,” but these situations have generally been conceptualized in terms intra- or interpersonal determinants of relapse (Marlatt, 1996; Witkiewitz & Marlatt, 2004) rather than on aspects of the surrounding environment. Moreover, very limited attention has been paid to where substance use services are delivered and how neighborhood factors may affect service use outcomes (Jacobson, 2004). This gap in the literature is surprising given that neighborhood characteristics are increasingly recognized as important determinants of health, more generally, and of substance use, in particular. For example, a variety of studies have shown that neighborhood disadvantage (e.g., neighborhoods characterized by high concentrations of poverty, unemployment, and abandoned buildings) is an important correlate of alcohol and drug use (Boardman, Finch, Ellison, Williams, & Jackson, 2001; Furr-Holden et al., 2011; Karriker-Jaffe, 2013; Latkin, Williams, Wang, & Curry, 2005), substance use disorders (Molina, Alegría, & Chen, 2012), and drug-related mortality (Hannon & Cuddy, 2006). Other neighborhood characteristics such as perceived drug availability (Bradizza & Stasiewicz, 2003; Lambert, Brown, Phillips, & Ialongo, 2004) and alcohol outlet density (Duncan, Duncan, & Strycker, 2002; Scribner, 2000) have also been identified as risk factors for substance use.
Although much less research has focused on neighborhood characteristics that deter substance use or that promote recovery, the notion of community recovery capital has been put forward to describe the resources available (e.g., treatment and self-help resources, as well as other community support institutions) to promote the resolution of alcohol and drug problems (White & Cloud, 2008). Indeed, there is evidence to suggest that proximity to treatment (Ross & Turner, 1994) and to self-help resources (Stahler, Mennis, Cotlar, & Baron, 2009) are related to treatment continuity following inpatient treatment, suggesting that a higher concentration of treatment and self-help resources in neighborhoods in which SLHs are located would be beneficial to residents and SLH operators.
Recovery residence operators commonly report barriers to opening houses in certain residential neighborhoods (Mericle, Miles, & Way, 2015; Troutman, 2014) and clustering of residences in particular areas has been also observed (Johnson, Marin, Sheahan, Way, & White, 2009). However, it is currently unknown what type of neighborhoods they are located in and whether it is better for them to be located in more affordable, low-income areas (where drug problems may be higher) or in middle-class neighborhoods where rent may be more expensive (but where drug problems may be reduced). Houses located in middle- or upper-income areas might feel foreign to low-income residents or be too removed from a culture to which they are accustomed. Ferrari et al. (Ferrari, Groh, & Jason, 2009) studied a relatively homogeneous sample of recovery residences across the US and did not find outcome differences by economic status of the neighborhood. However, in addition to limited variability of houses and neighborhoods, that study did not assess other potentially important neighborhood characteristics such as density of alcohol outlets or nearby treatment and self-help resources.
Understanding characteristics of neighborhoods in which SLHs are located is an important first step in examining how these characteristics may affect the residents living in them. LA County is an ideal location in which to explore neighborhood correlates of SLHs due to its large and diverse geographic and population characteristics, as well as the large number of SLHs and the diversity in monthly fees charged to residents to live in them. Using data on the location of SLHs in LA County, the aims of this exploratory study were: (1) to map and describe the distribution of SLHs; (2) to examine differences between LA neighborhoods with and without SLHs with respect to neighborhood socioeconomic status (resident and housing characteristics that would be indicative of neighborhood disadvantage), alcohol outlets, and treatment and self-help resources; and (3) to identify correlates of the presence and density of SLHs and to examine whether these neighborhood correlates vary depending on the amount of monthly fees charged.
Method
Data Sources
Information on the locations of and costs associated with SLHs in LA County were provided by the Sober Living Network in the summer of 2015. The Sober Living Network is a nonprofit organization dedicated to promoting excellence in the operation and management of sober living and other community recovery support resources in Southern California. It is comprised of five county-level coalitions, and it oversees each coalition’s application, quality control, inspection, and membership certification procedures. There are 500 member houses in Southern California, with the majority of these in LA County. The Sober Living Network is an affiliate of the National Alliance for Recovery Residences (NARR) and implements NARR housing standards that are used in recovery residences across the US.
We defined neighborhoods according to US census tracts, which are effective for delineating contextual determinants of health and substance use (Karriker-Jaffe, 2011; Krieger et al., 2002). Data on neighborhood characteristics were drawn from the 2010 Decennial Census and 2006–2010 American Community Survey (ACS), each collected by the US Bureau of the Census. The 2010 Census provided a limited set of population characteristics at the census tract level, and this was supplemented with additional 5-year, small-area estimates from the ACS. Data were purchased from ESRI (2016).
Information on alcohol outlets and recovery resources came from a variety of sources. Information on alcohol outlets came from the California Alcoholic Beverage Commission (California Department of Alcoholic Beverage Control, 2012), which maintains and makes publically available data on alcohol outlet locations, including census tract, licensure type and status (whether a license is active or not). Data were downloaded in the fall of 2014. Information on substance abuse treatment resources came from the SAMHSA’s treatment locator website (Substance Abuse and Mental Health Services Administration, 2015a), which provides regularly-updated information on mental health and substance abuse treatment programs to the general public. Information on locations of self-help resources came from a compilation of online 12-step meeting schedules for 7 different types of groups including Alcoholics Anonymous (AA), Narcotics Anonymous (NA) and Smart Recovery, following links available from the Substance Abuse and Mental Health Services Administration (Substance Abuse and Mental Health Services Administration, 2015b). These schedules were augmented with information on AA meetings for the greater LA area (Alcoholics Anonymous Central Office of Los Angeles, 2015). Data on treatment and self-help resources were downloaded in the summer of 2014.
Measures
SLH density
SLH density represents the number of SLHs within each census tract. Using the definition provided by the Department of Housing and Urban Development (HUD) that defines affordable housing as housing for which the occupant is paying no more than 30 percent of his or her income for gross housing costs (U.S. Department of Housing and Urban Development & Office of Policy Development and Research, 2015) and census data on median household income in LA County, we created separate variables to reflect the number of “affordable” and “high-cost” SLHs in each neighborhood. Affordable SLHs charged monthly fees of below $1400 (i.e., less than 30% of the median monthly household income in LA County) and high-cost SLHs charged monthly fees of $1400 or more. We also created variables to indicate whether a neighborhood had any affordable or any high-cost SLHs at all.
Neighborhood resident demographics and housing characteristics
Resident demographics included tract-level data on total population, population density (number of residents per square mile), percent of residents of different racial/ethnic identities (White, Black/African American, Hispanic/Latino, Asian), percent of residents over age 25 without a high school degree, unemployment rate among residents over age 16, and percent of residents living below the national poverty level. Neighborhood housing characteristics included median housing value and housing unit vacancy rate.
Alcohol outlet density
We included tract-level counts of bars as well as outlets in which alcohol is sold to be consumed off premises (e.g., liquor stores, convenience stores, and grocery stores).
Treatment resources and self-help resources
The number of treatment facilities in each tract included all inpatient and outpatient locations offering alcohol, drug, methadone or detoxification treatment. Self-help resources were separated into AA and other (NA, Marijuana Anonymous, Cocaine Anonymous, Crystal Meth Anonymous, Dual Recovery Anonymous, and Smart Recovery) self-help meetings. We included tract-level counts of the number of meetings per week.
Analyses
Descriptive analyses were used to summarize the number of neighborhoods with SLHs and the number of SLHs present in those neighborhoods, as well as the number and characteristics of affordable and high-cost SLHs in the sample and the number of neighborhoods in which these were located. Difference in means tests (i.e., independent t-tests with unequal variances) were run to compare characteristics of neighborhoods with SLHs to those without SLHs.
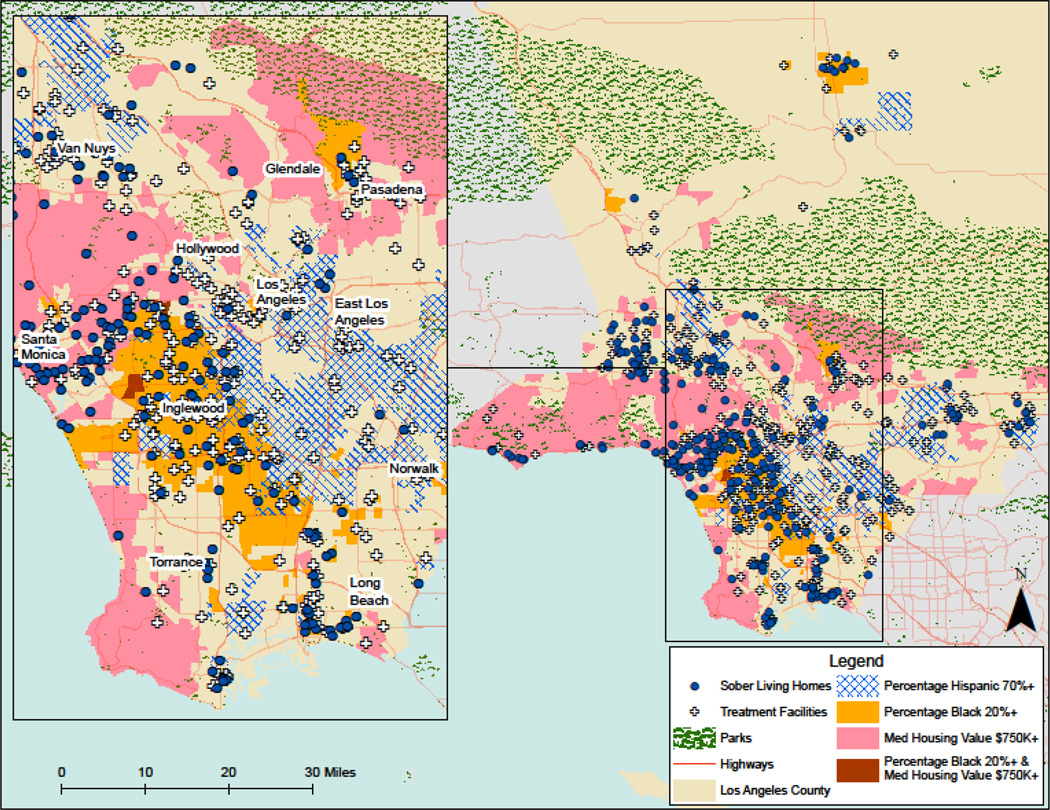
Locations of SLHs, alcohol outlets, treatment facilities and self-help resources were geocoded using ArcGIS 10.2 (ESRI, 2013). We mapped these locations to visually display where houses were located in relation to treatment programs and with respect to selected geographic markers (e.g., parks, highways, community boundaries) and neighborhood characteristics (e.g., concentrations of racial/ethnic minorities and median housing values) in LA County. We generated a contiguity-based queen weights matrix to characterize the adjacency of neighborhoods; this includes all neighborhoods that share borders as well as those that share corner points. Clustering (i.e., global spatial autocorrelation) of SLHs among neighborhoods was assessed using Moran’s I (Moran, 1950).
Our analyses of SLH density were stratified to separately examine geographic correlates of affordable and high-cost SLHs. Neighborhoods with no housing units (n=11) were dropped from these analyses. We implemented a hurdle approach (Mullahy, 1986), where we used logistic regression models to examine factors related to whether a neighborhood had any affordable or high-cost SLHs with a second set of zero-truncated Poisson models to examine factors related to the number of houses of each type in neighborhoods with either affordable or high-cost houses.
Following the general variable selection strategy outline by Hosmer & Lemeshow (2000), our model-building proceeded in stages. To assess the nature and strength of the relationship between each characteristic and the dependent variable in question, we first ran bivariate analyses. Characteristics significantly associated (p<0.05) at the bivariate level were then entered into a simultaneous regression model to assess their relative strength. Due to the exploratory nature of our analyses, we did not make corrections for the number of tests performed, but we did use the traditional p-value (0.05) for variable selection rather than using a higher level as suggested in the literature (e.g., p<0.25; Hosmer & Lemeshow, 1989; Mickey & Greenland, 1989).
Values for the neighborhood characteristics, alcohol outlet density, self-help and treatment resources were standardized for comparability, and model coefficients were reported as odds ratios (logistic models) or incident rate ratios (count models). In models examining correlates of SLH density, spatial autocorrelation was modeled as a function of either the presence or the number of SLHs in adjacent neighborhoods (Ward & Gleditsch, 2008) through inclusion of a covariate derived from the spatial weights matrix representing the spatially-lagged dependent variable (rho) in the model. Our count models also included an exposure parameter based on the natural log of housing units in each neighborhood (constrained to 1). All analyses were conducted in Stata (Stata Corp., 2015), which includes routines for assessing spatial autocorrelation (Pisati, 2001) and the creation of spatially-lagged variables (Drukker, Peng, Prucha, & Raciborski, 2013).
Results
A total of 260 SLHs in LA County were active members of the Sober Living Network during the study period. These houses were present in 9% (206/2343) of LA neighborhoods. Among the neighborhoods with SLHs, the number of houses in a neighborhood ranged from 1 to 6, with average of 1.26 (SD=0.66) houses per neighborhood. Information on monthly fees was missing on 18 houses located in 18 different neighborhoods. A total of 174 houses charged monthly fees below $1,400/month; these were present in 145 neighborhoods. Fees charged in these houses ranged from $300/month to $1,350/month, with an average of $650/month. High-cost houses (n=68) which charged monthly fees of $1,400 or higher were found in 49 neighborhoods. Fees charged in these high-cost houses ranged from $1,500/month to $10,000/month, with an average of $4,555/month. There were no differences on gender served between affordable and high-cost SLHs. Most SLHs in LA County (53%) served males; 24% were co-ed and 23% housed females only. On average, affordable (compared to high-cost) SLHs had significantly more residents living in them (14 vs. 11).
Table 1 compares neighborhoods with SLHs to those without them. On average, neighborhoods with SLHs had significantly more residents who were African American (13.6% vs 8.1%), fewer residents who were Hispanic (41.4% vs 47.7%) or Asian (8.7% vs. 14.1%), and fewer residents who had not graduated from high school by age 25 (22.7% vs 26.2%). Compared to those without SLHs, neighborhoods with SLHs also had, on average, higher median home values ($552,275 vs $509,417) and higher vacancy rates (6.8% vs. 5.7%), as well as more off-premise alcohol outlets (3.0 vs 2.6), more treatment facilities (0.4 vs 0.2), and more AA (2.5 vs. 1.1) and other self-help meetings (0.8 vs 0.3) each week.
Table 1.
Characteristics of Neighborhoods with and without Sober Living Houses (SLHs) in LA County (N=2343)
| All Neighborhoods in LA County (N=2343) |
Neighborhoods with SLHs (N=206) |
Neighborhoods without SLHs (N=2137) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | t | df | p | |
| Resident characteristics | |||||||||
| Total population | 4190.6 | (1491.9) | 4355.6 | (1309.6) | 4174.7 | (1507.6) | −1.9 | 260.3 | |
| Population density | 13091.6 | (10891.2) | 13050.1 | (9260.3) | 13095.6 | (11037.6) | 0.1 | 264.5 | |
| Racial/ethnic composition | |||||||||
| % Hispanic | 47.1 | (29.1) | 41.4 | (24.9) | 47.7 | (29.4) | 3.4 | 263.6 | *** |
| % White (non-Hispanic) | 28.6 | (26.6) | 33.9 | (28.1) | 28.1 | (26.5) | −2.8 | 241.6 | ** |
| % African American/Black | 8.6 | (13.4) | 13.6 | (16.6) | 8.1 | (12.9) | −4.6 | 229.8 | *** |
| % Asian | 13.6 | (15.6) | 8.7 | (7.7) | 14.1 | (16.0) | 8.5 | 408.7 | *** |
| % w/o high school diploma | 25.9 | (19.2) | 22.7 | (16.7) | 26.2 | (19.4) | 2.9 | 260.5 | ** |
| % Unemployed | 8.8 | (4.5) | 9.2 | (4.1) | 8.8 | (4.5) | −1.2 | 2315.0 | |
| Median household income | 60317.8 | (29739.4) | 61370.3 | (32960.3) | 60215.6 | (29414.3) | −0.5 | 2313.0 | |
| % Below poverty | 16.0 | (12.2) | 17.1 | (12.1) | 15.9 | (12.2) | −1.4 | 2316.0 | |
| Housing characteristics | |||||||||
| Median home value | 513270.1 | (199823.9) | 552275.0 | (236662.0) | 509417.1 | (195454.6) | −2.5 | 230.0 | * |
| Vacancy rate | 5.8 | (4.4) | 6.8 | (4.5) | 5.7 | (4.3) | −3.5 | 2330.0 | *** |
| Availability of alcohol outlets | |||||||||
| Number of active alcohol outlets | 10.2 | (15.0) | 12.0 | (19.9) | 10.0 | (14.4) | −1.4 | 226.1 | |
| Number of bars | 0.5 | (1.0) | 0.6 | (1.0) | 0.4 | (1.0) | −1.4 | 240.1 | |
| Number of off-premises alcohol outlets | 2.6 | (2.3) | 3.0 | (2.6) | 2.6 | (2.3) | −2.4 | 234.9 | * |
| Accessibility of recovery resources | |||||||||
| Number of treatment facilities | 0.2 | (0.5) | 0.4 | (1.0) | 0.2 | (0.5) | −3.4 | 214.2 | *** |
| Number of AA meetings | 1.2 | (4.6) | 2.5 | (7.4) | 1.1 | (4.2) | −2.6 | 218.1 | ** |
| Number of other self-help meetings | 0.4 | (1.4) | 0.8 | (1.9) | 0.3 | (1.3) | −3.4 | 225.1 | *** |
Notes. A total of 260 houses were active members of the Sober Living Network during the study period. These houses were located in 206 different LA neighborhoods.
In addition to visually depicting differences between areas with and without SLHs, Figure 1 shows that SLHs were not dispersed uniformly across the county. SLHs were spatially clustered, primarily in the densely populated southwestern portion of the county. This level of clustering was statistically significant (Moran’s I=0.12, p<.001).
Figure 1.
Distribution of SLHs in Los Angeles County
Table 2 displays the findings from fee-stratified, spatially-lagged bivariate analyses examining factors associated with whether a neighborhood had any SLHs and the number houses in those neighborhoods with at least one SLH. Factors associated with an increased likelihood of a neighborhood having any affordable SLHs (vs. none) included a greater percentage of residents who were African American (OR=1.34, p<0.001), were unemployed (OR=1.17, p=0.032) and had incomes below the poverty level (OR=1.22, p=0.012), as well as greater numbers of treatment facilities (OR=1.32, p<0.001), AA (OR=1.13, p=0.040) and other self-help meetings (OR=1.22, p<0.001). Factors that decreased the likelihood of a neighborhood having any affordable SLHs included higher percentage of Asian residents (OR=0.61, p=0.001) and housing with higher median home values (OR=0.79, p=0.022). Factors associated at the bivariate level with increased numbers of houses in neighborhoods with affordable SLHs included a greater percentage of residents who were unemployed (IRR=1.46, p=0.036) as well as greater number of bars (IRR=1.40, p<0.028), treatment facilities (IRR=1.16, p<0.001), and AA meetings (IRR=1.15, p=0.029).
Table 2.
Spatially-Lagged Bivariate Models Predicting Presence and Counts of Affordable and High-Cost SLHs (N=2332)
| Bivariate Correlates of Affordable SLHs | Bivariate Correlates of High-cost SLHs | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Logistic Regression (N=2332) |
Zero-Truncated Poisson Regression (N=147) |
Logistic Regression (N=2332) |
Zero-Truncated Poisson Regression (N=49) |
|||||||||
| OR | [95% CI] | p | IRR | [95% CI] | p | OR | [95% CI] | p | IRR | [95% CI] | p | |
| Neighborhood resident & housing characteristics |
||||||||||||
| Resident characteristics | ||||||||||||
| Population density | 1.10 | [0.93–1.29] | 0.99 | [0.65–1.53] | 0.53 | [0.33–0.84] | ** | 0.30 | [0.10–0.87] | * | ||
| Racial/ethnic minorities | ||||||||||||
| % Hispanic | 1.07 | [0.90–1.28] | 0.86 | [0.52–1.44] | 0.20 | [0.10–0.39] | *** | 1.18 | [0.35–3.91] | |||
| % African American/Black | 1.34 | [1.19–1.51] | *** | 0.79 | [0.54–1.17] | 0.76 | [0.46–1.24] | 0.37 | [0.05–2.67] | |||
| % Asian | 0.61 | [0.46–0.81] | ** | 1.17 | [0.61–2.23] | 0.73 | [0.46–1.17] | 0.46 | [0.06–3.41] | |||
| % w/o high school diploma | 1.06 | [0.89–1.26] | 0.77 | [0.46–1.30] | 0.21 | [0.11–0.43] | *** | 0.68 | [0.10–4.58] | |||
| % Unemployed | 1.17 | [1.01–1.36] | * | 1.46 | [1.02–2.07] | * | 0.69 | [0.47–1.00] | 0.52 | [0.21–1.29] | ||
| % Below poverty | 1.22 | [1.04–1.42] | * | 0.89 | [0.59–1.34] | 0.56 | [0.35–0.89] | * | 0.81 | [0.33–1.98] | ||
| Housing characteristics | ||||||||||||
| Median home value | 0.79 | [0.65–0.97] | * | 1.23 | [0.84–1.82] | 3.01 | [2.20–4.10] | *** | 1.35 | [0.67–2.74] | ||
| Vacancy rate | 1.08 | [0.94–1.23] | 0.96 | [0.61–1.51] | 1.12 | [0.97–1.30] | 1.29 | [0.94–1.78] | ||||
| Availability of alcohol outlets | ||||||||||||
| Number of bars | 0.95 | [0.80–1.14] | 1.40 | [1.04–1.90] | * | 1.30 | [1.10–1.53] | ** | 1.07 | [0.79–1.45] | ||
| Number of off-premises outlets | 1.16 | [0.99–1.35] | 1.10 | [0.84–1.45] | 1.38 | [1.06–1.79] | * | 0.84 | [0.55–1.29] | |||
| Accessibility of recovery resources | ||||||||||||
| Number of treatment facilities | 1.32 | [1.17–1.49] | *** | 1.16 | [1.09–1.24] | *** | 1.25 | [1.06–1.47] | ** | 1.05 | [0.81–1.36] | |
| Number of AA meetings | 1.13 | [1.01–1.28] | * | 1.15 | [1.01–1.31] | * | 1.19 | [1.00–1.41] | * | 0.92 | [0.70–1.22] | |
| Number of other self-help meetings | 1.22 | [1.10–1.36] | *** | 1.12 | [0.95–1.32] | 1.13 | [0.92–1.40] | 0.70 | [0.38–1.31] | |||
Notes. All models included a spatial lag covariate (rho) representing the spatially-lagged dependent variable. Rho was significant on all bivariate logistic regression models. All zero-truncated Poisson regression models included an exposure variable representing the natural log of the total number of housing units in the neighborhood (constrained to 1) as well as a rho. Rho was not significant in models predicting number of affordable SLHs but was significant in model predicting numbers of high-cost SLHs.
p<0.05;
p<0.01;
p<0.001
Table 2 also displays factors associated at the bivariate level with whether a neighborhood had any high-cost SLHs and with the number of such houses in those neighborhoods with at least one high-cost SLH. Factors associated with an increased likelihood of a neighborhood having any high-cost SLHs (vs. none) included housing with higher median home values (OR=3.01, p<0.001) and greater numbers of bars (OR=1.30, p=0.15), off-premise alcohol outlets (OR=1.38, p=0.015), treatment facilities (OR=1.25, p=0.009), and AA meetings (OR=1.19, p=0.045). Factors that decreased the likelihood of a neighborhood having any high-cost SLHs included greater population density (OR=0.53, p=0.007), high percentage of residents who were Hispanic (OR=0.20, p<0.001), residents without a high-school diploma (OR=0.21, p<0.001), and incomes below poverty (OR=0.56, p=0.014). Only one factor was related to the number of high-cost SLHs in neighborhoods that had these houses: Greater population density was associated with a decreased number of high-cost SLHs (IRR=0.30, p=0.027).
Table 3 includes results from simultaneous multivariate models including all factors associated at the bivariate level with neighborhoods having affordable SLHs. Neighborhoods with a greater percentage of African Americans (OR=1.22, p=0.003) and a greater number of treatment facilities (OR=1.21, p=0.003) were more likely to have affordable SLHs. Neighborhoods with more Asian residents were less likely to have affordable SLHs (OR=0.75, p=0.037). The zero-truncated Poisson model shows a greater number of treatment facilities in a given neighborhood was associated with an increased number of affordable SLHs (IRR=1.12, p=0.044) in the neighborhoods that had at least one. Similarly, Table 4 shows that neighborhoods with higher median home values (OR=2.44, p<0.001) and more treatment facilities (OR=1.27, p=0.011) were more likely to have high-cost SLHs. Only one factor (population density) was entered into the count model, so results are identical to those found in the bivariate model; greater population density was associated with decreased number of high-cost SLHs (IRR=0.30, p=0.027) in neighborhoods that had at least one.
Table 3.
Spatially-lagged Multivariate Hurdle Models Examining Correlates of Affordable SLHs
| OR | [95% CI] | p | |
| Logistic regression model examining correlates of any affordable SLHs (N=2332) | |||
| % Black | 1.22 | [1.07– 1.39] | ** |
| % Asian | 0.75 | [0.57– 0.98] | * |
| % Unemployed | 0.99 | [0.83– 1.19] | |
| % Below poverty | 1.04 | [0.85– 1.26] | |
| Median home value | 0.89 | [0.72– 1.10] | |
| Number of treatment facilities | 1.21 | [1.07– 1.38] | ** |
| Number of AA meetings | 1.07 | [0.93– 1.24] | |
| Number of other self-help meetings | 1.13 | [1.00– 1.28] | |
| Rho (spatially-lagged affordable SLH indicator) | 17.94 | [5.52– 58.28] |
*** |
| Constant | 0.04 | [0.03– 0.06] | *** |
| IRR | [95% CI] | p | |
| Zero-truncated Poisson model examining correlates of affordable SLHs density among neighborhoods with affordable SLHs (N=147) |
|||
| % Unemployed | 1.40 | [0.94– 2.08] | |
| Number of bars | 1.02 | [0.65– 1.58] | |
| Number of treatment facilities | 1.12 | [1.00– 1.26] | * |
| Number of AA meetings | 1.07 | [0.89– 1.29] | |
| Rho (spatially-lagged affordable SLH density) | 1.23 | [0.24– 6.34] | |
| Constant | 0.00 | [0.00– 0.00] | *** |
| Exposure (log of total housing units) | 1.00 | ||
p<0.05;
p<0.01;
p<0.001
Table 4.
Spatially-lagged Multivariate Hurdle Models Examining Correlates of High-cost SLHs
| OR | [95% CI] | p | |
| Logistic regression model examining correlates of any high-cost SLHs (N=2332) | |||
| Population density | 0.99 | [0.61– 1.59] | |
| % Hispanic | 0.55 | [0.18– 1.66] | |
| % w/o high school diploma | 0.75 | [0.22– 2.55] | |
| % Below poverty | 1.24 | [0.74– 2.09] | |
| Median home value | 2.44 | [1.59– 3.73] | *** |
| Number of bars | 1.21 | [0.97– 1.51] | |
| Number of off-premises alcohol outlets | 1.24 | [0.92– 1.67] | |
| Number of treatment facilities | 1.27 | [1.06– 1.54] | * |
| Number of AA meetings | 0.99 | [0.80– 1.24] | |
| Rho (spatially-lagged high-cost SLH indicator variable) | 80.66 | [11.89–547.10] | *** |
| Constant | 0.00 | [0.00– 0.01] | *** |
| IRR | [95% CI] | p | |
| Zero-truncated Poisson model examining correlates of counts of high-cost SLHs among neighborhoods with high-cost SLHs (N=49) |
|||
| Population density | 0.30 | [0.10– 0.87] | * |
| Rho (spatially-lagged high-cost SLH density) | 2.73 | [1.25– 5.94] | * |
| Constant | 0.00 | [0.00– 0.00] | *** |
| Exposure (log of total housing units) | 1.00 | ||
p<0.05;
p<0.01;
p<0.001
Discussion
The aims of this study were to map and describe the distribution of SLHs in LA County, identify correlates of SLH density, and examine whether these neighborhood correlates vary depending on the amount of monthly fees charged. During the study period, a total of 260 SLHs in LA County with a capacity of 3,265 beds were active members of the Sober Living Network. Despite this large number of houses, SLHs were present in only a small fraction (9%) of LA neighborhoods.
Having a safe and stable place to live is integral to recovery from substance use disorders (Substance Abuse and Mental Health Services Administration, 2012), and housing is commonly cited as an important priority among individuals in various stages of recovery (Laudet & White, 2010). Based on findings from the 2013–2014 National Survey on Drug Use and Health, it is estimated that 2,475,000 individuals age 18 or older in California met past-year criteria for a substance use disorder (Substance Abuse and Mental Health Services Administration & Center for Behavioral Health Statistics and Quality, 2015). Approximately 28% of California residents live in LA County (State of California & Department of Finance, 2015), meaning that 693,000 LA County residents likely meet criteria for a past-year substance use disorder. If just 1% of adults in LA County with a substance use disorder needed sober living to support their recovery, need would still exceed the number of available beds by a factor of slightly more than 2 to 1.
In addition to having relatively few SLHs, we found that SLHs were not evenly distributed across LA County, and neighborhoods with SLHs looked different from neighborhoods without them on a variety of dimensions of socioeconomic disadvantage and accessibility to recovery resources. Although affordability is a common hallmark of recovery residences like SLHs (Lo Sasso, Byro, Jason, Ferrari, & Olson, 2012; Mericle, Miles, & Cacciola, 2015), SLHs in LA County are available at a wide range of price points (monthly fees ranged from $300 to $10,000). The vast majority of SLHs on which information on monthly fees was available charged fees that would be considered “affordable,” however 28% charged monthly fees that were greater than 30% of the median monthly income of LA County residents. This diversity allowed us to examine correlates of neighborhoods with high-cost houses separately in models that also adjusted for spatial clustering of SLHs.
A number of factors pertaining to neighborhood socioeconomic disadvantage (population density, percentage of African Americans, rates of poverty and employment, median home values) were associated with the likelihood of whether neighborhoods had affordable or high-cost SLHs. However, the strongest factor associated with affordable SLHs in the multivariate model was the number of neighborhood treatment facilities. A greater number of treatment facilities also was correlated with the number of affordable SLHs in neighborhoods with this type of recovery residence and with neighborhoods having any high-cost SLHs at all. Operating SLHs in close proximity to treatment programs would seem advantageous for SLHs, treatment facilities, and most importantly, SLH residents. Individuals often live in recovery residences like SLHs while in outpatient treatment or to support a lifestyle in recovery upon completion of formal treatment (Mericle & Miles; Polcin et al., 2010a). Availability of SLHs near treatment facilities may enhance the likelihood of treatment completion and lead to better long-term outcomes. Because SLHs do not provide treatment, those with referral relationships with treatment programs may better serve residents who need additional support during their stays.
The co-location of treatment and SLHs may serve as the foundation for recovery-oriented systems of care representing “networks of organizations, agencies, and community members that coordinate a wide spectrum of services to prevent, intervene in, and treat substance use problems and disorders” (Sheedy & Whitter, 2009. p.3). In addition, SLHs embedded within neighborhoods with other treatment and recovery resources may enhance overall community recovery capital (White & Cloud, 2008) and improve neighborhood quality (Jason, Roberts, & Olson, 2005; Mericle, Miles, & Way, 2015). Traditions of helping others and giving back are common in mutual aid fellowships, and studies have found that sobriety is related to involvement in community projects (Zemore & Kaskutas, 2004). In addition to helping foster sobriety, recovery residences like SLHs may also foster second-order neighborhood change through increased community involvement (Jason, Schober, & Olson, 2008). Further research is needed to specifically address this question.
Our findings suggest there may be racial/ethnic communities that are underserved by SLHs. In addition to having a large number of SLHs, LA County is also demographically diverse, which allowed us to examine SLHs within neighborhoods of varying racial/ethnic compositions. We found that many neighborhoods without SLHs had high concentrations of Hispanics (greater than 70% of residents) and that neighborhoods with a greater percentage of Asians were less likely to have affordable SLHs. Although large epidemiologic studies generally find that Hispanics and Asians have a lower prevalence of alcohol (Hasin, Stinson, Ogburn, & Grant, 2007) and drug disorders (Compton, Thomas, Stinson, & Grant, 2007), members of these groups have been found to be less likely to access substance use treatment (Wu, Ringwalt, & Williams, 2003) and have more persistent psychiatric disorders (Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2005). It is possible that these ethnic groups have developed their own recovery support systems within their communities and are simply not a part of the Sober Living Network. For example, anexos, mutual-help recovery programs that provide structured daily routines, peer support, and daily Spanish-language Alcoholics Anonymous (AA) meetings that incorporate cultural elements from AA in Mexico (Garcia, 2015) are known to operate in Los Angeles (A. Pagano, personal communication, February 16, 2016). The experiences of these minority groups in SLHs and potential barriers to opening SLHs in neighborhoods with high concentrations of these groups warrant further study.
Although this study represents the most comprehensive examination to date of the neighborhoods where SLHs are located, it is not without limitations. An important strength of this study is that we had access to information on SLHs from the Sober Living Network, which implements standards for their houses that are used in recovery residences across the US. However, our findings on SLHs are limited to houses that are members of this network. Becoming a member of the Sober Living Network is voluntary and involves undertaking application, inspection, and certification procedures as well as paying annual dues when certified. Certified houses must also conform to membership requirements (e.g., adhering to standards of practice and ethical guidelines, holding general liability insurance, and participating in trainings and local coalition activities). Some houses may call themselves a sober living house but be unaware of the Network or know about it and choose not to become a member. It is impossible to know how many such houses exist, but these houses are likely qualitatively different from SLHs that are members of the network. Other types of recovery residences also may exist in LA County, but they are likely to be few in number. The California Consortium of Addiction Programs and Professionals also certifies affiliated recovery residences that operate in accordance with national recovery housing standards, but members of this organization largely operate in Northern California. There are four Oxford Houses listed as operating in California, but none are in LA County. As mentioned earlier, anexos also operate in LA County but the number and locations of these residences is unknown at this time.
Another limitation to this study is its exploratory nature. Due to the dearth of literature on neighborhoods in which recovery residences are located, we did not have a priori hypotheses about what neighborhoods with SLHs may look like. However, because we did focus our attention on neighborhood factors associated with alcohol and drug use, drug-related mortality, and improved substance use treatment outcomes, it possible that we failed to examine certain neighborhood characteristics that are common among those with SLHs or may otherwise influence the experience of residents living in them (e.g., proximity to public transportation and other community resources, access to employment opportunities, etc.). Additionally, although we combined data from a variety of sources (e.g., the Sober Living Network, the US census, the California Alcoholic Beverage Commission, the SAMHSA treatment locator, and listings of self-help meetings), we did not have data to reflect outcomes of the residents in the SLHs studied. Further, our analyses used census data from 2010 and information on SLHs collected in 2014. Though somewhat unlikely, neighborhood factors could have changed in the years between 2010 and 2014 due to economic climate, gentrification, or a host of other unmeasured factors. Finally, our data was cross-sectional in nature, and our study cannot speak to how neighborhoods with SLHs may change over time. The large number of SLHs and wide range of price points for those houses, as well as the geographic and demographic diversity, makes LA County an ideal location to conduct this research; however, it is important to conduct similar studies in other areas to determine the generalizability of findings.
Summary and Conclusions
Longitudinal studies of SLH residents show outcomes improve over time, however, we know relatively little about the neighborhood factors that may support or hinder resident recovery. Understanding characteristics of neighborhoods in which SLHs are located is an important first step in examining how these characteristics may affect the residents living in them. This exploratory study represents the first comprehensive examination of the characteristics of neighborhoods in which SLHs are located. Using data on the locations of SLHs in LA County, we found that despite a large number of houses, SLHs were present in only a small fraction of LA neighborhoods, there was clustering of neighborhoods with SLHs, and neighborhoods with SLHs differed from neighborhoods without them on a variety of indicators of neighborhood socioeconomic disadvantage and accessibility of recovery resources. We also found that accessibility of treatment facilities was robustly associated with the availability of affordable and high-cost SLHs, as well as evidence to suggest that SLHs may be under-represented in predominantly Hispanic neighborhoods and neighborhoods with a greater percentage of Asian Americans. Additional research is needed to augment the scope of neighborhood factors studied and to more comprehensively address questions about how SLHs may influence neighborhoods as well as how neighborhood in which SLHs are located may affect residents living in them using multilevel analyses.
Acknowledgments
This work was funded by the National Institute on Alcohol Abuse and Alcoholism (R01AA020328 to K. Karriker-Jaffe) and the National Institute on Drug Abuse (R01DA034973 to D. Polcin). The funding agencies had no role in study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDA, NIAAA or the National Institutes of Health.
Footnotes
Preliminary findings from this study were presented in a poster session at the 2015 Addiction Health Services Research conference in Los Angeles, CA. In addition to our funders, the authors would like to acknowledge Marylou Frendo for compiling data on 12-step meetings and Elizabeth Mahoney and Rachael Korcha for their comments on early versions of this manuscript.
Contributor Information
Amy A. Mericle, Alcohol Research Group at the Public Health Institute.
Katherine J. Karriker-Jaffe, Alcohol Research Group at the Public Health Institute.
Shalika Gupta, Alcohol Research Group at the Public Health Institute.
David M. Sheridan, Sober Living Network
Doug L. Polcin, Alcohol Research Group at the Public Health Institute.
References
- Alcoholics Anonymous Central Office of Los Angeles. Los Angeles, CA: 2015. [Accessed: 2016-04-20]. Find a Meeting. Archived by WebCite® at http://www.webcitation.org/6gvAcU1F1. [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42(2):151–165. [PubMed] [Google Scholar]
- Borkman TJ, Kaskutas LA, Room J, Bryan K, Barrows D. An historical and developmental analysis of social model programs. Journal of Substance Abuse Treatment. 1998;15(1):7–17. doi: 10.1016/s0740-5472(97)00244-4. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severly mentally ill substance abusers. Addictive Behaviors. 2003;28(1):157–168. doi: 10.1016/s0306-4603(01)00272-6. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Department of Alcoholic Beverage Control. Sacramento, CA: 2012. [Accessed: 2016-04-20]. License Query System (LQS) Archived by WebCite® at http://www.webcitation.org/6gvBd4XKe. [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on alcohol and related conditions. Archives of General Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Drukker DM, Peng H, Prucha IR, Raciborski R. Creating and managing spatial-weighting matrices with the spmat command. The Stata Journal. 2013;13(2):242–286. [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prevention Science. 2002;3(2):125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- ESRI. Redlands, CA: Environmental Systems Research Institute; 2013. ArcMap 10.2. [Google Scholar]
- ESRI. Redlands, CA: Environmental Systems Research Institute; 2016. [Accessed: 2016-04-21]. Esri Demographics: Census and ACS (An Esri white paper) Archived by WebCite® at http://www.webcitation.org/6gwFQnAWr. [Google Scholar]
- Evans E, Li L, Buoncristiani S, Hser Y-I. Perceived neighborhood safety, recovery capital, and successful outcomes among mothers 10 years after substance abuse treatment. Substance Use and Misuse. 2014;49(11):1491–1503. doi: 10.3109/10826084.2014.913631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari JR, Groh DR, Jason LA. The neighborhood environments of mutual-help recovery houses: comparisons by perceived socio-economic status. Journal of Groups in Addiction and Recovery. 2009;4(1–2):100–109. doi: 10.1080/15560350802712470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furr-Holden CDM, Lee MH, Milam AJ, Johnson RM, Lee K-S, Ialongo NS. The growth of neighborhood disorder and marijuana use among urban adolescents: a case for policy and environmental interventions. Journal of Studies on Alcohol And Drugs. 2011;72(3):371–379. doi: 10.15288/jsad.2011.72.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia A. Serenity: violence, inequality and recovery on the edge of Mexico City. Medical Anthropology Quarterly. 2015;9(4):455–472. doi: 10.1111/maq.12208. [DOI] [PubMed] [Google Scholar]
- Hannon L, Cuddy MM. Neighborhood ecology and drug dependence mortality: an analysis of New York City census tracts. The American Journal of Drug and Alcohol Abuse. 2006;32(3):453–463. doi: 10.1080/00952990600753966. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Hall SM, Wasserman DA. Social support and relapse: commonalities among alcoholics, opiate users and cigarette smokers. Addictive Behaviors. 1991;16(5):235–246. doi: 10.1016/0306-4603(91)90016-b. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley & Sons; 1989. [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd. New York, NY: John Wiley & Sons; 2000. [Google Scholar]
- Jacobson JO. Place and attrition from substance abuse treatment. Journal of Drug Issues. 2004;34(1):23–50. [Google Scholar]
- Jason LA, Mericle AA, Polcin DL, White WL. The role of recovery residences in promoting long-term addiction recovery. American Journal of Community Psychology. 2013;52(3–4):406–411. doi: 10.1007/s10464-013-9602-6. [DOI] [PubMed] [Google Scholar]
- Jason LA, Roberts K, Olson BD. Attitudes toward recovery homes and residents: does proximity make a difference. Journal of Community Psychology. 2005;33(5):529–535. [Google Scholar]
- Jason LA, Schober D, Olson BD. Community involvement among second-order change recovery homes. The Australian Community Psychologist. 2008;20(1):73–83. [PMC free article] [PubMed] [Google Scholar]
- Johnson R, Marin N, Sheahan T, Way F, White W. Philadelphia, PA: Philadelphia Department of Behavioral Health and Mental Retardation Services; 2009. [Accessed: 2015-09-15]. Recovery resource mapping: results of a Philadelphia recovery home survey. Archived by WebCite® at http://www.webcitation.org/6bZIk0vni. [Google Scholar]
- Karriker-Jaffe KJ. Areas of disadvantage: a systematic review of effects of area-level socioeconomic status on substance use. Drug and Alcohol Review. 2011;30(1):84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ. Neighborhood socioeconomic status and substance use by U.S. adults. Drug and Alcohol Dependence. 2013;133(1):212–221. doi: 10.1016/j.drugalcdep.2013.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA. Institute for Behavioral Research, University of Georgia Center for Research on Deviance and Behavioral Health. Distinguished Visitor Scholar Series. Athens, Georgia: 1998. Apr 13, Social model treatment for substance abuse: a radical approach in a changing environment. [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? American Journal of Epidemiology. 2002;156(5):471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. American Journal of Community Psychology. 2004;34(3–4):205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Williams CT, Wang J, Curry AD. Neighborhood social disorders as a determinant of drug injection behaviors: a structural equation model approach. Health Psychology. 2005;24(1):96–100. doi: 10.1037/0278-6133.24.1.96. [DOI] [PubMed] [Google Scholar]
- Laudet AB, White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. Journal of Substance Abuse Treatment. 2010;38(1):51–59. doi: 10.1016/j.jsat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton SL, Celentano DD, Kirk GD, Mehta SH. The longitudinal association between homelessness, injection drug use, and injection-related risk behavior among persons with a history of injection drug use in Baltimore, MD. Drug and Alcohol Dependence. 2013;132(3):457–465. doi: 10.1016/j.drugalcdep.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Sasso AT, Byro E, Jason LA, Ferrari JR, Olson B. Benefits and costs associated with mutual-help community-based recovery homes: the Oxford House model. Evaluation and Program Planning. 2012;35(1):47–53. doi: 10.1016/j.evalprogplan.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA. Taxonomy of high-risk situations for alcohol relapse: evolution and development of a cognitive-behavioral model. Addiction. 1996;91(12, Suppl. 1):S37–S49. [PubMed] [Google Scholar]
- Mericle AA, Miles J. Quality of life and the complex needs of recovery home residents. Substance Abuse. doi: 10.1080/08897077.2016.1213780. [under review] [DOI] [PubMed] [Google Scholar]
- Mericle AA, Miles J, Cacciola J. A critical component of the substance abuse continuum of care: recovery homes in Philadelphia. Journal of Psychoactive Drugs. 2015;47(1):80–90. doi: 10.1080/02791072.2014.976726. [DOI] [PubMed] [Google Scholar]
- Mericle AA, Miles J, Way F. Recovery residences and providing safe and supportive housing for individuals overcoming addiction. Journal of Drug Issues. 2015;45(4):368–384. [Google Scholar]
- Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. American Journal of Epidemiology. 1989;129(1):125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- Molina KM, Alegría M, Chen C-N. Neighborhood context and substance use disorders: a comparative analysis of racial and ethnic groups in the United States. Drug and Alcohol Dependence. 2012;125(Suppl. 1):S35–S43. doi: 10.1016/j.drugalcdep.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PAP. Notes on continuous stochastic phenomena. Biometrika. 1950;37(1–2):17–23. [PubMed] [Google Scholar]
- Mullahy J. Specification and testing of some modified count data models. Journal of Econometrics. 1986;33(3):341–365. [Google Scholar]
- Pisati M. Sg162: Tools for spatial data analysis. Stata Technical Bulletin. 2001;60:21–37. [Google Scholar]
- Polcin DL. What about Sober Living Houses for parolees? Criminal Justice Studies. 2006;19(3):291–300. [Google Scholar]
- Polcin DL, Henderson DM. A clean and sober place to live: philosophy, structure, and purported therapeutic factors in sober living houses. Journal of Psychoactive Drugs. 2008;40(2):153–159. doi: 10.1080/02791072.2008.10400625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Bond J, Galloway G. Eighteen-month outcomes for clients receiving combined outpatient treatment and sober living houses. Journal of Substance Abuse. 2010a;15(5):352–366. doi: 10.3109/14659890903531279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Bond J, Galloway GP. Sober living houses for alcohol and drug dependence: 18-month outcomes. Journal of Substance Abuse Treatment. 2010b;38(4):356–365. doi: 10.1016/j.jsat.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross SM, Turner C. Physical proximity as a possible facilitator in post-detoxification treatment-seeking among chemically dependent veterans. Addictive Behaviors. 1994;19(3):343–348. doi: 10.1016/0306-4603(94)90035-3. [DOI] [PubMed] [Google Scholar]
- Scribner R. Report on High Alcohol Content Malt Beverages and Related Products. A conference at Prevention Research Center, Berkeley, CA, May 31, 2000. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2000. An overview of issues related to outlet density; pp. 4–7. [Google Scholar]
- Sheedy CK, Whitter M. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2009. [Accessed: 2015-05-01]. Guiding Principles and Elements of Recovery-Oriented Systems of Care: What do we know from the research? p. 61. [HHS Publication No. (SMA) 09-4439] [Archived by WebCite® at http://www.webcitation.org/6YDADCmUP] [Google Scholar]
- Stahler GJ, Mennis J, Cotlar R, Baron DA. The influence of neighborhood environment on treatment continuity and rehospitalization in dually diagnosed patients discharged from acute inpatient care. The American Journal of Psychiatry. 2009;166(11):1258–1268. doi: 10.1176/appi.ajp.2009.08111667. [DOI] [PubMed] [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 14.0. College Station, TX: Stata Corporation; 2015. [Google Scholar]
- State of California, & Department of Finance. Sacramento, CA: 2015. [Accessed: 2016-04-21]. E-1 Population Estimates for Cities, Counties, and the State — January 1, 2014 and 2015. [Archived by WebCite® at http://www.webcitation.org/6gwRo4159] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: 2012. [Accessed: 2015-07-31]. SAMHSA's Working Definition of Recovery; p. 7. [Archived by WebCite® at http://www.webcitation.org/6aRHz0R8X] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: 2015a. [Accessed: 2016-04-21]. Behavioral Health Treatment Services Locator. [Archived by WebCite® at http://www.webcitation.org/6gwTyDPmt] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: 2015b. [Accessed: 2016-04-21]. Behavioral Health Treatment Services Locator: Self-Help, Peer Support, and Consumer Groups - Self-Help Groups (Addiction) [Archived by WebCite® at http://www.webcitation.org/6gwUE7SXD] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, & Center for Behavioral Health Statistics and Quality. Rockville, MD: 2015. [Accessed: 2016-04-21]. National Survey on Drug Use and Health, 2013 and 2014: California, Tables 19 and 20. [ http://www.samhsa.gov/data/sites/default/files/1/1/NSDUHsaeCalifornia2014.pdf] [Google Scholar]
- Troutman D. My life as the developer of Sober Living Homes: an experience report. International Journal of Self Help and Self Care. 2014;8(2):227–238. [Google Scholar]
- U.S. Department of Housing and Urban Development, & Office of Policy Development and Research. Washington, DC: 2015. [Accessed: 2016-04-21]. Resources. [Archived by WebCite® at http://www.webcitation.org/6gwUdS0i7] [Google Scholar]
- Ward MD, Gleditsch KS. Spatial regression models. Thousand Oaks, CA: SAGE Publications; 2008. [Google Scholar]
- White W, Cloud W. Recovery capital: a primer for addictions professionals. Counselor. 2008;9(5):22–27. [Google Scholar]
- White WL, Cloud W. Recovery capital: A primer for addictions professionals. Counselor. 2008;9(5):22–27. [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was zen, this is tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Wu L-T, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatric Services. 2003;54(3):363–369. doi: 10.1176/appi.ps.54.3.363. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA. Helping, spirituality, and Alcoholics Anonymous in recovery. Journal of Studies on Alcohol. 2004;65(3):383–391. doi: 10.15288/jsa.2004.65.383. [DOI] [PubMed] [Google Scholar]