Abstract
Study Objectives:
There is a growing body of research examining the relationship between sleep and functional outcomes. However, little is known about sleep and physical functioning in older African Americans.
Methods:
Data for this project included 450 community-dwelling older African Americans (71.4 ± 9.2 years of age) who participated in the Baltimore Study of Black Aging. Overall sleep pattern and quality was measured by the Pittsburgh Sleep Quality Index (PSQI). Physical functioning was measured by the number of activities of daily living that each participant reported difficulty (ADL; e.g. eating, dressing, and bathing). Negative binomial regression models were conducted to estimate the association between sleep quality and physical functioning.
Results:
Seventy-two percent of the participants reported poor sleep quality. African Americans who reported poor sleep quality had a greater likelihood of an increase in the number of difficulties in ADLs that they reported even after accounting for demographic characteristics and health conditions. The relationship between sleep quality and physical functioning did not vary by gender.
Conclusions:
Sleep may be an important factor to consider when seeking to improve physical functioning among community-dwelling older African Americans.
Citation:
Thorpe Jr RJ, Gamaldo AA, Salas RE, Gamaldo CE, Whitfield KE. Relationship between physical function and sleep quality in African Americans. J Clin Sleep Med 2016;12(10):1323–1329.
Keywords: sleep quality, physical function, activities of daily living (ADL), African Americans, gender
INTRODUCTION
Despite all of the medical and technological advances in the United States, community-dwelling older African Americans continue to exhibit worse physical functioning putting them at risk for adverse health outcomes.1–6 Several factors such as socioeconomic status (SES), psychological factors, biomedical factors, and specific chronic conditions have been examined to better understand why African Americans have worse functional status.7–12 Yet, modest progress has been achieved. This is largely because there are other factors such as sleep that might contribute to the functioning status of community dwelling older African Americans. Identifying and understanding specific factors that may be related to physical functioning is a key step in maintaining the independence and well-being of community-dwelling older African Americans.
Sleep is a basic human need and an important indicator of health and well-being. However, little attention has focused on how physical functioning is impacted by sleep, particularly among African Americans. There are a growing number of studies that consistently demonstrate disproportionately higher rates of sleep disorders (e.g., sleep apnea) and poor sleep quality/disturbance among African Americans.13–19 Specifically, African Americans are more likely to report poorer sleep quality, a larger disparity in overall sleep duration, and greater night-to-night variability compared to whites.14–16,18–21 Such sleep disturbances have been shown to be associated with a poorer quality of life.22–24 Poor sleep is associated with many adverse health conditions (i.e., hypertension, diabetes, and cardiovascular disease) that are commonly observed in African Americans.15,25–28 African Americans are at greater risk for morbidity and premature mortality than whites.29 Sleep disturbances are also associated with poor cognitive functioning in African Americans, particularly worse performance on tasks of memory and global cognition.30–32 Cognitive dysfunction is associated with shorter sleep duration,30,31,33,34 long sleep duration,30,31,34 changes in sleep duration,35 and poor sleep quality.36 While there is a growing body of work on sleep quality and health outcomes, little is known about how sleep impact physical functioning among older African Americans. Further it is unclear if this relationship varies by gender.
BRIEF SUMMARY
Current Knowledge/Study Rationale: There is a burgeoning body of research examining the relationship between sleep and functional outcomes particularly among older adults. However, there is a paucity of work focusing on sleep and physical functioning in older African Americans.
Study Impact: Sleep quality is an important correlate of difficulties of ADL among older African Americans regardless of gender. Understanding this relationship in this understudied population is important given that the number of older African Americans is expected to continue to grow over the next three decades in the United States.
There is limited research that has explored gender differences in sleep disturbances among African Americans. Prior research, which has explored gender differences, has observed significant differences between African males and females depending upon the sleep parameter investigated. For example, African American males tend report shorter sleep duration20 and are more risk for sleep apnea14 than African American females. In contrast, African American females are more at risk for insomnia than African American males.14 However, previous studies have also observed no significant gender differences among African Americans in trouble falling asleep14,32 and/or sleep efficiency.14 These results highlight the importance of further exploring gender differences in sleep disturbances among African Americans and how potential gender differences in sleep may assist in understanding gender differences in health outcomes.
To our knowledge, no study has investigated whether sleep quality in older African Americans are associated with physical functioning. Here, we focus on understanding the relationship between sleep and physical functioning among older African Americans in an effort to understand the heterogeneity that may exist among African Americans with regard to sleep quality and physical functioning.37 Further focusing solely on African Americans is a key initial step to advancing our understanding on how to reduce or eliminate race-related disparities in sleep quality and physical functioning.38,39 Information gained from understanding whether sleep quality impacts physical functioning among older African Americans will help us prepare for the needs of the growing segment of the United States population. Thus, the overall goal of this study is to examine whether sleep quality is associated with physical functioning in a large sample of urban community-dwelling older African Americans. The first aim is to evaluate the relationship between physical functioning and sleep quality after adjusting for demographic and health indices. It is anticipated that those with poor sleep quality will be associated with worse physical functioning. The second aim is to investigate whether the association between physical function and sleep quality varies between men and women. It is hypothesized that the relationship between physical function and sleep quality are worse among men than women.
METHODS
Participants
The study sample included urban and independently living African American older adults from the Baltimore Study of Black Aging: Patterns of Cognitive Aging (BSBA: PCA). The main objective of BSBA: PCA was to explore the patterns and individual factors that influence individual differences in cognitive functioning among older African Americans. Participants aged 50 years and older were recruited from 29 senior housing facilities that consisted primarily (> 75%) of African Americans living in the West Baltimore area. Data for BSBA was collected across two different waves: 2006–2008 (wave 1) and 2009–2011 (wave 2). Each testing session took approximately 2.5 hours and was conducted in a vacant, public room of the participant's apartment building or in a private room at a senior citizen facility. During each testing session, a trained research assistant assessed the participant using a battery of questions that included sociodemographic, physical health, and mental health measures. Each participant was compensated $30 at the first wave and $75 at the second wave. Additional details of the BSBA study design are described elsewhere.40,41
The BSBA: PCA wave 1 data collection included 602 participants (449 females and 153 males) with a mean age of 69.1 (SD = 9.8, range 48–95). Participants' average monthly income at wave 1 data collection was $1,000 (SD $600; range = < $100 to > $2,300), and the average educational level was 11.6 ± 3.0 years (range = 3–20). The BSBA: PCA wave 2 data collection included 450 of the 602 participants from wave 1. Sleep indices were only administered at wave 2; therefore, this paper will include only participants from wave 2. The mean age of the sample age was 68 years (SD 9.2) and mean level of education was 11 years (SD 2.9). All participants signed a written informed consent agreement approved by the institutional review board at Duke University.
Physical Function
The outcome variable, physical functioning, was based upon the participant's report of difficulty in performing basic activities of daily living (ADLs). This included eating, dressing, grooming, walking, bathing, using the toilet, and transferring in and out of bed.42 The 4 possible response categories included: (1) never need help; (2) have difficulty but can do without help; (3) have difficulty and need help; (4) never do the activity. A binary variable was created for each ADL representing those who reported any difficulty for that particular ADL. We summed across the binary variables to create the number of difficulties with ADLs that each participant reported.
Sleep Indices
The Pittsburgh Sleep Quality Index (PSQI)43 was used to assess participants' typical sleep habits and patterns within the last month. Questions were designed to assess 7 components, including sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. The PSQI has been shown to be strongly reliable (α = 0.83). In addition, it has been shown to have relatively high sensitivity (89.6%) and specificity (86.5%) in differentiating good and bad sleep habits and high correlation with the common sleep disorders to include insufficient sleep syndrome, primary insomnia, circadian rhythm disorders, restless legs syndrome, and sleep apnea. Global sleep quality scores can range from 0 (good sleeper) to 21 (poor sleeper). A global quality score ≤ 5 indicates the perception of “good sleep quality,” a global score > 5 indicates a perception of “poor sleep quality.” A binary variable was created to identify those who reported global sleep quality scores > 5 compared to those who reported ≤ 5.
Covariates
Covariates included demographic and health conditions. Demographic variables included age, gender, years of education, and family income. Age and years of education were measured as continuous variables. Gender was coded as a binary variable with 1 indicating those who were female. Family income was based on participants' selection of one of twenty-three categories ranging from under $100 to $2,300 or more per month in $100 dollar categories.
Health conditions included depressive symptoms and chronic conditions. Depressive symptoms were assessed using the 20-item Center for Epidemiological Studies Depression (CES-D) Scale.44,45 The CES-D is commonly used in detecting depressive symptoms in older adults across diverse populations.46 Chronic conditions were based on participants' report of physician diagnoses of the following: angina, asthma, arthritis, cancer, diabetes, stroke, heart attack, or high blood pressure.7,47,48 Each of the chronic conditions was coded as a binary variable (1 = present; 0 = absent). A variable representing the number of chronic conditions each participant reported was created by summing across each of the chronic condition binary variables.
Analyses
Student's t-tests for continuous variables were used to evaluate the mean and chi squares were used to examine proportional differences by gender for the demographic variables, number of chronic conditions, depressive symptoms, number of difficulties with ADLs, and sleep quality. Negative binomial regression models were specified to examine the association between sleep quality and number of difficulties with ADLs. The negative binomial regression model, rather than the Poisson regression model, was selected to account for the overdispersion of the outcome variable.49–52 Incident rate ratios and corresponding 95% confidence intervals were used to present findings from the four progressively more complex negative binomial models. The first model tested association between sleep quality and number of difficulties with ADLs. The second model tested whether that relationship remained after accounting for demographic variables. The third model tested whether the relationship between sleep quality and number of difficulties with ADLs remained after adjusting for demographic and health measures. The fourth model tested whether the relationship between sleep quality and number of difficulties with ADLs differed by gender after accounting for demographic and health measures. More specifically, an interaction term of sleep quality and gender will be entered into model 4. If the interaction term is significant (p < 0.05), additional stratified analyses will be performed to examine the relationship between sleep quality and number of difficulties with ADLs for men and women separately. A p value < 0.05 was considered statistically significant and all tests were two-tailed. Analyses were conducted using Stata, Version 13 (College Station, TX).
RESULTS
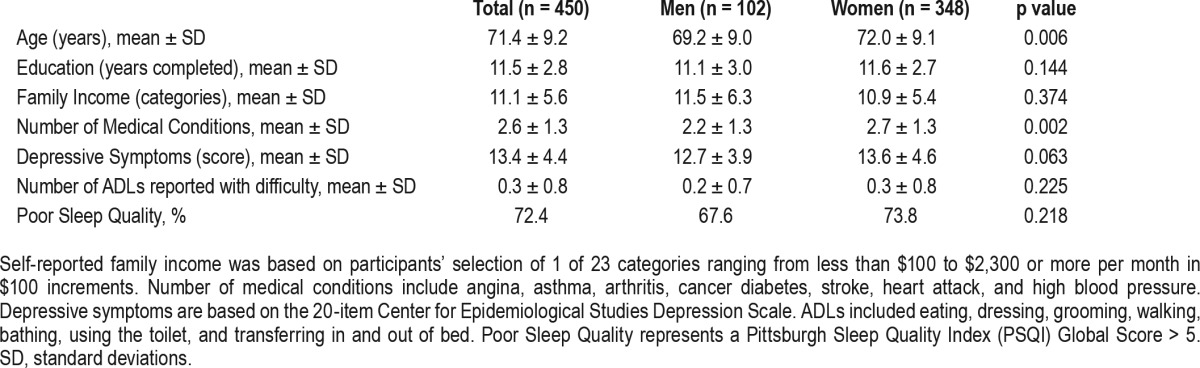
The distribution of the sample characteristics for the total sample and by gender is displayed in Table 1. Of the 450 African Americans, the majority of the sample was female, and the average age was 71.4 ± 9.2 years. With respect to socioeconomic status, the average number of years of education completed was 11.5 ± 2.8 years, and the average monthly income was between $1,100 and $1,200. On average, participants reported 2.6 ± 1.3 chronic conditions and reported a CES-D score of 13.5 ± 4.5. The average number of difficulties with ADLS was 0.4 ± 0.8. Seventy-two percent of the participants reported poor sleep quality. Examining the sample characteristics by gender revealed that women were older (72.0 vs. 69.2 years) and reported more chronic conditions (2.7 vs. 2.2 years) compared to men. There were no significant differences between men and women with respect to education, income, depressive symptoms, number of difficulties with ADLs, or poor sleep quality.
Table 1.
Distribution of sample characteristics of total sample and by gender among 450 older African Americans.
Association between Sleep Quality and Number of ADLS Reported Difficulty
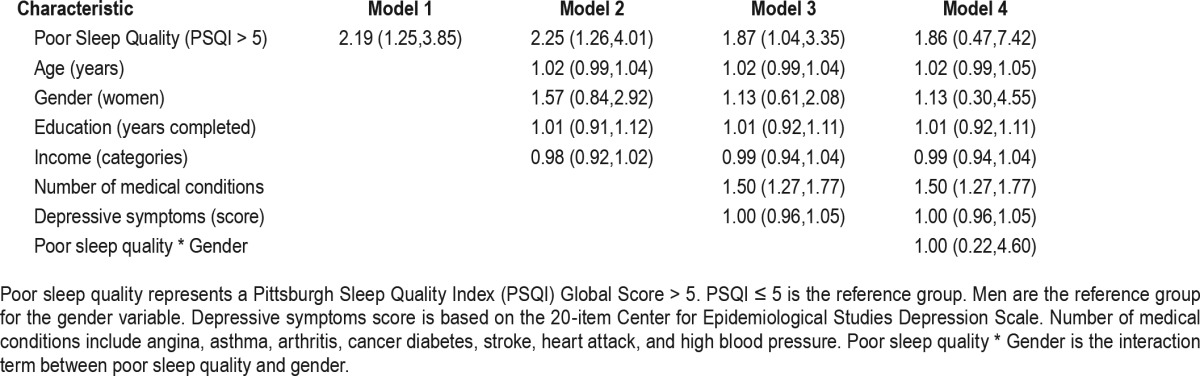
Table 2 displays the association between sleep quality and the number of difficulties with ADLs. Poor sleep quality was associated with the number of difficulties with ADLS for older African Americans across models 1–3. Specifically, in the un-adjusted model, African Americans who reported poor sleep quality had a higher likelihood of increasing the number of difficulties with ADLs than those who reported good sleep quality. After adjusting for demographics variables in model 2, African Americans who reported poor sleep quality had a greater likelihood of increasing the number of difficulties with ADLs (incidence rate ratio (IRR) = 2.25, 95% confidence interval (CI) 1.26, 4.01). The relationship remained even after adjusting including health-related factors in model 3 (IRR = 1.87, 95% CI 1.05, 3.35). In model 4 an interaction term of sleep quality and gender was added to model 3 to determine if the relationship between sleep quality and number of difficulties with ADLs was different for men and women. The relationship between sleep quality and the number of difficulties with ADLs did not differ by gender (IRR = 1.00, 95% CI 0.22, 4.60; p = 0.992).
Table 2.
Incidence rate ratios (95% confidence intervals) for the association between physical functioning and sleep quality in 450 older African Americans.
Additional analyses were conducted by examining the components of the PQSI. Of the seven components, 3 components were associated with number of difficulties with ADLS. Those who reported difficulty in sleep quality had a greater likelihood of increasing the number of difficulties with ADLs (IRR = 1.95, 95% CI 1.19, 3.19) compared to those who reported no difficulty in sleep quality. Those who reported difficulty in use of sleep medications had a greater likelihood of increasing the number of difficulties with ADLs (IRR = 2.15, 95% CI 1.23, 3.75) compared to those who reported no difficulty in use of sleep medications.
Those who reported difficulty in use of sleep medications had a greater likelihood of increasing the number of difficulties with ADLs (IRR = 2.15, 95% CI 1.23, 3.75) compared to those who reported no difficulty in use of sleep medications. Those who reported difficulty in daytime dysfunction due to sleep habits had a greater likelihood of increasing the number of difficulties with ADLs (IRR = 2.54, 95% CI 1.61, 3.98) compared to those who reported no difficulty in daytime dysfunction. No differences were observed between sleep latency, sleep duration, habitual sleep efficiency, or sleep disturbances and the number of difficulties with ADL reported.
DISCUSSION
We sought to understand the relationship between sleep quality and physical functioning in older African Americans and whether this relationship varies by gender. After accounting for demographic and health measures, poor sleep quality was associated with a greater likelihood of an increase in the number of difficulties with ADLs. The relationship between sleep quality and number of difficulties with ADLs that a participant reported did not vary by gender. Findings indicate that sleep quality is an important correlate of difficulties of ADL among older African Americans irrespective of gender. Understanding this relationship in this understudied population is important given that the number of older African Americans is expected to continue to grow over the next three decades in the United States.
We observed that reported poor sleep quality was associated with increasing difficulty in a number of ADLs. This finding is not only consistent with previous work in older adults, but extends previous research to older African Americans. In particular, a relationship between insomnia variables and impairment in ADLs has been previously reported in three community-based samples in the United States.46 Significant associations between insomnia symptoms and subjective reports of limitations in specific household activities (e.g., doing laundry, doing shopping, being social engaged), which may be important for independent living have also been demonstrated in older adults.53 One potential and interesting explanation for the relationship between sleep quality and physical functioning (i.e., ADLs) is that poor sleep quality can lead to mental fatigue during the day that can contribute to physical dysfunction.54 Recently, authors reported that older adults with difficulty staying asleep are at a greater risk for persistent severe fatigue.55 Thus, perhaps, poor sleep may negatively impact the capacity for performance.56,57 As such, the ability to perform tasks that require additional effort may be impaired when an individual is suffering from poor quality sleep. Future studies seeking to understand the mechanism by which sleep quality impacts functional status is needed within an older African American cohort.
In this study we demonstrated that the association between sleep quality and physical function did not vary by gender. This finding is inconsistent with the hypothesis. However this finding was in agreement with previous work.58,59 While there are some data suggesting that African American women are more likely to report poorer sleep quality than African American men,28 other studies have observed no significant gender differences among African Americans for sleep quality and/ or sleep duration.58,59 In the current study, African American women were significantly older and reported more chronic conditions than African American men. Thus, age-related factors such as the increase in the number of chronic health conditions may explain the lack of observed gender difference in the relationship between sleep quality and number of difficulties with ADLS reported.
It is well documented that African Americans report the least amount of sleep of all racial/ethnic groups surveyed.14,17–20,60 While data in the literature may be limited and at times, inconsistent for African Americans, data does suggest that young to middle aged African Americans sleep worse than white Americans.14 Specifically, African Americans take longer to fall asleep, report poorer sleep quality, tend to have more light while less deep sleep, and nap more often and longer than white Americans.14 Additionally, African Americans have a higher prevalence of sleep-disordered breathing such as sleep apnea and demonstrate more risk factors for poor sleep.14 These findings may suggest that the attitude and perspective regarding sleep as an important aspect of overall health and well-being may also differ across various sociocultural and ethnic groups.14
Several limitations of this study warrant comment. First, this study only included older African Americans who live in Baltimore, Maryland. Therefore, the external validity of this study may be limited to older African Americans who reside in urban areas similar to Baltimore, Maryland. Second, the findings of this study were based on self-reported data. The accuracy of self-report disability61,62 and chronic conditions2,63 in older adults has been previously documented. While our results point to differences in physical function in African Americans with poor quality sleep, it is unclear whether these findings are a consequence of chronic sleep disturbance present in patients with disrupted sleep from health conditions (e.g., obesity), health behaviors (e.g., nicotine use and exercise) and/ or an undiagnosed and untreated sleep disorder (restless legs syndrome, obstructive sleep apnea, chronic sleep deprivation) or sociodemographic factors (e.g., financial strain, food insecurity, noisy and/or unsafe environment) that may routinely be experienced by African Americans. The results presented here support the need for a more robust emphasis on the evaluation of sleep in the African American population in effort to improve physical function. Finally, because this is cross sectional data, the opportunity to draw inferences regarding directionality is limited. Specifically, with these data, it cannot be determined that an individual who report difficulty in a greater number of ADLs is more inclined to be less active in the day and/or stressed, anxious about being restricted in his/her activities, which impact their sleep that night. A longitudinal study with a sufficient number of older African Americans that seeks to understand how sleep quality impacts the course of ADL disability is needed.
Despite the limitations, this study has several strengths. First, to our knowledge, this is the first study to investigate the association between sleep quality and physical functioning in older African American adults. Second, this study includes a large number of community-dwelling older African Americans. Third, this study accounts for health and demographic variables that have previously been observed to be associated with sleep quality and/or physical functioning particularly within older African Americans.
As the older African American population is expected to increase over the next 30 years,64 older African Americans (compared to their other older ethnic cohorts) are more likely to be resource-limited both economically and medically.64 Subsequently, this particular group may be increasingly vulnerable to an ongoing state of suboptimal health conditions, restricted access to health care, and, subsequently, high rates of chronic health conditions (i.e., hypertension, diabetes, renal disease).64,65 As result, the high healthcare expenses associated with these health disparities66–68 is likely to increase without increased efforts to reduce and/or eliminate these issues. Studies building on the foundation established with this study should investigate the impact of modifiable health, cultural and environmental variables related to sleep disturbances to develop customized and targeted campaigns to improve sleep and physical function in older African Americans.
DISCLOSURE STATEMENT
This was not an industry supported study. The data for this paper came from a project supported by the National Institute on Aging (NIA; R01 AG24108 and AG24108-S1) to K.E.W. A.A-M. was supported by T32 AG000029 from the NIA. This research was also supported in part by the Intramural Research Program of the NIH, National Institute on Aging. Research conducted by the first author was supported by a grant from the National Center for Minority Health and Health Disparities (P60MD000214). The first author is a visiting scholar in the Center for Biobehavioral Health Disparities Research at Duke University. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- ADL
Activities of Daily Living
- BSBA
Baltimore Study of Black Aging
- BSBA:PCA
Baltimore Study of Black Aging: Patterns of Cognitive Aging
- CES-D
Center for Epidemiological Studies Depression Scale
- PSQI
Pittsburgh Sleep Quality Index
- SES
Socioeconomic Status
REFERENCES
- 1.Gill TM, Robison JT, Tinetti ME. Difficulty and dependence: two components of the disability continuum among community-living older persons. Ann Intern Med. 1998;128:96–101. doi: 10.7326/0003-4819-128-2-199801150-00004. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, LaCroix AZ, Abbott RD, et al. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137:845–57. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New Engl J Med. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP, Miller TR. Effect of subclinical status in functional limitation and disability on adverse health outcomes 3 years later. J Gerontol A Biol Sci Med Sci. 2007;62:101–6. doi: 10.1093/gerona/62.1.101. [DOI] [PubMed] [Google Scholar]
- 5.Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M43–52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 6.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. J Gerontol B Psychol Sci Soc Sci. 2005;60:S146–51. doi: 10.1093/geronb/60.3.s146. [DOI] [PubMed] [Google Scholar]
- 7.Thorpe RJ, Jr., Koster A, Bosma H, et al. Racial differences in mortality in older adults: factors beyond socioeconomic status. Ann Behav Med. 2012;43:29–38. doi: 10.1007/s12160-011-9335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barry LC, Thorpe RJ, Jr., Penninx BW, et al. Race-related differences in depression onset and recovery in older persons over time: the health, aging, and body composition study. Am J Geriatr Psychiatry. 2014;22:682–91. doi: 10.1016/j.jagp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koster A, Penninx BW, Bosma H, et al. Is there a biomedical explanation for socioeconomic differences in incident mobility limitation? J Gerontol A Biol Sci Med Sci. 2005;60:1022–7. doi: 10.1093/gerona/60.8.1022. [DOI] [PubMed] [Google Scholar]
- 10.Whitson HE, Hastings SN, Landerman LR, Fillenbaum GG, Cohen HJ, Johnson KS. Black-white disparity in disability: the role of medical conditions. J Am Geriatr Soc. 2011;59:844–50. doi: 10.1111/j.1532-5415.2011.03401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fried LP, Bandeen-Roche K, Kasper JD, Guralnik JM. Association of comorbidity with disability in older women: the Women's Health and Aging Study. J Clin Epidemiol. 1999;52:27–37. doi: 10.1016/s0895-4356(98)00124-3. [DOI] [PubMed] [Google Scholar]
- 12.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 13.Baker FC, Wolfson AR, Lee KA. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: findings from the 2007 National Sleep Foundation “Sleep in America Poll”. J Women's Health. 2009;18:841–9. doi: 10.1089/jwh.2008.0986. [DOI] [PubMed] [Google Scholar]
- 14.Durrence HH, Lichstein KL. The sleep of African Americans: a comparative review. Behav Sleep Med. 2006;4:29–44. doi: 10.1207/s15402010bsm0401_3. [DOI] [PubMed] [Google Scholar]
- 15.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: results of the National Health Interview Survey. J Natl Med Assoc. 2008;100:317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 16.Pigeon WR, Heffner K, Duberstein P, Fiscella K, Moynihan J, Chapman BP. Elevated sleep disturbance among blacks in an urban family medicine practice. J Am Board Fam Med. 2011;24:161–8. doi: 10.3122/jabfm.2011.02.100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. 2011;34:509–18. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178:1442–51. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Sleep Foundation. 2010 sleep in America poll. 2010. http://www.sleepfoundation.org/sites/default/files/nsaw/NSF%20Sleep%20in%20%20America%20Poll%20-%20Summary%20of%20Findings%20.pdf.
- 21.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25:117–29. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 23.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6:23–7. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Zeitlhofer J, Schmeiser-Rieder A, Tribl G, et al. Sleep and quality of life in the Austrian population. Acta Neurol Scand. 2000;102:249–57. doi: 10.1034/j.1600-0404.2000.102004249.x. [DOI] [PubMed] [Google Scholar]
- 25.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 26.Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:948–54. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 27.Ancoli-Israel S, Ayalon L. Diagnosis and treatment of sleep disorders in older adults. Am J Geriatr Psychiatry. 2006;14:95–103. doi: 10.1097/01.JGP.0000196627.12010.d1. [DOI] [PubMed] [Google Scholar]
- 28.Gamaldo AA, Gamaldo CE, Allaire JC, et al. Sleep complaints in older blacks: do demographic and health indices explain poor sleep quality and duration? J Clin Sleep Med. 2014;10:725–31. doi: 10.5664/jcsm.3858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arias E, Anderson RN, Kung HC, Murphy SL, Kochanek KD. Deaths: final data for 2001. Natl Vital Stat Rep. 2003;52:1–115. [PubMed] [Google Scholar]
- 30.Gamaldo AA, Allaire JC, Whitfield KE. Exploring the within-person coupling of sleep and cognition in older African Americans. Psychol Aging. 2010;25:851–7. doi: 10.1037/a0021378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gamaldo AA, Allaire JC, Whitfield KE. Intraindividual variability in psychometrically defined mild cognitive impairment status in older African Americans. Psychol Aging. 2012;27:989–97. doi: 10.1037/a0028557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gamaldo AA, Allaire JC, Whitfield KE. The relationship between reported problems falling asleep and cognition among African American elderly. Res Aging. 2008;30:15. [Google Scholar]
- 33.Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28:981–9. [PubMed] [Google Scholar]
- 34.Kronholm E, Sallinen M, Suutama T, Sulkava R, Era P, Partonen T. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res. 2009;18:436–46. doi: 10.1111/j.1365-2869.2009.00765.x. [DOI] [PubMed] [Google Scholar]
- 35.Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimaki M, Singh-Manoux A. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep. 2011;34:565–73. doi: 10.1093/sleep/34.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sivertsen B, Overland S, Pallesen S, et al. Insomnia and long sleep duration are risk factors for later work disability. The Hordaland Health Study. J Sleep Res. 2009;18:122–8. doi: 10.1111/j.1365-2869.2008.00697.x. [DOI] [PubMed] [Google Scholar]
- 37.Whitfield KE, Aiken Morgan A. Minority Populations and Cognitive Aging. In: Hofer SM, Alwin DF, editors. Handbook of Cognitive Aging: Interdisciplinary Perspectives. Los Angeles, CA: SAGE Publications; 2008. pp. 384–97. [Google Scholar]
- 38.Whitfield KE, Allaire JC, Belue R, Edwards CL. Are comparisons the answer to understanding behavioral aspects of aging in racial and ethnic groups? J Gerontol Psychol Sci. 2008;63:P301–8. doi: 10.1093/geronb/63.5.P301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whitfield KE, Baker-Thomas TA. Individual differences in aging among African-Americans. Int J Aging Hum Dev. 1999;48:73–9. doi: 10.2190/YGAQ-0D95-M0V4-820M. [DOI] [PubMed] [Google Scholar]
- 40.Allaire JC, Gamaldo A, Ayotte BJ, Sims R, Whitfield K. Mild cognitive impairment and objective instrumental everyday functioning: the everyday cognition battery memory test. J Am Geriatr Soc. 2009;57:120–5. doi: 10.1111/j.1532-5415.2008.02054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sims RC, Allaire JC, Gamaldo AA, Edwards CL, Whitfield KE. An examination of dedifferentiation in cognition among African-American older adults. J Cross Cult Gerontol. 2009;24:193–208. doi: 10.1007/s10823-008-9080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 43.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 44.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 45.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 46.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 47.Thorpe RJ, Jr., Koster A, Kritchevsky SB, et al. Race, socioeconomic resources, and late-life mobility and decline: findings from the Health, Aging, and Body Composition study. J Gerontol A Biol Sci Med Sci. 2011;66:1114–23. doi: 10.1093/gerona/glr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thorpe RJ, Jr., Szanton SL, Bell CN, Whitfield KE. Education, income and disability in African Americans. Ethnicity Dis. 2013;23:12–7. [PubMed] [Google Scholar]
- 49.Gaskin DJ, Price A, Brandon DT, Laveist TA. Segregation and disparities in health services use. Med Care Res Rev. 2009;66:578–89. doi: 10.1177/1077558709336445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Byers AL, Allore H, Gill TM, Peduzzi PN. Application of negative binomial modeling for discrete outcomes: a case study in aging research. J Clin Epidemiol. 2003;56:559–64. doi: 10.1016/s0895-4356(03)00028-3. [DOI] [PubMed] [Google Scholar]
- 51.Long JS. Thousand Oaks, CA: Sage Publications; 1997. Regression models for categorical and limited dependent variables. [Google Scholar]
- 52.Kennedy P. A guide to econometrics. 6th edition. Malden, MA: Blackwell Publishing; 2008. [Google Scholar]
- 53.Spira AP, Kaufmann CN, Kasper JD, et al. Association between insomnia symptoms and functional status in U.S. older adults. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S35–41. doi: 10.1093/geronb/gbu116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stenholm S, Kronholm E, Sainio P, et al. Sleep-related factors and mobility in older men and women. J Gerontol B Psychol Sci Soc Sci. 2010;65:649–57. doi: 10.1093/gerona/glq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Endeshaw YW. Do sleep complaints predict persistent fatigue in older adults? J Am Geriatr Soc. 2015;63:716–21. doi: 10.1111/jgs.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Engle-Friedman M. The effects of sleep loss on capacity and effort. Sleep Sci. 2014;7:213–24. doi: 10.1016/j.slsci.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Engle-Friedman M, Palencar V, Riela S. Sleep and effort in adolescent athletes. J Child Health Care. 2010;14:131–41. doi: 10.1177/1367493510362129. [DOI] [PubMed] [Google Scholar]
- 58.Gamaldo AA, McNeely JM, Shah MT, Evans MK, Zonderman AB. Racial Differences in Self-Reports of Short Sleep Duration in an Urban-Dwelling Environment. J Gerontol B Psychol Sci Soc Sci. 2015;70:568–75. doi: 10.1093/geronb/gbt117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Stability of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Questionnaires over 1 year in early middle-aged adults: the CARDIA study. Sleep. 2006;29:1503–6. doi: 10.1093/sleep/29.11.1503. [DOI] [PubMed] [Google Scholar]
- 60.Ancoli-Israel S. Sleep and ethnicity. Behav Sleep Med. 2010;8:191–3. doi: 10.1080/15402002.2010.509186. [DOI] [PubMed] [Google Scholar]
- 61.Rathouz PJ, Kasper JD, Zeger SL, et al. Short-term consistency in self-reported physical functioning among elderly women: the Women's Health and Aging Study. Am J Epidemiol. 1998;147:764–73. doi: 10.1093/oxfordjournals.aje.a009521. [DOI] [PubMed] [Google Scholar]
- 62.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 63.Ferraro KF, Wilmoth JM. Measuring morbidity: disease counts, binary variables, and statistical power. J Gerontol B Psychol Sci Soc Sci. 2000;55:S173–89. doi: 10.1093/geronb/55.3.s173. [DOI] [PubMed] [Google Scholar]
- 64.LaVeist TA, Isaac LAE. Race ethnicity and health: a public health reader. John Wiley & Sons. 2012 [Google Scholar]
- 65.Whitfield K, Baker TE. Handbook of minority aging. Springer Publishing Company. 2013 [Google Scholar]
- 66.LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv. 2011;41:231–8. doi: 10.2190/HS.41.2.c. [DOI] [PubMed] [Google Scholar]
- 67.Gaskin DJ, Richard P. The Economic Costs of Pain in the United States. J Pain. 2012;13:715–24. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 68.Gaskin DJ, LaVeist TA, Richard P, Ford JG. Washington, DC: C-Change; 2011. The societal and economic impact of cancer health disparities. [Google Scholar]


