Abstract
Study Objectives:
To perform a review of the current evidence regarding the use of a remotely controlled mandibular positioner (RCMP) and to analyze the efficacy of RCMP as a predictive selection tool in the treatment of obstructive sleep apnea (OSA) with oral appliances that protrude the mandible (OAm), exclusively relying on single-night RCMP titration.
Methods:
An extensive literature search is performed through PubMed.com, Thecochranelibrary.com (CENTRAL only), Embase.com, and recent conference meeting abstracts in the field.
Results:
A total of 254 OSA patients from four full-text articles and 5 conference meeting abstracts contribute data to the review. Criteria for successful RCMP test and success with OAm differed between studies. Study populations were not fully comparable due to range-difference in baseline apneahypopnea index (AHI). However, in all studies elimination of airway obstruction events during sleep by RCMP titration predicted OAm therapy success by the determination of the most effective target protrusive position (ETPP). A statistically significant association is found between mean AHI predicted outcome with RCMP and treatment outcome with OAm on polysomnographic or portable sleep monitoring evaluation (p < 0.05).
Conclusions:
The existing evidence regarding the use of RCMP in patients with OSA indicates that it might be possible to protrude the mandible progressively during sleep under poly(somno)graphic observation by RCMP until respiratory events are eliminated without disturbing sleep or arousing the patient. ETPP as measured by the use of RCMP was significantly associated with success of OAm therapy in the reported studies. RCMP might be a promising instrument for predicting OAm treatment outcome and targeting the degree of mandibular advancement needed.
Citation:
Kastoer C, Dieltjens M, Oorts E, Hamans E, Braem MJ, Van de Heyning PH, Vanderveken OM. The use of remotely controlled mandibular positioner as a predictive screening tool for mandibular advancement device therapy in patients with obstructive sleep apnea through single-night progressive titration of the mandible: a systematic review. J Clin Sleep Med 2016;12(10):1411–1421.
Keywords: device, mandibular advancement, mandibular positioner, mandibular protrusion, obstructive sleep apnea, oral appliances, overnight, prediction, remotely controlled, single-night, titration
INTRODUCTION
Obstructive sleep apnea (OSA) is a highly prevalent disease and public health issue, affecting approximately 34% of middle-aged men and 17% of middle-aged women in the United States.1 OSA is characterized by recurrent episodes of apnea and hypopnea during sleep, caused by complete or partial obstructive collapses of the upper airway, respectively, causing sleep fragmentation and hypoxemia.2 Currently apnea is defined as cessation of airflow lasting ≥ 10 sec and hypopnea is defined as a ≥ 30% reduction of airflow associated with ≥ 4% oxygen desaturation.2,3 The apnea-hypopnea index (AHI), representing the average number of apneas and hypopneas per hour of sleep, is determined by performing a polysomnography (PSG) or polygraphy using a portable sleep monitor. The AHI is used to classify the severity of OSA: mild OSA (5 < AHI ≤ 15 events/h), moderate OSA (15 < AHI ≤ 30 events/h) and severe OSA (AHI > 30 events/h).
OSA is associated with a range of harmful sequelae and is a proven risk factor for cardiovascular and cerebrovascular diseases associated with high rates of morbidity and mortality.1,4–12 It is, therefore, important to provide an effective treatment for this condition.
Continuous positive airway pressure (CPAP) is currently regarded as the gold standard treatment for moderate to severe OSA.13 It has been proven that CPAP therapy can be highly efficacious in reducing OSA severity and related morbidity and mortality.5,7 However, its clinical effectiveness is often limited by unsatisfactory adherence with around 50% of patients using CPAP at long-term follow-up.14–16 Classically, a CPAP single-night titration PSG is performed in patients who are eligible for CPAP treatment in order to determine the optimal individual air-pressure settings to prevent upper airway collapse. The sleep technician manually increases the applied pressure when respiratory events occur during polysomnographic evaluation.17
Oral appliances provide a noninvasive alternative to CPAP therapy and are suitable for treatment of snoring and OSA.18 The most common type of oral appliances that are prescribed for the treatment of snoring and OSA protrude the mandible (OAm) mechanically during the night in order to reduce the collapsibility of the upper airway during sleep.19 As compared to the habitual mandibular position, widening of the upper airway occurs in both the lateral and the anteroposterior dimension due to the anterior displacement of the base of the tongue, epiglottis, and soft palate with OAm in situ.18–20 Airway widening causes an increase in pharyngeal dilator muscle activity, a decrease in upper airway resistance, and decreased pharyngeal collapsibility, but the effect of OAm treatment varies largely between patients.20 Larger advancement is often related to higher efficacy, and smaller vertical opening is preferred by patients and leads to a decrease in pharyngeal collapsibility in most patients.20 Treatment with an OAm is generally well tolerated, has few serious side-effects, and higher adherence rates than CPAP.18,19,21 CPAP reduces AHI more effectively than OAm, whereas OAm therapy generally comes with higher rates of adherence.22,23 These findings probably explain why the positive effects on symptoms and health by CPAP and OAm are comparable, as a greater efficacy of CPAP is being offset by its inferior adherence relative to OAm.24–26 This indicates that further gain in therapeutic effectiveness for OAm therapy should be mainly found in optimizing the efficacy of OAm treatment by a reliable and faster titration protocol and a better patient selection possibly leading to a higher efficacy and thus improved effectiveness.22,23
Custom-made titratable OAm are recommended, but no gold standard design of OAm has been identified.18 Classically, the titratable OAm allows for gradual mandibular protrusion of the mandible, as the upper part is dynamically interconnected in some manner with the lower part.18 The titration has to be carried out individually, with an attempt to find the most effective mandibular protrusion with respect to the patient's physical limits. In daily clinical practice, titration of mandibular protrusion during OAm therapy often remains a time-consuming “trial and error” procedure of several weeks to months.19 Many possible titration protocols based on evolution of subjective symptoms and/or objective measurements of OAm treatment outcome during titration have been described in the literature but currently there is no defined gold standard.19
Over the years, prospective prediction of a successful OAm treatment outcome has become a key issue from both a therapeutic and financial perspective, but the ability to perform accurate “up front” selection of patients for OAm therapy is still limited in clinical practice.21,27,28 Clinical features that are associated with outcome of OAm therapy have been examined in retrospective studies, finding female side-sleepers, males with position-dependent OSA, younger patients with lower body mass index, neck circumference, and AHI more likely to respond to OAm therapy.29 Anteroposterior distance, mandibular length, and mandibular plane hyoid distance are cephalometric features that have been associated with treatment response.30,31 A recent study, however, has emphasized the low predictive power of cephalometric parameters.32
Several studies have examined different prediction tools, such as awake nasopharyngoscopic examination, drug-induced sedation endoscopy (DISE) or imaging techniques, to prospectively determine treatment outcome with OAm therapy.27,33–51
Although the effect of mandibular advancement on OSA is believed to be dose dependent, a larger protrusion is not always associated with a corresponding reduction in AHI.52,53 The utility and success of CPAP single-night titration PSG is widespread, but a similar paradigm for determining the suitability and the required protrusion of OAm therapy is currently not part of standard clinical practice.21
The concept of a remotely controlled mandibular positioner (RCMP) for single-night titration was introduced to determine an effective target protrusive position (ETPP) for every individual patient and to prospectively predict treatment success with OAm herewith to avoid a titration procedure for weeks or months.19 By progressively protruding the mandible during a single-night sleep study the mechanical action of the jaw advancement on the airway of the patient is simulated. An RCMP consists of impression trays filled with a rigid impression material mimicking the OAm positioned in the mouth of the patient, attached to a positioner, which progressively protrudes the mandible through a controller located in a patient monitoring room. Also auto-titrating mandibular positioners under computer control in an unattended setting are in development.54–57
This review presents an overview of the literature on single-night titration using RCMP and auto-titrating mandibular positioners.
METHODS
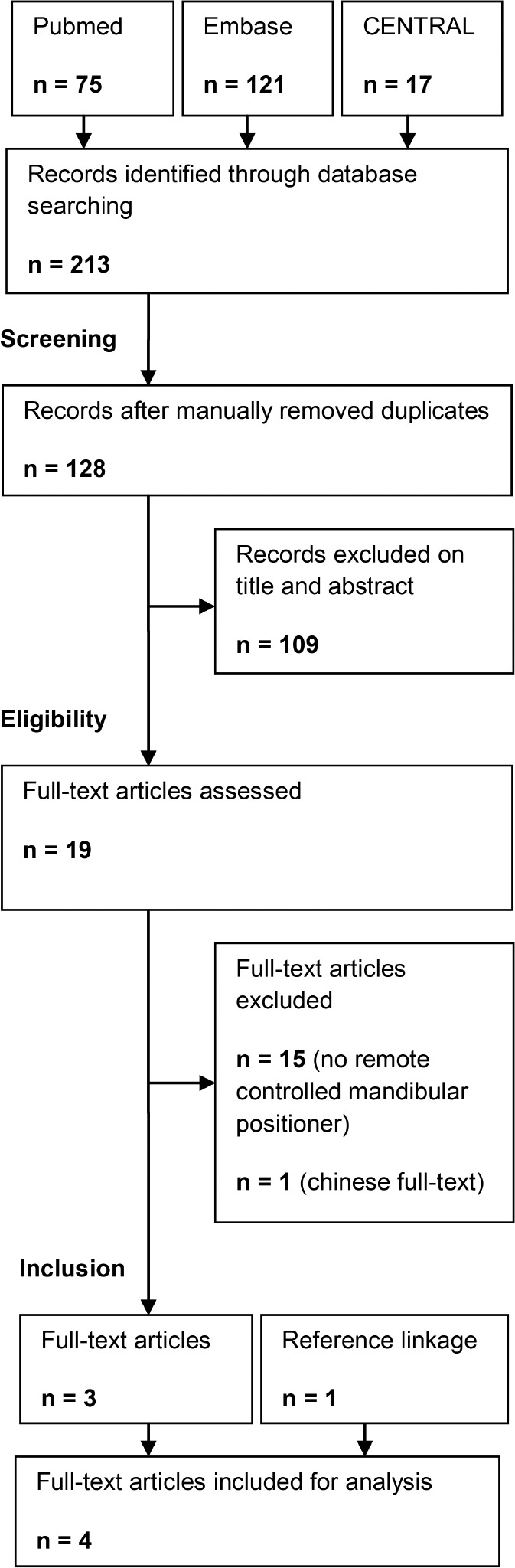
A systematic literature search for relevant studies regarding RCMP in the context of OSA treatment was performed on November 11, 2015 in PubMed.com, Thecochranelibrary.com (CENTRAL only) and Embase.com. By using MeSH terms and synonyms for “OSA,” “mandibular advancement” and “titration” a systematic search was carried out, as shown in Table 1. First, obviously irrelevant items were excluded by screening title and abstract of the records. Next, the full-text articles of the remaining papers were retrieved and carefully evaluated. The search was extended to screening the reference lists of the included full-text articles manually. Additional searches were carried out for recent meeting abstracts and symposium posters of the most important meetings in the field for the synthesis of review to complement the systematic review on evolution and innovation of RCMP. Figure 1 shows the search strategy in detail.
Table 1.
Overview of search terms and number of records identified through database searching on November 11, 2015.
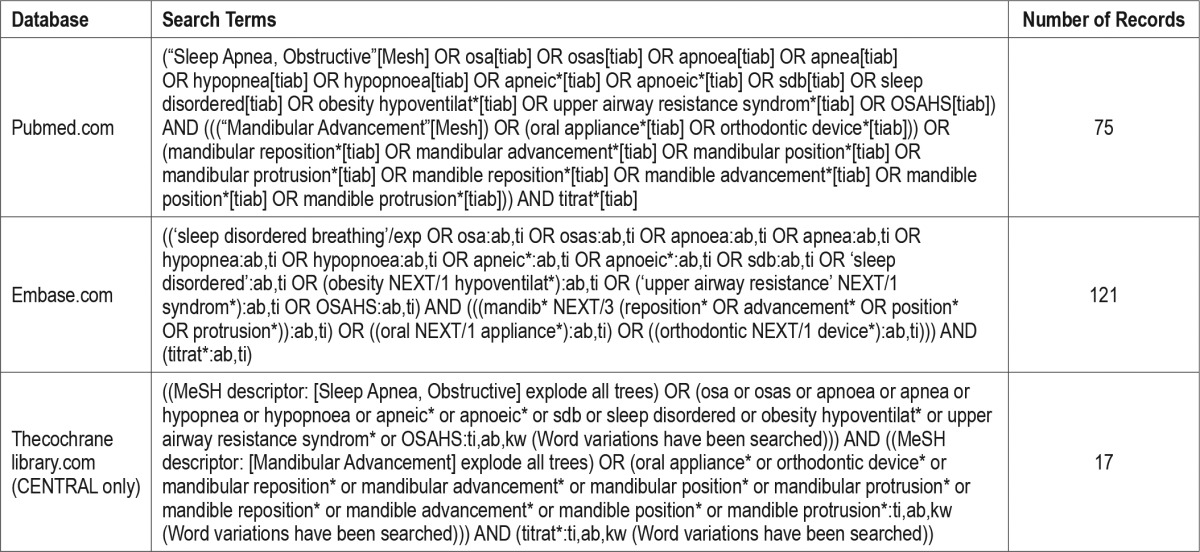
Figure 1. Search strategy displayed in a flow-chart.
RESULTS
Literature Search
The systematic literature search yielded 128 records. After screening, all but 19 papers were eliminated based on limited relevance, and 15 papers were eliminated based on mandibular titration without RCMP. An abstract by Liu et al.58 was published in 2006 and described a computer-aided mandibular repositioning system for efficacy prediction of OAm that could effectively titrate the mandible during PSG with little sleeping disturbance in 14 patients with OSA. Unfortunately this full-text article in Chinese did not allow thorough assessment and was excluded. Finally, four full-text articles were included that described titration with RCMP, which were conducted between 2002 and 2013.28–30,59
In additional searches, five recent meeting abstracts on RCMP and auto-titrating mandibular positioners were collected.54–57,60 The abstracts were presented at the SLEEP conferences 2014 and 2015, American Thoracic Society (ATS) International Conference 2015, and the meeting of the American Academy of Dental Sleep Medicine (AADSM) 2015.
Predictive Value of RCMP
Four included full-text articles28–30,59 focused exclusively on the predictive value of single-night titration with RCMP to prospectively identify an efficacious protrusive position of OAm in patients with OSA. A total of 126 patients with OSA were included in these studies. The authors hypothesized that the successful elimination of respiratory events and oxygen de-saturation by mandibular protrusion during sleep predicted effective OAm treatment response. In other words, it was hypothesized that, when the RCMP test was efficacious by eliminating respiratory events and oxygen desaturation, the protrusive position at which this occurred would also be effective for OAm treatment.30
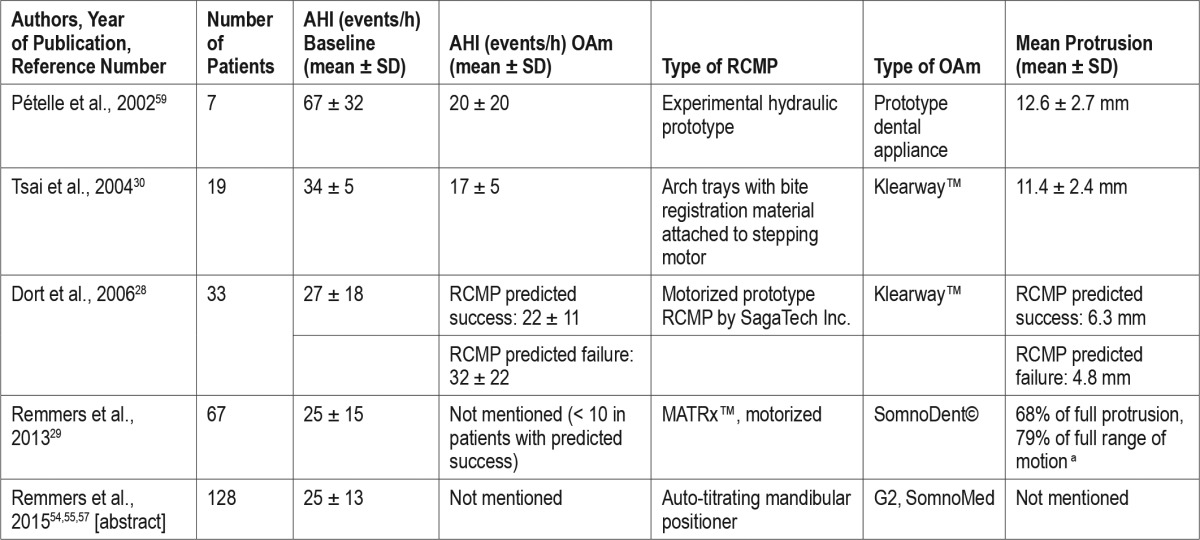
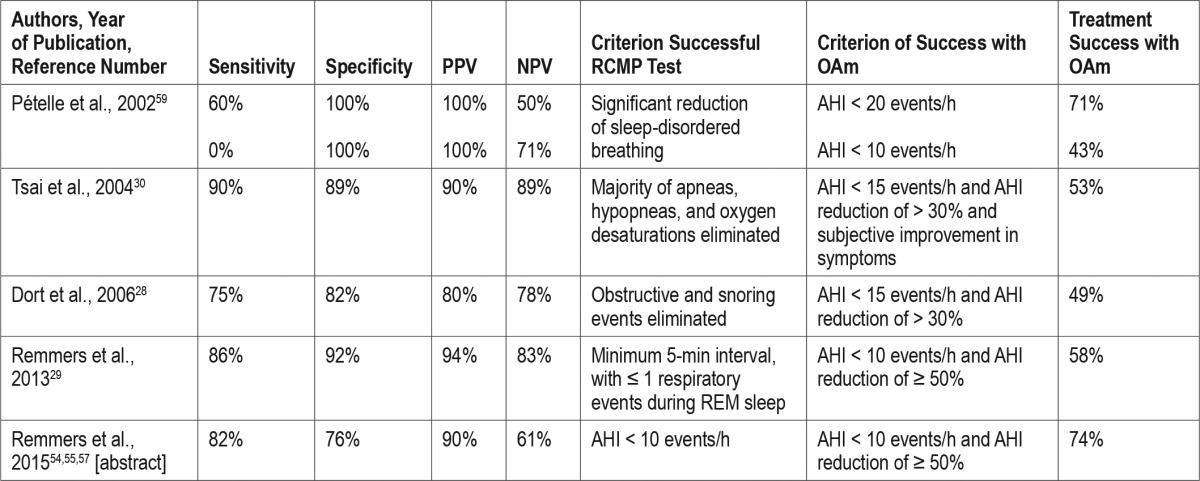
The aim in all these studies was first to evaluate the ability of determining an ETPP through mandibular titration performed with an RCMP during a sleep study. Second, these studies aimed at predicting treatment outcome with an OAm by investigating the association between the ETPP and success with the OAm therapy. Criteria for success differed between studies and are described in the next paragraphs The characteristics of the studies were summarized in Table 2.
Table 2.
Characteristics of studies exclusively focused on the predictive value of single-night titration with remotely controlled mandibular positioner for prospectively identifying an efficacious protrusive position of oral appliances which protrude the mandible in patients with obstructive sleep apnea.
RCMP Types
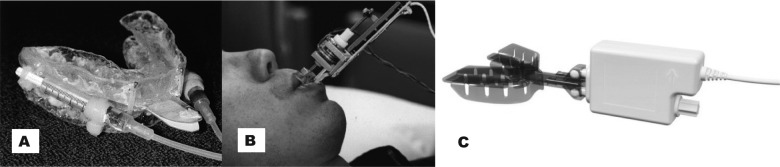
Pételle et al.59 used a prototype hydraulic RCMP device. Two studies28,30 used prototype motorized RCMP systems. Remmers et al.29 introduced a commercially available RCMP device (MATRx, Zephyr Sleep Technologies Inc., Calgary, Canada) that incorporated several improvements over the prototype devices as this device allowed small precise movements in the anterior-posterior dimension while restricting movements in other dimensions.29 Four abstracts (two studies)54–57 describe the use of an auto-titrating mandibular positioner. The RCMP types are depicted in Figure 2; Table 3 summarizes the predictive ability of RCMP, describing sensitivity, specificity, positive predictive value, and negative predictive value.
Figure 2. Historical depiction of RCMP-types.
From left to right: (A) prototype hydraulic remotely controlled mandibular positioner device, adapted from Pételle et al.61 (B) prototype motorized remotely controlled mandibular positioner device placed intra-orally, adapted from Dort et al.31 (C) Commercially available remotely controlled mandibular positioner device (MATRx™, Zephyr Sleep Technologies Inc., Calgary, Canada), adapted from Remmers et al.32
Table 3.
The predictive value of single-night titration with remotely controlled mandibular positioner.
Hydraulic RCMP Prototype
Pételle et al.59 included seven patients with mean baseline AHI of 67 events/h (range: 28–106 events/h) in a pilot study. Each patient underwent 2 consecutive nights under full polysomnographic observation: a titration night with RCMP (“temporary OAm”) and a permanent OAm treatment night. During the titration night with RCMP, the mandible was progressively protruded using a prototype hydraulic advancement mechanism connected to the two arches of a temporary OAm. The two arches were connected with two hydraulic systems made out of a syringe (Figure 2A). Mandibular advancement was induced by mobilization of the column of water in the syringe filled with physiologic saline outside of the patient's room. Mandibular advancement, by increments of 1 mm every 15 min, was started after the first episode of rapid eye movement (REM) sleep or after 2 h of recording after sleep onset. Protrusion was continued until a significant reduction of the incidence of apneas and hypopneas was obtained or until maximal comfortable protrusion was reached or until reaching 17 mm of protrusion, which indicated the maximum value allowed by the device.
The permanent OAm consisted of two separate full coverage acrylic appliances connected by Herbst attachments. Polysomnographic indices obtained during the titration night were compared with those obtained during the treatment night. The AHI decreased by an average of 56% in the RCMP titration night and by 69% during OAm treatment, respectively. AHI < 10 events/h was determined as criterion for treatment success with OAm. The OAm treatment efficacy rate was 43%.
Motorized RCMP Prototypes
Tsai et al.30 conducted a study with 19 patients with mean baseline AHI of 34 events/h (range: 15–89 events/h). An overnight level III home sleep study was performed both at baseline and with OAm. Motorized RCMP titration was performed during full night PSG in the sleep laboratory. With the patient in stable stage 2 sleep, the mandible was remotely protruded in 1-mm increments until optimal advancement. The titration night was scored “predictive” for OAm treatment success if the majority of apneas, hypopneas, and oxygen desaturations were eliminated with a total amount of advancement of < 15 mm. OAm therapy was scored “successful” if all of the following criteria were met: AHI < 15 events/h, AHI was reduced by more than 30% from baseline, and subjective improvement in symptoms. The mean AHI was significantly reduced after treatment with OAm at optimal advancement. The predictive ability of RCMP showed successful OAm therapy in 9 of 10 patients with RCMP predicted success. Eight patients were unsuccessful with OAm therapy, as RCMP predicted failure in nine patients. Tsai et al.30 concluded that the RCMP test had a high positive (90%) and negative (89%) predictive value for predicting OAm treatment outcome (Table 3).
Dort et al.28 completed a titration study with 33 recruited patients on the basis of an initial ambulatory level III home sleep study. The mean baseline AHI was 27 events/h. During the polysomnographic evaluation the mandible was advanced in 1-mm increments following documentation of obstructive respiratory events in stage 2 sleep. Mandibular advancement continued until elimination of obstructive apneas, hypopneas, and nocturnal oxygen desaturation was achieved or until maximal protrusion was reached. The RCMP test results were scored successful if obstructive events and snoring were eliminated. The RCMP test was a success in 15 of 33 (45%) and failed in 18 of 33 (55%). When the RCMP test was successful, OAm was set at the protrusive distance in which obstructive events and snoring were eliminated as determined during polysomnographic titration with RCMP (Figure 2B). Dort et al.28 reported that when the RCMP test failed the OAm was set at a protrusive distance of two-thirds of the subject's protrusive capabilities. The home sleep study with the portable monitor was repeated to assess the OAm outcome. OAm therapy was successful in 12 of 15 subjects (80%) who had a successful RCMP test and failed in 14 of 18 (78%), when RCMP test was a failure. A significant association (p = 0.001) between the results of the RCMP titration PSG and the treatment outcome with OAm was observed. The sensitivity and specificity of the RCMP test were 75% and 82%, respectively, as summarized in Table 3.
Commercially Available Motorized RCMP
Remmers et al.29 recruited 67 patients with OSA with a mean baseline AHI of 25 events/h (range: 11–56 events/h) in a level III sleep study. The mandible was protruded in 0.2- to 0.6-mm steps with RCMP (Figure 2C) during PSG in response to evidence of respiratory events, i.e., apneas and hypopneas. The RCMP study was deemed to predict OAm “therapeutic success” if a minimum 5-min interval, continuous or fragmented, where a frequency of one or fewer respiratory events occurred, was identified during REM sleep. The RCMP test results were scored by a sleep physician, who was blinded to all data of the patient, to determine in which patients the study was deemed to predict OAm “therapeutic success” and in which patients OAm “therapeutic failure” was expected. Furthermore, the ETPP provided efficacious mandibular protrusion in most patients with a RCMP test predicting OAm treatment success. In patients with predicted failure, OAm was set at a sham position equal to 70% of anteroposterior range of motion. The effectiveness of OAm was evaluated in a level III sleep study. RCMP mandibular titration PSG predicted therapeutic outcome with OAm with significant accuracy (p < 0.05), particularly with regard to predicting therapeutic success resulting in a high positive predictive value of 94%. The sensitivity and specificity of the RCMP test were 86% and 92%, respectively (see Table 3). Progressive adjustment was provided to produce AHI < 10 events/h, as measured by an outcome level III sleep study.
Burschtin et al.60 presented results at the SLEEP conference 2014 after including 46 patients with mean baseline AHI 31 events/h (range: 8–93 events/h). A full night PSG was performed while the RCMP was progressively advanced from baseline to maximum jaw advancement determined prior to the sleep night by a dental sleep professional. Success was defined by 50% reduction in AHI if AHI was < 20 events/h or AHI < 15 events/h. In 25 patients a mean baseline AHI 35 events/h dropped to 9 events/h with RCMP titration and were thus responders. Twenty-one patients were non-responders with a baseline AHI 27 events/h and AHI 25 events/h with RCMP. Evaluation with OAm in the position determined by RCMP was not described in this abstract.60
Automatically Adjusting Mandibular Positioner
A concept of an auto-adjusting RCMP was presented in an 2015 AADSM abstract by Brugarolas et al.56 consisting of a commercially available OAm, fabricated with a OAm-specific pneumatic actuator add-on capable of changing the position of the jaw. The actuator was connected to a small syringe pump connected to a controller. The controller wirelessly received signals from respiratory sounds sampled from the add-on in the patient's mouth, from a digital pulse oximeter and from a body position sensor. Changes in jaw position could be specified in response to respiratory related signals after short (a few consecutive breaths) or longer (a few consecutive nights) periods of time. A pilot testing was performed in one male adult. It turned out to be possible to advance jaw position as part of an auto-adjusting OAm.
Three abstracts54,55,57 described the use of auto-RCMP and were published by the same research group of Dr. John Remmers and his colleagues. The abstracts described an RCMP test that predicts outcome with OAm not only during attended sleep studies, but also unattended using an auto-titrating mandibular positioner in the home setting. One hundred twenty-eight patients were evaluated with a broad range of severity of OSA with a mean AHI of 25 events/h. The patients were studied for 2 nights at home using a temporary dental appliance attached to a computer-controlled actuator. The first night involved continuous repositioning of the mandible driven by the occurrence of respiratory events until AHI < 10 events/h. In the second night the mandible was held at a position predicted to be efficacious during the first night. Therapeutic success was defined as an outcome AHI < 10 events/h and 50% reduction of baseline AHI. Investigations predicting success were assigned an ETPP derived from the registration, and those predicting failure received a sham value of 70% maximal protrusion. Each patient received a custom OAm that was set to ETPP or the sham value. Baseline and OAm outcome AHI values were the mean of 2 nights each of home sleep testing. The overall therapeutic success rate with OAm was 74%. Prospective prediction rules showed a sensitivity of 82% and specificity of 76%, which yielded statistically significant predictive accuracy. Of 83 patients with RCMP predicted therapeutic success, 75 were therapeutically successful. The positive predictive value was thus high at 90% whereas the negative predictive value was less favorable being 61% (Table 3).
DISCUSSION
This paper provides an overview on the past evolution and the current evidence of the use of RCMP in detail and evaluates the efficacy of RCMP as a predictive tool for treatment of OSA with OAm, focusing on single-night titration. The existing evidence regarding the use of RCMP in OSA illustrates that it might be possible to protrude the mandible progressively during sleep under poly(somno)graphic observation by RCMP until respiratory events are eliminated without disturbing sleep or arousing the patient. In addition, it has been shown that an ETPP can be measured with RCMP and that this ETPP is correlated with success of OAm therapy with a relatively high sensitivity and specificity (see Table 3).
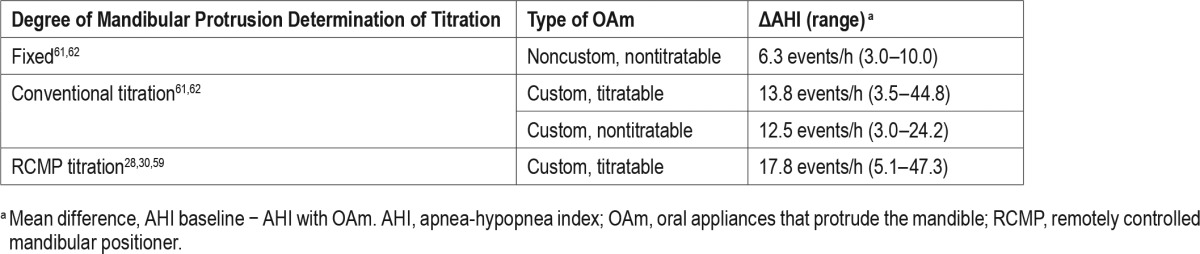
Table 4 provides the range of AHI changes during OAm therapy as compared to baseline, in relation to the different methods for determining the therapeutic degree of mandibular protrusion. The mean AHI reduction is expressed as ΔAHI (baseline − AHI with OAm). The treatment success obtained through the use of the RCMP is greater than the success obtained by conventional titration methods or no titration (Table 4). This emphasizes the additional value of determining an ETPP by RCMP. The most recent Clinical Practice Guideline by the American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine (AADSM)61,62 recommends the use of a custom, titratable OAm over noncustom OAm in all patients.
Table 4.
Characteristics of titration and treatment outcome with oral appliances that protrude the mandible based on remotely controlled mandibular positioner studies28,30,59 and clinical practice guidelines for OAm61,62
From a financial perspective the use of RCMP might be attractive for patients, as predicted success allows for reassurance that investment in an OAm is worthwhile. In conventional OAm titration protocols, the time interval ranges from weeks to months with several visits.19 A reduced number of visits for OAm titration is expected as ETPP is already determined during RCMP night, thereby reducing individual costs. Also the commercially available motorized RCMP is being reimbursed under existing codes for PSG in the United States of America and Canada.29 Follow-up testing is thought to be appropriate to evaluate therapeutic success with OAm after conventional titration.61,62 A polysomnographic study is the gold standard, but is relatively expensive. It could be questioned if follow-up testing is required after successful RCMP titration and fitting of OAm at fixed ETPP. For clinicians, individualized and optimized OSA management may result in higher patient turnover. However, an investment in special software and equipment has to be made in order to perform an RCMP procedure.
Based on the results of the studies in this concise review,28–30,59 a mandibular titration study with RCMP tends to predict therapeutic outcome with OAm with significant accuracy and could, therefore, be helpful to prospectively select patients with OSA that could be successfully treated with an OAm.29 One of the contributions of an overnight titration study using an RCMP was to provide a direct avenue to successful OAm therapy for patients who might otherwise not be considered for OAm as a first- or second-line therapy, e.g., obese patients with severe sleep apnea. Accordingly, RCMP titration might increase efficiency, reduce the time to successful treatment, decrease costs, and improve the overall therapeutic outcome.29 The negative predictive capability of the RCMP test could also be of potential clinical value in informing patients about the possible treatment options. When the result of the RCMP test was negative or equivocal, the patient could be informed in advance that the probability of being successfully treated with an OAm is rather poor. Giving such information to patients might enhance their acceptance of CPAP therapy.28 Alternatively, the finding of negative or equivocal RCMP test results might indicate the patient as a proper candidate for surgical therapy after proper upper airway assessment, e.g., by means of DISE and/or imaging.32,37,45
Furthermore, the importance of positional OSA (POSA), also known as supine-dependent OSA, has been highlighted.63 POSA is most common in the category of mild to moderate OSA.64 This phenomenon has been evaluated during DISE by assessing the upper airway of the patient in different body positions.65 DISE is usually performed in supine position, but the obstruction pattern of the upper airway appears to be different when DISE is performed in the lateral position.66 The outcomes of DISE performed with full body in the lateral position or head only in lateral position showed similar results in upper airway collapse pattern.65 The only exception is an anteroposterior collapse at the level of the velum. During lateral head rotation only, the collapse is less severe than during both lateral head and trunk position.65 One should take into account the influence and importance of different sleeping positions on upper airway collapse patterns during RCMP use in patients with OSA and POSA.
The results of the included studies (Table 2 and Table 3) in this review demonstrate that the ETPP for treatment with OAm could be predicted during an RCMP titration registration. This predictive capability of the RCMP study might have considerable clinical utility as no validated method for predicting an efficacious mandibular protrusive position was currently available. By using the RCMP to predict the ETPP, the time and number of dental visits could be decreased and the risk of over-protruding the mandible of the patient could be reduced. Furthermore, it should be possible to efficaciously treat the patient instantly from night 1, when the ETPP was predicted by the RCMP mandibular titration study29 on the condition that the patient could tolerate the ETPP. The possibility of predicting the ETPP should also increase OAm adherence and decrease the need for extensive titration capabilities of an oral appliance.28
These studies applied a prospective and blinded design. Because neither PSG technician, dental sleep professional, sleep physician, nor patient were informed about the results, no one was able to bias the final results. In the studies from Tsai et al.30 and Dort et al.28 the predictive criteria to consider an RCMP test as being successful, were less explicitly defined in comparison with the criterion used by Remmers et al.29 (Table 3).
Another possible advantage when using RCMP might be that the patients do not have to be awakened to perform the titration of the OAm during sleep.29,30 If patients had to be awakened to titrate the OAm, this could have had an effect on the sleep architecture of the patient and consequently influence the outcome of the titration study.67,68
The first pilot study by Pételle et al.59 demonstrated that it was possible to perform advancement of the mandible during PSG, without arousing the patient. These results suggested that the efficacy of OAm therapy and the effective degree of mandibular advancement could be predicted during a polysomnographic recording.
Some practical decisions made by the different study groups make it difficult, however, to compare the different studies.
First, the predictive criteria to consider an RCMP test as being successful differed between the studies (Table 3). Pételle et al.59 started RCMP titration after the first REM sleep episode. Tsai et al.30 and Dort et al.28 titrated with RCMP during stage 2 of sleep. For titration in the study of Remmers et al.29 REM sleep was necessary for determining prediction of success. Criticism could be directed toward the choice of criteria of success with OAm, such as cutoff of AHI 10 events/h, 15 events/h with or without a certain reduction percentage of the initial AHI. This makes it difficult to compare results in the current review, also because of the relatively small number of patients. The problem with small differences of AHI have been well illustrated in other studies30,69,70 where OAm treatment efficacy rate ranged from 43% to 71%, strongly depending on success criteria. Nevertheless, this rate was more or less comparable with the therapeutic efficacy rates in the existing literature ranging from 50% to 80%.30
Second, through the years, changing definitions of hypopnea in terms of desaturation in oxygen (≥ 3% versus ≥ 4%) with or without reduction of air flow (minimum 30% versus minimum 50%) have made results in AHI of sleep studies less comparable.2,3
Third, the study population of Pételle et al.59 was composed of patients with particularly severe OSA with baseline mean AHI = 67 events/h (range: 30–106 events/h). These results were therefore not fully comparable with the other study groups with a baseline mean AHI of 34 events/h, 27 events/h, and 25 events/h, respectively.28–30 In the study of Pételle et al.,59 average AHI decreased successfully by 56% during RCMP titration night and by 69% during OAm treatment evaluation, respectively. However, the treatment efficacy rate was only 43% when the criterion of success with OAm would be set at AHI < 10 events/h.
Furthermore, Pételle et al.59, Tsai et al.,30 and Dort et al.28 advanced the mandible in 1-mm increments, Remmers et al.29 protruded the mandible in 0.2- to 0.6-mm steps, in response to evidence of respiratory events. In order to constitute conclusive predictive data, in the study of Remmers et al.29 the participant should have undergone REM sleep for ≥ 5 min in the supine position or, if REM supine was not observed, in the lateral decubitus position as long as the baseline study indicated that the participant slept for most of the night in the lateral position. Success was predicted when ≤ 1 apnea and/or hypopnea occurred per 5 min of REM. This criterion strongly differs from the other studies,28,30,59 as stable stage 2 sleep was required for titration in the studies of Tsai et al.30 and Dort et al.28 In the study by Pételle et al.,59 mandibular titration was started after the first episode of REM sleep or after 2 h of recording after sleep onset. These differences in titration methods may influence eventual outcome and interpretation of results, as Remmers et al.29 rely solely on events during REM sleep for prediction purposes. All sleep stages have their own characteristics; typical for REM sleep is inhibition of motor neurons that induces muscle atonia and thus higher collapsibility of the upper airway.71
In addition, different types of OAm were used for OAm treatment. Tsai et al.30 and Dort et al.28 used the OAm Klearway (Space Maintainers Laboratories Canada Ltd., Vancouver, Canada), whereas a SomnoDent (SomnoMed) OAm was used in the study of Remmers et al.29 At this stage, regarding the OAm devices used in the respective studies, it is not yet known how the differences in OAm design would influence the therapy outcome.
A limitation of some of the selected studies28–30 was the use of a level III portable sleep monitor. This method has been validated in the sleep laboratory, but not in the home setting.29 Also, the possibilities of home-based auto-titrating mandibular positioners should be further explored to decrease the current false prediction rate of 19%.59 If AHI values derived from a baseline and outcome sleep study under polysomnographic monitoring were used, the predictive accuracy of the RCMP titration night probably would have been greater.29 Some articles suggest that treating OSA with AHI < 17 events/h separately increases the overall predictive accuracy.59 However, this statement requires prospective confirmation and is based on retrospective analysis.59
These studies28–30 illustrated the importance of patient selection, but addressed the need of separate evaluation of the long-term utility of suboptimal advancement, cost-effectiveness, prediction of futility, and sustained efficacy. There was a high risk of bias, but the available information on the validity of predictive index tests is very useful in clinical practice and allows for greater disease management efficiency.72 This was demonstrated in a recent case report on a morbid obese patient with REM-related moderate OSA.73 An RCMP provided objective efficacy data at specific protrusive positions. This allows the sleep physician to confidently prescribe an OAm at a predetermined target protrusion, as many physicians may have dissuaded from prescribing an OAm.73
Prospective identification of potential successful OAm candidates with instant determination of the ETPP is desirable from both a therapeutic and financial perspective. This review illustrates that the use of a RCMP during sleep studies has a clear potential in this particular purpose of selecting the proper patients for OAm treatment and in order to determine the ETPP.
In the future, it should be investigated whether the RCMP device could also be applied during awake endoscopy, drug-induced sedation endoscopy, or imaging studies. Vroegop et al.38 demonstrated that the use of a simulation bite during DISE is of predictive value for treatment outcome with OAm. Investigating the effect of progressive mandibular advancement on the upper airway of the patient, by using an RCMP during DISE, might be of additional value for the field. Civelek et al.17 compared conventional CPAP titration night during PSG with DISE-assisted CPAP titration. No statistically significant differences between the two techniques were observed. A limitation of DISE is the inability to induce REM sleep with the current methodology using midazolam and propofol.37,74 DISE-assisted CPAP titration was suggested as a cheaper and less time-consuming alternative to conventional CPAP titration during full-night PSG with similar results. Future research should assess the value of OAm titration during DISE as compared to OAm titration protocols during poly(somno)graphy.
CONCLUSIONS
The current literature review on the use of RCMP demonstrated that the RCMP could be a promising tool to prospectively predict OAm treatment outcome during a single-night titration study in the individual patient. Furthermore, the RCMP could effectively predict the ETPP during the RCMP titration studies.
DISCLOSURE STATEMENT
This was not an industry supported study. Prof. Hamans is consultant for Philips and investigator for ReVent and Nyxoah. Prof. Dr. Braem is promoter of a research grant from SomnoMed Ltd. at Antwerp University Hospital (2013–2016). Prof. Dr. Vanderveken is speaker and co-promoter of a research grant from SomnoMed Ltd. at Antwerp University Hospital (2013–2016), received research support for Inspire Medical Systems as consultant and speaker, received research support from Nyxoah as consultant, is consultant for Philips Electronics and is investigator and speaker for Nightbalance. The other authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- AADSM
American Academy of Dental Sleep Medicine
- AHI
apnea-hypopnea index
- ATS
American Thoracic Society
- CPAP
continuous positive airway pressure
- DISE
drug-induced sedation endoscopy
- ETPP
effective target protrusive position
- OAm
oral appliances that protrude the mandible
- OSA
obstructive sleep apnea
- POSA
positional OSA
- PSG
polysomnography
- RCMP
remotely controlled mandibular positioner
- REM
rapid eye movement
REFERENCES
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 3.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anandam A, Patil M, Akinnusi M, Jaoude P, El-Solh AA. Cardiovascular mortality in obstructive sleep apnoea treated with continuous positive airway pressure or oral appliance: an observational study. Respirology. 2013;18:1184–90. doi: 10.1111/resp.12140. [DOI] [PubMed] [Google Scholar]
- 5.He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988;94:9–14. [PubMed] [Google Scholar]
- 6.Kendzerska T, Gershon AS, Hawker G, Leung RS, Tomlinson G. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med. 2014;11:e1001599. doi: 10.1371/journal.pmed.1001599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marin JM, Carizzo SJ, Vincente E, Ahgusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 8.Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290:1906–14. doi: 10.1001/jama.290.14.1906. [DOI] [PubMed] [Google Scholar]
- 9.Vanderveken OM, Boudewyns A, Ni Q, et al. Cardiovascular implications in the treatment of obstructive sleep apnea. J Cardiovasc Trans Res. 2011;4:53–60. doi: 10.1007/s12265-010-9238-y. [DOI] [PubMed] [Google Scholar]
- 10.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373:82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 11.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 12.Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1:862–5. doi: 10.1016/s0140-6736(81)92140-1. [DOI] [PubMed] [Google Scholar]
- 14.Grote L, Hedner J, Grunstein R, Kraiczi H. Therapy with nCPAP: incomplete elimination of Sleep Related Breathing Disorder. Eur Respir J. 2000;16:921–7. doi: 10.1183/09031936.00.16592100. [DOI] [PubMed] [Google Scholar]
- 15.Lindberg E, Berne C, Elmasry A, Hedner J, Janson C. CPAP treatment of a population-based sample--what are the benefits and the treatment compliance? Sleep Med. 2006;7:553–60. doi: 10.1016/j.sleep.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc AmThorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Civelek S, Emre IE, Dizdar D, et al. Comparison of conventional continuous positive airway pressure to continuous positive airway pressure titration performed with sleep endoscopy. Laryngoscope. 2012;122:691–5. doi: 10.1002/lary.22494. [DOI] [PubMed] [Google Scholar]
- 18.Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10:215–27. doi: 10.5664/jcsm.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dieltjens M, Vanderveken OM, Heyning PH, Braem MJ. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev. 2012;16:177–85. doi: 10.1016/j.smrv.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Ng AT, Gotsopoulos H, Qian J, Cistulli PA. Effect of oral appliance therapy on upper airway collapsibility in obstructive sleep apnea. Am J Respir Crit Care Med. 2003;168:238–41. doi: 10.1164/rccm.200211-1275OC. [DOI] [PubMed] [Google Scholar]
- 21.Strollo PJ., Jr Another advance in oral appliance therapy? Sleep. 2013;36:1417–8. doi: 10.5665/sleep.3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vanderveken OM, Dieltjens M, Wouters K, De Backer WA, Van de Heyning PH, Braem MJ. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax. 2013;68:91–6. doi: 10.1136/thoraxjnl-2012-201900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dieltjens M, Braem MJ, Vroegop AV, et al. Objectively measured vs selfreported compliance during oral appliance therapy for sleep-disordered breathing. Chest. 2013;144:1495–502. doi: 10.1378/chest.13-0613. [DOI] [PubMed] [Google Scholar]
- 24.Chan AS, Cistulli PA. Oral appliance treatment of obstructive sleep apnea: an update. Curr Opin Pulm Med. 2009;15:591–6. doi: 10.1097/MCP.0b013e3283319b12. [DOI] [PubMed] [Google Scholar]
- 25.Vanderveken OM, Braem MJ, Dieltjens M, De Backer WA, Van de Heyning PH. Objective measurement of the therapeutic effectiveness of continuous positive airway pressure versus oral appliance therapy for the treatment of obstructive sleep apnea. Am J Respir Crit Care Med. 2013;188:1162. doi: 10.1164/rccm.201305-0809LE. [DOI] [PubMed] [Google Scholar]
- 26.Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med. 2013;187:879–87. doi: 10.1164/rccm.201212-2223OC. [DOI] [PubMed] [Google Scholar]
- 27.Vanderveken OM. Drug-induced sleep endoscopy (DISE) for non-CPAP treatment selection in patients with sleep-disordered breathing. Sleep Breath. 2013;17:13–4. doi: 10.1007/s11325-012-0671-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dort LC, Hadjuk E, Remmers JE. Mandibular advancement and obstructive sleep apnoea: a method for determining effective mandibular protrusion. Eur Respir J. 2006;27:1003–9. doi: 10.1183/09031936.06.00077804. [DOI] [PubMed] [Google Scholar]
- 29.Remmers J, Charkhandeh S, Grosse J, et al. Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea. Sleep. 2013;36:1517–25. 25A. doi: 10.5665/sleep.3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsai WH, Vazquez JC, Oshima T, et al. Remotely controlled mandibular positioner predicts efficacy of oral appliances in sleep apnea. Am J Respir Crit Care Med. 2004;170:366–70. doi: 10.1164/rccm.200310-1446OC. [DOI] [PubMed] [Google Scholar]
- 31.Vanderveken OM, Devolder A, Marklund M, et al. Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med. 2008;178:197–202. doi: 10.1164/rccm.200701-114OC. [DOI] [PubMed] [Google Scholar]
- 32.Denolf PL, Vanderveken OM, Marklund ME, Braem MJ. The status of cephalometry in the prediction of non-CPAP treatment outcome in obstructive sleep apnea patients. Sleep Med Rev. 2015;27:56–73. doi: 10.1016/j.smrv.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 33.Chan AS, Lee RW, Srinivasan VK, Darendeliler MA, Grunstein RR, Cistulli PA. Nasopharyngoscopic evaluation of oral appliance therapy for obstructive sleep apnoea. Eur Respir J. 2010;35:836–42. doi: 10.1183/09031936.00077409. [DOI] [PubMed] [Google Scholar]
- 34.Battagel JM, Johal A, Kotecha BT. Sleep nasendoscopy as a predictor of treatment success in snorers using mandibular advancement splints. J Laryngol Otol. 2005;119:106–12. doi: 10.1258/0022215053419916. [DOI] [PubMed] [Google Scholar]
- 35.Johal A, Battagel JM, Kotecha BT. Sleep nasendoscopy: a diagnostic tool for predicting treatment success with mandibular advancement splints in obstructive sleep apnoea. Eur J Orthod. 2005;27:607–14. doi: 10.1093/ejo/cji063. [DOI] [PubMed] [Google Scholar]
- 36.Eichler C, Sommer JU, Stuck BA, Hormann K, Maurer JT. Does drug-induced sleep endoscopy change the treatment concept of patients with snoring and obstructive sleep apnea? Sleep Breath. 2013;17:63–8. doi: 10.1007/s11325-012-0647-9. [DOI] [PubMed] [Google Scholar]
- 37.De Vito A, Carrasco Llatas M, Vanni A, et al. European position paper on drug-induced sedation endoscopy (DISE) Sleep Breath. 2014;18:453–65. doi: 10.1007/s11325-014-0989-6. [DOI] [PubMed] [Google Scholar]
- 38.Vroegop AV, Vanderveken OM, Dieltjens M, et al. Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res. 2013;22:348–55. doi: 10.1111/jsr.12008. [DOI] [PubMed] [Google Scholar]
- 39.Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65:726–32. doi: 10.1136/thx.2009.131094. [DOI] [PubMed] [Google Scholar]
- 40.Stuck BA, Maurer JT. Airway evaluation in obstructive sleep apnea. Sleep Med Rev. 2008;12:411–36. doi: 10.1016/j.smrv.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 41.Ikeda K, Ogura M, Oshima T, et al. Quantitative assessment of the pharyngeal airway by dynamic magnetic resonance imaging in obstructive sleep apnea syndrome. Ann Otol Rhinol Laryngol. 2001;110:183–9. doi: 10.1177/000348940111000215. [DOI] [PubMed] [Google Scholar]
- 42.Schwab RJ, Pasirstein M, Pierson R, et al. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med. 2003;168:522–30. doi: 10.1164/rccm.200208-866OC. [DOI] [PubMed] [Google Scholar]
- 43.Yucel A, Unlu M, Haktanir A, Acar M, Fidan F. Evaluation of the upper airway cross-sectional area changes in different degrees of severity of obstructive sleep apnea syndrome: cephalometric and dynamic CT study. AJNR Am J Neuroradiol. 2005;26:2624–9. [PMC free article] [PubMed] [Google Scholar]
- 44.Kyung SH, Park YC, Pae EK. Obstructive sleep apnea patients with the oral appliance experience pharyngeal size and shape changes in three dimensions. Angle Orthod. 2005;75:15–22. doi: 10.1043/0003-3219(2005)075<0015:OSAPWT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 45.De Backer JW, Vos WG, Verhulst SL, De Backer W. Novel imaging techniques using computer methods for the evaluation of the upper airway in patients with sleep-disordered breathing: a comprehensive review. Sleep Med Rev. 2008;12:437–47. doi: 10.1016/j.smrv.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 46.Zhao M, Barber T, Cistulli PA, Sutherland K, Rosengarten G. Simulation of upper airway occlusion without and with mandibular advancement in obstructive sleep apnea using fluid-structure interaction. J Biomech. 2013;46:2586–92. doi: 10.1016/j.jbiomech.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 47.Vos W, De Backer J, Devolder A, et al. Correlation between severity of sleep apnea and upper airway morphology based on advanced anatomical and functional imaging. J Biomech. 2007;40:2207–13. doi: 10.1016/j.jbiomech.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 48.Jeong SJ, Kim WS, Sung SJ. Numerical investigation on the flow characteristics and aerodynamic force of the upper airway of patient with obstructive sleep apnea using computational fluid dynamics. Med Eng Phys. 2007;29:637–51. doi: 10.1016/j.medengphy.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 49.De Backer JW, Vanderveken OM, Vos WG, et al. Functional imaging using computational fluid dynamics to predict treatment success of mandibular advancement devices in sleep-disordered breathing. J Biomech. 2007;40:3708–14. doi: 10.1016/j.jbiomech.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 50.Van Holsbeke C, De Backer J, Vos W, et al. Anatomical and functional changes in the upper airways of sleep apnea patients due to mandibular repositioning: a large scale study. J Biomech. 2011;44:442–9. doi: 10.1016/j.jbiomech.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 51.Zhao M, Barber T, Cistulli P, Sutherland K, Rosengarten G. Computational fluid dynamics for the assessment of upper airway response to oral appliance treatment in obstructive sleep apnea. J Biomech. 2013;46:142–50. doi: 10.1016/j.jbiomech.2012.10.033. [DOI] [PubMed] [Google Scholar]
- 52.Kato J, Isono S, Tanaka A, et al. Dose-dependent effects of mandibular advancement on pharyngeal mechanics and nocturnal oxygenation in patients with sleep-disordered breathing. Chest. 2000;117:1065–72. doi: 10.1378/chest.117.4.1065. [DOI] [PubMed] [Google Scholar]
- 53.Aarab G, Lobbezoo F, Hamburger HL, Naeije M. Effects of an oral appliance with different mandibular protrusion positions at a constant vertical dimension on obstructive sleep apnea. Clin Oral Invest. 2010;14:339–45. doi: 10.1007/s00784-009-0298-9. [DOI] [PubMed] [Google Scholar]
- 54.Remmers J, Topor Z, Grosse J, et al. Selection of patients for oral appliance therapy using an auto-titrating mandibular positioner in the home. Sleep. 2015;38:A193–4. (Abstract Suppl) [Google Scholar]
- 55.Topor Z, Grosse J, Zareian Jahromi S, et al. Predicting oral appliance therapy outcome using an auto-adjusting mandibular positioner in the home. Am J Respir Crit Care Med. 2015;191:A2472. [Google Scholar]
- 56.Brugarolas R, Valero-Sarmiento J, Essick G. Development of an auto-adjusting mandibular repositioning device for in-home use. J Dent Sleep Med. 2015;2:134–5. doi: 10.1109/EMBC.2016.7591677. [DOI] [PubMed] [Google Scholar]
- 57.Charkhandeh S, Topor Z, Grosse J, et al. An auto-titrating mandibular positioner: accuracy in predicting oral appliance therapy outcome and efficacious mandibular protrusion. J Dent Sleep Med. 2015;2:136–7. [Google Scholar]
- 58.Liu YH, Zhao XG, Xu BF, Li J, Lu MX. [Computer-aided mandibular repositioning system for efficacy prediction of oral appliance in patients with obstructive sleep apnea-hypopnea syndrome] Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41:86–9. [PubMed] [Google Scholar]
- 59.Pételle B, Vincent G, Gagnadoux F, Rakotonanahary D, Meyer B, Fleury B. One-night mandibular advancement titration for obstructive sleep apnea syndrome: a pilot study. Am J Respir Crit Care Med. 2002;165:1150–3. doi: 10.1164/ajrccm.165.8.2108056. [DOI] [PubMed] [Google Scholar]
- 60.Burschtin O, Binder D, Lim J, Marsiliani S, Ayappa I, Rapoport DM. Mandibular advancement device titration using a remotely controlled mandibular positioner. Sleep. 2014;37:A149. (Abstract Suppl) [Google Scholar]
- 61.Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11:773–827. doi: 10.5664/jcsm.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ramar K, Dort L, Katz S, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Dent Sleep Med. 2015;2:71–125. doi: 10.5664/jcsm.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath. 2013;17:39–49. doi: 10.1007/s11325-012-0683-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Casey KR. Positional therapy is worth a try in patients with mild obstructive sleep apnea. Point-counterpoint: is avoidance of supine sleep an adequate treatment for OSA? J Clin Sleep Med. 2015;11:89–90. doi: 10.5664/jcsm.4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Safiruddin F, Koutsourelakis I, de Vries N. Analysis of the influence of head rotation during drug-induced sleep endoscopy in obstructive sleep apnea. Laryngoscope. 2014;124:2195–9. doi: 10.1002/lary.24598. [DOI] [PubMed] [Google Scholar]
- 66.Safiruddin F, Koutsourelakis I, de Vries N. Upper airway collapse during drug induced sleep endoscopy: head rotation in supine position compared with lateral head and trunk position. Eur Arch Otorhinolaryngol. 2015;272:485–8. doi: 10.1007/s00405-014-3215-z. [DOI] [PubMed] [Google Scholar]
- 67.Raphaelson MA, Alpher EJ, Bakker KW, Perlstrom JR. Oral appliance therapy for obstructive sleep apnea syndrome: progressive mandibular advancement during polysomnography. Cranio. 1998;16:44–50. doi: 10.1080/08869634.1998.11746037. [DOI] [PubMed] [Google Scholar]
- 68.Rodway GW, Sanders MH. The efficacy of split-night sleep studies. Sleep Med Rev. 2003;7:391–401. doi: 10.1053/smrv.2002.0272. [DOI] [PubMed] [Google Scholar]
- 69.Redline S, Kapur VK, Sanders MH, et al. Effects of varying approaches for identifying respiratory disturbances on sleep apnea assessment. Am J Respir Crit Care Med. 2000;161:369–74. doi: 10.1164/ajrccm.161.2.9904031. [DOI] [PubMed] [Google Scholar]
- 70.Tsai WH, Flemons WW, Whitelaw WA, Remmers JE. A comparison of apneahypopnea indices derived from different definitions of hypopnea. Am J Respir Crit Care Med. 1999;159:43–8. doi: 10.1164/ajrccm.159.1.9709017. [DOI] [PubMed] [Google Scholar]
- 71.Eckert DJ, Malhotra A, Lo YL, White DP, Jordan AS. The influence of obstructive sleep apnea and gender on genioglossus activity during rapid eye movement sleep. Chest. 2009;135:957–64. doi: 10.1378/chest.08-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Okuno K, Pliska BT, Hamoda M, Lowe AA, Almeida FR. Prediction of oral appliance treatment outcomes in obstructive sleep apnea: a systematic review. Sleep Med Rev. 2015;30:25–33. doi: 10.1016/j.smrv.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 73.Hogg J. Remote controlled mandibular positional device to determine oral appliance efficacy and therapeutic protrusive position. J Dent Sleep Med. 2016;3:29–30. [Google Scholar]
- 74.Rabelo FA, Kupper DS, Sander HH, Fernandes RM, Valera FC. Polysomnographic evaluation of propofol-induced sleep in patients with respiratory sleep disorders and controls. Laryngoscope. 2013;123:2300–5. doi: 10.1002/lary.23664. [DOI] [PubMed] [Google Scholar]