Abstract
Using mice rendered insulin resistant with high fat diets (HFD), we examined blood glucose levels and insulin resistance after i.v. delivery of an adeno-associated virus type 8 encoding murine urocortin 2 (AAV8.UCn2). A single i.v. injection of AAV8.UCn2-normalized blood glucose and glucose disposal within weeks, an effect that lasted for months. Hyperinsulinemic-euglycemic clamps showed reduced plasma insulin, increased glucose disposal rates, and increased insulin sensitivity following UCn2 gene transfer. Mice with corticotropin-releasing hormone type 2-receptor deletion that were rendered insulin resistant by HFD showed no improvement in glucose disposal after UCn2 gene transfer, indicating that the effect requires UCn2’s cognate receptor. We also demonstrated increased glucose disposal after UCn2 gene transfer in db/db mice, a second model of insulin resistance. UCn2 gene transfer reduced fatty infiltration of the liver in both models of insulin resistance. UCn2 increases Glut4 translocation to the plasma membrane in skeletal myotubes in a manner quantitatively similar to insulin, indicating a mechanism through which UCn2 operates to increase insulin sensitivity. UCn2 gene transfer, in a dose-dependent manner, is insulin sensitizing and effective for months after a single injection. These findings suggest a potential long-term therapy for clinical type-2 diabetes.
Urocortin-2 gene transfer restores insulin sensitivity and reduces fatty infiltration of liver in two models of insulin resistance, suggesting a new therapeutic strategy for type 2 diabetes.
Introduction
The corticotropin-releasing hormone (CRH) family peptides — which includes urocortin 1 (UCn1), urocortin 2 (UCn2), urocortin 3 (UCn3), and others — stimulate CRH receptors 1 and 2 (CRHR1, CRHR2). UCn1 binds CRHR1 and CRHR2, but UCn2 and UCn3 exclusively bind CRHR2, which is present in brain, heart, vasculature, skeletal muscle, and gastrointestinal tract. CRHR2 activation increases satiety, reduces gut motility, increases heart function, and results in vasodilation (1–3).
UCn2, a 38 amino acid peptide, was discovered in 2001 (1). Studies in animals and human subjects with heart failure (HF) have shown favorable effects of UCn2 peptide infusion, including increased cardiac output (4). However, because of a short half-life (minutes) the peptide’s beneficial effects require continuous i.v. infusion, rendering such therapy impractical except for brief use in hospitalized subjects. We therefore investigated the usefulness of UCn2 therapy via gene transfer, which would circumvent the need for continuous i.v. infusion and enable long-term outpatient therapy.
We recently demonstrated in mice that i.v. delivery of an adeno-associated virus type 8 vector encoding murine UCn2 (AAV8.UCn2) results in increased plasma UCn2 levels within 6 weeks, an effect that persists for at least 7 months without inflammation or unfavorable hemodynamic effects (5). In the course of these experiments, it was noted that fasting blood glucose levels were significantly reduced in normal mice that had received UCn2 gene transfer. We therefore conducted studies in 2 murine models of insulin resistance analogous to clinical type 2 diabetes mellitus (T2DM) testing the hypothesis that a single i.v. injection of AAV8.UCn2 would increase glucose disposal by promoting insulin sensitivity.
Results
UCn2 gene transfer: effects in normal mice.
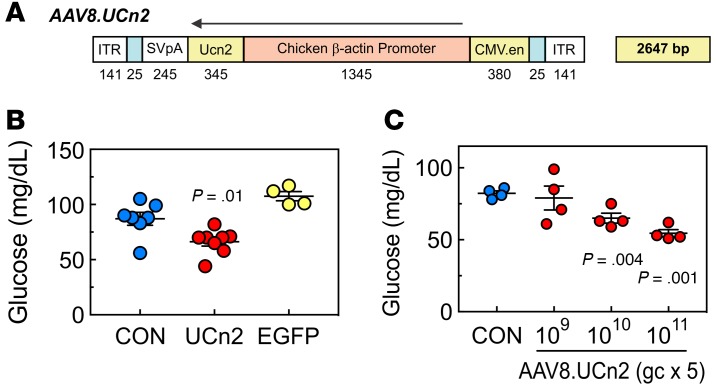
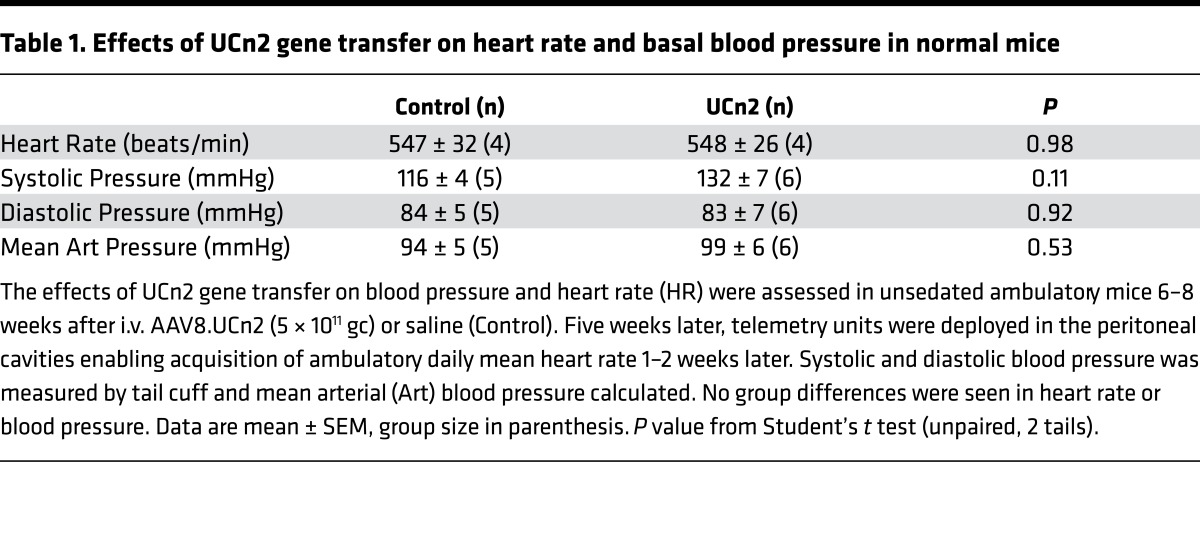
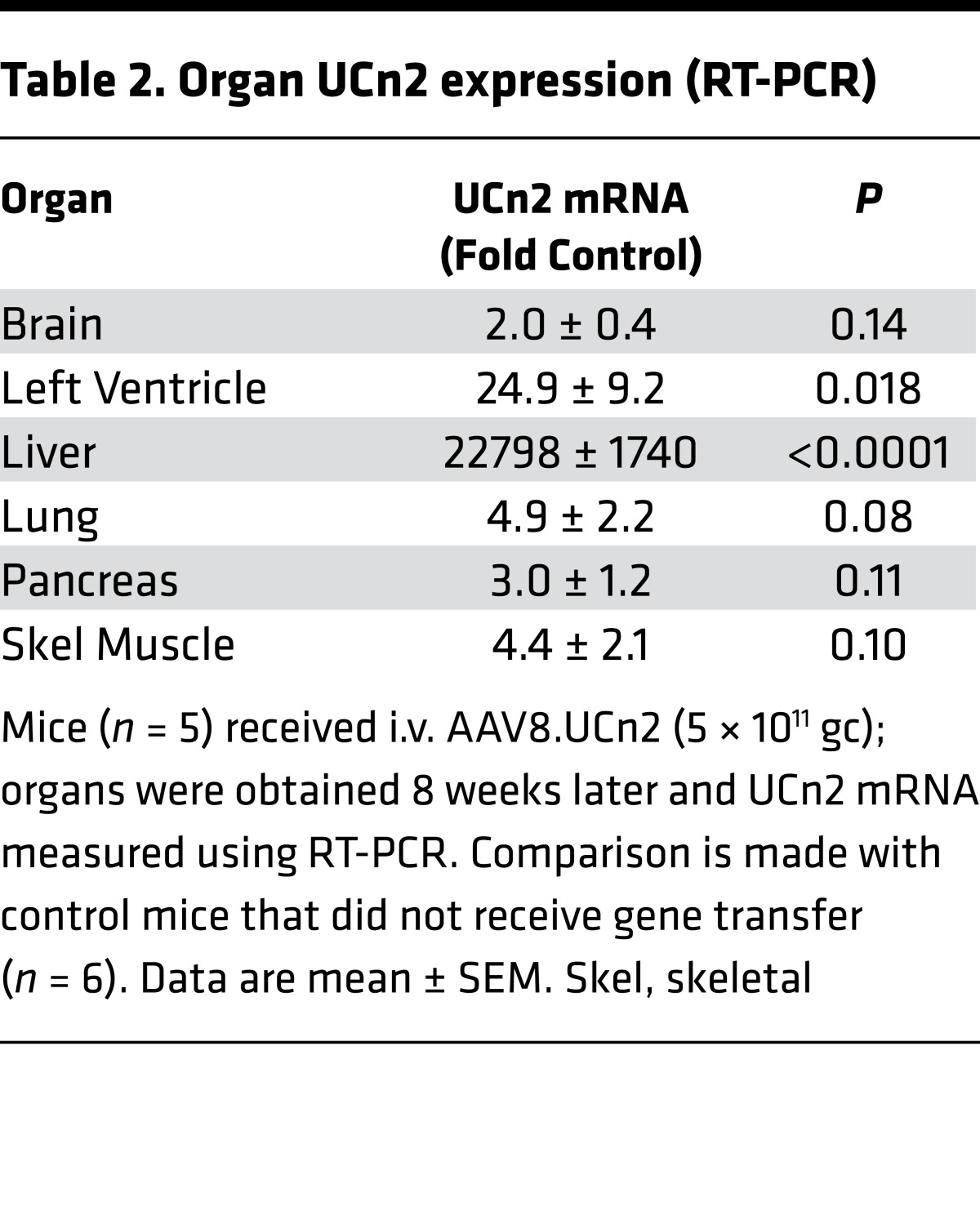
The AAV8.UCn2 vector map is shown in Figure 1A. Intravenous AAV8.UCn2 (5 × 1011 genome copies [gc] per mouse) reduced fasting glucose in normal mice maintained on a standard diet. This effect was transgene specific, since AAV9 encoding EGFP had no effect on fasting glucose (Figure 1B). To determine whether glucose effects were dose related, we used 3 doses of AAV8.UCn2 — 5 × 1011, 5 × 1010, and 5 × 109 gc — and found that the 2 higher doses reduced fasting blood glucose (Figure 1C). We subsequently used 5 × 1011 gc for most of the studies. We found no effect of UCn2 gene transfer on mean daily heart rate or on basal systolic, diastolic, or mean arterial blood pressure 6–8 weeks after gene transfer (Table 1). To assess UCn2 expression, UCn2 mRNA was measured (RT-PCR) in brain, heart, liver, lung, pancreas, and skeletal muscle. UCn2 expression was increased only in left ventricle and liver (Table 2).
Figure 1. Vector map and studies in normal mice on standard diets.
(A) AAV8.UCn2 map. Initial studies in mice determined that AAV8.CBA.UCn2 is the optimal AAV serotype and promoter for the proposed studies resulting in a sustained increase in plasma UCn2 levels over 7 months (5). (B) Fasting glucose. Normal mice received i.v. AAV8.UCn2 (5 × 1011 gc, n = 8), saline (CON, n = 8), or AAV9.EGFP (5 × 1011 gc, n = 4) and standard chow for 3 weeks. A 24% reduction in fasting glucose was seen after AAV8.UCn2 gene transfer (P = 0.01). (C) AAV8.UCn2 dose-glucose response relationship. AAV8.UCn2 doses of 5 × 109 to 5 × 1011 gc produced 21%–33% reduction in fasting glucose levels in normal mice. We selected the highest dose (5 × 1011 gc) for studies conducted in insulin resistant mice. In all graphs, data are mean ±SEM; P values are from Student’s t test for unpaired data, 2 tails, unless stated otherwise.
Table 1. Effects of UCn2 gene transfer on heart rate and basal blood pressure in normal mice.
Table 2. Organ UCn2 expression (RT-PCR).
UCn2 gene transfer and glucose disposal in HFD model of insulin resistance.
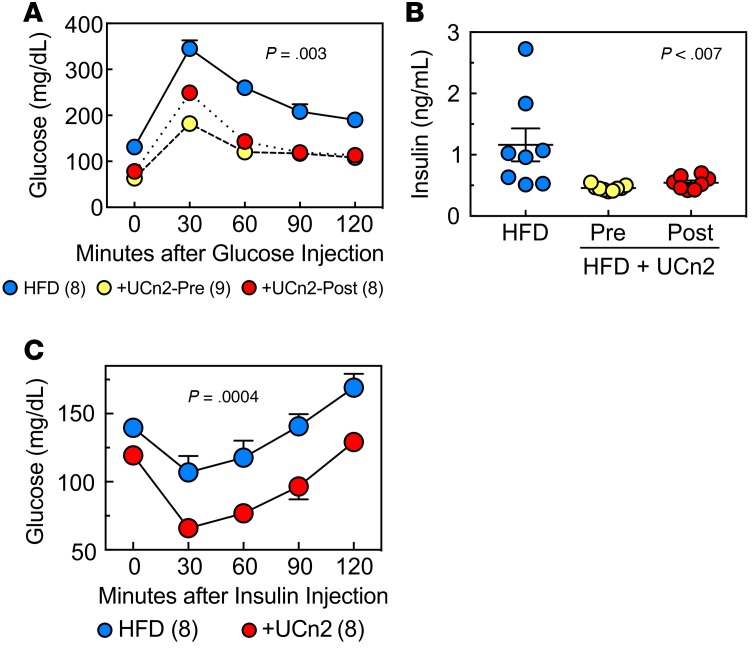
To determine whether UCn2 gene transfer increased glucose disposal in the setting of insulin resistance, we used high fat diets (HFDs) to induce insulin resistance in mice. HFD-fed mice that received UCn2 gene transfer showed consistently lower glucose levels. The AUC in glucose-tolerance tests was reduced by 40%–42% (Figure 2A; P = 0.003). Similar responses on glucose disposal were seen whether UCn2 was delivered before or after the onset of hyperglycemia (Figure 2A), confirming a treatment effect on preexisting hyperglycemia.
Figure 2. UCn2 gene transfer, glucose disposal, and insulin effectiveness in HFD-fed mice.
(A) Glucose tolerance test 16 weeks after HFD, UCn2 gene transfer before (Pre) vs. at 8 Weeks (Post). Mice received glucose (2 mg/g, i.p.), and glucose was measured sequentially for 120 min. AUC was reduced in mice that had received UCn2 gene transfer, whether it was administered before (+UCn2-Pre; n = 8) or 8 weeks after initiation of HFD (+UCn2-Post; n = 8) (P = 0.003, AUC). The similarity of UCn2-Pre and UCn2-Post glucose levels indicates that UCn2 not only prevented HFD-induced hyperglycemia, but also reduced it once present, indicating a treatment effect. (B) Plasma insulin. UCn2 gene transfer was associated with reduced insulin levels whether given before (Pre) or 8 weeks after (Post) initiation of HFD (P < 0.007; ANOVA). (C) Insulin tolerance test. Nonfasted mice received insulin (0.75 U/kg, i.p.) and blood glucose was assessed. UCn2 gene transfer (given at initiation of HFD) was associated with increased insulin sensitivity (P = 0.0004).
UCn2 gene transfer and effects on plasma insulin in HFD-induced insulin resistance.
UCn2 gene transfer was associated with reduction in plasma insulin levels in nonfasting mice (Figure 2B; P < 0.007) and promoted insulin-dependent glucose disposal (Figure 2C; P = 0.0004). Plasma C-peptide levels were similarly reduced (HFD: 5.4 ± 1.2 ng/ml, n = 3; HFD + UCn2: 1.0 ± 0.2 ng/ml, n = 8; P < 0.0002).
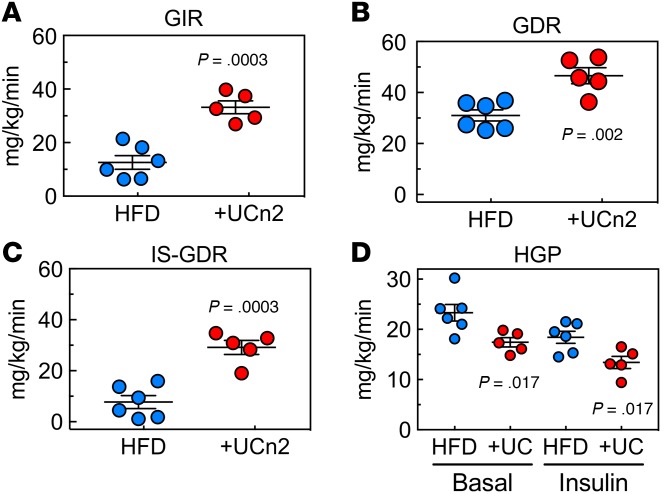
Hyperinsulinemic-euglycemic clamp in HFD-induced insulin resistance.
The hyperinsulinemic-euglycemic clamp was used to assess insulin sensitivity in normal mice rendered insulin resistant with a HFD. After UCn2 gene transfer, HFD-fed mice required a 2.6-fold increased glucose infusion rate to maintain blood glucose levels (Figure 3A; P = 0.0003). In addition, there was a 1.5-fold increase in glucose disposal rate (P = 0.002, Figure 3B) and a 3.8-fold increase in insulin-stimulated glucose disposal rate (P = 0.0003, Figure 3C), which reflects skeletal muscle insulin sensitivity. Hepatic glucose production (HGP) showed no group difference in the percentage by which insulin suppressed HGP (HFD: 21.6% ± 5.8%, n = 6; HFD + UCn2: 22.4% ± 7.5%, n = 5; P = 0.94). However, HGP was lower in mice that had received UCn2 gene transfer both before and after insulin stimulation (Figure 3D).
Figure 3. Hyperinsulinemic-euglycemic clamp.
Fasted (6 hr) HFD-fed mice received constant infusion of insulin and 3H-glucose tracer but variable glucose infusion rates to maintain blood glucose levels. Glucose infusion rate was recorded for 2 hr during the clamp, and blood was obtained before and after the clamp. Mice fed HFD and subsequent UCn2 gene transfer: (A) required higher glucose infusion rates (GIR) to maintain euglycemia during the clamp; (B) showed increased glucose disposal rate (GDR); (C) showed increased insulin-stimulated glucose disposal rate (IS-GDR), indicating increased insulin sensitivity; and (D) showed reductions in hepatic glucose production (HGP) before and after insulin stimulation. The relative reductions in HGP during insulin stimulation showed no group difference. HFD, high fat diet; UCn2, UC: urocortin-2 gene transfer.
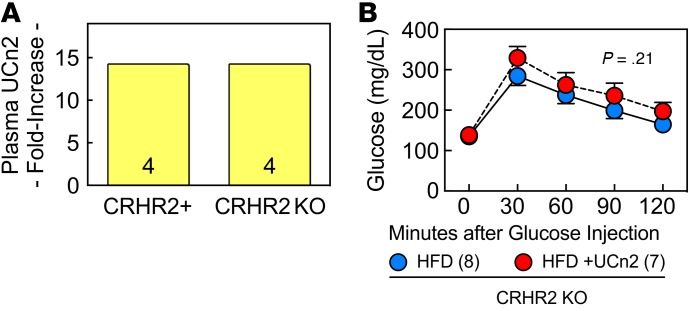
Effects of UCn2 gene transfer in HFD-fed CRHR2-deleted mice.
We next studied CRHR2-deleted mice to determine whether UCn2’s effects on glucose disposal required activation of its cognate receptor, CRHR2. CRHR2-deleted mice fed HFD for 17 weeks gained weight (Pre: 22.5 ± 0.9 g; 16 weeks: 38.9 ± 3.0 g; P = 0.0001) and exhibited fasting hyperglycemia (normal chow: 67 ± 7 mg/dl, n = 4; HFD: 135 ± 14 mg/dl, n = 8; P < 0.01). CRHR2-deleted mice had the expected increases in plasma UCn2 after gene transfer (>14-fold increases; Figure 4A). However, despite this, glucose tolerance testing showed no reduction in hyperglycemia in CRHR2-deleted mice (Figure 4B).
Figure 4. UCn2 gene transfer in HFD-induced insulin resistance in CRHR2-deleted mice.
(A) Plasma UCn2 in CRHR2-deleted mice. First, we confirmed that i.v. AAV8.UCn2 (5 × 1011 gc, i.v.) was associated with increased plasma UCn2 levels in CRHR2-deleted (KO) HFD-fed mice. Plasma UCn2 peptide was measured in pooled plasma (4 animals per group). High plasma levels of UCn2 were detected, in amounts similar to what we found in normal mice (5). (B) Glucose tolerance test 17 weeks after HFD, UCn2 gene transfer at 8 weeks. Fasted CRHR2-deleted mice received glucose (2 mg/g, i.p.), and glucose was measured sequentially for 120 min. There was no group difference in blood glucose levels (P = 0.21, AUC), indicating that UCn2’s cognate receptor, CRHR2, is required for UCn2 to increase glucose disposal rate. Contrast these data to those shown in Figure 2A, where a pronounced glucose lowering effect of UCn2 gene transfer is observed.
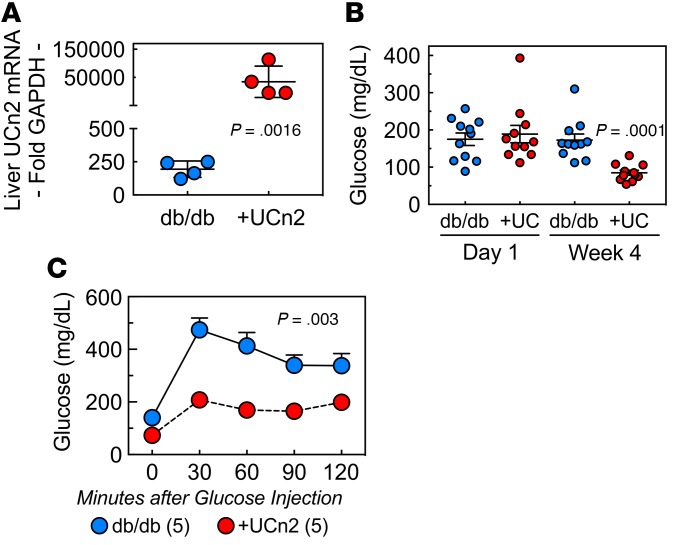
Effect of UCn2 gene transfer in db/db mice.
The effects of UCn2 gene transfer on glucose disposal were studied also in a second model of insulin resistance, the db/db mouse (6). UCn2 expression was documented by a > 450-fold increase in liver mRNA expression 1 month after i.v. AAV8.UCn2 (5 × 1011 gc) in db/db mice (Figure 5A; P = 0.0016). One day after gene transfer (Day 1) mice that had received saline (db/db; n = 11) and UCn2 gene transfer (n = 11) had similar levels of hyperglycemia (Figure 5B). Although females tended to have higher pre-UCn2 glucose levels (female: 218 ± 39 g/dl, n = 6; males: 154 ± 14 mg/dl, n = 5; P = 0.18), levels 4 weeks after UCn2 gene transfer were both normal (females: 85 ± 8 g/dl, n = 6; males: 85 ± 13 mg/dl, n = 5; P = 0.97), indicating that UCn2 increases glucose disposal in both sexes. Glucose tolerance tests in male db/db mice indicated that UCn2 gene transfer was associated with increased glucose disposal (Figure 5C; P = 0.003), similar to the results from mice rendered insulin resistant by HFD (Figure 2A). There were no group differences 5 weeks after gene transfer in body weight (saline: 34.1 ± 1 g, n = 5; AAV8.UCn2: 34.2 ± 2 g, n = 5; P = 0.71) or in 5-week food consumption (saline: 117 ± 10 g, n = 5; AAV8.UCn2: 109 ± 8 g, n = 5; P = 0.54).
Figure 5. UCn2 gene transfer increases glucose disposal in db/db mice.
Mice (db/db) received i.v. AAV8.UCn2 (5 × 1011 gc) or saline and were studied 4 weeks after gene transfer. (A) UCn2 expression. UCn2 gene transfer was associated with a > 450-fold increase in liver mRNA expression 4 weeks after gene transfer (P = 0.0016). (B) Fasting glucose. Blood was sampled after a 12-hr fast in 5 male and 6 female db/db mice. One day after gene transfer (Day 1), mice that had received saline (db/db; n = 11) and UCn2 gene transfer (+UC, n = 11) had similar levels of hyperglycemia. However, 4 weeks later (Week 4), mice that had received UCn2 gene transfer had a 42% reduction in blood glucose (P = 0.0001). (C) Glucose tolerance test in db/db mice. Mice (db/db) received i.v. AAV8.UCn2 (+UCn2; 5 × 1011 gc, n = 5) or saline (db/db, n = 5). One month later, fasted mice (12 hr) received glucose (2 mg/g, i.p.), and glucose levels were measured (C). The AUC was reduced by 57% (P = 0.003). These results indicate that UCn2 gene transfer promotes glucose disposal and protects against hyperglycemia, confirming its efficacy in a second model of insulin resistance.
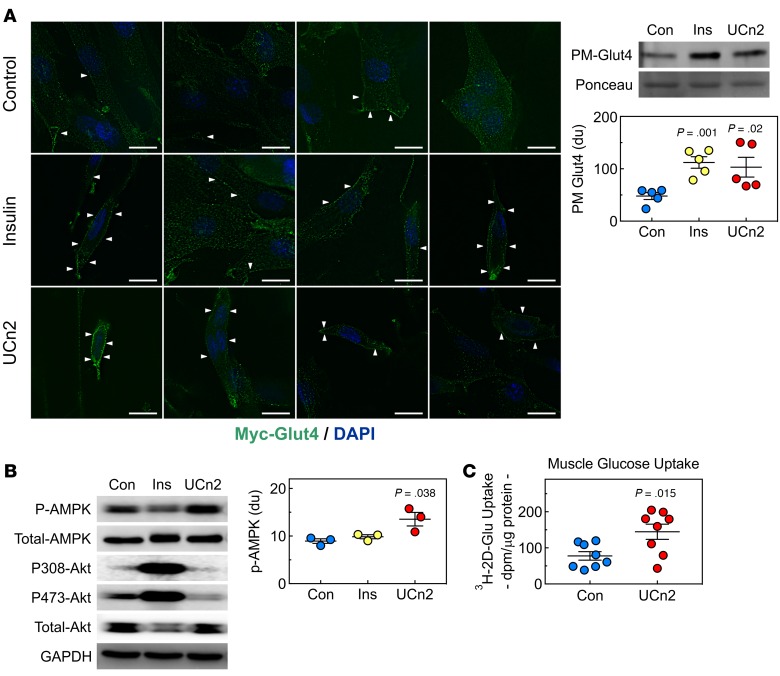
Glut4 translocation and AMPK activation.
To uncover possible mechanisms for UCn2’s effects on glucose disposal, we conducted studies in cultured cells exposed to UCn2 peptide. In differentiated L6 skeletal myotubes, UCn2 peptide (200 nM) induced plasma membrane translocation of Glut4 transporter, as shown by immunofluorescence staining (Figure 6A, left) and by immunoblotting analysis (Figure 6A, right). UCn2 peptide also activated AMP kinase in cultured L6 myotubes (Figure 6B), but Akt phosphorylation at Ser-473 was reduced versus control, an effect directionally opposite to insulin.
Figure 6. Effects of UCn2 on glucose uptake.
(A) UCn2 increases Glut4 translocation. Left: UCn2 increases Glu4 translocation in plasma membrane (PM). Myc-tagged Glut4-expressing L6 myotubes incubated (30 minutes) with insulin (100 nM) or UCn2 peptide (200 nM). Glut4 was detected using anti-Myc antibody (green); nucleus stained using DAPI (blue). White arrows indicate plasma membrane (PM) Glut4 localization (scale bars: 10 μm). Right: PM Glut4 translocation evaluated by immunoblotting; data are normalized to Ponceau S staining. Similar to insulin, UCn2 increased Glut4 translocation (data from 5 experiments). (B) UCn2 Signaling. Left: L6 myotubes incubated (60 minutes) with insulin (Ins; 100 nM) or UCn2 peptide (100 nM). UCn2 activated AMPK, but not Akt. Right: UCn2 increases phosphorylation of AMPK (mean ± SEM, 3 experiments; data normalized to GAPDH). (C) Skeletal muscle glucose uptake. In vivo studies show that UCn2 gene transfer increased glucose uptake in skeletal muscle. P values (vs. Control, Con) from Student’s t test (paired, 2-tailed).
Skeletal muscle glucose uptake in HFD-induced insulin resistance.
HFD-fed mice that received UCn2 gene transfer showed a 1.9-fold increased uptake of glucose in skeletal muscle (P = 0.015; Figure 6C).
Energy content in stool.
Because of potential effects of UCn2 on gut motility and to assess malabsorption as a cause for reduced weight gain in HFD-fed mice (see below), we assessed energy content in stool. There was no group difference in energy loss in stool (HFD: 3.73 ± 0.07 kcal/g, n = 6; HFD + UCn2: 3.84 ± 0.07 kcal/g, n = 6; P = 0.28).
Metabolic assessment.
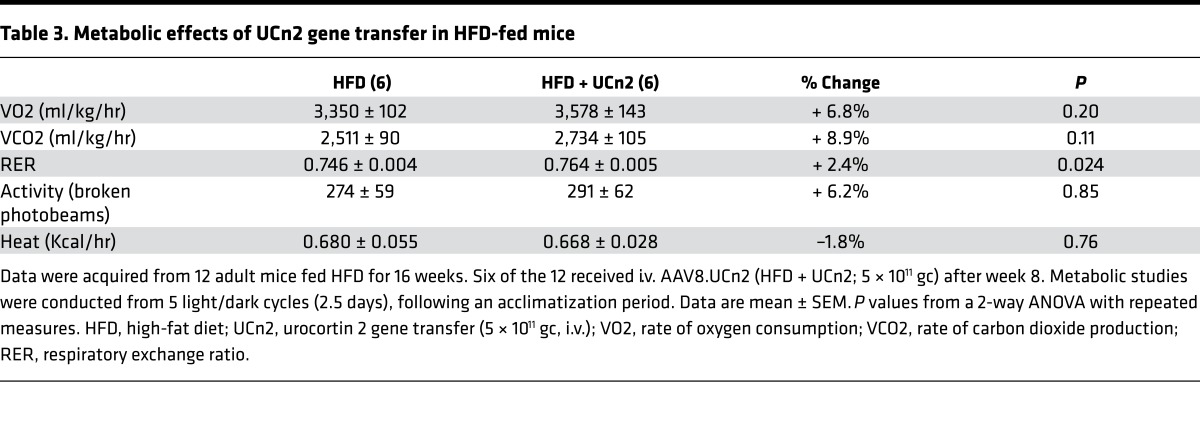
The Comprehensive Laboratory Animal Monitoring System (CLAMS) was used to assess the effects of UCn2 on metabolic features of HFD-fed mice. No group differences were seen in mean rates of oxygen consumption, carbon dioxide production, activity, or heat generation. HFD-fed mice that received UCn2 gene transfer showed small (2.4%) but statistically significant increases in respiratory exchange ratio (Table 3).
Table 3. Metabolic effects of UCn2 gene transfer in HFD-fed mice.
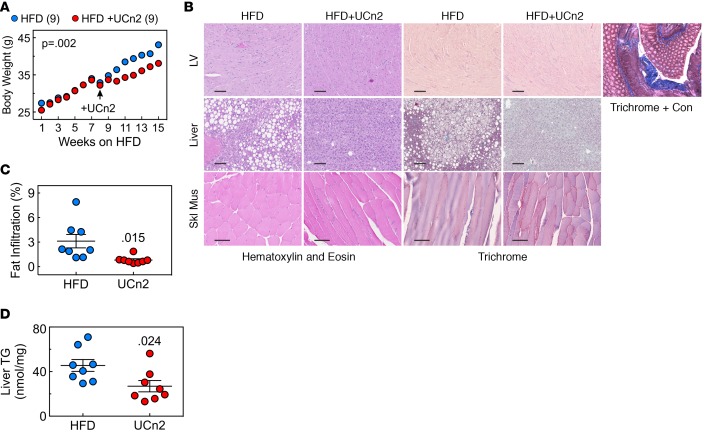
Weight gain.
UCn2 gene transfer in HFD-fed mice was associated with a trend toward reduced food consumption (P = 0.10) but with a 34% reduction in weight gained (P = 0.002) compared with saline-treated HFD-fed mice (Figure 7A). These mice had similar body weights 8 weeks after HFD was instituted — reduced weight gain did not occur until UCn2 gene transfer was performed. The ratio of gram of weight gained to gram of food consumed, a measure of feed efficiency, showed no group difference after 8 weeks of HFD (P = 0.53). However, UCn2 gene transfer, performed at 8 weeks, was associated with reduced feed efficiency for the subsequent 8-week period (HFD: 0.06 ± 0.01 g/g; n = 8; HFD + UCn2: 0.03 ± 0.004 g/g, n = 8; P < 0.014).
Figure 7. Weight gain and fatty infiltration of liver.
(A) Weight gain on HFD. Weights increased similarly in both groups for 8 weeks but were attenuated after UCn2 gene transfer (P = 0.002; repeated measures ANOVA). (B) Histology of liver and left ventricle. Mice fed HFDs for 5 weeks received i.v. UCn2 gene transfer (HFD + UCn2; 5 × 1011 gc) or saline (HFD), and HFD was maintained for 5 additional weeks. AAV8.UCn2 delivery and sustained urocortin 2 expression had no adverse effects on liver, LV, or skeletal muscle histology. Evident in the liver micrographs is fatty infiltration in HFD-fed but untreated mice. H&E and Masson’s trichrome staining were performed on sections of liver, transmural sections of left ventricle (LV), and skeletal muscle (Skl Mus). Trichrome + Con, positive control for Masson’s trichrome stain (scale bars: 100 μm). (C) Quantitative histological assessment of liver indicates that UCn2 gene transfer was associated with a 74% reduction in fatty infiltration of liver (P = 0.015; Student’s t test, unpaired, 2-tailed). Reduced fatty infiltration of the liver appeared to be independent of weight gain; it also was seen after UCn2 gene transfer in db/db mice despite no group difference in weight. (D) Liver triglyceride content. Livers from HFD-fed mice that received UCn2 gene transfer showed reduced triglyceride content (P = 0.024; Student’s t test, unpaired, 2-tailed).
Histology.
Intravenous AAV8.UCn2 (5 × 1011 gc) was not associated with inflammation or fibrosis in liver, left ventricle, or skeletal muscle. However, untreated HFD-fed mice showed fatty infiltration of the liver (Figure 7B). Quantitative assessment indicated that UCn2 gene transfer was associated with a 74% reduction of fatty infiltration of liver in the HFD model (P = 0.015; n = 8 per group; Figure 7C) and a 41% reduction in hepatic triglyceride content (P = 0.024; Figure 7D). A 43% reduction in fatty infiltration of liver was also seen after UCn2 gene transfer in db/db mice (n = 3 per group), even though there was no group difference in weight among db/db mice. Skeletal muscle showed a nonsignificant reduction in triglyceride content (HFD: 30 ± 3 nmol/mg, n = 5; HFD + UCn2: 24 ± 3 nmol/mg; P < 0.15).
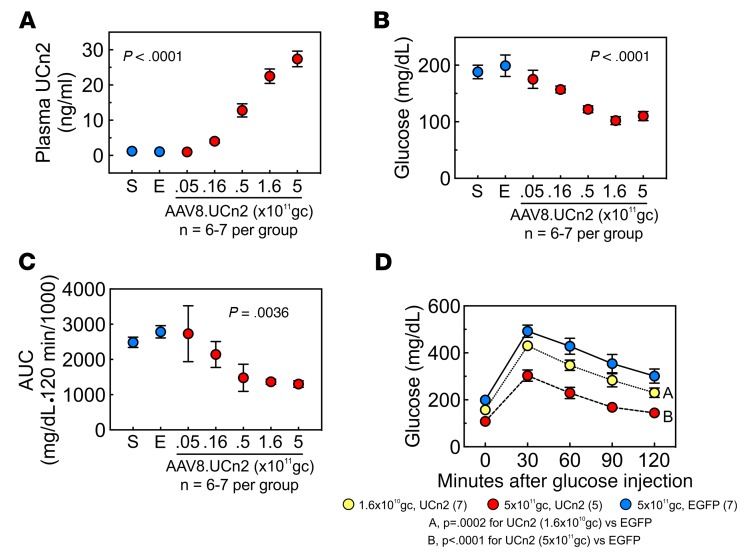
AAV8.UCn2 dose-response relationship.
To determine the amount of AAV8.UCn2 vector required for elevation in plasma UCn2 and increased glucose disposal, we conducted studies in mice rendered insulin resistant by HFD. AAV8.UCn2 doses in half-log increments from 5 × 109 to 5 × 1011 gc i.v. delivered to HFD-fed mice were associated, 9 weeks later, with a dose-related increase in plasma UCn2 levels (Figure 8A; P < 0.0001). A dose of 1.6 × 1010 gc increased mean plasma UCn2 concentration from 1.1 ± 0.1 ng/ml to 4.0 ± 0.5 ng/ml. The highest vector dose increased mean plasma UCn2 to 27.4 ± 2.2 ng/ml. Dose-related reductions in fasting glucose were seen (Figure 8B; P < 0.0001). The effects of AAV8.UCn2 on glucose disposal also were dose dependent (P = 0.0036; Figure 8, C and D). Intravenous saline and AAV8.EGFP (5 × 1011 gc, i.v.) had no effect, as anticipated.
Figure 8. AAV8.UCn2 dose-response relationship.
The effects of AAV8.UCn2 dose on plasma levels of UCn2 and glucose disposal were examined 9 weeks after institution of HFD. (A) AAV8.UCn2 dose vs. plasma UCn2 concentration. AAV8.UCn2 doses of 5 × 109 to 5 × 1011 gc i.v. produced a dose-related increase in plasma UCn2 levels (P < 0.0001, 1-way ANOVA). Plasma obtained 75 ± 5 days after delivery. (B) Fasting glucose. Fasting blood glucose was related to AAV8.UCn2 dose (P < 0.0001, 1-way ANOVA). (C) Vector dose and glucose tolerance testing. The effects of AAV8.UCn2 on glucose disposal were dose dependent (P = 0.0036, 1-way ANOVA). Shown is area under the glucose-time curve for each dose. (D) Highest and lowest effective AAV8.UCn2 dose. Shown are glucose concentrations after i.v. glucose load in 3 of the 7 groups shown in C: AAV8.EGFP (control, 5 × 1011 gc, i.v.), and 2 doses of AAV8.UCn2, i.v.: 5 × 1011 gc (the highest dose) and 1.6 × 1010 gc, the lowest effective dose. In A–C: S, saline; E, AAV8.EGFP 5 × 1011 gc i.v.
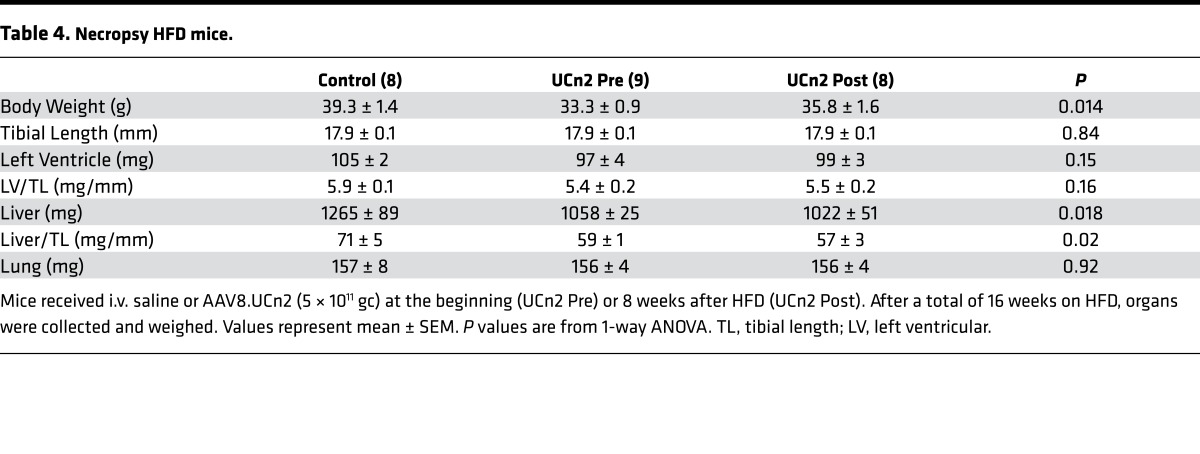
Necropsy.
Table 4 shows that mice fed HFD for 16 weeks who had received UCn2 gene transfer at onset of HFD or 8 weeks later had reduced body weight (P = 0.014) and reduced liver weight both in absolute terms (P = 0.018) and normalized for tibial length (P = 0.02). Left ventricular (LV) and lung weights showed no group differences.
Table 4. Necropsy HFD mice.
Discussion
The most important finding of the current study is that UCn2 gene transfer has a profound and enduring effect on insulin sensitivity in HFD-fed mice (Figure 3). A single i.v. injection of AAV8.UCn2: (a) prevents hyperglycemia from developing in mice fed a HFD and increases glucose disposal if delivered after hyperglycemia is present (Figure 2A); (b) increases insulin sensitivity, glucose disposal rate, and glucose uptake in skeletal muscle (Figure 3, B and C, and Figure 6C); (c) reduces fatty infiltration of the liver (Figure 7, B–D); (d) reduces weight gain on prolonged HFD (Figure 7A); and (e) decreases fasting hyperglycemia and increases glucose disposal in a second model of disordered glucose homeostasis (db/db mice) (Figure 5, B and C). These data confirm the efficacy of UCn2 gene transfer in reducing insulin resistance. These results have potential clinical application.
Clinical trials of i.v. infusions of UCn2 peptide (4) or a related peptide, stresscopin (7), in patients with HF have not reported reduced blood glucose levels. Perhaps the effects on glucose metabolism conferred by UCn2 gene transfer are a consequence of longer duration and higher plasma UCn2 concentrations obtained with gene transfer than with UCn2 peptide infusion. Indeed, 6 weeks after UCn2 gene transfer (5 × 1011 gc, i.v.) in mice, mean plasma levels were 15-fold control (5), while peak UCn2 levels in human subjects during 1- to 4-hour peptide infusions (5–30 ng/kg/min) were 3-fold control and short-lived, rapidly declining after termination of the infusion (4). However, it is unlikely that the high plasma UCn2 levels attained in the present study are required for an effect on glucose metabolism. Our dose-response data indicate that AAV8.UCn2 amounts 30-fold lower provide a glucose-lowering effect (Figures 8, A–D), which corresponds to a plasma UCn2 level of 4.0 ± 0.5 ng/ml, 4-fold above normal (Figure 8A).
The present study documents the effects of UCn2 gene transfer on glucose disposal in 2 murine models of insulin resistance. Although the study was primarily conducted in male mice, female db/db mice also showed normalization of fasting glucose after UCn2 gene transfer, suggesting that the effect occurs in both sexes.
Mechanism.
Our data show beneficial effects of UCn2 gene transfer on glucose uptake in skeletal muscle in the basal state (Figure 6C) and augmentation of glucose disposal upon insulin stimulation (Figure 3C). Therefore, skeletal muscle clearly contributes to the increased insulin sensitivity observed. UCn2 gene transfer also was associated with a 20% reduction in HGP (Figure 3D), which may have contributed to improved glucose homeostasis.
Insulin acts by increasing Akt phosphorylation of Ser-473, which promotes Glut4 translocation to the plasma membrane and increased glucose disposal. UCn2 peptide increases Glut4 translocation similarly to insulin (Figure 6B), but, in contrast to insulin, phosphorylation of Ser-473-Akt is decreased (Figure 6B), indicating a pathway for UCn2-related Glut4 translocation and increased glucose disposal. Glut4 translocation is associated with AMPK phosphorylation (Figure 6B) (8) and is an expected consequence of CRHR2 receptor activation, which triggers cAMP-PKA signaling (1, 2). The fact that UCn2 gene transfer did not increase glucose disposal in CRHR2-deleted mice rendered insulin resistant by HFD (Figure 4B) supports this idea. A previous study (9) found no change in fasting blood glucose after 4 weeks of HFD in a different CRHR2-deleted line, which may reflect a difference in line or an inadequate duration of HFD (4 weeks vs. 8–18 weeks in the current study).
Metabolic effects.
UCn2 activation of CRHR2 receptors in brain and the gastrointestinal tract can alter satiety and thereby reduce food consumption (3). Although we saw nonsignificant reductions in food consumption (5%; P = 0.10), there was a 34% reduction in weight gain (P = 0.002) in UCn2 mice on HFD (Figure 7A). However, db/db mice showed similar increases in glucose disposal after UCn2 gene transfer but no change in food consumption or weight gain, indicating that UCn2’s effects on glucose disposal are not due to reduced weight alone. Metabolic studies of mice fed HFD for 16–17 weeks indicated that UCn2 gene transfer did not increase total activity, heat generation, or the rates of oxygen consumption or carbon dioxide production (Table 3). The biological importance of a 2.4% increase in respiratory exchange ratio following UCn2 gene transfer is unknown, although it indicates a small increase in metabolism of carbohydrate vs. fat.
Gross malabsorption was not evident, but to evaluate this possibility, we performed bomb calorimetric studies on stool from HFD-fed mice. We found that UCn2 gene transfer had no effect on energy loss in stool, which makes malabsorption unlikely. We then evaluated feed efficiency, a measure of weight gained per food consumed (10), and documented that UCn2 gene transfer was associated with a 50% reduction in feed efficiency (P < 0.014). The values for feed efficiency in mice on HFD (0.06 ± 0.01 g/g) are in line with previous reports, where a mean feed efficiency of 0.06 g/g was reported (10).
A treatment for T2DM that increases insulin sensitivity and glucose disposal while attenuating weight gain and reducing fatty infiltration of liver would be a welcome addition to current clinical therapy. Reduced fatty infiltration of the liver appeared to be independent of weight gain; it also was seen after UCn2 gene transfer in db/db mice, despite no group difference in weight. HFD mice that received UCn2 gene transfer had reduced hepatic triglyceride content and reduced liver weight.
Previous studies.
Elevation in plasma UCn2 increased insulin sensitivity, an unanticipated and previously unreported phenomenon. Indeed, UCn2 deletion was reported to increase skeletal muscle glucose clearance (11). However, deletion of a gene is not the opposite of its expression vis-à-vis overall physiological integration. For example, this finding, which seems to contradict our studies, may reflect centrally mediated effects. In a transgenic line with general UCn3 overexpression, increased glucose clearance in HFD-fed mice was reported (12). However, these UCn3-expressing mice, unlike the mice that received UCn2 gene transfer in the present study, showed no change in insulin sensitivity. The mechanism for increased glucose clearance in the UCn3 transgenic line may relate to phenotypic features of the line, which included increased skeletal muscle mass and body weight. In addition, that study found a 44-fold increase in brain UCn3, which confounds data interpretation because of central effects of UCn3. In our study, UCn2 expression was not increased in the brain (Table 2).
UCn3, but not UCn2, is expressed in pancreatic β cells and is required for glucose- and incretin-stimulated insulin secretion (13). High levels of transgene UCn2 may activate CRHR2 receptors in pancreatic β cells and thereby influence insulin release. However, UCn2 gene transfer reduced plasma insulin levels in HFD mice (Figure 2B; P < 0.007). The normalization of fasting hyperglycemia combined with increased glucose disposal (HFD: Figure 2A, P = 0.003; db/db: Figure 5C, P = 0.003) and increased insulin sensitivity (Figure 2C, P = 0.0004) indicates that UCn2 gene transfer reduced insulin resistance, as confirmed by hyperinsulinemic-euglycemic clamp studies (Figure 3).
Gene and cell therapy.
The potential safety of i.v. delivery of an AAV8 vector was demonstrated in an early-phase gene transfer clinical trial in patients with hemophilia B (14). Although we can find no previous reports using gene transfer of an insulin-sensitizing peptide to treat insulin resistance or T2DM, there have been reports of other therapies. For example, islet-cell transplantation has been successful clinically (15), although donors are difficult to procure and rejection of donor islets has been a problem. An early-phase clinical trial showed that polyclonal regulatory T cell immunotherapy might be effective in treating type 1 diabetes (16). Gene transfer has been successful in preclinical models of diabetes. For example, insulin and glucokinase gene transfer (17) and gene transfer of both the NK1 fragment of hepatocyte growth factor (HGF/NK1) and glucagon-like peptide-1 (GLP-1), which appears to promote islet generation (18), have been successful in preclinical studies. However, these therapies have focused on insulin deficiency — type 1 diabetes and late-stage T2DM. In contrast, the current studies focused on earlier-stage insulin resistance using a transgene that increases insulin sensitivity.
Cardiac effects of UCn2.
We have demonstrated that UCn2 gene transfer in normal mice has beneficial effects on LV contractile function through augmentation of Ca2+ handling (5). The safety and efficacy of UCn2 peptide infusion has been confirmed in large-animal models of HF (19) and in patients with HF (4). A clinical HF study using infusion of an UCn2-related peptide, stresscopin, found similar results (7). We also recently showed that UCn2 gene transfer increases function of the failing heart in mice (20). T2DM is commonly present in patients with HF. In patients with both HF and T2DM, UCn2 gene transfer could, in theory, resolve insulin resistance and increase LV function concurrently.
In clinical trials, UCn2 peptide infusion has been bedeviled with hypotension and reflex tachycardia. In the present study, we saw no group differences in mean daily heart rate assessed by continuous telemetry or in basal blood pressure assessed by tail cuff (Table 1). This may reflect tachyphylaxis to vasodilation associated with long duration and gradual-onset UCn2 exposure. In contrast, the effects of UCn2 gene transfer on blood glucose persisted for the duration of testing (16–17 weeks) without decrement in degree of effect. The absence of basal hypotension and tachycardia is reassuring vis-à-vis prospects for future clinical trials.
Translation to clinical application.
AAV8.UCn2 dose-response data (Figures 8, A–D) indicate that a dose of 5 × 1010 gc (1.9 × 1012 gc/kg) is associated with a 44% reduction in AUC, and a dose of 1.6 × 1010 gc (6 × 1011 gc/kg) with an 18% reduction in AUC (Figure 8, C and D). Previous studies have shown that a 20% reduction in AUC is efficacious in treating clinical T2DM (21), suggesting that a dose of 6 × 1011 gc/kg, 30-fold lower than the highest dose used in the present study, may be effective in clinical settings. This would limit adverse effects that may be associated with higher doses of AAV8. These doses (1.9 × 1012 gc/kg and 6 × 1011 gc/kg) are similar to the highest 2 doses of an AAV8 vector encoding Factor IX used safely in a gene-transfer trial in human subjects with hemophilia B (2 × 1012 gc/kg, and 6 × 1011 gc/kg, i.v.) (14).
Clinical implications.
Diabetes was reported to affect 12%–14% of the US adult population in 2011–2012 (22), 95% of whom have T2DM. T2DM is a major risk factor for stroke, neuropathy, kidney failure, blindness, myocardial infarction, and HF. Few diseases affect so many organs or are as prevalent. The discovery and development of more effective therapies is imperative. Intravenous delivery of an AAV vector encoding UCn2 provides numerous possible advantages over oral T2DM agents and insulin: (a) the insulin-sensitizing effect of UCn2 gene transfer would be anticipated to preserve β-cell function, a goal in the management of patients with early T2DM; (b) some oral T2DM agents, including thiazolidinediones, appear to be hazardous in patients with coronary artery disease or HF (23), but in contrast, UCn2 has beneficial effects on the heart (2, 4, 5, 19, 20); (c) repeated insulin injections or frequent oral medications are a nuisance for many patients — UCn2 gene transfer would circumvent this with a one-time treatment; (d) insulin and some oral T2DM agents are associated with weight gain, but in contrast, UCn2 gene transfer is associated with reduced weight gain in mice fed HFD (Figure 7A); and (e) UCn2 gene transfer reduced fatty infiltration of the liver in both models of insulin resistance (Figures 7, B and C). Nonalcoholic fatty liver disease is a rapidly increasing problem, particularly among patients with T2DM and metabolic syndrome, and is a common cause for liver transplantation (24). So this effect of UCn2 gene transfer in the setting of insulin resistance has important clinical implications.
Limitations.
The precise molecular pathways beyond Glut4 translocation that explain the favorable effects of UCn2 gene transfer on glucose disposal will require additional studies. Elevation of UCn2, an endogenous peptide hormone, could potentially have adverse consequences in humans that are not apparent in mice. However, T2DM is a life-threatening disease, and despite many currently available medical options, few appear to effectively reduce its morbidity and mortality. The proposed therapy would serve an unmet medical need. Studies in nonhuman primates with T2DM will be initiated soon, and if insulin sensitivity and glucose disposal are safely increased in these studies, we hope to initiate a clinical trial.
Conclusion.
A one-time i.v. injection of an AAV8 vector encoding UCn2 increases insulin sensitivity and glucose disposal, provides long-lasting resolution of abnormal glucose homeostasis, and reduces fatty infiltration of liver in 2 murine models of insulin resistance, suggesting a potential long-term therapy in clinical type-2 diabetes.
Methods
AAV8.UCn2 vector production
An AAV8 vector encoding murine UCn2 with a chicken β-actin (CBA) promoter (Figure 1A) was produced as detailed previously (5). Plasmid pRep2/Cap8 was obtained from the University of Pennsylvania Vector Core.
Animal use
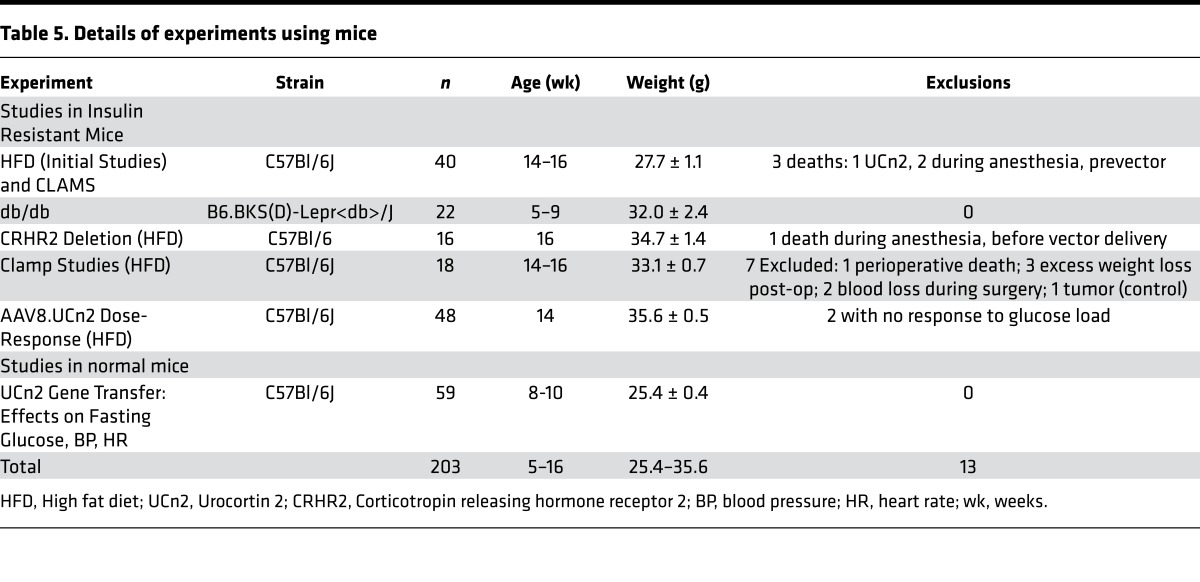
The numbers of animals used in each set of experiments, their weights, ages, sex, and animals that died or had unusable data are outlined in Table 5. There were 203 mice used (obtained from The Jackson Laboratory), ranging in age from 5–16 weeks, weighing 27.7–35.6 grams, depending on the protocol. All but 12 animals were male. Thirteen mice were excluded: 8 due to unusable data (determination made prior to unblinding) and 5 due to death during anesthesia or surgery — 4 prior to vector delivery (Table 5).
Table 5. Details of experiments using mice.
Studies in normal mice on normal diets
Fifty-nine normal mice on normal chow were used to evaluate the effects of UCn2 gene transfer on fasting blood glucose, blood pressure, and heart rate. AAV9 encoding EGFP (AAV9.EGFP) was used as an additional control to ensure the effect on blood glucose was UCn2 specific. Normal mice received i.v. AAV8.EGFP (5 × 1011 gc), saline, or AAV8.UCn2 in doses ranging from 5 × 109 to 5 × 1011 gc. The effects of UCn2 gene transfer on blood pressure and heart rate were assessed in unsedated ambulatory mice 6–8 weeks after UCn2 gene transfer (5 × 1011 gc, i.v.). To accomplish this, 5 weeks after gene transfer or saline, PhysioTel ETA-F20 transmitters (Data Sciences International) were implanted i.p.; continuous electrocardiographic recording was initiated 1 week later and continued for 5 days to enable acquisition of ambulatory daily mean heart rate as previously reported (25). Systolic and diastolic blood pressure was measured by tail cuff (Visitech Systems), and mean blood pressure was calculated.
HFD-induced insulin resistance
To determine the effect of UCn2 gene transfer on glucose disposal, we used HFD to induce insulin resistance and hyperglycemia in normal mice. Mice were provided (ad libitum) a cereal-based diet (Harlan Teklad Lab) for 5 weeks and then switched to a HFD (60 kcal%; Research Diets) for durations and group sizes indicated in individual experiments. Mice received i.v. AAV8.UCn2 (5 × 1011 gc) or saline either at the initiation of HFD or 8 weeks later. Mice were housed (20oC–21oC) with lights off from 6 pm to 6 am daily. Food consumption and body weight were recorded weekly. A second group of normal mice was fed HFD for 16 weeks. After week 8, they received i.v. injection of: saline, AAV8.EGFP (5 × 1011 gc), or AAV8.UCn2 in 1 of 5 doses from 5 × 109 gc to 5 × 1011 gc in half-log increments. These data were used to determine the relationship between AAV8.UCn2 dose and plasma UCn2 concentration and glucose disposal via glucose tolerance testing.
Murine genetic model of insulin resistance
B6.BKS(D)-Lepr<db>/J diabetic mice (db/db) maintain increased plasma insulin levels and insulin resistance until late in life, providing a suitable T2DM model (6). Mice (10 male; 12 female) received i.v. AAV8.UCn2 (5 × 1011 gc; n = 11) or saline (n = 11). They were provided (ad libitum) a cereal-based diet (Harlan Teklad Lab) for 6 weeks. Mice were housed (20oC–21oC) with lights off from 6 pm to 6 am daily. Food consumption and body weight were recorded weekly.
AAV8.UCn2 delivery
Under anesthesia (1.5% isoflurane via nose cone) a small incision was made on the neck to expose the jugular vein for i.v. delivery. Mice were injected with AAV8.UCn2 (in 50 μl PBS) or an equivalent volume of saline (control).
Glucose tolerance test
Mice were fasted for 12 hours and received glucose (2 g/kg, i.p.). Blood glucose levels were measured before and 30, 60, 90, and 120 minutes after glucose injection. Blood was collected via a small tail incision, and glucose was measured using Contour Blood Glucose Meter via Blood Glucose Test Strips (Bayer).
Insulin tolerance test (ITT)
Nonfasted mice received insulin (0.75 units/kg, i.p.), and blood glucose levels were measured before and 30, 60, 90, and 120 minutes later.
ELISA
Plasma UCn2 was measured as previously reported (5). Blood (1 ml) was collected and centrifuged (1,600 g, 15 min). Plasma was collected and stored at –80°C. Plasma UCn2 was measured with a mouse UCn2 enzyme immunoassay kit (Kamiya Biomedical). Plasma insulin was measured using the Mouse Insulin ELISA Kit (Crystal Chem Inc.). Plasma C-peptide was determined using Mouse C-peptide ELISA Kit (Alpco).
Hyperinsulinemic-euglycemic clamps
These studies were performed on HFD-fed mice (8 weeks old; Table 5). Upon receipt, they were continued on HFD and received i.v. UCn2 gene transfer (5 × 1011 gc; n = 9) or i.v. saline (n = 9) within 1 week. The 2 groups underwent clamp studies 17 ± 1 weeks after gene transfer, having been sustained on HFD continuously. Clamps were conducted in weight-matched conscious mice after a 6-hour fast as previously described (26). Mice were anesthetized using ketamine (100 mg/kg, Zoetis), acepromazine (3 mg/kg, Vet One), and xylazine (10 mg/kg, Aveco) and jugular vein was cannulated 4 days before clamp measurement. On the day of the clamp, body weight was recorded and blood glucose measured (6 hr fasting). Mice then were placed in a Lucite restrainer (Braintree Scientific) and blood samples obtained (–60 min) for plasma insulin concentration. Equilibrating [3-3H] D-glucose tracer solution (PerkinElmer; 41.6 μCi 3H/ml) was then infused (2 μl/min i.v., 60 min). At the end of the equilibration period (t = 0 min), two 15-μl blood samples were obtained and deproteinized using 125 μl ZnSO4 (0.3 N) and 125 μl BaOH (0.3 N) for assessment of tracer-specific activity and basal glucose disposal rate. To clamp after the equilibration period, a cocktail containing 8% BSA, insulin (Humulin R, Lilly, 10.0 mU/kg/min), and tracer (41.6 μCi/ml) was infused at a constant rate (2.0 μl/min) along with a variable glucose infusion (50% dextrose, 454 mg/ml). Blood glucose was assessed using blood glucose meter and test strips every 10 min, and infusion rate was adjusted until steady-state blood glucose (120 ± 10 mg/dl) was achieved. The clamp was terminated when steady-state conditions were maintained for ≥ 20 minutes (~120 min), at which time two 15-μl blood samples were obtained for assessment of tracer-specific activity and insulin-stimulated glucose disposal rate (t = ~120 min). Blood (70 μl) was collected before and after the clamp for measurement of plasma insulin concentration.
CRHR2-deleted mice
To determine whether UCn2 effects on glucose disposal were mediated through its cognate receptor, CRHR2, UCn2 gene transfer was performed in CRHR2-deleted mice 8 weeks after initiation of HFD, which was continued for a total of 17 weeks (9 weeks after gene transfer). CRHR2+/– × CRHR2+/– mice and CRHR2–/– × CRHR2–/– (C57BL/6 background) were bred to obtain CRHR2+/+ (WT) and CRHR2–/– mice (27). Mice were housed in a temperature and light-controlled room (22°C–24°C; 12 hr light/12 hr dark) and were bred at UCSF’s centralized vivarium.
After assessment of baseline glucose levels, CRHR2–/– littermates (10–12 weeks of age; 34.7 ± 1.4 grams) were put on a HFD for 8 weeks. Mice then underwent glucose tolerance testing and subsequently received either i.v. saline or AAV8.UCn2 (5 × 1011 gc). Mice were assigned to 2 groups: (a) HFD + AAV8.UCn2 (n = 8); (b) HFD + saline (n = 8). Nine weeks after AAV8.UCn2 or saline injection, mice again underwent glucose tolerance testing.
Skeletal muscle glucose uptake
Normal mice received i.v. UCn2 gene transfer (5 × 1011 gc, n = 6) or i.v. saline (n = 6) and underwent glucose uptake studies 6 weeks later. A mixture of glucose (2.5 g/kg), [3H]-2-deoxy glucose (10 μCi/mouse), and [14C]-L-glucose (1 μCi/mouse) was administrated i.p. 60 minutes before harvesting samples of gastrocnemius muscle. Tissues were homogenized in water and then were added to scintillation fluid to be counted. [3H]-2-dexoy-glucose uptake was corrected for nonspecific trapping of extracellular space by [14C]-L-glucose and divided by the [3H]-radioactivity of plasma glucose.
Glut4 translocation assay
Plasma membrane isolation.
L6-mycGlut4 cells (Kerafast) were differentiated by culturing in 2% FBS + MEM for 7 days. Cells were incubated in serum-free medium for 3 hours and then incubated with insulin (100 nM, 30 min) or UCn2 (200 nM, 30 min). Cells were washed once with cold DPBS and plasma membrane was isolated using Qproteome Plasma Membrane Protein Kit (Qiagen).
Glut4 translocation.
L6-mycGlut4 cells were prepared as outlined in the preceding section and washed once with cold DPBS containing 0.9 mM CaCl2 and 0.5 mM MgCl2 and fixed with cold 4% PFA in DPBS for 15 minutes, followed by 3 DPBS washes. Fixed cells were blocked with 5% goat serum in DPBS (21°C, 30 min) and then incubated with anti–myc tag antibody (clone 9B11, Cell Signaling Technology) in DPBS (4°C, 8 hr). After washing with DPBS, epitope-bound primary antibodies were detected using Alexa 488–conjugated anti–mouse IgG antibodies. Images were acquired using a Deltavision RT deconvolution microscope.
Energy content in stool
To determine if UCn2 gene transfer affected absorption of food, 12 mice were placed on HFD (33 weeks). At week 13, 6 of 12 received i.v. UCn2 gene transfer (5 × 1011 gc). The energy content in fecal samples was measured by Kinetica Inc. Stool samples (stored at –20°C) were dried in a convection oven (100°C, 6 hr). Energy content for each stool specimen was determined from the heat of combustion measured with an oxygen bomb calorimeter. Testing was conducted according to standard guidelines (28).
Metabolic Studies
The Comprehensive Laboratory Animal Monitoring System (CLAMS, Columbus Instruments) was used to assess oxygen consumption and activity level in 12 normal mice fed HFD for 16 weeks. Six of 12 mice received i.v. AAV8.UCn2 (5 × 1011 gc) midway through the 16-week HFD period. Mice were placed in standard metabolic cages for 5 days while measurements were continuously acquired. Data from 5 light/dark cycles following a 1.5-day acclimation period were used in the analysis.
RT-PCR and immunoblotting
RT-PCR and immunoblotting was conducted as previously described (5). The antibodies to the phosphorylated forms of AMPK, phosphatidylinositol-3-kinase (PI3K), protein kinase B (Akt), glycogen synthase kinase 3 (GSK3), and p70S6K were purchased from Cell Signaling Technology, and antibody to phosphorylated peroxisome proliferator-activated receptor γ (PPARγ) was purchased from Santa Cruz Biotechnology Inc.
Histology
A subset of mice fed HFD for 8 weeks received i.v. UCn2 gene transfer (5 × 1011 gc, n = 8) or saline (n = 8), were continued 8 additional weeks on HFD, and were then killed. Samples of liver and transmural sections of the LV free wall were formalin fixed and paraffin imbedded. Five micron sections were mounted and counterstained with H&E and with Masson’s trichrome and examined for fibrosis and inflammation. To quantify fatty infiltration of liver, slides were scanned (NanoZoomer 2.0HT Slide Scanner), planimetered, and reported as percentage of total area.
Hepatic and skeletal muscle triglyceride content
Hepatic and skeletal muscle triglyceride content was determined using a colorimetric/fluorometric kit (Biovision Inc.). Liver and skeletal muscle samples (100 mg) were homogenized in 1 ml of water containing 5% NP-40 using Tissuemiser (Thermo Fisher Scientific). Lysates were heated (100°C, 5 min) and cooled (25°C) twice. After centrifugation (15,000 g, 2 min) the supernatant was assayed for triglyceride content, which was reported as nmol per mg of liver or skeletal muscle (wet weight).
Necropsy
Body, liver, lung, and LV weight (including interventricular septum), as well as tibial length, were recorded. A short axis midwall LV ring, a short-axis sample of skeletal muscle at mid-calf level, and samples of liver were obtained; portions were quickly frozen in liquid nitrogen and stored at −80°C or fixed in formalin and embedded in paraffin.
Statistics
Data represent mean ± SEM; group differences were tested for significance using Student’s t test (unpaired, 2-tailed) or repeated measures ANOVA. In glucose tolerance tests, the trapezoidal rule was applied to determine AUC. The null hypothesis was rejected when P < 0.05. Analyses were performed using GraphPad Prism (GraphPad Software Inc.). Those collecting and analyzing data obtained from physiological experiments were blinded to group identity.
Study approval
The Guide for the Care and Use of Laboratory Animals. (National Academies Press. 2011.) was followed, and the Animal Use and Care Committees of the VA San Diego Healthcare System and the UCSF approved the studies.
Author Contributions
MHG, DG, NCL, EW, VAP, YCK, TG, ML, LL, ZT, TPC, SS, AB, DYO, and HKH conducted experiments or analyzed data. AM, AB, and ML provided AAV vector or CRHR2 deleted transgenic line. MHG, NCL, and HKH conducted the study design. HKH, MHG, and NCL wrote the paper.
Acknowledgments
We thank Ruoying Tang for her technical expertise and the UCSD Animal Care Program Phenotyping Core for performing the metabolic cage experiments. We thank Tamsin Lisa Kelly for reviewing the manuscript and providing helpful criticisms. This work was supported by NIH grants (P01 HL66941, HL088426, and DK080787); an NHLBI Gene Therapy Resource Program grant (HHSN268201200041C); VA Merit grant (1101BX001515); and UCSD School of Medicine Light Microscopy Facility (grant NS047101) for imaging.
Footnotes
Conflict of interest: HKH is a founder, board member, and unpaid consultant for Renova Therapeutics, a developmental-stage private biotechnology company.
Reference information:JCI Insight. 2016;1(15):e88322. doi:10.1172/jci.insight.88322.
Contributor Information
Mei Hua Gao, Email: 8582451824@vtext.com.
Dimosthenis Giamouridis, Email: dgiamouridis@vapop.ucsd.edu.
N. Chin Lai, Email: nclai@ucsd.edu.
Evelyn Walenta, Email: ewalenta@ucsd.edu.
Vivian Almeida Paschoal, Email: vpaschoal@ucsd.edu.
Young Chul Kim, Email: y8kim@vapop.ucsd.edu.
Atsushi Miyanohara, Email: amiyanohara@ucsd.edu.
Tracy Guo, Email: tracyguo@vapop.ucsd.edu.
Min Liao, Email: liaomin_01@hotmail.com.
Li Liu, Email: lucy301bj@sina.com.
Zhen Tan, Email: ztan@vapop.ucsd.edu.
Simon Schenk, Email: sschenk@ucsd.edu.
Aditi Bhargava, Email: aditi.bhargava@ucsfmedctr.org.
Da Young Oh, Email: d8oh@ucsd.edu.
References
- 1.Reyes TM, et al. Urocortin II: a member of the corticotropin-releasing factor (CRF) neuropeptide family that is selectively bound by type 2 CRF receptors. Proc Natl Acad Sci U S A. 2001;98(5):2843–2848. doi: 10.1073/pnas.051626398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davidson SM, Yellon DM. Urocortin: a protective peptide that targets both the myocardium and vasculature. Pharmacol Rep. 2009;61(1):172–182. doi: 10.1016/S1734-1140(09)70019-2. [DOI] [PubMed] [Google Scholar]
- 3.Zorrilla EP, et al. Human urocortin 2, a corticotropin-releasing factor (CRF)2 agonist, and ovine CRF, a CRF1 agonist, differentially alter feeding and motor activity. J Pharmacol Exp Ther. 2004;310(3):1027–1034. doi: 10.1124/jpet.104.068676. [DOI] [PubMed] [Google Scholar]
- 4.Chan WY, Frampton CM, Crozier IG, Troughton RW, Richards AM. Urocortin-2 infusion in acute decompensated heart failure: findings from the UNICORN study (urocortin-2 in the treatment of acute heart failure as an adjunct over conventional therapy) JACC Heart Fail. 2013;1(5):433–441. doi: 10.1016/j.jchf.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Gao MH, et al. Intravenous adeno-associated virus serotype 8 encoding urocortin-2 provides sustained augmentation of left ventricular function in mice. Hum Gene Ther. 2013;24(9):777–785. doi: 10.1089/hum.2013.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kodama H, Fujita M, Yamaguchi I. Development of hyperglycaemia and insulin resistance in conscious genetically diabetic (C57BL/KsJ-db/db) mice. Diabetologia. 1994;37(8):739–744. doi: 10.1007/BF00404329. [DOI] [PubMed] [Google Scholar]
- 7.Gheorghiade M, et al. Haemodynamic effects, safety, and pharmacokinetics of human stresscopin in heart failure with reduced ejection fraction. Eur J Heart Fail. 2013;15(6):679–689. doi: 10.1093/eurjhf/hft023. [DOI] [PubMed] [Google Scholar]
- 8.Kurth-Kraczek EJ, Hirshman MF, Goodyear LJ, Winder WW. 5’ AMP-activated protein kinase activation causes GLUT4 translocation in skeletal muscle. Diabetes. 1999;48(8):1667–1671. doi: 10.2337/diabetes.48.8.1667. [DOI] [PubMed] [Google Scholar]
- 9.Bale TL, Anderson KR, Roberts AJ, Lee KF, Nagy TR, Vale WW. Corticotropin-releasing factor receptor-2-deficient mice display abnormal homeostatic responses to challenges of increased dietary fat and cold. Endocrinology. 2003;144(6):2580–2587. doi: 10.1210/en.2002-0091. [DOI] [PubMed] [Google Scholar]
- 10.Parekh PI, Petro AE, Tiller JM, Feinglos MN, Surwit RS. Reversal of diet-induced obesity and diabetes in C57BL/6J mice. Metab Clin Exp. 1998;47(9):1089–1096. doi: 10.1016/S0026-0495(98)90283-9. [DOI] [PubMed] [Google Scholar]
- 11.Chen A, et al. Urocortin 2 modulates glucose utilization and insulin sensitivity in skeletal muscle. Proc Natl Acad Sci U S A. 2006;103(44):16580–16585. doi: 10.1073/pnas.0607337103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jamieson PM, et al. Urocortin 3 transgenic mice exhibit a metabolically favourable phenotype resisting obesity and hyperglycaemia on a high-fat diet. Diabetologia. 2011;54(9):2392–2403. doi: 10.1007/s00125-011-2205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li C, Chen P, Vaughan J, Lee KF, Vale W. Urocortin 3 regulates glucose-stimulated insulin secretion and energy homeostasis. Proc Natl Acad Sci USA. 2007;104(10):4206–4211. doi: 10.1073/pnas.0611641104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nathwani AC, et al. Adenovirus-associated virus vector-mediated gene transfer in hemophilia B. N Engl J Med. 2011;365(25):2357–2365. doi: 10.1056/NEJMoa1108046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robertson RP. Islet transplantation a decade later and strategies for filling a half-full glass. Diabetes. 2010;59(6):1285–1291. doi: 10.2337/db09-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bluestone JA, et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci Transl Med. 2015;7(315):e88322. doi: 10.1126/scitranslmed.aad4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Callejas D, et al. Treatment of diabetes and long-term survival after insulin and glucokinase gene therapy. Diabetes. 2013;62(5):1718–1729. doi: 10.2337/db12-1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gaddy DF, Riedel MJ, Pejawar-Gaddy S, Kieffer TJ, Robbins PD. In vivo expression of HGF/NK1 and GLP-1 From dsAAV vectors enhances pancreatic ß-cell proliferation and improves pathology in the db/db mouse model of diabetes. Diabetes. 2010;59(12):3108–3116. doi: 10.2337/db09-1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rademaker MT, Charles CJ, Ellmers LJ, Lewis LK, Nicholls MG, Richards AM. Prolonged urocortin 2 administration in experimental heart failure: sustained hemodynamic, endocrine, and renal effects. Hypertension. 2011;57(6):1136–1144. doi: 10.1161/HYPERTENSIONAHA.111.173203. [DOI] [PubMed] [Google Scholar]
- 20.Lai NC, et al. Intravenous AAV8 encoding Urocortin-2 increases function of the failing heart in mice. Hum Gene Ther. 2015;26(6):347–356. doi: 10.1089/hum.2014.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kautzky-Willer A, et al. Insulin sensitivity during oral glucose tolerance test and its relations to parameters of glucose metabolism and endothelial function in type 2 diabetic subjects under metformin and thiazolidinedione. Diabetes Obes Metab. 2006;8(5):561–567. doi: 10.1111/j.1463-1326.2005.00568.x. [DOI] [PubMed] [Google Scholar]
- 22.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021–1029. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 23.Graham DJ, et al. Risk of acute myocardial infarction, stroke, heart failure, and death in elderly Medicare patients treated with rosiglitazone or pioglitazone. JAMA. 2010;304(4):411–418. doi: 10.1001/jama.2010.920. [DOI] [PubMed] [Google Scholar]
- 24.Zezos P, Renner EL. Liver transplantation and non-alcoholic fatty liver disease. World J Gastroenterol. 2014;20(42):15532–15538. doi: 10.3748/wjg.v20.i42.15532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roth DM, Drumm JD, Bhargava V, Swaney JS, Gao MH, Hammond HK. Cardiac-directed expression of adenylyl cyclase and heart rate regulation. Basic Res Cardiol. 2003;98(6):380–387. doi: 10.1007/s00395-003-0429-4. [DOI] [PubMed] [Google Scholar]
- 26.Schenk S, et al. Sirt1 enhances skeletal muscle insulin sensitivity in mice during caloric restriction. J Clin Invest. 2011;121(11):4281–4288. doi: 10.1172/JCI58554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coste SC, et al. Abnormal adaptations to stress and impaired cardiovascular function in mice lacking corticotropin-releasing hormone receptor-2. Nat Genet. 2000;24(4):403–409. doi: 10.1038/74255. [DOI] [PubMed] [Google Scholar]
- 28. ASTM D4809. Standard test method for heat of combustion of liquid hydrocarbon fuels by bomb calorimeter (precision method). 2013; ASTM International. http://www.astm.org/Standards/D4809.htm Accessed August 24, 2016.