Summary
Malignant pleural mesothelioma is a rare malignant disease that in the majority of cases is associated with asbestos exposure. The incidence in Europe is about 20 per million inhabitants and it is increasing worldwide. Initial symptoms are shortness of breath, pleural effusion, cough, and chest pain. The typical growth pattern is along the pleural surface; however, infiltration of the lung and/or mediastinal and chest wall structures can occur in a more advanced stage. Ultimately, distant metastases outside the chest can result. Several histological subtypes of pleural mesothelioma exist, which must be differentiated from either benign diseases or metastases in the pleural space by other tumor entities. This differential diagnosis can be very difficult and a large panel of immunohistochemical markers is required to establish the exact diagnosis. The standard procedure for confirming the disease and obtaining sufficient tissue for the diagnosis is videothoracoscopy. Full thickness biopsies are required, while transthoracic needle puncture of pleural fluid or tissue is considered to be insufficient for a cytological diagnosis. Complete and detailed staging is mandatory for categorization of the disease as well as for therapeutic decision making.
Keywords: Malignant pleural mesothelioma, Epidemiology, Staging, Pathology, Diagnosis
Epidemiology
Asbestos exposure is the main risk factor for the development of malignant pleural mesothelioma (MPM) [1]. Asbestos comprises silicate minerals with very thin fibers: chrysotile, crocidolite as serpentines, amosite, anthophyllite, tremolite, and actinolite from the amphibole group [2]. Chrysotile is biologically active and detectable in the lungs for a shorter time. Chrysotile, amosite, and crocidolite were mined and used in ship and railway construction as well as in fire protection engineering. The first evidence of their high carcinogenic potential was found in the UK and South Africa as early as the 1960s [3]. Amosite and crocidolite seem to have a higher carcinogenicity than the other types of asbestos [2]. Asbestos exposure is typically labor-dependent and is recognized as an occupational disease. More recently, a shift has been observed from asbestos-removal workers to professionals involved in post-construction work, e. g., electricians, plumbers, or heat protection technicians. This is paralleled by a profession-dependent gender distribution, as more than 80 % of affected individuals are men [4].
“Environmental” occurrence of mesothelioma has been found in people growing up in the vicinity of natural asbestos resources (Turkey, Corsica, Cyprus) or in areas where asbestos was used for the whitening of house walls. The load in rooms built with asbestos-containing materials was initially seen as hazardous. The actual resulting asbestos dose is, however, extremely low and carcinogenic levels are not detectable [5].
Furthermore, there is an increasing incidence of nonoccupational asbestos disease among housewives and family members of asbestos workers as well as a high environmental impact in the vicinity of mining and processing facilities [6, 7].
There is a clear correlation between the amount of asbestos exposure and the incidence of MPM. The mean latency period between exposure to asbestos and the onset of symptoms is up to 40 years, and 99 % of cases show a latency of more than 15 years [8].
The occurrence of MPM is independent of other asbestos-associated diseases such as classic asbestosis of the lung (interstitial lung disease with fibrosis) and benign pleural plaques. Although pleural plaques are also associated with asbestos exposure, studies from Australia could not find any connection between plaques and an increased incidence of MPM [9].
The incidence of MPM varies between 7 per million inhabitants in Japan and 40 per million in Australia. In Europe, the average incidence is 20 per million inhabitants. The frequency is highly dependent on the amount of asbestos removal, asbestos import, and industrialization. In Europe, peak incidence is to be expected between 2015 and 2020 due to the long latency period [10].
By contrast, the incidence of mesothelioma without asbestos contact is extremely low (<1: 1 million). Other potential cofactors for the development of mesothelioma besides asbestos are synthetic materials (ceramics, nanoparticles), ionizing radiation, and SV-40 virus infections [11].
The impact of cigarette smoke as well as numerous other fibrous materials such as glass fibers and mineral glass wool is, however, excluded. Genetic factors may play a role, since both familial clustering and endemic accumulation in populations with high natural exposure are known in Turkey [5, 12].
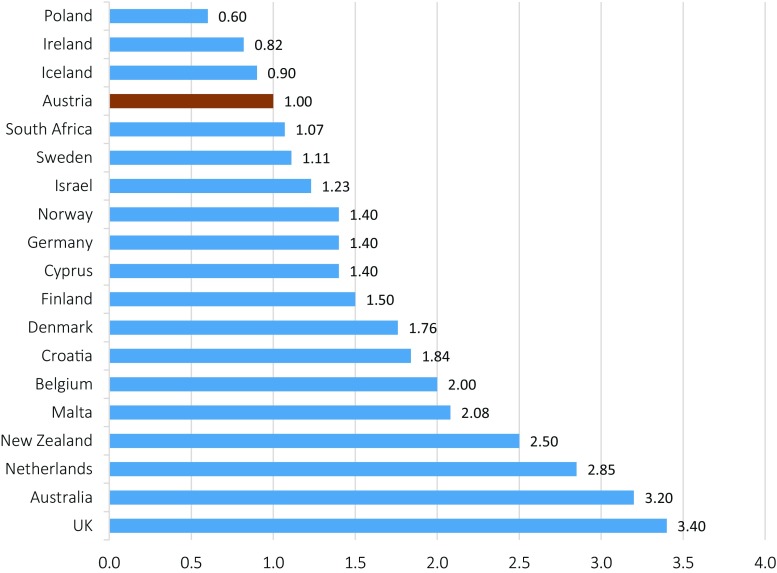
In Austria, there have been 276 cases of MPM approved by the AUVA (Allgemeine Unfallversicherungsanstalt – General accident insurance company) as being caused occupationally within the last 5 years. Of these, 53 were approved in 2014 only. In contrast to this, ten asbestos-related MPM cases were documented in 1995 and 41 in 2005. However, there is still uncertainty about the number of MPM cases not being reported to the AUVA. A comparison of the incidence of MPM worldwide and in Austria is depicted in Fig. 1.
Fig. 1.
Incidence of MPM in comparison to Austria [25]
Screening
In the current European Society of Thoracic Surgery (ESTS)/European Respiratory Society (ERS) guidelines no general screening methods are recommended [13]. This is based on the low sensitivity of even advanced imaging techniques such as low-dose computed tomography (CT) in screening of asbestos workers.
Circulating biomarkers, such as osteopontin, mesothelin-related peptides, and soluble mesothelin-related peptide (SMRP) [14], and fibulin-3 [15] have also been evaluated in MPM extensively. However, none of them are considered to be a reliable screening tool, since false-positive results are too frequent [16].
Diagnosis
Clinical symptoms
Specific symptoms of MPM are dyspnea, cough, and chest pain on initial examination. Shortness of breath is often initially caused by a pleural effusion and later by extensive restriction due to pleural and pulmonary tumor masses in the thoracic cavity. Patients describe chest pain as diffuse, sometimes radiating into the shoulders, arms, or abdomen. Tumor ingrowth into the neural structures of the brachial plexus and the intercostal or paravertebral structures can also cause neuropathic pain. Weight loss is a symptom of more advanced disease.
Typically, MPM occurs initially unilaterally. The tumor can, however, spread to the other pleural cavity or into the peritoneum in the further course of disease. Compared with lung cancer, distant metastases in the extrathoracic lymph nodes or in other parenchymal organs are usually rare, although they do occur in very advanced stages [17].
Diagnostic procedures
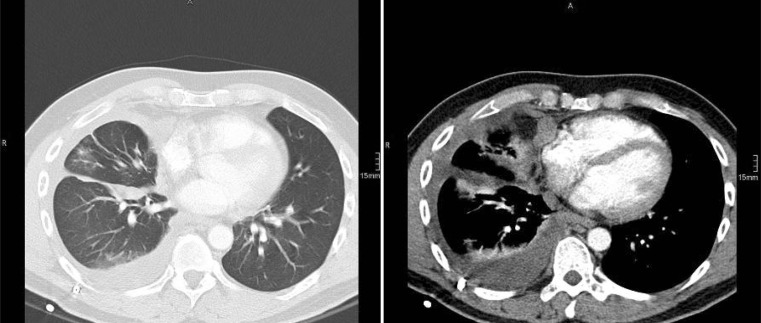
The typical finding on chest X‑rays of patients with MPM is pleural effusion or pleural thickening, which, however, is not specific. CT scan (Fig. 2) is more helpful, but it still does not allow a definitive diagnosis to be made since its sensitivity reaches only 40 %, and in most cases it does not distinguish between benign and malignant processes. The same holds true for positron emission tomography (PET)-CT where no clear standardized uptake value (SUV) level is considered suggestive for MPM and false-positive results can occur in other processes such as tuberculosis, parapneumonic effusions, and uremia [18].
Fig. 2.
Computer tomography of patient with malignant pleural mesothelioma showing circular involvement of the voscera and parietal pleura, pericardium and mediastinum. Pulmonary window (left) and mediastinal window (right)
Puncture of the pleural effusion that is usually present and cytological examination of the fluid is also not conclusive, especially since the differential diagnosis with pleural metastases of other tumors such as bronchial or breast cancer (e. g., adenocarcinomas) cannot be made in most cases. Also the macroscopic aspect of MPM is so variable that simple thoracoscopy does not confirm the diagnosis.
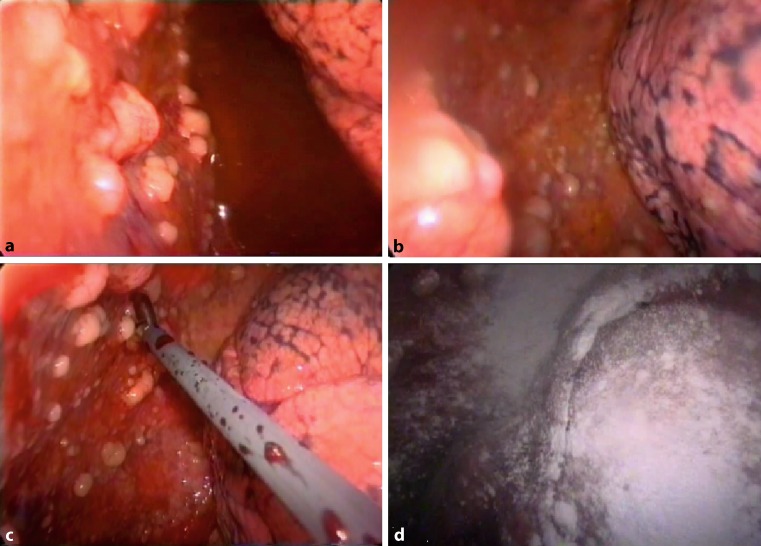
For these reasons, the precise diagnosis of MPM requires a histopathological confirmation and thoracoscopy remains the standard procedure for obtaining tissue and performing macroscopic staging of the pleural tumor spread at the same time (Fig. 3). Thoracoscopy can be performed with the patient under local anesthesia or as video thoracoscopy via a surgical approach. This allows one to combine the diagnostic procedure with the initial therapeutic step of talc pleurodesis (Fig. 3). Only in exceptional situations should a CT- or ultrasound-guided fine needle biopsy be performed, which, however, has a a clearly lower sensitivity.
Fig. 3.
Video-assisted thoracoscopic view of MPM mainly on the parietal pleura (a, b), forceps biopsy (c), and talc pleurodesis (d)
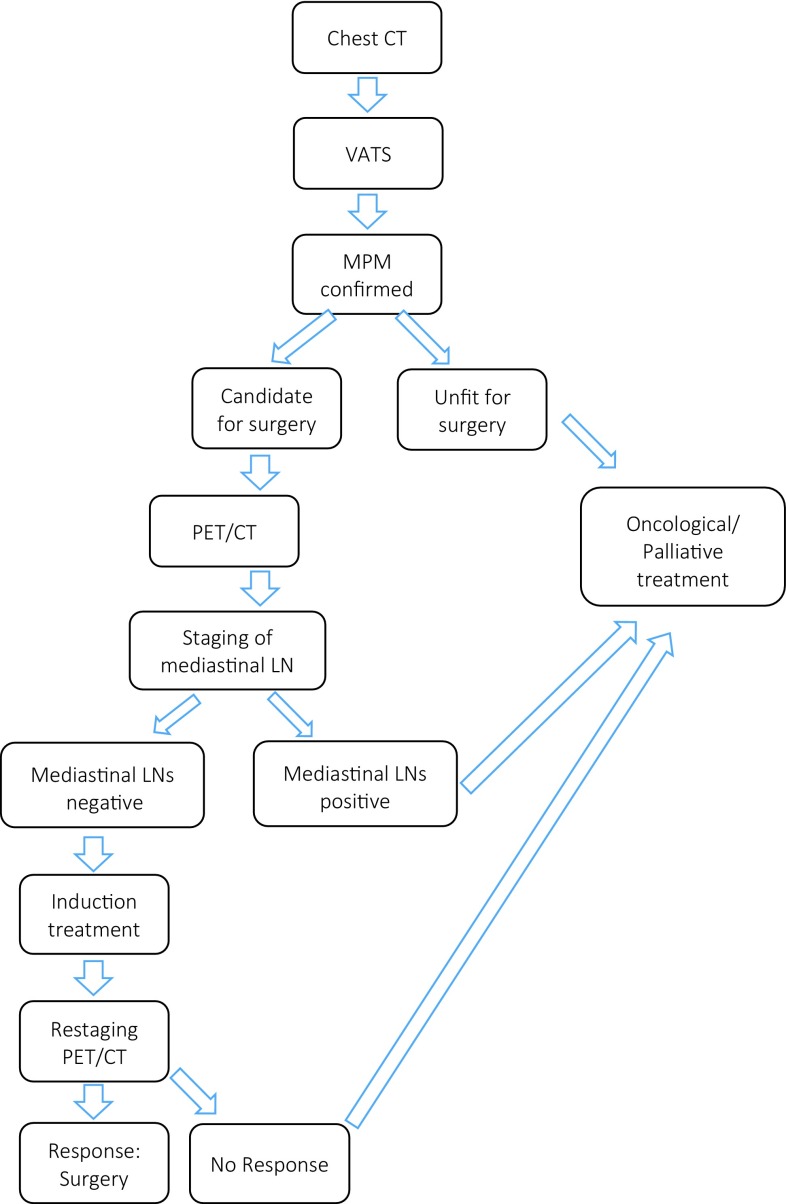
The typical diagnostic algorithm applied in most centers around the world is displayed in Fig. 4.
Fig. 4.
Proposed staging algorithm for MPM patients in Austria
Histopathology
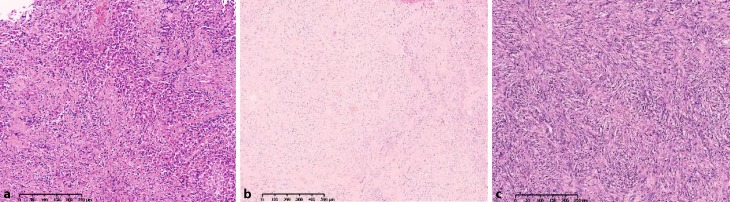
MPM derives from the pleural stem cell, which exhibits epithelioid and sarcomatoid growing patterns at the same time. Depending on which component is predominant, three histological types of MPM can be distinguished: epithelioid (50–70 %), sarcomatoid (7–20 %), and a mixed or biphasic form (20–35 %; Table 1 and Fig. 5).
Table 1.
Histological specification of malignant pleural mesothelioma [23]
| Epithelioid | Sarcomatoid | Biphasic mixed |
|---|---|---|
| – Tubulopapillary – Acinar – Glandular – Adenomatoid – Solid epithelioid patterns – Small cell – Oat cell Differential diagnosis: metastatic carcinomas and other epithelioid tumors |
Mimic malignant mesenchymal tumors: leiomyosarcoma synovial sarcoma Desmoplastic mesothelioma bland tumor cells Differential diagnosis: sarcomatoid carcinoma and other sarcomas |
Combination of all epithelioid and sarcomatoid features Differential diagnosis: Synovial sarcoma, other mixed or biphasic tumors |
Fig. 5.
Examples of malignant pleural mesothelioma (MPM): epithelioid MPM a), biphasic MPM (b), and sarcomatoid MPM (c). (Kindly provided by Dr. Luka Brcic, Department of Pathology, Medical University Graz)
The pathological diagnosis and differential diagnosis of MPM can be very challenging. In a French study, the initial diagnosis of MPM was revised as false positive in 13 % of cases [19]. This can be explained in part by the fact that MPM can present in very heterogeneous forms on the one hand and must be distinguished from benign processes and other tumors, especially metastases of various tumor entities, on the other hand. Such a differential diagnosis can be particularly difficult since mesothelioma-like features can also be found in some lymphomas, thymomas, and carcinomas, etc.
Full-thickness biopsies are required to separate invasive from noninvasive growth patterns and a panel of numerous immunohistochemical markers is required for the differentiation of epithelioid MPM from adenocarcinoma [13].
Staging
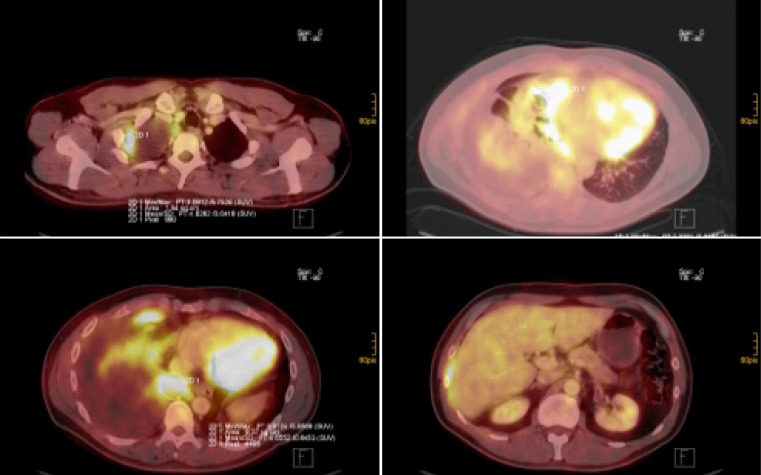
Both CT and PET-CT (Fig. 6), however, are useful for the further staging.
Fig. 6.
FDG PET-CT images: malignant pleural mesothelioma of the right pleural cavity (various slides of PET/CT fusion imaging). Varoius slides of CT/PET fusion imaging showing pleural tumor apical right (top left), involving the visceral and parietal pleura in the pleura costodiaphragmatic area (bottom left and right) and the pericardium (top right)
For all patients, the following assessments for staging and further treatment are required: After initial imaging with CT scan and confirmation of disease via video-assisted thoracic surgery (VATS), a potential candidate for surgical treatment should undergo PET-CT scanning to rule out distant metastasis and involvement of the abdomen and the mediastinal lymph nodes. To rule out the latter, histological confirmation has to be made either by endobronchial/endo-esophageal ultrasonography and transbronchial needle aspiration (EBUS/EUS-TBNA) or mediastinoscopy or VATS according to the lymph node station involvement and the involved side.
If nodes are negative, patients can proceed to induction treatment and should be re-staged with CT or PET-CT. In some cases of unclear involvement of adjacent structures (e. g., chest wall), magnetic resonance imaging (MRI) can be added in order to judge the resectability.
The investigations shown in Table 2 were recommended by many consensus groups.
Table 2.
Clinical approach and pretherapeutic evaluation according to ERS/ESTS recommendations [13]
| Investigation at presentation (all patients) | |
| Demographics | Gender, age, asbestos exposure |
| Clinical history | Performance status symptoms |
| Physical examination | Body weight |
| Radiology | Chest radiograph |
| Blood tests | – |
| Investigations for diagnosis and staging | |
| Biopsy of tumor, histological confirmation | – Thoracoscopy – Thoracocentesis – Needle aspiration |
| Radiology | – CT scan – Brain MRI or CT – Bone scan as required |
| Pulmonary function tests | – |
CT computer tomography, MRI magnetic resonance imaging
The most recent available and widely used TNM-based stating system was developed by the International Mesothelioma Interest Group (IMIG) and was also approved by the Union for International Cancer Control (UICC; Tables 3 and 4).
Table 3.
TNM staging of malignant pleural mesothelioma [24]
| T0 | No evidence of primary tumor |
| T1 | Tumor limited to the ipsilateral parietal pleura with or without mediastinal pleura and with or without diaphragmatic pleural involvement |
| T1a | No involvement of the visceral pleura |
| T1b | Tumor also involving the visceral pleura |
| T2 | Tumor involving each of the ipsilateral pleural surfaces (parietal, mediastinal, diaphragmatic, and visceral pleura) with at least one of the following: – Involvement of the diaphragmatic muscle – Extension of tumor from the visceral pleura into the underlying pulmonary parenchyma |
| T3 | Locally advanced but potentially resectable tumor; tumor involving all of the ipsilateral pleural surfaces (parietal, mediastinal, diaphragmatic, and visceral pleura) with at least one of the following: – Involvement of the endothoracic fascia – Extension into the mediastinal fat – Solitary, completely resectable focus of tumor extending into the soft tissue of the chest wall – Nontransmural involvement of the pericardium |
| T4 | Locally advanced, technically unresectable tumor; tumor involving all of the ipsilateral pleural surfaces (parietal, mediastinal, diaphragmatic, and visceral pleura) with at least one of the following: – Diffuse extension or multifocal masses of tumor in the chest wall, with or without associated rib destruction – Direct diaphragmatic extension of the tumor to the peritoneum – Direct extension of the tumor to the contralateral pleura – Direct extension of the tumor to a mediastinal organ – Direct extension of the tumor into the spine – Tumor extending through to the internal surface of the pericardium with or without a pericardial effusion or tumor involving the myocardium |
| Regional lymph nodes (N) | |
| NX | Regional lymph node(s) cannot be assessed |
| N0 | No regional lymph node metastases |
| N1 | Metastases in the ipsilateral bronchopulmonary or hilar lymph node |
| N2 | Metastases in the subcarinal or in the ipsilateral mediastinal lymph node, including the ipsilateral internal mammary and peridiaphragmatic nodes |
| N3 | Metastases in the contralateral mediastinal, contralateral internal mammary, ipsilateral, or contralateral supraclavicular lymph nodes |
| Distant metastases (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Table 4.
UICC–IMIG staging [24]
| UICC staging (7th edition) | |||
|---|---|---|---|
| Stage IA | T1a | N0 | M0 |
| Stage IB | T1b | N0 | M0 |
| Stage II | T2 | N0 | M0 |
| Stage III | T1, T2 T1, T2 T3 |
N1 N2 N0, N1, N2 |
M0 M0 M0 |
| Stage IV | T4 T1–4 T1–4 |
N0–3 N3 N0–3 |
M0 M0 M1 |
A possible staging algorithm for MPM patients is displayed in Fig. 4.
Prognosis
The prognosis for MPM depends on the patient’s age, gender, tumor stage, and geographic region [20]. Other factors such as weight loss and performance status are important for the prognosis as in other tumor entities as well as quality of life and symptom scores. Epithelioid MPM has a better overall prognosis than non-epithelioid histological subtypes. Low hemoglobin levels, high platelet levels, and high serum lactat dehydrogenase (LDH) are prognostically unfavorable characteristics [21]. Numerous new laboratory markers are in evaluation, but no validated data on their prognostic value are available yet [22].
Acknowledgments
Funding
The publication has not been funded by any pharmaceutical company.
Open access funding provided by Medical University of Vienna.
Conflict of interest
C. Geltner, P. Errhalt, B. Baumgartner, G. Ambrosch, B. Machan, J. Eckmayr, T. Klikovits, M.A. Hoda, H. Popper, and W. Klepetko declare that they have no competing interests.
Footnotes
All authors contribute on behalf of the Austrian Mesothelioma Interest Group (AMIG).
References
- 1.Offermans NS, Vermeulen R, Burdorf A, Goldbohm RA, Kauppinen T, Kromhout H, et al. Occupational asbestos exposure and risk of pleural mesothelioma, lung cancer, and laryngeal cancer in the prospective Netherlands cohort study. J Occup Environ Med. 2014;56:6–19. doi: 10.1097/JOM.0000000000000060. [DOI] [PubMed] [Google Scholar]
- 2.Barlow CA, Lievense L, Gross S, Ronk CJ, Paustenbach DJ. The role of genotoxicity in asbestos-induced mesothelioma: an explanation for the differences in carcinogenic potential among fiber types. Inhal Toxicol. 2013;25:553–567. doi: 10.3109/08958378.2013.807321. [DOI] [PubMed] [Google Scholar]
- 3.Wagner JC, Sleggs CA, Marchand P. Diffuse pleural mesothelioma and asbestos exposure in the North Western Cape Province. Br J Ind Med. 1960;17:260–271. doi: 10.1136/oem.17.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delfino RJ, Anton-Culver H, Saltzstein SL. Gender-related differences in the distribution of thoracic versus abdominal malignant mesothelioma. Cancer Detect Prev. 1995;19:301–307. [PubMed] [Google Scholar]
- 5.Dogan AU, Baris YI, Dogan M, Emri S, Steele I, Elmishad AG, et al. Genetic predisposition to fiber carcinogenesis causes a mesothelioma epidemic in Turkey. Cancer Res. 2006;66:5063–5068. doi: 10.1158/0008-5472.CAN-05-4642. [DOI] [PubMed] [Google Scholar]
- 6.Bourdes V, Boffetta P, Pisani P. Environmental exposure to asbestos and risk of pleural mesothelioma: review and meta-analysis. Eur J Epidemiol. 2000;16:411–417. doi: 10.1023/A:1007691003600. [DOI] [PubMed] [Google Scholar]
- 7.Maule MM, Magnani C, Dalmasso P, Mirabelli D, Merletti F, Biggeri A. Modeling mesothelioma risk associated with environmental asbestos exposure. Environ Health Perspect. 2007;115:1066–1071. doi: 10.1289/ehp.9900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lanphear BP, Buncher CR. Latent period for malignant mesothelioma of occupational origin. J Occup Med. 1992;34:718–721. [PubMed] [Google Scholar]
- 9.Reid A, de Klerk N, Ambrosini G, Olsen N, Pang SC, Musk AW. The additional risk of malignant mesothelioma in former workers and residents of Wittenoom with benign pleural disease or asbestosis. Occup Environ Med. 2005;62:665–669. doi: 10.1136/oem.2004.018531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson BW, Lake RA. Advances in malignant mesothelioma. N Engl J Med. 2005;353:1591–1603. doi: 10.1056/NEJMra050152. [DOI] [PubMed] [Google Scholar]
- 11.Kanbay A, Ozer Simsek Z, Tutar N, Yilmaz I, Buyukoglan H, Canoz O, et al. Non-asbestos-related malignant pleural mesothelioma. Intern Med. 2014;53:1977–1979. doi: 10.2169/internalmedicine.53.0900. [DOI] [PubMed] [Google Scholar]
- 12.Roushdy-Hammady I, Siegel J, Emri S, Testa JR, Carbone M. Genetic-susceptibility factor and malignant mesothelioma in the Cappadocian region of Turkey. Lancet. 2001;357:444–445. doi: 10.1016/S0140-6736(00)04013-7. [DOI] [PubMed] [Google Scholar]
- 13.Scherpereel A, Astoul P, Baas P, Berghmans T, Clayson H, de Vuyst P, et al. Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the management of malignant pleural mesothelioma. Eur Respir J. 2010;35:479–495. doi: 10.1183/09031936.00063109. [DOI] [PubMed] [Google Scholar]
- 14.Park EK, Thomas PS, Creaney J, Johnson AR, Robinson BW, Yates DH. Blood-based early detection of malignant mesothelioma. J Clin Oncol. 2009;27:160. doi: 10.1200/JCO.2008.19.3839. [DOI] [PubMed] [Google Scholar]
- 15.Pass HI. Biomarkers and prognostic factors for mesothelioma. Ann Cardiothorac Surg. 2012;1:449–456. doi: 10.3978/j.issn.2225-319X.2012.10.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park EK, Thomas PS, Yates DH. Biomarkers for early detection of mesothelioma in asbestos-exposed subjects. Clin Chem Lab Med. 2010;48:1673–1674. doi: 10.1515/CCLM.2010.306. [DOI] [PubMed] [Google Scholar]
- 17.Finn RS, Brims FJ, Gandhi A, Olsen N, Musk AW, Maskell NA, et al. Postmortem findings of malignant pleural mesothelioma: a two-center study of 318 patients. Chest. 2012;142:1267–1273. doi: 10.1378/chest.11-3204. [DOI] [PubMed] [Google Scholar]
- 18.Duysinx B, Nguyen D, Louis R, Cataldo D, Belhocine T, Bartsch P, et al. Evaluation of pleural disease with 18-fluorodeoxyglucose positron emission tomography imaging. Chest. 2004;125:489–493. doi: 10.1378/chest.125.2.489. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg M, Imbernon E, Rolland P, Gilg Soit Ilg A, Saves M, de Quillacq A, et al. The French National Mesothelioma Surveillance Program. Occup Environ Med. 2006;63:390–395. doi: 10.1136/oem.2005.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spirtas R, Connelly RR, Tucker MA. Survival patterns for malignant mesothelioma: the SEER experience. Int J Cancer. 1988;41:525–530. doi: 10.1002/ijc.2910410409. [DOI] [PubMed] [Google Scholar]
- 21.Herndon JE, Green MR, Chahinian AP, Corson JM, Suzuki Y, Vogelzang NJ. Factors predictive of survival among 337 patients with mesothelioma treated between 1984 and 1994 by the cancer and leukemia group B. Chest. 1998;113:723–731. doi: 10.1378/chest.113.3.723. [DOI] [PubMed] [Google Scholar]
- 22.Grigoriu BD, Scherpereel A, Devos P, Chahine B, Letourneux M, Lebailly P, et al. Utility of osteopontin and serum mesothelin in malignant pleural mesothelioma diagnosis and prognosis assessment. Clin Cancer Res. 2007;13:2928–2935. doi: 10.1158/1078-0432.CCR-06-2144. [DOI] [PubMed] [Google Scholar]
- 23.Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, editors. World Health Organisation Classification of Tumours. Pathology and Genetics of the Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004. pp. 9–124. [Google Scholar]
- 24.Rusch VW. A proposed new international TNM staging system for malignant pleural mesothelioma from the International Mesothelioma Interest Group. Lung Cancer. 1996;14:1–12. doi: 10.1016/0169-5002(95)00508-0. [DOI] [PubMed] [Google Scholar]
- 25.Bianchi C, Bianchi T. Global mesothelioma epidemic: Trend and features. Indian J Occup Environ Med. 2014;18:82–88. doi: 10.4103/0019-5278.146897. [DOI] [PMC free article] [PubMed] [Google Scholar]