Abstract
Aim
The purpose of the study was to improve the ultrasonographic assessment of the anterior cruciate ligament by an inclusion of a dynamic element. The proposed functional modification aims to restore normal posterior cruciate ligament tension, which is associated with a visible change in the ligament shape. This method reduces the risk of an error resulting from subjectively assessing the shape of the posterior cruciate ligament. It should be also emphasized that the method combined with other ultrasound anterior cruciate ligament assessment techniques helps increase diagnostic accuracy.
Methods
Ultrasonography is used as an adjunctive technique in the diagnosis of anterior cruciate ligament injury. The paper presents a sonographic technique for the assessment of suspected anterior cruciate ligament insufficiency supplemented by the use of a dynamic examination. This technique can be recommended as an additional procedure in routine ultrasound diagnostics of anterior cruciate ligament injuries.
Results
Supplementing routine ultrasonography with the dynamic assessment of posterior cruciate ligament shape changes in patients with suspected anterior cruciate ligament injury reduces the risk of subjective errors and increases diagnostic accuracy. This is important especially in cases of minor anterior knee instability and bilateral anterior knee instability.
Conclusions
An assessment of changes in posterior cruciate ligament using a dynamic ultrasound examination effectively complements routine sonographic diagnostic techniques for anterior cruciate ligament insufficiency.
Keywords: ultrasound ligament assessment, posterior cruciate ligament, anterior knee instability, anterior cruciate ligament, ultrasonography, knee ultrasound
Abstract
Cel pracy
Celem pracy jest ocena możliwości poprawienia ultrasonograficznej oceny niewydolności więzadła krzyżowego przedniego poprzez wprowadzenie elementu badania dynamicznego. Modyfikacja czynnościowa ma na celu przywrócenie prawidłowego napięcia więzadła krzyżowego tylnego, czemu towarzyszy widoczna zmiana jego kształtu. Opisywana metoda zmniejsza ryzyko popełnienia błędu wynikającego z subiektywnej oceny kształtu więzadła krzyżowego tylnego i – co należy podkreślić – w połączeniu z innymi sposobami ultrasonograficznej oceny więzadła krzyżowego przedniego pozwala zwiększyć trafność diagnozy.
Metoda
Jako metodę wspomagającą w diagnostyce uszkodzeń więzadła krzyżowego przedniego wykorzystuje się ultrasonografię. W pracy przedstawiono technikę badania i oceny ultrasonograficznej wydolności więzadła rozszerzoną o badanie dynamiczne. Technika ta może być rekomendowana jako dodatkowa procedura w diagnostyce ultrasonograficznej uszkodzeń więzadła krzyżowego przedniego.
Rezultaty
Podczas ultrasonograficznego badania pacjentów z podejrzeniem uszkodzenia więzadła krzyżowego przedniego uzupełnionego metodą dynamicznej oceny zmiany kształtu więzadła krzyżowego tylnego zmniejsza się ryzyko popełnienia subiektywnego błędu przy ocenie i zapewnia większą trafność diagnozy. Ma to znaczenie zwłaszcza u osób z niewielką niestabilnością przednią stawu kolanowego, jak również z niestabilnością przednią występującą jednocześnie w obu stawach kolanowych.
Wnioski
Ocena zmiany przebiegu więzadła krzyżowego tylnego w badaniu dynamicznym USG skutecznie uzupełnia dotychczasowe sposoby diagnozowania niewydolności więzadła krzyżowego przedniego.
Introduction
Traumatic knee injuries constitute one of the most common problems, especially in individuals who take active part in sports activities(1–11). Accounting for 30–70% of all bodily injuries, sport-related knee trauma is very common (boxing, taekwondo, soccer, skiing, basketball)(5, 7, 12–15). A growing interest in sports, especially among children and adolescents, results in an increasing incidence of anterior cruciate ligament (ACL) and meniscal injuries. ACL trauma may occur in people at any age, however it appears most common in young individuals, especially males (54%), who show a direct correlation between practicing a sport and experiencing traumatic knee injuries(13, 16). Moreover, studies have shown that the rate of ACL injuries in young female basketball players is 8 times higher than that in males. Other studies found that 55% of ACL injuries in young people are associated with simultaneous meniscal injuries. Bira et al. reported combined ACL and meniscal injuries in 73% of young people with active epiphyseal plates(17). Rubin et al. showed concomitant ACL and meniscal damage in 35–78% of the evaluated patients(3, 18). The complexity of injuries to the knee's articular capsule, ligaments, and menisci should be emphasized, as mentioned before by O'Donoghue, who had described a concomitant disruption to the medial collateral ligament, ACL, and the medial meniscus as the “unhappy triad”(19–22).
Magnetic resonance imaging (MRI) is an established imaging study for the evaluation of ACL(23–32).
For many years ultrasonography has also been used in the diagnostics of ACL injuries(23, 25, 28, 29, 33–39). Some authors generally question the use of ultrasound in diagnosing ligament and meniscal injuries of the knee, claiming that the method is characterized by low specificity and too many false positive findings(6, 40). Conversely, others report the method's high effectiveness (of 78% or more) in diagnosing traumatic soft tissue injuries of the knee joint, including ACL damage(39, 41, 42).
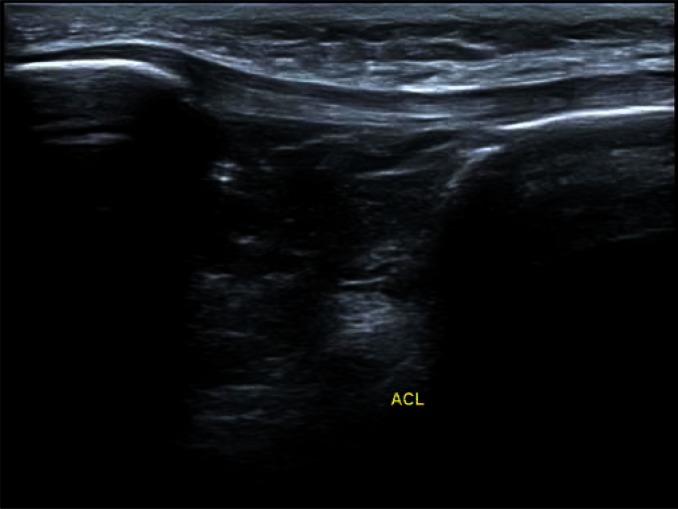
Nonetheless, a direct sonographic evaluation of the ACL structure is sometimes difficult or even impossible(32, 35, 36). Ultrasound images obtained from the anterior view of the knee with the joint flexed to up to approximately 90 degrees, typically help in good visualization of only a fragment of this ligament in the area of its distal insertion (Fig. 1).
Fig. 1.
Distal part of the anterior cruciate ligament – an anterior view
A dynamic examination of the knee joint, i.e. the ultrasoundguided anterior drawer test, can also be challenging, especially in fresh injuries accompanied by increased muscle tension that can mask the signs of ACL insufficiency(21, 43).
An ultrasound-based test for anterior knee instability developed by Grzelak et al. is a diagnostic method worth noting(29). This is a modified anterior drawer test, in which the patient sits at the edge of the examination bed with a bolster of approximately 20 cm in diameter inserted underneath the distal part of his or her thigh, causing the limb to hang loosely. An ultrasound transducer is then placed longitudinally, parallel to the patellar ligament. After identifying the anatomic landmarks (the intercondylar eminence, tibial tuberosity, and patellar ligament), the ultrasound technician exerts progressively increasing pressure onto the patient's hanging leg. The patient's knee joint bends creating a leverage, which results in anterior shifting of the intercondylar eminence with respect to the patellar ligament. Grzelak et al. claimed that the difference in the distance by which the intercondylar eminence shifts anteriorly with respect to the patellar ligament in the affected limb and the corresponding distance in the other (healthy) limb indicates a total ACL tear, which has been confirmed via arthroscopy(29).
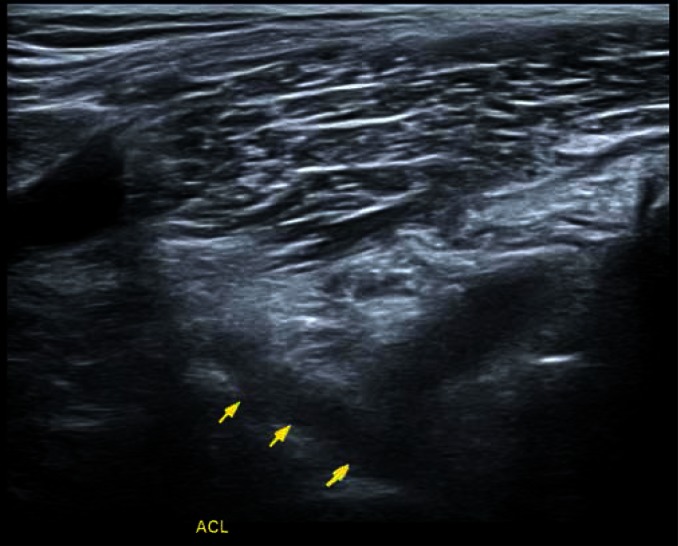
An ultrasound examination of the ACL from the posterior aspect of the knee (the popliteal fossa) can typically visualize the majority of the ligament (at least its proximal twothirds), however, this requires extensive experience of the ultrasonographist. If good quality images are difficult to obtain with a linear transducer, the ACL can be assessed with a convex array transducer (Fig. 2 and Fig. 3).
Fig. 2.
The anterior cruciate ligament – a posterior view
Fig. 3.
The transducer orientation needed for a posterior visualization of the anterior cruciate ligament
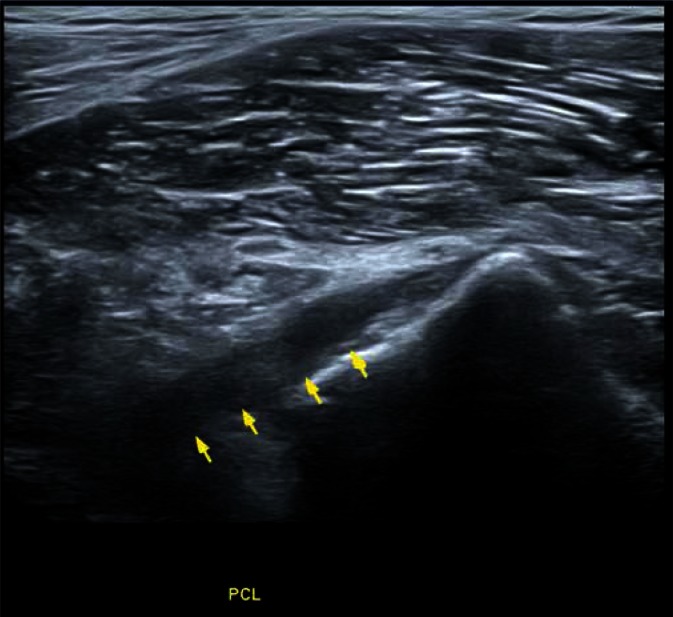
A number of investigators performing knee ultrasound examinations and preparing relevant reports have considered PCL shape (course) change as an important indicator of ACL insufficiency(32, 34, 35, 44) (Fig. 4).
Fig. 4.
The posterior cruciate ligament viewed posteriorly
Method
An ultrasound examination of the posterior cruciate ligament (PCL) is typically conducted in a patient lying prone (Fig. 5 and Fig. 6).
Fig. 5.
An ultrasonographic image of the posterior cruciate ligament
Fig. 6.
The orientation of a convex array transducer for examining the posterior cruciate ligament
This limits the possible masking effects of muscle tension on anterior knee instability. ACL insufficiency in a prone patient results in a slight anterior subluxation of the proximal tibia, which leads to a lowered tension in the PCL. As PCL relaxes, it forms a posteriorly convex arch(34, 35, 44).
A comparison between the knee joint with a suspected ACL injury and the other (healthy) joint allows the technician to evaluate the shape (course) of the PCL as an indirect sign of ACL insufficiency (anterior tibial subluxation). However, such an assessment of PCL shape is subjective and depends on ultrasound transducer placement(34, 35, 37, 38, 44).
The effects of slight changes in transducer orientation on the obtained images is greater in the case of convex array transducers, where a minute change in transducer placement often causes a dramatic change in the resulting image. Other challenges may be posed by assessing PCL shape change in mild or bilateral anterior knee instability.
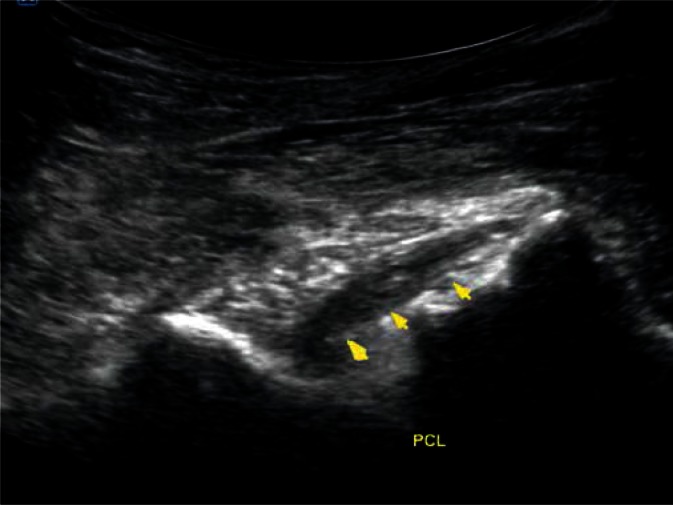
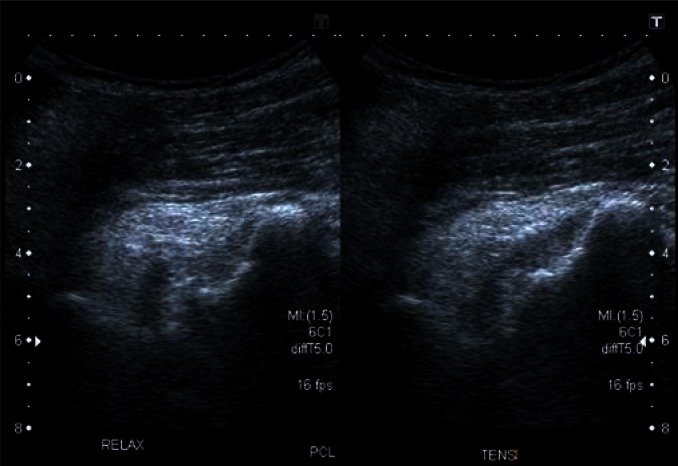
In such cases, we suggest introducing a functional modification involving PCL assessment during a dynamic examination (Fig. 7). During ultrasound examination, while watching the PCL on the screen, the ultrasonographist is holding the transducer with one hand while trying to displace the proximal tibial epiphysis posteriorly with the other. In cases of anterior knee instability, this maneuver restores normal tension to the lax and posteriorly convex PCL. The resulting change in PCL shape can be clearly seen on the monitor. Fig. 7 shows an image of the same PCL in these two extreme positions during a dynamic examination in a patient with anterior knee instability. The picture on the left shows the PCL showing an excessive posteriorly convex arch in the position of anterior subluxation, while the picture on the right shows a straight course of the PCL following a posterior manual displacement of the proximal tibial epiphysis.
Fig. 7.
An ultrasonographic view of the posterior cruciate ligament during a dynamic examination in a patient with anterior knee instability
Discussion
Although ultrasonography is a method commonly used in orthopedic diagnostics, its capacity for evaluating ACL injuries in anterior knee instability is still insufficient and incomplete. There is a growing need in orthopedic practice for a diagnostic method that would help assess ACL insufficiency in a simple, reliable, and accurate way. This paper presents the possibility of using an ultrasonographic technique in ACL injury diagnostics during a dynamic examination of PCL course in a position that is comfortable for the patient and, at the same time, it eliminates false images that are sometimes produced due to increased muscle tension following an injury. Unlike MRI scans, an ultrasound examination allows a dynamic assessment of the range of motion in the injured joint(28, 29, 32, 34–39).
Several ultrasound-based assessment methods have been suggested. They differed in transducer placement (anteriorly or posteriorly to the knee joint), the source of joint destabilizing forces (gravity or an externally applied force), and the number of persons engaged in the ultrasound examination(27, 29, 34, 35, 37, 38, 44).
The PCL shape (course) assessment technique presented here eliminates some of the flaws of previous methods. Although such an assessment, which is typically performed for comparison of both knees as a part of a single examination, requires extensive experience of the ultrasonographist, the extent to which diagnostic inaccuracy (due to such factors as transducer orientation) can be minimized is very high, which translates to increased reliability and repeatability of the presented method. At the same time, due to the patient's prone position, the examination may be conducted without the help of an assistant. Moreover, one advantage of the presented method is its adequate diagnostic effectiveness even in the acute injury phase. Additionally, due to its wide-spread use it can become an element of routine imaging in patients with suspected ACL injury.
Conclusion
Although considered to be the “golden mean” in skeletomuscular diagnostics, MRI in most cases is used only for a static examination in patients with anterior tibial subluxation, which is not necessarily synonymous with a functional knee instability. MRI is a relatively expensive diagnostic technique of limited availability. Furthermore, it is contraindicated in many patients (e.g. claustrophobia, the presence of certain metal implants), which often completely excludes the assessment of their knee.
Moreover, suspected ACL injury is required for the patient in order to be referred for an ACL MRI. However, patients may not be seen by an appropriate orthopedic surgeon, i.e. capable of identifying the signs of ACL damage, soon after knee injury. This is due to long waiting lists of patients needing specialist treatment, sometimes requiring 9 months or more of waiting time, which is characteristic for the Polish health care system. Therefore, before they can see a specialist through the state-funded system, patients sometimes seek medical assistance on their own and visit private ultrasonographic laboratories, where they can be offered a quick and accurate diagnosis. An accurate diagnosis is essential for successful treatment.
The functional modification proposed here, involving PCL assessment during a dynamic examination in patients with anterior knee instability, is a quick, non-invasive method helpful in ACL injury diagnosis, even in the acute phase, especially when combined with an assessment of ligament structure via an anterior and posterior view and ultrasound-guided assessment of ACL function in the anterior drawer test. This method is non-invasive, convenient for the patient, and it eliminates the effects of muscle tension on the possible anterior instability as well as significantly reduces the effects of the pain-induced limitation in the range of motion, typically present after an injury, on the feasibility of joint assessment.
Conflict of interest
Authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
References
- 1.Dziak A, Tayara S. Urazy i uszkodzenia sportowe. Kraków: Wydawnictwo Kasper; 2000. [Google Scholar]
- 2.Dziak A. Urazy i uszkodzenia sportowe. Acta Clinica. 2001;1:105–110. [Google Scholar]
- 3.Grzesiczak A, Wrzosek Z, Chantsoulis M, Ruta J, Sakowski J. Ocena funkcji stawu kolanowego po przebytym uszkodzeniu łąkotki przyśrodkowej leczonej metodą artroskopową. Kwart Ortop. 2011;3:235–242. [Google Scholar]
- 4.Kwiatkowski K. Patomechanizm śródstawowych, urazowych uszkodzeń stawu kolanowego. Stan Med. 2004;1:423–429. [Google Scholar]
- 5.Widuchowski J. Diagnostyka obrażeń stawu kolanowego u sportowców. Med Sportiva. 1998;2:279–288. [Google Scholar]
- 6.Patyk Cz, Kwiatkowski K, Orłowski J, Kuś WM. Uszkodzenia stawu kolanowego. In: Tylman D, Dziak A, editors. Traumatologia narządu ruchu. Vol. 29. Warszawa: Wydawnictwo Lekarskie PZWL; 2013. pp. 532–675. [Google Scholar]
- 7.Martínez HLE, Hernández DC, Pegueros PA, Franco Sánchez JG, Pineda Villaseñor C. Subclinical findings in the knees of taekwondo athletes: diagnostic ultrasound study. Gac Med Mex. 2014;150:259–265. [PubMed] [Google Scholar]
- 8.Unlu EN, Üstüner E, Saylisoy S, Yilmaz Ö, Özcan H, Erden I. The role of ultrasound in the diagnosis of meniscal tears and degeneration compared to MRI and arthroscopy. Acta Medica Anatolia. 2014;2:80–87. [Google Scholar]
- 9.Chrzanowska-Gawrońska A. Ocena znieczulenia podpajęczynówkowego z zastosowaniem 2% lidokainy i 25 μg fentanylu oraz 0,5% bupiwakainy do zabiegów artroskopii stawu kolanowego. Rozprawa doktorska. Poznań: Uniwersytet Medyczny; 2012. [Google Scholar]
- 10.Walczak M, Manikowski W, Gajewska E, Galasińska K. Urazy w obrębie stawu kolanowego u sportowców trenujących futbol amerykański. Piel Pol. 2012;4:181–186. [Google Scholar]
- 11.Dziak A. Leczenie zdestabilizowanego kolana. Acta Clinica. 2002;2:5–7. [Google Scholar]
- 12.Dziak A. Współczesne poglądy na leczenie i rehabilitację stawów kolanowych z patologią łąkotkową. Acta Clinica. 2001;1:193–198. [Google Scholar]
- 13.Kruczyński J, Ruszkowski K. Uszkodzenia wewnętrzne stawu kolanowego. In: Marciniak W, Szulc A, editors. Wiktora Degi ortopedia i rehabilitacja. Vol. 23. Warszawa: Wydawnictwo Lekarskie PZWL; 2003. pp. 233–250. [Google Scholar]
- 14.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 15.Dziak A, Rusin Z. Uszkodzenie łąkotek kolana. In: Dziak A, editor. Traumatologia sportowa: poradnik dla trenera. Warszawa: Centralny Ośrodek Sportu; 2000. pp. 117–120. [Google Scholar]
- 16.Słynarski K. Conference abstract. Treatment of early hyaline cartilage degeneration applying intra- and extraarticular techniques. Artroskopia i Chirurgia Stawów. 2009;5:31–32. [Google Scholar]
- 17.Bira M, Paradowski PT, Synder M, Witoński D. Ocena częstości występowania uszkodzeń struktur wewnątrzstawowych kolana u chorych z czynną chrząstką wzrostową. Pol Merk Lek. 2006;21:41–43. [PubMed] [Google Scholar]
- 18.Rubin DA, Paletta GA., Jr Current concepts and controversies in meniscal imaging. Magn Resons Imaging Clin N Am. 2000;8:243–270. [PubMed] [Google Scholar]
- 19.Shelbourne KD, Nitz PA. The O'Donoghue triad revisited. Combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19:474–477. doi: 10.1177/036354659101900509. [DOI] [PubMed] [Google Scholar]
- 20.O'Donoghue DH. Surgical treatment of fresh injuries to the major ligaments of the knee. J Bone Joint Surg Am. 1950;32:721–738. [PubMed] [Google Scholar]
- 21.Adamczyk G. Diagnostyka kliniczna uszkodzeń więzadeł krzyżowych stawu kolanowego. Acta Clinica. 2001;1:294–306. [Google Scholar]
- 22.Mioduszewski A. Strategia postępowania w uszkodzeniu więzadeł krzyżowych. Acta Clinica. 2002;2:17–25. [Google Scholar]
- 23.Czyrny Z. US and MR imaging of the postoperative knee. Eur J Radiol. 2007;62:44–67. doi: 10.1016/j.ejrad.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 24.Court-Payen M. Sonography of the knee: intra-articular pathology. J Clin Ultrasound. 2004;32:481–490. doi: 10.1002/jcu.20069. [DOI] [PubMed] [Google Scholar]
- 25.Lee D, Bouffard JA. Ultrasound of the knee. Eur J Ultrasound. 2001;14:57–71. doi: 10.1016/s0929-8266(01)00146-x. [DOI] [PubMed] [Google Scholar]
- 26.Jacobson JA. Musculoskeletal ultrasound: focused impact on MRI. AJR Am J Roentgenol. 2009;193:619–627. doi: 10.2214/AJR.09.2841. [DOI] [PubMed] [Google Scholar]
- 27.Dzianach M, Czwojdziński A, Piontek T, Sosnowski P. Diagnostic possibilities of ultrasound in estimation of the posterior cruciate ligament – anatomical and clinical study. Pol J Radiol. 2004;69:165–166. [Google Scholar]
- 28.Ptasznik R, Feller J, Bartlett J, Fitt G, Mitchell A, Hennessy O. The value of sonography in the diagnosis of traumatic rupture of the anterior cruciate ligament of the knee. AJR Am J Roentgenol. 1995;164:1461–1463. doi: 10.2214/ajr.164.6.7754893. [DOI] [PubMed] [Google Scholar]
- 29.Grzelak P, Podgórski M, Stefańczyk L, Domżalski M. Ultrasonographic test for complete anterior cruciate ligament injury. Indian J Orthop. 2015;49:143–149. doi: 10.4103/0019-5413.152432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donell ST, Marshall TJ, Darrah C, Shepstone L. Cruciate ligament assessment in MRI scans: a pilot study of a static drawer technique. Knee. 2006;13:137–144. doi: 10.1016/j.knee.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Skovgaard Larsen LP, Rasmussen OS. Diagnosis of acute rupture of the anterior cruciate ligament of the knee by sonography. Eur J Ultrasound. 2000;12:163–167. doi: 10.1016/s0929-8266(00)00109-9. [DOI] [PubMed] [Google Scholar]
- 32.Suzuki S, Kasahara K, Futami T, Iwasaki R, Ueo T, Yamamuro T. Ultrasound diagnosis of pathology of the anterior and posterior cruciate ligaments of the knee joint. Arch Orthop Trauma Surg. 1991;110:200–203. doi: 10.1007/BF00571059. [DOI] [PubMed] [Google Scholar]
- 33.Khan Z, Faruqui Z, Ogyunbiyi O, Rosset G, Iqbal J. Ultrasound assessment of internal derangement of the knee. Acta Orthop Belg. 2006;72:72–76. [PubMed] [Google Scholar]
- 34.Dzianach M. Rozprawa doktorska, Katedra Radiologii Klinicznej AM im. Poznań: Karola Marcinkowskiego w Poznaniu; 2006. Wartość oceny ultrasonograficznej wskaźnika łuku więzadła krzyżowego tylnego stawu kolanowego w rozpoznawaniu uszkodzeń więzadła krzyżowego przedniego. [Google Scholar]
- 35.Bianchi S, Martinoli C. Knee. In: Bianchi S, Martinoli C, editors. Ultrasound of the Musculoskeletal System. Vol. 14. Berlin Heidelberg: Springer-Verlag; 2007. pp. 637–744. [Google Scholar]
- 36.Jakubowski W, Serafin-Król M. Diagnostyka obrazowa w traumatologii narządu ruchu. In: Tylman D, Dziak A, editors. Traumatologia narządu ruchu. Vol. 2. Warszawa: Wydawnictwo Lekarskie PZWL; 2013. pp. 37–73. [Google Scholar]
- 37.Palm HG, Bergenthal G, Ehry P, Schwarz W, Schmidt R, Friemert B. Functional ultrasonography in the diagnosis of acute anterior cruciate ligament injuries: a field study. Knee. 2009;16:441–446. doi: 10.1016/j.knee.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 38.Friedl W, Glaser F. Dynamic sonography in the diagnosis of ligament and meniscal injuries of the knee. Arch Orthop Trauma Surg. 1991;110:132–138. doi: 10.1007/BF00395794. [DOI] [PubMed] [Google Scholar]
- 39.Krzyżanowski W, Szymańska A, Gawęda K, Tarczyńska M, Szczerbo-Trojanowska M. Ocena ultrasonograficzna uszkodzeń pourazowych stawu kolanowego. Pol J Radiol. 2007;72:253–254. [Google Scholar]
- 40.Słowiński W, Ruciński M, Słowiński K. Współistnienie złamań trzonu kości udowej i obrażeń stawu kolanowego – przypadek czy zależność? Nowiny Lekarskie. 2006;75:3–6. [Google Scholar]
- 41.Kotyla PJ, Rakoczy J, Lewicki M, Kucharz EJ. Teraźniejszość i przyszłość diagnostyki ultrasonograficznej narządu ruchu. Reumatologia. 2005;43:89–92. [Google Scholar]
- 42.Wasilczyk C. Rozprawa doktorska. Warszawa: CMKP; 2015. Wartość diagnostyki ultrasonograficznej uszkodzeń łąkotek stawu kolanowego weryfikowanych badaniem doświadczalnym i artroskopowym. [Google Scholar]
- 43.Donaldson WF, 3rd, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985;13:5–10. doi: 10.1177/036354658501300102. [DOI] [PubMed] [Google Scholar]
- 44.Dzianach M, Piontek T, Siwiński D, Owczarski T. Anterior cruciate ligament – sagittal popliteal view. A new sonographic ACL imaging method; 11th ESSKA 2000 Congress. 4th World Congress on Sports Trauma; May 5–8 2004; Athens, Greece: Abstracts & Presentations Hand Outs. [Google Scholar]