Abstract
Background
The use of bronchodilators in bronchiolitis lacks consensus. The efficacy of nebulised epinephrine versus salbutamol in bronchiolitis and the safety profile of the bronchodilators was studied.
Methods
Effects of nebulised epinephrine and salbutamol were compared in children with moderate to severe acute bronchiolitis. Thirty children between 2 to 24 months of age were recruited, 15 in each treatment group. Children received periodic (0,30,60 minutes followed by 4 hourly) doses of either 1:1000 laevo- epinephrine (0.5ml/kg subject to a maximum of 2.5ml with 3ml saline) or salbutamol (0.15mg/kg with 3ml saline) via nebuliser with oxygen. Changes in heart rate (HR), respiratory rate (RR), respiratory distress assessment instrument (RDAI), oxygen saturation (SpO2), oxygen requirement, duration of hospital stay and the side effects were studied.
Results
The respiratory status was better with significant improvement in RR, RDAI score and SpO2, decreased oxygen requirement and shorter hospital stay in the epinephrine group. There were no significant side effects in either group.
Conclusion
Nebulised epinephrine is a useful and safe drug for moderate/severe bronchiolitis and is superior to salbutamol.
Key Words: Bronchiolitis, Nebulised bronchodilators, Epinephrine, Salbutamol
Introduction
Acute viral bronchiolitis is one of the commonest lower respiratory tract infection in children less than 2 years of age. In the western countries, around 1% of healthy infants are hospitalised annually [1]. It is generally a self-limiting condition and is commonly associated with respiratory syncytial virus infection. It is characterised by bronchiolar obstruction due to oedema with or without spasm, with accumulation of mucus and cellular debris [2].
The treatment of infants with bronchiolitis has been supportive, with minimal handling of infant. Despite the proven role of bronchodilators in children below 2 years [3], its role in bronchiolitis is controversial [4]. The use of a combined α-adrenergic and β-adrenergic agonist, such as epinephrine was postulated to offer better benefit with its effect of reducing the mucosal oedema and achieving satisfactory bronchodilation [2]. Though several trials of bronchodilators in bronchiolitis have been reported including one from India, there have been varied results and conclusions [4]. Many studies used racemic epinephrine and reported short-term improvement, but condition of few patients worsened after they received epinephrine [5, 6, 7]. Only two studies looked into the usefulness with respect to hospital stay and the oxygen requirement in such children [8, 9].
We conducted a randomised study to examine the effect of readily available nebulised laevorotatory form of epinephrine versus salbutamol in hospitalised children with moderate to severe bronchiolitis with an aim to analyse the efficacy and side effects of these bronchodilators and to see whether there was anything more than a short term benefit as quoted in most studies.
Material and Methods
The study was conducted in children admitted with bronchiolitis to the paediatric ward of a zonal service hospital between Feb 2003 to Aug 2004. Children between 2 to 24 months of age and diagnosed as bronchiolitis based on the history of coryza and/or fever followed by respiratory distress were studied. Only children with moderately severe /severe bronchiolitis were included when there was respiratory distress with difficulty in feeding/nasal flare / chest retractions and hypoxia (SpO2< 94) requiring supplementary oxygen. These children underwent tests for blood urea, serum creatinine and electrolytes while blood culture was done in cases with fever >38.5°C.
Children with the history of similar episode of respiratory distress in the past, family history of atopy/asthma, history of prolonged respiratory distress in newborn period, those with any chronic cardiac/pulmonary illness and having received corticosteroids in any form in the preceding 72 hours were excluded. The children were randomly assigned to receive either nebulised 1:1000 dilution epinephrine (0.5ml/kg subject to a maximum of 2.5ml with 3ml saline) (Group 1) or salbutamol (0.15mg/kg with 3ml saline) (Group 2) via nebuliser along with oxygen for five minutes (apart from routine oxygen and intravenous fluids) at 0,30,60 minutes and then 4 hourly till child was stable with initiation of enteral feeds, normalisation of respiratory rates and oxygen saturation. Randomisation was done by simple random sampling with the prospective cases being allotted serial numbers in cards. The cards were shuffled and picked to enter Group I or Group II alternatively (Lottery method).
All the children were assessed in the beginning and after 10 minutes of nebulisation for the initial three nebulisations with special emphasis on heart rate (HR), respiratory rate (RR), respiratory distress assessment instrument (RDAI) score [10] and oxygen saturation by pulse oximetry (SpO2). A comparison between observations before and after intervention in the given groups and between the two groups was done. Data was recorded on a predetermined proforma and analysed using the Student's t-test.
Results
Thirty children in the age range of 2 to 24 months were included in the study with 15 in each group. The mean age and standard deviation (SD) of children was 6.67±3.01 months in Group 1 and 6.73± 2.95 months in Group 2. 66.7% of children in Group 1 and 60.0% in Group 2 were male. Only 20% of children in Group 1 and 26% in Group 2 were more than 12 months. The two groups were comparable with respect to their mean initial HR, RR, RDAI score and SpO2 (Table 1).
Table 1.
Initial mean and standard deviation (SD) of respiratory status in the two groups
| Mean ± SD | ||||
|---|---|---|---|---|
| HR/min | RR/min | RDAI score | SpO2% | |
| Group 1 | 161.71±14.38 | 85.14±7.43 | 12.92±0.99 | 88.86±2.66 |
| Group 2 | 160.29±12.86 | 84.14± 6.19 | 12.79±0.98 | 88.93±2.59 |
| t | 0.29 | 0.41 | 0.29 | 0.08 |
| p | Not significant | Not significant | Not significant | Not significant |
The trends of the various parameters through the initial three nebulisations (based on mean values at 0,10,40 and 70 minutes) in the two groups are as reflected in Fig 1, Fig 2, Fig 3, Fig 4. At the end of three nebulisations, the mean SD change in parameters in both groups are as given in Table 2. In Group 1, the post nebulisation mean heart rate increased by 10.27± 3.01, the mean respiratory rate decreased by 16.67± 3.17, the mean respiratory distress assessment score also decreased by 5.33± 0.72 and the mean SpO2 increased by 5.87± 1.71. In Group 2 there was a similar change after initial nebulisations with mean heart rate increasing by 8.93± 2.89, mean RR falling by 9.07± 1.91, mean RDAI falling by 3.93± 0.59 and mean SpO2 increasing by 4.2± 1.56. All the parameters in both the groups registered a statistically significant change (p<0.001).
Fig 1.
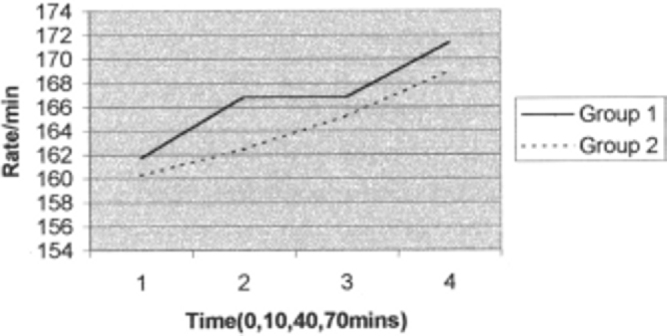
Trend of study parameter : Heart rate (HR)
Fig 2.
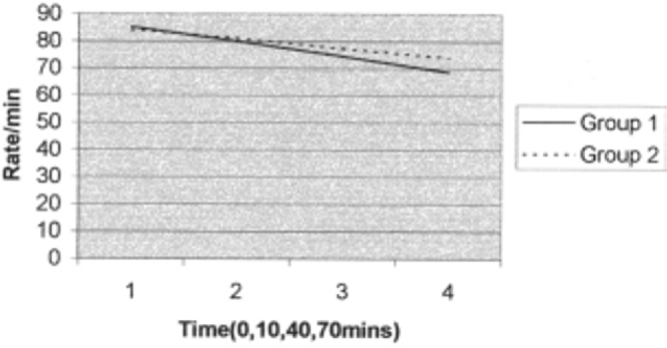
Trend of study parameter: Respiratory rate (RR)
Fig 3.

Trend of study parameter: Respiratory distress assessment instrument (RDAI)
Fig 4.

Trend of study parameter: Oxygen saturation by pulse oximetry (SpO2)
Table 2.
Changes in respiratory status parameters after initial three nebulisations in both groups
| Mean ± SD change in parameters | ||||
|---|---|---|---|---|
| HR/min | RR/min | RDAI score | SpO2% | |
| Group 1 | 10.27±3.01 | 16.67±3.17 | 5.33±0.72 | 5.87±1.71 |
| t = 13.15, p < 0.001 | t=20.32, p<0.001 | t=29.4,p<0.001 | t=13.30, p<0.001 | |
| Group 2 | 8.93±2.89 | 9.07±1.91 | 3.93±0.59 | 4.2±1.56 |
| t=12.06,p<0.001 | t=18.48,p<0.001 | t=26.2,p<0.001 | t=10.5,p<0.001 | |
| t | 1.26 | 8.09 | 5.83 | 2.81 |
| p | Not significant | <0.001 | <0.001 | <0.01 |
On analysis, there was no significant difference in the change of HR, but there was a significant difference in change in RR and RDAI favouring epinephrine group (p<0.001) and a significant difference in change in SpO2 favouring epinephrine group (p<0.01) (Table 2). The data on requirement of oxygen and time at which child was deemed fit for discharge is given in Table 3. The mean oxygen requirement was 54.71± 5.89 hours in Group 1 and 59.64± 5.92 hours in Group 2. The mean time at which the children were ready for discharge was 100.86± 6.74 hours in Group 1 and 107.07± 6.82 in Group 2. The oxygen requirement and hospital stay was significantly shorter (p<0.05 and <0.02 respectively) in epinephrine group. There were no significant side effects such as tachyarrythmia, irritability, tremors or facial blanching with either epinephrine or salbutamol initially or during subsequent nebulisations.
Table 3.
Oxygen requirement in the two groups
| Oxygen requirement (Hours) Mean ± SD | Time to readiness for Discharge (Hours) Mean ± SD | |
|---|---|---|
| Group 1 | 54.71±5.89 | 100.86±6.74 |
| Group 2 | 59.64±5.92 | 107.07±6.82 |
| t | 2.33 | 2.55 |
| p | <0.05 | <0.02 |
Discussion
Use of bronchodilators in bronchiolitis has been controversial [6]. A variety of agents ranging from parenteral epinephrine to nebulised racemic epinephrine, albuterol, salbutamol and routinely available laevo-epinephrine have been tried [11, 12, 13]. The interest in epinephrine has been significant owing to (i) the α-adrenergic vasoconstrictor action that can decongest the mucosa, limit its own absorption, besides regulating pulmonary blood flow, with little effect on ventilation–perfusion matching, (ii) β2- adrenergic bronchial muscle relaxant effect (iii) β-adrenergic action to suppress release of chemical mediators,(iv)physiological antihistamine effect that can reverse histamine effects, such as oedema and (v) reduction of catarrhal secretions [14, 15].
Over the last 15 years there have been 12 randomised control trials to evaluate the effect of salbutamol or albuterol on bronchiolitis, of which nine have shown that bronchodilators have no effect. Recently all the five randomised trials evaluating the effect of nebulised epinephrine on bronchiolitis have shown significant clinical improvement, with reductions in oxygen requirement, respiratory rate and wheeze after nebulised epinephrine [4]. The Indian study compared nebulised epinephrine and salbutamol in wheeze associated respiratory infection and found short-term beneficial effects of both and more so with epinephrine [16]. However this study used only three doses of 0.1ml/kg of 1:10000 epinephrine which is much less than the recommended useful dose for the same. Only few studies have considered long term outcomes such as hospital stay or oxygen requirement. Two of them showed lower hospital admission rates and reduced hospital stay with epinephrine [4].
Analysis of the results showed a significant improvement in respiratory status (RR, RDAI & SpO2) with better benefit in the epinephrine group. Unlike other studies [16, 17], this study did not see any significant difference in increase in HR in the two groups while there was a significant short term rise in HR in both groups after the initial nebulisation. There were no side effects of the bronchodilators, which was similar to other studies, including those that did not find any benefit with the bronchodilators [16, 18, 19]. In this study the oxygen requirement and time at which the children were deemed fit for discharge, was significantly shorter in the epinephrine group. These findings are at variance with a recent multicentric trial which points to a lack of benefit, in either short-term or long-term clinically relevant outcomes, of nebulised epinephrine in infants hospitalised with acute bronchiolitis [9]. However, the study used only 3 doses of nebulised epinephrine at 4 hourly intervals, which might have been insufficient to study the response, especially for the long-term outcomes. The study mentions of a possibility of increased oxygen consumption with epinephrine, based on the finding that amongst infants requiring supplemental oxygen and intravenous fluids, the time until the infant was ready for discharge was significantly longer in the epinephrine group than in the placebo group. This does not explain their findings in infants in whom only oxygen was required (without intravenous fluids), wherein the epinephrine group consumed lesser oxygen than the placebo group. They also had more infants with moderately severe illness assigned to epinephrine than to placebo group which could have affected their results.
Cochrane analysis describes insufficient evidence to support the use of epinephrine for the treatment of bronchiolitis among inpatients while there was some evidence to suggest that epinephrine may be favourable to salbutamol and placebo among outpatients [20]. The lack of consensus on usefulness of bronchodilators in bronchiolitis especially epinephrine is surprising when we consider the fact that approximately 68-96% of infants with bronchiolitis at tertiary paediatric centres in Canada are treated with bronchodilators [21, 22]. In a European survey of 88 paediatric centres, 54 centres reported using bronchodilators in all patients with bronchiolitis and 15 centres reported using bronchodilators only in high-risk patients [23]. 88% paediatricians used bronchodilators in infants with bronchiolitis in an Australian survey [24].
The drawbacks of the present study include small sample size, absence of a control group and possibility of at least some children in the study presenting with respiratory distress due to first episode of bronchial asthma rather than bronchiolitis. In conclusion, while it can be inferred that nebulised epinephrine and salbutamol are safe and useful in bronchiolitis, with epinephrine comparing better than salbutamol in both short term benefit in relieving respiratory distress and long term outcomes like reduced oxygen requirement and time to discharge, there is a need for large multicentric studies to confirm our results.
Conflicts of Interest
None identified
References
- 1.Glezen WP, Denny FW. Epidemiology of acute lower respiratory disease in children. N Engl J Med. 1973;288:498–505. doi: 10.1056/NEJM197303082881005. [DOI] [PubMed] [Google Scholar]
- 2.Wohl ME, Chernick V. State of the art: bronchiolitis. Am Rev Respir Dis. 1978;118:759–781. doi: 10.1164/arrd.1978.118.4.759. [DOI] [PubMed] [Google Scholar]
- 3.Soto ME, Sly PD, Uren E, Taussig LM, Landau LI. Bronchodilator response during acute viral bronchiolitis in infancy. Pediatr Pulmonol. 1985;1:85–90. doi: 10.1002/ppul.1950010206. [DOI] [PubMed] [Google Scholar]
- 4.Margrid Schindler. Do bronchodilators have an effect on bronchiolitis? Critical Care. 2002;6:111–112. doi: 10.1186/cc1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanchez I, De Coster J, Powell RE, Wolstein R, Chernick V. Effect of racemic epinephrine and salbutamol on clinical score and pulmonary mechanics in infants with bronchiolitis. J Pediatr. 1993;122:145–151. doi: 10.1016/s0022-3476(05)83508-5. [DOI] [PubMed] [Google Scholar]
- 6.Rusconi F, Sideri S. Efficacy of epinephrine and salbutamol in treatment of acute bronchiolitis. J Pediatr. 1996;128:441–443. doi: 10.1016/s0022-3476(96)70312-8. [DOI] [PubMed] [Google Scholar]
- 7.Numa AH, Williams GD, Dakin CJ. The effects of nebulised epinephrine on respiratory mechanics and gas exchange in bronchiolitis. Am J Respir Crit Care Med. 2001;164:86–91. doi: 10.1164/ajrccm.164.1.2008090. [DOI] [PubMed] [Google Scholar]
- 8.Bertrand P, Aranibar H, Castro E, Sanchez I. Efficacy of nebulised epinephrine versus salbutamol in hospitalized infants with bronchiolitis. Pediatr Pulmonol. 2001;31:284–288. doi: 10.1002/ppul.1040. [DOI] [PubMed] [Google Scholar]
- 9.Wainwright C, Altamirano L, Marise Cheney M. A multicentre, randomised, double-blind, controlled trial of nebulised epinephrine in infants with acute bronchiolitis. N Engl J Med. 2003;349:27–35. doi: 10.1056/NEJMoa022226. [DOI] [PubMed] [Google Scholar]
- 10.Lowell DI, Lister G, Von Koss H, McCarthy P. Wheezing in infants: The response to epinephrine. Paediatrics. 1987;79:939–945. [PubMed] [Google Scholar]
- 11.Klassen TP, Rowe CP, Sutcliffe T, Roop LJ, Mcdowell IW, Li MM. Randomised trial of salbutamol in acute bronchiolitis. J Pediatr. 1991;118:807–811. doi: 10.1016/s0022-3476(05)80051-4. [DOI] [PubMed] [Google Scholar]
- 12.Lenney W, Milner AD. Alpha and beta-adrenergic stimulants in bronchiolitis and wheezy bronchitis in children under 18 months of age. Arch Dis Child. 1978;53:707–709. doi: 10.1136/adc.53.9.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gadomski AM, Lichenstein R, Horton L, King J, Keane V, Permutt T. Efficiency of albuterol in the management of bronchiolitis. Paediatrics. 1994;93:907–912. [PubMed] [Google Scholar]
- 14.Katzung BG. Basic & clinical pharmacology. 7th ed. Appleton & Lange; Stamford: 1998. [Google Scholar]
- 15.Barr FE, Patel NR, Newth CJ. The pharmacologic mechanism by which inhaled epinephrine reduces airway obstruction in respiratory syncytial virus-associated bronchiolitis. J Pediatr. 2000;136:699–700. doi: 10.1067/mpd.2000.105358. [DOI] [PubMed] [Google Scholar]
- 16.Ray MS, Singh V. Comparison of nebulised adrenaline versus salbutamol in wheeze associated respiratory infection in infants. Indian Pediatr. 2002;39:12–22. [PubMed] [Google Scholar]
- 17.Menon K, Sutcliffe T, Klassen T. A randomised trial comparing the efficacy of epinephrine with salbutamol in the treatment of acute bronchiolitis. J Pediatr. 1995;126:1004–1007. doi: 10.1016/s0022-3476(95)70234-2. [DOI] [PubMed] [Google Scholar]
- 18.Abul-Ainine A, Luyt D. Short term benefits of adrenaline in bronchiolitis: a randomised controlled trial. Arch Dis Child. 2002;86:276–279. doi: 10.1136/adc.86.4.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kristjansson S, Carlsen K, Wennergren G. Nebulised racemic adrenaline in the treatment of acute bronchiolitis in infants and toddlers. Arch Dis Child. 1993;69:650–654. doi: 10.1136/adc.69.6.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartling L, Wiebe N, Russell K, Patel H, Klassen TP. The Cochrane Library. John Wiley & Sons; Chichester, UK: 2004. Epinephrine for bronchiolitis (Cochrane Review) Issue 3. [DOI] [PubMed] [Google Scholar]
- 21.Wang EE, Law BJ, Boucher FD. Paediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study of admission and management variation in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr. 1996;129:390–395. doi: 10.1016/s0022-3476(96)70071-9. [DOI] [PubMed] [Google Scholar]
- 22.Law BJ, De Carvalho V. Respiratory syncytial virus infections in hospitalised Canadian children: regional differences in patient populations and management practices. Pediatr Infect Dis J. 1993;12:659–663. [PubMed] [Google Scholar]
- 23.Kimpen JL, Schaad UB. Treatment of respiratory syncytial virus bronchiolitis:1995 poll of members of the European Society for Paediatric Infectious Diseases. Pediatr Infect Dis J. 1997;16:479–481. doi: 10.1097/00006454-199705000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Barben JU, Robertson CF, Robinson PJ. Implementation of evidence-based management of acute bronchiolitis. J Paediatr Child Health. 2000;36:491–497. doi: 10.1046/j.1440-1754.2000.00558.x. [DOI] [PubMed] [Google Scholar]


