Abstract
Objective
To determine associations between need, enabling, and predisposing factors with mental health service use among National Guard soldiers in the first year following a combat deployment to Iraq or Afghanistan.
Data Sources/Study Setting
Primary data were collected between 2011 and 2013 from 1,426 Guard soldiers representing 36 units.
Study Design
Associations between Guard soldier factors and any mental health service use were assessed using multivariable logistic regression models in a cross‐sectional study. Further analysis among service users (N = 405) assessed VA treatment versus treatment in other settings.
Principal Findings
Fifty‐six percent of Guard soldiers meeting cutoffs on symptom scales received mental health services with 81 percent of those reporting care from the VA. Mental health service use was associated with need (mental health screens and physical health) and residing in micropolitan communities. Among service users, predisposing factors (middle age range and female gender) and enabling factors (employment, income above $50,000, and private insurance) were associated with greater non‐VA services use.
Conclusion
Overall service use was strongly associated with need, whereas sector of use (non‐VA vs. VA) was insignificantly associated with need but strongly associated with enabling factors. These findings have implications for the recent extension of veteran health coverage to non‐VA providers.
Keywords: Mental health, VA health care system, access, utilization of services
National Guard soldiers activated for Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) are eligible for 5 years of free health care through the Department of Veterans Affairs (VA) health care system after their deployment. Comprehensive benefits and the unique expertise of VA clinicians in addressing many mental health consequences of deployments make the VA a key health care resource for Guard soldiers when they return. Among OIF and OEF veterans who entered and used the VA health care system between 2002 and 2008, 41 percent were Guard or Reserve veterans (Seal et al. 2009). This is not surprising given they represent one‐third of all soldiers deployed to Iraq and Afghanistan (IOM 2013). Moreover, Guard and Reserve soldiers may be more dependent upon treatment from the VA and community providers compared to their active‐duty counterparts who are able to access services at military treatment facilities.
Mental health has been a focal health concern among returning OEF/OIF Veterans, and it may be even more salient for those in the Guard. One‐fourth of the OEF/OIF veterans receiving medical care in the VA also had a mental health diagnosis (Seal et al. 2007) or PTSD (Sayer et al. 2010). Moreover, studies have suggested that Guard soldiers are at increased risk for PTSD and depression compared with their active‐duty counterparts (Thomas et al. 2010; Hyman et al. 2012; Valenstein et al. 2014). Prior research has also found that those with PTSD have high levels of comorbid major depressive disorder and alcohol‐use disorder (Erbes et al. 2011; Gorman et al. 2011) and increased risk for suicide (Hyman et al. 2012). Accessing treatment when a need is indicated is a critical health issue. The extent to which Guard soldiers with need access services is an area of active investigation. In two prior samples of Guard soldiers with identified mental health conditions, only 37 percent (Goodwin et al. 2014) and 50 percent (Gorman et al. 2011) had sought any type of treatment.
Given the high level of need of returning veterans and possible barriers to care, it is important to understand factors associated with mental health service utilization among the National Guard to ensure that both VA and community systems are equipped to treat those with an identified need. This study examines mental health service use among Guard soldiers who deployed to Iraq or Afghanistan. It also estimates associations between factors of interest and VA versus non‐VA service use among those who used services. The Behavioral Model of Healthcare Utilization (Andersen 1995; Andersen and Davidson 2013; see Figure 1) is the theoretical framework underlying the choice of need, predisposing, and enabling factors related to mental health use and VA versus non‐VA mental health utilization.
Figure 1.
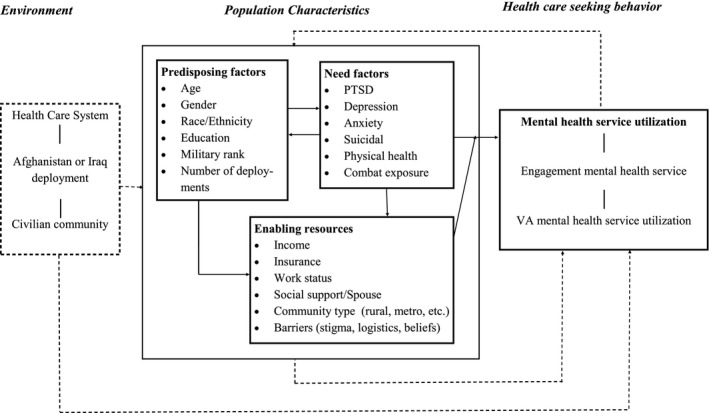
Conceptual Framework of Factors Associated with Mental Health Services Utilization
Mental Health Need
Traumatic events and exposure to combat increase risk for psychiatric disorders postdeployment (Hoge et al. 2004; Renshaw, Rodrigues, and Jones 2009). Combat exposure is associated with mental health disorders and service members' perceived need for treatment (Sareen et al. 2007, 2010). Need factors, such as symptom severity, are robust predictors of mental health service utilization in many populations (Fasoli, Glickman, and Eisen 2010), including Iraq and Afghanistan veterans who accessed VA mental health care between 2005 and 2009 (Hoerster 2012). Sayer et al. (2010) found that veterans with probable PTSD were more likely to struggle with reintegration problems and expressed interest in more kinds of services than veterans without probable PTSD. Further, a comorbid diagnosis versus an isolated PTSD diagnosis was associated with a greater likelihood of at least one follow‐up VA mental health visit in the first year following diagnosis (Seal et al. 2010). Elbogen et al. (2013) also found that veterans with the greatest mental health need were more likely to access services. We anticipated that need as defined by higher levels of symptoms and greater comorbidity would drive overall utilization in a sample of Guard soldiers. We also hypothesized that use of the VA system, which is free within 1 year of return, would be more heavily used by Guard soldiers with higher levels of symptoms and greater comorbidity. We expected Guard soldiers with greater levels of symptoms would preferentially access mental health services within the VA, given system expertise in addressing combat‐related sequalae.
Predisposing Factors
Demographic factors such as age, race, gender, cultural norms, and previous deployment/reintegration experiences may also predict service use. The literature suggests that OEF/OIF veterans who were older and female were more likely to utilize mental health services (Fasoli, Glickman, and Eisen 2010; Seal et al. 2010). Women were more likely than men to use non‐VA services (Elbogen et al. 2013), even though other studies reported a negligible gender difference in attitudes about VA care and perceived fit in the VA (Fox, Meyer, and Vogt 2015). When looking at race and ethnicity in a sample of Guard soldiers with mental health need, only black race predicted treatment use (Goodwin et al. 2014).
Enabling Factors
Enabling factors also impact service utilization. Prior to OEF and OIF, factors associated with VA rather than non‐VA service utilization for primary care included lower income and education attainment, lack of health insurance, and greater burden of illness (Borowsky and Cowper 1999). Veterans with insurance and more education were less likely to rely exclusively on the VA for health services (Borowsky and Cowper 1999; Liu et al. 2008). Hamilton et al. (2013) looked at attrition from VA health care use and found that those who left the VA were more likely to have moved farther away from the VA and have alternate health insurance. Seal et al. (2010) reported that a diagnosis from a non–mental health clinic and living greater than 50 miles from a VA facility were associated with not having at least one follow‐up treatment visit in the first year following a PTSD diagnosis.
In contrast to factors that enable treatment‐seeking behavior, the literature suggests that factors such as stigma may be a cultural barrier to treatment (Gorman et al. 2011; Elbogen et al. 2013). Gorman et al. (2011) found that 45 percent of Guard soldiers with a mental health condition did not want mental health treatment to appear on their military records. This barrier to service utilization remains among Guard soldiers who are students despite identified need (Bonar et al. 2015). While a recent study of this population indicated a reduction of stigma and beliefs barriers regarding mental health treatment (Valenstein et al. 2014), it still remains uncertain whether distance to treatment, scheduling, and other logistical barriers are being addressed or if they contribute to differential use of VA and non‐VA care.
Studies have also looked at social support and unit support as enabling factors (Sripada et al. 2015). While there is a great deal of evidence suggesting a link between social support and lower likelihood of mental health conditions (Sripada et al. 2015), the evidence that social support increases the likelihood that Guard soldiers will access mental health treatment is less robust. However, these enabling factors should be investigated among Guard soldiers as potential contributors to VA and non‐VA mental health service use.
Objective
The Behavioral Model of Healthcare Utilization (Andersen 1995) was the theoretical framework guiding the study. Our primary aim was to understand the factors associated with mental health service use and the type of service use (VA and non‐VA) among returning National Guard soldiers. Others have examined various components of this model, including Elnitsky et al. (2013), who looked at stigma and barriers to exclusive VA use. Meis et al. (2010) also studied PTSD symptom severity and relationship distress as predictors of use. The present study aims to complement the work of others (Meis et al. 2010; Elnitsky et al. 2013) and inform further development of the model by exploring in‐depth the National Guard community and cultural determinants that influence mental health treatment utilization. To explore cultural factors, we incorporated stigma, distance to treatment and other logistic barriers, military rank, and combat exposure into the model. Further, we explored potential enabling factors that might increase the soldier's access or ability to navigate complicated systems of care. Figure 1 illustrates the “adapted” model and the relationship between need, enabling and predisposing factors, and the use of mental health services. The variables used in the present study are represented in Figure 1.
Methods
Participants and Procedures
Survey participants were National Guard soldiers representing 36 units that deployed to Iraq or Afghanistan from a Midwestern state. Data were collected between August 2011 and December 2013, approximately 12 months following their return. Surveys were collected in person during monthly drill weekends. Soldiers not at drill weekends were mailed surveys via USPS, with follow‐up surveys being sent two additional times to nonrespondents. This is a slightly modified version of the Dillman method used to ensure those who had separated from the unit were not excluded from participation (Dillman, Smyth, and Melani 2010). Institutional Review Board approval was obtained through the Department of Veterans Affairs Ann Arbor Health System, and the protocol was reviewed and endorsed by the Army National Guard Office of the Chief Surgeon. Data were collected under an approved waiver of written informed consent. For further details of the study design, see Valenstein et al. (2014).
Measures
The outcome of interest was mental health service utilization in the past year, which was assessed from 10 items asking participants to indicate if they “had received mental health services for a stress, emotional, alcohol, or family problem” from non‐VA and VA settings. Affirmative responses were used to create categorical variables for any mental health treatment in the past year (yes/no) and type of mental health treatment (any VA mental health treatment, non‐VA mental health treatment only). Response options for VA mental health services use included a VA hospital, community‐based outpatient center (CBOC), and any Vet Center use. Response options for non‐VA mental health services use included general medical doctor or mental health professional at a civilian facility. For patients who used services in both VA and non‐VA sectors, we constructed a hierarchy of use. If soldiers received mental health care in both specialty and primary care settings, they were assigned to the sector in which they received specialty mental health services. Soldiers who only received primary care mental health services or only received specialty mental health services in both sectors were considered to have received VA treatment.
Needs Factors as Primary Predictors
We assessed soldier need for mental health services using validated measures for PTSD, depression, anxiety, and suicide risk. PTSD symptoms were measured using the Posttraumatic Stress Disorder Checklist‐Specific Version (PCL‐S), a self‐report measure of the 17 DSM‐IV PTSD symptoms (Weathers et al. 1993). Soldiers were considered to have significant PTSD symptoms if PCL‐S scores were ≥50. The presence or absence of significant depressive symptoms was assessed with the Patient Health Questionnaire (PHQ‐9) (Kroenke, Spitzer, and Williams 2001). The PHQ‐9 assesses nine DSM‐IV symptoms of depression over a 2‐week period and has a sensitivity of 88 percent and a specificity of 88 percent for major depression (Löwe et al. 2004). Soldiers were considered to have significant depressive symptoms if their PHQ‐9 scores were ≥10. Anxiety was assessed using the GAD‐7 (Spitzer et al. 2006), a brief measure for assessing generalized anxiety disorder with a sensitivity of 89 percent and a specificity of 82 percent (Spitzer et al. 2006). Scores ≥10 were used to indicate presence of anxiety.
To assess the number of mental health conditions, an ordinal variable was created for participants who met the cutoff criteria for PTSD, depression, or anxiety, as described above. Number of probable mental health conditions could be zero, one, two, or three.
The SF‐12 was used to assess mental and physical functioning and overall health‐related quality of life. The 12‐item measure is an abbreviated version of the SF‐36 Health Survey (Ware, Kosinski, and Keller 1996). Physical and mental health composite scores were computed and ranged from 0 to 100, where a zero score indicates the lowest and 100 indicates the highest level of health measured by the scale.
Combat exposure was considered a need factor. A soldier was considered to have combat exposure if they affirmed any of the following Post‐Deployment Health Assessment questions included in the study survey and pertaining to any of their deployments: “Did you encounter dead bodies or see people killed or wounded during deployment?” “Were you engaged in direct combat where you discharged a weapon?” or “Did you ever feel that you were in great danger of being killed?”
Predisposing Factors
Predisposing factors include individual‐level items such as demographics as well as contextual factors. Demographic variables include age group, gender, race/ethnicity, education, military rank, and number of deployments self‐reported by service members. Response options for race and ethnicity categories included African American, Asian and Native American, White, multiethnic, and Hispanic ethnicity. Ranks were grouped together with item responses for E1–E4 as junior enlisted and Ranks E5–E9 as noncommissioned officers (NCO). Warrant officers (WO1‐5) were included in the officer group for study analyses. Number of deployments was classified as one or more than one.
Enabling Factors
Income, insurance status, location, and work status were considered enabling factors that make it easier to access mental health treatment. Committed relationship status was considered a source of social support (Cutrona 1996; Laffaye et al. 2008; Kuwert, Knaevelsrud, and Pietrzak 2014). Insurance was assessed using a “check all that applies” option to the question, “What kind of health insurance or health care coverage do you have?” Nine options were available, including options for Medicaid, VA Healthcare System, no coverage of any type, and “I don't know what type of coverage I have.” Only a positive response to private health insurance, employer‐sponsored insurance, or military health care such as TRICARE was coded as “yes” for an indicator of private health insurance. Work status responses were grouped into three categories: employed, unemployed, and out of the workforce. Employed status includes the responses “working part‐time” and “working full‐time.” Unemployed status is denoted by the responses “unemployed, looking for work” and “unemployed, not looking for work.” Out of the work force includes responses such as “retired,” “student,” and “homemaker.”
Distance to the nearest VA facility was calculated using geographic coordinates from the respondent's zip code and the address of the nearest VA treatment facility. A variable for community type to assess accessibility of non‐VA mental health services was calculated with zip codes and categorized into three types based on population: metropolitan (greater than 50,000), micropolitan (10,000–50,000), and small town or rural (less than 10,000) (Office of Management and Budget 2013). These communities of residence may reflect the availability of non‐VA mental health services.
Barriers were assessed using an adaptation of the Perceived Stigma and Barriers to Care for Psychological Problems (Britt 2000; Hoge et al. 2004; Gorman et al. 2011; Vogt 2011). For this study, barriers were operationalized as follows: a 7‐item stigma factor, which included concerns that mental health treatment would be too embarrassing, harm one's career, affect perceptions of one's unit members, affect perceptions of one's leaders, cause one to be seen as weak, and appear on military records; a 7‐item logistics factor that included not knowing where to get help, inadequate transportation, difficulty scheduling or getting time off work, cost, and long distance to treatment; and a 2‐item beliefs factor that included not trusting mental health professionals and not believing that mental health care works (Valenstein et al. 2014). Soldiers were considered to have endorsed the barrier category if they agreed or strongly agreed with any of the items that comprised the categories as used in prior studies (Wright et al. 2009; Kehle et al. 2010; Valenstein et al. 2014).
Data Analysis
All of the analyses for this study were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Descriptive analyses were completed for the study sample, using means or frequencies as indicated. Bivariate analyses were completed using chi‐square tests to compare the utilization and type of mental health services by soldier demographics, need, enabling, and predisposing factors. Beyond basic demographics, factors that were not associated with mental health service use in bivariate analyses were excluded from regression analysis. Logistic regression models were used to calculate adjusted odds ratios (ORs) with 95 percent confidence intervals (CIs) for the receipt of mental health treatment and receipt of VA versus non‐VA treatment among mental health services users. To test study hypotheses, regression analyses were performed with mental health services use as the outcome and predictors entered into models in blocks, separately examining predisposing factors, need factors, and enabling factors, and then all factors were combined in a single model.
Results
The characteristics of the 1,426 subjects recruited for the study are shown in Table 1. Fifty‐two percent were age 30 or younger. A majority of participants were male, white, and had at least some college education. Thirty‐one percent had incomes of $25,000 or less. Nearly three‐fourths had five or more years of service in the National Guard and 69 percent reported combat exposure. One year following their deployment, participants were experiencing significant symptoms of PTSD (17 percent), depression (21 percent), and anxiety (16 percent) with 10 percent reporting suicidal risk. Of the 1,426 subjects in the study, 405 (28 percent) had received mental health services in the prior 12 months from the VA, community provider, or combination of the two. Approximately 56 percent of those who met the cutoff criteria for PTSD, MDD, or GAD at 12 months postdeployment used any mental health services.
Table 1.
Characteristics of Sample Overall and by Use of Mental Health Treatment in the Last Year
| Overall Sample (N = 1,426) | Any MH Treatment (N = 405) | No MH Treatment (N = 1,021) | χ2/Z | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Predisposing factors | |||||||
| Age (years) | |||||||
| 18–30 | 738 | 52 | 179 | 44 | 559 | 55 | 13.5** |
| 31–40 | 342 | 24 | 110 | 27 | 232 | 23 | |
| Over 40 | 340 | 24 | 115 | 28 | 225 | 22 | |
| Gender | |||||||
| Male | 1,306 | 92 | 369 | 91 | 937 | 92 | .27 |
| Female | 118 | 8 | 36 | 9 | 82 | 8 | |
| Race/ethnicity | |||||||
| White | 1,177 | 83 | 316 | 78 | 861 | 85 | 9.2** |
| Non‐white | 241 | 17 | 88 | 22 | 153 | 15 | |
| Education | |||||||
| High school/GED | 376 | 26 | 106 | 26 | 270 | 27 | .05 |
| Some college/Associates | 804 | 57 | 230 | 57 | 574 | 56 | |
| Bachelor or higher degree | 240 | 17 | 67 | 17 | 173 | 17 | |
| Military rank | |||||||
| Junior enlisted | 641 | 45 | 163 | 40 | 478 | 47 | 6.0* |
| Noncommissioned (NCO) | 643 | 45 | 203 | 50 | 440 | 43 | |
| Officer | 141 | 10 | 39 | 10 | 102 | 10 | |
| Number of deployments | |||||||
| 1 | 689 | 50 | 164 | 42 | 525 | 53 | 15.6*** |
| More than 1 | 688 | 50 | 230 | 58 | 458 | 47 | |
| Need factors | |||||||
| Number of mental health conditions (PTSD, depression, anxiety, suicidality) | |||||||
| 0 | 1,023 | 72 | 180 | 44 | 843 | 83 | 228.7*** |
| 1 | 177 | 12 | 82 | 20 | 95 | 9 | |
| 2 | 104 | 7 | 57 | 14 | 47 | 5 | |
| 3 | 122 | 9 | 86 | 21 | 36 | 4 | |
| Physical health SF‐12 score (mean ± SD) | 50.4 ± 9.0 | 46.9 ± 10.4 | 51.7 ± 8.0 | −8.3*** | |||
| Combat exposure | 949 | 69 | 313 | 80 | 636 | 64 | 32.1*** |
| Enabling factors | |||||||
| Income | |||||||
| $25,000 or less | 437 | 31 | 118 | 29 | 319 | 31 | 1.0 |
| $25,001–$50,000 | 491 | 35 | 147 | 36 | 344 | 34 | |
| Greater than $50,000 | 491 | 35 | 139 | 34 | 352 | 35 | |
| Insurance | |||||||
| Private health insurance | 966 | 68 | 267 | 66 | 699 | 68 | .9 |
| Work status | |||||||
| Unemployed | 215 | 15 | 66 | 16 | 149 | 15 | .68 |
| Employed | 1,049 | 74 | 295 | 73 | 754 | 74 | |
| Out of the workforce | 157 | 11 | 43 | 11 | 114 | 11 | |
| Marital status | |||||||
| In committed relationship | 880 | 62 | 258 | 64 | 622 | 61 | .83 |
| Barriers | |||||||
| Stigma | 412 | 29 | 167 | 42 | 245 | 24 | 43.9*** |
| Logistics | 437 | 31 | 177 | 44 | 260 | 26 | 46.8*** |
| Beliefs | 191 | 14 | 57 | 14 | 134 | 13 | .27 |
| Distance to VA in miles (mean ± SD) | 17.8 ± 13.3 | 18.8 ± 14.4 | 17.4 ± 12.8 | .83 | |||
| RUCA codes | |||||||
| Metropolitan | 991 | 70 | 271 | 68 | 720 | 71 | 8.39* |
| Micropolitan | 204 | 14 | 75 | 19 | 129 | 13 | |
| Small town/rural | 215 | 15 | 55 | 14 | 160 | 16 | |
*p < .05, **p < .01, ***p < .001.
Bivariate Descriptive Analysis
Chi‐square tests of independence were performed to examine the unadjusted relationship between any mental health treatment and characteristics of the overall sample. As reported in Table 1, the associations between any mental health use and age, race, military rank, and number of deployments were significant. Any mental health use was associated with need variables, including number of mental health conditions, combat exposure, and poorer physical health. Stigma associated with accessing mental health treatment in the military culture, logistics barriers, and community of residence was inversely associated with accessing any mental health treatment. Among the 405 survey respondents reporting mental health treatment in the prior 12 months, 327 (81 percent) received any VA treatment and 78 (19 percent) received only non‐VA treatment. Though not the focus of this study, it should be noted that approximately 30 percent of those receiving VA treatment had also received treatment from a non‐VA source. Of those with any VA mental health treatment, 73 percent received care from a mental health professional versus primary care. Of those with non‐VA treatment only, 42 percent received care from a mental health professional. The characteristics of the 405 veterans who reported mental health treatment are given in Table 2 along with the chi‐square tests of independence examining the unadjusted relationship between the location of mental health treatment and sample characteristics. The relationships between any VA mental health service use and gender, number of mental health conditions, as well as enabling factors like income, work, and insurance status, were significant.
Table 2.
Characteristics of Soldiers Who Used Any VA Treatment in the Last Year, among Those with Any Mental Health Service Use (N = 405)
| Any VA MH Treatment (N = 327) | Non‐VA MH Treatment only (N = 78) | χ2/Z | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Predisposing factors | |||||
| Age (years) | |||||
| 18–30 | 140 | 43 | 39 | 50 | 5.5 |
| 31–40 | 97 | 30 | 13 | 17 | |
| Over 40 | 89 | 27 | 26 | 33 | |
| Gender | |||||
| Male | 303 | 93 | 66 | 93 | 5.0* |
| Female | 24 | 7 | 12 | 7 | |
| Race/ethnicity | |||||
| White | 252 | 77 | 64 | 82 | .83 |
| Non‐white | 74 | 23 | 14 | 18 | |
| Education | |||||
| High school/GED | 90 | 28 | 16 | 21 | 4.8 |
| Some college/associates | 187 | 58 | 43 | 55 | |
| Bachelor or higher degree | 48 | 15 | 19 | 24 | |
| Military rank | |||||
| Junior enlisted | 133 | 41 | 30 | 38 | 5.6 |
| Noncommissioned (NCO) | 168 | 51 | 35 | 45 | |
| Officer | 26 | 8 | 13 | 17 | |
| Number of deployments | |||||
| 1 | 125 | 39 | 39 | 51 | 3.6 |
| More than 1 | 193 | 61 | 37 | 49 | |
| Need factors | |||||
| Number of mental health conditions PTSD, depression, anxiety | |||||
| 0 | 131 | 40 | 49 | 63 | 14.7** |
| 1 | 68 | 21 | 14 | 18 | |
| 2 | 51 | 16 | 6 | 8 | |
| 3 | 77 | 24 | 9 | 12 | |
| Physical health SF‐12 score (mean ± SD) | 46.5 ± 10.3 | 48.3 ± 10.8 | 1.8 | ||
| Combat exposure | 257 | 81 | 56 | 75 | 1.7 |
| Enabling factors | |||||
| Income | |||||
| $25,000 or less | 103 | 32 | 15 | 19 | 8.3* |
| $25,001–$50,000 | 121 | 37 | 26 | 33 | |
| Greater than $50,000 | 102 | 31 | 37 | 47 | |
| Insurance (private health insurance) | 200 | 61 | 67 | 86 | 17.2*** |
| Work status | |||||
| Unemployed | 61 | 19 | 5 | 6 | 9.3** |
| Employed | 235 | 72 | 60 | 77 | |
| Out of the workforce | 30 | 9 | 13 | 17 | |
| Marital status | |||||
| In committed relationship | 203 | 62 | 55 | 71 | 1.9 |
| Barriers | |||||
| Any stigma | 141 | 44 | 26 | 14 | 2.7 |
| Logistics | 147 | 46 | 30 | 39 | 1.1 |
| Beliefs | 48 | 15 | 9 | 12 | .53 |
| Distance to VA (mean ± SD) | 19.1 ± 14.6 | 17.5 ± 13.5 | −.68 | ||
| RUCA codes | |||||
| Metropolitan | 213 | 66 | 58 | 74 | 2.5 |
| Micropolitan | 65 | 20 | 10 | 13 | |
| Small town/rural | 45 | 14 | 10 | 13 | |
*p < .05, **p < .01, ***p < .001.
Multivariable Analysis
Separate logistic regression analyses were performed to assess prediction of any mental health treatment with need, enabling, and predisposing factors. Predictors with significant associations in bivariate analyses were included in the models. The first model explored predisposing factors only; the second model explored need factors; and the third model explored enabling factors. The final model estimating mental health treatment included all variables in the earlier models. Table 3 shows the results of the logistic regression models predicting any mental health use. In model 1, age, race, and having more than one deployment were associated with any mental health treatment but not after controlling for all the other covariates in the full model. In model 2, the need factors of combat exposure and physical health were associated with any mental health treatment. Soldiers who met the cutoff criteria for a mental health condition were more likely than those who did not to access any treatment. Those who met the criteria for three conditions were more likely than those with one condition to seek any treatment. Soldiers that endorsed stigma and logistical barriers were more likely to receive any mental health treatment in model 3 using the full cohort, but not after controlling for all the other covariates. When all factors were considered in final model, only needs factors and living in a micropolitan area remained significant predictors of any mental health services use. Seeking any mental health treatment was related to an increase in the number of mental health conditions, worse physical health functioning, and living in a micropolitan community.
Table 3.
Multivariable Logistic Regression Models Estimating Receipt of Any Mental Health Treatment in the Past Year (N = 1,426)
| Model 1: Predisposing Factors (N = 1,365) | Model 2: Need Factors (N = 1,298) | Model 3: Enabling Factors (N = 1,384) | Model 4: All Factors (N = 1,267) | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age (years) | ||||
| 31–40 versus 18–30 | 1.37 (0.98, 1.91) | 1.25 (0.86, 1.82) | 1.36 (0.98, 1.90) | 1.14 (0.78, 1.69) |
| Over 40 versus 18–30 | 1.43 (1.01, 2.04)* | 1.25 (0.84, 1.87) | 1.52 (1.07, 2.17)* | 1.15 (0.76, 1.74) |
| Gender | ||||
| Male versus female | 0.75 (0.49, 1.16) | 0.69 (0.42, 1.13) | 0.82 (0.53, 1.27) | 0.69 (0.42, 1.14) |
| Non‐white | 1.58 (1.17, 2.15)** | 1.31 (0.93, 1.86) | 1.66 (1.22, 2.27)** | 1.41 (0.99, 2.02) |
| Rank | ||||
| NCO versus enlisted | 0.88 (0.63, 1.21) | 1.01 (0.71, 1.43) | 1.08 (0.79, 1.47) | 0.93 (0.63, 1.35) |
| Officers versus enlisted | 0.75 (0.47, 1.19) | 1.44 (0.87, 2.39) | 0.95 (0.59, 1.51) | 1.35 (0.80, 2.28) |
| Deployments | ||||
| More than 1 versus 1 | 1.53 (1.15, 2.05)** | 1.28 (0.91, 1.82) | ||
| Mental health condition | ||||
| 0 versus 1 | 0.28 (0.19, 0.40)*** | 0.30 (0.21, 0.44)*** | ||
| 2 versus 1 | 1.53 (0. 90, 2.58) | 1.37 (0.80, 2.34) | ||
| 3 versus 1 | 2.33 (1.37, 3.97)** | 2.19 (1.26, 3.81)** | ||
| SF‐12 | ||||
| Physical health scale | 0.97 (0.95, 0.98)*** | 0.96 (0.95, 0.98)*** | ||
| Combat exposure | ||||
| Yes versus No | 1.62 (1.17, 2.24)** | 1.38 (0.98, 1.94) | ||
| Stigma barriers | 1.68 (1.28, 2.22)*** | 1.33 (0.96, 1.84) | ||
| Logistical barriers | 1.84 (1.40, 2.42)*** | 1.31 (0.95, 1.81) | ||
| RUCA codes | ||||
| Micropolitan versus metropolitan | 1.68 (1.20, 2.34)** | 1.54 (1.05, 2.25)* | ||
| Small town/rural versus metropolitan | 0.90 (0.63, 1.28) | 0.73 (0.48, 1.12) | ||
*p < .05, **p < .01, ***p < .001.
Logistic regression analyses were performed to assess association between factors and VA treatment among users of mental health treatment using a similar method as the prior analysis estimating any mental health treatment. Table 4 shows the results of the logistic regression models estimating the odds of any VA mental health use. Males and soldiers aged 31–40 were more likely to use any VA treatment. Guard soldiers with private insurance and income greater than $50,000 were more likely to utilize non‐VA treatment only. Those who were employed were less likely to use VA mental health services compared to those who were not in the workforce.
Table 4.
Multivariable Logistic Regression Models Estimating Receipt of VA Mental Health Treatment in the Past Year, among Those Who Used Services (N = 405)
| Model 1: Predisposing Factors (N = 403) | Model 2: Need Factors (N = 403) | Model 3: Enabling Factors (N = 401) | Model 4: All Factors (N = 401) | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age (years) | ||||
| 31–40 versus 18–30 | 2.00 (1.01, 3.98)* | 1.91 (0.95, 3.83) | 3.09 (1.45, 6.55)** | 2.91 (1.35, 6.23)** |
| Over 40 versus 18–30 | 0.83 (0.47, 1.49) | 0.85 (0.47, 1.54) | 1.72 (0.87, 3.42) | 1.78 (0.88, 3.60) |
| Gender | ||||
| Male versus female | 2.58 (1.18, 5.61)* | 2.54 (1.15, 5.63)* | 3.53 (1.50, 8.31)** | 3.41 (1.42, 8.20)** |
| Non‐white | 1.51 (0.79, 2.88) | 1.47 (0.76, 2.85) | 1.30 (0.66, 2.57) | 1.25 (0.62, 2.51) |
| Mental health conditions | ||||
| 0 versus 1 | 0.58 (0.30, 1.15) | 0.59 (0.29, 1.22) | ||
| 2 versus 1 | 1.71 (0.61, 4.84) | 1.99 (0.67, 5.91) | ||
| 3 versus 1 | 1.81 (0.73, 4.52) | 1.63 (0.63, 4.22) | ||
| Income | ||||
| $25,001–$50K versus ≤$25K | 0.69 (0.32, 1.52) | 0.67 (0.30, 1.48) | ||
| >$50,001 versus ≤$25K | 0.44 (0.19, 1.02) | 0.42 (0.18, 0.99)* | ||
| Private insurance | 0.28 (0.13, 0.60)** | 0.30 (0.14, 0.63)** | ||
| Work status | ||||
| Employed versus unemployed | 0.50 (0.18, 1.40) | 0.48 (0.17, 1.37) | ||
| Employed versus out of workforce | 0.24 (0.07, 0.79)* | 0.22 (0.07, 0.76)* | ||
$50K = $50,000 and $25K = $25,000.
*p < .05, **p < .01, ***p < .001.
Discussion
Approximately 28 percent of our overall sample of Guard soldiers and 56 percent of those screening positive for mental health conditions on symptom scales used mental health services in the prior 12 months from either a VA or community provider. Our findings are similar to the Ohio study, where 31 percent of Guard soldiers per year accessed psychiatric services (Fink et al. 2015). Reassuringly, in this study, the strongest associations between soldier factors and any services use were those related to need factors rather than predisposing or enabling factors. Given the positive predictive value (PPV) of 0.5 for having major depression with PHQ‐9 scores ≥10, and for having PTSD with PCL screen ≥50, overall use of services would appear to be reasonable and appropriate for the anticipated level of clinical disorders.
We note that the large majority of Guard soldiers in our study who use services are using VA services. This is consistent with the needs assessment conducted by Rand (Schell et al. 2011) that noted the VA system is one of the primary providers of mental health care for veterans. Analyses of VA versus non‐VA use among Guard soldiers indicated that enabling and predisposing factors but not need factors were important in the choice of treatment setting among those who reported use.
Although eligibility criteria for VA services have generally broadened and the duration of benefits has increased since 2001, eligibility for particular types of services depends upon such factors as combat exposure, discharge status, income, and disability rating. The cross‐section of data analyzed 1‐year postdeployment suggests that VA is reasonably accessible to those with the greatest need; however, a complicated system and difficulty accessing services may result in some veterans preferring to seek needed treatment from non‐VA sources. This is consistent with our study findings that Guard soldiers who were employed with incomes greater than $50,000 and had insurance were more likely to utilize non‐VA mental health treatment than unemployed, lower income, and uninsured individuals. The Veterans Choice Program is expected to expand health care access to thousands of veterans by allowing them to receive care from non‐VA health care providers (Veterans Access, Choice, and Accountability Act of 2014). This new program will cover VA‐approved health needs, and further study is needed to determine whether it increases use overall of mental health treatment for National Guard soldiers, or simply shifts mental health service use from VA to non‐VA treatment settings.
Ready access to community mental health treatment may be advantageous, but community providers may also be less familiar with the military culture, deployment experiences, or evidence‐based treatments for PTSD compared to health care providers in military treatment facilities or the VA. The VA has made enormous efforts to train all of its providers in evidence‐based treatments, including prolonged exposure and cognitive processing therapy for PTSD. The prevalence and availability of providers experienced in evidence‐based treatments in the community are unknown. And for veterans with higher level need, the impact that expanding the ability for the VA to purchase care from non‐VA providers will have on outcomes remains uncertain.
In addition to considering access to evidence‐based treatment in VA versus non‐VA settings, a potential shift in treatment setting may also influence whether individuals receive the recommended number of therapy sessions for their identified condition. Hoge et al. (2014) have identified opportunities to improve treatment engagement and retention among active‐duty soldiers; however, far less is known about treatment engagement among National Guard and Reserve.
This study expands our understanding of initial treatment engagement with VA and non‐VA mental health treatment and may serve as a beginning point for looking at change over time. Prior analysis demonstrated that the prevalence of mental health concerns 12 months postdeployment did not change for serial panel cohorts 45–90 days postdeployment, with 15.8 and 19.0 percent having PTSD and depression symptoms, respectively (Valenstein et al. 2014). Looking over time at changes in outcomes within individuals who are engaged in VA and non‐VA care is an important next step. Continued treatment engagement in both settings may be important. For example, in one study of 50,000 newly diagnosed VA patients, only 27 percent were able to receive the recommended nine or more therapy sessions in the first year and less than 10 percent received nine or more sessions in the recommended 15‐week time period (Seal et al. 2010). The population may benefit from a quality improvement initiative that monitors not only access but also engagement in evidence‐based treatment, number of sessions, reasons for early dropout, and change in symptom severity at the end of treatment in both VA and community settings.
Limitations
We studied mental health service utilization of Guard units from a specific state and at a specific time (2011–2013); therefore, our findings may not generalize to other Guard soldiers from other states who deployed at different times during the war. Local health system factors may have a major effect on access to services for these veterans. However, access to VA mental health care services in Veterans Integrated Service Network (VISN) 11 is likely comparable to the national average. For instance, in the final quarter of fiscal year 2013, 7.5 percent of local Veterans under the age of 45 received VA mental health care services, as compared to the national average of 7.4 percent (VA Office of Mental Health Operations Mental Health Evaluation Center Information System).
The single source of self‐report and cross‐sectional nature of the data also limit our ability to assess whether either VA or non‐VA mental health treatment improved symptoms. There were also a number of participants (N = 180) in this study whose symptoms did not reach the criteria for a mental health condition at the time of assessment, yet they had received any VA (n = 131) and non‐VA only (n = 49) mental health treatment during the past 12 months. We do not know if this number represents soldiers who never met clinical cutoffs for a mental health condition at some point during the year or if treatment within the last 12 months had alleviated their symptoms. Future studies should consider predisposing and enabling factors that predict nonuse in the presence of need, initiation of treatment with subsequent dropout, completion of evidenced‐based treatment, and factors that are associated with improved symptoms over time for Guard soldiers receiving treatment in both VA and community settings as well as those who did not receive treatment.
Conclusions
The results suggest that need is an important factor for Guard soldiers receiving any mental health treatment, as those soldiers screening positive for multiple mental health conditions were more likely to access services. The observed overall use of services appears to be appropriate for the anticipated level of clinical disorders, given the PPV of our screening measures. However, we do not know how well treatment is targeted to those with full clinical disorders. Additional assessment such as diagnostic interviews are needed to better estimate the numbers of mental health conditions present in Guard soldiers and the rates of service utilization for those who meet full diagnostic criteria for mental health conditions. The VA continues to be the primary source of mental health treatment for Guard soldiers who have been deployed in combat zones. Non‐VA treatment access is associated with enabling factors of employment status, higher levels of income, and insurance. These findings raise important questions about social determinants and suggest that Guard soldiers with greater resources may have access to more treatment options. Changes in these enabling factors with changes in veteran health coverage (i.e., Veteran Choice Program) may shift the locus of mental health care. Longitudinal research is needed to understand the role of access to treatment (VA and non‐VA), engagement in treatment in these settings, provision of evidence‐based care, and outcomes of veterans receiving treatment overall and in VA and non‐VA treatment sectors. Ensuring Guard soldiers with identified need have access to treatment and improved health outcomes is a priority for service providers.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the VA HSR&D Service SDP 10‐047. LAG is supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Psychological Health/Traumatic Brain Injury Research Program Award W81XWH‐12‐1‐0419. RKS is supported by the VA Advanced Fellowship Program in Mental Illness Research and Treatment, the VA Serious Mental Illness Treatment Resource and Evaluation Center (SMITREC), and the VA Ann Arbor Healthcare System. KMB is supported by VA HSR&D Service Grant CDA 11‐245.
Disclosures: None.
Disclaimers: None.
References
- Andersen, R. M. 1995. “Revisiting the Behavioral Model and Access to Medical Care: Does it Matter?” Journal of Health and Social Behavior 36 (1): 1–10. [PubMed] [Google Scholar]
- Andersen, R. M. , and Davidson P. L.. 2013. “Improving Access to Care in America: Individual and Contextual Indicators” In Changing the U.S. Healthcare System, edited by Anderson R., Rice T., and Kominski G. F., pp. 3–32. San Francisco, CA: Jossey‐Bass. [Google Scholar]
- Bonar, E. E. , Bohner K. M., Walthers H. M., Ganaczy D., and Valenstein M.. 2015. “Student and Nonstudent National Guard Service Members/Veterans and Their Use of Services for Mental Health Symptoms.” Journal of the American College of Health 63 (7): 437–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowsky, S. J. , and Cowper D. C.. 1999. “Dual Use of VA and Non‐VA Primary Care.” Journal of General Internal Medicine 14 (5): 274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britt, T. W. 2000. “The Stigma of Psychological Problems in a Work Environment: Evidence from the Screening of Service Members Returning from Bosnia.” Journal of Applied Social Psychology 30: 1599–688. [Google Scholar]
- Cutrona, C. E. 1996. Social Support in Couples: Marriage as a Resource in Times of Stress. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Dillman, D. A. , Smyth J. D., and Melani L.. 2010. Internet, Mail, and Mixed‐mode Surveys: The Tailored Design Method. Toronto: Wiley and Sons. [Google Scholar]
- Elbogen, E. B. , Wagner H. R., Johnson S. C., Kinneer P., Kange H., Vasterling J. J., Timko C., and Beckham J. C.. 2013. “Are Iraq and Afghanistan Veterans Using Mental Health Services? New Data from a National Random‐Sample Survey.” Psychiatric Services 64 (2): 134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnitsky, C. A. , Andresen E. M., Clark M. E., McGarity S., Hall C. G., and Kerns R. D.. 2013. “Access to the US Department of Veterans Affairs Health System: Self‐reported Barriers to Care among Returnees of Operations Enduring Freedom and Iraqi Freedom.” BMC Health Services Research 13 (1): 498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbes, C. R. , Meis L. A., Polusny M. A., and Compton J. S.. 2011. “Couple Adjustment and Posttraumatic Stress Disorder Symptoms in National Guard Veterans of the Iraq War.” Journal of Family Psychology 25 (4): 479–87. [DOI] [PubMed] [Google Scholar]
- Fasoli, D. R. , Glickman M. E., and Eisen S. V.. 2010. “Predisposing Characteristics, Enabling Resources and Need as Predictors of Utilization and Clinical Outcomes for Veterans Receiving Mental Health Services.” Medical Care 48 (4): 288–95. [DOI] [PubMed] [Google Scholar]
- Fink, D. S. , Sampson L., Tamburrino M. B., Liberzon I., Slembarski R., Chan P., Cohen G. H., Shirley E., Goto T., D'Arcangelo N., Fine T., Reed P., Galea S., and Clabrese J. R.. 2015. “Lifetime and 12‐Month Use of Psychiatric Services among U.S. Army National Guard Soldiers in Ohio.” Psychiatric Services 66 (5): 514–20. [DOI] [PubMed] [Google Scholar]
- Fox, A. B. , Meyer E. C., and Vogt D.. 2015. “Attitudes about the VA Health‐Care Setting, Mental Illness, and Mental Health Treatment and Their Relationship with VA Mental Health Service Use among Female and Male OEF/OIF Veterans.” Psychological Services 12 (1): 49–58. [DOI] [PubMed] [Google Scholar]
- Goodwin, R. D. , Cohen G. H., Tamburrino M., Calabrese J. R., Liberzon I., and Galea S.. 2014. “Mental Health Service Use in a Representative Sample of National Guard Soldiers.” Psychiatric Services 65 (11): 1347–53. [DOI] [PubMed] [Google Scholar]
- Gorman, L. A. , Blow A. J., Ames B. D., and Reed P. L.. 2011. “National Guard Families after Combat: Mental Health, Use of Mental Health Services, and Perceived Treatment Barriers.” Psychiatric Services 62 (1): 28–34. [DOI] [PubMed] [Google Scholar]
- Hamilton, A. B. , Frayne S. M., Cordasco K. M., and Washington D. L.. 2013. “Factors Related to Attrition from VA Healthcare Use: Findings from the National Survey of Women Veterans.” Journal of General Internal Medicine 28 (2): 510–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerster, K. D. , Malte C. A., Imel Z. E., Ahmad Z., Hunt S. C., and Jakupcak M.. 2012. “Association of Perceived Barriers with Prospective Use of VA Mental Health Care among Iraq and Afghanistan Veterans.” Psychiatric Services 63 (4): 380–2. [DOI] [PubMed] [Google Scholar]
- Hoge, C. W. , Castro C. A., Messer S. C., McGurk D., Cotting D. I., and Koffman R. L.. 2004. “Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care.” New England Journal of Medicine 351 (1): 13–22. [DOI] [PubMed] [Google Scholar]
- Hoge, C. W. , Grossman S. H., Auchterlonie J. L., Riviere L. A., Milliken C. S., and Wilk J. E.. 2014. “PTSD Treatment for Soldiers after Combat Deployment: Low Utilization of Mental Health Care and Reasons for Dropout.” Psychiatric Services 65 (8): 997–1004. [DOI] [PubMed] [Google Scholar]
- Hyman, J. , Ireland R., Frost L., and Cottrell L.. 2012. “Suicide Incidence and Risk Factors in an Active Duty US Military Population.” American Journal of Public Health 102 (S1): S138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM (Institute of Medicine). 2013. Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Kehle, S. M. , Polusny M. A., Murdoch M., Erbes C. R., Arbisi P. A., Thuras P., and Meis L. A.. 2010. “Early Mental Health Treatment‐Seeking among US National Guard Soldiers Deployed to Iraq.” Journal of Traumatic Stress 23 (1): 33–40. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer R. L., and Williams J. B. W.. 2001. “Validity of a Brief Depression Severity Measure.” Journal of General Internal Medicine 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwert, P. , Knaevelsrud C., and Pietrzak R. H.. 2014. “Loneliness among Older Veterans in the United States: Results from the National Health and Resilience in Veterans Study.” American Journal of Geriatric Psychiatry 22: 564–9. [DOI] [PubMed] [Google Scholar]
- Laffaye, C. , Cavella S., Drescher K., and Rosen C.. 2008. “Relationships among PTSD Symptoms, Social Support, and Support Source in Veterans with Chronic PTSD.” Journal of Trauma Stress 21: 394–401. [DOI] [PubMed] [Google Scholar]
- Liu, C. F. , Bolkan C., Chan D., Yano E. M., Rubenstein L. V., and Chaney E. F.. 2008. “Dual Use of VA and Non‐VA Services among Primary Care Patients with Depression.” Journal of General Internal Medicine 24 (3): 305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe, B. , Unützer J., Callahan C. M., Perkins A. J., and Kroenke K.. 2004. “Monitoring Depression Treatment Outcomes with the Patient Health Questionnaire‐9.” Medical Care 42 (12): 1194–201. [DOI] [PubMed] [Google Scholar]
- Meis, L. A. , Barry R. A., Kehle S. M., Erbes C. R., and Polusny M. A.. 2010. “Relationship Adjustment, PTSD Symptoms, and Treatment Utilization among Coupled National Guard Soldiers Deployed to Iraq.” Journal of Family Psychology 24 (5): 560. [DOI] [PubMed] [Google Scholar]
- Office of Management and Budget. 2013. Revised Delineations of Metropolitan Statistical Areas and Combined Statistical Areas and Guidances on Uses of the Delineations of These Areas. (OMB Bulletin No. 13‐01). Washington, DC: Office of Management and Budget. [Google Scholar]
- Renshaw, K. D. , Rodrigues C. S., and Jones D. H.. 2009. “Combat Exposure, Psychological Symptoms, and Marital Satisfaction in National Guard Soldiers who Served in Operation Iraqi Freedom from 2005 to 2006.” Anxiety, Stress, and Coping 22 (1): 101–15. [DOI] [PubMed] [Google Scholar]
- Sareen, J. , Cox B. J., Afifi T. O., Stein M. B., Belik S. L., Meadows G., and Asmundson G. J.. 2007. “Combat and Peacekeeping Operations in Relation to Prevalence of Mental Disorders and Perceived Need for Mental Health Care: Findings from a Large Representative Sample of Military Personnel.” Archives of General Psychiatry 64 (7): 843–52. [DOI] [PubMed] [Google Scholar]
- Sareen, J. , Belik S. L., Stein M. B., and Asmundson G. J.. 2010. “Correlates of Perceived Need for Mental Health Care among Active Military Personnel.” Psychiatric Services 61 (1): 50–7. [DOI] [PubMed] [Google Scholar]
- Sayer, N. A. , Noorbaloochi S., Frazier P., Carlson K., Gravely A., and Murdoch M.. 2010. “Reintegration Problems and Treatment Interests among Iraq and Afghanistan Combat Veterans Receiving VA Medical Care.” Psychiatric Services 61 (6): 589–97. [DOI] [PubMed] [Google Scholar]
- Schell, T. L. , Tanielian T., Farmer C. M., Jaycox L. H., Marshall G. N., Vaughan C. A., and Wrenn G.. 2011. “A Needs Assessment of New York State Veterans.” RAND Health Quarterly 1, 1. [PMC free article] [PubMed] [Google Scholar]
- Seal, K. H. , Bertenthal D., Miner C. R., Sen S., and Marmar C.. 2007. “Bringing the War Back Home: Mental Health Disorders among 103,788 US Veterans Returning from Iraq and Afghanistan Seen at Department of Veterans Affairs Facilities.” Archives of Internal Medicine 167 (5): 476–82. [DOI] [PubMed] [Google Scholar]
- Seal, K. H. , Metzler T. J., Gima K. S., Bertenthal D., Maguen S., and Marmar C. R.. 2009. “Trends and Risk Factors for Mental Health Diagnoses among Iraq and Afghanistan Veterans Using Department of Veterans Affairs Health Care, 2002‐2008.” American Journal of Public Health 99 (9): 1651–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal, K. H. , Maguen S., Cohen B., Gima K. S., Metzler T. J., Ren L., and Marmar C. R.. 2010. “VA Mental Health Services Utilization in Iraq and Afghanistan Veterans in the First Year of Receiving New Mental Health Diagnoses.” Journal of Traumatic Stress 23 (1): 5–16. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke K., Williams J. B., and Löwe B.. 2006. “A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD‐7.” Archives of Internal Medicine 166 (10): 1092–7. [DOI] [PubMed] [Google Scholar]
- Sripada, R. B. , Bohnert A. S. B., Teo A. R., Levine D. S., Pfeiffer P. N., Bowersox N. W., Mizruchi M. S., Chermack S. T., Ganoczy D., Walthers H., and Valenstein M.. 2015. “Social Networks, Mental Health Problems, and Mental Health Service Utilization in OEF/OIF National Guard Veterans.” Social Psychiatry and Psychiatric Epidemiology Epub 02 June, 1–12. [DOI] [PubMed] [Google Scholar]
- Thomas, J. L. , Wilk J. E., Riviere L. A., McGurk D., Castro C. A., and Hoge C. W.. 2010. “Prevalence of Mental Health Problems and Functional Impairment among Active Component and National Guard Soldiers 3 and 12 Months Following Combat in Iraq.” Archives of General Psychiatry 67 (6): 614–23. [DOI] [PubMed] [Google Scholar]
- Valenstein, M. , Gorman L., Blow A. J., Ganoczy D., Walters H., Kees M., and Dalack G. W.. 2014. “Reported Barriers to Mental Health Care in Three Samples of US Army National Guard Soldiers at Three Time Points.” Journal of Traumatic Stress 27 (4): 406–14. [DOI] [PubMed] [Google Scholar]
- Veterans Access, Choice, and Accountability Act of 2014 . 2014. S. 3230, 113th Cong.
- Vogt, D. 2011. “Mental Health‐Related Beliefs as a Barrier to Service Use for Military Personnel and Veterans: A Review.” Psychiatric Services 62 (2): 135–42. [DOI] [PubMed] [Google Scholar]
- Ware, J. E. Jr , Kosinski M., and Keller S. D.. 1996. “A 12‐Item Short‐Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity.” Medical Care 34 (3): 220–33. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W. , Litz B. T., Herman D. S., Huska J. A., and Keane T. M.. 1993. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Wright, K. M. , Cabrera O. A., Bliese P. D., Adler A. B., Hoge C. W., and Castro C. A.. 2009. “Stigma and Barriers to Care in Soldiers Post‐combat.” Psychological Services 6 (2): 108. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


