Abstract
Objectives
Mitral valve replacement with either a bioprosthetic or a mechanical valve is the treatment of choice for severe mitral stenosis. However, choosing a valve implant type is still a subject of debate. This study aimed to evaluate and compare the early and late outcomes of mitral valve replacement [mechanical (MMV) vs. bioprosthetic (BMV)] for severe mitral stenosis.
Methods
A retrospective cohort study was performed on data involving mitral stenosis patients who have undergone mitral valve replacement with either BMV (n = 50) or MMV (n = 145) valves from 1999 to 2012. Data were collected from the patients’ records and follow-up through telephone calls. Data were analyzed for early and late mortality, New York Heart Association (NYHA) functional classes, stroke, pre- and postoperative echocardiographic findings, early and late valve-related complications, and survival. Chi-square test, logistic regression, Kaplan–Meier curve, and dependent proportions tests were some of the tests employed in the analysis.
Results
A total of 195 patients were included in the study with a 30-day follow-up echocardiogram available for 190 patients (97.5%), while 103 (53%) were available for follow-up over the telephone. One patient died early postoperatively; twelve patients died late in the postoperative period, six in the bioprosthesis group and six in the mechanical group. The late mortality had a significant association with postoperative stroke (p < 0.001) and postoperative NYHA Classes III and IV (p = 0.002). Postoperative NYHA class was significantly associated with age (p = 0.003), pulmonary disease (p = 0.02), mitral valve implant type (p = 0.01), and postoperative stroke (p = 0.02); 14 patients had strokes in the mechanical (9) and in the bioprosthetic (5) groups. NYHA classes were significantly better after the replacement surgeries (p < 0.001). BMV were significantly associated with worse survival (p = 0.03), worse NYHA postoperatively (p = 0.01), and more reoperations (p = 0.006). Survival was significantly better with MMV (p = 0.03). When the two groups were matched for age and mitral regurgitation, the analysis revealed that BMV were significantly associated with reoperations (p = 0.02) but not significantly associated with worse survival (p = 0.4) or worse NYHA (p = 0.4).
Conclusion
MMV replacement in mitral stenosis patients is associated with a lower reoperation rate, but there was no difference in survival compared with BMV replacement.
Keywords: Bioprosthetic valves, Mechanical valves, Mitral stenosis, Outcome, Valve replacement
Abbreviations
- MS
Mitral Stenosis
- BMV
Bioprosthetic Mitral Valve
- MMV
Mechanical Mitral Valve
- NYHA
New York Heart Association
- DM
Diabetes Mellitus
- HTN
Hypertension
- CHF
Congestive Heart Failure
- LV
left Ventricle
- MR
Mitral Regurgitation
- EF
Ejection Fraction
- Op
operative
- MVR
Mitral Valve Replacement
- AVR
Aortic Valve Replacement
- TV
Tricuspid Valve
- AV
Aortic Valve
Introduction
Mitral stenosis (MS) is most commonly due to rheumatic fever resulting in rheumatic heart disease [1]. A surgical pathology series of 452 MS patients concluded that 99% of the patients had postinflammatory disease that was believed to be rheumatic in origin [2].
Symptomatic MS can be treated by percutaneous mitral balloon valvotomy, surgical valvotomy, or surgically replacing the dysfunctional valve with either a mechanical mitral valve (MMV) or a bioprosthetic mitral valve (BMV) [3]. Open valvotomy is a repair procedure that involves direct visualization of the valve and debridement of the valve structure and reconstruction of subvalvular apparatus. Mitral valve replacement is usually preserved for severe MS that is not fit for percutaneous mitral balloon valvotomy or valve repair [4].
The purpose of this study was to compare mitral valve replacement, with either a BMV or a MMV, in MS patients and evaluate their early survival and long-term outcome.
Materials and methods
Setting and patients
The study was conducted in a tertiary care cardiac center (King Abdulaziz Cardiac Center) in Riyadh, Saudi Arabia, and the study population included all consecutive adult mitral valve replacement (MVR) patients operated on for mitral valve stenosis from 1999 to 2012. All patients that fit the inclusion criteria were enrolled in the study regardless of their sex and nationality. All the available patients were included in the study.
Study design
This study is a retrospective cohort of patient data collected from the center and the follow-up data gathered by contacting the patients through the telephone.
Data collection
Eighty variables were collected. They were representing information related to demographics, preoperative underlying conditions, early and late valve related complications, and pre- and postoperative echocardiogram data. Patients’ demographics, underlying conditions, preoperative echocardiograms, and early postoperative complications were obtained from the records of the patients. Patients’ records were provided as a soft copy in the form of Excel sheets (Microsoft Corporation, Redmond, WA, USA), which was then transferred into SPSS statistical package software version 20.0 (SPSS Inc., Chicago, IL, USA) for analysis. Postoperative echocardiogram data were collected using the Picture Archiving and Communication System to access the echo database. Late follow-up data (long-term) was acquired by calling the patients’ phone numbers provided in their hospital records via the hospital telephone. The patients were called over a period of 1 month after the data were collected from the medical records. A total of three calls were made. The patients who did not respond to the first call were again contacted after 2 weeks and those remaining were contacted 1 week after the second phone call.
A standardized and Institutional Review Board, King Abdullah international Research Center, Riyadh approved consent form was used during telephone calls in gathering the long-term outcomes information (late follow-up) to collect the following: (1) late mortality; (2) New York Heart Association (NYHA) functional class; (3) late valve-related complications [bleeding (which required blood transfusion), stroke (embolic or hemorrhagic), abdominal embolism, and endocarditis]; and (4) reoperation.
Data management
The patients who underwent MVR were divided into a BMV group and a MMV group. NYHA Classes I and II were grouped together as one group in the analysis, and the same was done for NYHA Classes III and IV. Ejection fraction (EF) groups are as follows: (1) normal EF (⩾55%); (2) mild left ventricular dysfunction (45–54%); and (3) moderate (30–44%) to severe (<30%) left ventricular dysfunction.
Data analysis
Data were entered and analyzed using Microsoft Excel (Microsoft Corporation) and SPSS version 20 (SPSS Inc.). The categorical variables are presented as frequencies, percentages, and quantitative variables as mean ± standard deviation. Chi-square test and logistic regression were used to compare the categorical variables, and independent t test/analysis of variance to compare the numerical variables. Survival analysis using the Kaplan–Meier curve was employed. Dependent proportions test (McNemar test) was used to compare post- and preoperative categorical data. The primary outcomes were survival and NYHA functional classification. The secondary outcome was valve-related complications.
Results
Baseline characteristics
A total of 195 patients were enrolled in the study analysis (BMV = 50, MMV = 145). All of the patients enrolled in the study had their postoperative data available up to 30 days postoperatively in the records. As for the postoperative echocardiogram before discharge of the patient, five patients’ echo reports were not available (97.5% available). Regarding telephone calls, 103 (53%) of the 195 patients responded to the telephone calls.
The mean age of the patients at operation was 48 ± 13 years. There were 71 (36%) men [BMV (13) and MMV (58)] and 124 (64%) women [BMV (37) and MMV (87)]. The follow-up was complete in 190 patients (97.5%; five patients were lost to follow-up after discharge from the hospital). The follow-up period was a minimum of 1 month and a maximum of 15.5 years with an average of 5.6 ± 4 years of follow-up, a median of 5.2 years, and a total of 1055 patient years (Table 1). The patients in the BMV group were older (53.7 ± 16.4 years vs. 46.1 ± 11.5 years) and had a bigger proportion of severe MR (50% vs. 38%). Preoperatively, out of the 195 patients who had MS: 43 (22%) had mild MS, 59 (30%) had moderate MS, and 93 (48%) had severe MS.
Table 1.
Baseline characteristics of patients.
| BMV (n = 50) | MMV (n = 145) | p | ||
|---|---|---|---|---|
| Age (y) | 53.7 ± 16.4 | 46.1 ± 11.5 | 0.001 | |
| Female sex, n (%) | 37 (74) | 87 (60) | 0.08 | |
| NYHA pre-opa | I & II | 14 (31) | 39 (33) | 0.87 |
| III & IV | 31 (69) | 81 (68) | ||
| Pre-op underlying conditions | Smoker | 3 (6) | 16 (11) | 0.30 |
| Obesity | 12 (24) | 49 (34) | 0.20 | |
| Hyperlipidemia | 17 (34) | 39 (27) | 0.34 | |
| DM | 12 (24) | 25 (17) | 0.29 | |
| HTN | 13 (26) | 24 (17) | 0.15 | |
| Pulmonary disease | 7 (14) | 25 (17) | 0.59 | |
| CHF | 19 (38) | 36 (25) | 0.07 | |
| EFb (pre-op) | Normal | 34 (74) | 109 (78) | 0.32 |
| Mild LV dysfunction | 5 (11) | 20 (14) | ||
| Moderate to severe LV dysfunction | 7 (15) | 11 (8) | ||
| MS (pre-op) | Mild | 16 (32) | 27 (19) | 0.14 |
| Moderate | 13 (26) | 46 (32) | ||
| Severe | 21 (42) | 72 (50) | ||
| MR (pre-op) | No regurgitation | 4 (8) | 28 (19) | 0.005 |
| Mild | 11 (22) | 12 (8) | ||
| Moderate | 10 (20) | 50 (35) | ||
| Severe | 25 (50) | 55 (38) | ||
Data are presented as n (%) or mean ± standard deviation.
BMV = bioprosthetic mitral valve; CHF = chronic heart failure; DM = diabetes mellitus; EF = ejection fraction; HTN = hypertension; LV = left ventricular; MMV = mechanical mitral valve; MR = mitral regurgitation; MS = mitral stenosis; NYHA = New York Heart Association; op = operation.
New York Heart Association preoperation: BMV = 45, MMV = 120.
EF: BMV = 46, MMV = 140.
Mortality
Out of the 195 patients, one patient (0.5%) died early postoperatively (i.e., <30 days). He was in the MMV group, and the cause of death was multiple organ failure. No further analysis in early mortality was carried out due to the small number of events. During follow-up, 12 patients died (6 in the BMV group and 6 in the MMV group). Postoperatively, both NYHA Classes III and IV (p = 0.002) and occurrence of stroke (p < 0.001) were found to be significantly associated with late mortality. NYHA postoperative Classes III and IV were related to late mortality (p = 0.002). Postoperative stroke occurrence (embolic or hemorrhagic) was associated with late mortality (p < 0.001; Table 2).
Table 2.
Factors associated with late mortality.a
| Factors | p |
|---|---|
| NYHA post-op | 0.002 |
| Post-op stroke (MMV = 9 & BMV = 5) | <0.001 |
| Mitral valve implant type | 0.055 |
| Post-op ventricular tachycardia | 0.055 |
BMV = bioprosthetic mitral valve; MMV = mechanical mitral valve; op = operative.
Chi-square test.
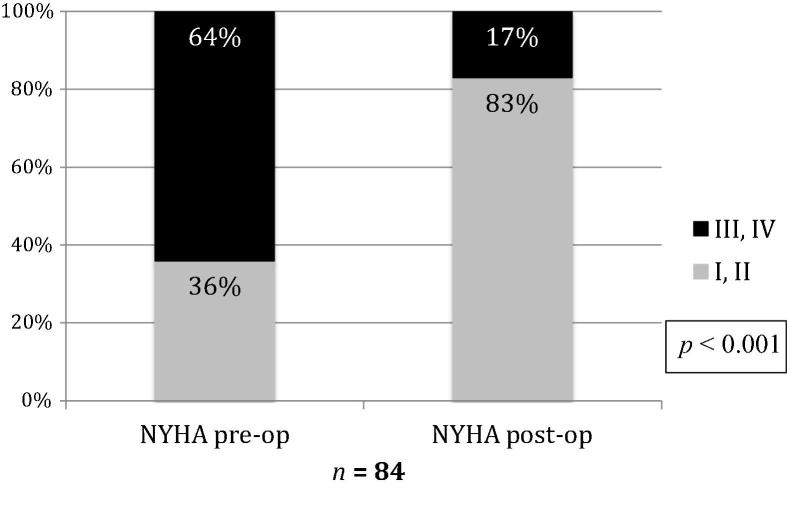
Functional class
Postoperatively, 83 (81%) patients were in NYHA Classes I and II and 20 patients (19%) were in NYHA Classes III and IV. Postoperative NYHA class was significantly associated with mitral valve implant type (p = 0.01) and postoperative stroke (p = 0.02). BMV was associated with NYHA Classes III and IV (p = 0.01; Fig. 1).
Figure 1.
Mitral valve implant type and postoperative New York Heart Association (NYHA). BMV = bioprosthetic mitral valve; op = operative; MMV = mechanical mitral valve.
Logistic regression analysis was used for postoperative NYHA and preoperative underling conditions and complications. It revealed that age (p = 0.003) and pulmonary disease (p = 0.02) were significantly associated with postoperative NYHA Classes III and IV. Moreover, it showed that postoperative stroke was the only significant complication (p = 0.04) associated with NYHA Classes III and IV and mortality.
Analysis of NYHA classes showed significant difference in proportions (p < 0.001). Most of the patients who were in NYHA Classes III and IV preoperatively shifted to Classes I and II postoperatively (Fig. 2). However, there was a significant drop in EF before and after the surgery (p < 0.001; Fig. 3). Before the surgery 137 (77%) patients had normal EF, and after the surgery 102 (57%) had normal EF. These findings might be attributed to the fact that 84 (43%) patients had MVR, 51 (26%) patients had MVR-tricuspid valve (TV) repair, 42 (22%) patients had MVR-aortic valve (AV) replacement, 13 (7%) patients had MVR-A replacement-TV repair, three (2%) patients had MVR-TV replacement, one (0.5%) patient had MVR-AV repair-TV repair, and one (0.5%) patient had MVR-TV valvectomy. The reduction of the EF could also be attributed to the fact that most of our patients had partial subvalvular apparatus preservation.
Figure 2.
New York Heart Association (NYHA) preoperative and postoperative. op = operative.
Figure 3.
Preoperative (pre-op) and postoperative (post-op) ejection fraction (EF). LV = left ventricular.
Complications
Regarding the early complications for the patients enrolled in the study (n = 195), atrial fibrillation or flutter, bleeding, and ventricular tachycardia were the most common early complications. The frequencies are as follows (n = 104): 19 (18%) patients had bleeding that required blood transfusion (13 in the MMV group and 6 in the BMV group), 14 (14%) patients had strokes (9 in the MMV group and 5 in the BMV group), 12 (12%) patients died, seven (7%) patients had reoperations (5 in the BMV group and 2 in the MMV group), one (1%) patient in the BMV group had an abdominal embolism, and one (1%) patient in the MMV group had endocarditis.
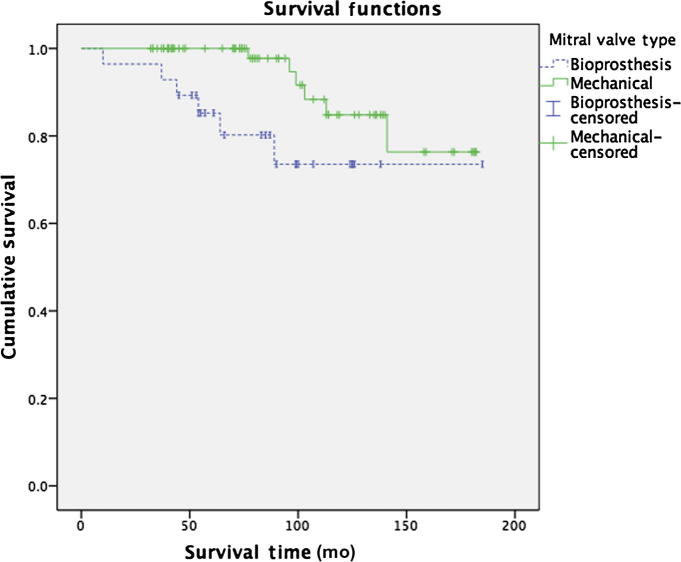
BMV versus MMV
MMV had significantly better survival than BMV (Fig. 4). In the analysis, the following were significant: MMV was associated with NYHA postoperative Classes I and II and BMV associated with NYHA Classes III and IV (Fig. 1); BMV was associated with reoperations (p = 0.006). BMV was also associated more with late mortality with p = 0.055.
Figure 4.
Kaplan–Meier survival curve of mitral valve replacement comparing mechanical mitral valves with bioprosthetic mitral valves; p = 0.03 (Mantel–Cox).
When the two groups (BMV and MMV) were matched for age and mitral regurgitation, the analysis revealed that BMVs were significantly associated with reoperations (p = 0.02) but not significantly associated with worse survival (p = 0.4) or worse NYHA (p = 0.4).
Survival
Twelve patients died (6 from BMV and 6 from MMV). Log rank (Mantel–Cox) test showed that there was a significant difference in survival between BMV and MMV with p = 0.03. The mean survival time of BMV is 150.6 ± 12 months (12.5 years), while MMV had a mean survival of 166 ± 6 months (13.8 years). The mean survival time of both BMV and MMV is 162 ± 6 months (13.5 years; Fig. 4). The analysis was carried out on the two groups (BMV and MMV) that were case matched for age and mitral regurgitation. There was no significant difference in survival (p = 0.4) between the case-matched groups.
Discussion
There have been a number of studies comparing MMVs to BMVs along with recommendations from the American Heart Association for the management of patients with valvular heart disease that mentioned the advantages and disadvantages for each of those valve implant types. This study results matches with the results of previous studies that were performed to compare BMVs to MMVs.
The Veterans Affairs trial randomized 575 patients to either a MVs or BMVs between 1977 and 1982. After 15 years of follow-up, the study found that the mortality was similar between the two groups, primary valve failure was more common with the BMV group in patients younger than 65 years, reoperations were more common in BMVs, and a there was a similar rate of valve-related complication incidences between the two groups, except for bleeding which was more common in MMVs [5]. Our study had similar results except for bleeding which was not significantly different between the two valve implant types.
In a 2003, a randomized prospective trial performed by Oxenham et al. [6] that involved 261 mitral valve replacements with either a MMV or a BMV, the survival between the two groups was similar. The reoperation rate was also higher in the BMV group. As for the other valve-related complications, only major bleeding was more prevalent in the MMV group. But there was no significant difference in endocarditis or major embolic events between the two groups. Our study showed that bleeding was not significantly different between the two valve types.
Comparable results were found in an observational study by Ruel et al. [7] that was published in 2007 that examined the long-term survival outcomes of heart valve replacement with either a BMV or a MMV in 567 adults who were younger than 60 years. They concluded that the survival in mitral valve replacement is similar between the two groups, but the reoperation rate was significantly higher in the BMV group.
With regards to perioperative mortality, our study shows a much lower incidence of early mortality compared with other studies. In our study, one patient died perioperatively (0.5%) compared with 4.3% [7], 7.7% [5], and 8.6% [6] in other studies. These results show us that in this new era, specialized centers with proper indication for surgeries can produce extremely good outcomes with low perioperative mortality, even in the setup of double and triple valve surgery.
In our study, some results were similar to what has been found in the literature. The late mortality was associated more with BMVs. Like the previous studies, the reoperation rates were also more common with the BMV group. Moreover, the other late valve-related complications (abdominal thromboembolism, stroke, severe bleeding, and endocarditis) were not significantly different between the two groups (MMV and BMV), similar to what has been demonstrated in some of the previous studies. Postoperative NYHA functional class analysis showed that the MMV group had significant association with Classes I and II. To adjust for the differences in terms of age and mitral regurgitation between the two groups, case matching was carried out. Case matching analysis revealed that BMVs were only significantly associated with reoperation rates, but not with worse survival or worse NYHA classes.
There was a significant drop in EF after the surgery. This drop is most likely attributed to two factors. Firstly, 84 (43%) of our patients had MVR while the remaining 111 (57%) patients had MVR plus another valve operation. Secondly, this drop might be due to the fact that most of our patients had partial subvalvular apparatus preservation which has been shown to be associated with lower EF in comparison to total subvalvular apparatus preservation in a number of studies. In a prospective study published in 2010 conducted by Zakai et al. [8] that included a total of 122 patients, it was noted that the EF improved in MVR in the preservation groups compared with the complete resection group which showed a decline in EF at follow-up. At the 6th month of follow-up, the mean EF of Group 1 (complete excision of the subvalvular apparatus) was 52.8%, Group 2 (preservation of the posterior leaflet) had a mean EF of 54.8%, and Group 3 (total chordal preservation) mean EF was 63.4%. In another retrospective study published in 2013 conducted by Ghavidel et al. [9] that included 151 patients, it was concluded that preserving the mitral annulus and the papillary muscle continuity may enhance cardiac performance and lower mortality and morbidity rates after MVR. A study published in 1999 by Yun et al. [10] that included 50 patients compared partial versus complete chordal preservation methods of MVR. The study concluded that complete retention of the subvalvular apparatus during MVR in comparison to posterior chordal preservation resulted in improved ejection performance. Many other studies have demonstrated that subvalvular apparatus preservation is superior to complete excision in MVR [11], [12], [13], [14].
Most of the studies in the literature are comparing MMV and BMV in the setting of both mitral and TV or mitral regurgitation and MS. Our study was focused on a specific subgroup of pathology, which is MS. Furthermore, we were not able to find a similar study in our region to display what the data are in relation to the population residing in this part of the world.
Study limitations
The study design is a retrospective cohort conducted in a single center. Long-term functional outcome information collection and late complication data gathering was done using telephone calls, and 53% of the patients responded at the time of writing the manuscript.
Conclusion
This retrospective cohort study involved 195 patients with MS who underwent MVR with either BMV or MMV. Late mortality had a significant association with postoperative stroke and postoperative NYHA Classes III and IV. Postoperative NYHA class was significantly associated with: age, pulmonary disease, and postoperative stroke. MMV was significantly better in terms of reoperation rate compared with BMV. Partial preservation of the subvalvular apparatus in MVR as opposed to total preservation might lead to a decrease in the postoperative EF.
Acknowledgments
We are grateful to Rawdené Van Onselen (clinical resource nurse, cardiac research/application analyst) for providing us with patients’ lists, preoperative patient data, and early postoperative events. We would also like to thank Emad Masuadi (Assistant Professor of Biostatistics, Department of Medical Education, King Saud Bin Abdulaziz University for health sciences, Riyadh) for helping us to conduct some statistical tests and interpret them.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Rahimtoola S.H. Mitral valve stenosis. In: Fuster V., King S.B., editors. Hurst’s the heart. 12th ed. McGraw-Hill Companies; New York: 2008. p. 1757. [Google Scholar]
- 2.Olson L.J., Subramanian R., Ackermann D.M., Orszulak T.A., Edwards W.D. Surgical pathology of the mitral valve: a study of 712 cases spanning 21 years. Mayo Clin Proc. 1987;62:22–34. doi: 10.1016/s0025-6196(12)61522-5. [DOI] [PubMed] [Google Scholar]
- 3.Runge M.S., Stouffer G.A., Patterson C. 2nd ed. Sauders; Philadelphia: 2010. Netter’s cardiology. [Google Scholar]
- 4.Lilly L.S. 5th ed. Lippincott Williams & Wilkins; Baltimore: 2011. Pathophysiology of heart disease: a collaborative project of medical students and faculty. [Google Scholar]
- 5.Hammermeister K., Sethi G.K., Henderson W.G., Grover F.L., Oprian C., Rahimtoola S.H. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36:1152–1158. doi: 10.1016/s0735-1097(00)00834-2. [DOI] [PubMed] [Google Scholar]
- 6.Oxenham H., Bloomfield P., Wheatley D.J., Lee R.J., Cunningham J., Prescott R.J. Twenty year comparison of a Bjork–Shiley mechanical heart valve with porcine bioprostheses. Heart. 2003;89:715–721. doi: 10.1136/heart.89.7.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruel M., Chan V., Bédard P., Kulik A., Ressler L., Lam B.K. Very long-term survival implications of heart valve replacement with tissue versus mechanical prostheses in adults <60 years of age. Circulation. 2007;116(Suppl. 11):I294–1300. doi: 10.1161/CIRCULATIONAHA.106.681429. [DOI] [PubMed] [Google Scholar]
- 8.Zakai S.B., Khan S.U., Rabbi F., Tasneem H. Effects of mitral valve replacement with and without chordal preservation on cardiac function: early and mid-term results. J Ayub Med Coll Abbottabad. 2010;22:91–96. [PubMed] [Google Scholar]
- 9.Ghavidel A.A., Mirmesdagh Y., Sharifi M., Sadeghpour A., Nakhaeizadeh R., Omrani G. The impact of sub-valvular apparatus preservation on prosthetic valve dysfunction during mitral valve replacement. Res Cardiovasc Med. 2013;2:55–61. doi: 10.5812/cardiovascmed.8054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yun K.L., Sintek C.F., Miller D.C., Schuyler G.T., Fletcher A.D., Pfeffer T.A. Randomized trial of partial versus complete chordal preservation methods of mitral valve replacement: a preliminary report. Circulation. 1999;100(Suppl. 19):II90–II94. doi: 10.1161/01.cir.100.suppl_2.ii-90. [DOI] [PubMed] [Google Scholar]
- 11.Wu Z.K., Sun P.W., Zhang X., Zhong F.T., Tong C.W., Lu K. Superiority of mitral valve replacement with preservation of subvalvular structure to conventional replacement in severe rheumatic mitral valve disease: a modified technique and results of 1-year follow up. J Heart Valve Dis. 2000;9:616–622. [PubMed] [Google Scholar]
- 12.Yang J.F., Hu J.G., Zhou X.M. Mitral valve replacement with a preserved subvalvular apparatus. Hunan Yi Ke Da Xue Xue Bao. 2002;27:49–50. [PubMed] [Google Scholar]
- 13.Straub U., Feindt P., Huwer H., Petzold T., Kalweit G., Volkmer I. Postoperative assessment of chordal preservation and changes in cardiac geometry following mitral valve replacement. Eur J Cardiothorac Surg. 1996;10:734–740. doi: 10.1016/s1010-7940(96)80333-2. [DOI] [PubMed] [Google Scholar]
- 14.Kowalik B. The effect of subvalvular apparatus preservation on the hemodynamic function of the heart in the early postoperative period after prosthetic mitral valve replacement. Ann Acad Med Stetin. 1997;43:181–192. [PubMed] [Google Scholar]