Abstract
Clopidogrel is a prodrug that requires bioactivation by cytochrome P450 (P450) enzymes to a pharmacologically active metabolite for antiplatelet action. The clinical limitations of clopidogrel are in large part due to its poor pharmacokinetics resulting from inefficient bioactivation by P450s. In this study, we determined the pharmacokinetics and pharmacodynamics of a novel conjugate of clopidogrel, referred to as ClopNPT, in animal models and we evaluated its potential to overcome the limitations of clopidogrel. Results from pharmacokinetic (PK) studies showed that ClopNPT released the active metabolite with a time to maximal plasma concentration of <5 minutes in C57BL/6 mice after either oral or intravenous administration, and plasma concentrations of the active metabolite reached Cmax values of 1242 and 1100 ng/ml after a 10-mg/kg oral dose and a 5-mg/kg intravenous dose, respectively. Furthermore, ClopNPT was highly effective in preventing arterial thrombosis in rabbits and mice after vascular injuries. Formation of occlusive thrombi was prevented by ClopNPT at the 1-mg/kg dose with no significant increase in tongue bleeding time, whereas clopidogrel was ineffective at the same dose. These results suggest that ClopNPT has favorable PK/pharmacodynamic properties that can potentially overcome the attenuated PK properties of clopidogrel and thus significantly improve the efficacy of antiplatelet therapy.
Introduction
Clopidogrel is an oral prodrug that inhibits the platelet P2Y12 receptor upon being bioactivated principally by CYP2C19 to a pharmacologically active metabolite (Savi et al., 1994; Ding et al., 2003; Dansette et al., 2012). Inhibition of the P2Y12 receptor by clopidogrel is irreversible due to covalent bonding of the active metabolite with the cysteinyl residues of the P2Y12 receptor (Boeynaems et al., 2005; Algaier et al., 2008). In combination with aspirin, clopidogrel is widely used in dual antiplatelet therapy (DAPT) to treat patients with acute coronary syndrome, especially those receiving percutaneous coronary intervention. Despite its broad use in clinical cardiology, clopidogrel has major limitations such as interindividual variability, delayed onset of action, and adverse drug–drug interactions (Gurbel and Tantry, 2007; Mega et al., 2009a). A large body of evidence indicates that approximately 30% of Caucasians and up to 60%–70% of Asians respond poorly to clopidogrel therapy, in part due to CYP2C19 polymorphism (Matetzky et al., 2004; Gurbel and Tantry, 2007; Mega et al., 2009b; Hasan et al., 2013). These patients are at increased risk of major adverse cardiovascular events (Matetzky et al., 2004; Bliden et al., 2007). In particular, patients with diabetes are more resistant to clopidogrel than individuals without diabetes. Angiolillo et al. (2014) showed that a low level of exposure to the active metabolite is mainly responsible for the poor response to clopidogrel therapy in patients with diabetes.
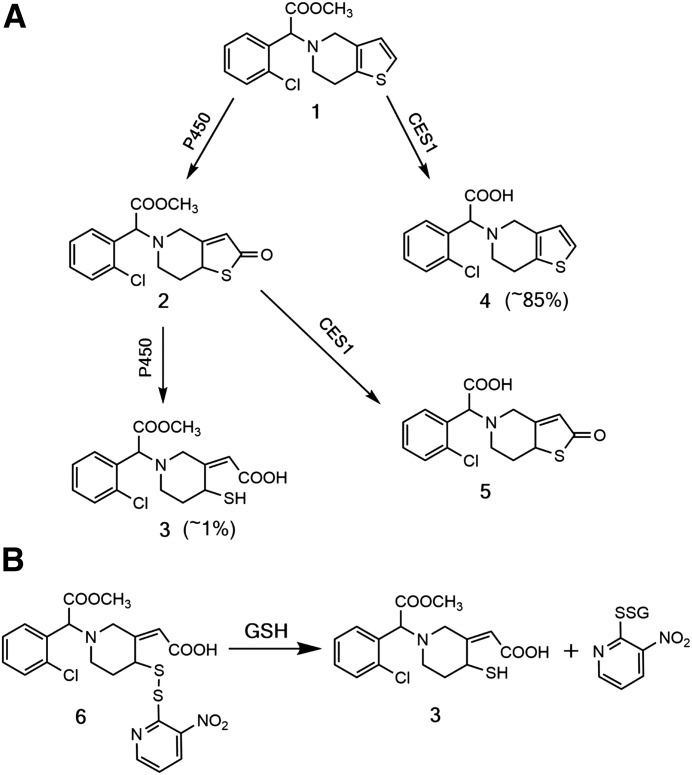
It is well documented that low levels of exposure to the active metabolite are closely related to the metabolism of clopidogrel. It was estimated that approximately 1%–5% of ingested clopidogrel is bioactivated to the active metabolite (Hagihara et al., 2009b; Zhu and Zhou, 2012). As illustrated in Scheme 1A, approximately 85% of ingested clopidogrel is hydrolyzed by carboxylesterase 1 in the liver to produce an inactive carboxylic acid metabolite (metabolite 4), whereas the remaining clopidogrel is extensively metabolized by cytochrome P450 (P450) enzymes to produce more than 15 metabolites (Tang et al., 2006; Hagihara et al., 2009b; Zhang and Hollenberg, 2014). This inefficient bioactivation is responsible, in large part, for the low level of drug exposure and delayed onset of action. Furthermore, because of genetic variability in CYP2C19 and carboxylesterase 1 genes, responses to clopidogrel therapy vary among patients of different ethnic groups (Mega et al., 2009a; Zhu et al., 2013). In light of these limitations, the US Food and Drug Administration approved two new P2Y12 antagonists, prasugrel (Effient; Lilly/Daiichi-Sankyo, Indianapolis, IN) and ticagrelor (Brilinta; AstraZeneca, Wilmington, DE), in 2009 and 2011, respectively. Both drugs induce faster and more potent inhibition of platelet aggregation than clopidogrel and are less associated with interindividual variability. However, these benefits come with an increased risk of bleeding (Wiviott et al., 2007; Wallentin et al., 2009).
Scheme 1.
(A) Metabolism of clopidogrel (1) by P450s and CES1 leading to the formation of 2-oxoclopidogrel (2), the active metabolite (3), and carboxylic acid metabolites (4 and 5). (B) Release of the active metabolite (3) from ClopNPT (6) in the presence of glutathione. CES1, carboxylesterase 1; GSH, glutathione.
Despite the availability of prasugrel and ticagrelor, clopidogrel is still widely used to prevent adverse thrombotic events. Thus, further improvement of the pharmacokinetic (PK)/pharmacodynamic (PD) properties of clopidogrel would provide more efficacious DAPT. We previously reported that ClopNPT, a mixed disulfide conjugate of the active metabolite with 3-nitropyridine-2-thiol (NPT), is readily converted to the active metabolite in the presence of glutathione through a thiol disulfide exchange reaction (Zhang et al., 2013; Scheme 1B). Furthermore, ClopNPT inhibits platelet aggregation in the platelet-rich plasma (PRP) of rabbits upon intravenous administration and its inhibitory effects do not require bioactivation by P450s (Zhang et al., 2014). In this work, we further characterized ClopNPT in animal models with respect to its PK/PD properties. Our results showed that ClopNPT releases the active metabolite with a time to maximal plasma concentration of <5 minutes in C57BL/6 mice via both oral and intravenous routes, and the plasma concentrations of the active metabolite reach Cmax values of >1000 ng/ml after a 5-mg/kg intravenous dose or a 10-mg/kg oral dose of ClopNPT. Furthermore, ClopNPT was highly effective in preventing arterial thrombosis in rabbits and mice after vascular injuries. These favorable PK/PD properties suggest that ClopNPT has great potential as a fast-acting antiplatelet agent that can overcome the limitations of existing P2Y12 antagonists.
Materials and Methods
Chemicals.
Chemicals used to biosynthesize ClopNPT were purchased from commercial sources. NPT, NADPH, glucose 6-phosphate, and glucose-6-phosphate dehydrogenase were purchased from Sigma-Aldrich (St. Louis, MO) and 2-oxoclopidogrel was purchased from Aquila Pharmatech (Waterville, OH). (S)-Clopidogrel bisulfate was purchased from Toronto Research Chemicals (Toronto, Canada).
Animal Care and Use.
The procedures used in this study were in accordance with University of Michigan Institutional Animal Care and Use Committee guidelines (National Institutes of Health publication no. 86-23). The University of Michigan Unit for Laboratory Animal Medicine provided all veterinary care.
Pharmacokinetics of ClopNPT in C57BL/6 Mice.
We determined the pharmacokinetics of ClopNPT and the active metabolite in C57BL/6 mice in triplicate according to the protocol approved by the University of Michigan Institutional Animal Care and Use Committee. C57BL/6 mice (n = 3) that were aged 6–8 weeks and weighed approximately 20 g were obtained from the Jackson Laboratory (Bar Harbor, ME). Racemic ClopNPT was biosynthesized as previously described (Zhang et al., 2014). After it was dissolved in a 5:15:80 (v/v) mixture of N,N-dimethylacetamide, polyethylene glycol 400, and saline, ClopNPT was administered either as an intravenous bolus via the tail vein or as an oral gavage. The intravenous and oral doses were 5 and 10 mg/kg, respectively. Aliquots (50 μl) of blood were sampled from the retro-orbital sinus by serial bleeding predose (t = 0) and postdose at various time points. The blood samples were immediately mixed with 5 μl 0.5 M 3′-methoxyphenacyl bromide and the mixture was incubated at room temperature for 10 minutes to obtain the active metabolite–3′-methoxyacetophenone derivative (AM-MP). The derivatized blood samples were stored at −80°C until use.
To quantify both ClopNPT and AM-MP in plasma, aliquots (15 µl) of the blood samples were mixed with 15 µl acetonitrile, followed by the addition of 60 µl acetonitrile containing 1 µM trans-clopidogrel-MP (13C, D) as the internal standard (IS). The mixture was then vortexed and centrifuged at 21,130g for 10 minutes. A 5-µl aliquot of the supernatant was injected for liquid chromatography–tandem mass spectrometry analysis. ClopNPT, AM-MP, and IS were chromatographed on an XBridge C18 column (4.6 × 50 mm, 3.5 µm; Waters, Milford, MA) using a binary mobile phase consisting of solvent A (0.1% formic acid in water) and solvent B (0.1% formic acid in acetonitrile). The fragment ions from transitions of mass-to-charge ratio (m/z) 510.0 → m/z 354.0 (ClopNPT), m/z 504.1 → m/z 354.1 (AM-MP), and m/z 508.2 → m/z 322.2 (IS) were used for quantifications. The standard solutions of ClopNPT and AM-MP were prepared by the addition of known amounts of ClopNPT (1–250 ng/ml) and AM-MP (1–2500 ng/ml) to blood samples from untreated mice.
The PK parameters for ClopNPT and the active metabolite were obtained by fitting the data to a noncompartmental model using Phoenix WinNonlin software (Certara, St. Louis, MO) to calculate the half-life (t1/2), area under the curve, and clearance rates. The t1/2 is terminal elimination half-life calculated based on data points (≥3) in the terminal phase with correlation coefficients > 0.90.
Pharmacodynamics of ClopNPT in Mice and New Zealand White Rabbits.
The PD responses to ClopNPT were determined in a ferric chloride injury model of arterial thrombosis in both mice and rabbits. Rabbits (Charles River Laboratories, Wilmington, MA), aged 10–12 weeks, were anesthetized with intravenous injections of xylazine (5 mg/kg) and ketamine (40 mg/kg). The surgical site was shaved and the animals were kept on a circulating water heating pad (approximately 37°C). A longitudinal incision was made in the midline of the neck and an endotracheal tube was inserted. The animals were then placed on a positive pressure ventilator (Harvard Apparatus Inc., Holliston, MA). Surgical anesthesia was maintained by intravenous injections of sodium pentobarbital (15 mg/kg). The left jugular vein was cannulated for drug or vehicle administration, and the left carotid artery was instrumented with a microtip pressure transducer (Millar Instruments Inc., Houston, TX). The catheter transducer was positioned immediately above the aortic valves to monitor aortic blood pressure. A 5-cm segment of the right carotid artery was exposed and a Doppler flow probe (model 1.5RB; Transonic System Inc., Ithaca, NY) was placed around the vessel. Carotid blood flow results were collected and analyzed using the PolyVIEW 16 data acquisition system (Grass Technologies, Warwick, RI). Carotid blood flow and the lead II electrocardiogram were monitored throughout the protocol.
To prevent FeCl3-induced thrombosis, ClopNPT was administered intravenously at a dose of 0, 0.4, 1, 2, or 5 mg/kg to the rabbits (n = 3) 30 minutes prior to the application of FeCl3. FeCl3-induced vascular injury was introduced according to an improved protocol as reported by Couture et al. (2013). Briefly, to induce vascular injuries, a small piece of Whatman filter paper saturated with 20% (w/v) FeCl3 was wrapped around the exposed left carotid artery caudal to the flow probe. The filter paper remained in contact with the vessel for the remainder of the experiment for 120 minutes to record blood flow. The time from the application of FeCl3 until the time of a stable zero blood flow was defined as the time to occlusion (TTO). In the control experiment, rabbits (n = 3) were given an intravenous dose of (S)-clopidogrel bisulfate instead.
C57BL/6 mice aged 10 weeks (Jackson Laboratory) were subjected to photochemical injury of the right carotid artery by rose bengal dye (Fisher Scientific, Hampton, NH), as previously described (Eitzman et al., 2000). Mice were anesthetized and placed under a dissecting microscope (Nikon SMZ2-T; Mager Scientific, Dexter, MA), and the right carotid artery was isolated. A Doppler flow probe (Transonic) was applied, and Rose Bengal dye (Fisher Scientific) diluted in phosphate-buffered saline was injected into the tail vein (50 mg/kg). A 1.5-mW green light laser (540 nm) (Melles Griot, Rochester, NY) was applied to the desired site of injury, from a distance of 6 cm, and vessel flow was monitored until occlusive thrombosis occurred, which was defined as flow cessation for at least 10 minutes. To prevent laser-induced thrombosis, ClopNPT was given as an intravenous bolus via the tail vein at a dose of 0, 0.5, 1, 2, or 5 mg/kg to the mice (n = 6–8) 30 minutes prior to laser-induced injury. Carotid blood flow was recorded for 120 minutes after laser-induced injuries.
Determination of Tongue Bleeding Time in New Zealand White Rabbits.
To evaluate the bleeding risk of ClopNPT, tongue bleeding time was determined as previously described (Hong et al., 2005). With the use of a SurgiCut device (International Technidyne Corp., Edison, NJ), a uniform incision 5 mm long and 1 mm deep was made on the upper surface of the tongue. Bleeding times were determined before and 1 hour after the administration of ClopNPT. The tongue lesion was blotted with filter paper every 5 seconds until the transfer of blood to the filter paper was no longer apparent. The interval from the time of the tongue incision until the time that blood was no longer transferred to the filter paper was recorded as the tongue bleeding time.
Statistical Analysis.
Results are reported as means ± S.E.M. and were subjected to a t test. Results were considered significant when P < 0.05. One-way analysis of variance was also performed to differentiate the difference in bleeding time at designated doses. Statistical analyses were performed using GraphPad Prism 6 software (GraphPad Software, La Jolla, CA).
Results
Pharmacokinetics of ClopNPT in C57BL/6 Mice.
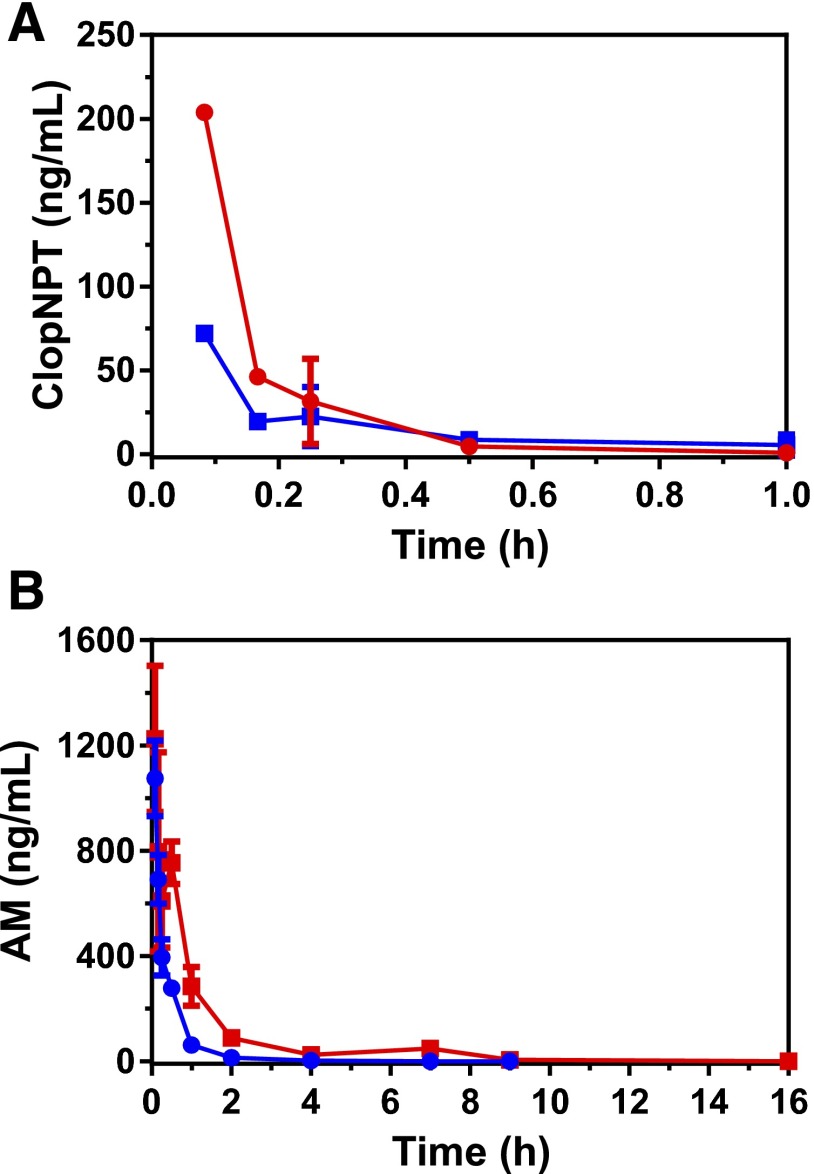
The PK results are shown in Fig. 1 and the corresponding parameters are summarized in Table 1. As shown in Fig. 1A, the plasma concentration of ClopNPT was 72 ± 3 ng/ml at 5 minutes after a 5-mg/kg intravenous dose and rapidly decreased with a t1/2 of 7.8 minutes. To examine whether the depletion of ClopNPT was due to its conversion to the active metabolite (metabolite 3), we also determined the concentration of the active metabolite in the plasma. As shown in Fig. 1B, the plasma concentration of the active metabolite was 1074 ± 143 ng/ml at 5 minutes after a 5-mg/kg intravenous dose, which is approximately 15-fold higher than that of the parent compound ClopNPT. Unlike ClopNPT, the half-life of the active metabolite was 1.3 hours, 10 times longer than that of ClopNPT.
Fig. 1.
Determination of the pharmacokinetics of ClopNPT (A) and the active metabolite (B) in C57BL/6 mice. ClopNPT was administered to C57BL/6 mice (n = 3) as a 5-mg/kg intravenous bolus or a 10-mg/kg oral gavage. Blood samples were drawn at various time points and amounts of ClopNPT and the active metabolite were quantified using liquid chromatography–tandem mass spectrometry as described in the Materials and Methods. The PK parameters were obtained by fitting the data to a noncompartmental model using WinNonlin software. The red and blue traces indicate the pharmacokinetics after oral and intravenous administration, respectively. AM, active metabolite.
TABLE 1.
PK parameters for ClopNPT and the active metabolite after administration of a 5-mg/kg intravenous dose and a 10-mg/kg oral dose to C57BL/6 mice
PK parameters were obtained by fitting the PK data in Fig. 1 to a noncompartmental model using WinNonlin software as described in the Materials and Methods.
| Parameter | ClopNPT |
Active Metabolite |
||
|---|---|---|---|---|
| Intravenous Dose | Oral Dose | Intravenous Dose | Oral Dose | |
| Cmax (ng/ml) | NA | 71.4 | 1100 | 1242 |
| Tmax (h) | NA | <0.083 | <0.083 | <0.083 |
| t1/2 (h) | 0.15 | 0.41 | 1.3 | 2.4 |
| AUC0–inf (h⋅ ng/ml) | 66.3 | 19.4 | 468.6 | 1136 |
| CLobs (ml/h per kg) | 76866 | NA | NA | NA |
AUC0–∞, area under the curve extrapolated from 0 to ∞; CLobs, observed clearance; NA, not applicable; Tmax, time to maximal plasma concentration.
Similar results were obtained after a 10-mg/kg oral dose. The plasma concentration of ClopNPT was 204 ± 4 ng/ml at 5 minutes and decreased with a t1/2 of 25 minutes. As observed after intravenous administration, the plasma concentration of the active metabolite after oral administration was also significantly higher than that of ClopNPT. At 5 minutes, it was 1225 ± 277 ng/ml followed by a gradual decrease with a t1/2 of 2.4 hours. As summarized in Table 1, the Cmax values of the active metabolite via intravenous and oral routes were 1100 and 1242 ng/ml, respectively. These observations provide strong evidence that ClopNPT is rapidly converted to the active metabolite in vivo upon intravenous and oral administration. Over a 24-hour period, we observed no sign of bleeding or changes of behavior due to the rapid release of the active metabolite in the dosed mice.
PD Responses to ClopNPT in New Zealand White Rabbits.
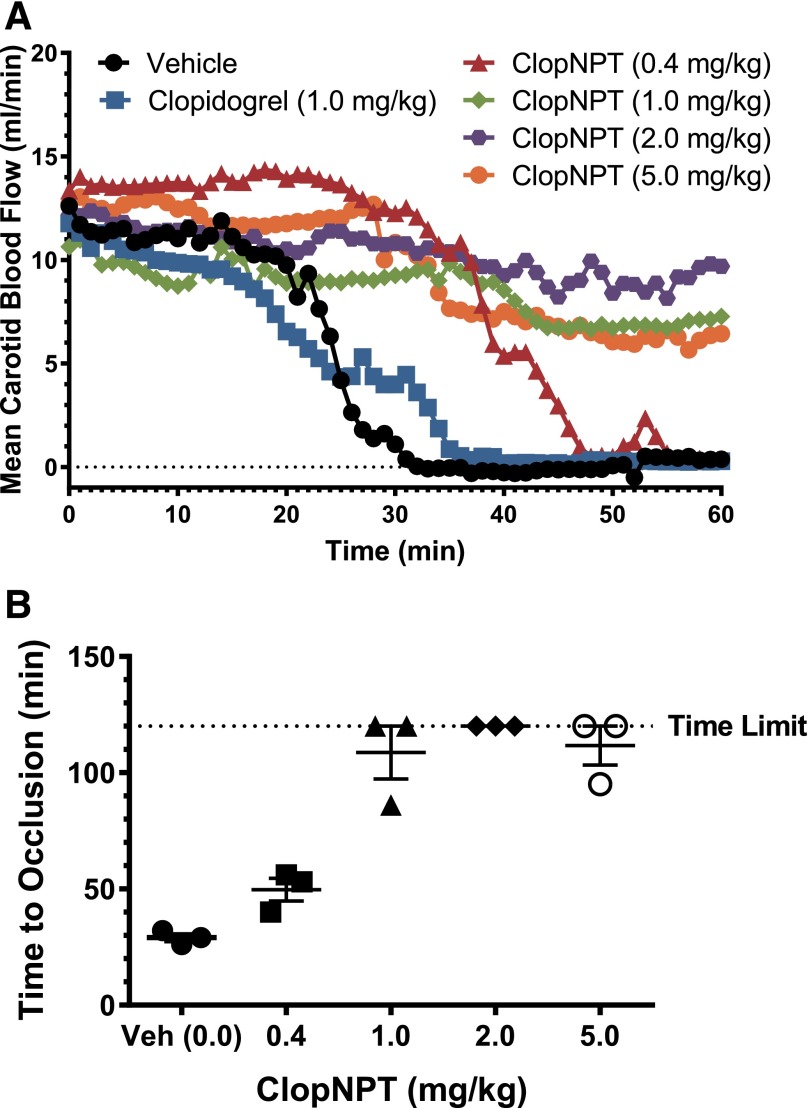
Figure 2 shows the mean carotid blood flow and TTO over a period of 2 hours after the application of FeCl3. As shown, the mean carotid blood flow prior to the application of FeCl3 varied little and was in the range of 11–14 ml/min among the experimental rabbits. However, the time dependence of the mean flow differed markedly between the control and dosed rabbits. In the rabbits administered vehicle, the mean flow was decreased to 0 in 30 minutes after FeCl3 was applied, which is indicative of the formation of stable occlusive thrombi. The averaged TTO for the vehicle group was 30 minutes as shown in Fig. 2B, which is consistent with a TTO of 25 minutes reported by Couture et al. (2013). The TTO showed a clear dose dependence in the rabbits administered ClopNPT. At the 0.4-mg/kg dose, the TTO was extended to 47 minutes, a 57% increase over that of the vehicle group. At higher doses, the TTO was significantly extended to over 110 minutes, which is indicative of effective prevention of arterial thrombosis. It is estimated from the dose dependence shown in Fig. 2B that the ED50 of ClopNPT for prevention of FeCl3-induced arterial thrombosis is approximately 0.6 mg/kg. In contrast, (S)-clopidogrel is ineffective in preventing arterial thrombosis at the 1-mg/kg dose, as shown in Fig. 2. This is consistent with a lack of ex vivo inhibition of platelet aggregation in the PRP of the rabbits administered 1 mg/kg (S)-clopidogrel intravenously (data not shown).
Fig. 2.
Determination of the mean carotid blood flow (A) and the TTO (B) in New Zealand White rabbits after FeCl3-induced arterial injury. The reported values of mean carotid blood flow and TTO were averaged over three independent measurements (n = 3). FeCl3 was applied to the carotid arteries of the rabbits 30 minutes after an intravenous bolus of ClopNPT, and the mean carotid blood flow and the TTO were determined as described in the Materials and Methods. Veh, vehicle.
PD Responses to ClopNPT in C57BL/6 Mice.
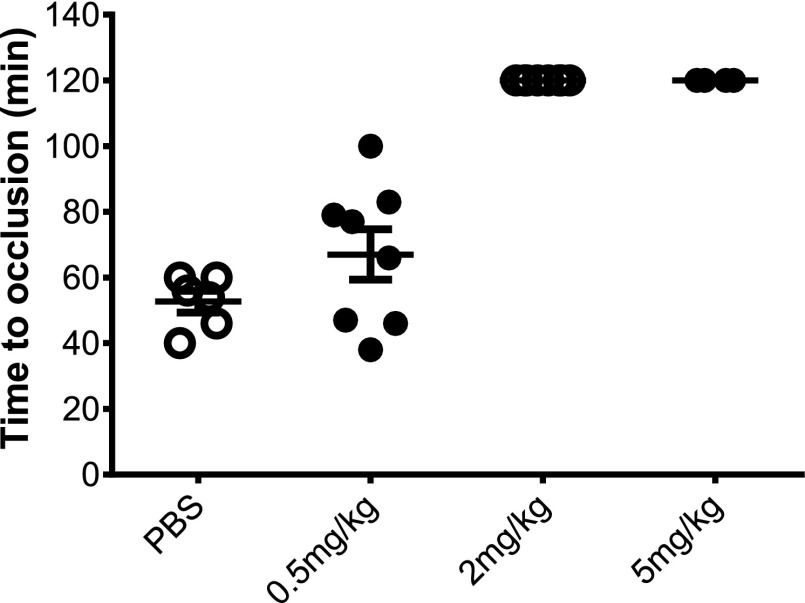
In addition to a nonrodent model, we also tested ClopNPT in a murine model. The results are shown in Fig. 3. The mean TTO of the control mice was 52 ± 8.2 minutes after laser-induced injury. At a 0.5-mg/kg dose, the mean TTO was 67 ± 21 minutes. An unpaired t test revealed that the two TTO values were statistically different (P < 0.05). At the 2- and 5-mg/kg doses, no occlusive thrombi were formed in the 120 minutes after laser-induced vascular injury, indicating that arterial thrombosis was prevented by ClopNPT.
Fig. 3.
Determination of the TTO in C57BL/6 mice after laser-induced arterial injury. C57BL/6 mice (n = 6–8) were administered either vehicle (control) or various doses of ClopNPT via the tail vein 30 minutes before laser-induced injuries. Blood vessel flow was monitored until occlusive thrombosis occurred as described in the Materials and Methods. PBS, phosphate-buffered saline.
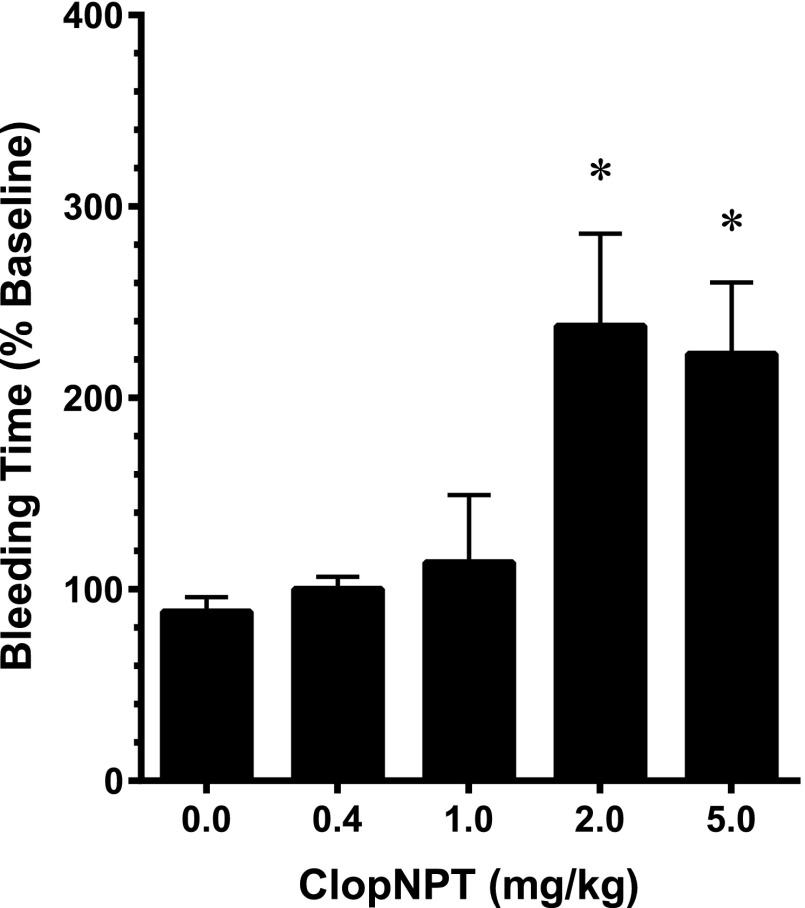
Tongue Bleeding Time in New Zealand White Rabbits.
Compared with clopidogrel, drug exposure to the active metabolite after administration of ClopNPT was significantly elevated. Rapid release of high levels of the active metabolite in the systemic circulation would raise concerns regarding bleeding. Therefore, we determined the tongue bleeding time in rabbits administered either vehicle or ClopNPT. Tongue bleeding time was measured predose (baseline bleeding time) and 1 hour postdose. The ratio of postdose bleeding time versus baseline bleeding time in percentages is plotted in Fig. 4. This relative bleeding time avoids the variations between individual rabbits and thus more realistically reflects the bleeding risk due to antiplatelet action of ClopNPT. The absolute bleeding time in the control rabbits was 1.5 minutes (data not shown). As shown in Fig. 4, tongue bleeding time was increased at elevated doses compared with the control. An increase by 2.5-fold in bleeding time at ≥2 mg/kg was observed. This increase is below the threshold of 3.5-fold conventionally used to determine the therapeutic window (van Giezen et al., 2009b). One-way analyses of variance showed that there were significant differences (P = 0.0167) in bleeding time between doses. Dunnett post hoc analyses showed that there was a significant increase in bleeding time at ≥2-mg/kg doses but not at lower doses that are effective to prevent thrombosis.
Fig. 4.
Determination of tongue bleeding time in New Zealand White rabbits. Bleeding time was determined using a SurgiCut device as described in the Materials and Methods. Both predose (baseline) and postdose bleeding times were determined from the same rabbit. The ratio of postdose bleeding time over baseline was expressed as the percentage of bleeding time. The postdose bleeding time was taken 1 hour after administration of ClopNPT. Asterisks indicate statistically different values (P < 0.05).
Discussion
We previously reported that ClopNPT rapidly inhibited ex vivo ADP-induced platelet aggregation in the PRP of rabbits upon intravenous administration, whereas clopidogrel was ineffective under the same conditions (Zhang et al., 2014). Here, we furthered our studies to characterize its PK/PD properties in animal models. Results from our PK studies showed that ClopNPT was rapidly converted to the active metabolite in vivo after either intravenous or oral administration. Upon oral administration, the molar ratio of the active metabolite to ClopNPT in plasma was 8.6 at 5 minutes, suggesting that approximately 90% of the administered ClopNPT was converted to the active metabolite. It should be pointed out that ClopNPT is a stable compound in marked contrast with the active metabolite. The rapid decrease in ClopNPT and simultaneous increase in the active metabolite in the plasma indicate that oral ClopNPT is rapidly absorbed in the small intestine and subsequently converted to the active metabolite. Although the exact mechanism by which ClopNPT is converted to the active metabolite in vivo remains to be elucidated, it is likely that ClopNPT is converted to the active metabolite by a thiol disulfide exchange reaction with glutathione (Zhang et al., 2013). This exchange may also be accelerated by glutaredoxin and thioredoxin (Hagihara et al., 2011, 2012). The rapid conversion of ClopNPT to the active metabolite also occurs after intravenous administration. As shown in Fig. 1, the molar ratio after intravenous administration was 21 at 5 minutes, which demonstrates an even faster conversion as expected. Based on the active metabolite’s area under the curve extrapolated from 0 to ∞, the estimated bioavailability of the active metabolite is approximately 80% (Table 1). This is a significant improvement over clopidogrel. Hagihara et al. (2009a) previously reported that the bioavailability of the active metabolite from clopidogrel was only 6.6% and 9.9% in rats and dogs, respectively.
In addition to the fast release of the active metabolite, drug exposure to the active metabolite was also significantly augmented. Cmax values of the active metabolite were 1100 and 1242 ng/ml for the intravenous and oral routes, respectively (Table 1). These values are significantly higher than those after administration of clopidogrel. Hagihara et al. (2009a) reported that the Cmax reached 35.5 ng/ml at 48 minutes after rats were administered a 7.7-mg/kg oral dose of clopidogrel. Tuffal et al. (2011) reported that the plasma concentration of the active metabolite in healthy human subjects receiving an oral dose of 300 mg clopidogrel reached a Cmax of 38 ng/ml. A Cmax of 91 ng/ml was reported in human subjects after a 300-mg intravenous dose of clopidogrel (Cushing et al., 2012). Using a relatively comparable dose of 10 mg/kg, we observed that ClopNPT reached a Cmax of 1242 ng/ml at 5 minutes in C57BL/6 mice, which represents a 35-fold increase in Cmax and an approximately 10-fold decrease in the time to maximal plasma concentration compared with the values obtained for rats. The high level of exposure to the active metabolite from ClopNPT demonstrates that the metabolic liabilities resulting in the low level of the active metabolite from clopidogrel were largely eliminated. It is clear that the PK properties of ClopNPT were drastically improved over clopidogrel.
The remaining question is whether ClopNPT prevents arterial thrombosis like P2Y12 antagonists do. Therefore, we elected to test the effectiveness of ClopNPT in both rodents and nonrodents using a well characterized arterial model of thrombosis. Arterial models of thrombosis after FeCl3- or laser-induced vascular injuries are widely used to evaluate the efficacy of antithrombotic drugs or drug candidates. As demonstrated in Figs. 2 and 3, a high level of exposure to the active metabolite of ClopNPT translates to effective prevention of arterial thrombosis in both rabbits and mice. Prolongation of arterial occlusion occurs at low doses of approximately 0.4 mg/kg and is dose dependent (Fig. 2). At ≥1 mg/kg, arterial thrombosis was almost completely prevented in the observed time period, which is indicative of the highly effective antiplatelet properties of ClopNPT. This is consistent with the observations that ClopNPT inhibits ex vivo ADP-induced platelet aggregation (Supplemental Fig. 1). It is of note that the PD responses in mice are more variable than in rabbits. It is unclear whether this variability is due to inherent difference in species or in experimental procedures. Nonetheless, ClopNPT is effective in both species.
The therapeutic index (TI) is often used to evaluate the efficacy and safety of antithrombotic drugs (van Giezen et al., 2009b). The TI is calculated as the ratio of EDBT = 3.5 to ED50, where EDBT = 3.5 is the dose at which a 3.5-fold increase in bleeding time occurs. With the 5-mg/kg dose, we observed a 2.5-fold increase in tongue bleeding time in rabbits. The TI of ClopNPT is estimated to be >4, which is greater than that of clopidogrel (2.1 in rats and 2.4 in dogs) (van Giezen et al., 2009a). Therefore, ClopNPT should have a wider therapeutic window than clopidogrel.
Fast release of the active metabolite and effective PD response with wider therapeutic window are advantageous in antiplatelet therapy for several reasons. First, studies have shown that early administration of clopidogrel improves patient prognosis and survival because of the role that platelets play in the early stage of thrombus formation (Yusuf et al., 2003). Second, a delayed onset of action that has plagued the use of clopidogrel can be overcome. Fast release of the active metabolite from ClopNPT in both routes of administration is especially desirable in acute clinical settings (Silvain and Montalescot, 2012; Franchi and Angiolillo, 2015) because it provides flexibility and convenience in dosing without switching P2Y12 inhibitors. Thus, ClopNPT has the potential to fill this unmet medical need. Finally, rapid release of high levels of the active metabolite from ClopNPT would benefit patients with diabetes. As mentioned previously, impaired P2Y12 inhibition in patients with diabetes is largely due to low drug exposure to the active metabolite of clopidogrel (Angiolillo et al., 2014). With much improved PK properties, we anticipate that ClopNPT would be more effective in DAPT for patients with diabetes.
In conclusion, we demonstrate that ClopNPT markedly improves the PK/PD properties in favor of effective antiplatelet action. ClopNPT rapidly releases the active metabolite after either intravenous or oral administration. Furthermore, the Cmax values reach >1000 ng/ml in the plasma after a 5-mg/kg intravenous dose or a 10-mg/kg oral dose. Rapid exposure to high levels of the active metabolite leads to effective prevention of arterial thrombosis in animal models with a wider therapeutic window. These results suggest that ClopNPT has the potential to overcome the limitations of existing P2Y12 inhibitors for DAPT.
Acknowledgments
The authors thank Miao He and Drs. Bo Wen and Ting Zhao (University of Michigan Pharmacokinetics Core Facility) for assistance with PK studies.
Abbreviations
- AM-MP
active metabolite–3′-methoxyacetophenone derivative
- ClopNPT
clopidogrel active metabolite conjugate with 3-nitropyridine-2-thiol
- DAPT
dual antiplatelet therapy
- IS
internal standard
- m/z
mass-to-charge ratio
- NPT
3-nitropyridine-2-thiol
- P450
cytochrome P450
- PD
pharmacodynamic
- PK
pharmacokinetic
- PRP
platelet-rich plasma
- t1/2
half-life
- TI
therapeutic index
- TTO
time to occlusion
Authorship Contributions
Participated in research design: Zhang, Lauver, Sun, Eitzman.
Conducted experiments: Zhang, Lauver, Wang.
Performed data analysis: Zhang, Lauver, Eitzman.
Wrote or contributed to the writing of the manuscript: Zhang, Hollenberg, Chen, Osawa, Eitzman.
Footnotes
This research was supported by the University of Michigan Center for Discovery of New Medicine; National Institutes of Health National Heart, Lung, and Blood Institute [Grants R01 HL088419 and R01 HL068878]; National Institutes of Health National Institute of General Medical Sciences [Grant R01 GM077430]; and National Institutes of Health National Cancer Institute [Grant P30 CA046952]. H.Z. and P.F.H. are inventors of a patent application (US 2015/0353492 A1) and receive royalties from Diapin Therapeutics LLC.
 This article has supplemental material available at jpet.aspetjournals.org.
This article has supplemental material available at jpet.aspetjournals.org.
References
- Algaier I, Jakubowski JA, Asai F, von Kügelgen I. (2008) Interaction of the active metabolite of prasugrel, R-138727, with cysteine 97 and cysteine 175 of the human P2Y12 receptor. J Thromb Haemost 6:1908–1914. [DOI] [PubMed] [Google Scholar]
- Angiolillo DJ, Jakubowski JA, Ferreiro JL, Tello-Montoliu A, Rollini F, Franchi F, Ueno M, Darlington A, Desai B, Moser BA, et al. (2014) Impaired responsiveness to the platelet P2Y12 receptor antagonist clopidogrel in patients with type 2 diabetes and coronary artery disease. J Am Coll Cardiol 64:1005–1014. [DOI] [PubMed] [Google Scholar]
- Bliden KP, DiChiara J, Tantry US, Bassi AK, Chaganti SK, Gurbel PA. (2007) Increased risk in patients with high platelet aggregation receiving chronic clopidogrel therapy undergoing percutaneous coronary intervention: is the current antiplatelet therapy adequate? J Am Coll Cardiol 49:657–666. [DOI] [PubMed] [Google Scholar]
- Boeynaems JM, van Giezen H, Savi P, Herbert JM. (2005) P2Y receptor antagonists in thrombosis. Curr Opin Investig Drugs 6:275–282. [PubMed] [Google Scholar]
- Couture L, Richer LP, Mercier M, Hélie C, Lehoux D, Hossain SM. (2013) Troubleshooting the rabbit ferric chloride-induced arterial model of thrombosis to assess in vivo efficacy of antithrombotic drugs. J Pharmacol Toxicol Methods 67:91–97. [DOI] [PubMed] [Google Scholar]
- Cushing DJ, Souney PF, Cooper WD, Mosher GL, Adams MP, Machatha S, Zhang B, Kowey PR. (2012) Pharmacokinetics and platelet aggregation inhibitory effects of a novel intravenous formulation of clopidogrel in humans. Clin Exp Pharmacol Physiol 39:3–8. [DOI] [PubMed] [Google Scholar]
- Dansette PM, Rosi J, Bertho G, Mansuy D. (2012) Cytochromes P450 catalyze both steps of the major pathway of clopidogrel bioactivation, whereas paraoxonase catalyzes the formation of a minor thiol metabolite isomer. Chem Res Toxicol 25:348–356. [DOI] [PubMed] [Google Scholar]
- Ding Z, Kim S, Dorsam RT, Jin J, Kunapuli SP. (2003) Inactivation of the human P2Y12 receptor by thiol reagents requires interaction with both extracellular cysteine residues, Cys17 and Cys270. Blood 101:3908–3914. [DOI] [PubMed] [Google Scholar]
- Eitzman DT, Westrick RJ, Nabel EG, Ginsburg D. (2000) Plasminogen activator inhibitor-1 and vitronectin promote vascular thrombosis in mice. Blood 95:577–580. [PubMed] [Google Scholar]
- Franchi F, Angiolillo DJ. (2015) Novel antiplatelet agents in acute coronary syndrome. Nat Rev Cardiol 12:30–47. [DOI] [PubMed] [Google Scholar]
- Gurbel PA, Tantry US. (2007) Clopidogrel resistance? Thromb Res 120:311–321. [DOI] [PubMed] [Google Scholar]
- Hagihara K, Kazui M, Ikenaga H, Nanba T, Fusegawa K, Takahashi M, Kurihara A, Okazaki O, Farid NA, Ikeda T. (2009a) Comparison of formation of thiolactones and active metabolites of prasugrel and clopidogrel in rats and dogs. Xenobiotica 39:218–226. [DOI] [PubMed] [Google Scholar]
- Hagihara K, Kazui M, Kurihara A, Ikeda T, Izumi T. (2012) Glutaredoxin is involved in the formation of the pharmacologically active metabolite of clopidogrel from its GSH conjugate. Drug Metab Dispos 40:1854–1859. [DOI] [PubMed] [Google Scholar]
- Hagihara K, Kazui M, Kurihara A, Kubota K, Ikeda T. (2011) Glutaredoxin and thioredoxin can be involved in producing the pharmacologically active metabolite of a thienopyridine antiplatelet agent, prasugrel. Drug Metab Dispos 39:208–214. [DOI] [PubMed] [Google Scholar]
- Hagihara K, Kazui M, Kurihara A, Yoshiike M, Honda K, Okazaki O, Farid NA, Ikeda T. (2009b) A possible mechanism for the differences in efficiency and variability of active metabolite formation from thienopyridine antiplatelet agents, prasugrel and clopidogrel. Drug Metab Dispos 37:2145–2152. [DOI] [PubMed] [Google Scholar]
- Hasan MS, Basri HB, Hin LP, Stanslas J. (2013) Genetic polymorphisms and drug interactions leading to clopidogrel resistance: why the Asian population requires special attention. Int J Neurosci 123:143–154. [DOI] [PubMed] [Google Scholar]
- Hong TT, Huang J, Driscoll E, Lucchesi BR. (2005) The antithrombotic effect of melagatran in combination with clopidogrel and/or aspirin (carotid artery primary thrombosis study). J Cardiovasc Pharmacol 46:526–533. [DOI] [PubMed] [Google Scholar]
- Matetzky S, Shenkman B, Guetta V, Shechter M, Beinart R, Goldenberg I, Novikov I, Pres H, Savion N, Varon D, et al. (2004) Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation 109:3171–3175. [DOI] [PubMed] [Google Scholar]
- Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, et al. (2009a) Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 360:354–362. [DOI] [PubMed] [Google Scholar]
- Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias WL, Braunwald E, et al. (2009b) Cytochrome P450 genetic polymorphisms and the response to prasugrel: relationship to pharmacokinetic, pharmacodynamic, and clinical outcomes. Circulation 119:2553–2560. [DOI] [PubMed] [Google Scholar]
- Savi P, Combalbert J, Gaich C, Rouchon MC, Maffrand JP, Berger Y, Herbert JM. (1994) The antiaggregating activity of clopidogrel is due to a metabolic activation by the hepatic cytochrome P450-1A. Thromb Haemost 72:313–317. [PubMed] [Google Scholar]
- Silvain J, Montalescot G. (2012) Rapid P2Y12 inhibition: still an unmet medical need. Circ Cardiovasc Interv 5:328–331. [DOI] [PubMed] [Google Scholar]
- Tang M, Mukundan M, Yang J, Charpentier N, LeCluyse EL, Black C, Yang D, Shi D, Yan B. (2006) Antiplatelet agents aspirin and clopidogrel are hydrolyzed by distinct carboxylesterases, and clopidogrel is transesterificated in the presence of ethyl alcohol. J Pharmacol Exp Ther 319:1467–1476. [DOI] [PubMed] [Google Scholar]
- Tuffal G, Roy S, Lavisse M, Brasseur D, Schofield J, Delesque Touchard N, Savi P, Bremond N, Rouchon MC, Hurbin F, et al. (2011) An improved method for specific and quantitative determination of the clopidogrel active metabolite isomers in human plasma. Thromb Haemost 105:696–705. [DOI] [PubMed] [Google Scholar]
- van Giezen JJ, Berntsson P, Zachrisson H, Björkman JA. (2009a) Comparison of ticagrelor and thienopyridine P2Y(12) binding characteristics and antithrombotic and bleeding effects in rat and dog models of thrombosis/hemostasis. Thromb Res 124:565–571. [DOI] [PubMed] [Google Scholar]
- van Giezen JJ, Nilsson L, Berntsson P, Wissing BM, Giordanetto F, Tomlinson W, Greasley PJ. (2009b) Ticagrelor binds to human P2Y(12) independently from ADP but antagonizes ADP-induced receptor signaling and platelet aggregation. J Thromb Haemost 7:1556–1565. [DOI] [PubMed] [Google Scholar]
- Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, et al. PLATO Investigators (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057. [DOI] [PubMed] [Google Scholar]
- Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, et al. TRITON-TIMI 38 Investigators (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Mehta SR, Zhao F, Gersh BJ, Commerford PJ, Blumenthal M, Budaj A, Wittlinger T, Fox KA, Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators (2003) Early and late effects of clopidogrel in patients with acute coronary syndromes. Circulation 107:966–972. [DOI] [PubMed] [Google Scholar]
- Zhang H, Hollenberg PF. (2014) From mechanism to therapeutics: overcoming inter-individual varibility in clopidogrel therapy, in Clopidogrel: Pharmacology, Clinical Uses and Adverse Effects (Alesci JP, Victorino A. eds) pp 121–147, Nova Science Publishers, Hauppauge, NY. [Google Scholar]
- Zhang H, Lauver DA, Hollenberg PF. (2014) CYP-independent inhibition of platelet aggregation in rabbits by a mixed disulfide conjugate of clopidogrel. Thromb Haemost 112:1304–1311. [DOI] [PubMed] [Google Scholar]
- Zhang H, Lauver DA, Lucchesi BR, Hollenberg PF. (2013) Formation, reactivity, and antiplatelet activity of mixed disulfide conjugates of clopidogrel. Mol Pharmacol 83:848–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu HJ, Wang X, Gawronski BE, Brinda BJ, Angiolillo DJ, Markowitz JS. (2013) Carboxylesterase 1 as a determinant of clopidogrel metabolism and activation. J Pharmacol Exp Ther 344:665–672. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Zhou J. (2012) Identification of the significant involvement and mechanistic role of CYP3A4/5 in clopidogrel bioactivation. ACS Med Chem Lett 3:844–849. [DOI] [PMC free article] [PubMed] [Google Scholar]