Introduction
The use of multiple informants has been recommended in child and adolescent mental health assessment to assure a comprehensive and more accurate view of presenting problems and contributing factors. Multiple informants, however, often bring conflicting perspectives on mental health issues of children and adolescents. Previous studies have shown parent and child informants to have considerable disagreement on the presence and severity of child depressive symptoms, with correlations in the low to moderate range (.20–.30) (De Los Reys & Kazdin, 2005). Such discrepancies pose a significant challenge for clinicians in determining the need for intervention and making treatment plans (De Los Reyes, 2011). In light of parents being the agents who enable their children to access mental health services, it is important to understand factors contributing to parent-child informant discrepancies in reports of child depression. Some studies have argued that discrepancies in results from multiple informants have potential clinical value (Achenbach, 2011). While parents report fewer symptoms, they are likely to bring unique perspectives about their children’s emotional health. Under-reporting of depressive symptoms becomes problematic if it means parents are unlikely to notice and promote help seeking when their child is suffering from emotional health problems.
Ethnic Differences of Discrepancy in Reporting of Child Depressive Symptoms
Few studies examine predictors of discrepancies between parent and child reports of child depressive symptoms. Previous studies on ethnic differences in informant discrepancies have revealed greater parent-child discrepancies among ethnic minority groups than among European Americans (Lau, Garland, Yeh, McCabe, Wood, & Hough 2004). Lau et al. (2004) found the greatest discrepancies in Asian dyads compared to European Americans, African Americans, and Hispanics. In terms of patterns of discrepancies, Lau et al. (2004) reported European American parents to report more internalizing problems than their children, while African American, Hispanic American, and Asian/Pacific Islander children report more internalizing problems than their parents (Lau et al. 2004).
Parenting, as well as parents’ appraisal and interpretation of child behaviors, is influenced by cultural beliefs and social factors (Kim, Im, Nahm, & Hong, 2012). Parenting in some immigrant cultures is characterized by expectations of obedience and conformity from children (Su & Hynie, 2011), whereas parenting from European American parents combines understanding and empathy, with valuing independence and autonomy (Kim et al., 2012). However, few empirical studies have examined parenting practices and/or the parent-child relationship as predictors of discrepancies in reporting child depressive symptoms. Fung and Lau (2010) found that when immigrant Chinese parents are more engaged in US culture, there are smaller parent-child discrepancies in reporting child internalizing problems. Parent-child relationship closeness predicted less discrepancy in reporting of children’s internalizing problems among Chinese immigrant families.
There is controversy in the literature as to whether parents with a history of depression are reliable reporters of children’s depressive symptoms. Ehrlich, Cassidy, and Dykas (2011) reported that more parents’ depressive symptoms were associated with higher parent-child reporting discrepancies, while Lewis et al. (2012) found that parents with a histroy of depression provided clinically meaningful ratings of childre’s depressive symptoms.
Given that 43% of all U.S. children age 19 and younger are ethnic minorities (Passel, 2011), nurse practitioners and other primary healthcare providers, should understand that parents from different ethnic groups have different ways of understanding, recognizing, and responding to their child’s emotional problems. Depending upon a parent’s ethnic heritage, the ways of understanding, recognizing, and responding may be different from the provider’s. They should also be familiar with the factors that contribute to discrepant reporting. The current study uses a large, diverse sample of school children to investigate discrepancies in parent/child reporting of child depressive symptoms across four ethnic groups.
The Present Study
The objectives of this study were to determine whether race/ethnicity influenced discrepancies between parent and child assessments of the child’s depressive symptoms and to determine whether history of parental depression and/or parenting practices also influenced discrepancies. Using a community sample of 516 11–12 year olds from a large urban school district, this study followed a four-step process to meet research objectives. First, we examined ethnic group differences in discrepancies between reports of parents/guardians and their children regarding child symptoms of depression. Second, we examined whether parental history of depression was associated with racial/ethnic group differences in the discrepancies. Third, we examined the role of parenting practice as a unique contributor to ethnic group differences in discrepancies. Lastly, we tested the ethnic group-specific effects of parenting on discrepancies by examining an interaction between parenting and ethnic group. Based on past studies (Lau et al., 2004), we first hypothesized that we would find significant differences across ethnic groups in the discrepancies noted between parent- and child-reports. Our second and third hypotheses, also based on previous studies (Ehrlich et al., 2011; Fung & Lau, 2010), were that both parental history of depression and parenting practices would affect discrepancies in parent-child reports across ethnic groups. Our last hypothesis was that there would be a significant interaction between parenting and ethnic group in predicting discrepancy.
Method
Design and Sample
This study used an existing data set from the Developmental Pathways Project (DPP), a community-based longitudinal study that examined depression and conduct problems in early adolescence. The XX Human Subjects Division approved the study. Student participants were recruited from four public middle schools. The DPP study carried out universal mental health screening for depression and conduct problems in sixth-grade students from 2000–2004. Of 2,920 eligible sixth graders, 2,187 (74.9%) were screened. Children who were screened did not differ significantly by sex or ethnicity from children who were not screened.
Following screening, eligible students were invited to the DPP longitudinal study. The criteria for eligibility included: 1) the student had one adult caregiver who could speak English; and 2) the student’s family resided in the school district. A random sample of 807 students was identified for the longitudinal study of which 521 students (64.6%) and their parents/guardians agreed to participate. Demographic characteristics of study participants are shown in Table 1.
Table 1.
Demographic Characteristics (N=516)
| N | % | |
|---|---|---|
| Female | 249 | (48.3) |
| Race/Ethnicity | ||
| European American | 232 | (45.0) |
| African American | 143 | (27.7) |
| Asian American | 88 | (17.1) |
| Hispanic American | 53 | (10.3) |
| Age, mean (SD) | 12.0 | (0.4) |
In-home interviews were administered to participating students and parents/guardians (76% biological mothers, 15% biological fathers, 9% other caregivers) by two trained research interviewers. Of the 521 participants originally enrolled in the DPP, between 86% and 90% were retained in each of the first four follow-up interviews that were conducted every 6 months. For the purposes of this study’s analyses five Native American students were excluded due to small sample size. This study focused on African American (AA), Asian American (ASA), Hispanic American (HA) and European American (EA) children. Therefore, study data were drawn from 516 students.
Measures
Depression was measured using the Mood and Feelings Questionnaire (MFQ: Angold & Costello, 1987). The MFQ is a 33-item measure of depression for children aged 8–18. Child and parent-versions assess common affective, cognitive, and vegetative features of childhood depression (Costello & Angold, 1988). Participating students and their parents/guardians were asked to complete the MFQ at baseline assessment. Previous studies have validated high content and criterion validity showing agreement with depressive diagnoses derived from standardized diagnostic interviews (Merry et al., 2012). Responses were summed with high scores reflecting high depressive symptoms. Evaluation of the MFQ in 6th and 8th graders revealed measurement equivalence in scores across racial/ethnic groups (Banh et al, 2012). Cronbach’s alpha coefficients in this sample were .90.
Parenting practices were measured using the child report of the Parenting Behavior Inventory (CRPBI) (Schaefer, 1965; Schludermann & Schludermann, 1970). CRPBI consists of 24-items that contribute to three sub-constructs, including emotional connection, parental knowledge, and respect for autonomy. Students completed the CRPBI during seventh grade. Sample items about parents/guardians include: ‘It is easy to talk to her/him,’ ‘He/she often praises me,’ and ‘He/she knows who my friends are.’ Respondents can characterize parents/guardians using three response options. Responses were summed, and high scores reflected high levels of the sub-construct. Internal consistency was acceptable for each sub-construct (alpha=.82, .69, .65).
Parental history of depression was measured using the parent-report Family History Questionnaire (FHQ: Weissman, Wickramaratne, Adams, Wolk, Verdeli, & Olfson, 2000). Lifetime history of depression in the parent who completed MFQ was measured with six items. Examples of items include ‘felt sad, blue, or depressed for most of the time,’ and had a ‘period of feeling quite tired, having less energy’. Response options were Yes/No. Items were summed to yield a score from 0–6.
Race/ethnicity of the participating students was provided via XX Public School District. Parents/guardians report their child’s race/ethnic identity when they enroll in the school system. Children were from four mutually exclusive racial/ethnic categories including AA (Black/African Americans), ASA (Asian Americans), EA (European Americans), and HA (Hispanic Americans).
Data analyses
All analyses were performed using SPSS 17.0. To calculate standardized discrepancy scores, we used standardized depressive symptom scores (z-score) and subtracted the parent-report score from the child-report score, as suggested by other scholars (Laird & Weems, 2011). A positive discrepancy score indicated that the parent was underreporting depressive symptoms, compared to the child.
We examined whether parenting was associated with parent-child informant discrepancies across race/ethnic groups. To analyze ethnic group differences, we created interaction terms between race/ethnic group and parental history of depression and parenting. A series of hierarchical regression analyses were conducted to capture the following: Step 1) whether there are racial/ethnic group differences in discrepancies; Step 2) whether, in addition to race/ethnicity, parental history of depression is associated with discrepancies, Step 3) whether parenting practices are associated with discrepancies; and Step 4) whether there were ethnic differences in the effects of parent depression or parenting practices on discrepancies. Child race/ethnicity was entered in the first model. In the second model, a history of parent depressive symptoms was entered as a covariate. In the third model, parenting practice variables were entered. In the fourth model, we added interaction terms between parent depression and ethnicity and between parenting and ethnicity.
Results
Descriptive Analyses
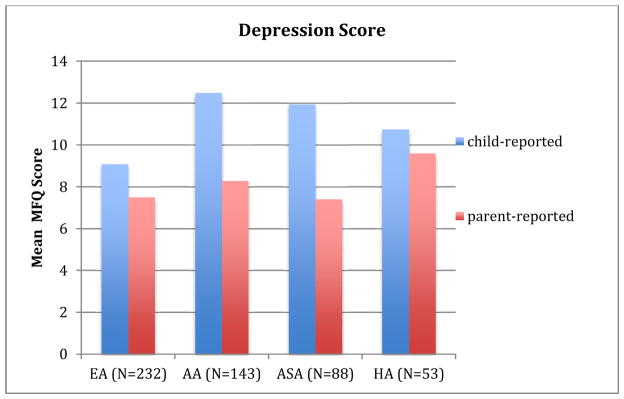
Descriptive statistics (means and standard deviations) are shown in Table 2, and bivariate correlations in Table 3. Child-reported and parent-reported MFQ scores across ethnic groups are illustrated in Figure 1. The correlation between the total MFQ scores in children and parents was 0.27 (p < .01). While among children, AAs reported the highest mean score of depressive symptoms, among parents HA reported the highest mean score of depressive symptoms in their children. Parents across all ethnic groups reported fewer depressive symptoms than children.
Table 2.
Descriptive Statistics for Key Study Variables
| Variable | M | SD |
|---|---|---|
| 1. Child depression-child report MFQ | 10.73 | 8.72 |
| 2. Child depression-parent report MFQ | 7.93 | 7.17 |
| 3. Discrepancy raw score | 2.80 | 9.68 |
| 4. Parent History of Depression (FHQ) | 1.75 | 1.85 |
| European American | 2.17 | 1.90 |
| African American | 1.61 | 1.77 |
| Asian American | 1.26 | 1.74 |
| Hispanic American | 1.54 | 1.77 |
| 5. Parenting practices (CRPBI) | 34.48 | 8.05 |
| European American | 36.22 | 8.29 |
| African American | 32.94 | 7.40 |
| Asian American | 32.03 | 8.20 |
| Hispanic American | 34.06 | 7.09 |
Table 3.
Summary of Hierarchical Regression Analyses Predicting Discrepancy in Parent-Child Report of Child Depressive Symptoms
| B | SE B | R2 | R2 change | model f | F | |
|---|---|---|---|---|---|---|
| Step 1 | 0.02 | 0.02 | 3.47 | 0.02 | ||
| African-American (AA) | 0.31* | 0.13 | ||||
| Asian-American (ASA) | 0.32* | 0.16 | ||||
| Hispanic-American (HA) | −0.10 | 0.18 | ||||
|
| ||||||
| Step 2 | 0.02 | 0.00 | 0.76 | 0.38 | ||
| Parent history of depression (FHQ) | −0.03 | 0.06 | ||||
|
| ||||||
| Step 3 | 0.03 | 0.01 | 5.21 | 0.02 | ||
| Parenting (CRPBI) | −0.15* | 0.06 | ||||
|
| ||||||
| Step 4 | 0.03 | 0.03 | 0.52 | 0.67 | ||
| Parenting x AA | −0.09 | 0.16 | ||||
| Parenting x ASA | −0.19 | 0.17 | ||||
| Parenting x HA | −0.01 | 0.20 | ||||
| PHD x AA | −0.16 | 0.15 | ||||
| PHD x ASA | 0.01 | 0.19 | ||||
| PHC x HA | 0.09 | 0.21 | ||||
p < .05.
Figure 1.
MFQ raw mean score for each ethnic group by reporters. EA: European-American. AA: African-American. ASA: Asian-American. HA: Hispanic-American.
Relative to child reports, more than 70 percent of ASA parents had lower depression scores than their children, while nearly 65 percent of AA parents, 60 percent of HA parents, and 51 percent of EA parents under-reported depression symptoms relative to their child’s depression. ASA had the highest mean discrepancy scores (M = 4.53, SD = 9.88), followed by AA (M = 4.43, SD = 10.77), EA (M = 1.60, SD = 8.88), then HA (M = 1.15, SD = 8.94). Paired t-test results demonstrate that depression scores reported by parents and children were statistically significantly different for EAs [t (231) = 2.74, p = .007], AAs [t (142) = 4.81, p < .001], and ASAs [t (87) = 4.20, p < .001], but not significant among HAs [t (52) = .94, p = .35].
Factors Influencing Discrepancies
Race/Ethnicity
The hierarchical linear regression indicated significantly greater parent-child discrepancies in the AA (b = 0.31, p = .017) and ASA (b = 0.32, p = .042) groups than in EA (Step 1). Although not statistically significant, HAs had lower discrepancies than EA.
Parental depressive history and parenting practices
In Step 2, we examined whether parental depressive history was associated with parent-child discrepancies in ratings of child’s depressive symptoms. After controlling for race/ethnicity, we found parental depressive history (b = −0.30, p = .617) was not a significant contributor to discrepancies. In Step 3, we entered the parenting practices variable. After controlling for ethnicity and parental history of depression, we found parenting practices (b = −0.15, p = .015) were a significant contributor to discrepancies in child depression ratings. Parenting practices that maintained emotional connection, high parental knowledge, and high respect for child’s autonomy were associated with the lowest discrepancies, while lower quality parenting practices was associated with greater discrepancies. In Step 4 interaction terms between parent depression and racial/ethnic group and parenting practices and ethnic group were entered, but neither was significant in predicting parent-child discrepancies in depression reporting. Table 3 displays findings from the hierarchical regression.
Post hoc analysis
To examine the racial/ethnic differences in discrepancies more closely, we evaluated discrepancies at the level of depression item. We compared the mean score of parent- versus child- report on each item using t-tests. Among a total of 33 items, 24 were significantly under-reported by parents relative to children, regardless of ethnicity, while two items “felt miserable or unhappy” and “felt grumpy and gross with parents” were more likely to be reported by parents than children. Specific items demonstrated greater discrepancies among certain groups, but no distinct patterns or symptoms emerged. However, AA and ASA reported significantly greater discrepancy on four out of five items assessing suicide ideation compared to EA and Hispanics. Those items included “thought there was nothing good for me in the future”, “thought life was not worth living”, “thought about death and dying”, and “thought family was better off without me”.
Discussion
The current study examined parent-child discrepancies in reports of child depressive symptoms. Our findings showed that: 1) the parent-child informant correlation for the MFQ score was 0.27, matching the mean of the De Los Reys and Kazdin (2005) study (0.20–0.30); and 2) there are significant differences in discrepancies across racial/ethnic groups. Further, regardless of racial/ethnic group, all groups of parents under-reported child depressive symptoms, relative to their children. In ethnic comparisons, ASA showed greater report discrepancies, followed by the AA and EA. These findings are somewhat inconsistent with a previous study (Lau et al., 2004) in which EA parents were found to over-report child’s depressive symptoms, while parents from other groups tended to under-report them.
Findings on item-level discrepancies shed light on parental under-awareness of child depressive symptoms. Among a total of 33 items, more than 70 percent were significantly under-reported by parents, highlighting that parents might not be aware of depressive symptoms in children. It may be that parents in our sample, particularly in the AA and ASA group, lack sufficient knowledge to identify child depression. Without understanding behavioral cues, parents might not initiate conversations with their children regarding their emotional status. There are behaviors related to depressive symptoms, such as aggression or grumpiness, that irritate other people, while symptoms like sadness, worthlessness, and hopelessness may be bothersome only to the child experiencing these symptoms. Therefore, having open communication would play an important role in parents recognizing a child’s internal problems.
The parent-child discrepancies in reporting of suicidal items were particularly wide in AA and ASA. Furthermore, AA and ASA parents have been shown in prior studies to have a significantly lower rate of utilization of any kind of mental health service when compared with non-Hispanic whites (Cumming & Druss, 2011) and to be less likely to pursue treatment when their child has suicidal thoughts (Ahmedani et al., 2015). Primary health care professionals, particularly those who work with AA and ASA families in clinics and school settings, should intentionally ask simple questions to assess how parents handle the child’s emotional issues within the family. AA and ASA parents might need practical advice on how to communicate with their children about emotional issues and suicide ideation. Providers can suggest to parents ways to create a family environment in which open communication is encouraged and where children are more comfortable disclosing emotional concerns.
One interesting finding of our study is that the discrepancy scores between parent-child reports in the HA group were small and statistically nonsignificant. While HA youth endorsed high levels of depression relative to other ethnic groups, reports of depressive symptoms by HA parents/guardians were consistent with child reports. These findings imply that HA parents were more attuned to recognizing depressive symptoms in their children. These findings should be interpreted with caution since the HA group was relatively small, making it difficult to detect discrepancies.
In contrast to previous findings of association between parental depression and greater discrepancy of reporting child’s depressive symptoms (Ehrlich et al., 2011), our findings support the notion that parent depressive history does not bias a parents’ reporting of their child’s depressive symptoms, regardless of ethnic identity. The observed difference in findings may reflect the fact that the current study assessed history of depressive symptoms experienced over the lifetime and not current symptoms. Additional research is needed on the question of whether parents suffering from depression can accurately report child behavioral and emotional problems (Ordway, 2011).
Consistent with previous studies (Fung & Lau, 2010; Ehrlich et al., 2011), our findings suggest that parenting practices are significant contributor to the level of discrepancy. We found that child perception of parent connection, knowledge, and respect is associated with a more congruent perspective on the child’s mental health status. Ehrlich et al. (2011) argue that families in which children’s decisions are respected, where there is a strong emotional bond between children and parents, and where parents have knowledge of their children’s friends and whereabouts, are families in which children and parents are more likely to have open communication. Again, this openness would be more likely to encourage a child to report his/her depressive symptoms to a parent/guardian, or to offer indirect/direct clues to a child’s emotional status. While replication is warranted, our findings suggest that professionals can recommend adoption of openness, knowledge, and respect for autonomy to parents regardless of ethnic background.
Several study limitations should be considered. The identity of the “parent” differed across children in the sample. Although almost 80 percent of adult participants were biological mothers, included among the sample were biological fathers, stepmothers, stepfathers, grandparents, foster parents, and siblings. Given that the quality of the relationship between a child and his/her caregiver might differ, depending upon the identity of the caregiver, the accuracy of the ‘parent’ rating may vary by the identity of the caregiver. Second, our assessment of parental depression is a history of depression and not a rating of current depressive symptoms. Future studies that compare parents with a history of depression to those with current depressive symptoms would improve our understanding of the role of parental depression in recognizing child emotional health status. Third, sample size of HA group was relatively small, which attenuated the power to detect discrepant reports. Future research is recommended with a larger sample of HA. Lastly, we did not know the immigration status of children and their family. Families from some groups are more likely to be immigrants, such that racial/ethnic differences might reflect either race/ethnicity per se or immigration status.
Findings from the current study confirm previous findings showing that: 1) children self-endorse more depressive symptoms than their parents endorse (Van Roy, Groholt, Heyerdahl, & Clench-Aas, 2010); and 2) parent-child informant discrepancies among AAs and ASAs are greater than among EAs (Lau et al., 2004). Clinicians should be attentive to the possibility of unrecognized and unreported child depression and suicidal ideation, particularly among parents from AA and ASA backgrounds. In addition, strategies and preventive interventions are needed to help all parents adopt parenting practices that enhance sensitivity and communication. These efforts could promote earlier identification of mental health problems for ethnic minority youth, particularly AA and ASA youth, which could lead to earlier utilization of mental health services.
Asian Americans reported the highest discrepancy in reporting of child depression.
Asian-, African-Americans reported significant discrepancy on suicide assessment.
Parents tended to under-reported child depression across all ethnic groups.
Parenting positively influenced on reporting discrepancy of child depression.
Acknowledgments
This research used data from the Developmental Pathways Project (DPP), which was funded by a grant from the National Institutes of Mental Health and Drug Abuse R01 MH63711, Drs. Ann Vander Stoep and Elizabeth McCauley (PIs). Authors thank the children and families who participated and the Seattle Public Schools for their collaboration during the recruitment process.
Footnotes
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
JaHun Kim, Email: kimj@seattleu.edu.
Ya-Fen Chan, Email: yfcuw@uw.edu.
Elizabeth McCauley, Email: eliz@uw.edu.
Ann Vander Stoep, Email: annv@uw.edu.
References
- Achenbach TM. Commentary: Definitely more than measurement error: but how should we understand and deal with informant discrepancies? Journal of Clinical Child and Adolescent Psychology. 2011;40:80–86. doi: 10.1080/15374416.2011.533416. [DOI] [PubMed] [Google Scholar]
- Ahmedani BK, Stewart C, Simon GE, Lynch F, Lu CY, Waitzfelder BE, … Williams K. Racial / Ethnic Differences in Health Care Visits Made Before Suicide Attempt Across the United States. Medical Care. 2015;53(5):430–435. doi: 10.1097/MLR.0000000000000335. org/10.1097/MLR.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Mood and Feelings Questionnaire (MFQ) Durham, NC: Duke University, Developmental Epidemiology Program; 1987. [Google Scholar]
- Banh MK, Crane PK, Rhew I, Gudmundsen G, Stoep A Vander, Lyon A, McCauley E. Measurement equivalence across racial/ethnic groups of the mood and feelings questionnaire for childhood depression. Journal of Abnormal Child Psychology. 2012;40:353–67. doi: 10.1007/s10802-011-9569-4. org/10.1007/s10802-011-9569-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Angold A. Scales to assess child and adolescent depression: Checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A. Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2011;40:1–9. doi: 10.1080/15374416.2011.533405. org/10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Ehrlich KB, Cassidy J, Dykas MJ. Reporter discrepancies among parents, adolescents, and peers: Adolescent attachment and informant depressive symptoms as explanatory factors. Child Development. 2011;82:999–1012. doi: 10.1111/j.1467-8624.2010.01530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung JJ, Lau AS. Factors associated with parent-child (dis)agreement on child behavior and parenting problems in Chinese immigrant families. Journal of Clinical Child and Adolescent Psychology. 2010;39:314–327. doi: 10.1080/15374411003691693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. The costs of depression. The Psychiatric Clinics of North America. 2012;35:1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E, Im H, Nahm E, Hong S. Korean American parents' reconstruction of immigrant parenting in the United States. Journal of Cultural Diversity. 2012;19(4):124–132. [PMC free article] [PubMed] [Google Scholar]
- Laird RD, Weems CF. The equivalence of regression models using difference scores and models using separate scores for each informant: Implications for the study of informant discrepancies. Psychological Assessment. 2011;23:388–397. doi: 10.1037/a0021926. [DOI] [PubMed] [Google Scholar]
- Lau AS, Garland AF, Yeh M, McCabe KM, Wood PA, Hough RL. Race/ethnicity and inter-informant agreement in assessing adolescent psychopathology. Journal of Emotional and Behavioral Disorders. 2004;12(3):145–156. [Google Scholar]
- Lewis KJ, Mars B, Lewis G, Rice F, Sellers R, Thapar AK, et al. Do parents know best? Parent-reported vs. child-reported depression symptoms as predictors of future child mood disorder in a high-risk sample. Journal of Affective Disorders. 2012;141:233–236. doi: 10.1016/j.jad.2012.03.008. [DOI] [PubMed] [Google Scholar]
- Merry SN, Stasiak K, Shepherd M, Frampton C, Fleming T, Lucassen MFG. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344:e2598–e2598. doi: 10.1136/bmj.e2598. org/10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordway MR. Depressed mothers as informants on child behavior: methodological issues. Research in Nursing & Health. 2011;34:520–32. doi: 10.1002/nur.20463. org/10.1002/nur.20463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel JS. Demography of immigrant youth: Past, present, and future. Future Child. 2011;21(1):19–41. doi: 10.1353/foc.2011.0001. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. A configurational analysis of children's reports of parent behavior. Journal of Consulting Psychology. 1965;29(6):552–557. doi: 10.1037/h0022702. [DOI] [PubMed] [Google Scholar]
- Schludermann E, Schludermann S. Replicability of factors in children's report of parent behavior (CRPBI) Journal of Psychology: Interdisciplinary and Applied. 1970;76(2):239–249. [Google Scholar]
- Su C, Hynie M. Effects of Life Stress, Social Support, and Cultural Norms on Parenting Styles Among Mainland Chinese, European Canadian, and Chinese Canadian Immigrant Mothers. Journal of Cross-Cultural Psychology. 2011;42:944–962. org/10.1177/0022022110381124. [Google Scholar]
- Van Roy B, Groholt B, Heyerdahl S, Clench-Aas J. Understanding discrepancies in parent-child reporting of emotional and behavioural problems: Effects of relational and socio-demographic factors. BMC Psychiatry. 2010;10:56. doi: 10.1186/1471-244X-10-56. org/10.1186/1471-244X-10-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The family history screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. yoa8214. [DOI] [PubMed] [Google Scholar]