Abstract
Objectives
In 2011, a consensus was reached defining “late presenters” (LPs) as individuals presenting for care with a CD4 count < 350 cells/μL or with an AIDS‐defining event, regardless of CD4 count. However, a transient low CD4 count is not uncommon in recent infections. The objective of this study was to investigate how measurements of late presentation change if the clinical stage at the time of diagnosis is taken into account.
Methods
Case surveillance data for newly diagnosed patients in Belgium in 1998–2012 were analysed, including CD4 count at diagnosis, the presence of AIDS‐defining events, and recent infections (< 6 months) as reported by clinicians in the case of acute illness or a recent negative test. First, proportions of LPs were calculated according to the consensus definition. Secondly, LPs were reclassified as “nonlate” if infections were reported as recent.
Results
A total of 7949 HIV diagnoses were included in the study. Recent infections were increasingly reported over time, accounting for 8.2% of new infections in 1998 and 37.5% in 2012. The consideration of clinical stage significantly modified the proportion of LPs: 18.2% of men who have sex with men (MSM) diagnosed in 2012 would be classified as LPs instead of 30.9% using the consensus definition (P < 0.001). The proportion of patients misclassified as LPs increased significantly over time: 5% in MSM in 1998 vs. 41% in 2012.
Conclusions
This study suggests that low CD4 counts in recent infections may lead to overestimation of late presentation when applying the consensus definition. The impact of transient CD4 count on late presentation estimates should be assessed and, if relevant, the introduction of clinical stage in the definition of late presentation should be considered.
Keywords: AIDS, consensus definition, HIV, late diagnosis, late presentation, men who have sex with men, testing
Introduction
In 2011, a consensus was reached defining “late presenters” (LPs) as individuals presenting for care with a CD4 count < 350 cells/μL or presenting with an AIDS‐defining event, regardless of CD4 count [1]. This consensus definition is broadly used in HIV surveillance to evaluate the prevalence and determinants of late presentation [2, 3, 4] and to assess the effectiveness of testing campaigns. At the European level, 47% of those diagnosed with HIV infection where information is available on CD4 count have a low count, < 350 cells/μL, at the time of diagnosis [5]. In Belgium, despite progress over the last 15 years, a considerable proportion (42%) of HIV diagnoses with information on CD4 count are still made “at a late stage” when the CD4 count has dropped below 350 cells/μL or when AIDS is diagnosed. In 2012, 31% of men who have sex with men (MSM) and 51% of heterosexuals diagnosed with HIV infection were classified as being diagnosed late.
However, looking only at CD4 count may lead to misclassification of late presentation. It has been shown that a transient low CD4 count is not uncommon in recent infections [6] and that early low CD4 counts may be predictive of fast disease progression [7]. Low CD4 counts during seroconversion were observed in various studies. The upper limit of the first quartile of the CD4 count was at 342 cells/μL in the CASCADE (Concerted Action on SeroConversion to AIDS and Death in Europe) cohort study, which included patients diagnosed within 6 months after seroconversion [7, 8, 9]. In a Brazilian study, the median CD4 count at presentation was 373 cells/μL [10]. In these cohorts, a significant proportion of patients in seroconversion (25 to 50%) would therefore have been considered as LPs according to the classical definition.
Late presentation is an essential indicator used to assess the effectiveness of prevention programmes and testing campaigns. This study aimed to determine how measurements of late presentation change when the clinical stage at the time of diagnosis is taken into account in order to elucidate how to more accurately interpret early CD4 cell counts and estimate the proportion of delayed diagnoses.
Methods
Case surveillance data for patients newly diagnosed with HIV infection in Belgium from 1998 to 2012 were analysed. These data included CD4 count at diagnosis, the presence of AIDS‐defining events and whether or not the HIV infection was considered as recent by the clinician. The criteria for a recent infection (< 6 months) included a recent negative test, a typical clinical presentation of acute infection and a history of recent risk behaviour with a known HIV‐positive partner. CD4 cell count data were available for 51% of the new diagnoses; the clinical stage was reported by clinicians for 67% of new diagnoses. First, proportions of LPs were calculated according to the classical definition using a CD4 count < 350 cells/μL or presentation with an AIDS‐defining event. Secondly, LPs were reclassified as “nonlate” if a recent infection was reported by clinicians. The reclassification was quantified and associated factors were identified using logistic regression.
Results
A total of 7949 HIV‐diagnosed individuals were included in the analysis, of whom 38.4% were Belgians, 43.2% sub‐Saharan Africans, 10.3% other Europeans and 8.2% of other nationalities. Sixty‐four per cent of individuals included were male, 54.4% were heterosexuals and 33.8% were MSM. The yearly number of new diagnoses reported as recent HIV infections increased by 700% between 1998 and 2012, accounting for 8.2% of new infections in 1998 and 37.5% in 2012. (Fig. 1). Among MSM, the proportion of infections reported as recent rose sharply and consistently, 56.3% of HIV diagnoses among MSM being recent infections in 2012. In contrast, the proportion of recent HIV infections in heterosexuals remained stable over the past decade, only 23.6% being reported as recent in 2012.
Figure 1.
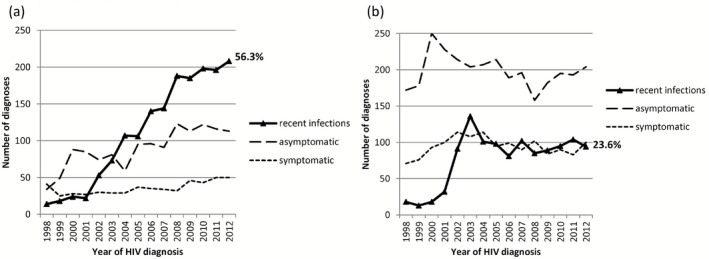
Clinical stage at HIV diagnosis in Belgium, in 1998–2012, in (a) men who have sex with men and (b) heterosexuals.
Among individuals with infections reported as recent, the median CD4 count was 457 cells/μL; 31.8% had a CD4 count < 350 cells/μL, which is close to the proportion observed in other cohorts of seroconverters [7, 8, 9, 10]. Furthermore, CD4 counts < 200 cells/μL were reported in 12.9% of recent infections.
A significant proportion of LPs according to the consensus definition were reclassified as non‐LPs when the clinical stage was taken into account. For the year 2012, only 33% of the new cases would have been considered as LPs instead of 42.4%. Among MSM, 18.2% of patients would have been considered as LPs instead of 30.9% (P < 0.001) (Fig. 2a). Among heterosexuals, the reclassification resulted in a limited and nonsignificant change in the percentage of LPs, from 51.3% to 44.5% for the year 2012 (Fig. 2b).
Figure 2.
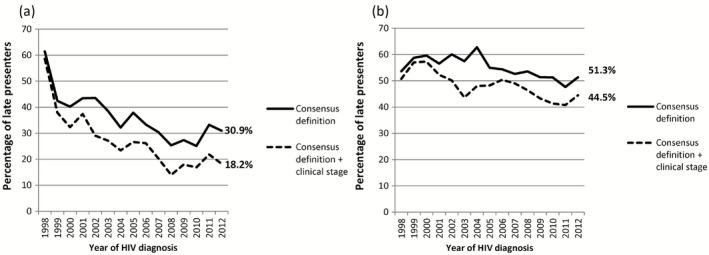
Reclassification of late presentation according to clinical stage in (a) men who have sex with men and (b) heterosexuals.
The reclassification was independently associated with younger age at diagnosis (P < 0.05), sex between men (P < 0.001), Belgian or other European nationality (P < 0.01) and later calendar year of diagnosis (P < 0.001). The strong association with year of diagnosis is reflected in an increasing proportion over time of patients falsely classified as LPs: among MSM, 5% of LPs were reclassified as non‐LPs in 1998 vs. 41% in 2012, meaning that the specificity of the classical definition of late presentation may have decreased over time.
Discussion
This study shows that taking into account the clinical stage at diagnosis significantly modifies the late presentation status assigned using the consensus definition and that the consensus definition for late presentation based only on CD4 count can overestimate the number of LPs. By excluding those with recent infections presenting a transient or early low CD4 count, this study aimed to more accurately identify patients whose diagnosis was delayed in time, whereas the consensus definition will rather identify patients presenting late from the point of view of evolving disease and its therapeutic implications.
This study has some limitations. First, we used routine surveillance data for all diagnosed HIV infections reported during a 15‐year period and, despite increasing comprehensiveness, a large proportion of CD4 count data at diagnosis are still missing in recent years (41% in 2013), which is slightly higher than the European Union (EU) average of 39% in 2013 [5]. This highlights the need to focus on improving epidemiological data collection to improve the completeness of CD4 count at diagnosis as well as data on clinical stage. Secondly, the validity of information on the recentness of the infection collected by the clinicians may be subject to subjectivity and recall bias. The validity of the criterion “recent risk behaviour with a known HIV‐positive partner”, which was not collected and analysed separately, may also be discussed. Nevertheless, the CD4 count distribution observed among the recent infections was comparable with what has been reported in other studies [7, 8, 9, 10]. Thirdly, specific tests for incidence analysis [enzyme‐linked immunosorbent assays (ELISAs) measuring antibody concentration or avidity] were not performed and results of other laboratory analyses to document the infection stage, for example using the Fiebig classification [11], were not available. Nor was analysis of subsequent CD4 counts possible because of the absence of data on antiviral treatment history.
The study shows a significant increase in recent infections among new diagnoses over the years, especially among MSM [12]; this trend may result from the screening campaigns implemented during the last decade. Taking into account the clinical stage data resulted in lower late presentation estimates. Nevertheless, even when corrected, late presentation levels remained too high. Late presentation to HIV testing and delays throughout the continuum of care have major consequences: increased morbidity and mortality, increased health costs, and increased opportunities for ongoing HIV transmission. The data provide strong support for campaigns to encourage early infection diagnosis and testing. The need for such campaigns was emphasized in the Belgian National HIV plan launched in October 2013 [13].
Late presentation is an essential indicator for monitoring prevention programmes, assessing the effectiveness of testing campaigns and allocating resources. This first study suggests that the possible drop in CD4 count in recent infections may lead to overestimation of late presentation when the common definition is applied, and that a proportion of LPs are possibly very early presenters, especially among MSM.
The presence of low and very low CD4 counts during the early phase of infection should be better known and quantified, and the impact of transient low CD4 counts and early low CD4 counts on LP estimates should be assessed. If relevant, the inclusion of clinical stage in the definition of late presentation should be considered in order to increase the specificity of the definition and provide a more reliable estimate of the proportion of delayed diagnoses.
Acknowledgements
We would like to acknowledge the AIDS Reference Laboratories and the AIDS Reference Centres for their collaboration in the collection of HIV surveillance data.
References
- 1. Antinori A, Coenen T, Costagiola D et al Late presentation of HIV infection: a consensus definition. HIV Med 2011; 12: 61–64. [DOI] [PubMed] [Google Scholar]
- 2. Johnson M, Sabin C, Girardi E. Definition and epidemiology of late presentation in Europe. Antivir Ther 2010; 15 (Suppl 1): 3–8. [DOI] [PubMed] [Google Scholar]
- 3. MacCarthy S, Bangsberg DR, Fink G, Reich M, Gruskin S. Late presentation to HIV/AIDS testing, treatment or continued care: clarifying the use of CD4 evaluation in the consensus definition. HIV Med 2014; 15: 130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zoufaly A, an der Heiden M, Marcus U et al Late presentation for HIV diagnosis and care in Germany. HIV Med 2012; 13: 172–181. [DOI] [PubMed] [Google Scholar]
- 5. European Centre for Disease Prevention and Control/WHO Regional Office for Europe . HIV/AIDS Surveillance in Europe 2013. Stockholm, European Centre for Disease Prevention and Control, 2014. [Google Scholar]
- 6. Pantaleo G, Graziosi C, Fauci AS. New concepts in the immunopathogenesis of human immunodeficiency virus infection. N Engl J Med 1993; 328: 327–335. [DOI] [PubMed] [Google Scholar]
- 7. Lodi S, Fisher M, Phillips A et al Symptomatic illness and low CD4 cell count at HIV seroconversion as markers of severe primary HIV infection. PLoS ONE 2013; 8: e78642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lodi S, Phillips A, Touloumi G et al CD4 decline in seroconverter and seroprevalent individuals in the precombination of antiretroviral therapy era. AIDS 2010; 24: 2697–2704. [DOI] [PubMed] [Google Scholar]
- 9. Lodi S, Phillips A, Touloumi G et al Time from human immunodeficiency virus seroconversion to reaching CD4+ cell count thresholds <200, <350, and <500 Cells/mm(3): assessment of need following changes in treatment guidelines. Clin Infect Dis 2011; 53: 817–825. [DOI] [PubMed] [Google Scholar]
- 10. Djomand G, Duerr A, Faulhaber JC et al Viral load and CD4 count dynamics after HIV‐1 seroconversion in homosexual and bisexual men in Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr 2006; 43: 401–404. [DOI] [PubMed] [Google Scholar]
- 11. Fiebig EW, Wright DJ, Rawal BD et al Dynamics of HIV viremia and antibody seroconversion in plasma donors: implications for diagnosis and staging of primary HIV infection. AIDS 2003; 17: 1871–1879. [DOI] [PubMed] [Google Scholar]
- 12. Sasse A, Defraye A. HIV infections and STI co‐infections in men who have sex with men in Belgium: sustained increase in HIV diagnoses. Euro Surveill 2009; 14. [DOI] [PubMed] [Google Scholar]
- 13. Federal Public Service Health, Food Chain Safety and Environment . Belgian Plan for action against HIV/AIDS – 2014–2019. October 16, 2013. Available at http://www.health.belgium.be/filestore/19089658_EN/HIV‐plan_ENG.pdf (accessed 29 May 2015).


