Abstract
Purpose
Age-related cognitivee decline is a growing public health concern worldwide. More than a quarter of adults with cognitive impairment experience sleep disturbance. The objective of this pilot study was to evaluate the preliminary effects of tai chi qigong (TCQ) on improving the night-time sleep quality of older adults with cognitive impairment.
Participants
Older adults with cognitive impairment who complain of sleep disturbance.
Methods
A randomized controlled trial with two groups. Fifty-two subjects were recruited from two district elderly community centers and randomly assigned to either the TCQ group (n=27) or the control group (n=25). The intervention group received TCQ training consisting of two 60-minute sessions each week for 2 months. The control group was advised to maintain their usual activities. Sleep quality was measured by the Chinese Pittsburgh Sleep Quality Index. Quality of life was measured by Short-form 12, cognitive functions measured by mini-mental state examination, and subjective memory deficits measured by the memory inventory for Chinese.
Results
Data were collected at baseline, 2 months, and 6 months. Significant results were noted at 6 months in the Chinese Pittsburgh Sleep Quality Index global score (P=0.004), sleep duration (P=0.003), habitual sleep efficiency (P=0.002), and the Short-form 12 mental health component (P<0.001). The TCQ participants reported better sleep quality and a better (quality of life) mental health component than the control group.
Conclusion
TCQ can be considered a useful nonpharmacological approach for improving sleep quality in older adults with cognitive impairment.
Clinical trial registration
CUHK_CCT00448 (https://www2.ccrb.cuhk.edu.hk/registry/public/287).
Keywords: cognitive decline, mind–body exercise, nonpharmacological approach, sleep disturbances
Introduction
Age-related cognitive decline is a growing public health concern worldwide. “Cognitive impairment” refers to reduced function in remembering, learning new things, concentrating or making decisions, and ranges from mild to severe. People with a mild version may demonstrate changes in their cognitive functions, but without affecting their daily activities. People with severe impairment may lose their ability to understand the meaning or importance of something and the ability to talk or write, rendering them unable to live independently – more than 16 million people in the US live with the condition.1 Five to eight out of every 100 people over 65 in Hong Kong suffer from dementia, while 20%–30% of those over 80 suffer from varying degrees of dementia.2
Sleep-related issues are the most frequent complaints among all noncognitive symptoms. More than a quarter of older adults with cognitive impairment experience sleep disturbance.3 Degenerative cognitive functions affect brain systems that are critical for regulation of the sleep-wake cycle.4 Frequent manifestations of sleep disturbance in people with cognitive impairment include day–night sleep pattern reversals: frequent night-time awakening and daytime sleep. Sleep disturbances also creates psychological, physical, and financial burdens for the older adults.4 Reducing nighttime sleep disturbance is therefore of great importance in clinical practice.
Conventional interventions to improve sleep consist primarily of pharmacological agents. However, medication may have negative side effects, including excessive daytime drowsiness, dizziness, cognitive disruptions, unsteadiness, and falls.5 The lack of pharmaceutical treatments for reversing age-related cognitive decline has led to a growing interest in low-cost behavioral interventions for improving cognition and sleeping patterns. It has been suggested that physical exercise may slow down decline in cognitive function.6 Increased daytime physical activities have also been recommended to improve the quality of night-time sleep.7,8 Although exercise may effectively maintain cognitive function and improve the night-time sleep of elderly people, many in the community who suffer from cognitive impairment are unable to exercise because of their low physical strength and medical condition.9 Exercise programs are therefore needed that are especially tailored to the reduced physical well-being and mental conditions.
The literature suggests that tai chi exercise may have beneficial effects by enhancing the sleep quality of healthy older adults.10,11 Tai chi is an increasingly popular mind–body form of exercise that incorporates physical, cognitive, social, and meditative components. It is a whole-body exercise that integrates breathing with harmonious movement of body training. It is designed to loosen the joints, promote deep, relaxed breathing, and cure many medical ailments. The tai chi movements are used to aid the Qi in its journey (meridians), dissolve blockages that can lead to sickness and disease, and increase general energy level. Tai chi includes training in sustained attention focusing and multitasking. The meditation component of tai chi may have direct benefits by enhancing attention and executive functions. Engaging in a group setting may have further benefits for cognition by improving mood and coping skills through social interaction and support. For conceptual and practical reasons, tai chi may be an effective intervention to slow cognitive impairment.12 However, the effects of tai chi on the sleep quality of older adults with cognitive impairment have rarely been investigated.
Prior studies suggest the potential benefits of tai chi to age-related decline as a result of pulmonary disease,13 Parkinson’s disease,14 problems concerned with balance,15 and psychological well-being.16 These studies suggest that tai chi is safe for older adults and an enjoyable activity, with potential for long-term adherence and exercise compliance. However, the lengthy sequential and complex tai chi movements are barriers to its use in people with cognitive impairment. But, tai chi in combination with qigong exercises may be a particularly suitable choice because tai chi qigong (TCQ) involves repetition of simple movements, which helps learning and retention, and avoids some participants being left behind. In addition, the mirroring of movements allows for constant visual feedback.17 The literature suggests using easy-to-follow, tai chi-like exercise rather than traditional tai chi practice for people with dementia.14 This pilot study therefore used simplified TCQ as an exercise aiming to investigate its preliminary effects on night-time sleep in older adults with cognitive impairment.
Objective
The objective of this pilot study is to estimate the preliminary effects of TCQ in enhancing sleep quality among older adults with cognitive impairment.
Methods
Subjects and settings
The subjects were recruited from district elderly community centers for the elderly operated by nongovernment organizations. These centers work in similar ways.
Inclusion criteria covered older adults who were 1) aged 60 years or above, 2) suffering from cognitive impairment with a mini-mental state examination (MMSE) score of 13–26 because those with scores lower than 13 would have difficulty in learning TCQ movements,18 and 3) suffering from sleep disturbance as defined by the Chinese Pittsburgh Sleep Quality Index (CPSQI), that is, with a score greater than 5.
Exclusion criteria covered older adults who 1) suffered from severely impaired ambulation or musculoskeletal problems that limited their ability to practice TCQ, 2) were receiving pharmacological treatment for their sleep disorder, and 3) had engaged in TCQ during the past 6 months.
Study design
This study was a single-blind, randomized controlled trial. The research assistants (RAs) responsible for data collection were blinded to group allocation of the subjects.
Sample size and randomization
For sample size estimation, a general rule of thumb is to take 30 participants or more to estimate a parameter in a pilot study.19 A total of 52 eligible subjects were recruited here. Subjects were randomly allocated to either the intervention (n=27) or the control group (n=25) by computer-generated random numbers. The grouping sequence list was password protected and stored on a computer. Only the authorized staff responsible for group allocation were allowed access to the list.
Interventions
TCQ group
The intervention group attended a 60-minute TCQ session twice a week for 2 months. The program included ten forms selected from the 18 TCQ movements. The ten were chosen by an experienced tai chi master to emphasize the elements of mind–body coordination. A TCQ expert had been consulted to examine the validity and feasibility of the simplified forms for use among older adults with cognitive impairment. The practice sessions were led by an experienced and qualified TCQ instructor, and the subjects replicated her motions, postures, and movement speed. The instructor also reviewed the skill mastery of the participants and rectified any incorrect performances. The number of participants in each session was limited to less than ten, which was considered manageable and feasible for teaching and learning. An RA was present during each class to monitor the consistency of participants’ practice by using a skill competence checklist. Attendance rates and any adverse events were also recorded.
The participants were encouraged to self-practice TCQ everyday. An audiovisual DVD and pictures of the ten forms, printed on a piece of A3-sized paper, were provided to all participants to help their self-practice and serve as an important reminder for participants to self-practice. To monitor compliance rates, a self-recording logbook was also given to the participants or their carers. The participants were asked to record the frequency and duration of their daily self-practice at home. The carers were also asked to assist the participants to record the logbook if needed.
Control group
Participants were advised to maintain their routine activities. To enhance the internal validity of the study findings, a weekly health talk in a community center was arranged for the control group over 2 months. These regular gatherings were organized to balance the emotional effect of the other group’s weekly gatherings during their TCQ training. The health talk program was delivered as a nonactive attention placebo, and no information relating to sleep and physical activity was included in these talks.
Outcome measurements
Primary outcome
Sleep quality
Sleep quality was measured by CPSQI, which is a self-reported questionnaire used to measure sleep quality and disturbance over a 1-month period. The index includes 19 individual items used to generate seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medication use, and daytime dysfunction. The seven component scores range from 0 to 3, and the global scores from 0 to 21, which can sensitively identify subjects with poor sleeping condition. Higher scores represent poorer subjective sleep quality. The CPSQI global score uses 5 as a cutoff value to indicate the presence of sleep disturbance. CPSQI has an overall reliability coefficient of 0.83, which indicates its high internal consistency.20
Secondary outcomes
Short-form 12 health survey (SF-12v2)
The SF-12v2 Health Survey is a popular generic health-related quality of life measure. The 12-item questionnaire measures functional health and well-being from the perspective of the participant and contains eight subscales, which were transformed into 0–100, with higher scores indicating better mental and physical health. The Hong Kong Chinese version of SF-12v2 has favorable internal consistency and test–retest reliabilities (from 0.67 to 0.82).21
MMSE questionnaire
MMSE is a frequently used instrument for assessing the cognitive functions of dementia patients. It is divided into two sessions in which the first requires oral responses and covers orientation, memory, and attention, while the second tests the ability of subjects to name objects as well as follow verbal and written commands. The maximum score is 30. The internal consistency of the Chinese MMSE has been validated with a Cronbach’s alpha of 0.86, and its excellent inter-rater reliability validated, with an intra-class correlation of 0.99. Scores of 27 or above (out of 30) are considered normal.22
Memory inventory for Chinese questionnaire
Memory inventory for Chinese (MIC) is used for assessing the awareness of memory deficits in a Chinese population. The questionnaire includes 27 items with scores ranging from 0 to 108. A higher score indicates a higher risk of memory deficits. The Cronbach’s alpha values for the patient and caregiver are 0.89 and 0.90, respectively, while the intra-class correlations for the patient and caregiver scores are 0.96 and 0.98, respectively.23
Ethical considerations
Ethics approval was obtained from the Joint Clinical Research Ethics Committee of the Chinese University of Hong Kong and New Territory East Cluster. Permission to conduct this study in the selected community centers was also obtained, as was informed consent from eligible participants or their guardians. The consenting algorithm, developed according to the legal and ethical principles listed in the Mental Capacity Act for obtaining consent from people with mental incapacity, was adopted for those older adults with cognitive impairment.24 If the participant failed at any stage of the algorithm, he or she could continue to participate if his or her assent was given (ie, agreed to join the study) and the guardian gave proxy consent.24
Data collection
To minimize researcher bias, the RAs responsible for data collection were blinded to the study. They attended a briefing session where the procedures were explained. Demographic data and baseline measurements were collected at the beginning of the study (T0). Postintervention data were collected at 2 months (T1) and 6 months (T2) after the study began.
Baseline assessment started with an interview. If the participant was unable to provide a reliable sleep history, the RA would also talk to family members or caregivers to obtain thorough and reliable information on the medical history, sleep habits, history of sleep problems, and any medications or other substances used to promote sleep, such as alcohol. This approach was also applied in the postintervention at 2 months and follow-up assessment at 6 months. As the participants were cognitive impaired, all the questionnaires were administered by the RAs through individual interviews. If the participants were unable to provide reliable answers, the RAs would talk to their family members or caregivers to obtain thorough and reliable information.
Data analysis
Baseline characteristics were summarized and presented using appropriate descriptive statistics. Normality of continuous variables was assessed using skewness statistics and normal probability plots. The MIC score was square root-transformed before being entered into analysis. Baseline characteristics of TCQ and control groups were compared using independent t, chi-square, or Fisher’s exact tests, as appropriate. The above statistical tests were also used to compare baseline characteristics of the participants who completed the study and with those who did not.
All primary and secondary outcomes were compared between the intervention and control groups on the basis of the intention-to-treat principle. The intention-to-treat population consisted of all randomized patients according to their allocated treatments. In view of the unbalanced sex distribution and baseline age difference between the two groups, a generalized estimating equation (GEE) model was used to assess differential change in each of the primary and secondary outcomes across the time points (T0: the baseline; T1: 2 months, postintervention; and T2: 6-month follow-up) between the two groups with adjustment for sex and age in order to obtain more precise estimates of the intervention effects. A dummy variable (group) was assigned to represent the intervention group with the control group as reference. Another two dummy variables (T1 and T2) were set to correspond to the two follow-up time points (T1 and T2) with the baseline (T0) as the reference. The interaction terms of the time point dummy variables and group were included in the GEE models to assess the differential change of the outcomes relative to the baseline between the two groups at each postintervention time point. The GEE model can account for intra-correlated repeated measures data and accommodate missing data caused by dropouts, provided the data are missing at random,25 and thus is particularly suitable for intention-to-treat analysis, without the need for imputation of missing data. In addition, this model can be used for outcome variables of various kinds of distributions with the use of appropriate link function. In particular, for normally distributed outcome data, including CPSQI total score, MMSE, square root-transformed MIC score, and physical component score and mental health component score of the SF-12, the identity link function was used in the GEE models, that is, no further transformation on the outcome data was made. For the ordinal data of the CPSQI component scores, ordinal logistic link function that assumes proportional odds across the ordered categories of each of the CPSQI component score was used. Sensitive analysis was conducted to assess the robustness of the statistical results. Specifically, repeated measures analysis of variance was performed for each of the continuous outcomes by including participants with complete data at both T0 and T1 only as well as both T0 and T2 only. All statistical analyses were performed using IBM SPSS 22.0 (IBM Corporation, Armonk, NY, USA). All statistical tests were two-sided and a P-value <0.05 was considered statistically significant.
Results
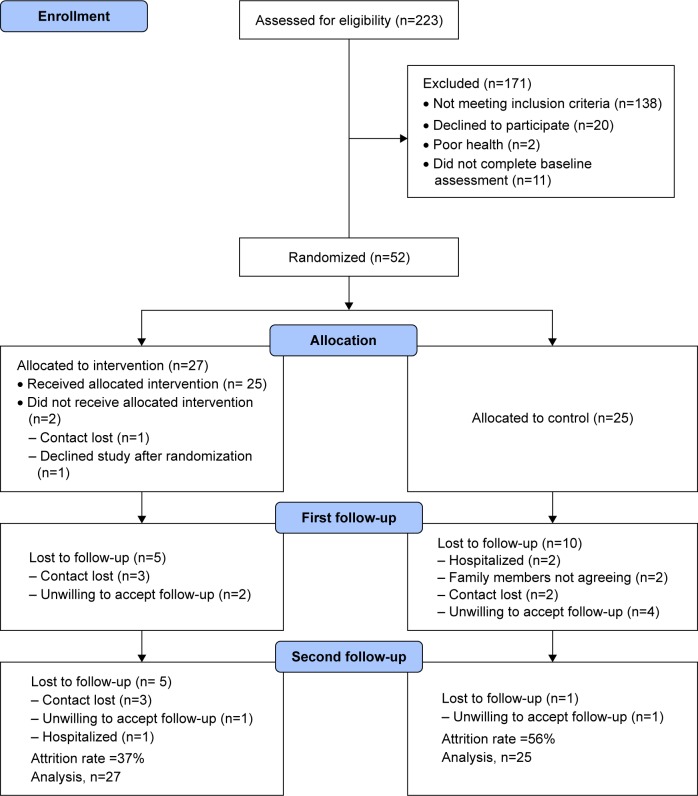
An initial pool of 223 older adults was assessed for eligibility. A total of 160 did not fulfill the inclusion criteria (Figure 1) and could not be accepted, while eleven did not complete the baseline assessment. A total of 52 subjects were recruited and randomly assigned to TCQ (n=27) or control group (n=25). Their ages ranged from 62 to 97, with a mean age of 80.6 (standard deviation =7.12). Their MMSE scores ranged from 15 to 26, with a mean score of 23.1 (standard deviation =3.2). Of these 52 subjects, 44 (85%) were female and eight (15%) male. We found no significant difference in demographic data between the two groups except in sex (P<0.001), as no male was in the TCQ group (Table 1). Of the 52, 31 (17 in TCQ, 14 in control) completed the study. The main reasons for attrition were loss of contact, unwillingness to follow-up, and admission to hospital. No significant difference was found in demographic data or baseline characteristics of those who completed the study and those who did not.
Figure 1.
Flowchart to track participants through a randomized controlled trial.
Table 1.
Baseline characteristics of the participants (n=52)
| Characteristics | Control (n=25) | Tai chi (n=27) | P-value# |
|---|---|---|---|
| Age (years)* | 82.2 (6.7) | 78.4 (7.1) | 0.051 |
| Sex | |||
| Male | 8 (32.0%) | 0 (0.0%) | 0.001ψ |
| Female | 17 (68.0%) | 27 (100.0%) | |
| Marital status | |||
| Single/divorced/separated/widowed | 17 (68.0%) | 19 (70.4%) | 0.853 |
| Married | 8 (32.0%) | 8 (29.6%) | |
| Educational level | |||
| No formal education | 11 (44.0%) | 9 (33.3%) | 0.477ψ |
| Primary school | 11 (44.0%) | 11 (40.7%) | |
| Secondary school or above | 3 (12.0%) | 7 (25.9%) | |
| Living alone | |||
| No | 16 (64.0%) | 16 (59.3%) | 0.726 |
| Yes | 9 (36.0%) | 11 (40.7%) | |
| Religion | |||
| No | 10 (40.0%) | 14 (51.9%) | 0.392 |
| Yes | 15 (60.0%) | 13 (48.1%) | |
| Smoking habits | |||
| Never smoke | 22 (88.0%) | 27 (100.0%) | 0.104ψ |
| Exsmoker | 1 (4.0%) | 0 (0.0%) | |
| Current smoker | 2 (8.0%) | 0 (0.0%) | |
| History of hypertension | |||
| No | 9 (36.0%) | 7 (25.9%) | 0.432 |
| Yes | 16 (64.0%) | 20 (74.1%) | |
| History of diabetes | |||
| No | 21 (84.0%) | 21 (77.8%) | 0.729ψ |
| Yes | 4 (16.0%) | 6 (22.2%) | |
| History of cardiac disease | |||
| No | 18 (72.0%) | 21 (77.8%) | 0.631 |
| Yes | 7 (28.0%) | 6 (22.2%) | |
| Weekly exercise, duration in hours* | 3.9 (3.0) | 4.7 (3.0) | 0.370 |
Notes: Data marked with
is presented as mean (standard deviation), otherwise as frequency (%).
Categorical and continuous variables were compared between the two groups using Pearson’s chi-square test and t-test, respectively; those marked with
used Fisher’s exact test.
The average attendance rate at the TCQ classes was 70% (ranged from 57% to 100%). Reasons for not attending included medical follow-up, forgetfulness, or illness. Subjects’ mastery of TCQ skills was assessed by the instructor at the end of the program. The majority of the TCQ participants (88%) were able to master the skills at the end of the program. Subgroup analysis of mild or moderate cognitive impairment was not performed because of the small cell size (eight subjects had an MMSE score <18).
Primary outcomes
The primary outcome measures were CPSQI global score and its seven component scores over 6 months. At 2 months, immediately after completing the training class, an improving trend was observed in the TCQ participants’ CPSQI global score and the seven component subscales, except sleep medication use, although these did not reach statistical significance.
The intervention effects estimated by GEE models with adjustment for age and sex are presented in Table 2. Ordinal logistic link function was used to accommodate ordinal outcomes of the component subscales of CPSQI in the GEE analysis, whereas identity link function was used for all other outcomes. Significant time by group interactions were found at 6 months in CPSQI global scores (P=0.004; Figure 2) and two subscales, sleep duration (P=0.004) and habitual sleep efficiency (P=0. 002). TCQ participants reported improvements in sleep duration (+48 minutes) and efficiency (+9. 1%). No statistical difference was observed between the two study groups in subjective sleep quality, sleep latency, sleep disturbance, use of sleep medication, and daytime dysfunction.
Table 2.
GEE models for the comparison of primary and secondary outcomes across time between control and tai chi qigong groups
| Outcomes | Regression coefficients of the GEE models
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group
|
T1
|
T2
|
Group by T1
|
Group by T2
|
||||||
| B (95% CI) | P-value | B (95% CI) | P-value | B (95% CI) | P-value | B (95% CI) | P-value | B (95% CI) | P-value | |
| Sleep quality (CPSQI) | ||||||||||
| CPSQI total score (range: 0–21) | 0.97 (−0.86, 2.80) | 0.300 | −0.23 (−1.74, 1.28) | 0.764 | 0.13 (−1.23, 1.49) | 0.854 | −1.37 (−3.19, 0.44) | 0.138 | −2.67 (−4.51, −0.83) | 0.004 |
| CPSQI componentsψ | ||||||||||
| Subjective sleep quality (range: 0–3) | 0.40 (−0.75, 1.55) | 0.493 | 0.00 (−1.39, 1.38) | 0.996 | −0.06 (−1.19, 1.08) | 0.924 | −0.36 (−1.97, 1.25) | 0.660 | −0.55 (−2.08, 0.99) | 0.487 |
| Sleep latency (range: 0–3) | −0.10 (−1.29, 1.09) | 0.869 | −1.03 (−2.12, 0.05) | 0.062 | 0.07 (−0.92, 1.07) | 0.884 | 1.13 (−0.21, 2.47) | 0.097 | −0.66 (−1.99, 0.67) | 0.330 |
| Sleep duration (range: 0–3) | 1.16 (0.09, 2.23) | 0.034 | 0.71 (−0.39, 1.81) | 0.205 | 1.11 (−0.31, 2.53) | 0.126 | −1.89 (−3.29, −0.49) | 0.008 | −2.69 (−4.53, −0.84) | 0.004 |
| Habitual sleep efficiency (range: 0–3) | 0.95 (−0.10, 2.01) | 0.075 | 0.08 (−1.00, 1.15) | 0.891 | 0.78 (−0.38, 1.94) | 0.190 | −1.15 (−2.51, 0.21) | 0.096 | −2.58 (−4.24, −0.91) | 0.002 |
| Sleep disturbance (range: 0–3) | 0.32 (−0.94, 1.58) | 0.615 | −0.48 (−1.64, 0.67) | 0.411 | −1.50 (−2.67, −0.33) | 0.012 | −1.38 (−2.97, 0.21) | 0.089 | 0.31 (−1.09, 1.70) | 0.669 |
| Use of sleeping medication (range: 0–3)# | – | – | – | – | – | – | – | – | – | – |
| Daytime dysfunction (range: 0–3) | −0.17 (−1.33, 0.99) | 0.772 | 0.37 (−0.79, 1.53) | 0.533 | −1.17 (−2.33, 0.00) | 0.050 | −0.77 (−2.36, 0.82) | 0.342 | 0.80 (−0.75, 2.36) | 0.310 |
| Cognitive functions | ||||||||||
| MMSE (range: 0–30) | 0.94 (−0.72, 2.60) | 0.268 | 1.79 (0.54, 3.04) | 0.005 | 2.36 (1.20, 3.52) | <0.001 | −0.75 (−2.46, 0.97) | 0.394 | −1.00 (−2.60, 0.59) | 0.219 |
| MIC (range: 0–108)* | 0.11 (−1.06, 1.28) | 0.854 | 0.45 (−0.29, 1.18) | 0.231 | −0.02 (−0.75, 0.72) | 0.965 | −0.82 (−1.72, 0.08) | 0.074 | −0.34 (−1.30, 0.62) | 0.486 |
| Health-related quality of life (SF-12) | ||||||||||
| PCS | 9.20 (1.77, 16.62) | 0.015 | 1.39 (−3.22, 6.00) | 0.555 | 3.92 (−0.08, 7.91) | 0.055 | −3.66 (−9.42, 2.09) | 0.212 | −2.91 (−8.93, 3.11) | 0.343 |
| MCS | −4.49 (−9.53, 0.55) | 0.081 | −6.04 (−10.20, −1.88) | 0.004 | −0.78 (−5.19, 3.62) | 0.727 | 11.53 (6.68, 16.39) | <0.001 | 0.70 (−6.18, 7.58) | 0.842 |
Notes: Only the model estimates of regression coefficients (B) of the dummy variables for the group (group: 0= control [reference]; 1= [tai chi]), time points (T1 and T2 with the baseline [T0] as reference), time points and group interaction terms (group by T1 and group by T2) are shown for the GEE models.
The CPSQI component scores were all treated as ordinal data, and the ordinal logistic link function was used in the GEE models, the coefficients reported were in log-odds ratios.
Square root-transformed before being entered into the GEE model.
The GEE analysis was not performed for this variable owing to sparseness of data other than 0. Effect sizes: CPSQI (T2 vs T0), Cohen’s d=0.70; CPSQI – Sleep duration component (T1 vs T0), odds ratio=6.6; CPSQI – Sleep duration component (T2 vs T0), odds ratio=14.7; CPSQI – Habitual sleep efficiency (T2 vs T0), odds ratio=13.2.
Abbreviations: CI, confidence interval; CPSQI, Chinese Pittsburgh sleep quality index; GEE, generalized estimating equation; MIC, memory inventory for Chinese; MCS, mental health component score; MMSE, mini-mental state examination; PCS, physical component score; SF-12, Short-form 12.
Figure 2.
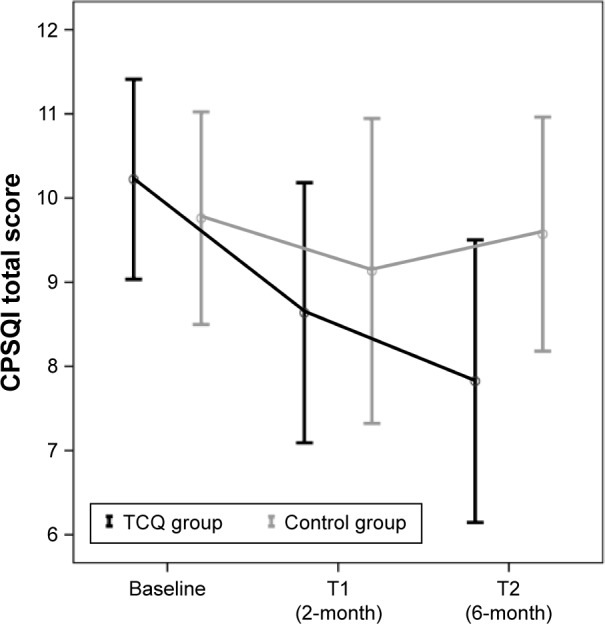
CPSQI score across time between control and TCQ groups.
Abbreviations: CPSQI, Chinese Pittsburgh sleep quality index; TCQ, tai chi qigong.
The effect size, Cohen’s d,26 of CPSQI global score (T2 vs T0) was d=0.70, indicating a medium to large effect size. For the sleep duration component, participants in the TCQ group had 6.6 and 14.7 times in increased odds to get a lower value in the component score from T0 to T1 and T0 to T2, respectively, than those on the control group; odds ratios (T1 vs T0) =6.6 and odds ratio (T2 vs T0) =14.7. For habitual sleep efficiency (T2 vs T0), odds ratio =13.2, TCQ participants were more likely than those in the control group to score a lower value in the component score at T2 compared with T0. By repeated measures analysis of variance, significant time by group interaction was also found at 6 months in CPSQI global score (P=0.011).
Secondary outcomes
The intervention effects on secondary outcomes are presented in the lower portion of Table 2. TCQ participants recorded significant improvement in their SF-12 mental health component scores (P<0.001) at 2 months, but no difference was observed at 6 months.
No significant difference was noted in the SF-12 physical component, MMSE score, or MIC score between the two groups. Similar results were also obtained by repeated measures analysis of variance; only mental health component score was found as a significant improvement in the TCQ group comparing with the control group at 2 months (time by group interaction P<0.001).
Regarding self-practice monitoring, only a third of the participants returned the self-recorded logbook. Their records indicated they had self-practiced TCQ at home for around 30 minutes each day. Participants who did not return the logbook also claimed that they had practiced daily but forgot to record the frequency. As the return rate of the logbook was low, we could not obtain a reliable self-compliance result for analysis.
In the program evaluation, subjects said they had enjoyed the TCQ training, and the majority (82%) said they would continue practicing after the program. They expressed a wish to extend the program to 3 months, and the class time to 1.5 hours per session. No adverse effects were reported from the TCQ classes indicating it was a safe form of exercise for this population group.
Discussion
This pilot study examined the feasibility and preliminary effects of TCQ exercise on the primary outcome of self-reported sleep quality in a randomized controlled trial of older adults with cognitive impairment. The participants reported an overall CPSQI score of more than 5 at baseline, which met the criteria for disturbed sleep.20
The major findings of the study were that older adults with cognitive impairment and sleep disturbance benefited from TCQ exercise in the areas of sleep duration, sleep efficiency, and the mental health component of quality of life. Compared with the control group, the TCQ participants achieved an improved sleep quality, as measured by the CPSQI global score, which was evident at 6 months. In the TCQ group, the findings were particularly clear in the case of sleep duration (increased by 48 minutes) and habitual sleep efficiency (increased by 9.1%). These results are generally congruent with other study findings10,11 showing that a 2-month TCQ intervention is able to increase sleep duration and efficiency.
No change was observed in the use of sleep medication. This was due to our exclusion of those taking sleep medications. Although no statistical change was noted for measures of subjective sleep quality, sleep latency, sleep disturbances, and daytime dysfunction, they were all in fact on an improving trend.
The study also found a concomitant change in quality of life measures. Compared with the control group, TCQ participants showed significant improvements in their SF-12 mental health component scores, which was possibly attributable to the fact that the TCQ program offered participants the opportunity for social interaction and companionship, which are expected to have a positive effect on mental well-being. This also explains the insignificant results at 6 months, as there was no more group practice after 2 months.
The underlying mechanism of the relationship between exercise and sleep has been explored in various studies,7,27,28 but the underlying relationship between TCQ and sleep requires further investigation. Previous literature shows that tai chi can be classified as moderate exercise, as its intensity does not exceed 55% of maximal oxygen intake.29 It is thought that exercise may improve sleep, body restoration, and energy conservation. Greater energy expenditure during the day is thought to require greater rest at night.30 However, Irwin et al10 argue that the physical energy expenditure of tai chi exercise does not change, improvements in sleep appearing to be independent of the energy expended during tai chi. A study by Chao et al31 shows that the average exercise intensity of TCQ is 3.1 MET (metabolic equivalent). This is a low intensity exercise. It is believed that the slow gentle movements, deep diaphragmatic breathing, and relaxation of TCQ may enhance feelings of well-being and alter the mental state, which may possibly lead to improved sleep quality.10,11
The self-practice compliance rate could not be assessed in this study – participants were elderly with cognitive impairment and so might have forgotten to record the frequency of practice because of memory failings.32,33 Future studies may therefore consider engaging community elderly centers as collaborators. This might be beneficial because center staff can mobilize the structure and resources of the center to support the interventions, for example, ensuring that there is a structured TCQ practice time on the schedule. The number of participants self-practicing at the center could be recorded. Furthermore, the likelihood of the intervention being sustained after the trial is over will be greater if the center staff members are engaged from the start of the project.
Limitations
This pilot study has several limitations. First, the small sample size may decrease the statistical power and have a reduced chance of detecting a true effect. Therefore, these findings must be interpreted with caution as they may not be generalizable to a larger population. Second, the excessive attrition rate recorded in the control group at 2 months could affect the sample’s representativeness. Future studies should plan attractive placebo activities in the standard-care control group in order to retain participants and minimize attrition. Third, the short intervention period may limit the level of skill mastery in older adults with cognitive impairment. The small improvement shown in the CPSQI component subscales might increase over a longer training period. The last limitation concerns the imbalance of the sexes, the result of the predominance of females attending community centers. A future study should recruit even number of males and females so that sex differences in the intervention’s effects can be evaluated.
Conclusion
This study addresses the high prevalence of sleep disturbance among older adults with cognitive impairment. Results from the study show preliminary evidence linking the benefits of TCQ exercise to decreased sleep disturbances. As a low intensity exercise, TCQ is an appropriate intervention for older adults with cognitive impairment.
Its potential benefits in enhancing sleep quality and the mental health component of quality of life need a full-scale randomized controlled trial to reveal its empirical effects.
Acknowledgments
This study is funded by the School Seeding Fund, the Nethersole School of Nursing, and the Chinese University of Hong Kong. Acknowledgments are extended to the St James Settlement Elderly Center and the Christian Family Service Centre for persistently supporting the subject recruitment and implementation of the trial.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Centers for Disease Control and Prevention Cognitive Impairment: A Call for Action, Now! [Accessed February 10, 2015]. Available from: http://www.cdc.gov/aging/pdf/cognitive_impairment/cogimp_poilicy_final.pdf. [Updated February 2011]
- 2.Hospital Authority Dementia. [Accessed February 10, 2015]. Available from: http://www21.ha.org.hk/smartpatient/en/chronicdiseases_zone/details.html?id=174. [Updated 2 February 2015]
- 3.Rose KM, Lorenz R. Sleep disturbances in dementia. J Gerontol Nurs. 2010;36(5):9–14. doi: 10.3928/00989134-20100330-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth HL. Dementia and sleep. Neurol Clin. 2012;30(4):1213–1248. doi: 10.1016/j.ncl.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000;162(2):225–233. [PMC free article] [PubMed] [Google Scholar]
- 6.Miller SM, Taylor-Piliae RE. Effects of tai chi on cognitive function in community-dwelling older adults: a review. Geriatr Nurs. 2014;35(1):9–19. doi: 10.1016/j.gerinurse.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Varrasse M, Li J, Gooneratne N. Exercise and sleep in community-dwelling older adults. Curr Sleep Med Rep. 2015;1(4):232–240. doi: 10.1007/s40675-015-0028-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartescu I, Morgan K, Stevinson CD. Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: a randomized controlled trial. J Sleep Res. 2015;24(5):526–534. doi: 10.1111/jsr.12297. [DOI] [PubMed] [Google Scholar]
- 9.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 10.Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of tai chi chih. Sleep. 2008;31(7):1001. [PMC free article] [PubMed] [Google Scholar]
- 11.Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. 2004;52(6):892–900. doi: 10.1111/j.1532-5415.2004.52255.x. [DOI] [PubMed] [Google Scholar]
- 12.Lam L, Chan W, Kwok T, Chiu H. Effectiveness of tai chi in maintenance of cognitive and functional abilities in mild cognitive impairment: a randomised controlled trial. Hong Kong Med J. 2014;20(3 Supplement 3):20–23. [PubMed] [Google Scholar]
- 13.Chan AW, Lee A, Lee DT, et al. The sustaining effects of tai chi qigong on physiological health for COPD patients: a randomized controlled trial. Complement Ther Med. 2013;21(6):585–594. doi: 10.1016/j.ctim.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Klein PJ. Tai chi chuan in the management of Parkinson’s disease and Alzheimer’s disease. Med Sport Sci. 2008;52:173–181. doi: 10.1159/000134298. [DOI] [PubMed] [Google Scholar]
- 15.Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of tai chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36(3):262–268. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 16.Chan AW, Lee A, Lee DT, Sit JW, Chair SY. Evaluation of the sustaining effects of tai chi qigong in the sixth month in promoting psychosocial health in COPD patients: a single-blind, randomized controlled trial. Scientific World Journal. 2013;2013:1–11. doi: 10.1155/2013/425082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tadros G, Ormerod S, Dobson-Smyth P, et al. The management of behavioural and psychological symptoms of dementia in residential homes: does tai chi have any role for people with dementia? Dementia (London) 2013;12(2):268–279. doi: 10.1177/1471301211422769. [DOI] [PubMed] [Google Scholar]
- 18.Yao L, Giordani BJ, Algase DL, You M, Alexander NB. Fall risk-relevant functional mobility outcomes in dementia following dyadic tai chi exercise. West J Nurs Res. 2013;35(3):281–296. doi: 10.1177/0193945912443319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Browne RH. On the use of a pilot sample for sample size determination. Stat Med. 1995;14(17):1933–1940. doi: 10.1002/sim.4780141709. [DOI] [PubMed] [Google Scholar]
- 20.Tsai P, Wang S, Wang M, et al. Psychometric evaluation of the Chinese version of the Pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(8):1943–1952. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 21.Lam ET, Lam CL, Fong DY, Huang WW. Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J Eval Clin Pract. 2013;19(1):200–208. doi: 10.1111/j.1365-2753.2011.01800.x. [DOI] [PubMed] [Google Scholar]
- 22.Chiu HF, Lee H, Chung W, Kwong P. Reliability and validity of the Cantonese version of mini-mental state examination-a preliminary study. J Hong Kong College of Psychiatrists. 1994;4(Suppl 2):25–28. [Google Scholar]
- 23.Cheong Lui VW, Lam W, Chiu L, Chiu K, Fung H. Validation of a memory inventory for the assessment of awareness of memory deficits in Alzheimer’s disease in Chinese elderly. Int J Geriatr Psychiatry. 2006;21(10):917–923. doi: 10.1002/gps.1580. [DOI] [PubMed] [Google Scholar]
- 24.Warner J, McCarney R, Griffin M, Hill K, Fisher P. Participation in dementia research: rates and correlates of capacity to give informed consent. J Med Ethics. 2008;34(3):167–170. doi: 10.1136/jme.2006.019786. [DOI] [PubMed] [Google Scholar]
- 25.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford university press; 2003. [Google Scholar]
- 26.Rosenthal R, Cooper H, Hedges L. Parametric measures of effect size. In: Copper H, Hedges LV, editors. The Handbook of Research Synthesis. New York: Sage; 1994. pp. 231–244. [Google Scholar]
- 27.Passos GS, Poyares DLR, Santana MG, Tufik S, Mello MTd. Is exercise an alternative treatment for chronic insomnia? Clinics. 2012;67(6):653–660. doi: 10.6061/clinics/2012(06)17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santos R, Viana V, Boscolo R, et al. Moderate exercise training modulates cytokine profile and sleep in elderly people. Cytokine. 2012;60(3):731–735. doi: 10.1016/j.cyto.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 29.Li JX, Hong Y, Chan KM. Tai chi: physiological characteristics and beneficial effects on health. Br J Sports Med. 2001;35(3):148–156. doi: 10.1136/bjsm.35.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Montgomery P, Dennis J. Physical exercise for sleep problems in adults aged 60. Cochrane Database Syst Rev. 2002;4(4):CD003404. doi: 10.1002/14651858.CD003404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chao YC, Chen S, Lan C, Lai J. The cardiorespiratory response and energy expenditure of tai-chi-qui-gong. Am J Chin Med. 2002;30(4):451–461. doi: 10.1142/S0192415X02000636. [DOI] [PubMed] [Google Scholar]
- 32.Chan D. So why ask me? are self-report data really that bad. In: Lance E, Vandenberg RJ, editors. Statistical and Methodological Myths and Urban Legends: Doctrine, Verity and Fable in the Organizational and Social Sciences. New York: Routledge/Taylor & Francis Group; 2009. pp. 309–336. [Google Scholar]
- 33.Dobbels F, Berben L, De Geest S, et al. The psychometric properties and practicability of self-report instruments to identify medication nonadherence in adult transplant patients: a systematic review. Transplantation. 2010;90(2):205–219. doi: 10.1097/TP.0b013e3181e346cd. [DOI] [PubMed] [Google Scholar]