Abstract
Introduction:
Severe defects in long bones can be caused by several factors such as trauma that lead to open wound and secondary infections after surgery. Induced membrane technique is one of the therapeutic strategies that can be used for these patients. Due to importance of this method and lack of information about this technique in Iran.
Aim:
this study was performed to investigate technical strengths and weakness of induced membrane technique.
Material and Methods:
This case series study conducted on 21 patients with bone defects in the femur and tibia and metatarsal bones referred to orthopedic clinic of Rasoul Akram Hospital, Tehran, Iran, for induced membrane surgery in 2012-2015. Demographic and clinical data were obtained using history, clinical examinations and observations for each patient. Union achievement was the main outcome of this study, which was confirmed by radiographic findings and physical examination. Obtained data was analyzed by SPSS ver. 16.
Results:
All patients were male except one and their mean age was 30.52 years old. Bone defects were in tibia, femur and metatarsus in 9, 9 and 3 patients, respectively. Three patients received soft tissue reconstruction with flap before induced membrane surgery. Age, defects size, cigarette addiction and drug use and delay to start the treatment had no significant effect on union status. In total, 90% of patients had successful surgery.
Conclusion:
using induced membrane technique in patients with defects in their long bone such as tibia, femur and metatarsus would lead to high success for reconstruction.
Keywords: induced membrane technique, union, tibia, femur, metatarsus
1. INTRODUCTION
Severe defects and loss of long bones such as tibia, femur and metatarsus can be caused by various factors, the most common among which is trauma that can lead to open wound. Loss of body parts or joints can be caused by both primary damages and secondary infections after surgery. Hematogenous osteomyelitis, bone tumors and failed arthroplasty can be mentioned as other causes (1, 2). Less common causes including congenital malformations, congenital shortening and various kind of pseudarthrosis are challenging cases for bone defect treatment (1). In all these cases, the ultimate goal of treatment would be appropriate direction, restoration of limb length and achieving the union. In the meantime, due to factors such as less damage to the surrounding soft tissues, reduction of required time and tolerable treatment type for patient is also important.
Balance between beauty and performance aspects of the body provides different treatment strategies according to the type of damaged limb. The simplest approach to reconstruction of bone defects would be shortening or amputation at different levels (1, 2). The other method is reviving the length of affected limb and induced membrane technique is one of the latest methods for bones with defect due to infections.
Induced membrane technique was first introduced in 1986 by Masquelet et al. and considered as an effective treatment for bone lesions up to 25 cm. Overall, previous infection or radiation is not an inhibition for this procedure if complete soft tissue coverage and suitable vessels are present prior to bone grafting stage (3-5). Several studies in animals and clinical trials have been performed to detect strengths and weaknesses of this technique (6-8).
This reconstruction technique requires a two-stage surgery. The first stage surgery includes complete debridement, soft tissue reconstruction by required flap and inserting the polymethyl methacrylate (PMMA) cement in defected place of bone. The second stage would be performed about 8 weeks after the first surgery when the soft tissue is healed completely, the secretion is interrupted, and the laboratory markers (ESR, CRP) are returned to normal. At this stage, the cement would be pulled out, but pseudomembrane would be retained. Then, the empty space would be filled by an iliac crest split bone graft (9-11).
In early phases of bone defect, especially in infectious cases, the cement is used as a spacer to prevent collapse. It was observed that the cement as a foreign object induced membrane around itself (Foreign body-induced membrane) (4). In some studies removing this membrane was avoided to reduce bleeding and their results showed that union increased and their absorption reduced (9). The membrane extract also caused proliferation and differentiation of bone marrow cells (12). This observation was confirmed in controlled studies as well (13, 14).
Due to the importance and positive outcomes of this method in restoration of large defects in bones, many studies are ongoing to improve clinical and biological results. Initial filling material type, the optimal type of used graft and proper means for fixation are the most important objectives in those researches.
Patients with infectious bone defects are the major health challenging patients in trauma clinics. These patients often have poor status of soft tissues around infection sites due to repeated surgeries. Furthermore, some other conditions such as diabetes and poor nutritional status would make more problems for patients to endure reconstructive surgeries. In addition, due to repeated surgeries, high costs and lack of appropriate response during long-term treatments, patients cooperation would be lower for next surgical procedures. This situation even causes voluntary amputation in patients with osteomyelitis.
According to investigations and lack of similar studies in Iran, this study was performed to identify technical strengths and weakness of induced membrane technique in patients with osteomyelitis.
2. MATERIALS AND METHODS
This case series study was performed on 21 patients with bone defects in the femur and tibia and metatarsal bones referred to orthopedic clinic of Rasoul Akram Hospital, Tehran, Iran, for induced membrane surgery in 2012-2015.
A written consent was obtained from all patients for the study. Various information including age, gender, defect location, presence or absence of infection, cigarette smoking, drug use, and duration of delay in treatment were recorded by both questionnaire and a checklist of observations and clinical examinations. Defect size assessment was performed based on the full-face and laterals radiographic as well as operation time measurements. Two-stage surgery of induced membrane technique was performed for all patients in this study.
In the first stage, an extensive debridement was performed in defected bone or infected tissue location and then the cement was placed within the defected bone location. Cement was poured in a 50 mL syringe and its body was cut to have smooth cement surface. As necessary, cover flap was used for reconstruction of soft tissue.
In the second stage performed about 8 weeks later, the cement graft was removed and the void was filled by cancellous auto-graft of iliac bone. A one to three ratio mixture of auto-graft and allograft was used in case of large defects. The second stage was performed after ensuring infection healing (discontinued secretion and negative ESR and CRP).
Surgery outcomes were evaluated in the first two weeks after the treatment and monthly until patient’s recovery in the orthopedic clinic. Union achievement was the main outcome of this study, which was confirmed by radiographic findings (welding three of four cortices in lateral and full-face radiography) and physical examination (ability of weight bearing without pain and instability). Confounding complications such as limitations in range of motion and iliac bone graft harvest site complications were secondary results of this study, which were evaluated using clinical examinations.
SPSS ver. 16 (SPSS Inc. Chicago, IL, USA) was used for data analysis. Quantitative and qualitative data were reported as average and percentage of distribution, respectively.
3. RESULTS
Only one out of twenty-one patients enrolled in the study was female. Growth hormone was not administered in any participants. Corrective action, osteotomy and angulation using plaque, was necessary for one of the patients. Bone defects were in tibia, femur and metatarsus in 9, 9 and 3 patients, respectively. Three patients received soft tissue reconstruction with flap before induced membrane surgery.
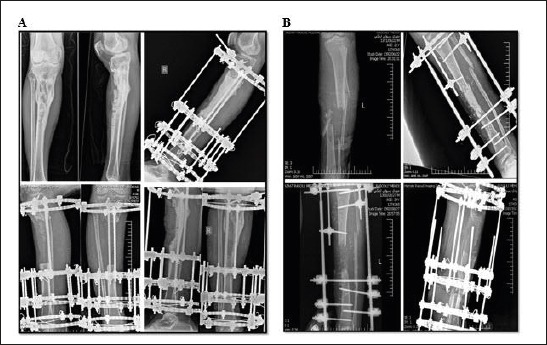
The mean age of patients was 30.52 years and the minimum and maximum were 19 and 65 years, respectively. The mean bone defects size was 85.71 mm ranged 30-150 mm. Five patients (23.8%) had cigarettes smoking and 2 cases (9.5%) used drugs with cigarettes. The average delay from onset of bone defects to start the treatment was 14.19 months ranged 0-90 months. None of these parameters had significant effect on union status (Table 1).
Table 1.
Study Participants Characteristics
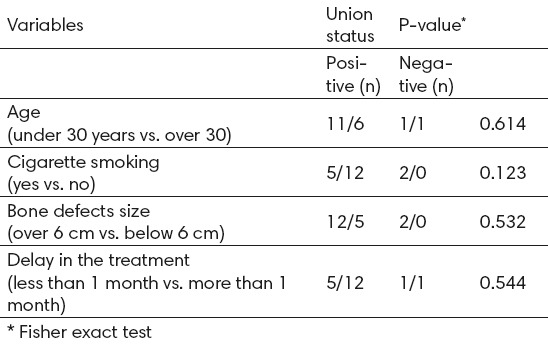
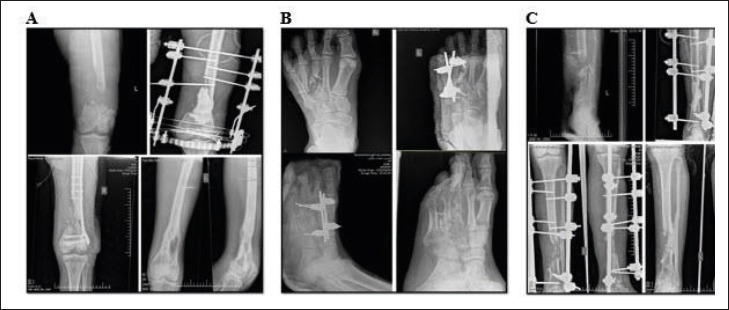
Finally, 17 patients (90%) had clinical and radiographic union in follow-up (Figure 1). Two patients did not finish their follow-up and needed more time to achieve final results. The remaining 2 patients did not respond to this method. One of them underwent amputation and the other one underwent the Ilizarov surgery (Figure 2).
Figure 1.
Successful Treatment Results by Induced Membrane Technique in Femur (A), Metatarsus (B) and Tibia (C)
Figure 2.
Induced Membrane Technique Failure for Tibia Bone. (A) Received Amputation and (B) Received Ilizarov Surgery
In the case of union, the average recovery time was 7.35 months ranging from 4-12 months. Traction was performed by observing union for all patients. Despite harvesting a large volume of iliac crest bone for this technique, none of the patients had movement limitation or any adverse effects in the harvesting place.
One of the failure treatments was in a 56-year-old male patient with schizophrenia and addiction to cigarettes and drugs (Figure 2A). The patient did not adhere to medical recommendation and put cigarette ash on surgical wound. Ultimately, amputation was performed due to severe infection.
The second case was a 20-year-old male patient who developed infection again after a bone graft (Figure 2B). It was found that the graft was reabsorbed. Due to removing high amount of graft from both sides of iliac crest, re-harvesting or access to RIA system was not possible and the Ilizarov surgery was performed to continue the treatment.
4. DISCUSSION
Induction membrane technique in 1986 was provided by Masquelet et al. and partly by accident (1, 2, 5). This technique was performed due to need to use a membrane to prevent graft resorption. To achieve this goal, it was tried to use synthetic polylactide membrane which was needed to be meshed for graft blood supplementation. Casual observation suggested that non-debrided membranes surrounding the cement to stop the bleeding were associated with subsequent graft union improvement. This organized idea confirmed in some studies needs to be further evaluated (9, 10, 14).
This important reconstructive surgery needs two stage of operation. Various studies have been performed by laboratory animals and clinical trials to investigate the strength and weakness points of this technique (12, 15). The results of this technique would be better if this point is considered during the operation (16).
The nature and function of the induced membrane has been focused on various histology studies. Remaining the cement for four weeks as a long bone defect spacer would induce a membrane around the cement. This membrane would be a protector for second stage bone graft and inhibit grafts resorption in high percentage (17). In addition to physical protection, secretion of growth and inflammatory factors lead to proliferation and differentiation of bone cells (12). This phenomenon has been proved by several histologic studies in laboratory animals and clinical trials.
Using this method in cases of infected bone defects was the noteworthy point of this study. The fundamental challenges of infectious bone defects, especially in trauma centers such as Rasoul Akram Hospital, are patients that have lesions with different surgery and soft tissue infection. These patients usually have soft tissue around the infection point due to repetitive surgeries (1, 2, 18). Delivering higher concentrations of antibiotics in the cement, keeping the limb length and relative stability with cement spacer, providing the perfect time to treat the infection and ensuring no recurrence are obvious characteristics of this method (19, 20).
Gouron et al. conducted a study to investigate the recovery time and complication of this technique in children (mean age of 11 years) with bone defects caused by trauma, tumor and congenital pseudarthrosis. Average follow-up was 30 months and the average percentage of restructuring was 32% in this study. Bone union was observed in 9.5 months which is partially similar to our results. About 35% of patients experienced non-union but by improving the fixation and bone grafting, union was observed. The low rate of achieving auto-graft and need to use bone chips and even tibial strut grafts in children were the reasons for poor results obtained in this study (21).
Karger et al. performed a study to investigate the treatment results of post-traumatic bone defects by induced membrane technique. This study was performed on 84 participants with long bone defects due to trauma. Totally, 70% of lesions were in the lower extremities and 50% associated with infection. In more than a half of cases, the lesions were more than 5 cm. Their results showed that 90% of patients had union after an average of 14 months after reconstruction surgery (18), which was partially the same as our results.
In 2012, Taylor et al published a paper to describe induced membrane technique for reconstruction to manage bone loss. Same to our obtained results, the achievement of their experiment showed excellent clinical results with successful reconstruction of segmental bone defects >20 cm (7).
Zappaterra et al (2011) published their experiment with aim of studying the achievement of induced membrane technique for the reconstruction of bone defects in upper limb. Although their participants number were low, but same to our results they showed union achievement in about 90% of the cases with a follow-up of 23 months (21).
Overall in this study, 21 cases of bone defects with an average of 9 cm (up to 15 cm) of the femur, tibia and metatarsus were treated with induction membrane technique. Two-thirds of patients had chronic infection and the rest of them had sub-acute infection. The average delay in treatment was 14 months with a maximum of 90 months. Our results showed that 90% of patients successfully treated at the end of follow-up. In successful treated patients, union average recovery time was 7.35 months with a range of up to 12 months.
5. CONCLUSION
Patients of this study were challenging cases due to having severe infection. It can be stated that using this method would have high success for patients with defects in their long bones. Comparison of this study results with previous ones showed the acceptable outcomes and correct use of this technique. At last, the procedure which is used for induced membrane technique in this experiment can be recommended for other cases with same lesions.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Nishida J, Shimamura T. Methods of reconstruction for bone defect after tumor excision: a review of alternatives. Medical Science and Technology. 2008;14(8):RA107–RA13. [PubMed] [Google Scholar]
- 2.Pipitone PS, Rehman S. Management of Traumatic Bone Loss in the Lower Extremity. Orthopedic Clinics of North America. 2014;45(4):469–82. doi: 10.1016/j.ocl.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Masquelet A, Fitoussi F, Begue T, et al. Reconstruction of the long bones by the induced membrane and spongy autograft. Annales de chirurgie plastique et esthétique. 2000 [PubMed] [Google Scholar]
- 4.Masquelet A, Obert L. Induced membrane technique for bone defects in the hand and wrist. Chirurgie de la main. 2010;29:S221–4. doi: 10.1016/j.main.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthopedic Clinics of North America. 2010;41(1):27–37. doi: 10.1016/j.ocl.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 6.Flamans B, Pauchot J, Petite H, et al. Use of the induced membrane technique for the treatment of bone defects in the hand or wrist, in emergency. Chirurgie de la main. 2010;29(5):307–14. doi: 10.1016/j.main.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Taylor BC, French BG, Fowler TT, et al. Induced membrane technique for reconstruction to manage bone loss. Journal of the American Academy of Orthopaedic Surgeons. 2012;20(3):142–50. doi: 10.5435/JAAOS-20-03-142. [DOI] [PubMed] [Google Scholar]
- 8.Viateau V, Bensidhoum M, Guillemin G, et al. Use of the induced membrane technique for bone tissue engineering purposes: animal studies. Orthopedic Clinics of North America. 2010;41(1):49–56. doi: 10.1016/j.ocl.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Giannoudis PV, Faour O, Goff T, et al. Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury. 2011;42(6):591–8. doi: 10.1016/j.injury.2011.03.036. [DOI] [PubMed] [Google Scholar]
- 10.Zwetyenga N, Catros S, Emparanza A, et al. Mandibular reconstruction using induced membranes with autologous cancellous bone graft and HA-βTCP: animal model study and preliminary results in patients. International journal of oral and maxillofacial surgery. 2009;38(12):1289–97. doi: 10.1016/j.ijom.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 11.Pannier S, Pejin Z, Dana C, et al. Induced membrane technique for the treatment of congenital pseudarthrosis of the tibia: preliminary results of five cases. Journal of children's orthopaedics. 2013;7(6):477–85. doi: 10.1007/s11832-013-0535-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelissier P, Masquelet A, Bareille R, et al. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. Journal of orthopaedic research. 2004;22(1):73–9. doi: 10.1016/S0736-0266(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 13.Chotel F, Nguiabanda L, Braillon P, et al. Induced membrane technique for reconstruction after bone tumor resection in children: a preliminary study. Orthopaedics & Traumatology: Surgery & Research. 2012;98(3):301–8. doi: 10.1016/j.otsr.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Yazar S, Lin CH, Lin YT, et al. Outcome comparison between free muscle and free fasciocutaneous flaps for reconstruction of distal third and ankle traumatic open tibial fractures. Plastic and reconstructive surgery. 2006;117(7):2468–75. doi: 10.1097/01.prs.0000224304.56885.c2. [DOI] [PubMed] [Google Scholar]
- 15.Mauffrey C, Hake ME, Chadayammuri V, et al. Reconstruction of Long Bone Infections Using the Induced Membrane Technique: Tips and Tricks. Journal of orthopaedic trauma. 2015 doi: 10.1097/BOT.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 16.Liu H, Hu G, Shang P, et al. Histological characteristics of induced membranes in subcutaneous, intramuscular sites and bone defect. Orthopaedics & Traumatology: Surgery & Research. 2013;99(8):959–64. doi: 10.1016/j.otsr.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Karger C, Kishi T, Schneider L, et al. Treatment of posttraumatic bone defects by the induced membrane technique. Orthopaedics & Traumatology: Surgery & Research. 2012;98(1):97–102. doi: 10.1016/j.otsr.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Tate MK, Chang H, Moore SR, et al. Surgical membranes as directional delivery devices to generate tissue: testing in an ovine critical sized defect model. PloS one. 2011;6(12):e28702. doi: 10.1371/journal.pone.0028702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ziran NM, Smith WR. The'Ziran'wrap: reconstruction of critical-sized long bone defects using a fascial autograft and reamer-irrigator-aspirator autograft. Patient safety in surgery. 2014;8(1):1–15. doi: 10.1186/s13037-014-0040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gouron R, Deroussen F, Plancq MC, et al. Bone defect reconstruction in children using the induced membrane technique: A series of 14 cases. Orthopaedics & Traumatology: Surgery & Research. 2013;99(7):837–43. doi: 10.1016/j.otsr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Zappaterra T, Ghislandi X, Adam A, et al. Induced membrane technique for the reconstruction of bone defects in upper limb. A prospective single center study of nine cases. Chirurgie de la main. 2011;30(4):255–63. doi: 10.1016/j.main.2011.06.005. [DOI] [PubMed] [Google Scholar]


