Abstract
Background
Obesity/overweight is a recognized risk factor for a host of disorders. The disease risk stratification is commonly based on the Quetelets Index (Body Mass Index- BMI), a surrogate measure of fatness. The currently used BMI cut-offs to classify people as overweight or obese in Armed Forces have been defined in studies on Caucasian populations. However, because of differences in body structure and composition in different ethnic, socioeconomic, cultural and regional groups the correspondence between BMI and body fat content varies between populations. We conducted this pilot study in the Indian Navy to define BMI cut-offs for overweight and obesity using body fat content derived from Skin Fold Thickness as the standard.
Material and Methods
The study was conducted on 121 volunteers from a naval hospital staff in the age range of 18 to 47 years. The mean age, height, weight, BMI, body fat in the study group was 26.73 years (± 5.5098), 168.56 cm (± 6.1034), 65.92 Kg (± 10.2746), 23.17 Kg/m2 (± 3.0265) and 19.91% (± 4.831) respectively.
Results
The prevalence of overweight/obesity was 20.66% by BMI and 47.11% by body fat content. Receiver operating characteristic (ROC) curve analysis defined a BMI of 23.85 kg/m2 as the cut off for overweight with a sensitivity of 70.2% (95% CI 56.6 – 81.6) and 87.5% specificity (95% CI 76.8-94.4) and a BMI of 24.38 kg/m2with 90% sensitivity (95% CI 68.3-98.5) and 81.2% specificity (95% CI 72.2-88.3) for obesity.
Conclusion
The results of our study suggest lower BMI cut offs for overweight and obesity in Indian populations than those recommended by WHO.
Key Words: Body Mass Index, Body fat content, Skin fold thickness
Introduction
Obesity is recognized as an important risk factor for various diseases. Studies have indicated an increase in all cause mortality with increased body mass index (BMI), especially death from cardiovascular disease in men [1]. The risk of diseases appears to increase as a function of the percent fat content in the body, above an upper limit of normal. For the purpose of risk stratification it is convenient to have cut-off values of body fat content based upon its observed association with disease.
The measurement of body fat is too complex to be of practical clinical application. Hence surrogate measures such as the Quetelet index (Body mass index – measured as weight in kg/height in metres2), are used in daily practice. This measure however suffers from two major drawbacks in that it does not differentiate between body fat and fat free compartments. Therefore a high BMI may indicate either increased fat or fat free mass and body composition being affected by ethnicity, growth patterns, socio-economic, cultural and behavioral patterns the same BMI in people of different ethnicities and background may reflect different fat contents and distribution [2].
The criteria that we use today are suggested by WHO guidelines [3] (Table 1). These have been developed by western researchers based on studies in Caucasian populations, and in no way are designed to be applicable to all populations. Important differences exist in the form of higher/lower body fat content for a given BMI in South-east Asians, Polynesians, Micronesians and Asian Indians to give a few examples [3, 4]. With this in mind the International Diabetes Federation has accepted BMI value of >25 kg/m2 and 23 kg/m2 as the cut-off for obesity for Asian men and women respectively [5].
Table 1.
WHO classification of overweight/obese
| BMI Kg/m2 | |
|---|---|
| Underweight | < 18.5 |
| Normal weight | 18.5-24.9 |
| Overweight/pre-obese | 25-29.9 |
| Class I obesity | 30-34.9 |
| Class II obesity | 35-39.9 |
| Class III (morbid) obesity | > 40 |
The percent of body fat that is considered normal varies with the age and sex of an individual. Thus, up to 20% body fat (BF%) may be considered normal in young healthy men, whereas with increasing age, greater amounts of BF% may be considered “normal” [6]. The exact value of BF% above which a person may be considered overweight or obese is debatable. However a value of 20% BF for defining overweight and 25% BF for defining obese has been suggested by various workers [6, 7]. In an Indian study comparing body fat with risk of coronary artery disease body-fat-percent categories used for analysis were <10 – under-body-fat, 10 to 20 – normal-fat, 20 to 25 – over-fat and >25 -higher-body-fat. These categories corresponded approximately to percentiles 0 to 25, 26 to 54, 55 to 64 and >65 of the body-mass index and were also in accordance with height-weight tables of average values for Indian men, advised by the Life Insurance Corporation of India [8]. In this study, a BF% content of 20 and 25 has been used to define overweight and obesity, respectively.
Material and Methods
The study was conducted on 121 healthy male volunteers from a Naval Hospital's staff, who were “FIT” and healthy in all respects as per the annual medical examination. An initial clinical history was taken and examination done to rule out any systemic disease. The measurements to be made were described and informed consent taken.
Body weight was measured to the nearest 100 gm using a balance beam weighing scale. The individuals were stripped to the waist before body weight measurement. Height was measured using a metal stadiometer and BMI was calculated.
Body fat content was measured by the skin-fold thickness method. Skin-fold thickness was measured at four sites, namely biceps, triceps, sub-scapular and supra-iliac skin-folds. A Harpenden skin-fold caliper with accuracy of 0.2 mm was used for the purpose. For the triceps and biceps skin-fold thickness, a horizontal line was circumferentially drawn at the midpoint between the acromion and the olecranon and the skin-fold thicknesses were measured over the biceps and triceps at this point with the arm pendant. The sub-scapular skin-fold was measured 1.5 to 2 cm below the lower angle of the scapula at 45° to the horizontal. The supra-iliac skin-fold was measured at a point halfway between the iliac crest and the lowermost margin of the ribs in the mid-axillary line at 45° to the horizontal. All measurements were made on the right side of the body in all the subjects. The measurement was repeated thrice at each site and the arithmetic mean of the three readings considered as the skin-fold thickness at the site. The sum of all four skin-fold thickness’ was used to calculate body fat content by the formula of Durnin & Womersley which has been validated in Asian Indians [9, 10].
The data was managed in a Microsoft Excel worksheet. Means and standard deviations of all anthropometric variables were calculated. Receiver operating characteristic (ROC) curves were drawn to determine appropriate cut-off points of the BMI for defining overweight and obesity. Body fat percentage measures as derived from skin-fold thickness were considered the standard. Analysis was done using MedCalc-version-9.1.0.1 statistical software. A p value of <0.05 was considered significant.
Results
The present study included 121 male sailors. Their details are as given in Table 2. The age distribution of the subjects is given at Fig. 1.. The distribution of overweight and obese by age groups, by BMI and body fat percent are as given in Table 3. The correlation between the two measures is also given.
Table 2.
Age, height, weight, BMI and body fat% in subjects
| Range | Mean (± SD) | |
|---|---|---|
| Age | 18-49 years | 26.73 (5.5098) |
| Height | 154-189 cm | 168.56 (6.1034) |
| Weight | 47.2-112 kg | 65.92 (10.2746) |
| BMI | 17.7-35.95 kg/m2 | 23.17 (3.0265) |
| Body fat% | 10.87-33.4% | 19.91 (4.831) |
Fig. 1.
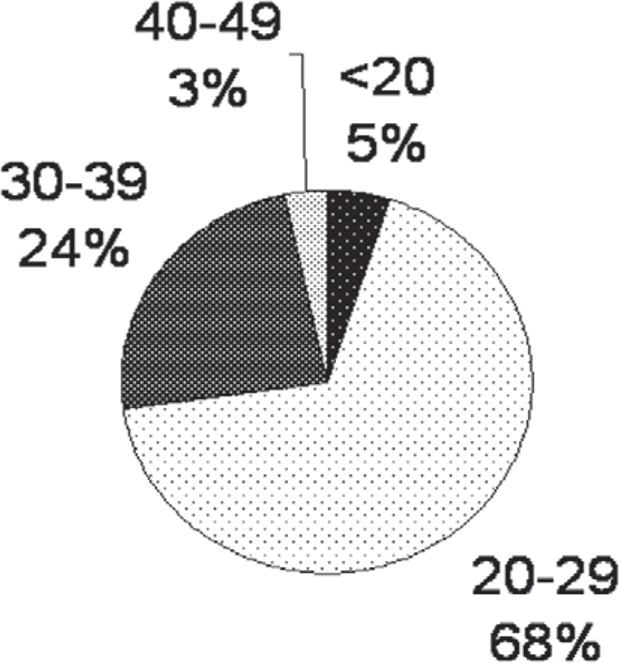
Age distribution of subjects of the study group
Table 3.
Distribution into obese/overweight of study subjects
| Age groups | Number overweight/obese | Percentage of group overweight/obese | Correlation | ||
|---|---|---|---|---|---|
| BMI | Body fat% | BMI | Body fat% | ||
| < 20 | - | - | - | - | 0.3645 |
| 20-29 | 10 | 30 | 12.2 | 36.59 | 0.6744 |
| 30-39 | 12 | 24 | 41.38 | 82.76 | 0.6819 |
| 40-49 | 3 | 3 | 75 | 75 | 0.7148 |
| Total | 25 | 57 | 20.66 | 47.11 | 0.7201 |
Of the 25 overweight/obese by BMI one had Grade II and three had Grade-I obesity, while the remaining 21 were overweight. By body fat percentage criteria, on the other hand, thirty-five people were overweight and twenty-two obese. Of those overweight by BMI, three (12%) had fat content in the normal range.
The sensitivity and specificity of BMI as a diagnostic tool for all overweight in our study was calculated to be 38.6% and 95.31% respectively with a positive predictive value of 88% and a negative predictive value of 63.54%. For a BMI cut-off of 30 kg/m2 for obesity the sensitivity was only 18.8% and specificity was 100% with a PPV of 100% and NPV of 84.62%.
ROC curves were drawn to delineate the cut-off for overweight and obesity. The data for both the curves at suggested cut-off points are given in Table 4.
Table 4.
ROC data for our study at suggested cut-off points
| Overweight | Obese | |
|---|---|---|
| Body fat% | 20 | 25 |
| Suggested BMI cut-off | > 23.85 | > 24.38 |
| Sensitivity | 70.2 | 90 |
| Specificity | 87.5 | 81.2 |
| Positive predictive value | 26.4 | 48.6 |
| Negative predictive value | 97.9 | 97.6 |
| p value | .0001 | .0001 |
Discussion
In this study we have attempted to define BMI cut-off points for defining overweight and obese using skin fold thickness as the standard test and 20 and 25% body fat as the cut off for overweight and obese respectively.
A BMI cut-off of 23.85 Kg/m2 for overweight was derived by ROC curve analysis in this study. Using this value the number of overweight increased to 49 whereas with conventional values of 25 kg/m2 the number was almost half, only 25. Further, although the number of false positives increased from 3 to 8 the number of false negatives decreased from 35 to 18. The BMI cut-off figure for obesity (corresponding to BF 25%) worked out to 24.38 kg/m2.
Similar data suggesting lower BMI cut-offs for Asian Indians has been found in other studies. In a study by Dudeja et al [11], in 123 North Indians (86 males and 37 females), the authors have proposed a BMI cut-off value of 21.5 Kg/m2 corresponding to 25% body fat for males and 19 Kg/m2 for females. Their data generated a sensitivity of 86.7, a specificity of 89.3 with a positive and negative predictive values of 81.3 and 92.6 respectively at a BMI cut-off of 21.5 kg/m2. The sensitivity, specificity and negative predictive value in our study at a BMI cut-off for obesity (BF- 25%) of 24.38 kg/m2 are similar, however the positive predictive value is significantly lower at 48.6%. This could be due to the fact that the subjects in former study had a prevalence of obesity of 34.8% and were north Indians, while in this study the prevalence of obesity was 18.18% and the subjects were a heterogeneous mix of populations from all parts of the country.
In another study on 141 men by Bhat et al [12], approximately equal number of men from rural background, urban slums and middle class city dwellers were studied. They reported that using a BF% of 25 as cut-off, 29.5% rural, 46% urban slum and 75% urban middle class subjects were obese. On the other hand using WHO recommended BMI cut-off's 9% rural, 22% slum dwellers and 27% urban middle class were overweight while only 4% of the slum dwellers and none of the rural or urban middle class were obese. They suggested the use of body fat measures and not BMI for risk stratification in Indian men. Piers et al [13], have contended that BMI is good for population studies but ill-applied in individuals, a fact that is borne out by this study. The need for population specific BMI cut-off is imperative and this measure must be applied to the individual with great caution.
However we have to bear in mind that amongst obesity related disorders; obesity is but one risk factor. The American Heart Association in its 2005 update of the 1997 Statement on Obesity and Heart Disease says “… even if weight loss is minimal, obese individuals with a good level of cardio-respiratory fitness show a reduced risk for cardiovascular mortality as compared with lean, poorly fit subjects” [14].
BF% derived from skin-fold thickness has been used as the standard for fat content measurement, in this study. This method gives a predicted value of fatness for an individual which is within 3- 5% of body fat as measured by use of hydrostatic weighing, which is considered as “gold standard” for body fat content assessment [6]. The small sample size of our study did not allow identification of cut-off level differences, if any, between people from different parts of the country.
No attempt has been made to correlate body fat content or BMI with other risk factors or disease prevalence. Longitudinal studies including anthropometric measures and measures of various disease incidences are required to define BMI cut-off, for the purpose of disease risk stratification in Asian Indian men from different parts of the country.
Based on these findings it is suggested that large-scale studies be conducted to define BMI cut-off points for overweight and obese specific to various subsets of the Asian Indian population group. A BMI cut-off of ≥ 25 kg/m2 for overweight and 30 kg/m2 for obesity has a very low sensitivity in our population. Hence due caution must be exercised when using these criteria in deciding on overweight/obesity.
Conflicts of Interest
None identified
Intellectual Contribution of Author
Study Concept : Lt Col SP Singh
Drafting & Manuscript Revision : Lt Col SP Singh, Lt Col MK Garg
Study Supervision : Lt Col SP Singh, Surg Lt Cdr G Sikri
References
- 1.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of US adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 2.Routh VH, Stern JS, Horwitz BA. Physiological Responses of mammals to overnutrition. In: Fregly MJ, Blatties CM, editors. Handbook of Physiology: Section 4: Environmental Physiology. Oxford University Press; New York: 1996. pp. 1411–1436. [Google Scholar]
- 3.WHO . WHO Tech Rep Ser, 894. WHO; Geneva, Switzerland: 1999. Obesity: preventing and managing the global epidemic: report of a WHO consultation (ISSN 05 12-3054) [PubMed] [Google Scholar]
- 4.Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord. 2000;24:1011–1017. doi: 10.1038/sj.ijo.0801353. [DOI] [PubMed] [Google Scholar]
- 5.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. The Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 6.McArdle WD, Katch FI, Katch VL, editors. Exercise Physiology: Energy, nutrition and human performance. Williams and Wilkins; Baltimore: 1996. [Google Scholar]
- 7.Bray GA. Nutrient balance and obesity: an approach to control of food intake in humans. Med Clin North Am. 1989;73:29–44. doi: 10.1016/s0025-7125(16)30690-3. [DOI] [PubMed] [Google Scholar]
- 8.Singh RB, Niaz MA, Beegom R, Wander GS, Thakur AS, Rissam HS. Body Fat Percent by Bioelectrical Impedance Analysis and Risk of Coronary Artery Disease Among Urban Men with Low Rates of Obesity: The Indian Paradox. Journal of the American College of Nutrition. 1999;18:268–273. doi: 10.1080/07315724.1999.10718862. [DOI] [PubMed] [Google Scholar]
- 9.Durnin JVGA, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77–97. doi: 10.1079/bjn19740060. [DOI] [PubMed] [Google Scholar]
- 10.Kuriyan R, Petracchi C, Ferro-Luzzi A, Shetty PS, Kurpad AV. Validation of expedient methods for measuring body composition in Indian adults. Indian J Med Res. 1998;107:37–45. [PubMed] [Google Scholar]
- 11.Dudeja V, Misra A, Pandey RM, Devina G, Kumar G, Vikram NK. BMI does not accurately predict overweight in Asian Indians in northern India. British Journal of Nutrition. 2001;86:105–112. doi: 10.1079/bjn2001382. [DOI] [PubMed] [Google Scholar]
- 12.Bhat DS, Yajnik CS, Sayyad MG, Raut KN, Lubree HG, Rege SS. Body fat measurement in Indian men: comparison of three methods based on a two-compartment model. Int J Obes (Lond) 2005;29:842–848. doi: 10.1038/sj.ijo.0802953. [DOI] [PubMed] [Google Scholar]
- 13.Piers LS, Soares MJ, Frandsen SL, O'Dea K. Indirect estimates of body composition are useful for groups but unreliable in individuals. Int J Obes Relat Metab Disord. 2000;24:1145–1152. doi: 10.1038/sj.ijo.0801387. [DOI] [PubMed] [Google Scholar]
- 14.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. An Update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. American heart association; Dallas (Texas): 2005. Obesity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss.http://circ.ahajournals.org/cgi/content/full/113/6/898 (Cited 2006 Feb 19). Available from. [DOI] [PubMed] [Google Scholar]


