Introduction
The increasing prevalence of tuberculosis in both immunocompetent and immunocompromised individuals makes tuberculosis a topic of universal concern. A high degree of clinical suspicion and familiarity with the various radiologic manifestations of tuberculosis allow early diagnosis and timely initiation of appropriate therapy, thereby reducing patient morbidity. Although manifestations of tuberculosis are usually limited to the chest, the disease can affect any organ system. Tuberculosis of sternoclavicular joint has been reported in 1-2% of all cases of peripheral tuberculosis [1]. Dhillon et al [2], found only 10 cases over a period of six years in a large tertiary care hospital. In the west primary disease is less prevalent as compared to the Indian subcontinent. In patients infected with human immunodeficiency virus ((HIV) or other immunocompromised status like haemodialysis, this disease usually involves multiple extra pulmonary sites including the skeleton, genitourinary tract and central nervous system.
Case Report
A 38 year old civilian factory worker presented with complaints of swelling and pain involving left lower part of neck for past two months. It was associated with low grade fever but there was no history of loss of appetite or loss of weight. He was treated with antibiotics by a civil doctor. The patient had no history of drug abuse, features suggestive of immuno-compromise or local trauma. Haemogram showed a raised ESR of 56 mm of fall at the end of first hour (Westergren's). A serological test done for HIV was negative. Mantoux test was strongly positive. Chest radiograph revealed normal lung fields with suspicion of irregularity of left sternoclavicular joint. An oblique view of left sternoclavicular joint showed irregularly moth-eaten appearance of sternal end of clavicle and mild sclerosis of articular surface of manubrium (Fig. 1). Computerised tomography (CT) scan done showed a lytic lesion involving left sternoclavicular joint. There was an associated hypodense soft tissue component located more on the posterior aspect of the joint (Fig. 2). Based on history, clinical findings and the radiological evidence, an infective aetiology was suggested. Ultrasound (USG) guided fine needle aspiration cytology (FNAC) of the lesion proved tuberculosis as the aetiology (Fig. 3). The patient was put on anti tubercular treatment (ATT) for a period of one year and he made an uneventful recovery.
Fig. 1.
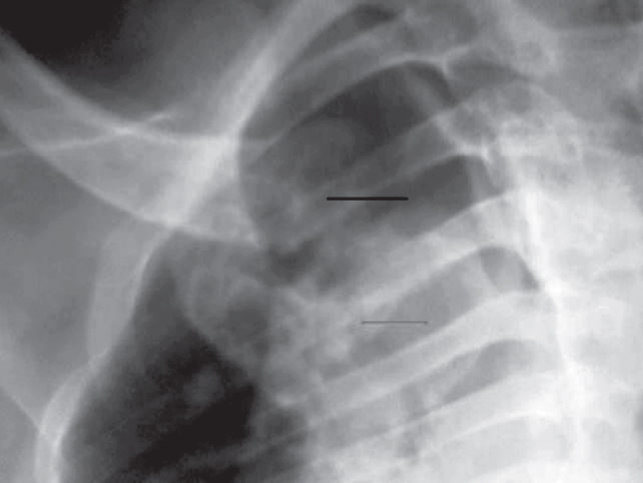
Radiograph of left sternoclavicular joint (oblique view) showing lytic lesion of sternal end of clavicle (top arrow), with mild sclerosis of articular surface of manubrium (bottom arrow).
Fig. 2.
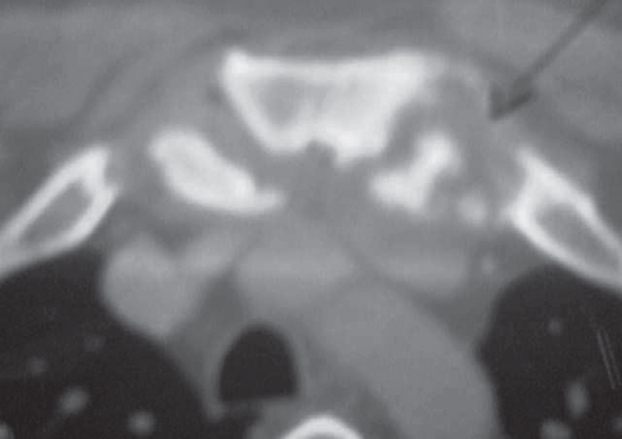
Non contrast CT scan shows destruction of clavicular and sternal end of left sternoclavicular joint (arrow) with a soft tissue component.
Fig. 3.

Histopathology showing granuloma.
Discussion
Sternoclavicular septic arthritis is a rare infection in healthy adults and immunocompromised individuals. Tuberculosis of the sternoclavicular joint is extraordinarily rare and can raise diagnostic problems. It accounts for 1- 9% of septic arthritis [3, 4]. Before the antibiotic era, the most common pathogenic species was from the genus Fusobacterium [5, 6]. In the post antibiotic era, anaerobic organisms have been rarely reported [7]. Instead the isolated organisms are frequently related to bacteremic complications of intravenous access devices or intravenous drug abusers. Dhillon et al [2] have suggested dual course for sternoclavicular tuberculosis; a more aggressive one leading to a painful, destroyed joint associated with constitutional symptoms or a slowly progressive, relatively painless disease without constitutional symptoms and minimal joint destruction, due to differences in the virulence of the organisms and host resistance.
The pathogenesis and source of infection are debatable. The prevalent view is that the infection could originate from a fresh or reactivated pulmonary focus which has spread haematologically. This is the usual pattern of osteoarticular tuberculosis in other joints. Few authors [4], suggest the possibility of contiguous spread from an apical pulmonary tuberculous focus to the sternoclavicular joint, while others feel that the primary focus could be the medial end of the clavicle [10].
In our case the patient had primary infection of sternoclavicular joint with no other demonstrable foci of tuberculosis in lung or any other part of body. The CT scan was suggestive of infectious aetiology and it was confirmed on biopsy.
Though plain radiograph forms the first line of investigation, CT scan is better suited for lesion identification around sternum and sternoclavicular joints as observed by Dhillon et al [2]. The manubrium is typically oblique to the plane of section and the anterior and posterior cortical margin may appear indistinct. The cortical surface of sternoclavicular joint is smooth and symmetric but degenerative changes produce spur formation or vacuum phenomenon within the joint.
Magnetic resonance imaging (MRI) has an advantage of better soft tissue delineation in these cases. It has a sensitivity and specificity of 88% and 93% respectively with focal enhancement on T1W fat suppressed enhanced images suggestive of osteomyelitis. Infection is identified as an area of decreased signal intensity on T1W1 as compared with high signal intensity of fatty marrow and high signal intensity on T2WI. It is useful for determining the extent of the lesion, marrow involvement and soft tissue spread. Abscess formation, destruction of articular cartilage and sinus tract formation is well depicted by MRI. These findings are not visualized on radiography until destructionis advanced [8]. Shah et al [9], suggested that all the modalities compliment each other though MRI is better in detecting marrow involvement and delineating the soft tissue involvement. An early case of sternoclavicular infection is treated conservatively. En block resection is reserved for infections which extends beyond the joint on imaging.
Conflicts of Interest
None identified
References
- 1.Bezza A. Tuberculosis of the sternoclavicular joint. Report of two cases. Rev Rhum Engl Ed. 1998;65:791–794. [PubMed] [Google Scholar]
- 2.Dhillon MS, Gupta RK, Bahadur ON, Nagi Tuberculosis of the sternoclavicular joints. Acta Orthopedic Scandinavia. 2001;72:514–517. doi: 10.1080/000164701753532862. [DOI] [PubMed] [Google Scholar]
- 3.Smith JW, Piercy EA. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 4th ed. Churchill Livingstone; New York: 1995. Infectious arthritis; pp. 2455–2475. [Google Scholar]
- 4.Yasuda T, Tamura K, Fujiwara M. Tuberculous arthritis of the sternoclavicular joint: report of three cases. Journal of Bone & Joint Surgery (Am) 1995;77:136–139. doi: 10.2106/00004623-199501000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Lemierre A. On certain septicemia due to anaerobic organisms. Lancet. 1936;1:701–703. [Google Scholar]
- 6.Gubler JG, Wuest J, Oneta C. Sepsis caused by Fusobacterium necrophorum: the rediscovered post anginal sepsis, Lemierre syndrome and other manifestations. Schweiz Med Wochenschr. 1990;120:440–445. [PubMed] [Google Scholar]
- 7.Lau ES, Shuckett R. Fusobacterium septic arthritis of the sternoclavicular joint. Journal of Rheumatology. 1993;20:1979–1981. [PubMed] [Google Scholar]
- 8.Schaefer PS, Burton BS. Radiographic evaluation of chest wall lesions. Surgical Clinics of North America. 1989;69:911–945. doi: 10.1016/s0039-6109(16)44930-3. [DOI] [PubMed] [Google Scholar]
- 9.Shah J. Tuberculosis of sternum and clavicle: imaging findings in 15 patients. Skeletal radiology. 2000;29:447–453. doi: 10.1007/s002560000207. [DOI] [PubMed] [Google Scholar]
- 10.Martini M. Tuberculosis of the bones and joints. Springer-Verlag; Berlin Heidelberg New York: 1988. pp. 149–150. [Google Scholar]


