Abstract
The presence of tumor-infiltrating lymphocytes (TILs) and tertiary lymphoid structures (TLSs) reflects an active inflammatory tumor microenvironment. High density of TILs as well as presence of TLS is associated with improved survival in various solid cancer types. We aimed to describe the density and distribution of TILs and TLS in pulmonary metastases (PMs) from primary colorectal cancer (CRC) and its correlation with clinicopathological variables. Fifty-seven CRC pulmonary metastasectomy specimen (PM) and 31 matched primary CRC specimen were included. Cluster of differentiation (CD)3+, CD8+, CD45RO+ and FoxP3+ TILs were evaluated by immunohistochemistry and density was scored semiquantitatively. TLS were evaluated based on morphological criteria. Survival time was defined from pulmonary metastasectomy to death or last follow up. A marked infiltration with CD3+, CD8+, CD45RO+ and FoxP3+ TILs was evident in CRC PM and matched primary CRC. Further assessment of the immune infiltrate in PM showed that a high density of FOXP3+ TILs at the invasive margin [HR 2.40 (1.11–6.96); P = 0.031] and low density of CD8+ cells in TLS [HR 0.30 (0.14–0.79); P = 0.016] were associated with a worse prognosis in univariate analysis. Moreover, a low CD8/FoxP3-ratio of TILs at the invasive margin (P = 0.042) and in TLS (P = 0.027) conferred an impaired prognosis after pulmonary metastasectomy. Our findings suggest that CRC PM harbor an immune active microenvironment. The balance of CD8+ and FoxP3+ T-cells at the tumor border and in TLS provides prognostic information in patients with CRC PM.
Electronic supplementary material
The online version of this article (doi:10.1007/s10585-016-9813-y) contains supplementary material, which is available to authorized users.
Keywords: Pulmonary metastasis, Colorectal cancer, Tumor-infiltrating lymphocytes, TILs, Tertiary lymphoid structures
Background
Despite advances in the early detection and treatment of colorectal cancer (CRC), the prognosis of patients is impaired as soon as distant metastases occur. Synchronous pulmonary spreading is evident in about one out of ten patients with newly diagnosed CRC. Subsequently, an average 5-year cumulative risk of 5.8 % for the development of metachronous pulmonary metastases (PMs) is additionally contributing to the disease burden of patients with CRC [1]. However, within the group of patients with CRC lung metastases long-term survival can be achieved by (repeated) pulmonary metastasectomy complemented by chemotherapeutic regimens. In contrast, some patients will present with diffuse recurrence of disease within months after pulmonary metastasectomy. The underlying tumor biology is considered to be the main cause for heterogeneity in the outcome of patients with CRC lung metastases. Several prognostic biomarkers have been proposed to define aggressive tumors associated with fatal outcome [2–4]. During the last years, the tumor microenvironment gained increasing attention in the scientific community, especially in groups focusing on metastatic CRC [5–7].
Immune escape is considered an emerging hallmark of cancer [8]. Various subsets of lymphocytes can be found in the tumor microenvironment, so called tumor-infiltrating lymphocytes (TILs). They can launch pro-inflammatory anti-tumor responses or mediate local immunosuppression. The amount of TILs has a prognostic value in various primary solid cancer types, including lung, renal, breast and CRC [9–14]. Commonly detected lymphocyte subsets with favorable prognostic impact are mature T-cells [cluster of differentiation (CD)3+] and cytotoxic T-cells (CD8+), memory-T-cells (CD45RO+), while immune suppressive regulatory T-cells (FoxP3+) are associated with impaired prognosis. Moreover, tertiary lymphoid structures (TLSs), which are ectopic lymphoid aggregates present in chronically inflamed tissue, can be found in the tumor stroma. TLS are believed to promote and maintain inflammation and anti-tumor response similar to secondary lymphoid organs. The presence of TLS in the tumor microenvironment is associated with favorable prognosis especially in CRC [15, 16].
So far little is known about the local immune response in CRC metastases, as previous studies focused on primary tumor specimen. Metastasis initiating cells have already successfully conquered immune escape during intravasation, survival in the blood stream and extravasation indicating that the composition of the immune microenvironment might differ from the primary tumor [17, 18]. Therefore, we aimed to investigate the local inflammatory microenvironment in CRC PM specimen and matched primary CRC specimen.
Materials and methods
Study population
From April 2009 to June 2014 57 patients with primary CRC receiving complete/curative pulmonary metastasectomy at the Medical University of Vienna were retrospectively recruited from a prospective institutional database. The study was approved by the Institutional Ethics Committee (# 1035/2014) and conducted according the Declaration of Helsinki. Resected pulmonary nodules were verified as metastases from primary CRC by a board certified pathologist. Additionally, samples of the corresponding primary tumor were available in 31/57 (54.4 %) patients. The patients underwent post-surgical tumor surveillance after pulmonary metastasectomy including periodical computed tomography (CT) scans.
Immunohistochemistry
Immunohistochemical (IHC) staining was performed on 4 μm thick sections of formalin-fixed, paraffin-embedded tissue samples using an automated staining platform (Ventana Benchmark Ultra immunostainer, Ventana Medical Systems, Inc., Tucson, USA).
Immunostaining was performed with anti-CD3 (clone SP7, #RM9107-S1, Thermo Fisher Scientific, Cheshire, UK), anti-CD8 (clone C8/144B, #M7103, Dako, Glostrup, Denmark), anti-CD45RO (clone UCHL1, #M074201, Dako, Glostrup, Denmark) and anti-FOXP3 (clone 206D, #320116, BioLegend, San Diego, CA, USA) antibodies using an autostainer (Benchmark Ultra, Ventana Medical Systems, Tucson, USA) according to the manufacturer’s instructions. In negative controls the primary antibody was omitted. A mediastinal lymph node served as positive control. The presence of lymphatic vessel invasion in PM was known from a previous study [19].
Quantification and scoring of TILs and TLS
The density of CD3+, CD8+, CD45RO+ and FoxP3+ TILs was evaluated in a semiquantitative manner on full size sections as described previously [20, 21]. In summary, scores reaching from 0 (absent infiltrate) to 4+ (very dense infiltrate) were assigned to the tissue samples. First, an overall impression was rated at low magnification (×100). Additionally, the spatial distribution of the immune infiltrate was assessed in the tumor center and at the invasive margin separately at higher magnification (×200–400). For further analyses, the TILs densities were dichotomized. The used cut-offs are provided in Supplementary Table 1. Moreover, the sections were screened for the presence of TLSs based on morphologic features (TLS; present vs. not present). Follicular aggregates of lymphatic cells were defined as TLS, whereas perivascular lymphatic aggregates were excluded. The presence of CD3+, CD8+, CD45RO+ and FoxP3+ cells in the TLS was assessed and, according to TILs quantification, scores from 0 to 4 were assigned to the samples. In general, negative and sparse infiltration (0 and 1+) were grouped in contrast to moderate, dense and very dense infiltration (2+, 3+ and 4+), which led to two group sizes as equal as possible. As CD3 were omnipresent, a higher cut-off had to be applied. Also for CD8 TILs, a higher cut off was chosen as described previously by others [22, 23]. The dichotomized variables were used for further calculations. CD8/FoxP3 ratios were calculated from dichotomized values. Samples with high CD8/low FoxP3 were described as CD8/FoxP3-ratio high, samples with high CD8/high FoxP3 or low CD8/low FoxP3 as equal and low CD8/high FoxP3 were described as low. Two observers (TS, ASB) blinded to the clinical data rated each section independently using a multi-head microscope. If the rating differed, the slide was re-discussed and a consensus was found.
Statistical analysis
The disease-free interval (DFI) was defined as the time between surgery for the primary tumor to pulmonary metastasectomy in months. Time to recurrence represented the time between pulmonary metastasectomy and evidence of recurrence at any organ site. Overall survival (OS) was defined as the period of time between pulmonary metastasectomy and death of any cause. If patients had a history of pulmonary metastasectomy before the inclusion period, the previously resected metastases were assessed and the outcome was calculated from the first pulmonary metastasectomy. Nominal variables were compared using χ2 test or Fisher’s exact test (if expected frequency <5). Survival curves were estimated using Kaplan–Meier plots and the difference of the groups were compared using the log-rank test. Statistically significant variables (P-values ≤0.05) in the univariate analysis were added to a multivariate Cox regression model. Statistics were performed using SPSS 23 (SPSS, Inc., Chicago, USA) and GraphPad Prism 6 (GraphPad Software, Inc., California, USA) software. All performed tests were two-sided. P-values ≤0.05 were considered statistically significant. Due to the hypothesis generating approach of the study no correction for multiple testing was used [24].
Results
Fifty-seven patients with histologically verified PMs from primary CRC were included in this study. Macroscopically and microscopically complete resection was achieved in all patients. 33 (57.9 %) patients were male and 24 (42.1 %) female. Median age at the time of pulmonary metastasectomy was 64 years (range 33–83). The primary tumor site was colon in 32 (56 %) patients and rectum in 25 (44 %) patients. A detailed description of the patients’ characteristics is provided in Table 1.
Table 1.
Demographic details of the study cohort (n = 57)
| Characteristics | Total study cohort (n = 57) |
|
|---|---|---|
| n | % | |
| Median age at surgery (range) | 64 (33–83) | |
| Median follow-up after metastasectomy in months (range) | 30 (4–137) | |
| Sex | ||
| Male | 33 | 57.9 |
| Female | 24 | 42.1 |
| Localization of primary tumor | ||
| Colon | 32 | 56.1 |
| Rectum | 25 | 43.9 |
| UICC stage of primary tumor | ||
| I | 4 | 7.4 |
| II | 14 | 25.9 |
| III | 27 | 50.0 |
| IV | 9 | 16.7 |
| Unknown | 3 | – |
| Previous liver metastasis | ||
| Yes | 17 | 29.8 |
| No | 40 | 70.2 |
| DFI | ||
| <36 months | 38 | 66.7 |
| 36–60 months | 9 | 15.8 |
| 60 months | 10 | 17.5 |
| No. of pulmonary metastases | ||
| Singular | 37 | 64.9 |
| Multiple | 20 | 35.1 |
| Chemotherapy before metastasectomy | ||
| Yes | 45 | 78.9 |
| No | 12 | 21.1 |
| Chemotherapy after metastasectomy | ||
| Yes | 43 | 75.4 |
| No | 14 | 24.6 |
DFI disease-free survival to first pulmonary metastasis
Density and distribution of TILs and TLS in pulmonary metastases
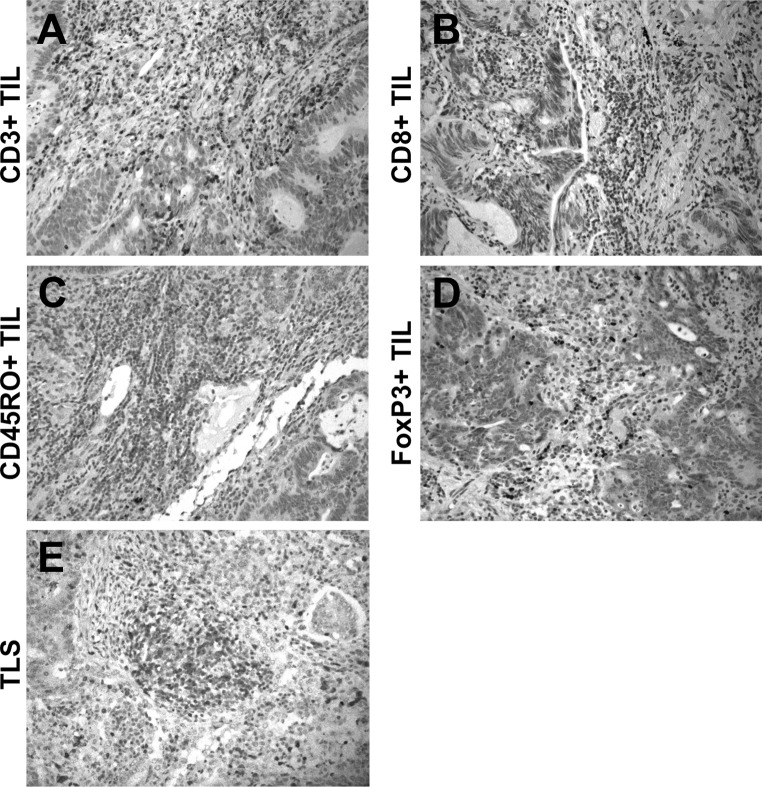
Sufficient IHC quality was achieved in 55/57 (96.5 %), 57/57 (100 %), 54/57 (94.7 %) and 53/57 (93.0 %) of PM specimen for CD3+, CD8+, CD45RO+ and FoxP3+ TIL evaluation, respectively. CD3+, CD8+, CD45RO+ and FoxP3+ TILs at variable density were evident in 55/55 (100 %), 55/57 (96.5 %), 50/54 (92.3 %) and 45/53 (84.9 %) of PM. A detailed description of the density and spatial distribution of TILs is shown in Table 2. Representative images of TILs are provided in Fig. 1. TLS were present in 45/57 (78.9 %) PM specimen. If TLS could be found, the density of CD3+, CD8+, CD45RO+ and FoxP3+ T-cells in TLS was assessed (Supplementary Table 2) and correlated with clinicopathological characteristics (Supplementary Table 3).
Table 2.
Semi-quantitative description of tumor-infiltrating lymphocytes in CRC pulmonary metastases
| TILs density | CD3+ TILs | CD8+ TILs | CD45RO+ TILs | FoxP3+ TILs | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Tumor center | ||||||||
| 0 | 0 | 0.0 | 2 | 3.5 | 4 | 7.0 | 8 | 14.0 |
| 1+ | 7 | 12.3 | 28 | 49.1 | 18 | 31.6 | 19 | 33.3 |
| 2+ | 21 | 36.8 | 15 | 26.3 | 28 | 49.1 | 24 | 42.1 |
| 3+ | 20 | 35.1 | 12 | 21.1 | 4 | 7.0 | 2 | 3.5 |
| 4+ | 7 | 12.3 | 0 | 0.0 | o | 0.0 | 0 | 0.0 |
| Total | 55 | 96.5 | 57 | 100.0 | 57 | 100.0 | 57 | 100.0 |
| Invasive margin | ||||||||
| 0 | 0 | 0.0 | 13 | 22.8 | 2 | 3.5 | 10 | 17.5 |
| 1+ | 3 | 5.3 | 21 | 36.8 | 13 | 22.8 | 26 | 45.6 |
| 2+ | 20 | 35.1 | 17 | 29.8 | 32 | 56.1 | 17 | 29.8 |
| 3+ | 22 | 38.6 | 6 | 10.5 | 7 | 12.3 | 0 | 0.0 |
| 4+ | 10 | 17.5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Total | 55 | 96.5 | 57 | 100.0 | 54 | 94.7 | 53 | 93.0 |
Fig. 1.
Representative images of high densities of a CD3+, b CD8+, c CD45RO+ and d FoxP3+ TILs (DAB; brown) in pulmonary metastases. e CD3+ tertiary lymphoid structure at the invasive margin between tumor cells and lung parenchyma (magnification ×200/400). (Color figure online)
The density of CD3+, CD8+, CD45RO+ and FoxP3+ TILs was correlated with clinicopathological characteristics of our patients. Intratumoral FoxP3+ TILs were more often present in patients with single PM (χ2P = 0.011). All (10/10 (100 %) patients with a DFI of more than 60 months had high levels of CD45RO+ TILs at the invasive margin, compared to 24/36 (66.6 %) patients in the group DFI <36 months (DFI >60 vs. <36 months; Fisher’s exact test P = 0.044). FoxP3+ TILs at the invasive margin were associated with evidence for lymphatic vessel invasion (χ2 test P = 0.050). High CD3+ infiltration in the tumor center was more often found in PM from colon cancer compared to rectal cancer (χ2P = 0.040). Otherwise, no association of TILs density with age, sex, tumor localization, UICC stage of the primary tumor, previous liver metastasis or chemotherapy before metastasectomy was evident (Table 3).
Table 3.
Association of CD3+, CD8+, CD45RO+ and FoxP3+ TILs in the tumor center and at the invasive margin with clinicopathological characteristics (significant values (P < 0.05) in bold)
| CD3+ TILs | CD8+ TILs | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tumor center | Invasive margin | Tumor center | Invasive margin | |||||||||
| Low | High | P | Low | High | P | Low | High | P | Low | High | P | |
| Age at surgery | ||||||||||||
| <64 | 12 | 15 | 0.346 | 9 | 18 | 0.210 | 21 | 7 | 0.473 | 24 | 4 | 0.423 |
| ≥64 | 16 | 12 | 14 | 14 | 24 | 5 | 27 | 2 | ||||
| Sex | ||||||||||||
| Male | 15 | 17 | 0.480 | 12 | 20 | 0.444 | 24 | 9 | 0.177 | 29 | 4 | 1.000 |
| Female | 13 | 10 | 11 | 12 | 21 | 3 | 22 | 2 | ||||
| Localization of primary tumor | ||||||||||||
| Colon | 12 | 19 | 0.040 | 13 | 18 | 0.984 | 23 | 9 | 0.138 | 28 | 4 | 0.686 |
| Rectum | 16 | 8 | 10 | 14 | 22 | 3 | 23 | 2 | ||||
| UICC stage of primary tumor | ||||||||||||
| I | 1 | 3 | 0.815 | 0 | 4 | 0.165 | 3 | 1 | 0.511 | 3 | 1 | 0.292 |
| II | 6 | 6 | 4 | 8 | 13 | 1 | 14 | 0 | ||||
| III | 15 | 12 | 15 | 12 | 20 | 7 | 23 | 4 | ||||
| IV | 4 | 5 | 3 | 6 | 7 | 2 | 8 | 1 | ||||
| Unknown (n = 3) | ||||||||||||
| Previous liver metastasis | ||||||||||||
| No | 17 | 22 | 0.090 | 18 | 21 | 0.309 | 30 | 10 | 0.315 | 35 | 5 | 0.657 |
| Yes | 11 | 5 | 5 | 11 | 15 | 2 | 16 | 1 | ||||
| DFI | ||||||||||||
| <36 months | 21 | 17 | 0.547 | 18 | 20 | 0.343 | 32 | 6 | 0.271 | 35 | 3 | 0.554 |
| 36–60 months | 4 | 4 | 3 | 5 | 7 | 2 | 8 | 1 | ||||
| 60 months | 3 | 6 | 2 | 7 | 6 | 4 | 8 | 2 | ||||
| No. of pulmonary metastases | ||||||||||||
| Singular | 17 | 18 | 0.646 | 13 | 22 | 0.352 | 29 | 8 | 1.000 | 32 | 5 | 0.410 |
| Multiple | 11 | 9 | 10 | 10 | 16 | 4 | 19 | 1 | ||||
| Lymphatic vessel invasion | ||||||||||||
| No | 20 | 14 | 0.135 | 15 | 19 | 0.660 | 29 | 6 | 0.506 | 31 | 4 | 1.000 |
| Yes | 8 | 13 | 8 | 13 | 16 | 6 | 20 | 2 | ||||
| Chemotherapy before metastasectomy | ||||||||||||
| No | 4 | 7 | 0.281 | 3 | 8 | 0.326 | 10 | 2 | 1.000 | 11 | 1 | 1.000 |
| Yes | 24 | 20 | 20 | 24 | 35 | 10 | 40 | 5 | ||||
| CD45RO+ TILs | FoxP3+ TILs | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tumor center | Invasive margin | Tumor center | Invasive margin | |||||||||
| Low | High | P | Low | High | P | Low | High | P | Low | High | P | |
| Age at surgery | ||||||||||||
| <64 | 10 | 17 | 0.580 | 6 | 21 | 0.362 | 15 | 12 | 0.494 | 19 | 8 | 0.697 |
| ≥64 | 12 | 15 | 9 | 18 | 12 | 14 | 17 | 9 | ||||
| Sex | ||||||||||||
| Male | 11 | 20 | 0.361 | 10 | 21 | 0.393 | 16 | 15 | 0.908 | 22 | 9 | 0.573 |
| Female | 11 | 12 | 5 | 18 | 11 | 11 | 14 | 8 | ||||
| Localization of primary tumor | ||||||||||||
| Colon | 13 | 8 | 0.836 | 11 | 20 | 0.142 | 16 | 15 | 0.908 | 22 | 9 | 0.573 |
| Rectum | 9 | 14 | 4 | 19 | 11 | 11 | 14 | 8 | ||||
| UICC stage of primary tumor | ||||||||||||
| I | 2 | 2 | 0.891 | 0 | 4 | 0.453 | 1 | 3 | 0.228 | 3 | 1 | 0.393 |
| II | 4 | 9 | 2 | 11 | 4 | 8 | 6 | 6 | ||||
| III | 11 | 15 | 8 | 18 | 17 | 9 | 20 | 6 | ||||
| IV | 3 | 5 | 3 | 5 | 4 | 4 | 6 | 2 | ||||
| Unknown (n = 3) | ||||||||||||
| Previous liver metastasis | ||||||||||||
| No | 14 | 24 | 0.369 | 9 | 29 | 0.333 | 16 | 21 | 0.088 | 23 | 14 | 0.172 |
| Yes | 8 | 8 | 6 | 10 | 11 | 5 | 13 | 3 | ||||
| DFI | ||||||||||||
| <36 months | 17 | 19 | 0.298 | 12 | 24 | 0.082 | 19 | 18 | 0.641 | 24 | 13 | 0.547 |
| 36–60 months | 3 | 5 | 3 | 5 | 5 | 3 | 7 | 1 | ||||
| 60 months | 2 | 8 | 0 | 10 | 3 | 5 | 5 | 3 | ||||
| No. of pulmonary metastases | ||||||||||||
| Singular | 15 | 21 | 0.845 | 10 | 26 | 1.000 | 14 | 22 | 0.011 | 22 | 14 | 0.122 |
| Multiple | 7 | 11 | 5 | 13 | 13 | 4 | 14 | 3 | ||||
| Lymphatic vessel invasion | ||||||||||||
| No | 14 | 19 | 0.752 | 11 | 22 | 0.253 | 17 | 15 | 0.695 | 25 | 7 | 0.050 |
| Yes | 8 | 13 | 4 | 17 | 10 | 11 | 11 | 10 | ||||
| Chemotherapy before metastasectomy | ||||||||||||
| No | 6 | 6 | 0.517 | 3 | 9 | 1.000 | 4 | 7 | 0.277 | 7 | 4 | 0.730 |
| Yes | 16 | 26 | 12 | 30 | 23 | 19 | 29 | 13 | ||||
DFI disease-free survival to first pulmonary metastasis
Correlation of TILs and TLS in pulmonary metastases and corresponding primary CRC
A detailed description of CD3+, CD8+, CD45RO+ and FoxP3+ TILs density in the tumor center and at the invasive margin of the corresponding primary tumors is provided in Supplementary Table 4. We found no significant correlation between the TIL density in the primary tumor and corresponding lung metastases (Supplementary Table 5). In general, PM had higher densities of CD3+, CD8+, CD45RO+ TILs, whereas the FoxP3 TIL were comparable (Supplementary Fig. 1). Significantly less primary CRC were rated as TLS positive compared to the paired PM samples [2/28 (7.1 %) vs. 22/28 (78.6 %); McNemar test P < 0.001].
Impact of TILs and TLS in PM on outcome parameters
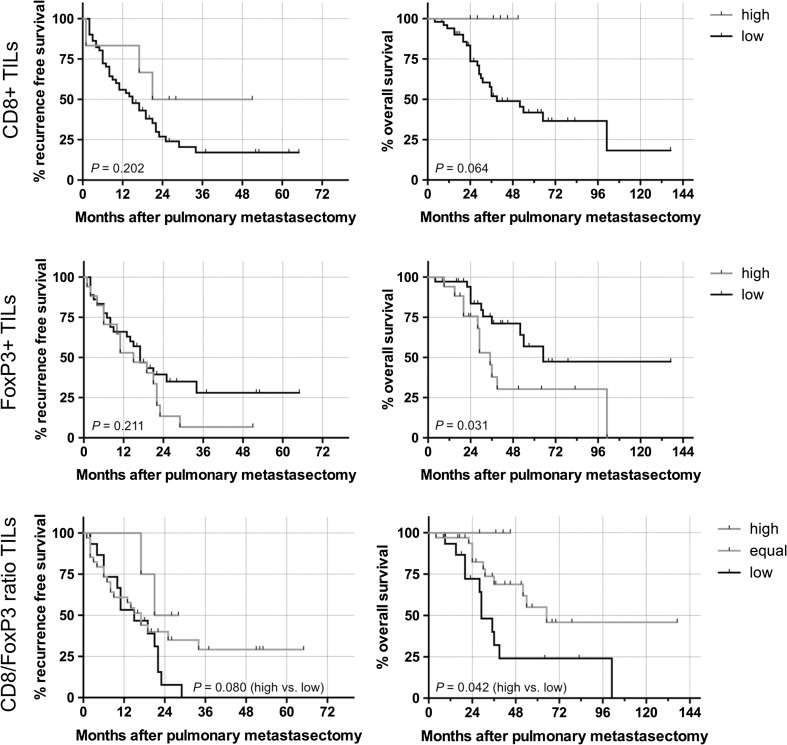
The presence of FoxP3+ TILs at the invasive margin was significantly associated with a decreased OS (35 vs. 65 months; HR 2.40; 95 % CI 1.11–6.96; log-rank test P = 0.031) (Fig. 2). Moreover, dense CD8+ infiltrates at the invasive margin were associated with improved OS (median survival not reached vs. 39 months; HR 0.00; 95 % CI 0.09–1.04; log-rank test P = 0.064).
Fig. 2.
Kaplan–Meier estimates regarding recurrence-free survival and overall survival of pulmonary metastases dependent on the density of CD8+ and FoxP3+ TILs. Additionally the outcome for the CD8/FoxP3-ratio was calculated
6/29 (20.7 %) patients had a high CD8/FoxP3-ratio, CD8/FoxP3 was equal in 10/29 (34.5 %) patients and a low ratio was found in 13/29 (44.8 %) patients. The CD8/FoxP3-ratio had significant impact on OS prognosis after pulmonary metastasectomy (log-rank test P = 0.021 and 0.042 for low vs. equal and low vs. high, respectively). Furthermore, patients with a high CD8/FoxP3-ratio at the invasive margin had a prolonged recurrence-free survival after pulmonary metastasectomy compared to patients with low CD8/FOXP3 ratio (26 vs. 15 months; HR 0.32; 95 % CI 0.12–1.03; log-rank test P = 0.080).
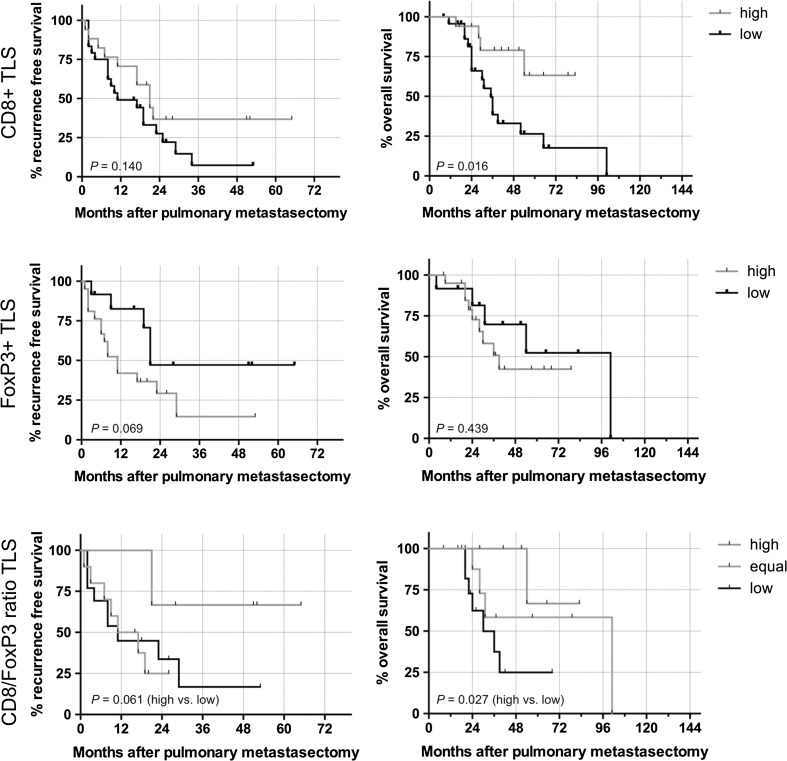
The presence of TLSs in PM alone was neither associated with recurrence-free survival (log-rank test P = 0.141) nor with OS (P = 0.813). However, when assessing the T cell subsets of TLS, we found a significant association of high levels of CD8+ cells in TLS and improved OS (median survival not reached vs. 35 months; HR 0.30; 95 % CI 0.14–0.79; log-rank test P = 0.016). Similarly to TILs, a strong prognostic effect was also found for the CD8/FOXP3-ratio in TLS (high vs. low HR 6.99; 95 % CI 1.28–20.48; log-rank test P = 0.027). Outcome analyses of CD3+, CD8+, CD45RO+ and FoxP3+ cells in TLS are summarized in Table 4 and Fig. 3. Adding CD8+ in TLS and FoxP3+ at the invasive margin into a multivariate Cox regression model, only CD8+ cells in TLS remained a significant prognosticator for OS after pulmonary metastasectomy (P = 0.020; HR 0.29; 95 % CI 0.07–0.79).
Table 4.
Univariate and multivariate outcome analysis of recurrence-free survival and overall survival after pulmonary metastasectomy (significant values (P < 0.05) in bold)
| Recurrence-free survival | Overall survival | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis (log-rank) | Univariate analysis (log-rank) | Multivariate Cox regression | ||||||
| Months | HR (95 % CI) | P-value | Months | HR (95 % CI) | P-value | HR (95 % CI) | P-value | |
| Sex | ||||||||
| Male | 21 | 0.65 (0.33–1.19) | 0.516 | 54 | 1.30 (0.59–2.86) | 0.516 | – | – |
| Female | 13.5 | 101 | – | – | ||||
| Age (years) | ||||||||
| <64 | 17 | 1.01 (0.54–1.88) | 0.974 | 52 | 1.09 (0.50–2.40) | 0.831 | – | – |
| ≥64 | 15 | 65 | – | – | ||||
| Location | ||||||||
| Colon | 19 | 0.97 (0.52–1.80) | 0.917 | 65 | 0.75 (0.34–1.62) | 0.465 | – | – |
| Rectum | 11 | 36 | – | – | ||||
| UICC stage | ||||||||
| I + II | 17 | 1.14 (0.59–2.24) | 0.683 | 36 | 1.95 (0.88–4.85) | 0.099 | – | – |
| III + IV | 15 | NR | – | – | ||||
| Unknown | 3 | – | – | |||||
| Chemotherapy before metastasectomy | ||||||||
| Yes | 15 | 1.19 (0.57–2.49) | 0.648 | 52 | 0.81 (0.30–2.09) | 0.644 | – | – |
| No | 22 | 65 | – | – | ||||
| Chemotherapy after metastasectomy | ||||||||
| Yes | 15 | 1.34 (0.65–2.72) | 0.443 | 39 | 2.08 (0.71–4.74) | 0.214 | – | – |
| No | 21 | NR | – | – | ||||
| Previous liver metastasis | ||||||||
| Yes | 9 | 1.99 (1.11–4.81) | 0.029 | 36 | 1.39 (0.61–3.44) | 0.414 | – | – |
| No | 21 | 54 | – | – | ||||
| DFI | ||||||||
| <36 | 17 | 1.20 (0.62–2.31) | 0.600 | 52 | 1.15 (0.51–2.62) | 0.741 | – | – |
| ≥36 | 17 | 65 | – | – | ||||
| No. of nodules | ||||||||
| Singular | 17 | 0.93 (0.48–1.78) | 0.811 | 54 | 0.85 (0.37–1.89) | 0.681 | – | – |
| Multiple | 16 | 36 | – | – | ||||
| CD3+ TILs TC | ||||||||
| High | 21 | 0.66 (0.35–1.23) | 0.199 | 54 | 1.10 (0.48–2.53) | 0.820 | – | – |
| Low | 15 | 52 | – | – | ||||
| CD3+ TILs IM | ||||||||
| High | 16 | 1.46 (0.77–2.78) | 0.254 | 54 | 1.68 (0.76–3.89) | 0.213 | – | – |
| Low | 19 | 101 | – | – | ||||
| CD8+ TILs TC | ||||||||
| High | 25 | 0.57 (0.29–1.24) | 0.181 | 65 | 0.36 (0.17–1.27) | 0.143 | – | – |
| Low | 15 | 39 | – | – | ||||
| CD8+ TILs IM | ||||||||
| High | 43 | 0.48 (0.23–1.34) | 0.202 | NR | 0.00 (0.09–1.04) | 0.064 | – | – |
| Low | 15 | 39 | – | – | ||||
| CD45+ TILs TC | ||||||||
| High | 17 | 0.88 (0.45–1.66) | 0.676 | 65 | 0.78 (0.34–1.69) | 0.515 | – | – |
| Low | 15 | 36 | – | – | ||||
| CD45+ TILs IM | ||||||||
| High | 17 | 0.91 (0.44–1.84) | 0.984 | 54 | 0.79 (0.32–1.78) | 0.451 | – | – |
| Low | 17 | 36 | – | – | ||||
| FoxP3+ TILs TC | ||||||||
| High | 17 | 0.99 (0.52–1.89) | 0.982 | 54 | 0.98 (0.43–2.27) | 0.969 | – | – |
| Low | 15 | 52 | – | – | ||||
| FoxP3+ TILs IM | ||||||||
| High | 15 | 1.50 (0.79–3.16) | 0.211 | 35 | 2.40 (1.11–6.96) | 0.031 | 0.61 (0.23–1.61) | 0.319 |
| Low | 17 | 65 | ||||||
| TLS | ||||||||
| Present | 17 | 1.00 (0.48–2.10) | 0.999 | 52 | 0.65 (0.26–1.71) | 0.413 | – | – |
| Not present | 15 | NR | – | – | ||||
| CD3+ TLS | ||||||||
| High | 21 | 1.85 (0.36–7.72) | 0.525 | 65 | 0.34 (0.02–1.70) | 0.136 | – | – |
| Low | 19 | 52 | – | – | ||||
| CD8+ TLS | ||||||||
| High | 21 | 0.58 (0.27–1.18) | 0.140 | NR | 0.30 (0.14–0.79) | 0.016 | 4.39 (1.25–15.32) | 0.020 |
| Low | 11 | 35 | ||||||
| CD45+ TLS | ||||||||
| High | 17 | 1.05 (0.40–2.80) | 0.918 | 65 | 1.03 (0.33–3.25) | 0.949 | – | – |
| Low | 17 | 30 | – | – | ||||
| FoxP3+ TLS | ||||||||
| High | 11 | 2.42 (0.96–5.59) | 0.069 | 39 | 1.50 (0.54–4.45) | 0.439 | – | – |
| Low | 21 | 101 | – | – | ||||
| CD8/FoxP3-ratio IM | ||||||||
| Low | 15 | 1 | 29 | 1 | – | – | ||
| Equal | 17 | 0.65 (0.30–1.26) | 0.197 | 65 | 0.39 (0.13–0.83) | 0.021 | – | – |
| High | 26 | 0.32 (0.12–1.03) | 0.080 | NR | n/a | 0.042 | – | – |
| CD8/FoxP3-ratio TLS | ||||||||
| Low | 11 | 1 | 30 | 1 | – | – | ||
| Equal | 14 | 0.89 (0.32–2.37) | 0.804 | 101 | 2.13 (0.71–7.60) | 0.191 | – | – |
| High | NR | 3.65 (1.02–10.96) | 0.061 | NR | 6.99 (1.28–20.48) | 0.027 | – | – |
DFI disease-free survival to first pulmonary metastasis, IM invasive margin, NR 50 % recurrence/survival not reached, TC tumor center, TILs tumor-infiltrating lymphocytes, TLS tertiary lymphoid structure
Fig. 3.
Kaplan–Meier estimates regarding recurrence-free survival and overall survival of pulmonary metastases dependent on the density of CD8+ and FoxP3+ cells in TLS. Additionally the outcome for the CD8/FoxP3-ratio was calculated
Discussion
The aim of this study was to evaluate the role of TILs and TLSs in PM assessing a cohort of patients with CRC lung metastases. CD3+ TILs were found in every resected pulmonary metastatic specimen, highlighting the pivotal role of the adaptive immune system in local tumor microenvironment. We could show that tumor infiltrating CD8+ and FoxP3 positive cells were associated with disease free survival after pulmonary metastasectomy and OS.
CD8+ T cells represent a subpopulation of T cells, also known as cytotoxic T cells. They play an important role in the defense against viruses but also cancer cells. Upon activation they release cytotoxins (e.g., perforin, granzymes, granulysin) into infected or tumorous somatic cells, which eventually leads to the induction of apoptosis. Tumor infiltrating CD8+ cells can induce a potent tumorlytic response, which has been shown for various malignancies [25].
FoxP3+ cells are known as regulatory T-cells (Tregs). The have the ability to suppress effector T-cell function both in a paracrine and cell–cell-contact dependent manner [26]. Tregs are important for the maintenance of immunological tolerance, however, can also dampen antitumor response of the immune system. An expansion of the Treg pool experimentally leads to enhanced vulnerability of carcinogens and worse outcome [27, 28].
The role of TILs has been extensively studied in primary CRC. The inflammatory infiltrate was shown to correlate with the T-stage of primary CRC and even allowed a more precise prognosis on patients’ outcome compared to the UICC–TNM staging alone [10]. In the subgroup of rectal cancer patients, the prognostic value of the immune infiltrate (CD3 and CD8) was confirmed and additionally found to be a predictive marker for the response to preoperative chemo-radiotherapy [9]. Based on this data, an international consortium was founded to standardize and implement an adapted staging system taking the immune infiltrate (“Immunoscore”) into account [29].
In contrast to the evidence of the role of TILs in primary CRC, sparse data exists on TILs in lung metastases. To the best of our knowledge, by now only two studies have examined TILs in CRC lung metastases. Remark et al. showed in a retrospective cohort with CRC PM that a high density of CD8+ TILs conferred an improved OS (P = 0.039 in univariate analysis). Interestingly, CD8+ TILs at the tumor center and at the invasive margin had a similar prognostic impact [30]. In another study conducted in a Korean patient cohort with UICC stage IV colon cancer, including 21 patients with PM and 58 with liver metastases, a high CD8+ TILs density in the primary tumor, but not in the metastatic tissue (liver and lung together) had a beneficial impact on OS (log-rank test P = 0.017 and 0.232, respectively). The strongest positive prognostic impact was found for high CD45RO+ TILs in the primary and metastatic tissue (log-rank test P = 0.009 and 0.027, respectively). The prognostic impact of CD45RO+ TILs in the primary tumor remained significant in a multivariate model (RR 0.108; 95 % CI 0.021–0.546; P = 0.007). Interestingly, a high density of FoxP3+ TILs at the metastatic site was also associated with a favorable prognosis (log rank test P = 0.050) in this study [31]. This is in contrast to most of the published evidence on immunosurveillance in CRC and this finding could not be confirmed in our patient cohort [32, 33]. This discrepancy might be explained by the mixture of liver (73 %) and lung metastases (27 %), which were not separated in the outcome analysis [31]. Another explanation might be the spatial distribution of FoxP3 cells. Salama et al. reported a decreased survival of stage II CRC patients with low content of FoxP3+ T-cells within the tumor (HR 0.65; 95 % CI 0.48–0.89; P = 0.007), whereas the opposite was found when assessing adjacent colonic tissue (HR 1.42; 95 % CI 1.05–1.92; P = 0.023) [11]. The authors speculated that FoxP3+ T-regulatory cells might lose their ability to suppress antitumor immunity when they are found within the tumor tissue. Our results suggest differing impact of FoxP3+ TILs depending on their localization. Dense infiltration of FoxP3+ TILs in the infiltration zone was associated with impaired survival, whereas infiltration of FoxP3+ TILs in the tumor center did not alter survival. Moreover, high levels of FoxP3+ TILs at the invasive margin were significantly more common in patients with evidence for lymphatic invasion, which is believed to be a key-determinant of the outcome after pulmonary metastasectomy [19, 31]. Similar to two recent publications, which described the ratio between CD8+ and FoxP3+ TILs as prognostic factor superior to CD8+ and FoxP3+ TILs alone, we found the CD8/FoxP3- ratio to have a strong impact on OS in our patient cohort [34, 35]. In general, our observations in PMs imply differential roles of TILs dependent on their localization within the metastatic tissue. This has to be taken in consideration when assessing TILs in histological specimen and when defining cut-offs for statistical evaluation.
The present work is, to the best of our knowledge, the first analysis of presence and composition of TLS in CRC lung metastases. We could demonstrate that high levels of CD8+ cells as well as a high CD8/FoxP3-ratio in TLS correlated positively with patients’ OS after pulmonary metastasectomy (P = 0.016 and 0.027, respectively). Similar to our findings on TILs at the invasive margin, the balance of CD8+ and FoxP3+ in TLS seems to be a crucial factor for the survival of CRC patients with dissemination to the lung. Di Caro et al. found that TLS were present in 78.6 % of stages II and III primary CRC. The presence of TLS was a positive prognosticator only in stage II CRC (log rank P = 0.02), whereas the prognostic impact was lost in an advanced tumor stage (UICC stage III) [16]. Also in our cohort of stage IV CRC patients, the presence of TLS alone had no impact on recurrence-free and OS. Salama et al. evaluated the distribution of FoxP3+ cells in TLS in stage II colon cancer and described the high density of FoxP3+ cells in TLS as negative prognostic factor of OS (HR 4.22; 95 % CI 1.49–11.91; P = 0.007 in multivariate analysis) [36]. In our cohort, patients with high number of FoxP3+ cells in TLS evidenced a decreased recurrence-free and OS, without reaching the level of significance. Only 7.1 % of the primary CRC samples were rated as TLS positive in our cohort. This might indicate an insufficient immune response at the primary tumor site in patients subsequently developing metastatic disease. However, caution is warranted when interpreting this finding due to the small sample size.
Interestingly, the density of the immune infiltrate in primary tumors did not correlate with the infiltrate in PM. Considering the heterogeneity of tumors, the metastatic spreading of subpopulations of tumor cells of the primary cancer to distant organs might explain the different immuno-phenotype observed in our cohort [37]. In general, lung metastases appear to consist of more immunogenic tumor cells compared to the primary tumor site, since the density of CD3+, CD8+ and CD45+ TIL increased during progression of disease. Another possible explanation for this observation might be the unique immunological state of the lung. It is constantly exposed to environmental pathogens and therefor rich in residing immune cells.
Our findings suggest that patients with CRC lung metastases is a heterogeneous group regarding the tumor biology. This might have implications on the management of these patients. Histological evidence for an aggressive tumor biology might have consequences regarding the offered adjuvant chemotherapy, tumor surveillance strategies and a possible future re-metastasectomy.
There are several limitations to this study. First, no uniform protocol for pseudo-neoadjuvant and pseudo-adjuvant chemotherapeutic regimens was applied. According to the preferences of the referring oncologist, different schemes of chemotherapy were administered to the patients. As chemotherapeutic agents might contribute to the immune-editing of tumors, this is a possible confounder of this study. However we could not find a significant association between administration of chemotherapy before metastasectomy and the immune infiltrate in PMs. Moreover, the history of chemotherapy before metastasectomy did not affect the outcome after lung metastasectomy. Second, patients eligible for surgery are a subgroup and do not represent the whole population of patients with lung metastases from CRC. Thus, our findings might not be extrapolated to all patients with CRC PMs due to this selection bias. Last, although this is currently the biggest cohort of patients with CRC PM in which the CD3+, CD8+, CD45RO+ and FoxP3+ TILs and TLS was assessed, the study might still be underpowered. A multi-institutional study with a considerable sample size will be necessary to further clarify the prognostic value of TILs and TLS in CRC lung metastases.
In summary, this is the first structured analysis of CD3+, CD8+, CD45RO+ and FoxP3+ TILs and TLS in the setting of curative pulmonary metastasectomy, including more than 50 patients with CRC lung metastases. Our results suggest that especially the balance of effector CD8+ and regulatory FoxP3+ TILs play a crucial role during immune-editing of metastatic CRC and thus, predicting outcome of patients after pulmonary metastasectomy with curative intent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (TIFF 14823 kb)
Supplementary Table 1 Cut-offs used for dichotomization
Supplementary Table 2 Semi-quantitative description of CD3+, CD8+, CD45RO+ and FoxP3+ TLS in CRC pulmonary metastases
Supplementary Table 3 Association of CD3+, CD8+, CD45RO+ and FoxP3+ TLS with clinicopathological characteristics. The number of samples in which TLS could be found is provided in the first row 26
Supplementary Table 4 Semi-quantitative description of tumor-infiltrating lymphocytes in corresponding primary colorectal cancer (n = 31)
Supplementary Table 5 Spearman’s rho and P-values comparing the semiquantitative CD3+, CD8+, CD45RO+ and FoxP3+ TIL density in primary CRC and corresponding pulmonary metastases
Supplementary Fig. 1 Comparison of CD3+, CD8+, CD45RO+ and FoxP3+ TILs in CRC pulmonary metastases (m) and primary tumors (p) in percent
Acknowledgments
This study was supported by a Research Grant (#15880) provided by the Austrian Federal Bank (OeNB), by a Grant provided by Initiative Krebsforschung (Project Title “Tumorimmunologie von Hirnmetastasen”) and by the Christian Doppler Laboratory for Cardiac and Thoracic Diagnosis and Regeneration.
References
- 1.Mitry E, et al. Epidemiology, management and prognosis of colorectal cancer with lung metastases: a 30-year population-based study. Gut. 2010;59(10):1383–1388. doi: 10.1136/gut.2010.211557. [DOI] [PubMed] [Google Scholar]
- 2.Erstad DJ, Tumusiime G, Cusack JC., Jr Prognostic and predictive biomarkers in colorectal cancer: implications for the clinical surgeon. Ann Surg Oncol. 2015;22(11):3433–3450. doi: 10.1245/s10434-015-4706-x. [DOI] [PubMed] [Google Scholar]
- 3.Renaud S, Falcoz PE. How can we identify new biomarkers for patients with for lung metastasectomy in colorectal cancer. Future Oncol. 2015;11(15):2109–2111. doi: 10.2217/fon.15.124. [DOI] [PubMed] [Google Scholar]
- 4.Owusu BY, et al. Prognostic and predictive significance of stromal fibroblasts and macrophages in colon cancer. Biomark Cancer. 2015;7(Suppl 1):29–37. doi: 10.4137/BIC.S25247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schweiger T, et al. Prognostic factors in pulmonary metastasectomy: spotlight on molecular and radiological markers. Eur J Cardiothorac Surg. 2014;45(3):408–416. doi: 10.1093/ejcts/ezt288. [DOI] [PubMed] [Google Scholar]
- 6.Schweiger T, et al. Stromal expression of heat-shock protein 27 is associated with worse clinical outcome in patients with colorectal cancer lung metastases. PLoS One. 2015;10(3):e0120724. doi: 10.1371/journal.pone.0120724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Junttila MR, de Sauvage FJ. Influence of tumour micro-environment heterogeneity on therapeutic response. Nature. 2013;501(7467):346–354. doi: 10.1038/nature12626. [DOI] [PubMed] [Google Scholar]
- 8.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Anitei MG, et al. Prognostic and predictive values of the immunoscore in patients with rectal cancer. Clin Cancer Res. 2014;20(7):1891–1899. doi: 10.1158/1078-0432.CCR-13-2830. [DOI] [PubMed] [Google Scholar]
- 10.Mlecnik B, et al. Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol. 2011;29(6):610–618. doi: 10.1200/JCO.2010.30.5425. [DOI] [PubMed] [Google Scholar]
- 11.Salama P, et al. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol. 2009;27(2):186–192. doi: 10.1200/JCO.2008.18.7229. [DOI] [PubMed] [Google Scholar]
- 12.Donnem T, et al. Stromal CD8+ T-cell density—a promising supplement to TNM staging in non-small cell lung cancer. Clin Cancer Res. 2015;21(11):2635–2643. doi: 10.1158/1078-0432.CCR-14-1905. [DOI] [PubMed] [Google Scholar]
- 13.Miyashita M, et al. Prognostic significance of tumor-infiltrating CD8+ and FOXP3+ lymphocytes in residual tumors and alterations in these parameters after neoadjuvant chemotherapy in triple-negative breast cancer: a retrospective multicenter study. Breast Cancer Res. 2015;17(1):124. doi: 10.1186/s13058-015-0632-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giraldo NA, et al. Orchestration and prognostic significance of immune checkpoints in the microenvironment of primary and metastatic renal cell cancer. Clin Cancer Res. 2015;21(13):3031–3040. doi: 10.1158/1078-0432.CCR-14-2926. [DOI] [PubMed] [Google Scholar]
- 15.McMullen TP, et al. Survival in rectal cancer is predicted by T cell infiltration of tumour-associated lymphoid nodules. Clin Exp Immunol. 2010;161(1):81–88. doi: 10.1111/j.1365-2249.2010.04147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Caro G, et al. Occurrence of tertiary lymphoid tissue is associated with T-cell infiltration and predicts better prognosis in early-stage colorectal cancers. Clin Cancer Res. 2014;20(8):2147–2158. doi: 10.1158/1078-0432.CCR-13-2590. [DOI] [PubMed] [Google Scholar]
- 17.Halama N, et al. Hepatic metastases of colorectal cancer are rather homogeneous but differ from primary lesions in terms of immune cell infiltration. Oncoimmunology. 2013;2(4):e24116. doi: 10.4161/onci.24116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keim S, et al. Sequential metastases of colorectal cancer: immunophenotypes and spatial distributions of infiltrating immune cells in relation to time and treatments. Oncoimmunology. 2012;1(5):593–599. doi: 10.4161/onci.20179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schweiger T, et al. Increased lymphangiogenesis in lung metastases from colorectal cancer is associated with early lymph node recurrence and decreased overall survival. Clin Exp Metastasis. 2015;33(2):133–141. doi: 10.1007/s10585-015-9763-9. [DOI] [PubMed] [Google Scholar]
- 20.Berghoff AS, et al. Density of tumor-infiltrating lymphocytes correlates with extent of brain edema and overall survival time in patients with brain metastases. Oncoimmunology. 2016;5(1):e1057388. doi: 10.1080/2162402X.2015.1057388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berghoff AS, et al. Characterization of the inflammatory response to solid cancer metastases in the human brain. Clin Exp Metastasis. 2013;30(1):69–81. doi: 10.1007/s10585-012-9510-4. [DOI] [PubMed] [Google Scholar]
- 22.Menon AG, et al. Immune system and prognosis in colorectal cancer: a detailed immunohistochemical analysis. Lab Investig. 2004;84(4):493–501. doi: 10.1038/labinvest.3700055. [DOI] [PubMed] [Google Scholar]
- 23.Koelzer VH, et al. CD8/CD45RO T-cell infiltration in endoscopic biopsies of colorectal cancer predicts nodal metastasis and survival. J Transl Med. 2014;12:81. doi: 10.1186/1479-5876-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bender R, Lange S. Adjusting for multiple testing—when and how? J Clin Epidemiol. 2001;54(4):343–349. doi: 10.1016/S0895-4356(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 25.Nesbeth Y, Conejo-Garcia JR. Harnessing the effect of adoptively transferred tumor-reactive T cells on endogenous (host-derived) antitumor immunity. Clin Dev Immunol. 2010;2010:139304. doi: 10.1155/2010/139304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zou W. Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol. 2006;6(4):295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 27.Nishikawa H, et al. Accelerated chemically induced tumor development mediated by CD4+ CD25+ regulatory T cells in wild-type hosts. Proc Natl Acad Sci USA. 2005;102(26):9253–9257. doi: 10.1073/pnas.0503852102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishikawa H, et al. CD4+ CD25+ T cells responding to serologically defined autoantigens suppress antitumor immune responses. Proc Natl Acad Sci USA. 2003;100(19):10902–10906. doi: 10.1073/pnas.1834479100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galon J, et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J Pathol. 2014;232(2):199–209. doi: 10.1002/path.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Remark R, et al. Characteristics and clinical impacts of the immune environments in colorectal and renal cell carcinoma lung metastases: influence of tumor origin. Clin Cancer Res. 2013;19(15):4079–4091. doi: 10.1158/1078-0432.CCR-12-3847. [DOI] [PubMed] [Google Scholar]
- 31.Lee WS, et al. Clinical impact of tumor-infiltrating lymphocytes for survival in curatively resected stage IV colon cancer with isolated liver or lung metastasis. Ann Surg Oncol. 2013;20(2):697–702. doi: 10.1245/s10434-012-2752-1. [DOI] [PubMed] [Google Scholar]
- 32.Lee WS, et al. Clinical impact of tumor-infiltrating lymphocytes for survival in stage II colon cancer. Cancer. 2010;116(22):5188–5199. doi: 10.1002/cncr.25293. [DOI] [PubMed] [Google Scholar]
- 33.Hanke T, et al. High intratumoral FOXP3(+) T regulatory cell (Tregs) density is an independent good prognosticator in nodal negative colorectal cancer. Int J Clin Exp Pathol. 2015;8(7):8227–8235. [PMC free article] [PubMed] [Google Scholar]
- 34.Zeestraten EC, et al. FoxP3- and CD8-positive infiltrating immune cells together determine clinical outcome in colorectal cancer. Cancer Microenviron. 2013;6(1):31–39. doi: 10.1007/s12307-011-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suzuki H, et al. Intratumoral CD8(+) T/FOXP3 (+) cell ratio is a predictive marker for survival in patients with colorectal cancer. Cancer Immunol Immunother. 2010;59(5):653–661. doi: 10.1007/s00262-009-0781-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salama P, et al. FOXP3+ cell density in lymphoid follicles from histologically normal mucosa is a strong prognostic factor in early stage colon cancer. Cancer Immunol Immunother. 2012;61(8):1183–1190. doi: 10.1007/s00262-011-1191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Hajj M, et al. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100(7):3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1 (TIFF 14823 kb)