Introduction
Lupus miliaris disseminatus faciei (LMDF) is an inflammatory dermatosis characterized by 1- to 3-mm red-to-yellow-brown papules on the central and lateral face, particularly on and around the eyelids. Lesions can occur singly or in crops. The discrete papules appear yellow-brown (“apple-jelly”) on diascopy and as epithelioid cell granulomas histologically, thus, resembling tuberculosis, sarcoidosis, or other granulomatous diseases.1 LMDF classically presents on the face; however, an increasing number of cases are reported with extrafacial involvement.1, 2, 3, 4, 5, 6 We describe a unique presentation of LMDF characterized predominantly by bilateral axillae involvement.
Case
A healthy, 48-year-old white woman presented with a persistent 2.5-month history of an asymptomatic, nonpruritic papular eruption in her bilateral axillae and a similar but less robust eruption on the lateral eyelids. She had a history of zirconium-based antiperspirant deodorant and shaving cream use but otherwise denied application of topical products to her axillae. Physical examination found numerous reddish-brown, firm, nonblanching, 2- to 3-mm papules spread throughout the left axilla (Fig 1) and right axilla. There were a few, very subtle, 2- to 3-mm skin-to-pink-colored papules around the lateral canthi of both eyes, superiorly and inferiorly. There was no appreciated lacrimal gland hypertrophy. Punch biopsies from the left superior axilla (Figs 2 and 3) and left zygoma were performed.
Fig 1.
Diffuse red-brown 2- to 3-mm firm papules within the axillary vault.
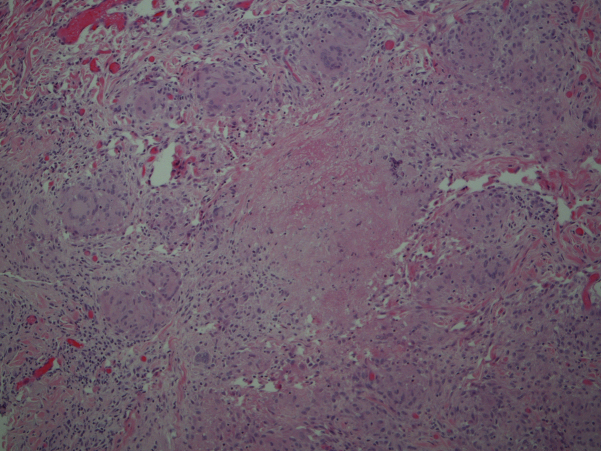
Fig 2.
Histologic examination of a punch biopsy taken from the patient's left axilla shows aggregates of palisading epithelioid cells, caseation necrosis, and multinucleated giant cells. (Hematoxylin-eosin stain; original magnification: ×10.)
Fig 3.
High-power view of multinucleated giant cells and caseation necrosis (Hematoxylin-eosin stain; original magnification: ×40.)
Histopathologic analysis found dermal aggregates of palisading epithelioid cells with occasional neutrophils and fibrin deposition. Multinucleated giant cells were noted and occasionally exhibited phagocytosis of elastic fibers. Focal necrosis occurred in some of the granulomas. Staining for fungi and acid-fast bacilli was negative.
Given the granulomatous histology, the patient underwent further workup for sarcoidosis, including chest radiograph, complete blood count, comprehensive metabolic panel, and serum electrophoresis, all of which were normal. Her tuberculin skin test result was negative. She had no lymphadenopathy, hepatosplenomegaly, lacrimal enlargement, or family history of sarcoidosis. Clinicopathologic correlation led to the final diagnosis of LMDF. The patient was started on minocycline, 100 mg by mouth once daily. She noted near complete resolution of the rash 12 months after therapy.
Discussion
The cause of LMDF remains unclear. In 1878, Fox7 reported on disseminated follicular lupus, and soon after in 1903 Radcliffe-Crocker designated the term acne agminata to describe the grouped eruptions of discrete, dull red-brown papules, which spontaneously involuted leaving pigmented scars.8 Initially, LMDF was considered a variant of lupus vulgaris or a tuberculid, but Mycobacterium tuberculosis has not been found in active lesions.9 LMDF was proposed to be a variant of sarcoidosis given its similar features on diascopy; however, the variably present caseous necrosis and lack of systemic disease argue against this. Others have highlighted the clinical overlap between LMDF and granulomatous-type rosacea. Although the conditions are quite similar, patients with LMDF lack flushing and telangiectasia, have eyelid involvement, and heal with scarring. Thus, many now view LMDF as its own distinct rosacealike syndrome.1
This patient's clinical presentation is striking given the predominate bilateral axillae involvement and the very subtle, more classic facial manifestations. Throughout the last 2 decades, there have been a number of reported cases with extra-facial LMDF, with most involving the neck, axillae, groin, or extremities.1, 2, 3, 4, 5, 6 Notably, in 2003, van de Scheur and colleagues1 reported 3 different cases of LMDF, and, as in our case, extrafacial lesions were prominent, and a full workup for granulomatous skin diseases was negative.2
A variety of treatments for LMDF have been attempted, but controlled studies are lacking, and clinicians often find LMDF difficult to control. Topical steroids are ineffective and are not recommended for LMDF. Other reported therapies of variable benefit include prednisone, injectable steroids, tetracyclines, erythromycin, dapsone, clofazimine, isotretinoin, and topical tacrolimus.3, 10 Additionally, treatment-resistant LMDF responds to fractioned laser and the 1450-nm diode laser.11 Active disease usually persists for 1 to 2 years and resolves spontaneously, unfortunately with the potential for disfiguring scarring.
In 2000, Skowron et al12 proposed a name change from LMDF to FIGURE (facial idiopathic granulomas with regressive evolution). To date, it does not appear that this name change has been widely used. Given the increasingly reported appearance of LMDF in nonfacial sites, we propose that this entity would be more suitably described as lupus miliaris disseminatus. We are hopeful that this knowledge leads to improved diagnostic acumen and speedier identification of extrafacial lupus miliaris disseminatus.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.van de Scheur M.R., van der Waal R.I., Starink T.M. Lupus miliaris disseminatus faciei: a distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology. 2003;206:120–123. doi: 10.1159/000068457. [DOI] [PubMed] [Google Scholar]
- 2.Kim D.S., Lee K.Y., Shin J.U., Roh M.R., Lee M.G. Lupus miliaris disseminatus faciei without facial involvement. Acta Derm Venereol. 2008;88:504–505. doi: 10.2340/00015555-0483. [DOI] [PubMed] [Google Scholar]
- 3.Mullan E., Green P., Pasternak S. Lupus miliaris disseminatus faciei with extrafacial involvement in a 17-year-old white girl. J Cutan Med Surg. 2011;15:340–343. doi: 10.2310/7750.2011.10034. [DOI] [PubMed] [Google Scholar]
- 4.Bedlow A.J., Otter M., Marsden R.A. Axillary acne agminata (lupus miliaris disseminatusfaciei) Clin Exp Dermatol. 1998;23:125–128. doi: 10.1046/j.1365-2230.1998.00333.x. [DOI] [PubMed] [Google Scholar]
- 5.Farrar C.W., Bell H.K., Dobson C.M., Sharpe G.R. Facial and axillary acne agminata. Br J Dermatol. 2003;149:1076. doi: 10.1111/j.1365-2133.2003.05641.x. [DOI] [PubMed] [Google Scholar]
- 6.Hillen U., Schröter S., Denisjuk N., Jansen T., Grabbe S. Axillary acne agminata (lupus miliaris disseminatus faciei with axillary involvement) J Dtsch Dermatol Ges. 2006;4:858–860. doi: 10.1111/j.1610-0387.2006.06112.x. [DOI] [PubMed] [Google Scholar]
- 7.Fox T. Disseminated follicular lupus (simulating acne) Lancet. 1878;112:5–76. [Google Scholar]
- 8.Radcliffe-Crocker H. 3rd ed. Lewis; London: 1903. Diseases of the Skin. [Google Scholar]
- 9.Hodak E., Trattner A., Feuerman H. Lupus miliaris disseminatus faciei–the DNA of Mycobacterium tuberculosis is not detectable in active lesions by polymerase chain reaction. Br J Dermatol. 1997;137:614–619. doi: 10.1111/j.1365-2133.1997.tb03797.x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Mutairi N. Nosology and therapeutic options for lupus miliaris disseminatus faciei. J Dermatol. 2011;38:864–873. doi: 10.1111/j.1346-8138.2011.01244.x. [DOI] [PubMed] [Google Scholar]
- 11.Jih M.H., Friedman P.M., Kimyai-Asadi A., Friedman E.S., Hymes S.R., Goldberg L.H. Lupus miliaris disseminatus faciei: Treatment with the 1450-nm diode laser. Arch Dermatol. 2005;141:143–145. doi: 10.1001/archderm.141.2.143. [DOI] [PubMed] [Google Scholar]
- 12.Skowron F., Causeret A.S., Pabion C., Viallard A.M., Balme B., Thomas L. FIGURE: facial idiopathic granulomas with regressive evolution. Is Lupus miliaris disseminatus faciei still an acceptable diagnosis in the third millennium? Dermatology. 2000;201:287–289. doi: 10.1159/000051539. [DOI] [PubMed] [Google Scholar]