Abstract
Objective
Little is known about the patterns among individuals in the long-term course of suicidal thoughts and behaviors (STBs). The objective of this study was to identify developmental trajectories of STBs from adolescence through young adulthood, as well as risk and protective covariates, and nonsuicidal outcomes associated with these trajectories.
Method
180 adolescents (ages 12–18 at recruitment) were repeatedly assessed over an average of 13.6 years (2,273 assessments) since their psychiatric hospitalization. Trajectories were based on ratings of STBs at each assessment. Covariates included psychiatric risk factors (proportion of time in episodes of psychiatric disorders, hopelessness, trait anxiety, impulsivity, and aggression in adulthood, sexual and physical abuse, parental history of suicidal behavior), protective factors (survival and coping beliefs, social support in adulthood, parenthood), and nonsuicidal outcomes (social adjustment and functional impairment in adulthood, school drop-out, incarcerations).
Results
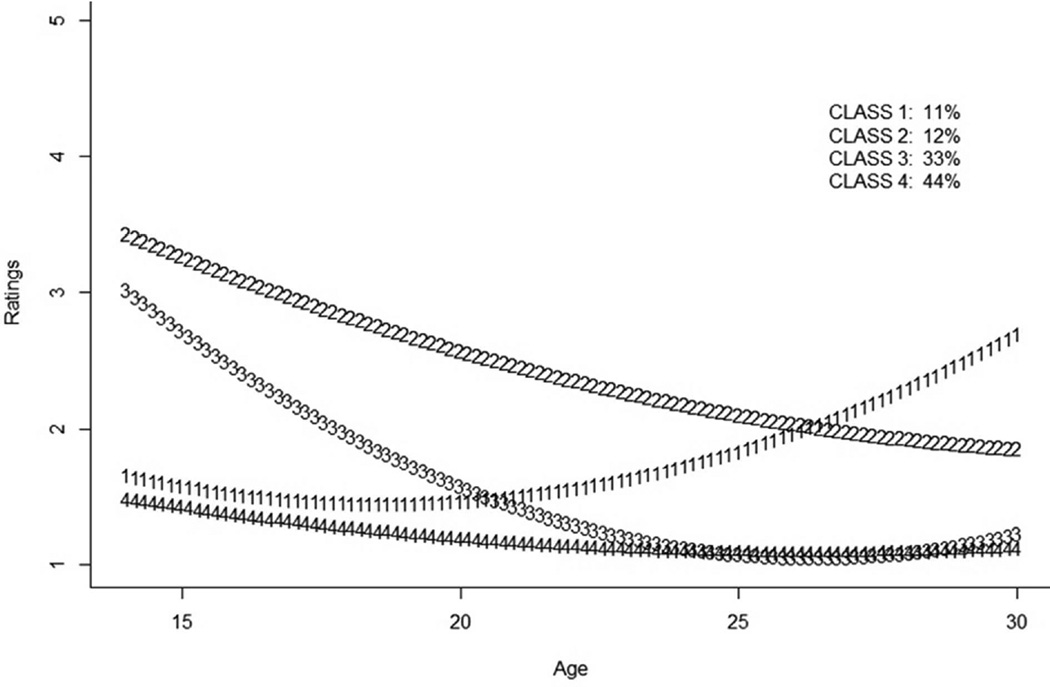
Using a Bayesian group-based trajectory model, four trajectories of STBs were identified: (1) an Increasing Risk class (11%), (2) a Highest Overall Risk class (12%), (3) a Decreasing Risk class (33%), and (4) a Low Risk class (44%). The four classes were associated with distinct patterns of correlates in risk and protective factors and nonsuicidal outcomes.
Conclusion
Adolescents and young adults have heterogeneous developmental trajectories of STBs. These trajectories and their covariates may inform strategies for predicting STBs and targeting interventions for individuals at risk for suicidal behavior.
Keywords: Suicide ideation, Suicide attempts, Development, Longitudinal, Trajectories
INTRODUCTION
The developmental period of adolescence through young adulthood is a peak time for the emergence of suicidal thoughts and behaviors (STBs).1–3 After emergence of STBs, however, adolescents differ strikingly in the degree to which they continue to have suicidal thoughts or engage in suicidal behavior. Over the course of development, some adolescents and young adults have suicidal thoughts but never consider specific plans, whereas others have plans but never act on them.3 Some individuals attempt suicide on a single occasion but then never attempt suicide again, whereas others are chronically suicidal, with recurring STBs. Nonetheless, few prospective studies have examined the heterogeneity in developmental trajectories of STBs or the correlates of these patterns over time.
The characterization of developmental trajectories of a range of STBs and their correlates from adolescence through young adulthood may have significant implications for prevention and treatment interventions. To date, several longitudinal studies have focused on trajectories of other characteristics (e.g., depression, sexual identity) in relation to STBs,4,5 or on trajectories of STBs defined by covariates (e.g., body weight perceptions, sexual orientation).6–8 In other studies, trajectories of suicide ideation have been examined in relation to other variables, including suicide attempts and rehospitalization.9–13 Few studies have focused on trajectories of both suicidal thoughts and suicide attempts,7,14 and none to our knowledge have examined trajectories, not a priori defined by other characteristics, of a continuum of suicidal ideation and behavior over a prolonged period of time. Moreover, none of the longitudinal studies to our knowledge have examined the heterogeneous course of STBs through adolescence in relation to functioning across multiple domains in adulthood.
The present naturalistic, prospective study of adolescents followed after psychiatric hospitalization into adulthood, with multiple assessments per participant, provided an opportunity to examine different developmental trajectories of STBs, as well as associated demographic variables, risk factors, protective factors, and nonsuicidal outcomes. The sample was high risk because participants had histories of psychiatric hospitalization, which is associated with increased rates of suicidal behaviors.9,12,15 Risk factors examined in relation to the trajectories included psychiatric disorders,16,17 histories of sexual and other physical abuse,18,19 family histories of suicidal behavior,20 trait anxiety and hopelessness over time,21 and impulsivity and hostility in adulthood.22,23 Protective factors included survival and coping beliefs,24 parenthood,25,26 and social support.27 The risk and protective factors were chosen primarily because of the strength of their relationship to STBs in the literature; however, these variables also are prominent of familial transmission of suicidal behavior proposed by Brent et al.,28 the stress diathesis model proposed by Mann et al.,29 as well as cognitive behavioral intervention approaches to suicidal behavior.30,31 Nonsuicidal outcomes examined in relation to the trajectories included school drop-out, incarcerations, functional impairment during adulthood, and social adjustment during adulthood. To the extent that suicidal behavior often occurs in the context of more generalized emotional and behavioral dysregulation, we expected that STBs would be associated with other areas of impairment or adjustment.5,32
METHOD
Participants
The 180 participants in this study were recruited from adolescents consecutively discharged from a psychiatric inpatient unit between September 1991 and April 1995. Inclusion criteria included (a) ages 12 to 19 years at hospitalization, (b) hospitalization for 10 or more days (the national length of stay was an average of 23.6 days at study initiation),33 (c) ability to complete the assessments in the hospital, and (d) residency in North Carolina or Virginia at recruitment. Exclusion criteria included (a) a serious physical disease, (b) intellectual disability, and (c) prior enrollment of a sibling in the study. To recruit the sample, we tried to contact 225 adolescents and their parents/legal guardians following hospital discharge. We reached 96% of the eligible sample, not counting one youth who died of medical reasons prior to the follow-up. Of these, 84% (N = 180) agreed to participate. The demographic characteristics of the sample are presented in Table 1.
Table 1.
Demographic Information for Longitudinal Sample (N=180)
| Variable | Distribution |
|---|---|
| Gender, n (%) | |
| Female | 91 (51) |
| Male | 89 (49) |
| Race/ethnicity, n (%) | |
| European American | 144 (80) |
| African American | 30 (16.7) |
| Other | 6 (3.3) |
| Agea, M (SD; range) | 14.8 y (1.6 y; 12.0–18.4 y) |
| Department of Social Services Custodya, n (%) |
29 (16) |
| SES for individuals not in Department of Social Services Custodya, n (%) |
|
| I | 5 (3.3) |
| II | 19 (12.6) |
| III | 33 (21.9) |
| IV | 45 (29.8) |
| V | 49 (32.4) |
Note: SES = socioeconomic status
At index hospitalization.
By study entry, 42% of youths (n = 75) had attempted suicide and another 33% (n = 60) reported current suicide ideation. Thirty-four of the 105 individuals (32%) who had not attempted suicide by their index hospitalization made a subsequent suicide attempt following discharge. As of December 9, 2011, participants had been followed up to 19.3 years (M = 13.6 years, Median = 15.0 years; SD = 4.5 years), for a total of 2,273 assessments. The average age of participants at last assessment was 28.5 years (SD = 4.9 years; range = 12.9 years to 34.6 years). The number of assessments per participant ranged from 2 to 26 (Mean = 12.6, Median = 13, SD = 5.1). By the cutoff date, 11% (n = 20) of the sample had actively dropped out of the study, and 4.4% (n = 8) of participants had died, but none had died due to suicide. The causes of death for individuals who died included vehicular accident (n=3), pedestrian accident (n=1), fire (n=1), homicide (n=2), and physical illness (n=1). Four of these deaths were related to use of substances. Six participants (3.3%) were administratively withdrawn from the study because of prolonged lost contact.
Instruments and Assessments
STBs: STBs were examined as an ordinal variable reflecting severity, as suggested in an Institute of Medicine report34 and consistent with the emphasis by the National Institute of Mental Health on dimensional measures of functioning.35 The most severe STB since the last assessment (or index hospitalization) was rated for each assessment: (1) no suicide ideation, (2) suicide ideation without means envisioned, (3) suicide ideation with means envisioned, (4) one suicide attempt, or (5) multiple suicide attempts. The dimensional approach to characterizing STBs has previously been shown to have validity36 and follows a logical progression of severity. Namely, even if very briefly, one has to think about suicide before choosing a method; one must choose a method before acting on suicidal thoughts; and one has to make a single suicide attempt before engaging in multiple attempts. A suicide attempt was defined as a potentially self-injurious behavior with at least some intent to die, and suicide ideation was defined as any thoughts about attempting suicide, regardless of intent.37,38 The primary source of information for ratings was the semi-structured clinical interview administered to participants, either the Interview Schedule for Children and Adolescents (ISCA) or the Follow-Up Interview Schedule for Adults (FISA).39 The former was administered to adolescents and adult informants, and the latter was administered to participants only after their 18th birthday. Ratings were made on the basis of all available information including diagnostic interviews and treatment records. Each rating was independently reviewed; discrepancies were discussed and resolved by consensus among the investigators. An interrater reliability trial indicated high levels of agreement (96.4%; κ = 0.92) in ratings of severity of STBs.40
Demographic Variables
Gender, age, race/ethnicity, and socioeconomic status (SES) were assessed with the structured Intake and Follow-Up Information Sheet.
Risk Factors
The amounts of time that an individual spent in an episode (or episodes) of the most common psychiatric disorders, divided by that individual’s total time observed during the follow-up, were calculated as summary indices of psychiatric morbidity. Psychiatric disorders examined in this study included major depressive disorder (MDD), dysthymic disorder, generalized anxiety disorder (GAD), panic disorder, attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder, conduct disorder/antisocial personality disorder, and substance use disorders (SUD). The symptoms of psychiatric disorders (and their time course) were assessed with the ISCA and the FISA.39 Diagnoses were assigned using DSM-IV diagnostic criteria.41 To avoid losing potentially important clinical information, diagnoses of GAD were given even when the symptoms occurred exclusively in the context of mood disorders. Operational rules specified by Kovacs et al. were used to determine onset and offset dates of episodes of disorder.42 Diagnoses were independently reviewed, discussed in conference, and discrepancies were resolved by consensus.
In addition to diagnoses, trait anxiety and hopelessness were repeatedly assessed over the follow-up with the State-Trait Anxiety Inventory43 and the Beck Hopelessness Scale.44,45 Self-reported hostility and aggression and impulsivity during adulthood were repeatedly assessed with the Buss-Durkee Hostility Inventory and the Barrett Impulsiveness Scale.46,47 These repeated assessments of trait anxiety, hopelessness, hostility and aggression, and impulsivity were considered as time-varying covariates of trajectories.
The presence/absence of sexual and/or other physical abuse prior to the age of 18 was determined on the basis of all available information, including the diagnostic interview, hospitalization and other treatment records, legal records, and Department of Social Services records. Discrepancies between independent coders were reviewed and resolved by consensus. An interrater reliability trial indicated good agreement regarding presence of physical and sexual abuse (86%; κ = .68 and 0.70). Parental history of suicide and suicide attempts were assessed retrospectively at the first assessment after February 2004 with the Family History Screen.48 Abuse and parental history were considered as fixed, discrete covariates in models.
Protective Factors
Survival and coping beliefs were repeatedly assessed with the Survival and Coping Beliefs subscale of the Reasons for Living Inventory.49 Beginning in February 2004, perceptions of social support in adulthood were repeatedly assessed with the Multidimensional Scale of Perceived Social Support.50 Parenthood (whether participants had biological children during the follow-up) was assessed at each follow-up using structured interview. Survival and coping beliefs and social support were considered timevarying covariates, whereas parenthood was reduced to a fixed, dichotomous variable.
Nonsuicidal Outcomes
School drop-out was assessed at each follow-up via structured interview until secondary school graduation or award of high school graduate equivalency diploma (GED). Incarcerations were coded from our structured study interview and verified when possible with legal records. Social adjustment in adulthood was repeatedly assessed after February 2004 with the total score from the Social Adjustment Scale – Self-Report (SAS-SR).51 Functional impairment in adulthood in the areas of Behavior toward Others and Role Performance were assessed with an adult extension of the Child and Adolescent Functional Assessment Scale (CAFAS), the CAFAS Young Adult Version.52
Procedures
Follow-up assessments were initially scheduled every six to eight months post-hospitalization but were later tapered to reduce participant burden and study costs until assessments were scheduled annually (please see40 for additional details). The number of assessments and the timing between assessments varied within and between participants due to multiple factors, including participant preferences, lost contact, and lapses in grant funding. Research interviewers were trained doctoral- and master-level clinicians. Initial informed assent and consent forms were signed by youth and parents/guardians. Participants were reconsented as adults. The study was approved by the institutional review boards of involved institutions.
Analysis Methods
A Bayesian finite mixture model was used for identifying the longitudinal trajectories of STBs and their correlates.53,54 This modeling approach was chosen because it (1) accommodates differing numbers of assessments, missing data, and unequal spacing between and within participants timing of assessments; (2) accounts simultaneously for uncertainty in the model and parameters; and (3) assumes that individuals have different probabilities of belonging to each class.
Data analysis occurred in three stages (technical details are provided in Supplement 1, available online). In the first stage, using Monte Carlo/Markov Chain (MCMC) simulations, we fit a semi-parametric mixture quadratic growth model of STBs as a function of age, and probabilistically determined the number of latent classes.55,56 To minimize the chances of identifying classes with small probabilities of estimated membership, we stipulated that latent classes would include at least 10% of the sampled population. In the second stage of modeling, using simulations of class memberships, we determined the differing probabilities individuals had of belonging to each of the different classes. In the third stage of modeling, risk and protective factors and nonsuicidal outcomes were modeled as dependent variables as a function of the simulated class variables, using the simulations from the second set of modeling. Logistic models were used for dichotomous covariates, and normal regression models were used to examine continuous variables.
RESULTS
Identification of Trajectories
Four latent class trajectories were identified using MCMC simulation approaches: (1) a class with increasing risk beginning in adulthood (11%; “Increasing Class”); (2) a class that began at high risk in adolescence but gradually decreased risk through young adulthood (12%; “Highest Overall Risk Class”); (3) a class with markedly decreasing risk from adolescence through young adulthood (33%; “Decreasing Class”); and, a class that remained at relatively low risk throughout the follow-up (44%; “Lowest Risk Class”) (see Figure 1). The Low Risk class served as the reference class for analyses of covariates. This class had average ratings of close to 1 throughout the follow-up, indicating that individuals primarily associated with this class rarely reported suicidal ideation. In contrast, the Highest Overall Risk class had average ratings of between 3 and 4 (corresponding to suicide ideation with a method envisioned or a suicide attempt) at each assessment point through late adolescence.
Figure 1.
Developmental trajectories of suicide ideation and attempts. Note: Trajectories of suicide ideation and attempt ratings across 2,273 assessments from 180 participants. Ratings of the most severe suicidal thoughts and behaviors since the last assessment (or index hospitalization) correspond to the following scale: (1) no suicide ideation, (2) suicide ideation without means envisioned, (3) suicide ideation with means envisioned, (4) one suicide attempt, (5) multiple suicide attempts.
Lending validity to the trajectories, the number of pre-hospitalization suicide attempts was most strongly related to the two trajectories with highest risk in adolescence (see Table 2). Post-hospitalization attempts were higher in all three of the risk classes relative to the reference class, and were especially strongly related to the Highest Risk class. None of the trajectories were differentially related to whether participants died or had dropped out of the study.
Table 2.
Covariates of the Three Trajectory Classes With Increased Risk
| Covariates | Class 1 (Increasing) | Class 2 (Highest Overall) | Class 3 (Decreasing) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| b | se | z | b | se | z | b | se | z | |
| Internal Indicators of Validity | |||||||||
| Attrition (dropout + death) | 0.432 | 0.418 | 1.06 | −0.188 | 0.415 | −0.46 | −0.274 | 0.241 | −1.13 |
| Prehospitalization attempts | 0.080 | 0.289 | 0.27 | 1.062** | 0.287 | 3.724 | 0.877*** | 0.167 | 5.27 |
| Posthospitalization attempts | 0.936* | 0.415 | 2.24 | 4.417*** | 0.411 | 10.71 | 0.617* | 0.240 | 2.58 |
| Demographic | |||||||||
| Age at hospitalization | −0.374 | 0.435 | −0.86 | 0.931 | 0.431 | 2.16 | 0.861*** | 0.251 | 3.43 |
| Gender | 0.140 | 0.580 | 0.24 | 0.761 | 0.588 | 1.29 | 0.648 | 0.336 | 1.92 |
| Race/ethnicity | 0.775 | 0.862 | 0.90 | 1.215 | 0.989 | 1.23 | 0.203 | 0.402 | 0.51 |
| Diagnostic Risk Factorsa | |||||||||
| ADHD | −0.312 | 0.492 | 0.63 | 0.789 | 0.464 | 1.70 | 0.302 | 0.367 | 0.83 |
| CD | 0.103 | 0.507 | 0.20 | 0.694 | 0.441 | 1.57 | −0.053 | 0.236 | −0.23 |
| Dysthmic disorder | −0.043 | 0.479 | −0.09 | 0.718 | 0.459 | 1.56 | 0.165 | 0.388 | 0.43 |
| GAD | −0.546 | 0.807 | −0.68 | 1.603** | 0.571 | 2.81 | 0.589 | 0.358 | 1.52 |
| MDD | 0.424 | 0.406 | 1.04 | 1.227*** | 0.377 | 3.25 | 0.346 | 0.249 | 1.39 |
| ODD | 0.105 | 0.438 | 0.24 | 0.296 | 0.605 | 0.49 | −0.099 | 0.324 | −0.28 |
| Panic disorder | 0.031 | 0.829 | 0.04 | 0.995 | 0.538 | 1.85 | 0.756 | 0.503 | 1.51 |
| Phobic disorder | −0.527 | 0.691 | 0.76 | 1.151* | 0.585 | 1.97 | 0.056 | 0.551 | 0.10 |
| SUD | 0.176 | 0.481 | 0.37 | −0.084 | 0.412 | 0.21 | 0.032 | 0.281 | 0.12 |
| Other Risk Factors | |||||||||
| Aggression (adulthood) | 6.232* | 2.887 | 2.16 | 4.275 | 3.680 | 1.19 | 1.629 | 1.873 | 0.87 |
| Family history suicidal behavior | −1.000 | 0.991 | −1.00 | 0.826 | 0.626 | 1.32 | 0.250 | 0.411 | 0.61 |
| Hopelessness | 0.496 | 0.612 | 0.81 | 2.645** | 0.847 | 3.13 | 0.531 | 0.382 | 1.39 |
| Impulsivity (adulthood) | 10.017** | 3.296 | 3.05 | 7.108* | 2.954 | 2.40 | 2.073 | 1.927 | 1.07 |
| Physical abuseb | 0.610 | 0.587 | 1.04 | 0.892 | 0.579 | 1.54 | 0.249 | 0.347 | 0.72 |
| Sexual abuse | 0.340 | 0.597 | 0.60 | 1.218* | 0.591 | 2.06 | 0.597 | 0.343 | 1.74 |
| Trait anxiety | 4.391* | 2.246 | 1.96 | 11.800*** | 2.691 | 4.37 | 4.610** | 1.441 | 3.20 |
| Protective Factors | |||||||||
| Parenthood | −0.622 | 0.592 | −1.06 | −0.283 | 0.573 | −0.49 | 0.529 | 0.344 | 1.54 |
| Perceived social support | −0.430 | 0.292 | −1.47 | −0.159 | 0.344 | −0.46 | −0.113 | 0.185 | −0.62 |
| Survival and coping beliefs | −0.218 | 0.125 | −1.75 | −0.787** | 0.249 | −3.16 | −0.287** | 0.107 | 2.68 |
| Nonsuicidal Outcomes | |||||||||
| Impairment in behavior to others | 0.942* | 0.432 | 2.18 | 0.617 | 0.408 | 1.51 | 0.118 | 0.289 | 0.41 |
| Impairment in role performance | 1.077* | 0.515 | 2.08 | 0.874* | 0.443 | 1.97 | 0.269 | 0.320 | 0.84 |
| Overall social adjustment in adulthood |
9.734** | 3.108 | 3.13 | 11.074** | 3.625 | 3.05 | 1.810 | 2.159 | 0.83 |
| Incarcerationsc | −0.336 | 0.581 | −0.58 | −0.250 | 0.573 | 0.44 | −0.400 | 0.333 | −1.21 |
| School drop-outc,d | 0.335 | 0.600 | 0.56 | 0.444 | 0.595 | 0.76 | 0.107 | 0.333 | 0.32 |
Note: ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; GAD = generalized anxiety disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder; SUD = substance use disorder
Log(proportion) of time in episode of disorder, approximately normally distributed.
Other than sexual abuse.
Coded as binary variable (yes, no)
Participants were coded as dropping out of school even if they re-entered school and completed at a later time, or later received their Graduate Equivalency Degree
p ≤ .05,
p < .01,
p < .001
Four groups of covariates of the trajectories were examined in relation to the trajectories: demographic variables, risk factors, protective factors, and nonsuicidal outcomes. The specific results of analyses are presented in Table 2.
Demographic Variables
The four classes did not differ in gender or race/ethnicity distribution. The Decreasing Risk class was older at hospitalization than the Lowest Risk class.
Risk Factors
Each of the three classes with increased risk for STBs had higher levels of trait anxiety over the follow-up than the Lowest Risk class. The Highest Overall Risk class was associated with a greater proportion of time in episodes of MDD and GAD, a higher likelihood of sexual abuse, and more hopelessness than the Lowest Risk class. Moreover, the two classes with highest risk in adulthood (Highest Overall class and Increasing class) were both associated with increased impulsivity in adulthood, relative to the Lowest Risk class. The Increasing Risk class also had higher levels of self-reported aggression during adulthood than the Lowest Risk class.
Protective Factors
The two classes with increased risk during adolescence (Highest Overall Risk class, Decreasing class) were associated with lower survival and coping beliefs. There were no differences among the classes in perceptions of social support or parenthood.
Nonsuicidal Outcomes
The two classes with the highest risk in adulthood (Highest Overall Risk class, Increasing class) had more overall social adjustment difficulties and functional impairment in the area of role performance in adulthood than the Lowest Risk class. The Increasing Risk class also reported greater impairment in appropriateness of behavior towards others. The classes did not differ in likelihood of incarceration or school drop-out.
DISCUSSION
In this longitudinal study of high-risk adolescents followed through adulthood, we used a Bayesian approach to identify four distinct developmental trajectories of STBs. Each of the participants in this study had differing probabilities of being associated with each of the four trajectories. Previous studies have described the risk of individuals who are suicidal as a single group, examined trajectories of other risk factors in relation to STBs, examined trajectories of STBs in a priori defined subgroups, or examined separate trajectories of suicidal thoughts and suicide attempts. Building on these findings, this is the first prospective study to our knowledge to examine differences in the developmental trajectories of a continuum of STBs from adolescence through young adulthood, and individuals’ differing probabilities of being associated with each. This approach allowed examination of fluctuations over time in different levels of risk from suicidal thoughts to repeat suicide attempts; the large number of assessments per participant enabled greater precision in the modeling of these trajectories, and the relationship of other covariates with these trajectories.
The Highest Risk class appeared to be associated with particular vulnerability, as underscored not only by the higher risk for STBs in adolescence, but also by the fact that this was the only class with a higher likelihood of sexual trauma, and higher proportion of time in episodes of MDD and GAD. This class also was chronically anxious and hopeless, with fewer reasons for living over time, and had increased impulsivity during adulthood.
This was also one of two classes associated with greater impairment and social adjustment during young adulthood. The relationship between the Highest Risk trajectory and sexual abuse is important in terms of prediction. For most of the youths in this study who had been sexually abused, this was recognized prior to the index hospitalization. Hence, sexual abuse was an important predictor, available at the time of hospitalization, of particularly high risk for suicidal thoughts and behavior (as well as continuing high levels of depression and anxiety) from adolescence through adulthood. Because of the vulnerability associated with this class, clinicians should be aware that youths with characteristics similar to this class may need more intensive intervention to reduce STBs than some of the other at-risk youths.
The pattern of covariates associated with the Highest Risk class is similar to those described in a model by Brent et al.28 for the transmission of suicidal behavior from parent to child. In that model, sexual abuse was both directly related to increased suicidal behavior, and indirectly related through increased anxiety (and mood disorder, via the path with increased anxiety). Impulsivity additionally contributed to increased risk, both directly, and indirectly through increased anxiety and mood disorders. Family history of suicidal behavior did not distinguish the various groups of previously hospitalized youths, but the pattern of covariates does suggest the potential utility of this model for high risk of suicidal behavior that is not specific to familial transmission. The pattern is also similar to that described in the stress diathesis model of Mann et al.,29 wherein the combination of objective states (e.g., objective indices of depression, life stresses) and diatheses such as the tendency to experience hopelessness, impulsivity, greater perceived depression, or lower reasons for living, increases risk for a suicidal act.
The Increasing Risk class was marked by greater impulsivity and self-reported aggression in adulthood, as well as elevated trait anxiety. This class also was associated with impairment in role performance and interpersonal difficulties through adulthood. Because of the observational nature of the data, it is not clear if the interpersonal difficulties and impairment contribute to the risk of STBs, or if the other areas of impairment and STBs are all consequences of more general emotional and behavioral dysfunction, and the factors that contribute to that dysfunction. The possibility of more general emotional and behavioral dysfunction is consistent with research indicating that trajectories of higher depression and higher externalizing behavioral problems are associated with increased risk of suicide attempts.5 Therefore, even among high-risk individuals who are not evidencing high rates of STBs in adolescence, clinicians should be aware that the combination of impulsivity, aggression, anxiety, and interpersonal difficulties may be markers for increased risk as individuals begin the transition to adulthood.
The Decreasing Risk class also had high levels of trait anxiety and lower reasons for living, but in general, was the most similar to the Lowest Risk class. Whether they developed greater skills with emotional and behavioral regulation as they matured, or benefited from the changes in circumstances as they transitioned into living more independently, individuals associated with this class appeared to be at much less risk as they got older. The fact that there are a significant group of individuals whose risk markedly decreases as they reach adulthood underscores the heterogeneity among individuals who are suicidal and their outcomes over time. Given this heterogeneity, a logical next step would be to develop and examine the effectiveness of targeted interventions that are “personalized” to not only the STBs, but also their associated risk factors.
These findings need to be considered in the context of the limitations of our approach. First, we were able to closely characterize this cohort over a sizable window of time from adolescence through adulthood, but the sample at study entry was recruited from a single inpatient psychiatric facility, which may limit the generalizability of results. Second, interview-based information from the repeated assessments was not blindly collected, introducing the possibility of bias in data collection. Third, we chose to characterize STBs along a continuum. This approach allowed us to examine severity of STBs over time, but also limited our ability to directly compare these results to other studies focusing only on either suicidal ideation or attempts. Fourth, because of the number of covariates and outcomes examined in this study, our results could have been affected by Type I error. Fifth, it should be acknowledged that we chose the potential covariates in this study primarily because of their established relationship with STBs in the literature, not on the basis of an overarching theoretical model being tested. While our findings are certainly consistent with some models of suicidal behavior, it is also true that there are a number of established covariates of STBs (e.g., gender identity and sexual orientation, number of adversities, religiosity) that were not examined in this study.
With those caveats notwithstanding, the current results highlight the heterogeneity of developmental patterns of STBs among different groups of at-risk youths and young adults, and the factors that are associated with this risk over time. This information, in turn, has significant implications for prediction by clinicians, the development of better predictive tools, and the development and evaluation of targeted intervention efforts.
Supplementary Material
Acknowledgments
This longitudinal study was initiated with funding from the William T. Grant Foundation. The research receives current support from the National Institute of Mental Health of the National Institutes of Health (R01MH048762). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Dr. Erkanli served as the statistical expert for this research.
The authors appreciate the assistance of Andrew M. Mitchell, MMFT, Wake Forest University School of Medicine, with this study.
Disclosure: Dr. Goldston has received support from the National Institute of Mental Health, the National Institute on Alcohol Abuse and Alcoholism, the Department of Defense (via contract with the Henry M. Jackson Foundation), the Substance Abuse and Mental Health Services Administration (via contract with ICF International), the American Foundation for Suicide Prevention, and the James B. Duke Endowment. Dr. Erkanli has received support from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Biomedical Engineering and Bioengineering. Dr. Daniel has received support from the National Institute of Mental Health, the National Institute of Child Health and Human Development, the Kate B. Reynolds Charitable Trust, the NC Department of Health and Human Services, and Centerpoint Human Services. Dr. Heilbron has received support from the National Institute on Alcohol Abuse and Alcoholism, the Department of Defense (via contract with the Henry M. Jackson Foundation), the James B. Duke Endowment, and the Marcus Foundation. Dr. Weller has received support from Pfizer, the National Institute of Mental Health, and the Department of Defense (via contract with the Henry M. Jackson Foundation). Dr. Doyle has received support from the National Institute of Mental Health and the Institute for Race and Public Policy’s Faculty Fellowship Program at the University of Illinois, Chicago.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental material cited in this article is available online.
REFERENCES
- 1.Boeninger DK, Masyn KE, Feldman BJ, Conger RD. Sex differences in developmental trends of suicide ideation, plans, and attempts among European American adolescents. Suicide Life Threat Behav. 2010;40:451–464. doi: 10.1521/suli.2010.40.5.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40:427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fish JN, Pasley K. Sexual (minority) trajectories, mental health, and alcohol use: a longitudinal study of youth as they transition to adulthood. J Youth Adolesc. 2015;44:1508–1527. doi: 10.1007/s10964-015-0280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kerr DCR, Reinke WM, Eddy JM. Trajectories of depressive symptoms and externalizing behaviors across adolescence: associations with histories of suicide attempt and ideation in early adulthood. Suicide Life Threat Behav. 2013;43:50–66. doi: 10.1111/j.1943-278X.2012.00127.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee CG, Seo D. Trajectory of suicidal ideation in relation to perceived overweight from adolescence to young adulthood in a representative United States sample. J Adolesc Health. 2013;53:712–716. doi: 10.1016/j.jadohealth.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Marshal MP, Dermody SS, Cheong J, et al. Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. J Youth Adolesc. 2013;42:1243–1256. doi: 10.1007/s10964-013-9970-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selby EA, Yen S. Six-month trajectory of suicidal ideation in adolescents with borderline personality disorder. Suicide Life Threat Behav. 2014;44:89–100. doi: 10.1111/sltb.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Czyz EK, King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. J Clin Child Adolesc Psychol. 2015;44:181–193. doi: 10.1080/15374416.2013.836454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giletta M, Prinstein MJ, Abela JRZ, Gibb BE, Barrocas AL, Hankin BL. Trajectories of suicide ideation and nonsuicidal self-injury among adolescents in mainland China: Peer predictors, joint development, and risk for suicide attempts. J Consult Clin Psychol. 2015;83:265–279. doi: 10.1037/a0038652. [DOI] [PubMed] [Google Scholar]
- 11.Musci RJ, Hart SR, Ballard ED, et al. Trajectories of suicide ideation from sixth through tenth grades in predicting suicide attempts in young adulthood in an urban African American cohort. Suicide Life Threat Behav. 2015 Sep 23; doi: 10.1111/sltb.12191. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Prinstein MJ, Nock MK, Simon V, Aikens JW, Cheah CSL, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psychol. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reuter MA, Holm KE, McGeorge CR, Conger RD. Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide Life Threat Behav. 2008;38:564–575. doi: 10.1521/suli.2008.38.5.564. [DOI] [PubMed] [Google Scholar]
- 14.Nkansah-Amankra S. Adolescent suicidal trajectories through young adulthood: prospective assessment of religiosity and psychosocial factors among a population-based sample in the United States. Suicide Life Threat Behav. 2013;43:439–459. doi: 10.1111/sltb.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, Kelley AE. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiatry. 1999;386:660–671. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Foley DL, Goldston DB, Costello EJ, Angold A. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63:1017–1024. doi: 10.1001/archpsyc.63.9.1017. [DOI] [PubMed] [Google Scholar]
- 17.Goldston DB, Daniel SS, Erkanli A, et al. Psychiatric diagonses as contemporaneous risk factors for suicide attempts among adolescents and young adults: developmental changes. J Consult Clin Psychol. 2009;77:281-190. doi: 10.1037/a0014732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 19.Molnar BE, Berkman LF, Buka SL. Psychopathology, childhood sexual abuse and other childhood adversities: relative links to subsequent suicidal behaviour in the US. Psychol Med. 2001;31:965–977. doi: 10.1017/s0033291701004329. [DOI] [PubMed] [Google Scholar]
- 20.Brent DA, Melhem NM, Oquendo M, et al. Familial pathways to early-onset suicide attempt: a 5.6 year prospective study. JAMA Psychiatry. 2015;72:160–168. doi: 10.1001/jamapsychiatry.2014.2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldston DB, Reboussin BA, Daniel SS. Predictors of suicide attempts: state and trait components. J Ab Psychol. 2006;115:842–849. doi: 10.1037/0021-843X.115.4.842. [DOI] [PubMed] [Google Scholar]
- 22.Brent DA, Oquendo M, Birmaher B, et al. Familial pathways to early-onset suicide attempt: Risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry. 2002;59:801–807. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]
- 23.Dougherty DM, Mathias CW, Marsh DM, Papageoglou TD, Swann AC, Moeller FG. Laboratory measured behavioral impulsivity relates to suicide attempt history. Suicide Life Threat Behav. 2004;34:374–385. doi: 10.1521/suli.34.4.374.53738. [DOI] [PubMed] [Google Scholar]
- 24.Goldston DB, Daniel SS, Reboussin BA, Reboussin DM, Frazier PH, Harris AE. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: a prospecive naturalistic study. J Am Acad Child Adolesc Psychiatry. 2001;40:91–99. doi: 10.1097/00004583-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Clark DC, Fawcett J. The relation of parenthood to suicide. Arch Gen Psychiatry. 1994;51:160. doi: 10.1001/archpsyc.1994.03950020084009. [DOI] [PubMed] [Google Scholar]
- 26.Hoyer G, Lund E. Suicide among women related to number of children in marriage. Arch Gen Psychiatry. 1993;50:134–137. doi: 10.1001/archpsyc.1993.01820140060006. [DOI] [PubMed] [Google Scholar]
- 27.Kleiman EM, Liu RT. Social support as a protective factor in suicide: findings from two nationally representative samples. J Affect Disord. 2013;150:540–545. doi: 10.1016/j.jad.2013.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brent DA, Oquendo M, Birmaher B, et al. Familial transmission of mood disorders: convergence and divergence with transmission of suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2004;43:1259–1266. doi: 10.1097/01.chi.0000135619.38392.78. [DOI] [PubMed] [Google Scholar]
- 29.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 30.Wenzel A, Brown GK. Cognitive therapy for suicidal patients: scientific and clinical applications. Washington, DC: American Psychological Association; 2008. [Google Scholar]
- 31.Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- 32.Weinberg A, Klonsky ED. Measurement of emotion dysregulation in adolescents. Psychol Assess. 2009;21:616–621. doi: 10.1037/a0016669. [DOI] [PubMed] [Google Scholar]
- 33.National Association of Psychiatric Health Systems. Annual survey report. Washington, DC: Author; 2002. [Google Scholar]
- 34.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, editors. Reducing suicide: A national imperative. Washington, DC: National Academies Press; 2002. Committee on Pathophysiology and Prevention of Adolescent and Adult Suicide, Board on Neuroscience and Behavioral Health, Institute of Medicine. [PubMed] [Google Scholar]
- 35.National Institute of Mental Health. The National Institute of Mental Health strategic plan. [Accessed February 4, 2016]; (MH Publication No. 08-6368). from http://www.nimh.nih.gov/about/strategic-planning-reports/nimh_strategicplanforresearch_508compliant_corrected_final_149979.pdf.
- 36.Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicide ideation and attempts: prevalence, risk factors, and clinical implications. Clin Psychol Sci Prac. 1996;3:25–46. [Google Scholar]
- 37.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): Classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164:1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Silverman MM, Berman AL, Sanddal ND, O'Carroll PW, Joiner TE. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life Threat Behav. 2007;37:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- 39.Sherrill JT, Kovacs M. Interview Schedule for Children and Adolescents (ISCA) J Am Acad Child Adolesc Psychiatry. 2000;39:67–75. doi: 10.1097/00004583-200001000-00018. [DOI] [PubMed] [Google Scholar]
- 40.Goldston DB, Daniel SS, Erkanli A, et al. Suicide attempts in a longitudinal sample of adolescents followed through adulthood: Evidence of escalation. J Consult Clin Psychol. 2015;83:253–264. doi: 10.1037/a0038657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 42.Kovacs M, Feinberg TL, Crouse-Novak MA, Paulauskas SL, Finkelstein R. Depressive disorders in childhood. I. A longitudinal prospective study of characteristics and recovery. Arch Gen Psychiatry. 1984;41:229–237. doi: 10.1001/archpsyc.1984.01790140019002. [DOI] [PubMed] [Google Scholar]
- 43.Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 44.Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- 45.Steer RA, Beck AT. Use of the Beck Depression Inventory, Hopelessness Scale, and Suicidal Intent Scale with adolescents. Advances in adolescent mental health. 1988;3:19–231. [Google Scholar]
- 46.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21:343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 47.Barratt ES, Patton JH. Impulsivity: Cognitive, behavioral, and psychophysiological correlates. In: Zuckerman M, editor. Biological bases of sensation seeking, impulsivity, and anxiety. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. pp. 77–122. [Google Scholar]
- 48.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The Family History Screen. Arch Gen Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 49.Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing yourself: The Reasons for Living Inventory. J Consult Clin Psychol. 1983;51:276–286. doi: 10.1037//0022-006x.51.2.276. [DOI] [PubMed] [Google Scholar]
- 50.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 51.Weissman MM MHS Staff. Social Adjustment Scale - Self-Report (SAS-SR) North Tonowanda, NY: Multi-Health Systems, Inc.; 1999. [Google Scholar]
- 52.Hodges K. Child and adolescent functional assessment scale (CAFAS) In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 3rd. Mahwah NJ: Lawrence Erlbaum Associates, Inc.; 2011. [Google Scholar]
- 53.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 54.Neelon B, Swamy GK, Burgette LF, Miranda ML. A Bayesian growth mixture model to examine maternal hypertension and birth outcomes. Stat Med. 2011;30:2721–2735. doi: 10.1002/sim.4291. [DOI] [PubMed] [Google Scholar]
- 55.Escobar MD, West M. Bayesian density estimation and inference using mixtures. J Am Stat Assoc. 1995;90:577–588. [Google Scholar]
- 56.Sethuraman J. A constructive definition of Dirichlet priors. Statistica Sinica. 1994;4:639–650. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.