Abstract
Background
Group exercise programs for older adults often exclude the timing and coordination of movement. Stakeholder involvement in the research process is strongly encouraged and improves the relevance and adoption of findings. We describe stakeholder involvement in the design of a clinical trial of a group-based exercise program that incorporates timing and coordination of movement into the exercises.
Methods
The study was a cluster randomized, single-blind intervention trial to compare the effects on function, disability and mobility of a standard group exercise program and the “On the Move” group exercise program in older adults residing in independent living facilities and senior apartment buildings, and attending community centers. Exercise classes were twice weekly for 12 weeks delivered by study exercise leaders and facility activity staff personnel.
Outcomes
The primary outcomes function, disability and mobility were assessed at baseline and post-intervention. Function and disability were assessed using the Late Life Function and Disability Instrument, and mobility using the Six-Minute Walk Test and gait speed.
Stakeholders
Patient and provider stakeholders had significant input into the study aims, design, sample, intervention, outcomes and operational considerations.
Summary
A community-based exercise program to improve walking can be developed to address both investigator identified missing components in current exercise to improve walking and stakeholder defined needs and interest for the activity program. Involvement of stakeholders substantially improves the relevance of research questions, increases the transparency of research activities and may accelerate the adoption of research into practice.
Keywords: stakeholders, exercise, community-based, aging, disability
Disability is a common, costly condition in older adults. Walking difficulty in older adults contributes to loss of independence, higher rates of morbidity and increased mortality.(1–5) Mobility loss is also an early predictor of other disabilities that restrict independent living.(6, 7) Compared to older adults without self-reported walking difficulty, those who developed mild walking difficulty over one year had higher healthcare costs (mean $1,128 per person). Extrapolated to the estimated 22% of older adults who develop walking difficulty annually, the cost to society is an additional 3.6 billion dollars per year.(8) Therefore, preventing or delaying the onset of walking difficulty will have a substantial impact on older adults’ independence and their healthcare costs.
Exercise is beneficial to physical and mental health, and may prevent mobility disability.(9, 10) There are many types of community-based group exercise programs available for older adults. In our experience, many of these group exercise programs are seated programs that focus on improving range of motion, strength, and endurance. Fewer group exercise programs include standing strength and balance exercises or walking for fitness.(11–13) Though most programs include some type of strength and endurance exercise, many of the programs exclude an important component of exercise that is critical to walking, the timing and coordination of movement.(14–16) Therefore, a program designed to address the timing and coordination of movement that is critical for walking may promote independence in older adults.
Based on previous research and with critical input from older adults, a novel exercise program that includes timing and coordination and focuses on improving walking was developed.(17) The program, entitled “On the Move”, differs from current group exercise programs in that 1) it contains timing and coordination exercises based on the biomechanics and motor control of walking, 2) the majority of the program consists of challenging standing and walking exercises, and 3) the exercises progress in difficulty over the course of the program. Pilot testing of “On the Move” established the initial feasibility of the program.(17)
Stakeholder involvement in research has been strongly encouraged by some and mandated by other research funding agencies such as the Patient Centered Outcomes Research Institute (PCORI). Stakeholders are “individuals or groups who are responsible for or affected by health- and healthcare-related decisions that can be informed by research evidence”.(18) The 7Ps Framework for Stakeholder Engagement suggest stakeholders can be organized into seven types: patients and the public, providers, purchasers, payers, policy makers, product makers, and principal investigators.(19) Stakeholder involvement should occur throughout the research process (i.e. in the preparation, execution and translation phases). It is thought that involvement of stakeholders may improve the relevance of research questions, increase the transparency of research activities and may accelerate the adoption of research into practice.(18) In general, reports of stakeholder engagement in the literature are minimal and vary in content and quality.(18) Therefore, as we describe the design and methods of our single-blind cluster randomized trial to establish the effectiveness and sustainability of the “On the Move” exercise program in community-dwelling older adults, we will also describe the key aspects of input and the participation of our stakeholders in the preparation and conduct of the study.
METHODS
Stakeholders
We included two main types of traditionally non-investigator stakeholders in our research: participants and providers. Stakeholders were identified through personal and professional networks, and our pilot work in the community. We identified two main provider stakeholders who are co-investigators on the project. The two provider stakeholders included 1) a representative of Senior Management from University of Pittsburgh Medical Center health system (UPMC) Senior Communities department and 2) a Lead Geriatric Outreach Nurse also from UPMC Senior Communities. We selected these two providers as they represent different levels of the provider: senior management which has influence over the staff and facilities, and also a more hands-on provider which has close connections to the community and daily interactions with various facilities and residents.
Our participant stakeholders are community-dwelling older adults who reside in Independent Living Facilities or senior housing buildings, or who live in private residences of the community and regularly attend senior community centers. Participant stakeholders were involved in the preparation phase of the study by participating in our pilot studies and focus groups to help develop the intervention. They are also involved in the execution and translation phases as members of our Community Advisory Boards (CABs) which are described below.
Community Advisory Boards (CABs). The purpose of the CABs was to provide ongoing engagement of our participant and provider stakeholders. We created two CABs, one representing the Independent Living Facilities, and another representing the senior housing buildings and senior community centers. Two separate CABs were created for logistical purposes. Our provider stakeholder co-investigators were instrumental in identifying and suggesting members of the CABs. We attempted to have a diverse representation on the CABs with the goal of including individuals representative of a variety of genders, races, types of facilities and both participants and providers (Table 1). The CABs meet twice a year throughout the study. The meetings are a two-way engagement between investigators and stakeholders to provide ongoing input into the execution and translation phases as well as to be briefed on present progress and challenges.
Table 1.
Stakeholders Participating in the Community Advisory Boards
| Independent Living Facility (ILF) Community Advisory Board | ||||
|---|---|---|---|---|
| Stakeholder Category |
Race | Gender | Age | Affiliation |
| Participant | White | Female | >65 years old | Resident in one of the northern ILFs |
| Participant | White | Male | >65 years old | Resident in one of the northern ILFs |
| Participant | White | Female | >65 years old | Retired physical education teacher and resident in one of the southern ILFs |
| Participant | White, | Female | >65 years old | Resident of one of the southern ILFs |
| Participant | White, | Female | >65 years old | Resident in one of the northern ILFs |
| Provider | White | Male | <65 years old | Fitness Director at a large ILF |
| Provider | White | Female | Executive Director of eight ILFs | |
| Provider | White | Female | <65 years old | Vice President for Sales, marketing and activities for eight ILFs (manager of activities directors) |
| Provider | White | Female | <65 years old | Activity Director at two ILFs |
| Provider | White | Female | <65 years old | Director of Independent Resident Services at an ILF |
| Senior Housing and Senior Center Community Advisory Board | ||||
| Stakeholder Category |
Race | Gender | Age | Affiliation |
| Participant | White | Female | >65 years old | Senior community center member |
| Participant | White | Female | >65 years old | Senior community center member |
| Participant | Black | Female | >65 years old | Senior community center member |
| Participant | Black | Male | >65 years old | Senior community center member |
| Participant | White | Male | >65 years old | Community member and caregiver |
| Participant | White | Female | >65 years old | Community member and caregiver |
| Provider | Black | Female | <65 years old | Social service coordinator for senior housing |
| Provider | White | Female | <65 years old | Senior Center Services Regional manager |
| Provider | White | Female | <65 years old | Nurse coordinator for the Living at Home/Staying at Home programs |
| Provider | Black | Female | <65 years old | Manager of a senior center |
| Provider | White | Female | <65 years old | Enrollment specialist for an agency that provides services at no cost to qualified older adults who wish to remain independent in their own homes |
| Provider | Black | Male | <65 years old | Social worker and a community geriatric care coordinator |
Study Design
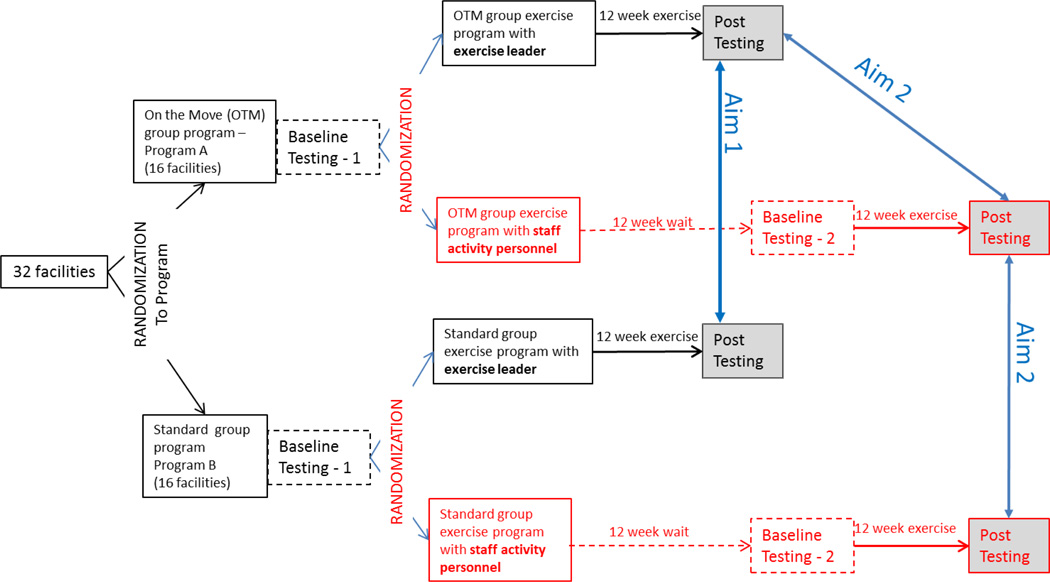
The study is a cluster randomized, single-blind intervention trial to compare the effects of a standard group exercise program and a novel “On the Move” group exercise program on function, disability and mobility in community-dwelling older adults who reside in independent living facilities (ILFs) and senior apartment buildings, and who live in private residences but regularly attend senior community centers (Figure 1). Randomization to interventions was at the facility level, stratified by facility type (ILFs, senior apartment buildings or senior community centers). Group exercise classes were twice weekly for 12 weeks, and were delivered by study exercise leaders (i.e. research staff) and facility staff activity personnel (i.e. staff employed by the facilities). Function, disability and mobility were assessed pre- and post-intervention.
Figure 1.
Study design. Black text indicates original study design, red text indicate changes made based on stakeholder input.
The sustainability of the program was examined by randomly assigning participants within each site to either class 1, taught by a study exercise leader, or class 2, taught by staff activity personnel. Study exercise leaders were research staff with training and experience in administering the exercise programs, and were exercise physiologists, physical therapists, physical therapy assistants or from a similar background. Facility staff activity personnel were employees of the facilities themselves who were involved in providing services to the residents. They could have been fitness staff, activity directors, social workers, outreach coordinators, care coordinators or other employees with a similar role. At sites that did not have staff activity personnel willing or with the availability to be trained, we identified (an) older adult(s) from the facility to be trained as a “peer” leader. Individuals randomized to class 1 exercised for the first 12 weeks at the site with the exercise leader. During class 1, the exercise leader trained the staff activity personnel or peer leader who then taught class 2 at the facility.
Rationale for Cluster Randomized Trial
We carefully considered the advantages and disadvantages of randomizing at the level of the facility and the resident. To avoid cross-contamination, it was imperative that we conduct a cluster randomize trial, and randomized facilities to exercise programs. If randomized at the resident level, participants would discuss details of their intervention and cause cross-contamination between the intervention arms. Unlike a traditional randomized clinical trial in which participants are randomized as they are being recruited, a cluster randomized trial also affords the additional benefit of examining the facility characteristics such as type (independent living/senior high rise/community center), and ensuring a balance in those characteristics is achieved by design via stratification rather than chance. Once the facilities were randomized to exercise program, we then randomized participants within each facility to delivery mode (study exercise leader/facility staff activity person or peer leader). We used the pseudo-random deviate generator in SAS® (SAS Institute, Inc., Cary, North Carolina) to randomize facilities to the two arms in a 1:1 ratio stratified by facility type; and participants within facilities to classes run by exercise leader or staff activity personnel.
Provider stakeholder input to study design
Initially, aims were limited to examining the effectiveness of the “On the Move” program using a simple two arm study design. In our pilot work, though the “On the Move” program was generally well received, we found there was a consistent complaint at the end of the pilot testing –sites and participants were sad to see the “On the Move” program come to an end. Based on this feedback, our provider stakeholders expressed interest in finding a way to sustain the “On the Move” program once the research was finished. The provider stakeholder suggested we train someone at the facilities to deliver the exercise program. Valuing the input of our stakeholders, we modified our study design and aims to include an aim examining the sustainability of the program overtime with facility staff and peer leaders. Figure 1 shows the original study design and the modified study design based on stakeholder input and Table 2 shows the initial and final modified study aims.
Table 2.
Initial study aims and final study aims based on stakeholder input.
| Aim | Initial study aims | Final study aims revised based on stakeholder input |
|---|---|---|
| 1 | Compare the effects of the “On the Move” group exercise program to a standard group exercise program on walking ability |
Compare the effects of the “On the Move” group exercise program to a standard group exercise program on self-reported function and disability and walking ability. |
| 2 |
When delivered by staff activity personnel, assess the effectiveness of “On the Move” compared to a standard program; and sustainability compared to delivery by exercise leaders. |
|
| 3 | Compare the acceptability and the risks of the “On the Move” and standard exercise programs. |
Compare the acceptability and the risks of the “On the Move” and standard exercise programs delivered by exercise leaders and staff activity personnel. |
| 4 |
Explore potential baseline predictors of benefit and risks of participation in “On the Move” program to facilitate informed patient decision making |
Participant stakeholder input into study design
Input from study participants during screening and baseline testing at the first site influenced modifications to our randomization scheme for classes within each facility. Participant couples inquired about the possibility of participating in the same class as their partner. We felt accommodating such resident preferences in our study design contributed towards study quality via potential for greater exercise adherence and participant retention. Consequently, we operationally defined a couple as two individuals who were married, living together, or dependent on each other for transportation, and stratified our randomization scheme based on whether participation was as a couple or individual persons. Inquiries about not participating in the same class (eg. estranged spouses) were neither received nor considered.
Participants
We recruited participants from independent living facilities (ILFs), senior apartment buildings, and senior community centers around the greater Pittsburgh, Pennsylvania area. To be eligible for the study, participants must: 1) be 65 years of age or older, 2) be a resident of the ILF or apartment building, or member of the senior community center, 3) ambulate independently (with or without a straight cane) for household distances, and 4) have a usual gait speed of at least 0.60 m/s. Individuals who 1) are non-English speaking, 2) have impaired cognition, defined as unable to follow a 2-step command or understand the informed consent process, 3) plan to leave the area for an extended period of time over the ensuing 4 months, 4) have a progressive neuromuscular disorder, 5) have any acute medical condition or illness that is not stable, or 6) have an inappropriate physiologic response to the 6 minute walk test (i.e. exercise hear rate ≥ 120 beats per minute, exercise systolic blood pressure ≥ 220 or a drop in systolic blood pressure > 10 mmHg, or diastolic blood pressure ≥ 110 mmHg) will be excluded. The study was approved by the University of Pittsburgh Institutional Review Board and signed informed consent was obtained from all participants. The study was registered in clinicaltrials.gov (NCT01986647).
Provider stakeholder input to participant selection
Our provider stakeholders provided valuable input on our inclusion/exclusion criteria. Because ours was to be a community-based exercise program to promote health and wellness, they wanted the criteria to be more inclusive than exclusive. If the program were to be offered at the facilities in the future, it needed to be available to the majority of the participants. On the one hand, the providers wanted to be able to offer the program to as many people as possible; but on the other hand, they were concerned about the safety of their residents. At times, the provider stakeholders raised questions as to if one program would be best for all people or we could identify which people would likely benefit from which program. Based on the discussion, we added Aim 4 (Table 2) which plans to explore potential baseline predictors of benefit and risks of participation in “On the Move” program to incorporate an informed participant decision making component into the study.
Participant stakeholder input to participant selection
Our initial pilot work was conducted in ILFs. The residents of the ILFs were mostly older (mean age 85), white and well-educated, and they did not need to leave the building in which they lived to attend the exercise class. During our focus groups at the ILFs, the participant stakeholders encouraged us to include other settings that were “different” from the ILFs. Such input reinforced our belief that we needed greater inclusion of our sample, and with the help of our provider stakeholder (i.e. lead geriatric outreach nurse), we decided to include low income housing buildings (greater diversity) and senior community centers (greater diversity and people need to travel to the center). Our provider stakeholder (i.e. Lead geriatric outreach nurse) had an established rapport with these settings and was able to facilitate access to these sites.
Interventions
Both exercise programs (“On the Move” and standard) were group-based and delivered by trained exercise leaders (primary aim) or trained staff activity personnel/peer leaders (sustainability component). The frequency and duration of the programs were identical (50 minutes, twice a week for 12 weeks) with a maximum of 10 participants in a class. The main difference between the standard and the “On the Move” group exercise programs was the program content described below.
The “On the Move” exercise program was based on principles of motor learning that enhance “skill” or smooth and automatic movement control.(20–25) The program contained a warm-up (5 minutes), stepping patterns (15 minutes), walking patterns (15 minutes), strengthening exercises (10 minutes), and cool-down exercises (5 minutes). The warm-up and cool down contained gentle range of motion exercises and stretches for the lower extremities and trunk. The stepping and walking patterns were goaloriented progressively more difficult patterns which promoted the timing and coordination of stepping, integrated with the phases of the gait cycle.(21, 22, 24, 25) The majority of the program was conducted in standing position (40 minutes) with only a small portion conducted while sitting (10 minutes). A detailed description of the On the Move exercise program can be found in Brach et al, 2016.(17)
The standard group exercise program was based on exercise programs that were currently being conducted in community-based facilities (i.e. standard group exercise). The operationally defined program contained a warm-up (5 minutes), upper and lower extremity strength exercises (20 minutes), aerobic activities (20 minutes) and a cool-down (5 minutes). The entire program was conducted while sitting (50 minutes).
Provider stakeholder input to interventions
Our provider stakeholder had approached us and inquired about potential alternatives to their exercise programming. The programs that were currently being offered were often seated programs and delivered through videos. During prior focus groups, our participant stakeholders specifically mentioned that the “On the Move” exercise program was definitely different from their experience in other exercise programs. They described “On the Move” exercise to be both physically and mentally challenging.
Participant stakeholder input to interventions
In our pilot work, which included participant stakeholder focus groups, we developed the “On the Move” program.(17) During the pilot study, the participant stakeholders provided valuable input into the intervention protocol. For example, the music to be played during exercise had been initially selected by the study team. The participants expressed a strong preference to music of their generation, and we incorporated music from the 1950s and 1960s to our intervention protocol. We believe such seemingly minor changes potentially contributed to improved exercise adherence and participant retention. Also, we worked with the provider stakeholders and the various facilities to define and operationalize the standard group exercise program so it would be consistent from site to site and be based on current practice.
Measures
Overview
The primary outcome of function and disability was the Late Life Function and Disability Instrument (LLFDI) basic lower extremity function and disability limitation domains and the primary outcomes of walking ability are Six Minute Walk Test (6MWT) and gait speed. Confidence in walking (Gait Efficacy Scale), walking performance under challenging conditions (challenging gait tasks and figure of 8 walk), and gait variability were collected as secondary outcomes of walking ability. All measures were collected at baseline prior to randomization, immediately prior to intervention in those randomized to class 2 (see Figure 1), and immediately following the 12 week intervention by research personnel who are blinded to the intervention group assignment. All testing was conducted on site at the ILFs, Senior Housing sites, or community centers.
Function and Disability
Late Life Function and Disability Instrument (LLFDI).(26, 27)
The primary function and disability outcome was the LLFDI. The LLFDI is a pair of self-report measures targeted for assessing physical function and disability in older adults with acute or chronic problems, and designed to be more sensitive to change than similar measures. The two components of the LLFDI correspond to the activity (LLFDI – function) and participation (LLFDI – disability) components of the World health Organization’s International Classification of Function, Disability and Health model. The LLFDI function component has 32 items in three domains, basic lower extremity (BLE), advance lower extremity (ALE) and upper extremity (UE) and the LLFDI disability component has 16 items representing two domains, frequency of performance and limitation in performance of life tasks. The LLFDI was selected because 1) it measures both function and disability which are critical components of independence, 2) it includes a wide variety of life tasks in various social areas thus extending beyond the traditional focus of just activities of daily living, 3) the scale was designed with sufficient breadth of items and increments of rating in order to minimize ceiling and floor effects and maximize the scale’s ability to detect change over time, and 4) it is a continuous outcome which gives us greater statistical power than a dichotomous outcome to detect change over time and make comparisons thereof. The analyses will focus on the LLFDI function and disability domain scores (i.e. BLE function, ALE function, UE function, disability frequency and disability limitation). The disability domain scores (social role, personal role, instrumental role and management role) will also be examined as secondary outcomes because they may provide insight into the impact of the disability on frequency of performance and perceived limitations.(27) The LLFDI function and disability scales have established known groups validity, and the test-retest reliability is moderate to high for the disability component (ICC=0.68–0.82) and extremely high for the function component (ICC=0.91–0.98). Scores range from 0–100; higher scores represent less difficulty and less disability.
Walking Ability
Six-Minute Walk Test (6MWT)
One of the main walking ability outcomes was the Six-Minute Walk Test (6MWT) of distance walked (meters) in six minutes, including time for rest as needed.(28) The 6MWT is 1) a performance-based measure of walking ability and walking ability is an important component of independence, 2) an indicator of community ambulation (i.e. the ability to walk 300m in 6 minutes),(29, 30) 3) a continuous outcome which gives us greater statistical power than a dichotomous outcome to detect change over time,(31) and 4) a widely used measure of mobility that is included in the NIH Patient Reported Outcomes Measurement Information System (PROMIS) project to establish measures of clinical assessment. The 6MWT has established psychometric properties, excellent test-retest reliability (Pearson r=.95) in older adults,(32, 33) construct validity for graded exercise test and functional classification.(34) A 50m change in 6MWT is considered clinically meaningful.(35)
Gait Speed
The second main walking ability outcome was gait speed. Gait speed is a strong indicator/predictor of disability, morbidity and mortality in the older adult.(2, 3, 5, 7) Gait speed is assessed in usual walking with an instrumented walkway. The instrumented walkway was 2 feet wide by 14 feet long and contained pressure sensors which detected and captured pressure data as the participant walked on the walkway. After receiving instructions, the participant completed 6 passes at their usual, self-selected walking speed. For each pass, gait speed was determined as the distance traveled (sum of all stride lengths) by the time to travel the distance (sum of all stride times). Gait speed was averaged over the 6 passes. The test-retest reliability of gait speed measured using instrumented walkways is excellent (ICC=0.98).(36) A 0.10 m/s change in gait speed is considered clinically meaningful.(35)
Additional Mobility Measures
Gait Efficacy Scale
In order to determine if changes in walking ability are associated with changes in confidence in walking, confidence was assessed using the self-reported Gait Efficacy Scale.(37–39) The items include a range of gait activities such as walking over different surfaces, up and down curbs, and negotiating stairs. Each item is scored on a 10 point Likert scale, with the total score for the 10 items ranging 0–100. A higher score represents greater confidence.
Figure of 8 Walk
The Figure of 8 Walk was designed to measure motor skill in walking.(40) The test involves walking a figure of eight pattern about two markers placed 5 feet apart. Performance was scored based on the time to complete the figure 8 walk and the number of steps. Faster and fewer steps are better.
Challenging Gait Tasks
Challenging gait tasks were used to examine an individual’s ability to adapt their gait to different environmental conditions.(41) Subjects completed two, 12-meter trials of each challenging condition, obstacle and narrow path. The time to complete each task, averaged over two trials, was the summary indicator of gait during challenging tasks. In a sample of 40 community-dwelling older adults, the one-week test re-test reliability of the timed measures was excellent (ICC=0.70–0.94). The additional time for completing each challenging walk over usual gait is the operational measure and lower marginal time is better.
Gait Variability
Gait variability, defined as fluctuations in gait characteristics from one step to the next,(42) is an important indicator of impaired mobility in older adults.(43) Gait variability was quantified using established measures of temporal and spatial gait characteristics including stance time, step length, and step width. Variability was calculated as the standard deviation of the set of steps/stances recorded over 6 passes on the instrumented walkway (described above). In general, lower variability is better although there are exceptions.(43, 44)
Satisfaction, Adherence, and Adverse Events
Satisfaction
Participant satisfaction was assessed using in-depth interviews and a satisfaction survey. In-depth phone interviews were used to assess satisfaction in a random 20% subsample. We systematically selected every 5th participant from a range of settings representing the different intervention arms (“On the Move”, Standard, exercise leader, activity staff personnel) and site types (ILF, community center and senior housing). The interview included a mixture of closed and open-ended questions. Topics included in the interviews included perceived benefits and risks, satisfaction with the program, facilities, and instructor, and amount of individualized instruction.
Satisfaction was also assessed by surveys in all participants at the conclusion of the exercise program. The satisfaction survey included five items measured on a 5-point Likert scale, six items measured on a 3-point scale (changed a lot, some or no change) and two open ended questions. The items assessed degree of satisfaction with various components of the exercise program (i.e. the exercises, safety, individualized instruction, satisfaction, and likelihood of continued participation). A series of yes/no questions were used to determine if the program met the participants’ expectations, perception of benefit from the program, and likelihood of recommending the program to others.
Adherence
A roster of participants was maintained for each class. At the beginning of each class, attendance was recorded by the instructor. Reasons for missed classes were recorded when available. Attendance rate ([number of sessions attended by the participant/total number of classes offered, i.e. 24] X100%) for each participant was the main indicator of adherence.
Adverse events
Events that occurred during testing or intervention were recorded on a clinical event form. Events included but were not limited to muscle soreness which was greater than anticipated, labored breathing, chest pain, fall or other injury. All events were forwarded to the study consulting physician (NKN) for adjudication and direction.
Participant stakeholder input to study outcomes
In the preparation phase of the study we conducted focus groups with our participant stakeholders. During the focus groups, the participant stakeholders identified maintaining independence as an important outcome. Given the time constraints of the funding (3 years) it was not feasible to use an outcome of loss of independence. Therefore, we focused on intermediate markers of independence which are outcomes of function, disability, and mobility as primary outcomes. The primary outcomes, function, disability, and walking ability are highly associated with independence and are extremely important to the older adult.(4, 7)
Sample Size
We based sample size on pilot studies,(45–47) two-tailed α=0.05 tests, an attrition rate of 10% , a class size of 10 participants, intra-cluster correlation of 0.1, published methodologies and commercially available sample size and power software (PASS 2002® Number Cruncher Statistical Systems, Kayesville, Utah), and ability to detect clinically meaningful(48) or moderate effect sizes (Cohen’s d=0.5).(49) We estimated that 90 participants per arm would allow us, with 80% statistical power, to detect statistical significance of a difference as small as 3.1 points in LLFDI overall function change between the two interventions; 80 per arm for 3.2 points in LLFDI disability frequency; 140 per arm for 0.1 m/s in gait speed; and 40 per arm for 50m in six-minute walk distance. We estimated 70 per arm receiving “On the Move” intervention would allow us, with 95% statistical power, to detect a similar difference in LLFDI overall function change between the two types of instructors; 60 per arm for LLFDI disability frequency; 110 per arm for gait speed; and 30 per arm for 6-minute walk distance. We had used 95% statistical power (rather than the customary 80%) for the sustainability hypothesis to reduce the likelihood of a type II error, thereby minimizing the chances of a finding in favor of sustainability being due to lack of statistical power rather than an actual similarity. Therefore, a total of 560 participants were deemed necessary to accommodate all primary outcomes and both Aims 1–2.
Analyses
Aim 1
We will perform all main analyses based on the intention-to-treat philosophy using the two exercise leader intervention arms. Baseline participant characteristics will be compared between the two arms. We will perform a multivariate Hotelling t-test to simultaneously compare the pre- to post-intervention change in the four primary outcomes. We will fit linear mixed models with pre- to post-intervention change in continuous outcomes as the dependent variable; intervention arm as the main fixed effect; pre-intervention value of outcome as a covariate; and a facility random effect.
Aim 2
Using all four arms, we will fit linear mixed models with pre- to post-intervention change in continuous outcomes as the dependent variable; intervention arm, delivery mode and their interaction as fixed effects; pre-intervention value of outcome as a fixed effect covariate; and a facility random effect. We will construct appropriate contrasts for testing the effectiveness and sustainability hypotheses.
Aim 3
Analyses will be similar to Aims 1–2, but to accommodate dichotomous adherence and safety outcomes we will use generalized estimating equations models with a binomial distribution, logit link function and an exchangeable working correlation structure.
Aim 4
Using only those receiving “On the Move”, we will explore the predictive association between participant baseline characteristics and outcomes of interest using logistic and multiple regression, and classification and regression tree models with proportion of explained variability (R2) and area under receiver operator characteristic curve (c) to quantify strengths of associations.
DISCUSSION
Exercise is beneficial to physical and mental health(50); however, group exercise programs have been only modestly successful in improving mobility and preventing disability in older adults. Many of the standard group exercise programs currently offered to older adults primarily focus on strength and endurance training and do not include timing and coordination exercises developed to specifically improve walking (i.e. task-specific exercises). Exercise programs which have primarily focused on addressing underlying impairments (i.e. strength and endurance) have failed to substantially impact walking, function and disability in older adults.(9, 51, 52) We aim to determine if a novel, group-based program (“On the Move”) which focuses on the timing and coordination of movements critical for walking improves mobility and prevents functional decline and disability without any increased risk to the older adult. If successful, this group exercise program would be a viable alternative for the older adult who wishes to improve mobility and prevent functional decline and disability.
One limitation of the study, is the selection of a standard seated exercise program as the comparison group. We selected the standard seated exercise program because it was often the norm at many of our intervention sites. Since we are comparing the “On the Move” program to a standard seated program, we will not be able to isolate the effects of the timing and coordination exercises from the standing and walking components of the program.
Participant and provider stakeholders played a critical role in the preparation and conduct of this study. They had significant input into the study aims, design, sample, intervention and outcomes as well as operational decisions. Though stakeholder involvement was extremely helpful to us and necessary, it is not always easy. We found it is important to involve stakeholders early in the process and to interact with them frequently. Initially, it is important to meet in-person, when able, as it is critical to building lasting relationships. We would also suggest allocating more time than estimated when meeting with stakeholders. Stakeholders typically do not want to be rushed, and when building relationships, it is important to take the time to listen and to socialize. The overarching goal is to develop genuine, lasting partnerships and a rapport. In our study, it was important to demonstrate, both by words and actions, that we valued their input, and that we were willing to listen and make changes to the study aims and design even if it increased the complexity of the study.
Though we primarily described the involvement of our stakeholders in the preparation and conduct of the study, we will also involve our stakeholders throughout the research process as we come to the completion of the study and begin analysis and dissemination activities. Through our stakeholder co-investigators and CABs we continue to include our stakeholders in the execution and translation phases of the research process. Specifically, they assist in the development of recruitment material, review study enrollment and provide suggestions to increase enrollment as needed, serve as project ambassadors and spread the word about the study, pilot test the satisfaction survey, provide interpretation of results, and provide insight on any ambiguous opinions expressed therein. We will continue to engage our stakeholders in eliciting their insight as to how best to disseminate our findings.
CONCLUSION
A community-based exercise program to improve walking can be developed to address both investigator identified missing components in current exercise to improve walking and stakeholder defined needs and interest for the activity program. The involvement of stakeholders throughout the research process (preparation, execution and translation phases) has been tremendously beneficial to the design and implementation of the clinical trial. We believe the stakeholder involvement will also improve the relevance of our research and will increase the likelihood of the adoption of our research findings into practice.
Acknowledgments
Funding: Research reported in this article was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (CE-1304-6301) and the Pittsburgh Older Americans Independence Center (NIA P30 AG024827). The statements in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Parts of this work was presented at APTA Combined Sections meeting 2016 in Anaheim, CA
REFERENCES
- 1.Guralnik J, Ferrucci L, Simonsick E, Salive M, Wallace R. Lower extremity function in persons over the age of 70 years as a predictor of subsequent disability. New Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cesari M, Kritchevsky S, Bauer D, Visser M, Rubin S, Harris T, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik J, Ferrucci L, Pieper C, Leveille S, Markides K, Ostir G, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol Med Sci. 2000;55A:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guralnik J, Simonsick E, Ferrucci L, Glynn R, Berkman L, Blazer D, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 5.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried L, Bandeen-Roche K, Chaves P, Johnson B. Preclinical Mobility Disability Predicts Incident Mobility Disability in Older Women. Journal of Gerontology. 2000;55A(1):M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 7.Perera S, Patel K, Rosano C, Rubin S, Satterfield S, Harris T, et al. Gait speed predicts incident disability: a pooled analysis. J Gerontol Med Sci. 2016;71(1):63–71. doi: 10.1093/gerona/glv126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffman J, Ciol M, Huynh M, Chan L. Estimating transitions probabilities in mobility and total costs for Medicare beneficiaries. Arch Phys Med Rehabil. 2010;91:1849–1855. doi: 10.1016/j.apmr.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LIFE S Investigators. Effects of a physical activity intervention on measures of physical performance: results of the Lifestyle Interventions and independence for elders pilot (LIFE-P) study. J Gerontol Med Sci. 2006;61A:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 10.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The life study randomized clinical trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faber M, Bosscher R, Paw MCA, Wieringen Pv. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87:885–8896. doi: 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Binder E, Schectman K, Ehsani A, Steger-May K, Brown M, Sinacore D, et al. Effects of exercise training on frailty in community-dwelling elderly adults: results of a randomized controlled trial. J Am Geriatr Soc. 2002 doi: 10.1046/j.1532-5415.2002.50601.x. in press. [DOI] [PubMed] [Google Scholar]
- 13.Sherrington C, Tiedemann A, Fairhall N, Close J, Lord S. Exercise to prevent falls in older adults: an updated metaanalysis and best practice recommendations. NSW Public Health Bulletin. 2011;22:78–83. doi: 10.1071/NB10056. [DOI] [PubMed] [Google Scholar]
- 14.Buchner D, Cress M, de LBJ, Esselman P, Margherita A, Price R, et al. A comparison of the effects of three types of endurance training on balance and other fall risk factors in older adults. Aging Clin Exp Res. 1997;9:112–119. doi: 10.1007/BF03340136. [DOI] [PubMed] [Google Scholar]
- 15.Buchner D, Cress M, de LBJ, Esselman P, Margherita A, Price R, et al. The effects of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. Journal of Gerontology: Medical Sciences. 1997;52A(4):M218–M224. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- 16.Liu C, Latham N. Progressive resistance strength training for improving physical function in older adults. Cochrane Database of Systematic Reviews. 2009;(3) doi: 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brach J, Francois S, VanSwearingen J, Gilmore S, Perera S, Studenski S. Translation of a motor learning walking rehabilitation program into a group-based exercise program for community-dwelling older adults. PMR. 2016;8:520–528. doi: 10.1016/j.pmrj.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Concannon T, Fuster M, Saunders T, Patel K, Wong J, Leslie L, et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. Journal of General Internal Medicine. 2014;29(12):1692–1701. doi: 10.1007/s11606-014-2878-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Concannon T, Meissner P, Grunbaum J, McElwee N, Guise J, Santa J, et al. A new taxonomy for stakeholder engagement in patient centered outcomes research. Journal of General Internal Medicine. 2012;27:985–991. doi: 10.1007/s11606-012-2037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson W. Physical principles for economies of skilled movements. Biol Cybernetics. 1983;46:135–147. doi: 10.1007/BF00339982. [DOI] [PubMed] [Google Scholar]
- 21.Daly J, Ruff R. Construction of efficacious gait and upper limb functional interventions based on brain plasticity evidence and model-based measures for stroke patients. The Scientific World Journal. 2007;7:2031–2045. doi: 10.1100/tsw.2007.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lay B, Sparrow W, Hughes K, O’Dwyer N. Practice effects on coordination and control, metabolic energy expenditure, and muscle activation. Human Movement Science. 2002;21:807–830. doi: 10.1016/s0167-9457(02)00166-5. [DOI] [PubMed] [Google Scholar]
- 23.Newman M, Dawes H, van d, Berg M, Wade D, Burridge J, Izadi H. Can aerobic treadmill training reduce the effort of walking and fatigue in people with multiple sclerosis: a pilot study. Multiple Sclerosis. 2007;13:113–119. doi: 10.1177/1352458506071169. [DOI] [PubMed] [Google Scholar]
- 24.Brooks V. The Neural Basis of Motor Control. New York: Oxford University Press; 1986. [Google Scholar]
- 25.Gentile A. Skill acquisition: action, movement, and neuromotor processes. In: JH C, RB S, J G, AM G, JM H, editors. Movement Sciences. 1. Rockville: Aspen Publishers; 1987. pp. 93–154. [Google Scholar]
- 26.Haley S, Jette A, Coster W, Kooyoomijian J, Levenson S, Heeren T, et al. Late life function and disability instrument:II. Development and evaluation of the function component. J Gerontol. 2002;57A:M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- 27.Jette A, Haley S, Coster W, Kooyoomijian J, Levenson S, Heeren T, et al. Late life function and disability instrument: I. Development and evaluation of the disability component. J Gerontol. 2002;57A:M209–M216. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- 28.Butland R, Pang J, Gross E, Woodcock A, Geddes D. Two-, six-, and 12-minute walking tests in reespiratory disease. BMJ. 1982;284:1607–1608. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lerner-Frankiel M, Vargas S, Brown M, Krusel L, Schoneberger W. Functional community ambulation: what are your criteria? Clinincal Management. 1986;6(2):12–15. [Google Scholar]
- 30.Robinett C, Vondran M. Functional ambulation velocity and distance requirements in rural and urban communities. Phys Ther. 1988;68(9):1371–1373. doi: 10.1093/ptj/68.9.1371. [DOI] [PubMed] [Google Scholar]
- 31.Solway S, Brooks D, Lacasse Y, Tomas S. A qualitative, systematic overview of the measurement properties of the functional walk tests used in the cardioresepiratory domain. Chest. 2001;119:256–270. doi: 10.1378/chest.119.1.256. [DOI] [PubMed] [Google Scholar]
- 32.Harada N, Chiu V, Darmon-Rodriguez J, Fowler E, Siu A, Reuben D. Screening for balance and mobility impairment in elderly individuals living in residential care facilities. Phys Ther. 1995;75(6):462–469. doi: 10.1093/ptj/75.6.462. [DOI] [PubMed] [Google Scholar]
- 33.Harada N, Chiu V, Stewart A. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–841. doi: 10.1016/s0003-9993(99)90236-8. [DOI] [PubMed] [Google Scholar]
- 34.Guyatt G, Sullivan M, Thompson P. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 35.Brach J, Studenski S, Perera S, VanSwearingen J, Newman A. Values of stance time variability related to mobility disability. J Geriatric Phys Ther. 2006;29:118. doi: 10.1519/JPT.0b013e318243e5f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brach J, Perera S, Studenski S, Newman A. Reliability and validity of measures of gait variability in community-dwelling older adults. Arch Phys Med Rehabil. 2008;89:2293–2296. doi: 10.1016/j.apmr.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McAuley E, Mihalko S, Rosengren K. Self-efficacy and balance correlates of fear of falling in the elderly. J Aging Phys Activity. 1997;5:329–340. [Google Scholar]
- 38.Rosengren K, McAuley E, Mihalko S. Gait adjustments in older adults: Activity and efficacy influences. Psychology and Aging. 1998;13:375–380. doi: 10.1037//0882-7974.13.3.375. [DOI] [PubMed] [Google Scholar]
- 39.Newell A, VanSwearingen J, Hile E, Brach J. The modified gait efficacy scale: establishing the psychometric properties in older adults. Phys Ther. 2012;92:318–328. doi: 10.2522/ptj.20110053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hess R, Brach J, Piva S, VanSwearingen J. Walking skill can be assessed in older adults: Validity of figure-of-8 walk test. Phys Ther. 2010;90:89–99. doi: 10.2522/ptj.20080121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brach J, Perera S, VanSwearingen J, Hile E, Wert D, Studenski S. Challenging gait conditions predict 1-year decline in gait speed in older adults with apparently normal gait. Phys Ther. 2011;91:1857–1864. doi: 10.2522/ptj.20100387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gabell A, Nayak U. The effect of age and variability in gait. Journal of Gerontology. 1984;39(6):662–666. doi: 10.1093/geronj/39.6.662. [DOI] [PubMed] [Google Scholar]
- 43.Brach J, Studenski S, Perera S, VanSwearingen J, Newman A. Gait variability and the risk of incident mobility disability. J Gerontol Med Sci. 2007;62A:983–988. doi: 10.1093/gerona/62.9.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brach J, Berlin J, VanSwearingen J, Newman A, Studenski S. Too much or too little step width variability is associated with a fall history in older persons who walk at or near normal gait speed. J Neuroengineering Rehabil. 2005;2(21) doi: 10.1186/1743-0003-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brach J, Lowry K, Perera S, Wert D, Hornyak V, Studenski S, et al. Improving motor control in walking: a randomized clinical trial in older adults with subclinical walking difficulty. Arch Phys Med Rehabil. 2014 doi: 10.1016/j.apmr.2014.10.018. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brach J, VanSwearingen J, Perera S, Wert D, Studenski S. Motor learning versus standard walking exercise in older adults with subclinical gait dysfunction: A randomized clinical trial. J Am Geriatr Soc. 2013;61:1879–1886. doi: 10.1111/jgs.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.VanSwearingen J, Perera S, Brach J, Cham R, Rosano C, Studenski S. A randomized trial of two forms of therapeutic activity to improve walking: effect on the energy cost of walking. J Gerontol A Biol Sci Med Sc. 2009;64A:1190–1198. doi: 10.1093/gerona/glp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Perera S, Mody S, Woodman R, Studenski S. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale: Lawrence erlbaum Associates; 1988. [Google Scholar]
- 50.Pate R, Pratt M, Blair S, Haskell W, Macera C, Bouchard C, et al. Physical activity and public health: a recommendation from the Centers of Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 51.Lord S, Lloyd D, Nirui M, Raymond J, Williams P, Stewart R. The effect of exercise on gait patterns in older women: a randomized controlled trial. J Gerontol. 1996;51A:M64–M70. doi: 10.1093/gerona/51a.2.m64. [DOI] [PubMed] [Google Scholar]
- 52.Keysor J, Brembs A. Exercise: Necessary but not sufficient for improving function and preventing disability? Curr Opin Rheumatol. 2011;23(211–218) doi: 10.1097/BOR.0b013e3283432c41. [DOI] [PubMed] [Google Scholar]