Abstract
This review article aimed to introduce a category of jaw lesions associated with impacted tooth. General search engines and specialized databases such as Google Scholar, PubMed, PubMed Central, MedLine Plus, Science Direct, Scopus, and well-recognized textbooks were used to find relevant studies using keywords such as "jaw lesion", "jaw disease", "impacted tooth", and "unerupted tooth". More than 250 articles were found, of which approximately 80 were broadly relevant to the topic. We ultimately included 47 articles that were closely related to the topic of interest. When the relevant data were compiled, the following 10 lesions were identified as having a relationship with impacted tooth: dentigerous cysts, calcifying odontogenic cysts, unicystic (mural) ameloblastomas, ameloblastomas, ameloblastic fibromas, adenomatoid odontogenic tumors, keratocystic odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibro-odontomas, and odontomas. When clinicians encounter a lesion associated with an impacted tooth, they should first consider these entities in the differential diagnosis. This will help dental practitioners make more accurate diagnoses and develop better treatment plans based on patients' radiographs.
Keywords: Jaw, Tooth Diseases, Radiography, Diagnosis
Introduction
One definition of an impacted tooth is a tooth that was prevented from erupting into the correct position due to lack of space, malposition, or other impediments.1 Subsequently, impacted teeth have been defined as those that have failed to erupt into the dental arch within the expected time frame.2 Tooth impaction is a frequent phenomenon, and the prevalence and distribution of this entity in different regions of the jaws may vary considerably.3 The third molars, maxillary canines, maxillary and mandibular premolars, and maxillary central incisors are the most commonly affected teeth.4 According to the literature, the prevalence of impacted tooth has been estimated to be between 8% and 38% in different countries,3,5,6 with a female predilection.7,8 An impacted tooth can result in carious lesions, infection, destruction of adjacent teeth, periodontal disease, and even oral and maxillofacial cysts or tumors.5 It has been found that cystic or neoplastic lesions arise in close proximity to the impacted tooth in 16% of cases, most commonly during the second and third decades of life.7
Radiography remains the first step in the diagnostic approach to jaw lesions, and the panoramic view is employed as the initial imaging technique for the evaluation of impacted teeth and related lesions.5,9
Other factors that may be associated with tooth impaction include trauma, reconstructive surgery, thickened overlying bone or soft tissue, and systemic disorders or conditions.10
Impaction can be further classified as mesioangular, distoangular, vertical, horizontal, or inverted according to the tooth angulation in relationship to the remaining dentition.10
Impacted teeth in children and adolescents are rarely associated with pathological changes, but the prevalence of problems has been found to increase in later decades. Hence, careful follow-up must be carried out as an ongoing process in patients with an impacted tooth, rather than being limited to just a few years.10
Watchful waiting throughout life, orthodontic interventions, and surgical removal are among the treatment modalities for patients with tooth impaction. If left untreated, an impacted tooth could cause tooth crowding or damage to adjacent teeth.10
Based on a review of the literature, we propose a category of 10 types of jaw lesions comprising cysts and tumors associated with impacted or unerupted teeth. When clinicians encounter a lesion in intimate association with an impacted tooth, they should first consider these entities in the differential diagnosis. This will help dental practitioners make more accurate diagnoses and develop better treatment plans based on patients' radiographs.
Materials and Methods
General search engines and specialized databases including Google Scholar, PubMed, PubMed Central, MedLine Plus, Science Direct, and Scopus, as well as well-recognized textbooks,10,11,12 were used to find relevant studies by using keywords such as "jaw lesion", "jaw disease", "impacted tooth", and "unerupted tooth". More than 250 articles were found, of which approximately 80 were broadly relevant to the topic. We ultimately included 47 articles that were closely related to the topic of interest.
When the data were compiled, the following 10 lesions were found to have a relationship with impacted teeth: dentigerous cysts, calcifying odontogenic cysts, unicystic (mural) ameloblastomas, ameloblastomas, ameloblastic fibromas, adenomatoid odontogenic tumors, keratocyst odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibro-odontomas, and odontomas (Table 1).
Table 1. General characteristics of jaw lesions associated with impacted tooth.
Results
Dentigerous cysts
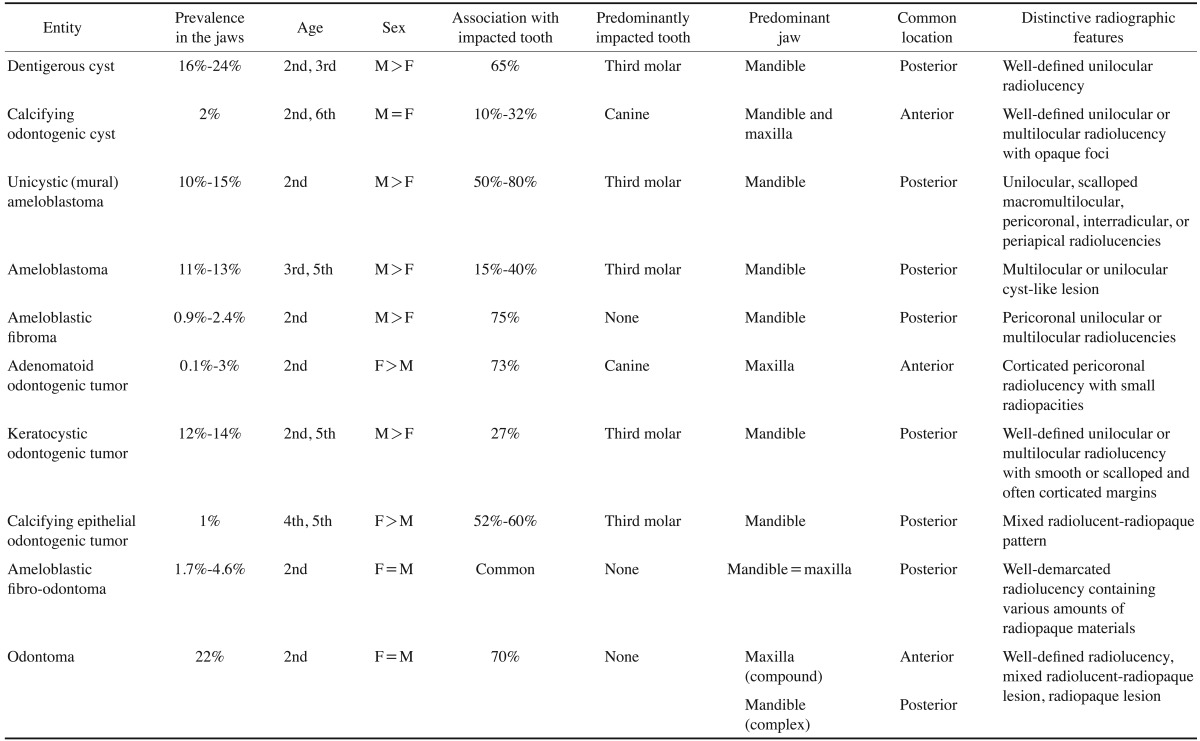
Dentigerous cysts are epithelium-lined developmental odontogenic cysts enclosing the crown of an unerupted tooth at the cementoenamel junction.10 After radicular cysts, dentigerous cysts are the second most common type of odontogenic cysts, accounting for 16% to 24% of all true cysts in the jaws.13,14 The frequency is 1.44 cysts in every 100 unerupted teeth in the general population.13 Most cases have been reported in the second and third decades of life, with a slight male predilection.10,15 Although they may occur in association with any unerupted tooth, dentigerous cysts most often involve the mandibular third molars (65%), followed by the maxillary canines, maxillary third molars, and mandibular second premolars.10 In most cases, dentigerous cysts involve the permanent dentition, but are rarely encountered in association with unerupted primary teeth, supernumerary teeth, or odontomas.10,11,12,13,16 Small lesions are usually asymptomatic, but can grow to a considerable size.10 Radiographically, dentigerous cysts typically show a well-defined unilocular radiolucent area close to the crown of an unerupted tooth (Fig. 1). The radiolucent space should be at least 3 to 4 mm in diameter.10,16 Due to its slow-growing pattern, it expands to the outer cortical boundary of the involved jaw.11 A critical diagnostic fact is that this type of cyst attaches at the cementoenamel junction.11 The relationship between dentigerous cysts and the crown of the impacted tooth shows 3 types of radiographic patterns: central, lateral, and circumferential.11,12,15 The central variety is the most common type. The lateral variety is usually associated with a mesioangular impacted mandibular third molar. In the circumferential variant, the dentigerous cyst surrounds the crown and extends for some distance along the root.11,12 Displacement of the involved tooth and root resorption of the adjacent erupted tooth have been reported.11,12 Cysts associated with the upper third molars frequently grow into the maxillary sinus, and those attached to the crown of the mandibular molars may extend into the ascending ramus.11
Fig. 1. A panoramic view demonstrates a dentigerous cyst in an adolescent enclosing the permanent right mandibular impacted canine.
Calcifying odontogenic cysts
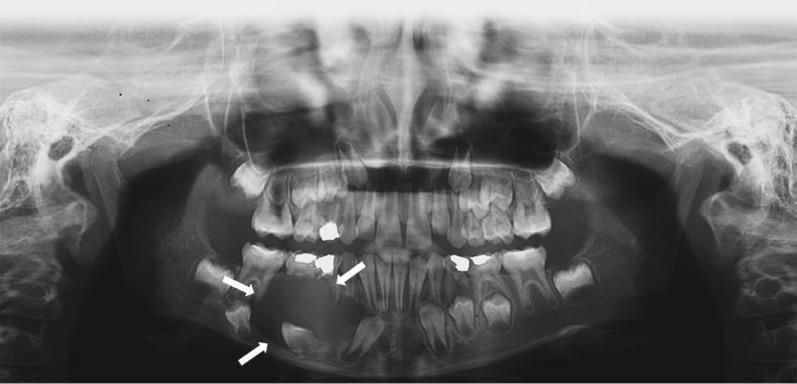
Calcifying odontogenic cysts, a type of developmental odontogenic cyst, present in intraosseous and extraosseous forms.17 They comprise 2% of all odontogenic lesions, with approximately equal frequency in both jaws.18 However, a predilection for the upper jaw has been noted in Asians, in contrast to a predilection (62%) for the lower jaw in whites.19 The age range of patients with these cysts has been reported to be between 5 to 92 years, with the peak incidence in the second and sixth decades of life.18 No sex predominance has been found in patients with calcifying odontogenic cysts.18 Approximately 65% of lesions have been found to occur near the incisors and canines. Calcifying odontogenic cysts are associated with impacted teeth (mostly canines) in 10%-32% of cases.18,20 However, in two studies by Wang et al.21 and Iida et al.,22 more than 60% of calcifying odontogenic cysts were found to be related to impacted teeth. Radiographically, calcifying odontogenic cysts appear as a well-defined unilocular or multilocular radiolucency containing small irregular calcified bodies. In addition, they may be associated with an odontoma or an unerupted tooth (Fig. 2).18 According to Iida et al.,22 adjacent teeth are most likely to show some changes such as dental impaction or displacement, which is more common in the posterior segment of the jaws. Meanwhile, root resorption of neighboring teeth has been reported with some frequency.10 The lack of these changes in anteriorly located lesions may be attributed to the chronology of calcifying odontogenic cyst development.22
Fig. 2. A calcifying odontogenic cyst associated with the right maxillary impacted third molar with dense opaque foci throughout the cystic cavity.
Unicystic ameloblastomas
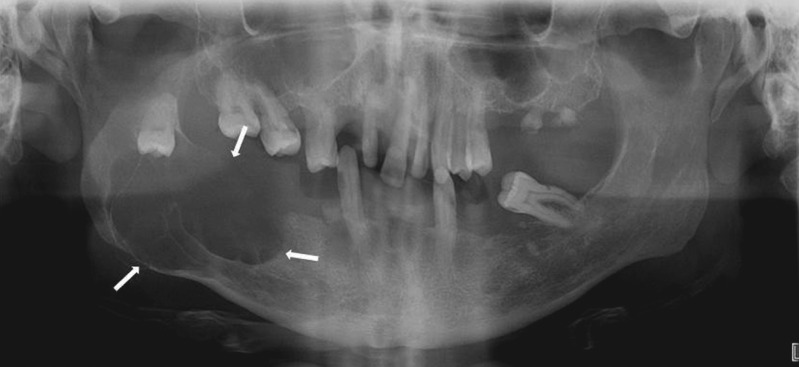
Unicystic ameloblastomas are a variant of ameloblastomas, comprising 10% to 15% of all intraosseous ameloblastomas.23 The mean age of patients is 25.5 years, with approximately 50% of cases occurring in the second decade of life.24,25 The gender distribution shows a male predilection, with a male-to-female ratio of 1.6 : 1. However, when unicystic ameloblastomas are not associated with an unerupted tooth, this ratio changes to 1 : 1.8.24 Between 50% and 80% of cases are associated with at least one unerupted tooth (mostly the third molar).23 More than 90% of lesions are found in the posterior portion of the mandible, followed by the parasymphysis region, anterior maxilla, and the posterior maxilla.23,24,25 It has also been noted that the majority of unicystic ameloblastomas are associated with dentigerous cysts, and that all such cases occurred in patients less than 30 years of age. Unicystic ameloblastomas can also arise from other cysts, such as residual, radicular, globulomaxillary, and primordial cysts.12 Unicystic ameloblastomas are usually asymptomatic, but large lesions may cause painless swelling of the jaws with facial asymmetry.24 The predominant radiographical patterns of unicystic ameloblastoma are unilocular, scalloped macromultilocular, pericoronal, interradicular, or periapical expansive radiolucencies (Fig. 3).24 Typically, they appear as a circumscribed radiolucency surrounding the crown of an unerupted mandibular third molar.10 Bone expansion, cortical perforation, and root resorption have been reported in radiographic views of unicystic ameloblastomas.24,25
Fig. 3. A panoramic view shows a unicystic ameloblastoma presenting as a unilocular radiolucent lesion associated with the right mandibular impacted third molar.
Ameloblastomas
Ameloblastomas are benign odontogenic tumors, accounting for 11% to 13% of all odontogenic tumors.12 They originate from epithelium of the enamel organ, tooth germ, and odontogenic cysts.26 The age of patients ranges from 10 to 90 years, with the peak incidence occurring in the third to fifth decades of life.27 This condition has a slight male predilection, with a male-to-female ratio of 1.3 : 1.2. More than 80% of cases occur in the mandible, with 70% arising in the molar-ramus area and the remaining 20% in the maxilla.26,27 Ameloblastomas occur in association with an impacted or unerupted tooth (mostly the mandibular third molar) in 15% to 40% of cases.28 Clinically, they are slow-growing tumors and are usually asymptomatic until they achieve a large size.27 Radiographically, ameloblastomas can be multilocular (69%) or unilocular cyst-like lesions (Fig. 4).28 The lesions vary from totally radiolucent to mixed, with the presence of coarse and curved bony septae. These septae often make soap-bubble (large compartments of variable size) or honeycomb (several small compartments) patterns.11 The margins of the lesion in the mandible are well-defined, occasionally scalloped, and frequently corticated; in contrast, in the maxilla, the margins are ill-defined because the lesion tends to grow along the bone rather than expanding it.27 Patients with ameloblastoma may exhibit root resorption, tooth displacement, bone expansion, and perforation.26,27,28
Fig. 4. A multilocular extensive ameloblastoma is found on the right aspect and ramus of the mandible in relation to an impacted molar tooth.
Ameloblastic fibromas
Ameloblastic fibromas are mixed odontogenic tumors accounting for 0.9% to 2.4% of all odontogenic tumors.29 Patients with this condition range in age from 6 years to 51 years, with a mean age of 15 years, and more than 70 % of cases occur in patients under 20 years of age. This condition has a slight male predilection.12,29,30 Ameloblastic fibromas commonly appear near the crest of the alveolar process, or in a follicular relationship with an unerupted tooth, or they may arise in an area where a tooth failed to develop.11 The majority of cases are located in the mandible, and the highest incidence is in the premolar and molar regions.12 An association between impacted teeth and the presence of ameloblastic fibromas has been documented in 75% of cases.10,29,31 Ameloblastic fibromas usually produce a painless, slow-growing expansion and displacement of the involved teeth.29 Radiographically, ameloblastic fibromas are usually seen as a well-defined, potentially corticated, pericoronal radiolucency, and may vary from a small unilocular lesion to an extensive multilocular lesion.10,29,31
Adenomatoid odontogenic tumors
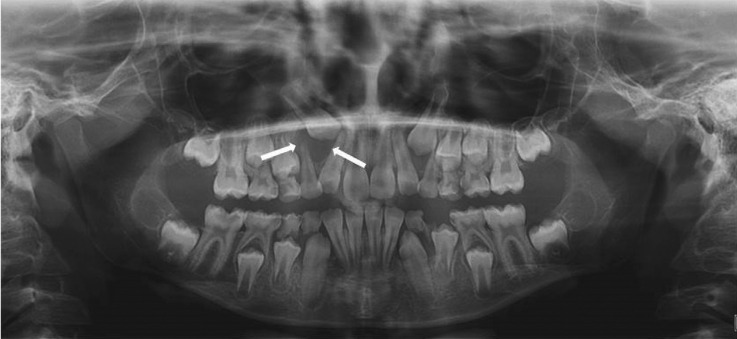
Adenomatoid odontogenic tumors are benign lesions that constitute approximately 3% of all odontogenic tumors and 0.1% of jaw tumors.32 Adenomatoid odontogenic tumors are almost twice as common in females as in males, and usually occurs in the second decade of life, with a mean age of 17 years.12 The female predilection is even more prominent in Asian populations.33 Approximately 90% of cases occur in the anterior portion of the jaws. More than 60% of adenomatoid odontogenic tumors are found in the maxilla, while 35% occur in the mandible. Of the maxillary lesions, 80% are located in the anterior region, 14% in the premolar region, and 6% in the molar region. In contrast, 70% of mandibular lesions occur in the anterior region, 27% in the premolar region, and very few in the molar region.12,33,34 According to the literature,11,12 at least 73% of adenomatoid odontogenic tumors occur in association with an impacted or unerupted tooth, most commonly maxillary canines (40% to 60% of cases), lateral incisors, and mandibular premolars.12,32,33 Adenomatoid odontogenic tumors are usually asymptomatic and do not exceed 1-3 cm in diameter.33 As the tumor enlarges, adjacent teeth may be displaced, but root resorption is rare. An adenomatoid odontogenic tumor may inhibit eruption of the involved tooth. Although some degree of jaw expansion may occur, the outer cortex is spared.11 Radiographically, in approximately 75% of cases, these tumors appear as a corticated circumscribed unilocular radiolucency surrounding an impacted tooth. In addition, internal radiopaque foci develop in two-thirds of cases (Fig. 5).10,11,12,32
Fig. 5. A panoramic view shows an adenomatoid odontogenic tumor occurring as a unilocular radiolucent lesion surrounding the crown of the right maxillary impacted permanent canine.
Keratocystic odontogenic tumors
In 2005, the World Health Organization defined odontogenic keratocysts as intraosseous tumors of odontogenic origin and recommended the term keratocystic odontogenic tumor for this entity.35,36 This type of lesion accounts for 12% to 14% of all odontogenic cysts of the jaws, with a slight male predilection.12,35 The mean age of patients is 42 years, with the peak incidence occurring in the second and fifth decades of life.35 More than 80% of tumors have been reported in the mandible, most commonly in the body (20%), angle (18%), and vertical ramus (10%). Only 16% of cases have been reported to occur in the maxilla, frequently in the posterior region. Overall, the mandible-to-maxilla ratio of these tumors is 5 : 1.35 Approximately 82% of these lesions occur in tooth-bearing areas, and roughly 27% of cases show an association with at least one impacted tooth (mostly the mandibular third molar).35,37 The most common clinical symptoms include swelling, discharge, and pain, which are reported by approximately 40% of patients.35,36 Radiographically, keratocystic odontogenic tumors demonstrate a well-defined unilocular or multilocular radiolucency with smooth or scalloped and often corticated margins. Keratocystic odontogenic tumors tend to grow in an anteroposterior direction within the jawbone without causing considerable expansion (Fig. 6). Maxillary lesions are usually smaller than mandibular lesions. Keratocystic odontogenic tumors can also present as an interradicular radiolucency, similar to lateral periodontal cysts.35,36,37 In some instances, dystrophic calcifications may develop in long-lasting cysts as small radiopacities.11
Fig. 6. An extensive keratocystic odontogenic tumor as a multilocular radiolucent lesion in the left mandibular ramus in close approximation to the impacted third molar.
Calcifying epithelial odontogenic tumors
Calcifying epithelial odontogenic tumors or Pindborg tumors are benign odontogenic tumors that account for less than 1% of all odontogenic tumors,38 with a female predilection of 1.5 : 1. In addition, the mandible is affected more commonly than the maxilla, with a mandible-to-maxilla ratio of 2 : 1 or 3 : 1.12,38,39 The age of patients ranges from 8 to 92 years, with a mean age of 37 years. The peak incidence of this lesion is in the fourth to fifth decade of life.38,39 Most cases of calcifying epithelial odontogenic tumors (52% to 60%) are associated with an impacted or unerupted tooth (mostly the mandibular third molar) or an odontoma.38,39 The highest prevalence of these lesions is in the mandibular molar region (3 times greater than in the premolar area), followed by the molar region of the maxilla and the premolar region of the mandible.12,38 These tumors usually present as a slow-growing painless mass that can lead to expansion of the jaws.12,40 The two most prevalent radiographic features of calcifying epithelial odontogenic tumor are pericoronal radiolucency, as well as radiolucent areas with diffuse opacities. A mixed radiolucent-radiopaque pattern is the most common pattern (65%), followed by radiolucent areas (32%), and radiopaque cases (3%) (Fig. 7). In addition, unilocular radiolucencies are more frequent in the maxilla than in the mandible.39 The most characteristic and pathognomonic feature is the appearance of radiopacities close to the crown of an unerupted tooth. In some cases, small, thin, opaque trabeculae may cross the radiolucency in many directions.11
Fig. 7. A calcifying epithelial odontogenic tumor is seen in the left posterior mandible as a mixed lesion with dense opaque foci associated with an impacted tooth.
Ameloblastic fibro-odontomas
Ameloblastic fibro-odontomas, which are benign mixed odontogenic tumors, account for 0.3% to 1.7% of all odontogenic tumors, but comprise 4.6% of odontogenic tumors in children.41,42 Most cases are diagnosed in patients between 9 years to 11 years of age.41 According to Chang et al.,42 ameloblastic fibro-odontomas usually occur in people younger than 20 years of age, such that age is an important factor in the differential diagnosis. Although this condition has no clearly defined sex predilection,41,43 some authors have found a slightly higher incidence in males.43,44 Ameloblastic fibro-odontomas are generally slow-growing asymptomatic tumors that are seen with equal frequency in the maxilla and mandible (mostly in the molar region).41,42 They are commonly associated with an unerupted or impacted tooth. The involved tooth is often displaced in an apical position, which indicates that the origin of the lesion is above the tooth.43 Radiographically, ameloblastic fibro-odontomas present as a well-demarcated unilocular or infrequently multilocular radiolucency containing various amounts of radiopaque material of irregular size and shape.41,43 However, in roughly 5% of cases, a minimal amount of opaque foci is present and the lesion appears completely radiolucent.10 The lesions are usually small (1-2 cm in diameter), but they can reach to a considerable size in the body of the maxilla and mandible.42 The malignant transformation of ameloblastic fibro- odontomas into ameloblastic fibrosarcoma has been reported, which can change the clinical and radiographical features of this entity.43,45
Odontomas
The term odontoma refers to any tumor of odontogenic origin; however, it specifically refers to a growth in both the epithelial and mesenchymal cells that exhibits complete differentiation. Odontomas comprise approximately 22% of odontogenic tumors of the jaws. This entity has no sex predilection and an odontoma can occur at any age, but they most commonly occur in the second decade of life.11,12,46
Overall, 67% of odontomas occur in the maxilla and 33% occur in the mandible. Compound odontomas mostly involve the anterior maxilla (61%), whereas only 34% of complex odontomas occur in this location. In contrast, complex odontomas have a predilection for the posterior jaws (59%) (Fig. 8) and, to a lesser extent, the premolar area (7%). Interestingly, both types of odontoma occur more frequently on the right side of the jaws (compound, 62%; complex, 68%).46
Fig. 8. A panoramic view shows a large complex odontoma associated with the impacted left mandibular third molar.
The neighboring teeth may be affected in 70% of cases by changes such as malformation, malposition, devitalization, aplasia, delayed eruption, and cystic transformation.47
Radiographically, odontomas exhibit 3 characteristic stages of development. In the first stage, they exhibit radiolucency due to a lack of calcification, in the intermediate stage partial calcification may be observed, and in the third stage, the lesion usually appears as radiopaque masses surrounded by radiolucent areas.12,47
Discussion
This review proposed a category of jaw lesions that occur in association with impacted tooth. This category contains 10 entities, including dentigerous cysts, calcifying odontogenic cysts, unicystic ameloblastomas, ameloblastomas, ameloblastic fibromas, adenomatoid odontogenic tumors, keratocystic odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibro-odontomas, and odontomas. The characteristics of these lesions are summarized in Table 1, with information about their overall prevalence in the jaw, age, sex, their association with impacted tooth, the predominantly involved jaw and tooth, location, and radiographic features.
Dentigerous cysts are the most common jaw lesion in this category, followed by odontomas, unicystic ameloblastomas, and keratocystic odontogenic tumors. The least commonly encountered lesions are calcifying epithelial odontogenic tumors and calcifying odontogenic cysts.
The highest frequency of association with an impacted tooth was seen for unicystic ameloblastomas, ameloblastic fibro-odontomas, adenomatoid odontogenic tumors, odontomas, and dentigerous cysts. In contrast, the lowest prevalence of such an association was observed for calcifying odontogenic cysts and keratocystic odontogenic tumors. The mandibular third molar was found to be the most commonly associated tooth for these lesions, except for adenomatoid odontogenic tumors, calcifying odontogenic cysts, and compound odontomas, for which the anterior maxillary teeth were found to be most commonly involved.
Most of these lesions occur in the second decade of life, except for calcifying epithelial odontogenic tumors, which have a peak incidence in the fourth and fifth decades of life. Meanwhile, some lesions demonstrate two peak age ranges for their incidence, one in youth and another in middle or old age, such as calcifying odontogenic cysts, ameloblastomas, keratocystic odontogenic tumors, and calcifying epithelial odontogenic tumors.
Most of the jaw lesions associated with impacted tooth appear more commonly in men; however, a significant female predilection has been found for adenomatoid odontogenic tumors and calcifying epithelial odontogenic tumors. In addition, no gender predilection has been detected for calcifying odontogenic cysts, ameloblastic fibro-odontomas, and odontomas.
Although most of these lesions tend to appear in the posterior aspect of the mandible, adenomatoid odontogenic tumors and compound odontomas frequently occur in the anterior portion of the maxilla. Moreover, no jaw predilection has been reported for calcifying odontogenic cysts and ameloblastic fibro-odontomas.
Although various radiographic features have been described in jaw lesions associated with impacted tooth, most of them first appear as unilocular radiolucencies with the potential to evolve into multilocular lesions with well-defined borders. Some lesions contain radiopaque foci within the radiolucency as well, such as calcifying odontogenic cysts, adenomatoid odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibro-odontomas, and odontomas. The presence and special patterns of radiopaque material might help clinicians differentiate among these lesions.
When clinicians encounter a lesion with an impacted tooth, they should first consider these entities in the differential diagnosis. This will help dental practitioners make more accurate diagnoses and create better treatment plans based on patients' radiographs.
Acknowledgements
The authors are greatly thankful to Dr. Abbas Shokri and Dr. Yaser Safi for providing the pictures contained in the figures.
References
- 1.Juodzbalys G, Daugela P. Mandibular third molar impaction: review of literature and a proposal of a classification. J Oral Maxillofac Res. 2013;4:e1. doi: 10.5037/jomr.2013.4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson LJ. Principles of management of impacted teeth. In: Peterson LJ, Ellis E III, Hupp JR, Tuker MR, editors. Contemporary oral and maxillofacial surgery. 3rd ed. St. Louis: Mosby-Yearbook Inc; 1998. pp. 215–248. [Google Scholar]
- 3.Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies-a radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003;9:158–163. [PubMed] [Google Scholar]
- 4.Bedoya MM, Park JH. A review of the diagnosis and management of impacted maxillary canines. J Am Dent Assoc. 2009;140:1485–1493. doi: 10.14219/jada.archive.2009.0099. [DOI] [PubMed] [Google Scholar]
- 5.Ahlqwist M, Gröndahl HG. Prevalence of impacted teeth and associated pathology in middle-aged and older Swedish women. Community Dent Oral Epidemiol. 1991;19:116–119. doi: 10.1111/j.1600-0528.1991.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 6.Hugoson A, Kugelberg CF. The prevalence of third molars in a Swedish population. An epidemiological study. Community Dent Health. 1988;5:121–138. [PubMed] [Google Scholar]
- 7.Kruger E, Thomson WM, Konthasinghe P. Third molar outcomes from age 18 to 26: findings from a population-based New Zealand longitudinal study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:150–155. doi: 10.1067/moe.2001.115461. [DOI] [PubMed] [Google Scholar]
- 8.Santosh P. Impacted mandibular third molars: review of literature and a proposal of a combined clinical and radiological classification. Ann Med Health Sci Res. 2015;5:229–234. doi: 10.4103/2141-9248.160177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mortazavi H, Baharvand M, Rahmani S, Jafari S, Parvaei P. Radiolucent rim as a possible diagnostic aid for differentiating jaw lesions. Imaging Sci Dent. 2015;45:253–261. doi: 10.5624/isd.2015.45.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neville BW, Damm DD, Allen CM, Chi AC. Oral and maxillofacial pathology. St Louis: Elsevier; 2016. pp. 632–690. [Google Scholar]
- 11.White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St Louis: Elsevier; 2014. [Google Scholar]
- 12.Wood NK, Goaz PW. Differential diagnosis of oral and maxillofacial lesions. 5th ed. St Louis: Mosby-Yearbook Inc; 1997. [Google Scholar]
- 13.Rohilla M, Namdev R, Dutta S. Dentigerous cyst containing multiple impacted teeth: a rare case report. J Indian Soc Pedod Prev Dent. 2011;29:244–247. doi: 10.4103/0970-4388.85834. [DOI] [PubMed] [Google Scholar]
- 14.Agacayak KS, Kose I, Gunes N, Bahsi E, Yaman F, Atilgan S. Dentigerous cyst with impacted canine: case report. J Int Dent Med Res. 2011;4:21–24. [Google Scholar]
- 15.Wali GG, Sridhar V, Shyla HN. A study on dentigerous cystic changes with radiographically normal impacted mandibular third molars. J Maxillofac Oral Surg. 2012;11:458–465. doi: 10.1007/s12663-011-0252-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Avril L, Lombardi T, Ailianou A, Burkhardt K, Varoquaux A, Scolozzi P, et al. Radiolucent lesions of the mandible: a pattern-based approach to diagnosis. Insights Imaging. 2014;5:85–101. doi: 10.1007/s13244-013-0298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gadipelly S, Reddy VB, Sudheer M, Kumar NV, Harsha G. Bilateral calcifying odontogenic cyst: a rare entity. J Maxillofac Oral Surg. 2015;14:826–831. doi: 10.1007/s12663-014-0706-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rastogi V, Pandilwar PK. Calcifying epithelial odontogenic cyst associated with complex odontome of maxilla. J Maxillofac Oral Surg. 2013;12:85–89. doi: 10.1007/s12663-010-0165-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rajendran R, Sivapathasundharam B. Shafer's textbook of oral pathology. 5th ed. New Delhi: Elsevier; 2006. pp. 357–432. [Google Scholar]
- 20.Shiva A, Nosrati K. A calcifying odontogenic cyst associated with complex odontoma: a case report. J Babol Univ Med Sci. 2015;17:57–61. [Google Scholar]
- 21.Wang YP, Chang YF, Wang JT, Liu BY, Sun A, Chiang CP. Characteristics of calcifying odontogenic cyst in Taiwanese. J Formos Med Assoc. 2003;102:715–721. [PubMed] [Google Scholar]
- 22.Iida S, Fukuda Y, Ueda T, Aikawa T, Arizpe JE, Okura M. Calcifying odontogenic cyst: radiologic findings in 11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:356–362. doi: 10.1016/j.tripleo.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 23.Sharma B, Balaji N, Sumathi MK, Sunitha JD. Unicystic ameloblastoma of mandible - a diagnostic dilemma. TMU J Dent. 2014;1:131–133. [Google Scholar]
- 24.Nagalaxmi V, Sangmesh M, Maloth KN, Kodangal S, Chappidi V, Goyal S. Unicystic mural ameloblastoma: an unusual case report. Case Rep Dent. 2013;2013:957418. doi: 10.1155/2013/957418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta N, Saxena S, Rathod VC, Aggarwal P. Unicystic ameloblastoma of the mandible. J Oral Maxillofac Pathol. 2011;15:228–231. doi: 10.4103/0973-029X.84511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gümgüm S, Hoşgören B. Clinical and radiologic behaviour of ameloblastoma in 4 cases. J Can Dent Assoc. 2005;71:481–484. [PubMed] [Google Scholar]
- 27.More C, Tailor M, Patel HJ, Asrani M, Thakkar K, Adalja C. Radiographic analysis of ameloblastoma: a retrospective study. Indian J Dent Res. 2012;23:698. doi: 10.4103/0970-9290.107436. [DOI] [PubMed] [Google Scholar]
- 28.Santos Tde S, Piva MR, Andrade ES, Vajgel A, Vasconcelos RJ, Martins-Filho PR. Ameloblastoma in the Northeast region of Brazil: a review of 112 cases. J Oral Maxillofac Pathol. 2014;18(Suppl 1):S66–S71. doi: 10.4103/0973-029X.141368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melo Lde A, Barros AC, Sardinha Sde C, Cerqueira A, dos Santos JN. Ameloblastic fibroma: a rare case report with 7-year follow-up. Srp Arh Celok Lek. 2015;143:190–194. doi: 10.2298/sarh1504190a. [DOI] [PubMed] [Google Scholar]
- 30.Chen Y, Li TJ, Gao Y, Yu SF. Ameloblastic fibroma and related lesions: a clinicopathologic study with reference to their nature and interrelationship. J Oral Pathol Med. 2005;34:588–595. doi: 10.1111/j.1600-0714.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- 31.JK DR, Sharma A, Sharma S, Arya V, Das R. An aggressive ameloblastic fibroma in maxilla of a 5-year-old child - reconstruction of the defect with buccal flap advancement - a conservative approach. Int J Clin Med. 2015;6:579–585. [Google Scholar]
- 32.John JB, John RR. Adenomatoid odontogenic tumor associated with dentigerous cyst in posterior maxilla: a case report and review of literature. J Oral Maxillofac Pathol. 2010;14:59–62. doi: 10.4103/0973-029X.72502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.More CB, Das S, Gupta S, Bhavsar K. Mandibular adenomatoid odontogenic tumor: radiographic and pathologic correlation. J Nat Sci Biol Med. 2013;4:457–462. doi: 10.4103/0976-9668.116965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mortazavi H, Sotoode SM, Khodadoustan A, Baharvand M. Adenomatoid odontogenic tumor: report of a rare case in terms of size and location. Int J Clin Dent. 2014;7:235–240. [Google Scholar]
- 35.Sánchez-Burgos R, González-Martín-Moro J, Pérez-Fernández E, Burgueño-García M. Clinical, radiological and therapeutic features of keratocystic odontogenic tumours: a study over a decade. J Clin Exp Dent. 2014;6:e259–e264. doi: 10.4317/jced.51408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Borgonovo AE, Bernardini L, Francinetti P, Rizza F, Re D. Odontogenic keratocyst mimicking paradental cyst. Case Rep Dent. 2014;2014:974241. doi: 10.1155/2014/974241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh M, Gupta KC. Surgical treatment of odontogenic keratocyst by enucleation. Contemp Clin Dent. 2010;1:263–267. doi: 10.4103/0976-237X.76398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deboni MC, Naclério-Homem Mda G, Pinto Junior DS, Traina AA, Cavalcanti MG. Clinical, radiological and histological features of calcifying epithelial odontogenic tumor: case report. Braz Dent J. 2006;17:171–174. doi: 10.1590/s0103-64402006000200017. [DOI] [PubMed] [Google Scholar]
- 39.Müller D, Manojlović S, Luksić I, Grgurević J. Calcifying epithelial odontogenic tumor of the maxilla (Pindborg tumor) Coll Antropol. 2012;36(Suppl 2):205–208. [PubMed] [Google Scholar]
- 40.Kaushal S, Mathur SR, Vijay M, Rustagi A. Calcifying epithelial odontogenic tumor (Pindborg tumor) without calcification: a rare entity. J Oral Maxillofac Pathol. 2012;16:110–112. doi: 10.4103/0973-029X.92985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cavalcante AS, Anbinder AL, Costa NC, Lima JR, Carvalho YR. Ameloblastic fibro-odontoma: a case report. Med Oral Patol Oral Cir Bucal. 2009;14:e650–e653. doi: 10.4317/medoral.14.e650. [DOI] [PubMed] [Google Scholar]
- 42.Chang H, Precious DS, Shimizu MS. Ameloblastic fibro-odontoma: a case report. J Can Dent Assoc. 2002;68:243–246. [PubMed] [Google Scholar]
- 43.Silva GC, Jham BC, Silva EC, Horta MC, Godinho SH, Gomez RS. Ameloblastic fibro-odontoma. Oral Oncol Extra. 2006;42:217–220. [Google Scholar]
- 44.Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenic tumors: a study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006;64:1343–1352. doi: 10.1016/j.joms.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 45.Philipsen HP, Reichart PA, Praetorius F. Mixed odontogenic tumours and odontomas. Considerations on interrelationship. Review of the literature and presentation of 134 new cases of odontomas. Oral Oncol. 1997;33:86–99. doi: 10.1016/s0964-1955(96)00067-x. [DOI] [PubMed] [Google Scholar]
- 46.Baldawa RS, Khante KC, Kalburge JV, Kasat VO. Orthodontic management of an impacted maxillary incisor due to odontoma. Contemp Clin Dent. 2011;2:37–40. doi: 10.4103/0976-237X.79312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choudhary PJ, Gharote HP, Hegde K, Gangwal P. Compound odontoma associated with impacted teeth: a case report. IJSS Case Rep Rev. 2014;1:12–15. [Google Scholar]