Abstract
Purpose
The purpose of this study was to detect the anterior loop of the mental nerve and the mandibular incisive canal in panoramic radiographs (PAN) and cone-beam computed tomography (CBCT) images, as well as to determine the anterior/mesial extension of these structures in panoramic and cross-sectional reconstructions using PAN and CBCT images.
Materials and Methods
Images (both PAN and CBCT) from 90 patients were evaluated by 2 independent observers. Detection of the anterior loop and the incisive canal were compared between PAN and CBCT. The anterior/mesial extension of these structures was compared between PAN and both cross-sectional and panoramic CBCT reconstructions.
Results
In CBCT, the anterior loop and the incisive canal were observed in 7.7% and 24.4% of the hemimandibles, respectively. In PAN, the anterior loop and the incisive canal were detected in 15% and 5.5% of cases, respectively. PAN presented more difficulties in the visualization of structures. The anterior/mesial extensions ranged from 0.0 mm to 19.0 mm on CBCT. PAN underestimated the measurements by approximately 2.0 mm.
Conclusion
CBCT appears to be a more reliable imaging modality than PAN for preoperative workups of the anterior mandible. Individual variations in the anterior/mesial extensions of the anterior loop of the mental nerve and the mandibular incisive canal mean that is not prudent to rely on a general safe zone for implant placement or bone surgery in the interforaminal region.
Keywords: Radiography, Panoramic; Cone-Beam Computed Tomography; Mandible; Anatomic Variation
Introduction
Increases in life expectancy worldwide have led to an increased demand for oral rehabilitation surgical procedures, such as implant therapies and bone grafts. Although dental implant placement in the mandibular interforaminal region is regarded as a relatively safe procedure, patients may experience sensory disturbances after surgery.1
Some anatomical structures should be carefully observed when considering surgery in the anterior mandible, such as the anterior loop of the mental nerve and the mandibular incisive canal, to avoid the risk of nerve injury and hemorrhage.1
The anterior loop is defined as an anterior/mesial extension of the mental nerve in the interforaminal region of the mandible, with a path that creates a loop before turning posterosuperiorly to exit the bone through the mental foramen.2,3,4,5,6,7,8,9
The mandibular incisive canal is a mesial extension of the mandibular canal, containing the incisive nerve and vessels, which irrigate and innervate the lower anterior teeth.10 The intraosseous pathway of the incisive canal can be a determining factor in the success of surgical procedures in the interforaminal region.11
A large number of surgical procedures are still conducted using only conventional radiographs. However, visualization of neurovascular bony canals in the mandible using 2-dimensional (2-D) radiographs may be difficult. Alternatively, cross-sectional techniques such as cone-beam computed tomography (CBCT) may provide 3-dimensional images, resulting in a more accurate preoperative examination because such techniques allow the fuller assessment of the relevant structures.9 Several studies have evaluated the prevalence of the anterior loop and incisive canal, either in direct evaluations of cadavers or in anatomical samples.4,5,6,10,12,13 Two-dimensional imaging techniques such as panoramic (PAN) and intraoral radiographs,10,11,12,13,14 have also been used to evaluate these variations, as well as CT scans.12,14,15,16,17,18,19,20,21 However, results regarding the prevalence of these structures are still contradictory, and conflicting results have also been obtained in comparisons of different imaging methods in detecting anatomical variations. The prevalence of the anterior loop has been reported to range from 28% to 71%.2,3,4,5,6,7,9,22,23 The prevalence of the incisive canal has been found to range from 15% in PAN images to as high as 93% on CT scans.11
This cross-sectional observational study aimed to assess the detection of the anterior loop and incisive canal by PAN and CBCT, and to measure and compare the anterior/mesial extension of these anatomical structures from the mental foramen in PAN and CBCT reconstructions.
Materials and Methods
The Research Ethics Committee of Piracicaba Dental School, State University of Campinas, approved this work without restrictions (Protocol 102/2012).
The sample consisted of PAN and CBCT images of 180 hemimandibles from 90 patients (56 males and 34 females; age range, 15-76 years; mean age, 26.3 years). The images had been previously taken for clinical purposes (removal of third molars and orthognathic surgeries), and retrieved from a database of the institutional imaging center. The following inclusion criteria were used: the presence of at least 8 lower teeth from the first right premolar to first left premolar, PAN and CBCT images taken within an interval of <6 months, and the absence of local or systemic osseous pathologies in the anterior mandible. PAN images with positioning errors were excluded.
PAN images were acquired with a digital charge coupled device sensor (OP100D; Instrumentarium Corp., Imaging Division, Tuusula, Finland), with an acquisition protocol of 66 kVp, 12 mA, and an exposure time of 17.6 s. CBCT images were acquired with a Classic i-CAT apparatus (Imaging Sciences International Inc., Hatfield, PA, USA), with an acquisition protocol of 120 kVp, 7 mA, an exposure time of 40 s, 0.25 mm voxels, and field of view of 16×8 cm (removal of third molars) or 16×13 cm (orthognathic surgery).
All images were evaluated on a high-resolution 19-inch monitor (LG FLATRON W1942SB, LG Electronics Inc., Seoul, Korea), at 32-bit, 60 Hz, and 1680×1050 resolution. Brightness, contrast, and zoom were manipulated freely for the best visualization of the structures of interest.
The following parameters were assessed on the PAN and CBCT images for each hemimandible: presence of the anterior loop of the mental nerve; presence of the mandibular incisive canal; and mesial extension of the anterior loop and/or incisive canal.
Visualization of the structures (anterior loop and incisive canal) was scored as present, absent, or difficult to interpret. To ensure that the findings were clinically relevant, visualization of these structures was considered positive only when the bony canal was at least 1 mm in diameter.
PAN images were analyzed on Radiocef Studio 2 software (Radio Memory, Belo Horizonte, Brazil). In order to obtain more reliable linear measurements, the magnification was estimated by taking a PAN image of 3 dry mandibles with an orthodontic wire (9 mm long and 0.7 mm thick) placed horizontally on the alveolar crest, adjacent to the mental foramen. This was performed on the same panoramic machine from which data were collected. The magnification was then estimated based on the average of 3 repeated measurements in each image. The mean horizontal magnification was 8.3%.
CBCT images were analyzed on i-CAT Vision software (Imaging Sciences International Inc., Hatfield, PA, USA). Panoramic reconstructions (CBCTp) and cross-sections (CBCTcs) were analyzed. The thickness used in CBCTcs was 0.25 mm. The thickness of CBCTp could be adjusted freely to better visualize the structures.
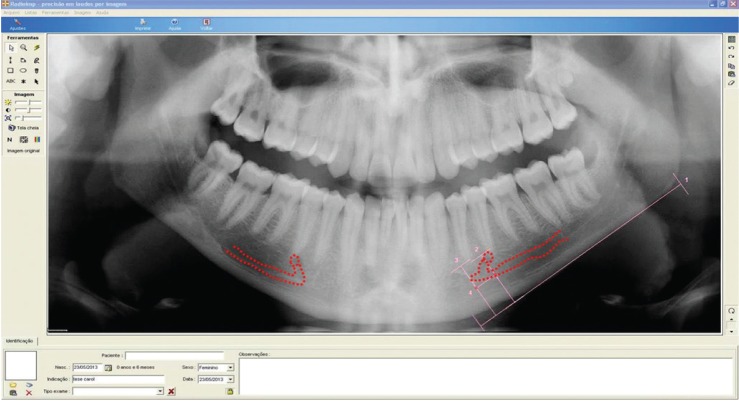
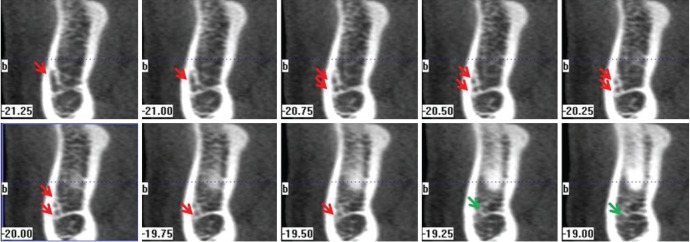
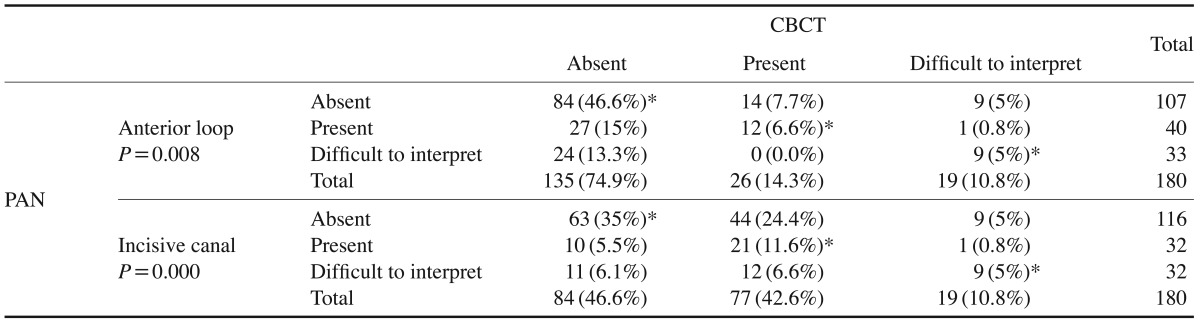
The extension of the anterior loop and incisive canal consisted of the distance between the mental foramen and the most mesial part of these structures. For PAN (Fig. 1) and CBCTp (Fig. 2), the mandibular lower cortex was used as the guiding plane. In CBCTcs (Fig. 3), measurements were obtained by counting the number of slices mesial to the mental foramen in which the structures were identifiable, based on the occlusal plane of the patient.
Fig. 1. A panoramic radiograph shows the anterior loop and incisive canal (right side) and the anterior loop (left side). 1. The lower mandibular cortex as the plane of reference. 2. The line perpendicular to the line passing through the mesial border of the mental foramen. 3. The line perpendicular to the line passing through the most mesial point of the anterior loop of the mental nerve with the mandibular incisive canal. 4. The distance between lines 2 and 3, corresponding to the mesial length of the extent of the anterior loop or incisive canal.
Fig. 2. Visualization of the anterior loop and incisive canal (red dotted line) on the panoramic reconstructions. a: The lower mandibular cortex as the plane of reference. b: The line perpendicular to the line passing through the mesial border of the mental foramen. c: The line perpendicular to the line passing through the most mesial point of the anterior loop of the mental nerve and the mandibular incisive canal. d: The distance between lines b and c, corresponding to the mesial length of the extent of the anterior loop or incisive canal.
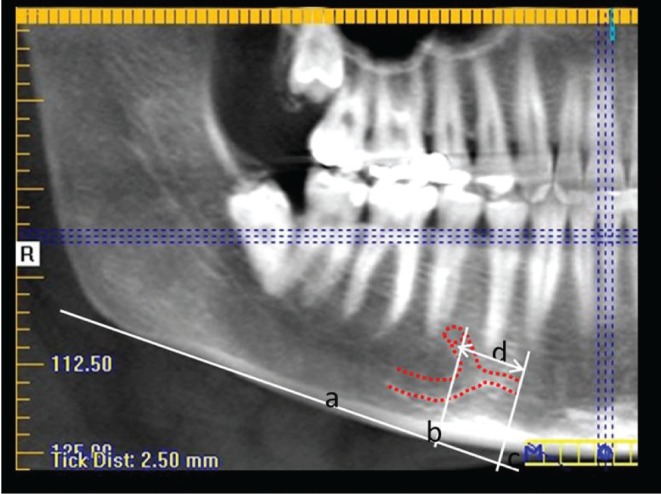
Fig. 3. Cross-sectional images (perpendicular to the occlusal plane) demonstrate the presence of the anterior loop (red arrows) and the incisive canal (green arrows).
Initially, two experienced (5 years of experience) oral radiologists who had previously undergone calibration training evaluated all images individually in a quiet, dimly lit room. All measurements were performed 3 times; the mean was considered to be the definitive measurement. In cases of disagreement between observers, the images were reassessed and a consensus was reached. One month after the first assessments, one-third of the sample (30 PANs and 30 CBCTs) was reassessed to evaluate intraobserver consistency.
The statistical analysis was performed using IBM SPSS Statistics for Windows version 22.0 (IBM Corp., Armonk, NY, USA) at the 5% significance level. Intraobserver consistency for structure visualization was determined using the kappa coefficient. Intraobserver consistency for measurements was assessed using the intraclass correlation coefficient (ICC). The McNemar-Bowker test was used to compare the accuracy of each imaging technique (PAN and CBCT) for visualization of the structures. Analysis of variance (ANOVA) with the post-hoc Tukey test was used to compare the measurements obtained using the 3 imaging methods (PAN, CBCTp, and CBCTcs). The t test was used to compare differences between the left and right sides and between genders.
Results
Intraobserver agreement for structure visualization was substantial for CBCT, ranging from 0.715 (incisive canal) to 0.802 (anterior loop), and almost perfect for PAN, ranging from 0.849 (incisive canal) to 0.878 (anterior loop), according to the interpretation of kappa presented by Landis and Koch.24 Intraobserver agreement (ICC) was excellent for both of the CBCT measures (0.971, panoramic reconstruction; and 0.931, cross-sectional reconstruction) and for the PAN measurements (0.961).
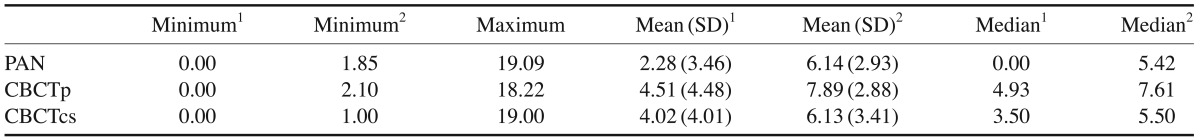
The responses of the evaluators for PAN images regarding the visualization of anatomical structures, in comparison to the results obtained for the reference standard (CBCT), are shown in Table 1. The McNemar-Bowker test indicated that the PAN images disagreed with the reference standard for both anatomical structures (P<0.05). The incisive canal was detected more frequently in CBCT images. The anterior loop was detected more frequently in the PAN images. PAN was the method that presented the highest frequency of cases scored as difficult to interpret.
Table 1. Contingency table comparing the responses obtained using panoramic radiography (PAN) and cone-beam computed tomography (CBCT) for the visualization of the anterior loop and incisive canal.
*Indicates agreement between the radiographic methods evaluated. P-values<.05 were considered to indicate statistical significance (McNemar-Bowker test).
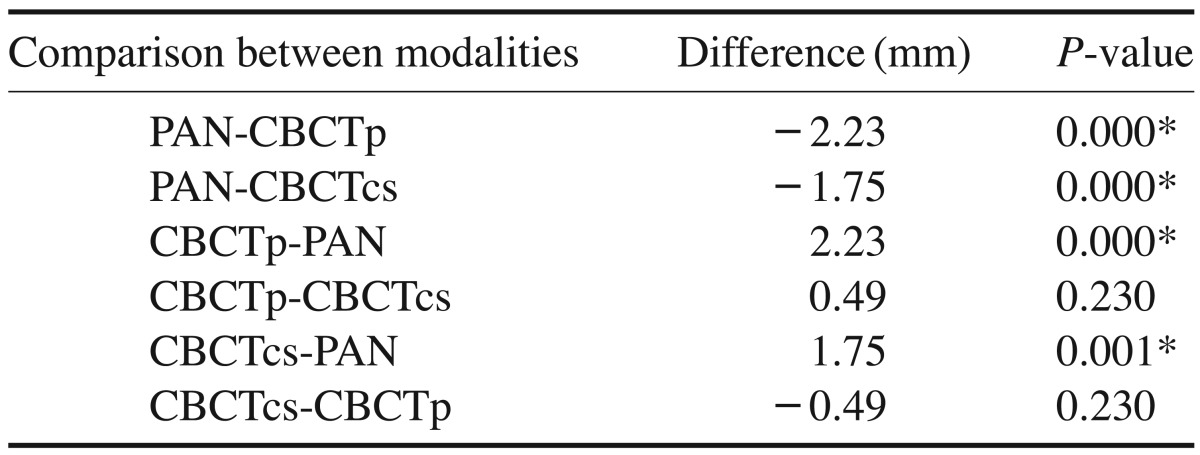
The mesial extensions of the anterior loop and incisive canal in the 3 imaging methods (PAN, CBCTp, and CBCTcs) are shown in Table 2. ANOVA using the post hoc Tukey test demonstrated that the measurements were significantly shorter in PAN images than in CBCT images (mean, 2.0 mm shorter; P<0.05) (Table 3). The difference between the two types of CBCT reconstructions was submillimetric and had no statistical significance (P>0.05).
Table 2. Minimum and maximum values, means, medians, and standard deviations, in millimeters, of the mesial length of the structures from the mental foramen in panoramic radiography (PAN), cone-beam computed tomography panoramic reconstruction (CBCTp), and cone-beam computed tomography cross-section (CBCTcs).
1All cases, including those where the anterior loop or incisive canal was not present.
2Considering only cases where the anterior loop and/or the incisive canal was present.
Table 3. Comparison among measures for the mesial length from the mental foramen in the 3 imaging modalities.
l-way ANOVA with post hoc comparisons using the Tukey test. *P<0.05
No significant difference was found in the visualization of the anterior loop of the mental nerve or the mandibular incisive canal, or according to genders or the side of the mandible. However, incisive canal detection was slightly higher for the right side in CBCT images (56%).
Discussion
Visualization of anterior loop and incisive canal
The presence and extension of the anterior loop have been reported to vary widely in the radiology literature. In the present study, the anterior loop was visualized in 7.7% of the CBCT images and 15% of the PAN images. Previous anatomical studies in cadavers and anatomical specimens reported the prevalence of the anterior loop to range from 10% to 62.7%.2,3,4,5,8,25,26 Kieser et al.'s study27 did not show the measurable anterior loop that would have any significant impact on treatment planning for implants in the anterior mandible. Benninger et al.8 considered the anterior loop to be an anomaly, rather than an anatomical finding. Rosenquist28 visualized the anterior loop directly in inferior alveolar nerve transposition operations, reporting that the loop was absent in 74.1% of the sample and, when present, it measured <1 mm. However, even though the anterior loop was found to have a low prevalence in our study, implants should not be installed close to the mental foramen without a careful evaluation.
The importance of the location of the incisive canal should be highlighted. Direct contact of an implant with this structure can lead to migration of the soft tissue around the metallic device, preventing osseointegration, and, upon reaching its neurovascular content, may cause sensory disturbances and bleeding in the region.28 The prevalence of the mandibular incisive canal ranged from 20% to 100% in previous anatomical studies.10,13 Incisive canal detection in CT scans ranged from 71.9% to 100%,14,16,17,18,19,20,21 whereas in PAN and intraoral radiographs, it ranged from 11% to 56%, depending on the degree of canal corticalization.10,11,13,14 In our study, incisive canal visualization ranged from 5.5% in PAN to 24.4% in CBCT. CBCT provides accurate linear measurements, so this imaging modality was considered to be reference standard in this study. Discrepancies observed between CBCT and PAN confirm the limitations of 2-D imaging in the assessment of the anterior loop and incisive canal, as demonstrated by the higher difficulty in detecting these structures and the underestimation of the length of the anterior loop and incisive canal. These results mean that the use of only PAN should be discouraged for surgical planning in the anterior mandible.
In the present study, although the anterior loop and incisive canal were considered isolated structures in terms of determining their presence, they were not considered separately when performing the measurements for their anterior/mesial extensions. Detecting the anterior loop and the incisive canal is a difficult task. The sample size (180 hemimandibles) may also have contributed to the low incidence of these two structures. However, the ICC for these structures was satisfactory, ranging from 0.931 to 0.971. Thus, although the difficulty in distinguishing between the anterior loop and incisive canal may have influenced the ability of the observer to detect these structures, measurements of their anterior/mesial extension from the mental foramen, which did not require such a distinction, were more reliable and reproducible.
Significant differences were found between PAN and CBCT images regarding the detection of both the anterior loop and incisive canal. Moreover, significantly more PAN images were difficult to interpret. Previous studies have shown that the interpretation of 2-D images has limitations and often results in false negatives and false positives, as well as misestimating anterior loop extension.2,3,22,26 The presence of the anterior loop was overestimated by as much as 40% in PAN images in a previous study, in which false positives were determined by dissection of the radiographed anatomical specimens.2 Image overlapping and the degree of corticalization of the bony canals are factors that may affect the visualization of structures such as the anterior loop and incisive canal.9,11
Statistically significant differences in laterality or gender were not identified with regards to the presence and length of anterior loop. However, some authors have found such structures more frequently in men,5,6,29 and suggested that visibility of the anterior loop decreases with age.7,19 For the anterior loop, no significant differences regarding its measurements were found using either imaging modality. However, there was a slightly higher (56%) detection rate of this variant on the right side on CBCT exams.
Mesial distances from the mental foramen and clinical implications
Mesial extensions from the mental foramen have been measured thoroughly to determine a safe zone for implant placement in the interforaminal region.2,3,5,6,9,22,29,30 However, an important factor to consider is the reference used to conduct the measurements. Depending on the reference plane adopted, the distances from the mental foramen are different. Uchida et al.5,6 used only the lower border of the mandible as the reference, while de Oliveira-Santos et al.9 and Couto-Filho et al.26 used two references: the lower border of the mandible (measurements performed in CBCTp) and the occlusal plane, which could be more representative of the field of vision of the surgeon during the implant placement procedure (for CBCTcs).
In this study, when cases of anterior loop and incisive canal absence were included, the mean mesial distances from the mental foramen in CBCTp and CBCTcs were similar (4.51 mm and 4.02 mm, respectively). Excluding cases where the anterior loop and incisive canal were not present, the mean measures were 7.89 mm (CBCTp) and 6.13 mm (CBCTcs). Comparing the imaging methods based on the accuracy of measurements, the difference between measurements in the two reconstruction planes was submillimetrical. We found no statistically significant difference between the imaging methods, suggesting that both methods are comparable. It is always prudent to assess all preoperative CBCT reconstructions in the anterior mandible.
PAN images underestimated the distances by a mean of 2.0 mm, which was found to be statistically significant. PAN images underestimated the presence and extent of these structures, suggesting that this 2-D imaging modality does not offer reliable information about the location of the neurovascular structures of the anterior mandible.
Some studies have suggested a safe zone for implant placement in the anterior mandible.3,30 In the present study, the overall mean mesial distance from the mental foramen, regardless of the presence and absence of the anterior loop or the incisive canal ranged from 2.28 mm in PAN to 4.51 mm in CBCT. Considering only cases where the anterior loop and incisive canal were present, the mean distance was approximately 8 mm. Our results were indicative of considerable anatomical variability, as distances from the mental foramen reached up to 20 mm (2.0 cm). Couto-Filho et al.,26 evaluating only the anterior loop, obtained mesial measures of the mental foramen similar to those obtained this study. This variability could be related to the incisive canal, a structure not evaluated in the previous study by Couto-Filho et al.26 Due to these discrepancies, it is recommended that all surgical cases involving the anterior mandible be assessed individually rather than relying on averages.
Considering the previously known limitations of 2-D imaging, as well as the discrepancies observed between PAN and CBCT in visualization and measurements of the extension of the anterior loop of the mental nerve and the mandibular incisive canal, CBCT is the best choice as an imaging method for preoperative planning for procedures involving the anterior mandible. Moreover, the considerable individual variation for measurements obtained from both imaging methods (PAN and CBCT) shows that it is not prudent to rely on a general safe zone for implant placement or bone surgery in the interforaminal region.
References
- 1.Liang X, Lambrichts I, Corpas L, Politis C, Vrielinck L, Ma GW, et al. Neurovascular disturbance associated with implant placement in the anterior mandibular and its surgical implications: literature review including report of a case. Chin J Dent Res. 2008;11:56–64. [Google Scholar]
- 2.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anterior loop of the mental canal: an anatomical-radiologic study. Implant Dent. 2000;9:120–125. doi: 10.1097/00008505-200009020-00003. [DOI] [PubMed] [Google Scholar]
- 3.Kuzmanovic DV, Payne AG, Kieser JA, Dias GJ. Anterior loop of the mental nerve: a morphological and radiographic study. Clin Oral Implants Res. 2003;14:464–471. doi: 10.1034/j.1600-0501.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 4.Hu KS, Yun HS, Hur MS, Kwon HJ, Abe S, Kim HJ. Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg. 2007;65:2288–2294. doi: 10.1016/j.joms.2007.06.658. [DOI] [PubMed] [Google Scholar]
- 5.Uchida Y, Yamashita Y, Goto M, Hanihara T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region. J Oral Maxillofac Surg. 2007;65:1772–1779. doi: 10.1016/j.joms.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–750. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 7.Ngeow WC, Dionysius DD, Ishak H, Nambiar P. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–237. doi: 10.2334/josnusd.51.231. [DOI] [PubMed] [Google Scholar]
- 8.Benninger B, Miller D, Maharathi A, Carter W. Dental implant placement investigation: is the anterior loop of the mental nerve clinically relevant? J Oral Maxillofac Surg. 2011;69:182–185. doi: 10.1016/j.joms.2010.07.060. [DOI] [PubMed] [Google Scholar]
- 9.de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16:387–393. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 10.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anatomic and radiologic course of the mandibular incisive canal. Surg Radiol Anat. 2000;22:157–161. doi: 10.1007/s00276-000-0157-5. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26:329–333. doi: 10.1007/s00276-004-0242-2. [DOI] [PubMed] [Google Scholar]
- 12.Mraiwa N, Jacobs R, Moerman P, Lambrichts I, van Steenberghe D, Quirynen M. Presence and course of the incisive canal in the human mandibular interforaminal region: two-dimensional imaging versus anatomical observations. Surg Radiol Anat. 2003;25:416–423. doi: 10.1007/s00276-003-0152-8. [DOI] [PubMed] [Google Scholar]
- 13.Jalili MR, Esmaeelinejad M, Bayat M, Aghdasi MM. Appearance of anatomical structures of mandible on panoramic radiographs in Iranian population. Acta Odontol Scand. 2012;70:384–389. doi: 10.3109/00016357.2011.629625. [DOI] [PubMed] [Google Scholar]
- 14.Pires CA, Bissada NF, Becker JJ, Kanawati A, Landers MA. Mandibular incisive canal: cone beam computed tomography. Clin Implant Dent Relat Res. 2012;14:67–73. doi: 10.1111/j.1708-8208.2009.00228.x. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs R, Mraiwa N, vanSteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofac Radiol. 2002;31:322–327. doi: 10.1038/sj.dmfr.4600719. [DOI] [PubMed] [Google Scholar]
- 16.Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, van der Stelt PF. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using conebeam computed tomography. Clin Oral Implants Res. 2010;21:766–771. doi: 10.1111/j.1600-0501.2009.01903.x. [DOI] [PubMed] [Google Scholar]
- 17.Sokhn S, Nasseh I, Noujeim M. Using cone beam computed tomography to determine safe regions for implant placement. Gen Dent. 2011;59:e72–e77. [PubMed] [Google Scholar]
- 18.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:e420–e425. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kajan ZD, Salari A. Presence and course of the mandibular incisive canal and presence of the anterior loop in cone beam computed tomography images of an Iranian population. Oral Radiol. 2012;28:55–61. [Google Scholar]
- 20.Apostolakis D, Brown JE. The dimensions of the mandibular incisive canal and its spatial relationship to various anatomical landmarks of the mandible: a study using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:117–124. doi: 10.11607/jomi.2372. [DOI] [PubMed] [Google Scholar]
- 21.Al-Ani O, Nambiar P, Ha KO, Ngeow WC. Safe zone for bone harvesting from the interforaminal region of the mandible. Clin Oral Implants Res. 2013;24(Suppl A100):115–121. doi: 10.1111/j.1600-0501.2011.02393.x. [DOI] [PubMed] [Google Scholar]
- 22.Kaya Y, Sencimen M, Sahin S, Okcu KM, Dogan N, Bahcecitapar M. Retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–925. [PubMed] [Google Scholar]
- 23.Kilic C, Kamburoğlu K, Ozen T, Balcioglu HA, Kurt B, Kutoglu T, et al. The position of the mandibular canal and histologic feature of the inferior alveolar nerve. Clin Anat. 2010;23:34–42. doi: 10.1002/ca.20889. [DOI] [PubMed] [Google Scholar]
- 24.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 25.Liang X, Jacobs R, Corpas LS, Semal P, Lambrichts I. Chronologic and geographic variability of neurovascular structures in the human mandible. Forensic Sci Int. 2009;190:24–32. doi: 10.1016/j.forsciint.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Couto-Filho CE, Moraes PH, Alonso MB, Haiter-Neto F, Olate S, Albergaria-Barbora JR. Accuracy in the diagnosis of the mental nerve loop. A comarative study between panoramic radiography and cone beam computed tomography. Int J Morphol. 2015;33:327–332. doi: 10.4067/S0717-95022015000100051. [DOI] [PubMed] [Google Scholar]
- 27.Kieser J, Kuzmanovic D, Payne A, Dennison J, Herbison P. Patterns of emergence of the human mental nerve. Arch Oral Biol. 2002;47:743–747. doi: 10.1016/s0003-9969(02)00067-5. [DOI] [PubMed] [Google Scholar]
- 28.Rosenquist B. Is there an anterior loop of the inferior alveolar nerve? Int J Periodontics Restorative Dent. 1996;16:40–45. [PubMed] [Google Scholar]
- 29.Rosa MB, Sotto-Maior BS, Machado Vde C, Francischone CE. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:388–392. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 30.Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23:1022–1030. doi: 10.1111/j.1600-0501.2011.02261.x. [DOI] [PubMed] [Google Scholar]